Abstract
Background
Emergency department (ED) crowding causes increased patient morbidity and mortality. ED occupancy rate (OR; patients by treatment beds) is a common measure of crowding, but the comparability of ORs between EDs is unknown. The objective of this investigation was to investigate differences in ORs between EDs using staff‐perceived workload as reference.
Methods
This was a national cross‐sectional study in Sweden. EDs provided data on census, treatment beds, staffing, and workload (1–6) at 5 time points. A baseline patient turnover was calculated as the average daily census by treatment beds, denoted turnover per treatment bed (TTB), for each ED. A census ratio (CR), current by daily census, was calculated to adjust for differences in the number of treatment beds.
Results
Data were returned from 37 (51%) EDs. TTB varied considerably (mean = 4, standard deviation = 1.6; range, 2.1–9.2), and the OR was higher in EDs with TTB >4 compared with ≤4, 0.86 versus 0.43 (0.43; 95% confidence interval [CI], 0.27–0.59), but not workload, 2.75 versus 2.52 (0.23; 95% CI, −0.19 to 0.64). After adjusting for confounders, both TTB (k = −0.3; 95% CI, −0.49 to −0.14) and OR (k = 3.4; 95% CI, 1.76–5.03) affected workload. Correlation with workload was better for CR than for OR (r = 0.75 vs 0.60, respectively).
Conclusion
OR is affected by patient‐to‐treatment bed ratios that differ significantly between EDs and should be accounted for when measuring crowding. CR is not affected by baseline treatment beds and is a better comparable measure of crowding compared with OR in this national comparator study.
Keywords: crowding, emergency department, health policy, occupancy rate, overcrowding, workload
1. INTRODUCTION
1.1. Background
Emergency department (ED) crowding occurs when resources do not match the demand for care and has been shown to increase morbidity and mortality and decrease the quality of ED care. 1 , 2 , 3 , 4 There is no consensus on how to measure ED crowding, but several metrics have been suggested and shown to be associated with decreased quality of care. 4 Occupancy rate (OR), that is, the number of patients in the ED divided by the number of treatment beds, is one of the most widely used measures of crowding because of its face validity and ease of use. 1 , 5 Because of this, it has been promoted over other more complex measures with similar ability to identify crowding. 4 , 6 An OR above 1.0, indicating more patients than treatment beds at a given time, is generally used as a marker of crowding. 6 , 7 However, such a fixed cutoff assumes that different EDs are affected similarly by a change in OR that, among other things, requires that the number of treatment beds in relation to the census of patients are comparable between EDs. These potential differences in endogenous ED factors was one of the reasons why less emphasis was put on volume and census measures at the 2014 benchmarking summit. 8 To our knowledge, differences in census to treatment bed ratios have not been investigated, and neither is there a regulated minimum ratio for the number of treatment beds in the ED. In addition, there are several different operational models for EDs, such as fast‐track, 9 rapid assessment zones, 10 and vertical split flow, 11 which use ED space and treatment beds differently.
1.2. Importance
With no legislated minimum number of beds and different operational models, the comparability of crude OR as a measure of crowding between EDs is unclear. A staff‐perceived crowding measure might not suffer from this limitation because it can be assumed to be relative to the normal state at each ED. Staff perception has been used as a reference for crowding in several previous studies with consistent results. 12 , 13 , 14 Our hypothesis was that baseline differences in the number of treatment beds in relation to daily census lead to differences in OR between EDs, which could make crude OR a less reliable crowding measure.
1.3. Goals of this investigation
In the present study, we aimed to investigate how the number of treatment beds differ in Swedish EDs and how this affects crowding estimated by OR compared with the staff perception of crowding.
The Bottom Line.
Current emergency department crowding measures do not always reflect staff‐perceived workload, partly because of differences in the numbers of beds. Looking at 37 Swedish hospitals, census ratio (current/daily census) correlated better with workload than simple occupancy rate (current patients/treatment beds).
