Abstract
Objectives
Investigations of the impact of residents on emergency department (ED) timeliness of care typically focus only on global ED flow metrics. We sought to describe the association between resident complement/supervisory ratios and timeliness of ED care of a specific time‐sensitive condition, acute stroke.
Methods
We matched ED stroke patient arrivals at 1 academic stroke center against resident and attending staffing and constructed a Cox proportional hazards model of door‐to‐activation (DTA) time (ie, ED arrival [“door”] to stroke team activation). We considered multiple predictors, including calculated ratios of residents supervised by each attending physician.
Results
Among 462 stroke activation patients in 2014–2015, DTA ranged from 1 to 217 minutes, 72% within 15 minutes. The median number of emergency and off‐service residents supervised per attending were 1.7 (interquartile range [IQR], 1.3–2.3) and 0.7 (IQR, 0–1), respectively. A 1‐resident increase in off‐service residents was associated with a 24% decrease (hazard ratio [HR], 0.76; 95% confidence interval [CI], 0.64–0.90) in the probability of stroke team activation at any given time. An independent 1‐resident increase in the number of emergency residents was associated with a 13% increase (HR, 1.13; 95% CI, 1.01–1.25) in timely activation.
Conclusion
Timeliness of care for acute stroke may be impacted by how academic EDs configure the complement and supervisory structures of residents. Higher supervisory demands imposed by increasing the proportion of rotating off‐service residents may be associated with slower stroke recognition and DTA times, but this effect may be offset when more emergency residents are present.
Keywords: clinical supervision, learner ratio, medical education, residency, stroke, time‐to‐treatment
1. INTRODUCTION
1.1. Background
A limited number of studies have investigated the association of trainees, resident complement, and resident/supervisor ratios on timeliness of care in emergency departments (EDs). 1 , 2 , 3 , 4 These investigations have reported varying effects on global flow metrics among a mixed population of ED patients. Although certain conditions commonly cared for in EDs are particularly time‐sensitive (eg, ST‐segment–elevation myocardial infarction, sepsis, trauma, acute stroke), we are not aware of any previous reports describing the potential effects of ED resident staffing and supervision on the provision of timely care for such conditions.
1.2. Importance
Stroke is a leading cause of disability and death in the United States, 5 , 6 and national guidelines call for the rapid diagnosis and treatment of acute stroke to reduce morbidity and mortality. 7 , 8 These guidelines include several well‐accepted timeliness‐of‐care thresholds. One key metric is the time from patient arrival in the ED until activation of the stroke team (door‐to‐activation time [DTA]) because that process is a rate‐limiting step in downstream interventions. 7 A number of diverse factors are known to affect care processes in the ED management of acute stroke; 9 , 10 , 11 , 12 , 13 , 14 , 15 however, the effects of resident staffing and supervision in the ED are unclear.
1.3. Goals of this investigation
In 2017, 2 of the authors in this investigation reported the effects of ED overcrowding on timeliness of acute stroke care. 15 That investigation used a prospective stroke registry database augmented by a robust electronic health record (EHR) data abstraction by trained research assistants for additional patient‐specific data and EHR queries for ED occupancy data at the time of arrival of each stroke patient. Considered within that study were patient factors, stroke care process factors, and general ED operational factors. However, resident and supervision factors were not included. Subsequent to that investigation, a review of the literature related to the effects of residents on global ED clinical operations prompted consideration that resident complement and supervisory ratios also may affect timeliness of acute stroke care. Therefore, we theorized that supervisory ratios of residents per attending physician might affect timeliness of acute stroke care, further postulating that the complement of emergency versus rotating off‐service residents may also have an effect. The latter was attributed to a commonly held notion among emergency faculty that emergency residents are typically more reliable and efficient than off‐service residents in providing patient care in the ED setting given their additional experience and comfort level in that environment. Therefore, we sought to describe the association between ED resident complement/supervision and DTA in the same academic stroke center.
The Bottom Line
Although resident staffing, supervision ratios, and learner complement play a role in global emergency department (ED) flow, the effect on specific disease processes is unknown. This single institution observational cohort study found that for each additional off‐service resident in the ED, there was a 24% decrease in probably of timely stroke team activation, whereas for each additional emergency resident, there was a 13% increase in probability of stroke team activation at any given time.
2. METHODS
2.1. Study design
This was an observational cohort study in which we employed a previously developed methodology 15 to retrospectively query the prospective stroke registry of our urban, regional referral stroke center hospital to identify all consecutive patients who presented to the adult ED and met the criteria for stroke team activation between June 15, 2014, and June 15, 2015. Our study was limited to this relatively remote, single‐year period out of necessity because of the highly workload‐intensive requisite patient‐specific data abstraction having been previously completed for the registry patients during this time frame. This was not a hypothesis‐testing study, so there was no prospective power calculation.
