Abstract
Even when older adults monitor hypertension at home, it is difficult to understand trends and share them with their providers. MyHealthNetwork is a dashboard designed for patients and providers to monitor blood pressure readings to detect hypertension and ultimately warning signs of changes in brain health. A multidisciplinary group in a Digital Health course at Tufts University School of Medicine used Design Thinking to formulate a digital solution to promote brain health among older adults in the United States (US). Older adults (aged 65 and over) are a growing population in the US, with many having one or more chronic health conditions including hypertension. Nearly half of all American adults ages 50-64 worry about memory loss as they age and almost all (90%) wish to maintain independence and age in their homes. Given the well-studied association between hypertension and dementia, we designed a solution that would ultimately promote brain health among older adults by allowing them to measure and record their blood pressure readings at home on a regular basis. Going through each step in the Design Thinking process, we devised MyHealthNetwork, an application which connects to a smart blood pressure cuff and stores users’ blood pressure readings in a digital dashboard which will alert users if readings are outside of the normal range. The dashboard also has a physician view where users’ data can be reviewed by the physician and allow for shared treatment decisions. The authors developed a novel algorithm to visually display the blood pressure categories in the dashboard in a way straightforward enough that users with low health literacy could track and understand their blood pressure over time. Additional features of the dashboard include educational content about brain health and hypertension, a digital navigator to support users with application use and technical questions. Phase 1 in the development of our application includes a pilot study involving recruitment of Primary Care Providers with patients who are at risk of dementia to collect and monitor BP data with our prototype. Subsequent phases of development involve partnerships to provide primary users with a rewards program to promote continued use, additional connections to secondary users such as family members and expansion to capture other health metrics.
Keywords: Brain health, older adults, aging in place, blood pressure, digital health, patient-generated health data
Introduction
In the US, there is growing concern around the health of older adults, defined as those aged 65 years old and over [1]. Older adults are an expanding population, living longer than ever before. As of 2018, 52 million Americans were over age 65 and it is estimated that this population will nearly double to 95 million by 2060 [2]. Eighty-five percent of older adults live with one or more chronic conditions, including hypertension, commonly known as high blood pressure, which affects 63.6% percent of adults over age 65 [3,4]. Nearly 90% of older adults aspire to stay in their current home with some level of independence for as long as possible, a concept termed “aging in place” [5,6]. To promote healthy aging in place, public health initiatives aimed towards increasing the safety and well-being of older adults are needed.
Declines in brain health pose one of the biggest threats to the safety and well-being of older adults aging in place. The US Centers for Disease Control and Prevention define brain health as “an ability to perform all the mental processes of cognition, including the ability to learn and judge, use language, and remember” [7]. One of the strongest threats to brain health among older adults includes dementia, defined as “the loss of cognitive functions including thinking, reasoning and remembering, as well as behavioral abilities to a degree at which the affected individual’s daily life and activities are compromised” [8].
The most common form of dementia includes Alzheimer’s disease (AD), a progressive neurological disorder characterized by a progressive decline in thinking and social and behavioral skills, ultimately inhibiting the affected individual’s ability to function independently [9].Dementia begins to develop before the disease is formally diagnosed [10]. Results from the National Poll on Healthy Aging found that nearly half (44%) of Americans ages 50-64 worried about developing dementia as they age [11]. It is imperative that novel public health initiatives, such as the one reported on here, are developed to detect and prevent brain health disorders which meet older adults where they are truly at: in their homes.
Studies have indicated that a number of behavioral factors, such as smoking, physical activity and diet, as well as physiological factors, such as blood pressure, cholesterol and fasting blood glucose, have been associated with the onset and progression of dementia [12]. Many epidemiological studies have revealed a link between dementia and lifestyle-related diseases, such as hypertension [13,14]. Importantly, cohort studies have revealed that hypertension in midlife (around 45-64 years old) is associated with poorer cognitive function or dementia twenty years later, during older adulthood [15]. As blood pressure is a physiological metric which can be measured and recorded at home quickly, non-invasively and relatively easily at a low cost, compared to other metrics, measuring and recording one’s blood pressure routinely in the home may serve as one means by which older adults can slow or prevent the acquisition of diseases which threaten brain health, such as Alzheimer’s disease and other dementias.
Problem Statement and Process
Among older adults, conditions of poor brain health can lead to cognitive difficulties beyond those associated with normal aging, including dementia.As the number of American older adults living with dementia continues to grow, we recognize the utility of a digital health solution which can allow older adults to prevent brain health decline as they age in place.
Within the context of a graduate-level course on Digital Health, the authors were tasked by AARP to design a digital health solution aimed towards promoting brain health for older adults who wish to successfully age in place. After speaking with content experts from AARP as well as potential end users, we recognized the need to create a solution which would be available to users at a low-cost. We also believed that users would benefit from ease-of-use in the home and wanted to design a solution that can record and store data related to a health-focused behavior which older adults already do regularly in their homes (i.e. weighing themselves or recording periods of sleep). Finally, we aimed to create a solution that would record these measurements in a way that would provide the user with insight regarding trends or patterns within their health metrics which could be shared with their healthcare providers to be used in a predictive manner.
We incorporated a design thinking methodology to guide the steps taken to develop a solution to the problem. Design thinking is a structured process used to achieve a deep understanding of a target audience and their needs. This iterative process typically includes the following steps taken to create a solution to the identified problem: (1) inspiration, which involves understanding the initial problem and opportunities for change, (2) definition, which involves identifying the needs, constraints, and receptivity of the defined target population, (3) ideation, during which brainstorming is done to create novel solutions for the problem at hand, (4) experimentation, at which point a potential solution is designed and flaws are identified and rectified and finally (5) evolution, the stage in which the prototype is shared with potential end users and feedback is gathered and used to modify shortcomings of the solution [16]. The authors completed these five steps in order to design and validate a digital health solution aimed towards addressing the pervasive and complex problem of helping older adults maintain brain health in response to the challenge posited to us by AARP.
Given the well-studied association between hypertension and poor brain health, and the relative ease with which older adults can measure and record their own blood pressure at home, we proposed a solution which empowers older adults to measure, record and monitor their blood pressure at home to detect and prevent declines in brain health. By regularly monitoring blood pressure and maintaining it within a healthy range, the blood vessels which supply nutrients to the brain would be less likely to become diseased, in turn preventing physiological damage to the brain which can lead to cognitive impairment among older adults. Additionally, sharing blood pressure measurements with healthcare practitioners can give older adults and their providers information on primary users’ vascular health, which, in turn, may give insight into the status of users’ brain health and allow detection of brain health problems before they begin or progress [17].
Monitoring their own blood pressure gives older adult users the additional opportunity to engage with their own health maintenance; research indicates that engaged and informed patients take more responsibility for their health, which may slow or prevent potential degradation associated with aging [18,19]. To this end, the Office of the National Coordinator for Health Information, a federal organization tasked with coordinating efforts “to implement and use the most advanced health information technology and the electronic exchange of health information” publicly announced a goal for “PGHD to seamlessly and securely flow from patient to clinicians and research as part of routine care and research” by 2024 [20,21]. Therefore,we recognized that preventative care for brain health can include consistent recording and understanding of patient-generated health data (PGHD) by patients and discussion of this data with their healthcare providers.
