Abstract
In 2018, there were approximately 570,000 new cases of cervical cancer worldwide. More than 85% of cases occurred in low- and middle-income countries (LMICs), primarily because of poor access to screening and a limited number of medical providers trained to diagnose and treat cervical precancerous lesions. Our objective was to provide locally arranged, hands-on training courses for medical providers in LMICs to learn to perform cervical cancer screening, diagnosis, and treatment procedures. The courses included didactic lectures and hands-on training stations using low-cost simulation models developed by bioengineers and students at Rice University in Houston, TX, United States, and the Malawi Polytechnic in Blantyre, Malawi. The hands-on training stations included visual inspection with acetic acid (VIA), colposcopy, cervical biopsy, endocervical curettage, loop electrosurgical excision procedure (LEEP), and thermal ablation. Provider pre- and postcourse confidence levels in performing the procedures were evaluated. From February 2017 to January 2020, we arranged 15 hands-on training courses in seven cities across six countries (El Salvador, Mozambique, Trinidad and Tobago, Lesotho, Malawi, and Nepal). Overall, there were 506 participants. The average number of participants per course was 38 (range 19-92). The participants included doctors, nurses, and midwives. The course duration varied from 1 to 3 days. Increased confidence in performing VIA, colposcopy and cervical biopsy, ablation, and LEEP was reported by 69%, 71%, 61%, and 76% of participants, respectively. Our findings suggest that locally arranged, hands-on cervical cancer prevention training courses in LMICs can improve provider confidence in performing cervical cancer screening, diagnosis, and treatment procedures. These courses are part of a larger strategy to build local capacity for delivering and improving cervical cancer prevention services in LMICs.
BACKGROUND
Despite the availability of a prophylactic vaccine against the human papillomavirus (HPV) and effective screening methods to detect preinvasive disease, cervical cancer still ranks as the fourth most common cancer and one of the leading causes of cancer death among women worldwide. There were an estimated of 604,127 new cases and 341,831 deaths in 2018.1 More than 85% of these cases occur in low- and middle-income countries (LMICs), where cervical cancer is frequently the leading cause of cancer among women and the death rate is up to 18 times higher compared with more developed countries.2 The global disparities in the incidence of and mortality from cervical cancer are due in part to a lack of organized and effective screening and prevention programs. The regions in the world with highest cervical cancer incidence rates are sub‐Saharan Africa, Micronesia and Melanesia, South-eastern Asia, South America, and Caribbean.1
CONTEXT
Key Objective
Our objective was to provide locally arranged, hands-on training courses for medical providers in low- and middle-income countries on cervical cancer screening, diagnosis, and treatment procedures.
Knowledge Generated
From February 2017 to January 2020, we arranged 15 hands-on training courses across six countries (El Salvador, Mozambique, Trinidad and Tobago, Lesotho, Malawi, and Nepal). The assessment of pre- and postcourse confidence levels reported increased confidence in performing visual inspection with acetic acid, colposcopy and cervical biopsy, ablation, and loop electrosurgical excision procedure by 69%, 71%, 61%, and 76% of participants, respectively.
Relevance
Our findings suggest that locally arranged, hands-on cervical cancer prevention training courses in low- and middle-income countries can improve provider confidence in performing cervical cancer screening, diagnosis, and treatment procedures.
In May 2018, the WHO Director-General made a global call for action toward the elimination of cervical cancer as a public health problem and it was enhanced to accelerate this initiative in November 2020.3 The initiative includes three targets to be met by 2030: (1) 90% of girls to be fully vaccinated with HPV vaccine by age 15 years; (2) 70% of women to be screened with a HPV or other high-performance test at age 35 years and age 45 years; and (3) 90% of women with identified cervical lesions receive appropriate treatment. The third target can be challenging to achieve in LMICs because of lack of resources and required equipment to deliver treatment and a limited number of medical providers trained to diagnose and treat cervical precancerous lesions and invasive cancer.4 Clinical capacity is an issue in many low-resource areas. There is a significant shortage of specialists such as gynecologists, colposcopists, pathologists, and oncologists. In addition, there may be limited availability and access to effective screening programs and limited awareness of cervical cancer among community and health care workers. These shortages can be coupled with a lack of trained providers, equipment, and treatment facilities.5 As a result, effective screening services may be unavailable, leading to patients presenting with advanced-stage cervical cancer when there are limited options for treatment in LMICs.