2.2. Study setting and population
This was a single‐site study conducted at an academic center with 67,795 annual adult ED visits. The center housed multiple residencies, including emergency medicine and neurology programs, with a stroke team available in house 24 hours per day, 7 days per week. During the enrollment period, the ED was staffed by board‐certified/board‐eligible attending emergency physicians who supervised both emergency residents (post‐graduate years [PGYs] 1–3) and off‐service rotating residents (PGYs 1–2 internal medicine, medicine/pediatrics, plastic surgery, psychiatry, and obstetrics/gynecology), all of whom were eligible to participate in the care of all patients with acute stroke. Neurology residents did not have a dedicated emergency rotation but did participate in the care of ED patients as consultants for neurology cases, including stroke team activations. Attendings did not typically see patients primarily, and residents of all levels/specialties typically had access to see the same patient population. Fourth‐year medical students rotated in the ED during the study period. When students were present in the ED, there were at most 2 across all care teams in the ED at any given time, resulting in 0 to 1 student per ED attending/resident team.
There were the following 2 typical team configurations during the study period: (1) a supervising emergency resident role in 1 area of the ED during peak times and (2) a team of residents who presented directly to the attending in other care areas and during times when the supervising resident was not present. The typical supervising resident staffing model consisted of 1 to 2 emergency PGY‐1 residents, 0 to 2 off‐service residents, and occasionally students presenting to a supervising emergency resident, typically a PGY‐3 emergency resident, although sometimes a PGY‐2 emergency resident. The supervising emergency resident would present patients directly to the attending and would typically not see patients independently. The second typical resident staffing model consisted of 1 to 3 emergency residents of any PGY level and 1 to 2 off‐service residents, all of whom presented directly to the attending. Those resident shift start times were often staggered throughout the day to correspond to ED volume curves. The precise number of residents and level of training varied depending on educational mission needs, including the number of residents on the emergency medicine block at any given time, resulting in considerable heterogeneity in daily staffing patterns.
All American Heart Association (AHA)/American Stroke Association Get With The Guidelines 7 recommendations were implemented, and ED nurses, residents, and attending physician staff underwent periodic acute stroke continuing education. We used a traditional nurse triage model. 16 During the study period, only physicians were empowered to activate the stroke team. However, nursing staff were educated and empowered to immediately notify an attending or senior emergency resident if a patient had symptoms concerning for an acute stroke. If such a patient was identified at triage by nursing staff, the attending or senior resident would assess the patient immediately at triage. If determined to meet acute stroke activation criteria, the patient was bedded immediately in an open bed, if available in the main ED, or 1 of 4 resuscitation bays, generally at least 1 of which was always available. Activation was not delayed for bed assignment or patient movement.
2.3. Selection of participants
Local protocol dictated that the stroke team be activated for any patient presenting to the ED with symptoms or findings potentially consistent with an acute stroke within 12 hours of symptom onset. The institution maintained a prospective registry of all patients for whom the stroke team was activated, which included patient demographics and time stamps for care events, including ED arrival, stroke team activation, computed tomography completion, and thrombolytic administration time. A stroke nurse coordinator maintained the registry and verified its accuracy based on established institutional guidelines. Numerous automated and manual processes existed to ensure 100% registry capture of all patients for whom stroke resources were activated. Because the key criterion for stroke team activation was presenting symptoms consistent with stroke, some patients in the registry had an ultimate diagnosis other than stroke, such as transient ischemic attack or complex migraine.
2.4. Data validation
Research assistants blinded to the study aims were trained in data abstraction and retrospectively reviewed the EHR (ED PulseCheck, Optum Clinical Solutions, Inc., Eden Prairie, MN; Soarian, Cerner Corporation, North Kansas City, MO; and OnBase, Hyland Software, Inc., Westlake, OH) for each patient in the registry to validate the registry data and abstract additional fields (determined a priori) using standardized abstraction forms. One study author independently abstracted at least the first 10 encounters reviewed by each research assistant to test for interrater reliability, and there were no discrepancies. We did not report a κ value because there was perfect agreement. Details of fields abstracted, missing value handing, management of documented treatment delays, duplicate checking, and stroke symptoms handling that may have begun while a patient was already in the ED are described in detail in the parent study. 15
ED clinical shift schedules for all faculty and residents were exported from the electronic scheduling software (Shift Admin, Shift Administrators LLC, Columbia, SC) and verified for accuracy by departmental administrators. For each patient in the stroke registry, we calculated the number of attending faculty and residents (emergency residents and off‐service rotating residents) staffing the ED at the moment of patient arrival. Medical students were present in the ED far less frequently than residents and were limited to 2 in number. Their role was also more limited, and their reporting structure typically flowed through a dedicated teaching senior resident who interacted directly with attending faculty and were included in our resident counts. We were not able to identify a reliable data source of medical student clinical schedules, and because medical students presented directly to an emergency resident, we did not account separately for students in calculating attending supervisory ratios.
2.5. Outcome assessment
Based on the electronic time stamps for ED arrival and stroke team activation, we calculated the DTA time for each patient in the stroke registry. DTA has an inherent threshold effect for timely stroke care, as subsequent processes are dependent on timely recognition of stroke syndromes and activation of resources. We chose continuous DTA, as opposed to the more often cited door‐to‐imaging time or door‐to‐thrombolytic time AHA goals, to isolate any subsequent variation in stroke care processes from the process we wished to study, which was timely stroke recognition and resource mobilization as a function of ED resident complement.