Target Audience Interest in Digital Health Solutions
The original problem focused on the needs of older adults, but a digital solution can only be successful if the target users are receptive to digital health. Studies have shown that a majority of older adults and their caretakers are interested in using digital health solutions to monitor their health conditions in their homes [22,23]. One study of in-home sensor technology to detect cognitive changes and other health issues among older adults found that over 90% of participants accepted the in-home monitoring as long as the data collected would be useful to their doctors [24]. Based on their high level of interest, and their role as the demographic most directly impacted by a digital health solution aimed at promoting brain health, the authors believed a digital health solution would be feasible for older adults as the primary target user population during the design thinking process. Importantly, we aim to include all adults over age 45, capturing those who have not yet reached older adulthood by definition but are in the critical period during which hypertension can lead to problems with brain health. In addition to defining age, the primary user population we chose to focus on would be living in their homes,, have at least one chronic health condition as four out of five American adults over age 50 do [25], and .would have internet access, basic digital literacy skills and access to a device which can access the internet, such as a smart-phone or personal computer.
After considering the main sources of support on whom these primary users rely for their well-being, we identified healthcare providers as well as caretakers as the secondary users. Identifying the network of individuals who would be involved in this application of digital health led us to consider additional stakeholders in this solution. Finally, we identified another potential partner to be AARP, who provided the original problem and with whom we consulted during the design thinking process for the digital health solution. From these consultations we learned that AARP would be open to working with designers of the solution to recruit potential users, as well as smart blood pressure cuff manufacturers, such as Withings, from whom we could order the smart device in bulk to ultimately offer lower prices to primary users.
Target Audience Assessment
Following the design thinking process, to better understand our target population, we conducted a four-step process to identify the needs of older adults who wish to maintain their brain health. Our first step involved developing a set of interview questions to get valuable feedback around the topics of brain health, health/technology literacy, and more from potential end users. Secondly, we used feedback from these interviews to develop personas that would represent different types of potential end users who may potentially use a digital solution for brain health. We then developed a fictitious scenario for each persona which might prompt them to seek a digital solution for their brain health. Finally, we ran multiple Q&A sessions with content experts working at AARP in the fields of healthy aging in place and brain health to both learn what solutions to which they already have access and what gaps they have identified that we can address through our product ideation.
Interviews
We planned and conducted four key informant interviews with potential primary users. To learn as much as possible from a small convenience sampling, we developed our interview questions around seven major categories each relevant to maintaining brain health in older adults.
Category 1 investigates the interviewee’s baseline healthcare practices and resources.
Category 2 investigates to what extent memory issues currently impact the interviewee’s life.
Category 3 investigates whether the interviewee has had any concerns about memory or independence issues to date.
Category 4 investigates the interviewee’s motivation(s) to explore a potential intervention related to brain health.
Categories 5 investigates the interviewee’s health literacy.
Category 6 investigates the interviewee’s digital literacy.
Category 7 investigates the interviewee’s openness about home-based health monitoring and data-sharing.
To recruit interview subjects, we used a convenience sample; each interview was conducted by a member of our team with an acquaintance of choice aged 50 or older. Four interviews with potential primary end users were completed via phone calls and answers were electronically transcribed.
Interview Results
By creating the interview guide and using it with potential primary end users, our team was able to further consider all stakeholder populations involved in the need for a digital health solution to preserve older adults’ brain health at home. (The complete interview guide instrument can be found in the appendix A). Responses obtained from these interviews provided greater insight into the baseline healthcare practices and resources of our interviewees. From these questions, we were able to ascertain the extent to which older adults are presently involved in their own health care. All (n=3) had some degree of contact with their PCP but it varied from in-person communication (50%) to the telephone (25%) and using their patient portals (50%). All (n=3) had baseline knowledge of their own health conditions and most (75%) were motivated to be involved in their health care. Those with chronic health issues self-reported to be more motivated and likely to be interested in using digital health technology to assist in managing their health.
Interviewees were also asked to explain any memory problems they currently experience. All older adult interviewees (n=3) expressed that they had experienced mild memory impairments recently. None (n=0) had been diagnosed with memory disorders, such as Alzheimer’s Disease, and none (n=0) reported not having memory issues.
When asked about any concerns they had about their memory, all interviewees (n=3) expressed interest in strengthening their memories as they aged to avoid any further loss. All interviewees (n=3) expressed concerns with maintaining memory or independence issues to date.
When asked about their motivation to use technology for brain health, interest varied among interviewees. From one of our interviewees, we heard that “most technology is not relevant to them, inefficient and difficult to use.” This comment underscores the importance of building digital literacy among older adults so that they can easily adopt and use digital technologies routinely to manage and maintain their health. Fifty percent (n=2) of the interviewees were aware that blood pressure affects many aspects of health including memory, underscoring the need to promote health literacy among older adults.
The results from our four interviews revealed varying degrees of comfort in using technology among older adults. The range was from very comfortable for half (50%) of the interviewees (i.e. commonly uses multiple mobile and web-based applications for health purposes and their patient portal) to no desire or lack of knowledge (50%) in accessing their own health information or any health technology. Three out of the four (75%) interviewees had specific concerns related to privacy and security of personal health information were brought up in conversations of routine use of a potential digital solution for brain health. In addition, while each individual uses technology daily, interviewees’ experiences with digital literacy were mixed. For 25% of the interviewees, some barriers experienced in using any health technology included a lack of interest and/or motivation to monitor, record and share their own health data.
Despite the limitation of a small number of interviewees, the responses were helpful in defining next steps. Based on the analysis, important and necessary considerations to include in our product design are:
Creating a product that will be easy and convenient to use at home,
Promoting patient engagement in adopting and operating the technology daily without the direct assistance of a healthcare provider,
Providing assistance when using the technology via a digital navigator,
Providing educational materials specific to relevant health issues, such as elevated blood pressure and,
Maintaining the primary users’ privacy and ensuring that the data is transmitted securely between the primary user, their physician and their health insurance company.
Personas and Scenarios
After conducting interviews, we used the feedback to develop five unique personas and scenarios to represent each use case we identified that would benefit from digital solutions for brain health. These fictitious personas are distilled from the interviews and reflect the research conducted in the project’s initial stage. The first three are primary personas, which we define as user populations that are directly impacted by brain health issues and would be the main users of our digital health solution. The last two are secondary personas, whom we define as populations who are impacted by the primary users themselves; an example would be a family member who provides most of the caregiving or a doctor of a primary user.
Our first primary persona is Victor, a 65 year old retiree living in upstate New York. He lives at home with his wife and lives a generally healthy life which includes a healthy diet and exercise habits (by traditional American standards). He has been diagnosed with hypertension but has had it managed for years by taking a daily statin. However, for the third time in a row, he has forgotten to take his wallet with him to his regular PCP appointment. He starts to worry whether this is a fluke memory issue or something more significant. Internet searches make him even more worried. He plans to bring this up with his PCP during his next appointment.
Our second primary persona is Amy, a 55 year old clinical assistant living in Hanover, Massachusetts. She is divorced and lives with her elderly parents, acting as a caregiver. Her mother has hypertension, with which Amy is very involved in managing. After a long night shift, Amy comes home and realizes she forgot whether her mother took her blood pressure medication that day. She questions her mother and a verbal argument ensues between the two, with both accusing the other of being forgetful. Amy starts to worry whether her ability to take care of her parents might be affected by the long hours she spends at work, or if something more serious might be affecting her ability to care for them. She starts researching online and finds that tracking data with her smartphone could help her keep an eye on both her and her mother’s patterns of memory loss.