2. METHODS
2.1. Study design and data collection
As described previously, 15 we conducted a cross‐sectional, multicenter study for 24 hours on April 25, 2018. All Swedish EDs listed in the national healthcare institution registry (HSA) were offered to participate by written invitation (e‐mail) to the officially listed head of department. The written invitation was followed by a telephone call, and participation was confirmed in writing by the department head. During the 24‐hour period, each ED collected data at 5 prespecified time points (12:00 AM, 6:00 AM, 12:00 PM, 6:00 PM, and 11:59 PM). Data at each time point included the number of registered patients at the ED, staff workload, and number of ED nurses and physicians. Sampling time points were spread out during the day to allow for temporal differences in ED attendances, working shift and different assessors. One senior staff did the workload assessment at each ED and time point and have previously shown to be a valid approximation of workload. 14 We did not collect data on scheduling models but collected data on healthcare staff to account for different scheduling models. Each ED also provided information on the annual and average daily census in the previous year (2017) and the number of treatment beds. Data were recorded on a paper report form by a senior staff member and subsequently submitted in a digital form to the study coordinator. This study was carried out in accordance with the Declaration of Helsinki. 16 This study was approved for all sites by the regional ethics review board in Linköping, Sweden (permit reference: 2018/50‐31). Informed consent was waived because no identifiable personal data were collected.
2.2. Definition of data
We defined OR according to McCarthy et al 6 as the number of patients divided by the number of beds where basic care could be provided, excluding corridor spaces. Physicians were defined as any intern, resident, or attending staffing the ED. Workload was assessed by staff on a graded Likert scale with anchors from 1 (very low workload) to 6 (very high workload) and used as a reference standard for crowding. 14 EDs were classified by their hospital status (academic, community, and rural) in Sweden, where academic centers are the only centers with tertiary, highly specialized care within neurosurgery, cardiothoracic surgery, transplantations, and advanced burn care. To assess baseline differences in treatment beds between EDs, we calculated turnover per treatment bed (TTB) for each ED by dividing the average daily census with the current number of treatment beds in the ED. We dichotomized EDs to above and below the mean TTB to investigate its impact on OR and workload. In a post hoc analysis, we hypothesized that the census ratio (CR), defined as the number of present patients divided by the daily census, may differ less between EDs because it removes the baseline differences in the number of ED beds.
2.3. Statistical analysis
Annual census is reported as a median with interquartile range (IQR). OR and workload are reported as means with standard deviations (SDs). Correlation is assessed using linear regression and reported as Pearson's correlation coefficient (r). The workload assessment is treated as a continuous scale in the regression analysis because previous research by our group has indicated that research participants treat it as a continuous scale with internally and externally replicable results. 14 , 17 , 18 A similar methodology has been used for the National Emergency Department Overcrowding Study with comparable, replicable results. 19 , 20 , 21 Mixed model linear regression, using the restricted maximum likelihood function, was used to test the effects of TTB on OR with additional fixed effects and hospital type, hospital size, staff‐to‐patient ratio, and ED as random effect variables. The effects of OR and TTB on assessed workload were investigated similarly. There was evidence that TTB affected the association between workload and OR in a linear regression model. To test if this effect was relative to the value of TTB, an interaction variable was created as OR × TTB and added as a variable to the model. The results of the regression analysis are reported as coefficients with 95% confidence interval (CIs) and P values with and without adjustment for multiple comparisons according to Holm. 22 A P value below 0.05 with a 95% CI not crossing 1.0 was defined as statistically significant. Only EDs that reported complete data at all time points were included in the analysis. Confounding was assessed in the mixed models linear regression analyses by adjusting for time point, hospital type, hospital size, and staff‐to‐patient ratios. Assessment at 06:00 was used as a reference for the time point variable, and for hospital type, rural hospital was used as reference.
Data were imported from comma‐separated text files submitted by participating EDs into Pandas data frames (version 0.23.4; https://pandas.pydata.org/) 23 and analyzed with computer scripts in the Python programming language (version 3.7.2; https://www.python.org) using the scipy scientific library (version 1.1; https://www.scipy.org/) 24 , 25 and statsmodels (version 0.10; https://www.statsmodels.org) 26 for statistical calculations.
3. RESULTS
Complete data were returned from 37 EDs (51%, n = 72). Of 7 university hospitals with tertiary care, 5 (75%) reported data, and the geographical distribution of EDs was representative of the population as reported previously. 15 The median census was 37807 (IQR, 22221–53851). Average OR was 0.6 (SD = 0.5), with a mean assessed workload of 2.6 (SD = 1.3). Both workload and OR showed a diurnal variation with a nadir at 6:00 AM and peak at 6:00 PM (Table 1).