Secondary clinical outcomes were admission to a neurology service, final ED diagnosis of stroke or intracranial hemorrhage, and administration of intravenous thrombolytics or neurointerventional procedure, which were recorded directly in the registry and verified in the EHR.
2.6. Primary comparison
Our primary predictor of interest was the supervisory ratio, the number of residents divided by the number of emergency attending physicians present in the ED at the moment of patient arrival. We posited that there would be larger between‐group differences in entrustability 17 of emergency versus off‐service residents compared with the within‐group differences among individual residents. Our analysis also accounted for the proportion of off‐service residents in the ED at any given time. Because resident staffing patterns created a consistent distribution of emergency resident PGY levels throughout any given day, we did not consider resident experience level to be a distinct independent variable.
Because the EHR is a legacy system, registry data did not readily permit structured linkage between any individual patient and the specific care team members who initially evaluated that patient. Thus, we calculated supervisory metrics for the ED as a whole at the moment of arrival for each stroke patient.
2.7. Analysis
We identified 17 additional candidate predictors and patient characteristics of interest for multivariable analysis (listed in Tables 1, 2, 3) by investigator consensus based on their plausibility as confounders and/or inclusion in prior studies. The proportion of off‐service residents in the ED was higher on Wednesdays, when emergency residents were released for educational conferences from 7 am to 1 pm. (Off‐service residents were also excused for didactic education during their ED rotations. Generally, this also occurred on Wednesday mornings, but not necessarily, depending on their specialty.) This educational release time effect was wholly accounted for by our existing measures (namely supervisory ratio), and preliminary analysis did not reveal a significant marginal contribution of other temporal effects (ie, arrival hour of day, day of week, month/year), so we did not include Wednesday conference, for example, as a separate variable. We did not include ED crowding measures in this investigation because previous investigations showed that crowding affected time to imaging in acute stroke care but not stroke team activation. 15
TABLE 1.
Characteristics of study patients
| Characteristic | Among all patients, n (%) | Among 333 patients with DTA time ≤15 minutes, n (%) | Among 207 patients with final ED diagnosis of stroke or ICH, n (%) | |
|---|---|---|---|---|
| Sex, female | 276 (59.7) | 194 (58.3) | 119 (57.5) | |
| History of diabetes mellitus | 143 (31.0) | 101 (30.3) | 62 (30.0) | |
| History of hypertension | 321 (69.5) | 236 (70.9) | 152 (73.4) | |
| History of stroke/TIA | 170 (36.8) | 122 (36.6) | 65 (31.4) | |
| Range for all patients | Median (IQR) for all patients | Median (IQR) among patients with DTA ≤15 minutes | Median (IQR) among patients with final ED diagnosis of stroke or ICH | |
| Age, years | 19–99 | 71 (58–82) | 73 (59–84) | 75 (62–85) |
Abbreviations: DTA, door to activation; ED, emergency department; ICH, intracranial hemorrhage; TIA, transient ischemic attack.
TABLE 2.
Discrete predictors
| Discrete predictor | Among all patients | Among 333 patients with DTA time ≤15 minutes | Among 207 patients with final ED diagnosis of stroke or ICH |
|---|---|---|---|
| EMS mode of arrival | 375 (81.2) | 289 (86.8) | 177 (85.5) |
| GCS score <14 a | 87 (19.6) | 76 (23.5) | 52 (26.3) |
| Supplemental oxygen (intubated or high‐flow or non‐rebreather mask vs nasal cannula or none) | 7 (1.5) | 3 (0.9) | 4 (1.9) |
| Resuscitation room use | 297 (64.3) | 283 (85.0) | 156 (75.4) |
Note. Data are provided as n (%).
Abbreviations: DTA, door to activation; ED, emergency department; EMS, emergency medical services; GCS, Glasgow Coma Scale; ICH, intracranial hemorrhage.
A total of 75 patients did not have GCS scores documented explicitly but had other exam documentation that supported a score of 15.
TABLE 3.
Continuous predictors
| Continuous predictor | Range for all patients | Median (IQR) for all patients | Median (IQR) among 133 patients with DTA time ≤15 minutes | Median (IQR) among 207 patients with final ED diagnosis of stroke or ICH |
|---|---|---|---|---|
| Age, years | 19–99 | 71 (58–82) | 73 (59–84) | 75 (62–85) |
| Blood glucose, mg/dL (n = 4 missing) a | 37–379 | 117 (99–114) | 116 (99–147) | 117 (102–153) |
| Blood pressure, systolic, mmHg (n = 1 missing) a | 97–250 | 148 (130–167) | 152 (133–170) | 153 (134–168) |
| Blood pressure, diastolic, mmHg (n = 1 missing) a | 31–169 | 82 (72–94) | 82 (72–97) | 84 (74–98) |
| Heart rate, min−1 (n = 1 missing) a | 37–170 | 79 (69–90) | 80 (69–92) | 80 (70–92) |
| NIHSS (0–42 points) | 0–36 | 4 (1–11) | 5 (2–14) | 8 (3–17) |
| Oxygen saturation, % (n = 1 missing) a | 81–100 | 97 (96–99) | 97 (95–99) | 97 (95–99) |
| Respiratory rate, min−1 (n = 1 missing) a | 8–40 | 18 (16–20) | 18 (16–20) | 18 (16–20) |
| Time since patient last known to be at baseline neurologic condition, hours | 0.5–>12 | 2 (1–5) | 2 (1–5) | 2 (1–5.75) |
Abbreviations: DTA, door to activation; ED, emergency department; ICH, intracranial hemorrhage; IQR, interquartile range; NIHSS, National Institutes of Health Stroke Scale.