Our third primary persona is Allen, a 60 year old consultant who recently moved to his vacation home in the countryside of rural Maine to become a full time teleworker. He lives 45 minutes away from the closest hospital. He has type 2 diabetes and hypertension, for which he takes a daily statin. He recently downloaded a medication tracking app on his phone, as he noticed he hasn’t been as consistent about taking his statin everyday as he used to. Ever since the move away from the city, he also realized he hasn’t been as active since there’s no gym located nearby. In order to stay independent, he knows that he needs to keep himself as healthy as possible, physically and mentally. He decides to set up a telehealth visit to ask his doctor about remote healthcare and at-home monitoring.
Our first secondary persona is Stephen, a 35 year old software engineer that lives across the country from his parents, whom he regularly video calls. His father has always been generally healthy, but his grandmother on his father’s side died of dementia when Stephen was in college. During their most recent call, as Stephen’s father was about to say goodbye, he accidentally called him the wrong name. Stephen didn’t think much of it but started to worry as the day went on. Was his father distracted? Was he messaging somebody else and accidentally said their name? Or is his grandmother’s dementia genetic and has possibly been passed down to her son? Stephen started to worry about being so far away from his father to help address these potential issues.
Our second secondary persona is Dr. Sevilla, a 45 year old physician in Los Angeles, CA and Stephen’s father’s PCP. Ever since Epic healthcare software was installed at her clinic in 2015, she started using telehealth capabilities with her patients. During the pandemic, Dr. Sevilla notices that while most patients transitioned smoothly to telehealth, Stephen’s father had not. She worries about him as she has heard from his son Stephen about memory-related concerns and knows that Stephen doesn’t have much support in monitoring it with his son across the country. She starts looking into remote monitoring technologies that could be integrated into Epic.
Discussion with AARP Subject Matter Experts
Before beginning our ideation phase, we set up three meetings with different AARP leaders in the fields of digital technology and brain health. Our first meeting was with Nataki Edwards, Senior Vice President of Digital Marketing at AARP. Below were our three prepared talking points with her:
What is AARP’s experience with members using their existing digital tools? What feedback (positive and negative) has AARP received about them? What are the barriers to using these tools have members expressed?
Does AARP have a digital navigator to assist members in using their digital tools as needed?
Does AARP have partnerships with any health monitoring device companies, such as manufacturers of smart blood pressure monitors, to offer discounts to members?
Our second meeting was with Rachael Lazarus, Ph.D, a neuroscientist working for the Staying Sharp initiative within AARP, and Kathy Washa, the Director of the Staying Sharp Program at AARP. This meeting focused on getting more information about AARP’s Staying Sharp platform and how it was developed and implemented to support the brain health of AARP members. During this meeting, we learned how the platform encourages older adults to maintain their brain health through the following six pillars. Later, during our ideation process, we took these into consideration and contemplated designing educational content integrated into our digital solution centered on how each pillar could be used to prevent hypertension and, in turn, promote brain health (Figure 1).
Figure 1.
The Six Pillars of Brain Health emphasized in AARP’s ‘Staying Sharp’ program. Source: AARP, n.d.
Our third meeting was with Alison Bryant, PhD, Senior Vice President of AARP Research and Digital Equity Lead. Our goal for this final meeting was to understand how AARP could potentially accommodate storage of patient-generated health data (PGHD) and whether the digital health solution that we have designed would be something that they could embrace and encourage for their members.
Ideation
We began our ideation process by reviewing pre-existing studies designed to understand brain health among older adults as they age in place. Our focus was on the ones we identified a number of studies centered on the use of digital solutions to promote mental health among older adults (including solutions aimed towards depression and social anxiety), but few focused on loss of cognition and/or memory, one of the most prevalent conditions among older adults [26,27]. While digital solutions have been created to use biometric data from primary users’ electronic health records to predict outcomes related to brain health, including hypertension, none have been designed to be used on a daily basis by the primary user in his or her home [28]. As such, we recognized the need to create a digital health solution which could promote brain health maintenance for older adults in their homes and take into consideration barriers such as health literacy. To our knowledge, our proposed digital solution is the first to be directly used by the primary end user, the patient, in the home to detect and alert secondary users, the primary user’s support team of caretakers and healthcare providers, to changes in blood pressure which might predict a primary user’s risk for dementia.
From our interviews with potential primary target users, we identified some triggers that might prompt an older adult to use our solution. These included fears surrounding memory decline and resulting inability to stay independent as well as the inability to continue to age in place in the home. This understanding is essential for a solution to be adopted and used by the target user population.
Through a review of the existing literature, as well as conversations with potential primary users as well as content experts at AARP, we identified four barriers to adoption (1-3) and use (4) that their members, who are 50 years of age or older, including older adults, face in managing their health care and their ability to use technology to record and view their health data. These barriers include:
Inability to completely understand personal health data among some primary users, due to low health literacy
Lack of familiarity with internet-enabled devices and web-based applications due to low digital literacy
Poor access to the internet services and/or lack of technology used to access the internet (i.e. personal computer, smartphone) can affect a primary user’s ability to record their own health data, limiting their ability to share this data with physicians.
Concerns about privacy and security of data.
All of these triggers and barriers were taken into consideration during the ideation phase of the design thinking process to promote uptake, utility and ease of use among primary and secondary end users.
One of the main challenges in the development of our product design included narrowing our focus on the broad topic of “brain health” to achieve the goal of collecting and tracking data to improve brain health outcomes for older adults. We aimed to target improvement in the areas of overall health and wellness, health knowledge and digital literacy, while specifically designing an intervention centered on brain health. Initially we formulated the idea of creating a platform with AARP that would collect the primary user’s blood pressure each day and provide alerts when elevated blood pressure was detected. The solution would also offer links to educational content related to high blood pressure and brain health to help users with varying levels of health literacy put their measurements into context.
In our discussion with Dr. Alison Bryant we learned that AARP would be interested in providing incentives through the AARP Rewards program to encourage primary users to collect and measure their blood pressure. However, AARP declined the role of storing primary users’ data or providing medical advice to prevent liabilities on their end. From this point, we pivoted in our design process and developed our application, a service that would be instrumental in collecting health metrics, starting with blood pressure in our first iteration, to better assist primary users in monitoring their own health trends and share them with their care team.
The design thinking process for our solution benefitted from the diversity of professional backgrounds of the authors. Our team consisted of two clinicians: one pediatrician currently practicing at a major Boston-based hospital who is currently earning a Master of Health Informatics and Analytics degree and a dentist with a Master of Public Health degree. Additionally, our team included one current Master of Health Information and Analytics degree candidate with a background in software engineering (and current employee at Mitre). Our team also consisted of a Master of Public Health and current first-year medical student with a background in epidemiology research. Our work was ultimately supported by our course instructor, Dr. Lisa Gualtieri, an expert in the field of digital health and creator of RecycleHealth, a non-profit organization which collects and distributes wearable activity trackers to underserved patient populations. Along with content experts from AARP, we leveraged the strengths and insights of all team members to develop a comprehensive, practical and novel digital solution to promote brain health among older adults wishing to age in place.