TABLE 1.
Mean workload and OR at each time point
| Time point | Workload (SD) | OR (SD) |
|---|---|---|
| 12:00 AM | 2.7 (1.3) | 0.6 (0.4) |
| 6:00 AM | 1.3 (0.6) | 0.2 (0.1) |
| 12:00 PM | 3.0 (1.0) | 0.8 (0.3) |
| 6:00 PM | 3.2 (1.1) | 1.0 (0.6) |
| 11:59 PM | 2.9 (1.2) | 0.6 (0.4) |
Abbreviations: OR, occupancy rate; SD, standard deviation.
Figure 1 shows that the correlation between the 2 crowding measures workload and OR was moderate (r = 0.61). At similar ORs, staff in EDs with high baseline patient flow generally (gray to red color) seemed to perceive a lower workload compared with EDs with low baseline patient flow (blue to gray color).
FIGURE 1.
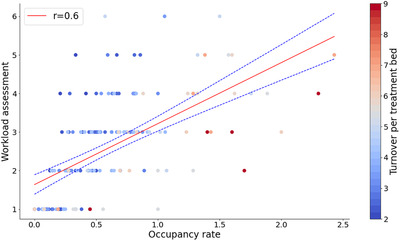
Correlation between occupancy rate and assessed workload with colors indicating baseline patient flow measured as patient turnover per treatment bed. Dashed line denotes the 95% confidence interval for the correlation
The average baseline patient turnover (TTB) was 4 (SD = 1.6; range, 2.1–9.2) patients per treatment bed per day. The mean OR was significantly higher in EDs with high TTB (>4) compared with low TTB (≤4), 0.86 versus 0.43 (difference, 0.43; 95% CI, 0.27–0.59; P < 0.001), but there was no significant difference in mean assessed workload between the 2 groups: 2.75 versus 2.52 (difference, 0.23; 95% CI, −0.19 to 0.64; P = 0.22). In a mixed model linear regression, the nurse‐to‐patient ratio and TTB significantly influenced OR when adjusting for ED size, hospital type, average length of stay, and patient‐to‐physician ratio (Table 2).
TABLE 2.
Result of the mixed model linear regression model, indicating the measured variables affects occupancy rate
| Coefficient (95% CI) | P value | Adjusted P value a | |
|---|---|---|---|
| Hospital type | |||
| Community | 0.07 (−0.09 to 0.22) | 0.41 | 1.00 |
| Academic | 0.02 (−0.15 to 0.20) | 0.80 | 1.00 |
| Patients per staff | |||
| Nurses | 0.20 (0.16 to 0.25) | <0.01 | <0.01 |
| Physicians | 0.00 (−0.03 to 0.03) | 0.83 | 1.00 |
| Metrics | |||
| TTB | 0.15 (0.12 to 0.18) | <0.01 | <0.01 |
| Length of stay | 0.00 (0.00 to 0.00) | 0.11 | 1.00 |
| Census | 0.00 (−0.00 to 0.00) | 0.72 | 1.00 |
| Intercept | −0.28 (−0.53 to −0.02) | 0.04 | 0.24 |
| Random effects | 0.02 (−0.13 to 0.17) | 0.80 | 1.00 |
Abbreviations: CI, confidence interval; TTB, turnover per treatment bed.
Adjustment according to Holm. 22
The correlation between workload and OR improved when splitting the data set based on high (TTB >4) versus low (TTB ≤4) baseline patient turnover, with r = 0.66 and r = 0.73, respectively. When adjusting OR levels by baseline patient turnover (OR/TTB), the correlation with workload in the whole data set improved considerably (r = 0.75). This may be further simplified as suggested in Equation (1) to yield a CR. The correlation between census and treatment beds was good (r = 0.77). Following is how to simplify and calculate the CR:
| (1) |
where Np = number of patients, Nb = number of treatment beds, and up = average daily census
Table 3 shows that in a mixed model linear regression, OR and TTB (measured by the interaction variable) significantly affected the assessed workload. The coefficient of the interaction between OR and TTB was −0.3 (95% CI, −0.49 to −0.14; P < 0.001), suggesting that under similar conditions, staff at EDs with high baseline patient turnover assessed workload lower at similar OR compared with EDs with lower baseline patient turnover. This association remained statistically significant when correcting for multiple comparisons according to Holm. 22
TABLE 3.