Missing values for vital signs or glucose for these 5 patients were replaced with multiple imputation.
Because time‐to‐event data, such as DTA, tend not to be normally distributed, are bounded above zero by definition, and violate many of the assumptions of classical parametric regression models, we constructed a Cox proportional hazards model of continuous DTA including each of the 17 predictors in the model. In this case, DTA was known precisely for all patients, so there was no need to account for censoring explicitly, although the capability to account for censoring is another general benefit of using time‐to‐event methods. Additional statistical details are available as supplemental content accompanying the online article. The local Institutional Review Board approved this study with expedited review, including waiver of consent, as part of a larger research initiative surrounding timeliness of ED stroke care.
3. RESULTS
3.1. Characteristics of study patients
There were 490 consecutive stroke activation patients in the registry during the study period, 28 of whom were excluded because of documented delay in stroke activation attributed to a more emergent management consideration (airway/breathing intervention, n = 18; hypertension, n = 6; hypotension, n = 1; multiple, n = 3). 15 Clinical outcomes of included and excluded patients are shown in the study flow diagram (Figure 1). The remaining 462 patients were included and had DTA times ranging from 1 to 217 minutes (median, 6; interquartile range [IQR], 1–18), and 72% of patients achieved DTA time within 15 minutes. Table 1 reports the characteristics of included patients, and Tables 2 and 3 report the discrete and continuous predictors, respectively.
FIGURE 1.
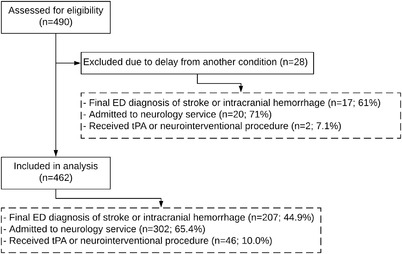
Study flow and clinical outcomes. ED, emergency department; tPA, tissue plasminogen activator
3.2. Staffing and supervisory ratios
Attending and resident staffing and supervisory ratios are reported in Table 4. For 21 registry patients (4.5%), there were no residents in the ED at the time of arrival. Figure 2 visually depicts the 2 primary supervisory schema.
TABLE 4.
Staffing and supervisory ratios
| Median (IQR) | Range | |
|---|---|---|
| Absolute staffing across entire ED | ||
| Attending physician staffing | 3 (2–3) | 2–6 |
| Resident staffing | 6 (4–8) | 0–13 |
| Proportion of residents who were off service, % | 30 (0–43) | 0–100 |
| Patients per physician across entire ED | ||
| ED patients per attending | 18.5 (15.0–22.3) | 5.3–36.5 |
| ED patients per resident | 11.3 (9.0–14.3) | 0–42 |
| Supervisory ratio at any given time | ||
| Total residents per attending | 2.5 (2.0–3.3) | 0–7 |
| Emergency residents per attending | 1.7 (1.3–2.3) | 0–6 |
| Off‐service residents per attending | 0.7 (0–1) | 0–2 |
Abbreviations: ED, emergency department; IQR, interquartile range.
FIGURE 2.
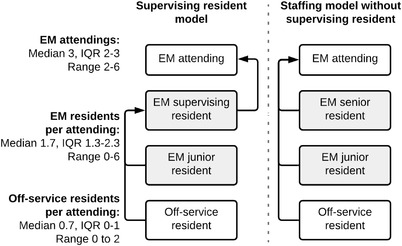
Supervision schema. EM, emergency medicine; IQR, interquartile range
3.3. Main results
A 1‐unit (1 resident) increase in the number of off‐service residents supervised per attending was associated with a 24% decrease (95% confidence interval [CI], 10–36) in the probability of stroke recognition and stroke team activation at any given time. Independently increasing by 1 the number of emergency residents per attending was associated with a 13% increase (95% CI, 1–25) in the probability of stroke team activation at any given time.
Arrival via emergency medical services (EMS), usage of a resuscitation room, higher initial stroke score, and higher Glasgow Coma Scale score were also associated with faster DTA in our primary multivariable model. Table 5 provides the multivariable Cox proportional hazards model estimates of achieving faster DTA time.
TABLE 5.