Introducing: MyHealthNetwork
Overview
MyHealthNetwork is the working title for the prototype of a digital health application which can store blood pressure readings as inputted by the primary user and share these data with additional stakeholders, including the primary user’s primary care physician (PCP), to detect changes that might predict the user’s risk for dementia (Figure 2). The application as designed will connect to a digital blood pressure cuff via Bluetooth, and users can manually input their data if they own a conventional blood pressure monitor. From the moment the primary user begins monitoring their blood pressure through the application, they will have access to a digital navigator, a chatbot, which can connect to a live person available for assistance to help answer non-urgent questions related to health and assist in using and connecting the app and blood pressure monitor.
Figure 2.
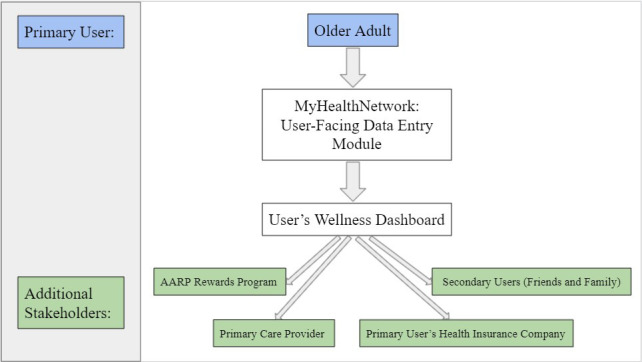
Flow chart describing the transmission of patient-generated health data from primary user into MyHealthNetwork to additional stakeholders.
After using MyHealthNetwork for at least thirty days, the primary user is alerted if their blood pressure readings diverge from normal values and will be encouraged to continue to monitor daily or seek medical care as needed. There will be an option to download the raw data onto their personal mobile device so that primary users can show this information to their PCP during their next appointment. During the later stages of piloting, MyHealthNetwork will be integrated into electronic health records so that the patient-generated health data will become part of the patient’s existing medical record. During times where blood pressure readings are consistently higher or lower than expected (but within non-life threatening levels), primary users will be prompted to contact their PCP to review the data. In cases where blood pressure readings reach dangerously high or low levels, primary users will be alerted to seek medical attention immediately.
MyHealthNetwork offers a feature through which the primary user can choose to share their blood pressure readings with family members and friends. The application was designed with this feature in mind based on a large body of research which indicates that older adults who have stronger social support tend to have healthier blood pressure levels [29,30].
Through conversations with AARP representatives, we learned about the AARP Loyalty Rewards Program which currently provides rewards for AARP members who provide data from their fitness trackers. As the AARP Loyalty Rewards Program is well-established, it would be a useful tool which could be integrated into our solution to encourage older adults to monitor their blood pressure and provide incentives to continue monitoring. Our app sends metadata (no user-generated raw data) to the AARP Rewards program on how often they are checking their blood pressure weekly. The primary user receives an alert from the app on the total number of points they have accumulated and could redeem a reward at the end of each month of monitoring.
In addition to AARP, the back-end of the application links to the primary user’s health insurance provider. Initially, we will partner with United Healthcare, as we learned from our conversations with AARP content experts that AARP already has an existing partnership with United Healthcare and trusts the health insurance company to securely store raw health-related data. Ideally, additional health insurance companies would consider collecting, storing and monitoring data output from MyHealthNetwork and potentially decrease annual premiums for primary users who demonstrate intentionality in maintaining their own health through consistent use of the product.
Dashboard Prototype
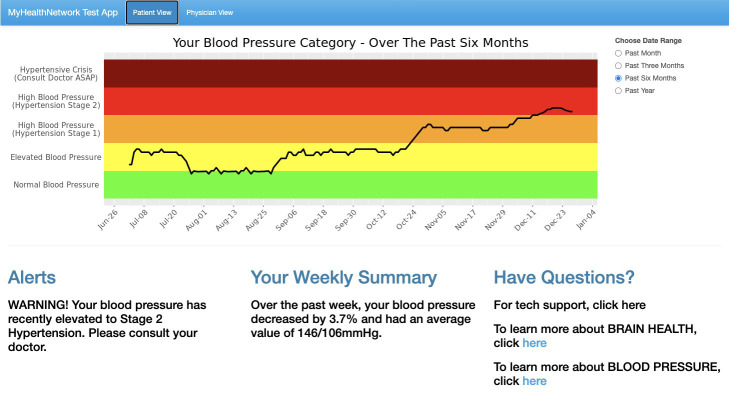
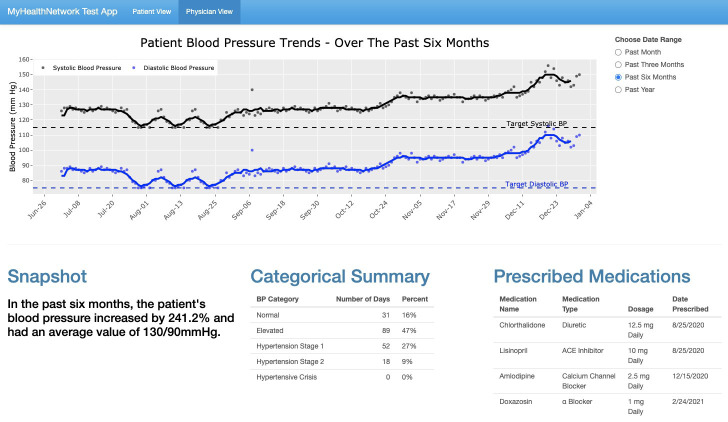
The authors developed a prototype to display the look and functionality of the wellness dashboard. The dashboard is a simple web application with two tabs, one depicting a view that the patient could access (see Figure 3) as well as a view for their physician (see Figure 4). Both views share a similar layout with a temporal plot of blood pressure data in the top half (with adjustable date ranges) and then three different summaries of data/information on the bottom half. The goal for both views is to allow for quick and easy interpretation of data relevant to each party.
Figure 3.
Patient View tab of the wellness dashboard prototype.
Figure 4.
Physician View tab of the wellness dashboard prototype.
The Patient View tab was designed with health literacy in mind, as interpreting blood pressure trends can be a complicated subject with multiple values to monitor over time. The bottom three summaries have large and easy to read text, covering the following three areas from left to right: (1) “Alerts”: displays either automated warnings if certain negative trends can be seen or messages directly from the doctor, (2) “Your Weekly Summary” - shows the percent change in blood pressure in the past week as well as the average value, and (3) “Have Questions?” - provides links to multiple resources, including technical support and educational modules centered on brain health and blood pressure. Through an AARP partnership, the Staying Sharp initiative, which is designed to offer curated educational content on brain health to older adults, would be linked here as well as an additional resource.
For the application to be successful, one of the most important features is the Patient View of blood pressure data. To be effective with users of varying degrees of health literacy, we knew a graphical approach was needed. Further, we recognized the necessity of having a display of long term trends in blood pressure since the underlying point is to see changes and trends in data..