Our objective was to create a training and mentoring program to build local capacity to provide effective cervical cancer screening, diagnosis, and treatment services. We implemented locally held, hands-on training courses to teach medical providers the necessary procedures for cervical cancer screening, diagnosis, and treatment of preinvasive cervical disease. In addition, we provided ongoing mentoring and support for local providers through regular Project ECHO (Extension for Community Healthcare Outcomes) videoconferences.6
COURSE DEVELOPMENT
Specialists from The University of Texas MD Anderson Cancer Center (MD Anderson) worked in collaboration with bioengineers from Rice University and international and local partners to implement the program in 2016. The team collaborated with ministries of health (MOH), medical schools, hospitals, and nongovernmental organizations (NGOs) in LMICs to understand the context of cervical cancer, specific gaps in services, and the public health situation in each region. The course content was specifically tailored to the needs and requests of colleagues in each region. The courses were all held at the request and in collaboration and partnership with local colleagues.
COURSE STRUCTURE AND CONTENT
The training curricula are based on the guidelines of the WHO, the American Society for Colposcopy and Cervical Pathology and the Johns Hopkins Program for International Education in Gynecology and Obstetrics and ASCO-stratified guidelines for low-resource settings. The MD Anderson curriculum considers local resources and local standards of care and is adapted appropriately for each setting. The courses include didactic lectures and hands-on training stations. The topics of didactic lectures include an overview of cervical cancer, screening