Mixed model linear regression on staff‐assessed workload with coefficients and 95% confidence intervals (CIs) for each variable
| Coefficient (95% CI) | P value | Adjusted P value a | |
|---|---|---|---|
| Time point | |||
| 12:00 AM | 0.38 (−0.05 to 0.8) | 0.08 | 0.66 |
| 12:00 PM | 0.29 (−0.24 to 0.81) | 0.28 | 1.00 |
| 6:00 PM | 0.28 (−0.27 to 0.84) | 0.32 | 1.00 |
| 11:59 PM | 0.55 (0.11 to 1) | 0.02 | 0.15 |
| Hospital type | |||
| Community | 0.27 (−0.26 to 0.81) | 0.32 | 1.00 |
| Academic | 0.1 (−0.58 to 0.77) | 0.78 | 1.00 |
| Patients per staff | |||
| Nurse | 0.1 (−0.1 to 0.3) | 0.35 | 1.00 |
| Physician | 0.01 (−0.09 to 0.1) | 0.85 | 1.00 |
| Occupancy | |||
| OR | 3.4 (1.76 to 5.03) | <0.01 | <0.01 |
| TTB >4 | −0.26 (−0.82 to 0.29) | 0.35 | 1.00 |
| Interaction (OR × TTB) | −0.3 (−0.48 to −0.12) | <0.01 | 0.01 |
| Intercept | 0.84 (0.42 to 1.26) | 0.00 | 0.00 |
| Random effects | 0.48 (0.06 to 0.89) | 0.02 | 0.22 |
Abbreviations: OR, occupancy rate; TTB, turnover per treatment bed.
Adjustment according to Holm. 22
4. LIMITATIONS
The response rate among the invited EDs was only 50%, which limits the generalizability of the results. We believe that this was somewhat mitigated by the diversity in geographical location and size and type of the participating EDs, making them reasonably lurepresentative of the healthcare system in Sweden. The study was conducted during a single day in the spring, and seasonal differences could therefore not be analyzed. 27 Several studies have found seasonal variation in specific populations in the ED 28 , 29 ; however, the importance of seasonal variation on crowding is uncertain. 30 , 31 , 32 We were unable to adjust for patient case mix at each time point, which may influence staff assessments of workload. Furthermore, the assessment of workload was made by 1 senior staff member at each ED, which may limit the generalizability to all staff. It was not possible to ask all working staff at each time point, and previous work by our group indicates that assessments by senior staff have similar predictive values as the average assessments of all staff. 14
We used workload as the reference standard for crowding in this study because of its potential to incorporate many contributing factors of crowding. When evaluating crowding operationally, any 1 measure of crowding should not be used in isolation but in conjunction with other operational metrics.
5. DISCUSSION
In this national cross‐sectional study, we found considerable differences in baseline patient turnover, measured as TTB, between EDs, and this affects OR but not staff‐assessed workload. EDs with low TTB had lower average ORs compared with EDs with high TTB. This is unsurprising because more beds are likely to be occupied at any given time in EDs with fewer beds in relation to the daily inflow of patients. However, the large variation in TTB (from 2.1 to 9.2 patients per bed per day) suggests considerable differences in organization and operations between EDs in Sweden. The impact of TTB on measured OR was unchanged when adjusting for possible confounding variables, indicating that TTB is an important factor to consider when using OR as a measure of crowding.
Because of its simplicity, OR has become a popular measure of crowding, but our findings indicate that crude OR alone may not be ideal for comparing crowding between EDs. By definition, 2 EDs are equally full at equal ORs. 6 However, a given OR may not have equal effects on the level of crowding and the quality of care at different EDs because of the different operational models or patient population differences. 9 , 10 , 11 , 15 Furthermore, there is evidence that the effect of crowding on patient outcome is non‐linear, 1 , 2 , 3 with more of the negative effects at the highest crowding levels. The observed differences in TTB between EDs in our study and the non‐linear relation between crowding and quality of care may explain some of the mixed results from studies using OR as a measure of crowding. 1 , 5 , 33 In a recent study by af Ugglas et al, arrival at hours with an OR in the top 5 percentile was associated with an increased hazard ratio for death at 30 days. 1 Similarly, Jo et al found an association between the top quartile of OR and short‐term mortality in an urban Korean ED. 34 By using a relative cutoff of OR when defining crowding, that is, the top quartile or top percentiles, these authors adjusted for baseline differences between the EDs of the type seen in our study. In contrast, Jones et al made no such adjustment in a multicenter study 5 and found no effect on mortality of different absolute OR cutoffs (0.85–1; 1–1.25; >1.25).