After examining many mechanisms to help patients understand blood pressure readings, we believed that the color-coded blood pressure categories provided from the American Heart Association were the easiest to interpret, as they include a simple green, yellow, orange, red, and dark red scale for the following categories: Normal Blood Pressure, Elevated Blood Pressure, Hypertension Stage 1, Hypertension Stage 2, and Hypertensive Crisis. Each category is based on the value of both the systolic blood pressure (SBP) and diastolic blood pressure (DBP), with specific conditions that can be found at the American Heart Association’s website [31]. However, as authors we were challenged by the fact that there was no literature found on how to display these categories in a temporal view. The two main challenges included: (1) the need to include two inputs as opposed to one (SBP and DBP), meaning a single line for blood pressure on a plot over time could not be used, and (2) the American Heart Association blood categories do not have a numerical output that can be plotted on a y-axis over time. Therefore, we developed an algorithm to display the trends of a patient’s blood pressure readings in a single line over time.
The algorithm is based on taking in both blood pressure inputs (SBP and DBP) and calculating what is being defined as an alpha value, which is a number between 0 and 5 and will act as the y-axis value on a plot to describe what blood pressure category the two given inputs indicate. The final plot will have an x-axis for dates and a y-axis for blood pressure categories on a numerical scale from 0 to 5, with each category taking up a span of 1 unit. This results in the green Normal category spanning from 0 to 1, the yellow Elevated category spanning from 1 to 2, the orange Hypertension Stage 1 category spanning from 2 to 3, the red Hypertension Stage 2 category spanning from 3 to 4, and the Hypertensive Crisis Category spanning from 4 to 5. A line reflecting the seven day moving average of each value will be fitted to account for outliers.
Finding the alpha value is dependent on another value, delta, which takes into account where exactly the current blood pressure inputs fall within their category range - (for example, is the reading in the middle of the category’s range [i.e. SBP=125 in a scale of 120-129] or is it closer to the border of this category [i.e. SBP=128 along the same scale]). Therefore, we created the delta value (), a numerical value to represent a given blood pressure input’s position in its category’s range. There will be a delta value for both SBP and DBP, with the general equation for equating the delta value being the following:
In the delta equation, the “lower” and “upper” limits reflect the lowest and highest blood pressure readings in a given blood pressure range, respectively” For a given set of inputs, there will be a delta for both the SBP (δS) and for the DBP (δD). Table 1 summarizes how each delta value would be calculated for both SBP and DPB, showing the specific upper and lower limit values denoted by the American Heart Association (AHA).
One issue that we encountered, however, was that the highest category (Hypertensive Crisis) defined by the American Heart Association did not have upper limits, which are required for this algorithm to work. Therefore, upper limits were chosen based on the ranges of the previous category (Hypertension Stage 2). The total range for SBP in Hypertension Stage 2 was 40 mmHg, therefore that same range was used for δS, Hypertensive Crisis. The total range for DBP in Hypertension Stage 2 was 30 mmHg, therefore the same range was used for δD, Hypertensive Crisis.
| Blood Pressure Category | δS | δD |
| Normal | ||
| Elevated | ||
| Hypertension Stage 1 | ||
| Hypertension Stage 2 | ||
| Hypertensive Crisis |
Table 1. Delta values are defined as a numerical representation of where a given blood pressure value falls within its blood pressure category’s range on a scale of 0 to 1. This table represents the expressions used to calculate the delta value for both SBP (δS) and DBP (δD), which are based off of the American Heart Association’s Blood Pressure Category chart.
Because there are two delta values and only one can be used, we decided to choose the larger of the two values for the final delta value of a given category. This was decided on the basis that the goal of the visual display is to highlight potentially increasing trends in blood pressure readings and hoping to catch the user’s attention whenever possible. With a delta value found, the final alpha value will be that delta value added to a constant related to its given blood pressure category, since the final scale is from 0-5.
Below, the algorithm will be displayed three different times, with each successive time providing more granularity than the former. The following version is the highest level view, explaining the process of how an alpha value is calculated for a given input. It essentially includes five different “if” statements, with each one representing a different blood pressure category. As seen below, the delta value chosen is added to 0 for Normal Blood Pressure Category, 1 for Elevated Blood Pressure Category, and so on. For example, if the delta value of a given set of blood pressure inputs was found to be 0.6 and fell within the Hypertension Stage 1 category, its final alpha value would be 2 + 0.6, which would result in a y-value of 2.6 on the final graph.
The next version of the algorithm includes two more levels of granularity. The first inclusion is the specifics of what each blood pressure category is defined as based on SBP and DBP inputs. The second shows the math behind choosing the higher value between δS and δD, which is based off of the general equation below:
This equation is utilized below:
And finally, the equation below provides the highest level of granularity, where each delta value is replaced with the simplified expressions from Table 1. This is the final version that was used in the app development, with the only variables being the two inputs of SBP and DBP.
The Physician View was designed to integrate seamlessly and efficiently into clinical workflows with the ultimate goal of allowing a physician to get actionable insights on a patient’s blood pressure trends in under 30 seconds. As can be seen in Figure 3, the top graphical section shows the actual values for SBP (black) and DBP (blue) over time. The dots show the raw data inputs and the lines reflect the seven-day moving averages, allowing for outliers to be incorporated into the long term trends. The dotted black and blue dotted lines correspond to respective patient-centered SBP and DBP goals that can be set by the physician.
The bottom summaries provide information that was deemed most important from conversations with physician colleagues on this team. The bottom left shows the patient’s average blood pressure as well as percent change for the chosen date range. The middle summary shows how many days and what percentage of days a patient has been in each blood pressure category in the given timeline. This summary also updates whenever a date range is chosen. And finally, the bottom right summary lists all medications the patient is currently taking.
Development Process
To ensure the utility and technical fidelity of our digital health solution, we created a four-stage development process to introduce, test, refine and expand our product over a period of three years (Figure 5). Phase one will include a pilot program during which we will recruit the following groups to test the solution: primary end users (older adults aged 50 and over at risk for dementia) and primary care physicians interested in a digital solution for predicting adverse brain health conditions for their older adults. In phase one, primary users will collect and store their blood pressure data using the beta version of our application. Feedback will be collected from both primary users and their healthcare providers in the form of a survey during this time so that the application, still in development at this point, can be refined in response. Importantly, surveys dispersed to physicians will inquire as to how the data collected by the digital solution can best confer value to the physicians and their patients and minimize the burden of incorporating patient-generated data into their clinical workflow.
Figure 5.
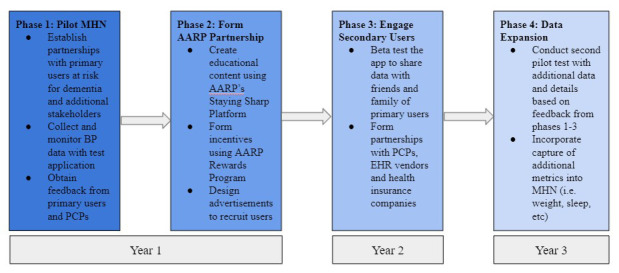
Phases of development for MyHealthNetwork (MHN)
During phase two of development, educational content will be created and integrated into the front end of the application for primary users and their caretakers to consume for the purpose of learning more about brain health and blood pressure. Educational content will be rooted in the six pillars of AARP’s Staying Sharp Platform. (Together, phases one and two will last for about one year after the beta version of the application has been developed). During phase two, we will work with AARP to integrate incentives to use MyHealthNetwork into the preexisting AARP Rewards Program. Potential incentives might include reduced annual AARP membership fees, the ability to earn points, redeemable for prizes or discounts at major retailers, and more. Finally, phase two will also include the development of advertisements targeted towards potential primary users and the secondary users who support them (including clinicians and the caretakers). By the end of phases one and two, we plan to have built our primary user base.