guidelines, HPV vaccination, colposcopy and visual inspection with acetic acid (VIA), low-grade and high-grade cervical dysplasia diagnosis and management, loop electrosurgical excision procedure (LEEP), and ablative therapies (cryotherapy and thermal ablation). Specific course topics vary by the request and need of each partnering site.
The courses are 1 to 3 days in duration and are free of charge to all participants. The target audience includes physicians, residents, nurses, and advance practice providers (nurse practitioners, physician assistants, nurse midwives, or their local equivalents). The courses are delivered in the host country language and include trainers and faculty from the region. Certificates of course completion are granted to all participants.
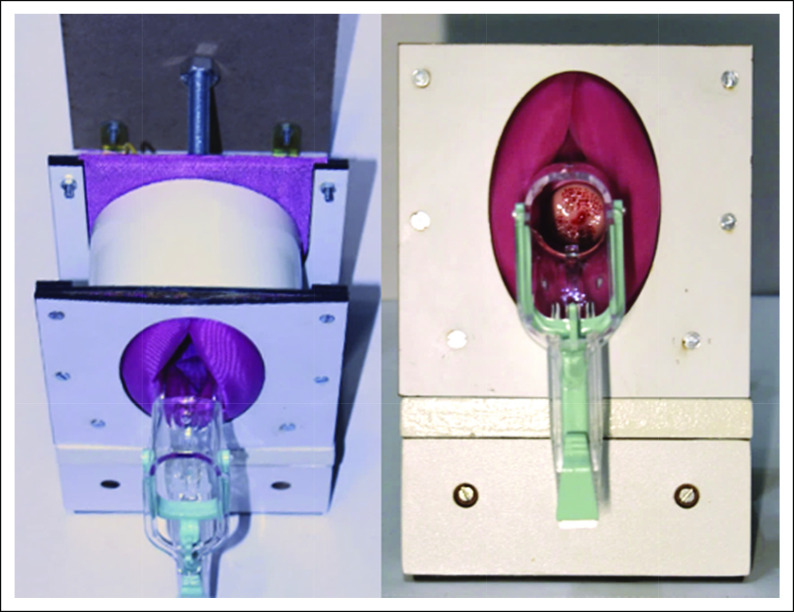
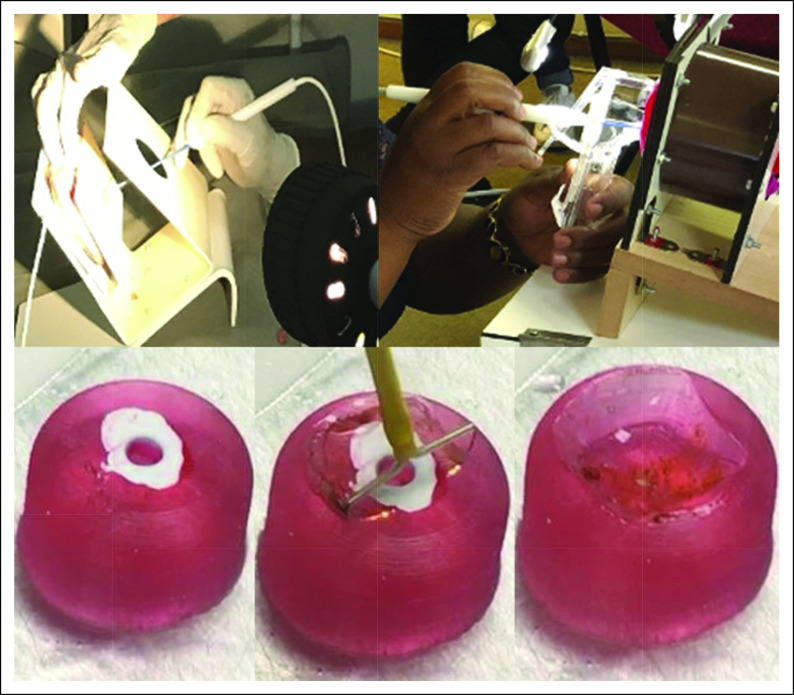
The hands-on portion of the course consists of four to five different stations each with a duration of 30-50 minutes. The stations provide hands-on practice for VIA, thermal ablation, cryotherapy, colposcopy, cervical biopsy, endocervical curettage (ECC), and LEEP. Bioengineers and students from Rice University (Houston, TX) and Malawi Polytechnic (Blantyre, Malawi) developed portable simulation models for hands-on training known as the Low-cost Universal Cervical Cancer Instructional Apparatus (LUCIA; Fig 1).7 These low-cost training models provide the platform for participants to practice the procedures required for cervical cancer screening, diagnosis, and treatment before performing them in the clinic. The LUCIA models mimic precancerous lesions and help providers learn to identify abnormalities. The specific stations are described below.
FIG 1.
Low-cost Universal Cervical Cancer Instructional Apparatus pelvic model.