Cox hazard ratios (HRs) for achieving faster door‐to‐activation (DTA) time
| Predictor | HR (95% CI) |
|---|---|
| Associated with faster DTA | |
| Emergency residents per attending (per 1‐resident increase) | 1.13 (1.01–1.25) |
| Resuscitation room used | 7.55 (5.76–9.89) |
| EMS mode of arrival | 2.65 (1.98–3.54) |
| NIHSS ≥2 | 1.39 (1.11–1.73) |
| Associated with slower DTA | |
| Off‐service residents per attending (per 1‐resident increase) | 0.76 (0.64–0.90) |
| Initial GCS score <14 | 0.66 (0.50–0.86) |
| Non‐significant model terms | |
| Supplemental oxygen (vs none) | 0.65 (0.20–1.62) |
| History of hypertension | 0.78 (0.60–1.00) |
| Sex, female | 0.85 (0.69–1.04) |
| History of stroke/TIA | 0.96 (0.77–1.18) |
| Oxygen saturation a | 0.96 (0.92–1.00) |
| Respiratory rate a | 0.99 (0.96–1.02) |
| Blood pressure‐diastolic a | 1.00 (0.99–1.00) |
| Age a | 1.00 (0.99–1.01) |
| Blood glucose a | 1.00 (1.00–1.00) |
| Heart rate a | 1.00 (1.00–1.01) |
| Blood pressure, systolic a | 1.01 (1.00–1.01) |
| History of diabetes mellitus | 1.02 (0.80–1.30) |
Note. HRs (the ratio of the hazard function between levels of a covariate) are defined as the conditional probability of a given patient achieving DTA in the next instant (ie, their stroke symptoms being recognized), provided their stroke had not been recognized by that point. HR = 1 implies no difference in DTA, and HR <1 implies proportionally slower DTA. "Hazard" is a misnomer in this context, where it is desirable to have a shorter time to event, and the term is used in its statistical definition—similar to risk ratio—not its colloquial meaning.
Abbreviations: CI, confidence interval; EMS, emergency medical services; GCS, Glasgow Coma Score; NIHSS, National Institutes of Health Stroke Scale; TIA, transient ischemic attack.
HRs for non‐significant terms are reported per unit change in predictor.
3.4. Secondary outcomes
There were no significant associations between supervisory ratios and admission to a neurology service, final ED diagnosis of stroke or intracranial hemorrhage, or administration of intravenous thrombolytics or neurointerventional procedure in secondary logistic regression testing.
4. LIMITATIONS
As is typical in any single‐site study, questions of generalizability of our results are important to consider. This was an observational analysis, not a prospective hypothesis‐testing approach. However, our study design included a comprehensive constellation of evidence‐based factors known to influence the timeliness of stroke care. We limited the study period to a single, somewhat remote year out of necessity due to data abstraction being extremely workload intensive. Leveraging the abstraction work from a prior acute stroke investigation was necessary given that support for the requisite data abstraction was no longer available at the time of this investigation. Nevertheless, we are not aware of any significant changes related to resident staffing models since the study period and feel that our observations are still relevant at the time of this report.
Limitations in the scheduling software prohibited determination of the PGY level and specific specialty for off‐service residents and additionally did not allow for specific attribution of residents to attending physicians. An EHR that permitted structured patient‐level linkage of each resident on a treatment team, with that resident's level of training and specialty, would have been preferable and may benefit future replication studies. Although the distribution of PGY levels of emergency residents was generally fixed throughout any given day and during study period, the schedule data available similarly were not conducive to stratified analysis by PGY level within emergency medicine. Therefore, we did not stratify by PGY level nor off‐service resident specialty. Presumably, more advanced residents, emergency or off service, may be both more efficient and more experienced, and PGY level should be considered in future studies. Similarly, considering off‐service resident specialty in future work would be important. Our investigation was not designed to assess the impact of students specifically; it was not feasible to obtain the student schedule retrospectively for the study period, and EHR limitations similarly limited patient‐level linkage of students. However, because students in our ED were typically supervised by a designated resident who was included in the resident staffing counts in our investigation, supervision of medical students was neither ignored entirely from our study nor explicitly measured. This is an important limitation to consider, particularly as it relates to generalizability, as different student teaching configurations may result in different faculty workloads than were observed in our ED. Nonetheless, the fact that students presented to emergency residents and not off‐service residents in theory may strengthen our observations given that their presence would preferentially slow activations for cases in which emergency residents were involved as opposed to off‐service residents. Individual attending or resident performance was not measured in our investigation, and therefore the potential influence of individual practice patterns may have been missed by our methodology. Finally, we selected door‐to‐stroke team activation time as our primary outcome because it is wholly dependent on the ED team and is a nationally recognized marker of timely stroke care. Nonetheless, it is a surrogate marker for patient‐centered distal end points, such as stroke scale improvement, neurologic morbidity, and mortality—meaningful evaluation of which were precluded by our relatively small sample size.