By dividing OR with TTB, accounting for baseline differences in crowding, we improved the correlation with assessed workload considerably by using each ED as its own control (Equation 1). The CR is easy to calculate and understand and potentially more comparable between EDs. This is similar to the methods in a study by af Ugglas et al, in which they used the current census in relation to the expected census for a given workshift and ED as the exposure of crowding and found it to be associated with 30‐day mortality. 1 Furthermore, McCusker et al observed an association between a relative OR, defined as OR/average OR, and mortality in a large Canadian study. 35 In our study, the correlation between treatment beds and census was good (r = 0.77) but not perfect, indicating variability in treatment bed ratios that CR may better account for and still be easy to use. However, further validation is needed to investigate the generalizability of our results.
Interestingly, there was no difference in average workload between EDs with low versus high TTB, which indicates that staff may account for baseline differences in ED beds when they assess workload. Whether this is attributed to different ED operational models or patient populations was not studied. There may also be a psychological blunting effect of working in a constantly crowded ED, which may lead to lower scores of perceived workload and/or perhaps a selection of individuals who stay and work in EDs with high degrees of crowding.
6. CONCLUSION
Differences in the number of treatment beds in relation to the number of presenting patients differ substantially between EDs in Sweden and affect OR but not necessarily staff‐assessed crowding. These differences should be accounted for when using OR as a comparator of crowding between EDs and propose the CR as a simple and readily available alternative by dividing the current census by the daily average census.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Jens Wretborn conceived the study. Daniel B. Wilhelms and Jens Wretborn designed the trial. Daniel B. Wilhelms and Ulf Ekelund obtained research funding. Daniel B. Wilhelms supervised the conduct of the trial. Jens Wretborn collected and managed the data, with assistance from Daniel B. Wilhelms and Ulf Ekelund. Jens Wretborn drafted the manuscript, and all authors contributed substantially to its revision. Jens Wretborn takes responsibility for the article as a whole.
ACKNOWLEDGMENT
We acknowledge Erika Hörlin for her invaluable assistance in data collection.
Biography
Jens Wretborn, MD, is an emergency physician at Linköping University Hospital in Linköping, Sweden.

Wretborn J, Ekelund U, B. Wilhelms D. Differentiating properties of occupancy rate and workload to estimate crowding: A Swedish national cross‐sectional study. JACEP Open. 2022;3:e12648. 10.1002/emp2.12648
Funding and support: This work was supported by 2 grants from Region Östergötland to Daniel B. Wilhelms (LIO‐532001 and LIO‐700271) and from Region Skåne to Ulf Ekelund.
Supervising Editor: Christian Tomaszewski, MD, MS.
Presented at the Society for Academic Emergency Medicine 2021 virtual meeting May 14–16, 2020 and as a poster at the Swedish Emergency Medicine Talks March 14, 2020.