Phase three will begin during the second year of development. Phase three will focus mostly on engaging secondary users. During this phase, we will test sharing the data input by primary users with main secondary users: primary users’ healthcare providers and their caregivers at home. Additionally, this phase will be used to develop partnerships with physicians (mostly primary care providers for older adults), electronic health records vendors and health insurance companies, with all of whom we aim to share and store primary users’ recorded data. During this phase, we would survey healthcare practitioners once more to gather their impressions around the ease of use and utility of the patient-generated health data captured by MyHealthNetwork in their clinical workflow.
In Phase four, we would begin the fourth and final phase of development: data expansion. Based on feedback from the previous three phases, we would design and implement a second piloting process to test collection of additional health data metrics to predict brain health outcomes. These metrics could include weight, activity levels, heart rate, adherence to prescribed medication and more. By expanding the MyHealthNetwork application to store additional health metrics related to brain health, we aim to eventually create a holistic and comprehensive digital health solution which can mitigate the public health problem of poor brain health among older adults in the US.
Addressing barriers to adoption and/or use
Collectively, the four phases of development of our digital health solution address the four aforementioned barriers that the authors identified through literature review as well as interviews and conversations with potential primary users and AARP content experts, respectively. The first barrier we identified included the inability to understand health data among primary users with low health literacy. The inclusion of educational media in the application will enable primary users to find answers to their health-related questions quickly and conveniently without the need for consulting sources outside of the application. Secondly, we expect that using MyHealthNetwork consistently will be challenging at first for primary users with low digital literacy, defined as the ability to use information technologies for learning, work, and recreation [32]. For this reason, we have included a feature which guarantees primary users around-the-clock access to a Digital Navigator, an on-demand chatbot with whom users can ask technological questions around the proper use of the MyHealthNetwork application. Users will have the option to speak to a human digital navigator if they prefer it to the chatbot.
Additionally, we expect that potential primary end users with lack of access to devices able to access the internet for the purposes of health data input may be unable to fully utilize MyHealthNetwork. To counter this, we plan to initially provide smart blood pressure cuffs to the users in the pilot study at a reduced cost to primary users with financial need by pairing with smart blood pressure cuff companies, such as Withings, to purchase the devices in bulk at below market price. Finally, we learned that primary users and other stakeholders might have concerns about the security and primary of users’ personal and health data. To address this, we plan to partner with health insurance companies, beginning with United Healthcare with whom AARP has a pre-existing relationship and trusts to store sensitive user data. To address similar concerns among clinicians who will integrate MyHealthNetwork into their workflow, we plan to partner with credible EHR vendors whose operational practices meet our high standards for security and privacy of patient data.
Limitations
A number of limitations to our design thinking process should be noted, particularly within the context of this exercise being completed in a graduate course on Digital Health. Our most significant limitation includes our inability to launch and test the prototype of MyHealthNetwork with both primary end users and their healthcare providers in their homes and clinical environments, respectively. We were limited by the short time frame (one semester) during which the entire design thinking process took place. To address this limitation, we capitalized upon opportunities to gather feedback similar to that which we may have received through a true implementation of our solution, including interviews with potential primary users, conversations with AARP content experts and creation of a rudimentary prototype of MyHealthNetwork’s primary user-facing dashboard.
Additional limitations of our study include the use of a convenience sample for interviews of a small number of potential primary end users (n=4). However, we did make it a priority to represent a variety of races, sexes, ages, locations and literacy levels in our small sample of interviewees. Reaching new customers might present another challenge as the user base might reflect mostly individuals who are health-literate, digitally-literate and have a membership to the AARP; therefore, reaching potential primary users without a membership or with low health and/or digital literacy might be challenging. While we recognize that this might limit our ability to reach a broader group of users, we only limit our recruitment to members of the AARP during the pilot testing phase of our design process, after which we would work with clinicians involved in the pilot to attract harder-to-reach older adult populations. Additionally, we plan to have interactive educational video modules integrated into the MyHealthNetwork platform which will explain the medical and technical aspects of our solution to older adult primary users and their caretakers, facilitating ease of use for users with varying levels of health literacy.
Another limitation includes the acknowledgement that this final algorithm is not a perfect solution. It is a first attempt at temporally plotting something that has yet to be done so in mainstream medicine. It is not meant to give precise data points, but to show patients with potentially low health literacy a general idea of how healthy they are and where their health may be heading. This algorithm has the potential to continuously be improved upon to find the best approximation of blood pressure category over time. One area of improvement could be with the fact that we normalized each category into a span of 1 unit, even though the blood pressure ranges for each category vary. Another issue is the lack of an upper bound for the Hypertensive Crisis category, with other solutions potentially being a better fit.
Furthermore, we are presently limited by our lack of access to data that would predict how much a potential user would be willing to pay for the MyHealthNetwork. However, to address this limitation, we held discussions with AARP representatives during the design thinking process to consider how we could drive down costs and ensure that access to MyHealthNetwork is as inclusive as possible. Some ideas included partnering with a smart medical device manufacturer, buying hardware in bulk, offering discounts to AARP members and working with health insurance companies to create discounts to users in exchange for access to their private health data. Finally, the digital health solution would only have utility among users who have an internet connection and a device with connection to the internet to allow access to the platform. To address this limitation, we considered trying to partner with internet service providers who might be able to offer discounted prices to potential users in areas with low internet connectivity.
Future Directions
As previously mentioned, once a prototype of our solution is created, centered on the collection of blood pressure data, future phases of development will include expansion of the platform to capture additional metrics related to brain health including blood glucose levels, weight, physical activity, resting heart rate, sleep pattern and more [33-37]. These expanded features can capture richer insights about primary users’ brain health. We also intend to add a feature to future versions in which the user can input to the plot when each of their medications was newly prescribed, allowing for correlations to be made with different medical cocktails. Conversely, MyHealthNetwork can be refined over time so that users’ blood pressure readings can be used to predict additional outcomes beyond brain health alone, including heart attack, stroke and vision loss and more [38]. Additionally, opportunities for primary users to strengthen and maintain brain health will be provided as they collect and record more data, as studies show that using certain digital technologies can improve memory, fluid intelligence and other cognitive abilities [39].
A second future direction will include potentially partnering with technological companies which already store users’ health data with their permission. One such potential stakeholder could include Apple, who recently included the ability to securely share health and wellness data with select individuals, including loved ones and physicians, in their newest iPhone software update, iOS 15. Through a partnership such as this, we aim to eventually integrate our user-generated health database and wellness dashboard into iOS to promote ease of use for primary users who have access to an iPhone.
Finally, we plan to expand our digital health solution to accommodate use by individuals outside of the United States. Broadening our user base on a global scale may allow us to better mitigate the public health issue of poor brain health among older adults at a global level. Solutions to detect and prevent dementia are heavily needed outside of the US, particularly in Asian nations; for example, South Korean residents are currently expected to experience the longest lifespans of any nation, with a projected life expectancy of 90 years by 2030. Concurrently, cases of dementia are expected to triple on a global scale, from 47.5 million individuals affected in 2015 compared to 135.5 million in 2050 [40]. As older adult populations of this and other nations continue to grow, there will be a need for digital health solutions which can help empower older adults to maintain brain health in their homes.