5. DISCUSSION
Our investigation revealed that timeliness of stroke recognition in the ED, as measured by door‐to‐stroke team activation time, varied with differences in resident complement; the presence of more off‐service residents was associated with slower DTA, and the presence of more emergency residents was associated with faster DTA. Prioritizing both high‐quality, efficient patient care and the educational mission of an academic ED is vitally important. Our investigation, the first in this body of literature to focus on the care of a specific, time‐sensitive condition and the first study to consider differential effects of emergency and off‐service residents, highlights that effectively balancing educational and clinical missions can be complex.
Our findings suggest that the education and supervision of off‐service residents may demand a different approach than that of emergency residents, at least in a time‐sensitive condition such as stroke. During the study period, we employed an orientation program for off‐service residents at the beginning of their rotation that focused primarily on general workflows in the ED. It is possible that off‐service residents and their patients could have benefited from stroke‐specific education being added to our orientation program. In 2009, the American College of Emergency Physicians Academic Affairs Committee proposed a standardized curriculum for off‐service residents that addressed specific diseases, injuries, and emergency medicine priorities. 18 Although the committee did not include stroke as a core topic, they did include "altered mental status," and their suggested supplemental reading for off‐service residents included an article on acute stroke management. A subsequent survey of US allopathic emergency residency programs indicated that only 5% of respondents had established didactic curricula designed to meet the needs of off‐service rotators. 19 Estimates for the use of such curricula have not been reported in the literature since 2010, but our anecdotal experience is that implementation remains infrequent. Uncommon implementation, coupled with variation among such curricula in practice, limits the assessment of educational and patient care outcomes. However, our findings emphasize the potential benefit of education specific to off‐service residents, at least in the area of acute stroke diagnosis and management.
Attending supervisory practices of off‐service residents versus emergency residents was not standardized per se in our ED during the study period, but our attending physician culture was one of tending to verify more cautiously the history and examination findings reported by off‐service residents. It remains possible, however, that this culture was not sufficient in driving timely attending assessment of off‐service residents’ patients, a tactic that could potentially have mitigated the effects of off‐service residents theoretically being less efficient and less knowledgeable in the core areas of emergency medicine. Furthermore, our culture of increased caution with off‐service residents may have resulted in perceptions of increased scrutiny, which paradoxically could have disempowered the off‐service residents from committing to a stroke activation when the diagnosis was suspected. 20 Moreover, consideration could be given to the concept that attending physician supervision of off‐service residents contributes to division of faculty attention away from the care of other patients, thereby affecting the care of all ED patients, including patients with acute stroke. This notion could lead one to consider establishing limitations on the number of off‐service residents assigned to an ED attending physician at any given time.
A traditional nurse triage model was in place during this investigation. Although not ostensibly designed to preempt identification of critical patients by residents, a physician intake model might have mitigated delays in stroke syndrome recognition by non‐emergency residents by "prescreening" incoming ED patients by an attending emergency physician. 21 Non‐attending physician intake models may be less equipped to identify stroke patients, particularly those with subtle presentations, and may contribute to delays in stroke syndrome recognition and stroke team activation, especially among learners with less experience. For off‐service residents, this may have had the effect of delaying DTA times, as prescreening by an attending likely creates a safety net not available if a less‐experienced resident is the first to evaluate a patient.
Furthermore, although arrival via EMS was generally associated with faster DTA in this cohort, we have previously shown that ED staff may be overly reliant on prehospital stroke screening, and failure of EMS to recognize stroke syndromes may introduce disproportionate delays in subsequent DTA after ED arrival. 22 Off‐service residents could have been more deferential to EMS assessments, prompting DTA delays if EMS did not recognize a stroke syndrome before arrival. Because our data set did not permit linkage between an individual stroke patient and the composition of his or her care team, we were unable to model these potential interaction effects.
Our findings, although focused on acute stroke recognition and management, naturally raise concerns about the development of off‐service residents’ abilities to recognize and respond to critical illness in general. Although each specialty training program has distinct outcomes in mind when sending residents to rotate in the ED, it is likely that the development of the critical thinking skills needed to recognize and intervene on time‐sensitive emergencies among undifferentiated patients is chief among them. Theoretically, the ED is an ideal training environment for residents who will later be expected to respond to deteriorating patients in clinical environments that may lack the immediately available supervision and other resources present in a large academic ED. Emergency faculty have an important role to play in teaching this skillset to off‐service residents. Upon reflection, we recognized that there may be an opportunity to better coordinate ED off‐service resident curriculum development with the individual off‐service programs both to gain a better understanding of the specialty‐specific goals for the ED rotation and to better anticipate potential ED‐specific knowledge gaps that each specialty's residents may have before rotating in the ED. Such coordination stands to improve the quality of off‐service resident education as well as ED patient care. Given the previously mentioned low use of structured off‐service curricula nationally, we suspect similar opportunities may exist for many programs across the country.