REFERENCES
- 1. af Ugglas B, Djärv T, Ljungman PLS, Holzmann MJ. Emergency department crowding associated with increased 30‐day mortality: a cohort study in Stockholm Region, Sweden, 2012 to 2016. J Am Coll Emerg Physicians Open. 2020;1(6):1312‐1319. 10.1002/emp2.12243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Berg LM, Ehrenberg A, Florin J, Östergren J, Discacciati A, Göransson KE. Associations between crowding and ten‐day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019;74(3):345‐356. 10.1016/j.annemergmed.2019.04.012 [DOI] [PubMed] [Google Scholar]
- 3. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605‐611. 10.1016/j.annemergmed.2012.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stang AS, Crotts J, Johnson DW, Hartling L, Guttmann A. Crowding measures associated with the quality of emergency department care: a systematic review. Acad Emerg Med. 2015;22(6):643‐656. 10.1111/acem.12682 [DOI] [PubMed] [Google Scholar]
- 5. Jones PG, van der Werf B. Emergency department crowding and mortality for patients presenting to emergency departments in New Zealand. Emerg Med Australas. 2021;33(4):655‐664. 10.1111/1742-6723.13699 [DOI] [PubMed] [Google Scholar]
- 6. McCarthy ML, Aronsky D, Jones ID, et al. The emergency department occupancy rate: a simple measure of emergency department crowding? Ann Emerg Med. 2008;51(1):15‐24. 10.1016/j.annemergmed.2007.09.003 [DOI] [PubMed] [Google Scholar]
- 7. Hwang U, McCarthy ML, Aronsky D, et al. Measures of crowding in the emergency department: a systematic review. Acad Emerg Med. 2011;18(5):527‐538. 10.1111/j.1553-2712.2011.01054.x [DOI] [PubMed] [Google Scholar]
- 8. Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone‐Griffith S. Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad Emerg Med. 2015;22(5):542‐553. 10.1111/acem.12654 [DOI] [PubMed] [Google Scholar]
- 9. Oredsson S, Jonsson H, Rognes J, et al. A systematic review of triage‐related interventions to improve patient flow in emergency departments. Scand J Trauma Resusc Emerg Med. 2011;19:43. 10.1186/1757-7241-19-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Anderson JS, Burke RC, Augusto KD, et al. The effect of a rapid assessment zone on emergency department operations and throughput. Ann Emerg Med. 2020;75(2):236‐245. 10.1016/j.annemergmed.2019.07.047 [DOI] [PubMed] [Google Scholar]
- 11. Garrett JS, Berry C, Wong H, Qin H, Kline JA. The effect of vertical split‐flow patient management on emergency department throughput and efficiency. Am J Emerg Med. 2018;36(9):1581‐1584. 10.1016/j.ajem.2018.01.035 [DOI] [PubMed] [Google Scholar]
- 12. Boyle A, Coleman J, Sultan Y, et al. Initial validation of the International Crowding Measure in Emergency Departments (ICMED) to measure emergency department crowding. Emerg Med J. 2015;32(2):105‐108. 10.1136/emermed-2013-202849 [DOI] [PubMed] [Google Scholar]
- 13. Weiss SJ, Derlet R, Arndahl J, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS). Acad Emerg Med. 2004;11(1):38‐50. 10.1197/S1069-6563(03)00583-9 [DOI] [PubMed] [Google Scholar]
- 14. Wretborn J, Khoshnood A, Wieloch M, Ekelund U. Skåne emergency department assessment of patient load (SEAL)—a model to estimate crowding based on workload in Swedish emergency departments. PLoS One. 2015;10(6):e0130020. 10.1371/journal.pone.0130020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wretborn J, Henricson J, Ekelund U, Wilhelms DB. Prevalence of crowding, boarding and staffing levels in Swedish emergency departments—a National cross sectional study. BMC Emerg Med. 2020;20(1):50. 10.1186/s12873-020-00342-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191‐2194. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 17. Wretborn J, Starkenberg H, Ruge T, Wilhelms DB, Ekelund U. Validation of the modified Skåne emergency department assessment of patient load (mSEAL) model for emergency department crowding and comparison with international models; an observational study. BMC Emerg Med. 2021;21(1):21. 10.1186/s12873-021-00414-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wretborn J, Ekelund U, Wilhelms DB. Emergency department workload and crowding during a major electronic health record breakdown. Front Public Health. 2019;7:267. 10.3389/fpubh.2019.00267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weiss SJ, Ernst AA, Nick TG. Comparison of the National Emergency Department Overcrowding Scale and the Emergency Department Work Index for quantifying emergency department crowding. Acad Emerg Med. 2006;13(5):513‐518. 10.1197/j.aem.2005.12.009 [DOI] [PubMed] [Google Scholar]
- 20. Hargreaves D, Snel S, Dewar C, Arjan K, Parrella P, Hodgson LE. Validation of the National Emergency Department Overcrowding Score (NEDOCS) in a UK non‐specialist emergency department. Emerg Med J. 2020;37(12):801‐806. 10.1136/emermed-2019-208836 [DOI] [PubMed] [Google Scholar]
- 21. Hoot NR, Zhou C, Jones I, Aronsky D. Measuring and forecasting emergency department crowding in real time. Ann Emerg Med. 2007;49(6):747‐755. 10.1016/j.annemergmed.2007.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Holm S. A simple sequentially rejective multiple test procedure. Scand Stat Theory Appl. 1979;6(2):65‐70. http://www.jstor.org/stable/4615733 [Google Scholar]
- 23. McKinney W. Data structures for statistical computing in Python. In: van der Walt S, Millman J eds. Proceedings of the 9th Python in Science Conference. Vol. 445. Austin, Texas: Scientific Python; 2010;51‐56. 10.25080/majora-92bf1922-00a [DOI] [Google Scholar]
- 24. Jones E, Oliphant T, Peterson P, Others . SciPy: open source scientific tools for Python. http://www.scipy.org/. Accessed January 9, 2022.