Conclusion
In using the design thinking process to address the challenge of older adults who are concerned about brain health, we chose hypertension as a proxy and developed a prototype solution to target the needs of older adults. Given the well-studied association between healthy blood pressure and brain health [12], the authors hypothesized that if users actively monitor their blood pressure and review temporal trends along with their primary care physician, this could promote a healthier lifestyle and preserve their brain health.
Our aim was to design a user-friendly digital solution that would store and analyze the patient-generated health data. Our prototype ”MyHealthNetwork” is a digital solution which allows users to: 1) input and store daily blood pressure values, 2) over time visually monitor and review their blood pressure trends and 3) share the data with their primary care provider. The dashboard view was designed using our novel algorithm developed by the authors to display the blood pressure categories in a visually straightforward representation devoid of medical jargon. The algorithm provides a 7-day moving average that most users with limited health literacy would be able to understand and follow their blood pressure trends over time. Our application encourages shared decision-making between the user and physician with the goal of supporting users in their mission to maintain their brain health, age in place and ultimately lead healthier lives.
One challenge that we faced included developing an uncomplicated solution that would encourage patient engagement in the process of monitoring blood pressure and yield the secondary benefits of improving users’ health and digital literacy. The design thinking process guided us through each step from initial problem to ideation and building our solution. Our background research, defining user characteristics and stakeholders, real-life interviews with various points of view and discussions with AARP subject matter experts assisted us in identifying barriers for our primary end users and limitations of current technology. In addition, our group members had a variety of backgrounds in healthcare, engineering, public health research and technology, which proved advantageous in assembling our solution.
Future directions for our digital health solution include expansion of the platform to capture other health metrics, refinement of the algorithm to predict other health outcomes such as stroke, an increase in partnerships with technology companies for broader utilization and growth of our user base to include end users outside of the United States.
Our project highlights the value of involving end users and primary care physicians in the development process with the goal of continued participation in the long term. As the number of digital devices used to monitor health increases, the need to ensure that users have the health knowledge and technological skills to navigate is critical; for this reason, we incorporated a digital navigator in our application. Furthermore, our digital solution illustrates the need to advance integration of digital health technology into mainstream health care. Incorporating “Patient-Generated Health Data” effortlessly into health care systems could have the positive effects of healthier individuals and potentially shift health management and treatment from reactionary to prevention medicine.
Acknowledgments
The authors would like to thank Alison Bryant, PhD, Senior Vice President, AARP Research & Enterprise Lead, Tech & Digital Equity, for her contribution to this study by proposing the original challenge which inspired this work. We appreciate her guidance and feedback throughout the design thinking process.
Appendix A: Interview Questions
Establishing baseline health care practices and resources
1. What do you do when you have a health question or concern? (see a doctor, go to the ER, urgent care clinic, ask a friend, search the internet)
2. Where do you go for health care? Do you have a doctor or health care provider that you see when you are ill? Do you have regular check-ups (annually) or only seek care when you don’t feel well?
3. Is there anything that holds you back in having regular checkups with a doctor? (transportation, mobility, time, insurance coverage, cost)
Establishing awareness/impact of patient’s memory issues
4. In the last month, how often did forgetting something interfere with your daily activities?
(everyday, most days, somedays, rarely, or never)
5. Can you describe a specific instance of being “forgetful”? Or have you been worried about someone else’s memory? (family member, friend?
6. How do you feel when you have these lapses in memory? Why? (worries, anxious, frustrate)
Establishing interviewee’s concern about any memory/independence
7. How often are you worried about your forgetful moments? Have they ever made you worry about your ability to be independent?
a. If often: Have you ever done anything about it? Have you mentioned it to your doctor?
Establishing interviewee’s motivation to explore an intervention
8. How interested would you be in learning about a tool that can help your mind stay sharper? Very interested, somewhat interested, or not at all?
Establishing health literacy
9. Did you know that blood pressure has been linked with many aspects of health, including memory loss?
10. Do you know how to take your blood pressure? If so, do you know how to interpret what your blood pressure means?
Establishing digital literacy
11. What technology do you currently use? (smartphone, wearable)
a. If none: Why not? (internet connection)
12. Do you use any digital health application currently? (patient portal, activity tracker)
a. If none: Why not?
Establishing openness to home-based monitoring and data sharing
13. If you had a device that could monitor your blood pressure daily easily, would you be interested in doing that?
a. If yes: Would you want to look at the data you collected? Would you be interested in sharing this information with your PCP? With you family members?
14. What other aspects of your health and daily life would you be comfortable recording and/or sharing? (weight, food, activity, mood, sleep)
15. What would you like to know before you try such a device at home? Would it help to have some simple instructions on how to use it? Would you prefer to have someone to talk with to go over setting up/using the device?
References
- 1.Office of Disease Prevention and Health Promotion. 2020. Older Adults. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/older-adults. Accessed May 22, 2021.
- 2.Population Reference Bureau. 2019. Fact Sheet: Aging in the United States. Available at: https://www.prb.org/resources/fact-sheet-aging-in-the-united-states/. Accessed: June 14, 2021.
- 3.Ausubel J. 2020. Older people are more likely to live alone in the U.S. than elsewhere in the world. Available at: https://www.pewresearch.org/fact-tank/2020/03/10/older-people-are-more-likely-to-live-alone-in-the-u-s-than-elsewhere-in-the-world/. Accessed: May 17, 2021.
- 4.Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, et al. 2020. Trends in Blood Pressure Control Among US Adults With Hypertension, 1999-2000 to 2017-2018. JAMA. 324(12), 1190-200. doi:. 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davey J, de Joux V, Nana G, Arcus M. Accommodation Options for Older People in Aotearoa/New Zealand. Center for Housing Research Aotearoa/New Zealand (CHRANZ). June 2004. Available at: https://www.beehive.govt.nz/sites/default/files/Accomodation%20Options%20for%20Older%20People.pdf. Accessed May 29, 2021.
- 6.Farber N, Lynott J. Aging in Place: A State Survey of Livability Policies and Practices. National Conference of State Legislatures and the AARP Public Policy Institute. December 2011. Available at: https://assets.aarp.org/rgcenter/ppi/liv-com/ib190.pdf. Accessed July 1, 2021.
- 7.Healthy Aging. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/aging/pdf/perceptions_of_cog_hlth_factsheet.pdf. Accessed June 22, 2021.
- 8.What is Dementia? Symptoms, Types, and Diagnosis. National Institutes of Health, National Institute on Aging. Available at: https://www.nia.nih.gov/health/what-dementia-symptoms-types-and-diagnosis. Accessed June 11, 2021.
- 9.Alzheimer’s Disease. Mayo Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/symptoms-causes/syc-20350447. Accessed June 11, 2021.
- 10.Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, et al. 2011. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging - Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7(3), 280-92. doi:. 10.1016/j.jalz.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thinking About Brain Health. University of Michigan, National Poll on Healthy Aging. Available at: https://www.healthyagingpoll.org/reports-more/report/thinking-about-brain-health. Accessed June 11, 2021.