VIA
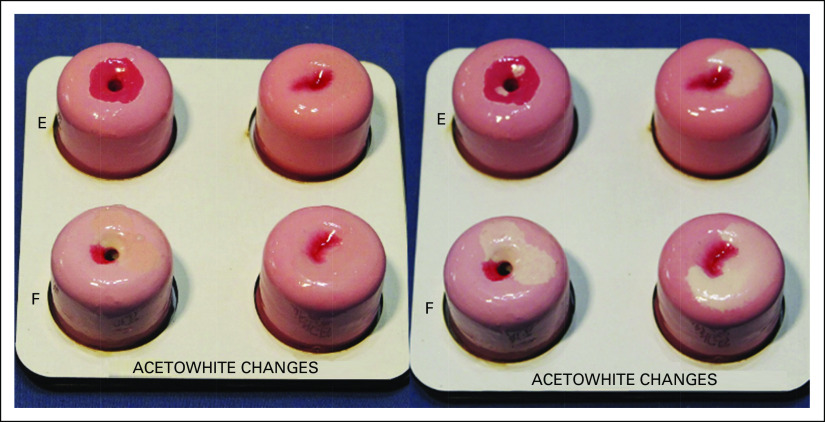
This hands-on training station is included in regions of the world that use VIA as part of their cervical cancer screening program. Three-dimensional cervical models designed to represent different abnormalities are used. These models are covered with temperature-sensitive paint that results in a white lesion appearing with the application of hot water. This mimics the appearance of an acetowhite cervical lesion that appears when acetic acid is applied to the cervix (Fig 2). In addition, participants view photographic images of normal and abnormal findings on the cervix after the application of acetic acid. With each image, the participants are asked whether the lesion is suspicious for cancer, whether the squamocolumnar junction and transformation zone are fully visible, and to note the presence of any lesions. Each lesion is evaluated for eligibility for ablative therapy versus LEEP.
FIG 2.
Three-dimensional cervical models covered with temperature-sensitive paint that mimics the appearance of acetowhite cervical lesions when hot water is applied.
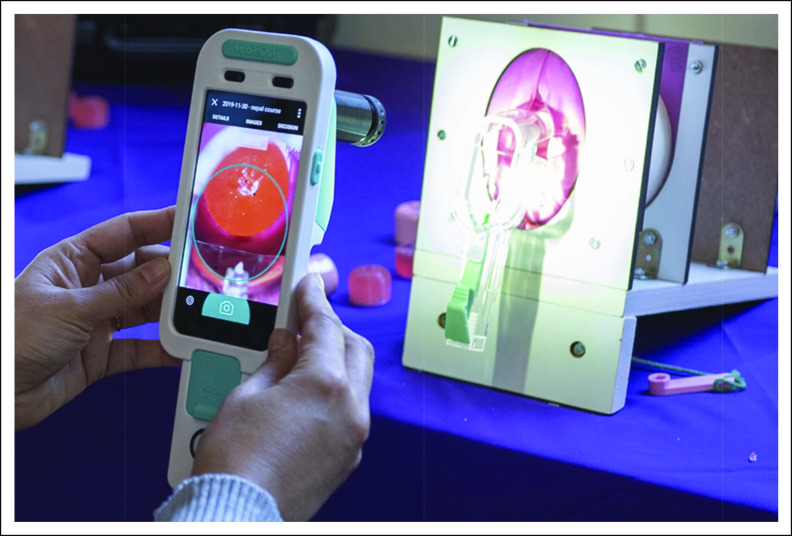
Colposcopy
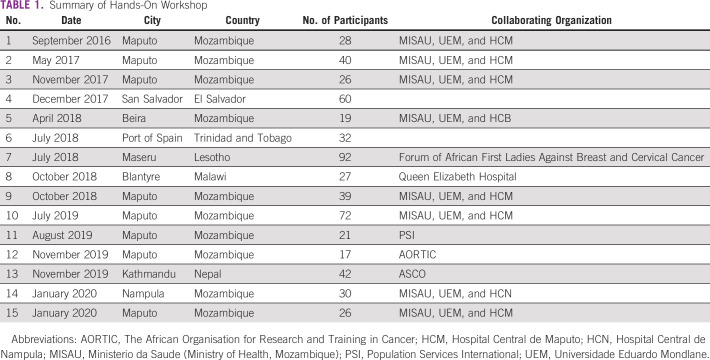
The participants practice using a standard (fixed) colposcope and a mobile colposcope to view cervical models placed in the LUCIA pelvic frame. The participants are asked to identify the squamocolumnar junction, the transformation zone, and any acetowhite lesions. They learn to use the different colposcope settings such as the optical zoom and the green filter to identify vascular changes. They then practice performing cervical biopsies and ECC on the LUCIA cervical models. Small black beads are embedded into LUCIA models made from ballistic gelatin to serve as targets for biopsy (Fig 3).