It is important to note that our investigation was not designed to test for ideal resident/attending staffing ratios. This was an observational study of our actual resident/attending staffing patterns, which were likely influenced by both intentional and unintentional factors, including local and regional historical practices, departmental leadership experiences, local economic and political pressures, and so on. It remains probable that increasing the number of emergency residents to a certain extent is useful, but eventually it may create an overwhelming supervision problem that will ultimately erode the efficiency of the attending emergency physician (analogous to a Starling curve). In a hypothetical scenario where 40 patients are cared for by 2 attendings, it would be reasonable to imagine that working alongside 1 resident (0.5 supervisory ratio), 4 residents (2.0 supervisory ratio), or 20 residents (10.0 supervisory ratio) would impose dramatically different cognitive and logistical demands on the attending, even though the attending‐to‐patient ratio is constant at 1:20 in each scenario. Not addressed in our study was consideration for level of training both in emergency and off‐service residents, which also intuitively would affect optimal staffing ratios. In the previous hypothetical scenario considerations, 2.0 or 10.0 supervisory ratios with 2 or 10 senior residents versus 2 or 10 PGY‐1 residents would impose similarly dramatic differences in cognitive and logistical demands on the attending. Nonetheless, although our results may lend some insight into tradeoffs with particular resident staffing models, we are unable to recommend an optimal model based on our observations.
It is likely that the number of total residents, the proportion of emergency versus off‐service residents, overall supervisory ratio, level of resident training, and number of patients per supervising physician are all important and interdependent factors in delivering high‐quality, efficient patient care. Each of these factors warrants consideration when designing ED staffing models and both emergency and off‐service resident schedules that optimize the relationship between expeditious patient care and learning outcomes. As our approach was observational, we were limited to evaluating only actual scenarios and actual combinations of these factors. Although this conundrum lends itself more easily to discrete event simulation, a quasi‐experimental design may be more enlightening in future work.
To date, investigations of the effects of residents on clinical outcomes in emergency medicine have been limited in number and have focused on global ED flow metrics, such as length of stay, 1 , 2 , 3 , 23 , 24 , 25 resource use, 23 , 26 or mortality across all ED patients. 26 Our investigation is the first to provide insight into resident‐related effects on the care of a specific, time‐sensitive condition, and it is the first study to consider differential effects of emergency and off‐service residents. In fact, we are aware of only 1 prior study addressing the concept of ED supervisory ratios, and that study was limited to discrete event simulation modeling of a pediatric ED. 24
Although limited by a single‐center observational data set, our findings suggest that the timeliness of care for acute stroke may be impacted by how academic EDs choose to configure the complement and supervisory structures of residents. Higher supervisory demands imposed by increasing the proportion of off‐service rotating residents may be associated with slower stroke recognition and DTA times, but this effect may be offset when more emergency residents are present. In addition, our observations support the previously suggested potential benefit of a supplemental emergency‐based curriculum specifically geared toward off‐service rotating residents, which may benefit both off‐service rotating residents and ultimately patient care.
AUTHOR CONTRIBUTIONS
Sean S. Michael and Martin A. Reznek conceived and designed the study and supervised the conduct of the study and data collection. Martin A. Reznek supervised data acquisition. Sean S. Michael supervised data analysis, and all authors participated in data interpretation. Sean S. Michael, Richard J. Church, Martin A. Reznek, and Sarah H. Michael drafted the manuscript, and all authors contributed substantially to its revision and intellectual content. Sean S. Michael takes responsibility for the article as a whole.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Supporting information.
Biography
Sean S. Michael, MD, MBA, is the Medical Director and Administrative Fellowship Director as well as Assistant Professor in the Department of Emergency Medicine at the University of Colorado School of Medicine in Aurora, Colorado.

Michael SS, Church RJ, Michael SH, Clark RT, Reznek MA. Effect of resident complement on timeliness of stroke team activation in an academic emergency department. JACEP Open. 2022;3:e12643. 10.1002/emp2.12643
Supervising Editors: Katherine Edmunds, MD, Med; Sing‐Yi Feng, MD.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
The abstract was presented at the American College of Emergency Physicians Research Forum, Denver, CO, October 27, 2019.