- 25. Millman KJ, Aivazis M. Python for scientists and engineers. Comput Sci Eng. 2011;13(2):9‐12. 10.1109/MCSE.2011.36 [DOI] [Google Scholar]
- 26. Seabold S, Perktold J. Statsmodels: econometric and statistical modeling with python. In: van der Walt S, Millman J eds. Proceedings of the 9th Python in Science Conference. Vol 445; Austin, Texas: Scientific Python; 2010;92‐96. [Google Scholar]
- 27. Andrew Taylor R, Venkatesh A, Parwani V, et al. Applying advanced analytics to guide emergency department operational decisions: a proof‐of‐concept study examining the effects of boarding. Am J Emerg Med. 2018;36(9):1534‐1539. 10.1016/j.ajem.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 28. Silverman RA, Stevenson L, Hastings HM. Age‐related seasonal patterns of emergency department visits for acute asthma in an urban environment. Ann Emerg Med. 2003;42(4):577‐586. 10.1067/s0196-0644(03)00410-4 [DOI] [PubMed] [Google Scholar]
- 29. Hind J, Lahart IM, Jayakumar N, Athar S, Fazal MA, Ashwood N. Seasonal variation in trauma admissions to a level III trauma unit over 10 years. Injury. 2020;51(10):2209‐2218. 10.1016/j.injury.2020.07.014 [DOI] [PubMed] [Google Scholar]
- 30. Marcilio I, Hajat S, Gouveia N. Forecasting daily emergency department visits using calendar variables and ambient temperature readings. Acad Emerg Med. 2013;20(8):769‐777. 10.1111/acem.12182 [DOI] [PubMed] [Google Scholar]
- 31. Schull MJ, Szalai JP, Schwartz B, Redelmeier DA. Emergency department overcrowding following systematic hospital restructuring: trends at twenty hospitals over ten years. Acad Emerg Med. 2001;8(11):1037‐1043. 10.1111/j.1553-2712.2001.tb01112.x [DOI] [PubMed] [Google Scholar]
- 32. Batal H, Tench J, McMillan S, Adams J, Mehler PS. Predicting patient visits to an urgent care clinic using calendar variables. Acad Emerg Med. 2001;8(1):48‐53. 10.1111/j.1553-2712.2001.tb00550.x [DOI] [PubMed] [Google Scholar]
- 33. Jo S, Jeong T, Jin YH, Lee JB, Yoon J, Park B. ED crowding is associated with inpatient mortality among critically ill patients admitted via the ED: post hoc analysis from a retrospective study. Am J Emerg Med. 2015;33(12):1725‐1731. 10.1016/j.ajem.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 34. Jo S, Jin YH, Lee JB, Jeong T, Yoon J, Park B. Emergency department occupancy ratio is associated with increased early mortality. J Emerg Med. 2014;46(2):241‐249. 10.1016/j.jemermed.2013.05.026 [DOI] [PubMed] [Google Scholar]
- 35. McCusker J, Vadeboncoeur A, Lévesque J‐F, Ciampi A, Belzile E. Increases in emergency department occupancy are associated with adverse 30‐day outcomes. Acad Emerg Med. 2014;21(10):1092‐1100. 10.1111/acem.12480 [DOI] [PubMed] [Google Scholar]