FIG 3.
Low-cost Universal Cervical Cancer Instructional Apparatus cervical ballistic gel models used to practice colposcopy and cervical biopsy. Hands-on training courses improved provider confidence in cervical cancer screening, diagnostic, and treatment in LMICs.
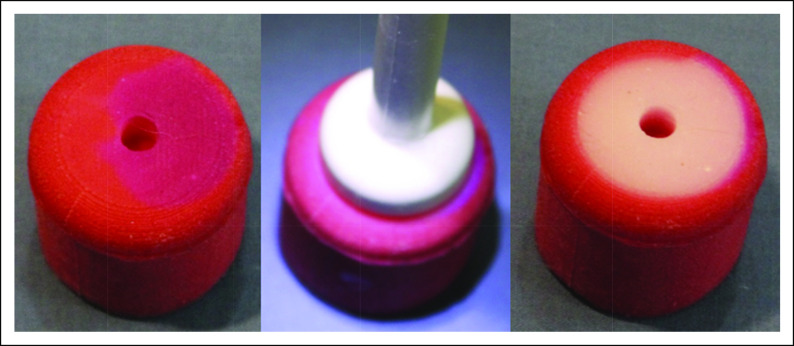
Ablation Therapy
The participants practice cryotherapy and/or thermal ablation using the LUCIA models and/or chicken breast. The LUCIA cryotherapy gel models are made from ballistic gelatin, and the thermal ablation models (Fig 4) are made from a combination of silicone rubber and thermochromic paint. The LUCIA models and the chicken breast turn white when ablated and return to normal color after a few minutes, simulating the procedure on the cervix.
FIG 4.
Silicone models to practice cervical ablation therapy.
LEEP
The instructors explain the LEEP machine functionality and demonstrate the procedure. The participants then practice performing a LEEP using cow tongue and/or the LUCIA cervical ballistic gelatin models (Fig 5).
FIG 5.
Low-cost Universal Cervical Cancer Instructional Apparatus ballistic gel models and cow tongue to practice loop electrosurgical excision procedure.
ADAPTATIONS
Ongoing Education
In Mozambique, the training courses are supplemented with the Project ECHO Cervical Cancer Prevention telementoring program, which began in January 2019. It consists of videoconferences, which are held monthly, in Portuguese. Attendees include the local health care providers including gynecologists, nurses, and gynecologic oncologists from MD Anderson Cancer Center and Portuguese-speaking faculties at collaborating institutions in Brazil and other countries. The local providers present deidentified patient cases and, following a discussion, receive feedback from colleagues and mentors. The ECHO sessions last for 1 hour with 45 minutes of case presentations and discussion and a 15-minute lecture on topics relevant to the curriculum.6
Assessment
The hands-on training course participants were asked to complete a self-evaluation of their confidence and ability to perform the procedures including VIA, colposcopy with cervical biopsy, LEEP, cryotherapy, and thermal ablation. The scores are rated on a 5-point scale, with 5 being the most confident and 1 being no confidence in performing procedures.
Ethical Considerations
The study was approved by the institutional review board at The University of Texas MD Anderson Cancer Center.