REFERENCES
- 1. James C, Harper M, Johnston P, Sanders B, Shannon M. Effect of trainees on length of stay in the pediatric emergency department. Acad Emerg Med. 2009;16(9):859‐865. [DOI] [PubMed] [Google Scholar]
- 2. Kawano T, Nishiyama K, Hayashi H. Adding more junior residents may worsen emergency department crowding. PLoS One. 2014;9(11):e110801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lammers RL, Roiger M, Rice L, Overton DT, Cucos D. The effect of a new emergency medicine residency program on patient length of stay in a community hospital emergency department. Acad Emerg Med. 2003;10(7):725‐730. [DOI] [PubMed] [Google Scholar]
- 4. McGarry J, Krall SP, McLaughlin T. Impact of resident physicians on emergency department throughput. West J Emerg Med. 2010;11(4):333‐335. [PMC free article] [PubMed] [Google Scholar]
- 5. Kochanek KD, Murphy SL, Xu J, Arias E. Mortality in the United States. NCHS Data Brief. 2013(178):1‐8. [PubMed] [Google Scholar]
- 6. Centers for Disease C, prevention. Prevalence of stroke–United States, 2006‐2010. MMWR Morb Mortal Wkly Rep. 2012;61(20):379‐382. [PubMed] [Google Scholar]
- 7. Jauch EC, Saver JL. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870‐947. [DOI] [PubMed] [Google Scholar]
- 8. Kelly AG, Hellkamp AS, Olson D, Smith EE, Schwamm LH. Predictors of rapid brain imaging in acute stroke: analysis of the Get With the Guidelines–Stroke program. Stroke. 2012;43(5):1279‐1284. [DOI] [PubMed] [Google Scholar]
- 9. Fonarow GC, Smith EE, Saver JL, et al. Improving door‐to‐needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association's target: stroke initiative. Stroke. 2011;42(10):2983‐2989. [DOI] [PubMed] [Google Scholar]
- 10. Ruff IM, Ali SF, Goldstein JN, et al. Improving door‐to‐needle times: a single center validation of the target stroke hypothesis. Stroke. 2014;45(2):504‐508. [DOI] [PubMed] [Google Scholar]
- 11. Ekundayo OJ, Saver JL, Fonarow GC, et al. Patterns of emergency medical services use and its association with timely stroke treatment: findings from Get With the Guidelines–Stroke. Circ Cardiovasc Qual Outcomes. 2013; 6(3): 262‐269. [DOI] [PubMed] [Google Scholar]
- 12. Ferrari J, Knoflach M, Seyfang L, Lang W. Differences in process management and in‐hospital delays in treatment with iv thrombolysis. PLoS One. 2013;8(9):e75378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harsany M, Kadlecova P, Svigelj V, et al. Factors influencing door‐to‐imaging time: analysis of the safe implementation of treatments in Stroke‐EAST registry. J Stroke Cerebrovasc Dis. 2014;23(8):2122‐2129. [DOI] [PubMed] [Google Scholar]
- 14. Sauser K, Bravata DM, Hayward RA, Levine DA. A national evaluation of door‐to‐imaging times among acute ischemic stroke patients within the Veterans Health Administration. J Stroke Cerebrovasc Dis. 2015;24(6):1329‐1332. [DOI] [PubMed] [Google Scholar]
- 15. Reznek MA, Murray E, Youngren MN, Durham NT, Michael SS. Door‐to‐imaging time for acute stroke. Stroke. 2017;48(1):49‐54. [DOI] [PubMed] [Google Scholar]
- 16. Yiadom MYAB, Napoli A, Granovsky M, et al. Managing and measuring emergency department care: results of the Fourth Emergency Department Benchmarking Definitions Summit. Acad Emerg Med. 2020;27(7):600–611. [DOI] [PubMed] [Google Scholar]
- 17. ten Cate O. Entrustability of professional activities and competency‐based training. Med Educ. 2005;39(12):1176‐1177. [DOI] [PubMed] [Google Scholar]
- 18. Kessler CS, Marcolini EG, Schmitz G, et al. Off‐service resident education in the emergency department: outline of a national standardized curriculum. Acad Emerg Med. 2009;16(12):1325‐1330. [DOI] [PubMed] [Google Scholar]
- 19. Branzetti JB, Aldeen AZ, Mark Courtney D. Rotating resident didactics in the emergency department: a cross‐sectional survey on current curricular practices. Acad Emerg Med. 2010;17(suppl 2):S49‐S53. [DOI] [PubMed] [Google Scholar]
- 20. Olmos‐Vega FM, Dolmans DHJM, Vargas‐Castro N, Stalmeijer RE. Dealing with the tension: how residents seek autonomy and participation in the workplace. Med Educ. 2017; 51(7):699‐707. [DOI] [PubMed] [Google Scholar]
- 21. Michael SS, Bickley D, Bookman K, Zane R, Wiler JL. Emergency department front‐end split‐flow experience: physician in intake. BMJ Open Qual. 2019;8(4):e000817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tennyson JC, Michael SS, Youngren MN, Reznek MA. Delayed recognition of acute stroke by emergency department staff following failure to activate stroke by emergency medical services. West J Emerg Med. 2019;20(2):342‐350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. French D, Zwemer FL, Schneider S. The effects of the absence of emergency medicine residents in an academic emergency department. Acad Emerg Med. 2002;9(11):1205‐1210. [DOI] [PubMed] [Google Scholar]
- 24. Genuis ED, Doan Q. The effect of medical trainees on pediatric emergency department flow: a discrete event simulation modeling study. Acad Emerg Med. 2013;20(11):1112‐1120. [DOI] [PubMed] [Google Scholar]
- 25. Harvey M, Al Shaar M, Cave G, Wallace M, Brydon P. Correlation of physician seniority with increased emergency department efficiency during a resident doctors' strike. N Z Med J. 2008;121(1272):59‐68. [PubMed] [Google Scholar]
- 26. Salazar A, Corbella X, Onaga H, Ramon R, Pallares R, Escarrabill J. Impact of a resident strike on emergency department quality indicators at an urban teaching hospital. Acad Emerg Med. 2001;8(8):804‐808. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.