- 12.Gorelick PB, Furie KL, Iadecola C, Smith EE, Waddy SP, et al. 2017. Defining Optimal Brain Health in Adults: A Presidential Advisory From the American Heart Association/American Stroke Association. Stroke. 48, e284-303. doi:. 10.1161/STR.0000000000000148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakakura K, Ishikawa J, Okuno M, Shimada K, Kario K. 2007. Exaggerated Ambulatory Blood Pressure Variability Is Associated with Cognitive Dysfunction in the Very Elderly and Quality of Life in the Younger Elderly. Am J Hypertens. 20(7), 720-27. doi:. 10.1016/j.amjhyper.2007.02.001 [DOI] [PubMed] [Google Scholar]
- 14.Nagai M, Hoshide S, Ishikawa J, Shimada K, Kario K. 2008. Ambulatory blood pressure as an independent determinant of brain atrophy and cognitive function in elderly hypertension. J Hypertens. 26(8), 1636-41. doi:. 10.1097/HJH.0b013e3283018333 [DOI] [PubMed] [Google Scholar]
- 15.Gottesman RF, Schneider AL, Albert M, Alonso A, Bandeen-Roche K, et al. 2014. Midlife Hypertension and 20-Year Cognitive Change: The Atherosclerosis Risk in Communities Neurocognitive Study. JAMA Neurol. 71(10), 1218-27. doi:. 10.1001/jamaneurol.2014.1646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McLaughlin JE, Wolcott MD, Hubbard D, Umstead K, Rider TR. 2019. A qualitative review of the design thinking framework in health professions education. BMC Med Educ. 19(98). doi:. 10.1186/s12909-019-1528-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.High Blood Pressure. National Institutes of Health, National Heart, Lung, and Blood Institute. Available at: https://www.nhlbi.nih.gov/health-topics/high-blood-pressure. Accessed May 16, 2021.
- 18.Graffigna G, Barello S, Riva G, Bosio AC. 2014. Patient Engagement: The Key to Redesign the Exchange Between the Demand and Supply for Healthcare in the Era of Active Ageing. Stud Health Technol Inform. 203, 85-95. [PubMed] [Google Scholar]
- 19.Lloyd A, Bonner A, Dawson-Rose C. 2013. The health information practices of people living with chronic health conditions: Implications for health literacy. J Librarian Inform Sci. 46(3), 207-16. doi:. 10.1177/0961000613486825 [DOI] [Google Scholar]
- 20.About ONC. HealthIT.gov. Available at: https://www.healthit.gov/topic/about-onc. Accessed July 22, 2021.
- 21.Wu DT, Xin C, Bindhu S, Xu C, Sachdeva J, et al. 2020. Clinician Perspectives and Design Implications in Using Patient-Generated Health Data to Improve Mental Health Practices: Mixed Methods Study. JMIR Form Res. 4(8), e18123. doi:. 10.2196/18123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steele R, Lo A, Secombe C, Wong YK. 2009. Elderly persons’ perception and acceptance of using wireless sensor networks to assist healthcare. Int J Med Inform. 78(12), 788-801. doi:. 10.1016/j.ijmedinf.2009.08.001 [DOI] [PubMed] [Google Scholar]
- 23.Wild K, Boise L, Lundell J, Foucek A. 2008. Unobtrusive In-Home Monitoring of Cognitive and Physical Health: Reactions and Perceptions of Older Adults. J Appl Gerontol. 27(2), 181-200. doi:. 10.1177/0733464807311435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boise L, Wild K, Mattek N, Ruhl M, Dodge H, et al. 2013. Willingness of older adults to share data and privacy concerns after exposure to unobtrusive in-home monitoring. Gerontechnology (Valkenswaard). 11(3), 428-35. doi:. 10.4017/gt.2013.11.3.001.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chronic Care. A Call to Action for Health Reform - Chronic Conditions Among Older Americans. American Association of Retired Persons. Available at: https://assets.aarp.org/rgcenter/health/beyond_50_hcr_conditions.pdf. Accessed June 11, 2021.
- 26.Sauve L, Renaud L, Kaufman D, Duplaa E. 2016. Can Digital Games Help Seniors Improve Their Quality of Life? Commun Comput Inf Sci. 739. doi:. 10.5220/0005800200940102 [DOI] [Google Scholar]
- 27.Pugh NE, Hadjistavropoulos HD, Klein B, Austin DW. 2014. A Case Study Illustrating Therapist-Assisted Internet Cognitive Behavior Therapy for Depression, Cognitive and Behavioral Practice. Cognit Behav Pract. 21(1), 64-77. doi:. 10.1016/j.cbpra.2013.08.002 [DOI] [Google Scholar]
- 28.Barnes DE, Zhou J, Walker RL, Larson EB, Lee SJ, et al. 2020. Development and Validation of eRADAR: A Tool Using EHR Data to Detect Unrecognized Dementia. J Am Geriatr Soc. 68(1), 103-11. doi:. 10.1111/jgs.16182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanchez-Martínez M, López-García E, Guallar-Castillón P, Cruz JJ, Orozco E, et al. 2016. Social support and ambulatory blood pressure in older people. J Hypertens. 34(10), 2045-52. doi:. 10.1097/HJH.0000000000001036 [DOI] [PubMed] [Google Scholar]
- 30.Piferi RL, Lawler KA. 2006. Social support and ambulatory blood pressure: An examination of both receiving and giving. Int J Psychophysiol. 62(2), 328-36. doi:. 10.1016/j.ijpsycho.2006.06.002 [DOI] [PubMed] [Google Scholar]
- 31.Understanding Blood Pressure Readings. American Heart Association. Available at: https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings. Accessed June 11, 2021.
- 32.Ba H, Tally W, Tsikalas K. 2002. Investigating Children’s Emerging Digital Literacies. J Technol Learn Assess. 1(4). https://ejournals.bc.edu/index.php/jtla/article/view/1670. [Google Scholar]
- 33.Crane PK, Walker R, Hubbard RA, Li G, Nathan DM, et al. 2013. Glucose levels and risk of dementia. N Engl J Med. 369(6), 540-48. doi:. 10.1056/NEJMoa1215740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma Y, Ajnakina O, Steptoe A, Cadar D. 2020. Higher risk of dementia in English older individuals who are overweight or obese. Int J Epidemiol. 49(4), 1353-65. doi:. 10.1093/ije/dyaa099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou Z, Fu J, Hong YA, et al. 2017. Association between exercise and the risk of dementia: results from a nationwide longitudinal study in China. BMJ Open. 7, e017497. doi:. 10.1136/bmjopen-2017-017497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang S, Fashanu OE, Zhao D, Guallar E, Gottesman RF. 2019. Relation of Elevated Resting Heart Rate in Mid-Life to Cognitive Decline Over 20 Years (from the Atherosclerosis Risk in Communities [ARIC] Study). Am J Cardiol. 123(2), 334-40. doi:. 10.1016/j.amjcard.2018.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sabia S, Fayosse A, Dumurgier J, van Hees VT, Paquet C, et al. 2021. Association of sleep duration in middle and old age with incidence of dementia. Nat Commun. 12, 2289. doi:. 10.1038/s41467-021-22354-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.High blood pressure (hypertension). Mayo Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410. Accessed July 3, 2021.
- 39.Small GW, Lee J, Kaufman A, Jalil J, Siddarth P, et al. 2020. Brain health consequences of digital technology use. Dialogues Clin Neurosci. 22(2), 179-87. doi:. 10.31887/DCNS.2020.22.2/gsmall [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dementia: A Public Health Priority. World Health Organization. Available at: https://www.who.int/mental_health/neurology/dementia/dementia_thematicbrief_executivesummary.pdf. Accessed July 3, 2021.