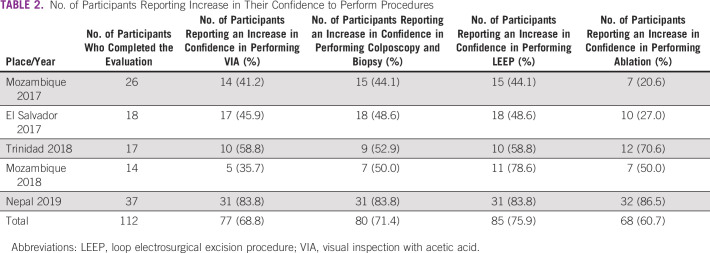
Achievements
From February 2016 to January 2020, 15 hands-on training courses were held in seven cities across six countries (El Salvador, Mozambique, Trinidad and Tobago, Lesotho, Malawi, and Nepal8; Table 1). The average number of participants per course was 38 (range 19-92) and included gynecologists, general physicians, nurses, and midwives. The course duration varied from 1 to 3 days. Each course included a half or full day of didactic lectures followed by hands-on training. In some courses, local specialists received training, so they could then serve as mentors for local colleagues to deliver the hands-on training (train-the-trainer model). The majority of courses were followed by 1 or 2 days of clinical practice where the participants performed the procedures in the clinic under the supportive supervision of the faculty. Half of all participants in Mozambique attended the course more than once to gain more experience and confidence.
TABLE 1.
Summary of Hands-On Workshop
Evaluation
We evaluated pre- and postcourse confidence levels in doing procedures in five of the courses. Increased confidence in performing VIA, colposcopy and cervical biopsy, ablation, and LEEP was reported by 69%, 71%, 61%, and 76% of participants, respectively (Table 2).
TABLE 2.
No. of Participants Reporting Increase in Their Confidence to Perform Procedures
Training Program Adaptation During COVID-19
Because of the COVID-19 travel restrictions and social distancing requirements, all planned in-person courses had to be canceled. We transitioned the course to combine the virtual platform for didactic lectures and small-group in-person hands-on training. We started this platform in Mozambique, where the local staff were previously trained by the international faculty and worked together for many years. Future courses are planned in more countries and adapted to be more beneficial and practical.9
DISCUSSION
Our findings suggest that hands-on cervical cancer prevention courses can increase provider confidence in performing the required procedures for management of women with abnormal cervical cancer screening tests. These courses are part of a larger strategy to build local capacity for cervical cancer screening, diagnosis, and treatment in LMICs. Developing effective training courses for enhancing knowledge and skill capacity in LMICs remains a critical challenge and requires collaboration from many sectors and on-going support and refresher training to be impactful.
The participants included both doctors and nurses. Some participants, particularly the nurses, had previously performed VIA, but had never learned to perform a cervical biopsy or LEEP. This may explain the difference in pre- and postcourse confidence in performing cervical biopsy or LEEP compared with procedures that they had previously performed before the course such as VIA or ablation.
Repeated training and practice in surgical procedures is essential for competency.10 In Mozambique, participants attended the course repeatedly to achieve more experience and feel more confident. Simulation training is valuable in building these skills before performing them in the clinic.
We asked the participants to do a self-assessment on pre- and postcourse confidence levels in doing procedures. We used a self-assessment because it was more suitable for our project and our participants, who were the local providers. The evaluation by self-assessment may not be as objective and accurate as an observer assessment by experts. However, a previous study suggested that self-assessment promoted a different and more powerful view of the trainee.11 The benefits of self-assessment also include increased provider morale and motivation, as well as improvements in knowledge and performance.12
Partnerships in public health offer an opportunity to share resources, experience, and knowledge across organizations. This initiative made an effort to strengthen the capacities of in-country partner institutions and hospitals. As recommended by the WHO, building collaborations during the planning phase for national cancer control program planning is important in all income level countries.13,14 Partnerships are an essential foundation for success. Partnerships at the international and local levels, such as between governments, MOH, local hospitals, providers, and private sectors in the country, are required to build sustainable programs.15-17 Our hands-on training courses along with the Project ECHO telementoring educational program include the efforts of multiple groups and international partnerships. These partnerships are essential for the sustainability of the program.8
Most LMICs do not have up-to-date national guidelines for cervical cancer screening and management of preinvasive disease.18,19 Adopting guidelines used in high-income countries is not appropriate in many LMICs because of the lack of resources and different health care systems.18 WHO and ASCO have issued resource-stratified recommendations for cervical cancer screening, which outline different strategies on the basis of resource settings.20,21 It is essential to develop national guidelines suitable to the country's resources and to ensure adequate training of the clinical providers to carry out the recommendations in the guidelines.
The availability of equipment, instruments, and supplies can be a challenge in LMICs.22 In Mozambique, many facilities do not have functioning colposcopes, LEEP machines, cryotherapy guns, and the gas tanks needed for cryotherapy. There is also a shortage of speculums, biopsy forceps, and the consumables needed to perform LEEPs. These shortages are another barrier to the sustainability of cervical screening and prevention programs in many countries.23
Many health care providers in LMICs have limited experience and skills in delivering cervical cancer prevention and treatment services. Providing only one training course, even with on-going videoconferences, is not enough for the training team to understand the challenges of the local health care system and the barriers faced by the local providers. The development of partnerships among local government, academics, NGO, and others takes time, and their commitment to ensure support and sustainability for the program is essential.
In conclusion, the hands-on training cervical cancer prevention workshops suggested an improvement in the ability and confidence of participants to perform cervical cancer screening and diagnostic procedures. However, long-term partnerships and ongoing learning and mentoring programs are necessary to translate knowledge into practice and to sustain health care provider capabilities and skills in low-resource settings.
Katelin Cherry
Employment: Koda Health, Inc
Stock and Other Ownership Interests: Koda Health, Inc
Patents, Royalties, Other Intellectual Property: Koda Health has submitted two provisional patents to provide digital, personalized health care planning
Kathleen Schmeler
Patents, Royalties, Other Intellectual Property: UpToDate
No other potential conflicts of interest were reported.
SUPPORT
Supported in part by the National Institutes of Health (NIH) through MD Anderson's Cancer Center Support Grant P30CA016672 and R01CA251911 (Rice University, Dr Rebecca Richards-Kortum), the Prevent Cancer Foundation, the Dunaway Family Fund, the Joe Family Fund, and the Giles-O'Malley Foundation.
AUTHOR CONTRIBUTIONS
Conception and design: Natacha Phoolcharoen, Melissa Lopez Varon, Ellen Baker, Sonia Parra, Theresa Sonka, Cesaltina Lorenzoni, Rebecca Richards-Kortum, Kathleen Schmeler, Mila Pontremoli Salcedo
Administrative support: Ellen Baker, Cesaltina Lorenzoni, Kathleen Schmeler
Provision of study materials or patients: Sonia Parra, Cesaltina Lorenzoni, Kathleen Schmeler, Mila Pontremoli Salcedo
Collection and assembly of data: Ellen Baker, Sonia Parra, Jennifer Carns, Katelin Cherry, Chelsey Smith, Theresa Sonka, Kathleen Doughtie, Kathleen Schmeler, Mila Pontremoli Salcedo
Data analysis and interpretation: Natacha Phoolcharoen, Kathleen Schmeler, Mila Pontremoli Salcedo
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Katelin Cherry
Employment: Koda Health, Inc
Stock and Other Ownership Interests: Koda Health, Inc
Patents, Royalties, Other Intellectual Property: Koda Health has submitted two provisional patents to provide digital, personalized health care planning
Kathleen Schmeler
Patents, Royalties, Other Intellectual Property: UpToDate
No other potential conflicts of interest were reported.
REFERENCES
- 1.Sung H, Ferlay J, Siegel RL, et al. : Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209-249, 2021 [DOI] [PubMed] [Google Scholar]
- 2.Small W Jr, Bacon MA, Bajaj A, et al. : Cervical cancer: A global health crisis. Cancer 123:2404-2412, 2017 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) . Accelerating cervical cancer elimination 2018. https://www.who.int/reproductivehealth/publications/screening-cervical-pre-cancer-lesions-women-with-hiv/en/
- 4.Sankaranarayanan R, Budukh AM, Rajkumar R: Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bull World Health Organ 79:954-962, 2001 [PMC free article] [PubMed] [Google Scholar]
- 5.Shah SC, Kayamba V, Peek RM Jr, et al. : Cancer control in low- and middle-income countries: Is it time to consider screening? JCO Glob Oncol 5:1-8, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez MS, Baker ES, Milbourne AM, et al. : Project ECHO: A telementoring program for cervical cancer prevention and treatment in low-resource settings. JCO Glob Oncol 3:658-665, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parra S, Oden M, Schmeler K, et al. : Low-cost instructional Apparatus to improve training for cervical cancer screening and prevention. Obstet Gynecol 133:559-567, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phoolcharoen N, Kremzier M, Eaton V, et al. : American Society of Clinical Oncology (ASCO) Cervical Cancer Prevention Program: A hands-on training course in Nepal. JCO Glob Oncol 7:204-209, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salcedo MP, Varon ML, Phoolcharoen N, et al. : Building local capacity for cervical cancer prevention in low resource settings: Changing strategy during the COVID-19 Pandemic. J Glob Health 11:03044, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andersen SA, Konge L, Cayé-Thomasen P, et al. : Learning curves of virtual mastoidectomy in distributed and massed practice. JAMA Otolaryngol Head Neck Surg 141:913-918, 2015 [DOI] [PubMed] [Google Scholar]
- 11.Brown S, Knight P: Assessing Learners in Higher Education. London, United Kingdom, Kogan page, 1994 [Google Scholar]
- 12.Evans AW, McKenna C, Oliver M: Self-assessment in medical practice. J R Soc Med 95:511-513, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winchester MS, BeLue R, Oni T, et al. : The pan-University network for global health: Framework for collaboration and review of global health needs. Glob Health 12:13, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amuyunzu-Nyamongo M: Need for a multi-factorial, multi-sectorial and multi-disciplinary approach to NCD prevention and control in Africa. Glob Health Promot 17:31-32, 2010. (2 suppl) [DOI] [PubMed] [Google Scholar]
- 15.Frech S, Muha CA, Stevens LM, et al. : Perspectives on strengthening cancer research and control in Latin America through partnerships and diplomacy: Experience of the National Cancer Institute's Center for Global Health. JCO Glob Oncol 4:1-11, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salcedo MP, Lorenzoni C, Schmeler KM: Working together to eliminate cervical cancer: A partnership across three countries "as mudancas no mundo sao criadas por nos. Int J Gynecol Cancer 29:981, 2019 [DOI] [PubMed] [Google Scholar]
- 17.Moretti-Marques R, Salcedo MP, Callegaro Filho D, et al. : Telementoring in gynecologic oncology training: Changing lives in Mozambique. Int J Gynecol Cancer 30:150-151, 2020 [DOI] [PubMed] [Google Scholar]
- 18.Chakkalakal RJ, Cherlin E, Thompson J, et al. : Implementing clinical guidelines in low-income settings: A review of literature. Glob Public Health 8:784-795, 2013 [DOI] [PubMed] [Google Scholar]
- 19.Olson B, Gribble B, Dias J, et al. : Cervical cancer screening programs and guidelines in low- and middle-income countries. Int J Gynaecol Obstet 134:239-246, 2016 [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization (WHO) : Guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. 2013. http://www.who.int/reproductivehealth/publications/cancers/screening_and_treatment_of_precancerous_lesions/en/ [PubMed]
- 21.Jeronimo J, Castle PE, Temin S, et al. : Secondary prevention of cervical cancer: ASCO resource-stratified clinical practice guideline. JCO Glob Oncol 3:635-657, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Randall TC, Ghebre R: Challenges in prevention and care delivery for women with cervical cancer in sub-Saharan Africa. Front Oncol 6:160, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Binagwaho A, Wagner CM, Farmer PE: A vision for global cancer medicine: Pursuing the equity of chance. J Clin Oncol 34:3-5, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]