Abstract
Background
Valid assessment of drug efficacy and safety requires an evidence base free of reporting bias. Using trial reports in Food and Drug Administration (FDA) drug approval packages as a gold standard, we previously found that the published literature inflated the apparent efficacy of antidepressant drugs. The objective of the current study was to determine whether this has improved with recently approved drugs.
Methods and findings
Using medical and statistical reviews in FDA drug approval packages, we identified 30 Phase II/III double-blind placebo-controlled acute monotherapy trials, involving 13,747 patients, of desvenlafaxine, vilazodone, levomilnacipran, and vortioxetine; we then identified corresponding published reports. We compared the data from this newer cohort of antidepressants (approved February 2008 to September 2013) with the previously published dataset on 74 trials of 12 older antidepressants (approved December 1987 to August 2002).
Using logistic regression, we examined the effects of trial outcome and trial cohort (newer versus older) on transparent reporting (whether published and FDA conclusions agreed). Among newer antidepressants, transparent publication occurred more with positive (15/15 = 100%) than negative (7/15 = 47%) trials (OR 35.1, CI95% 1.8 to 693). Controlling for trial outcome, transparent publication occurred more with newer than older trials (OR 6.6, CI95% 1.6 to 26.4). Within negative trials, transparent reporting increased from 11% to 47%.
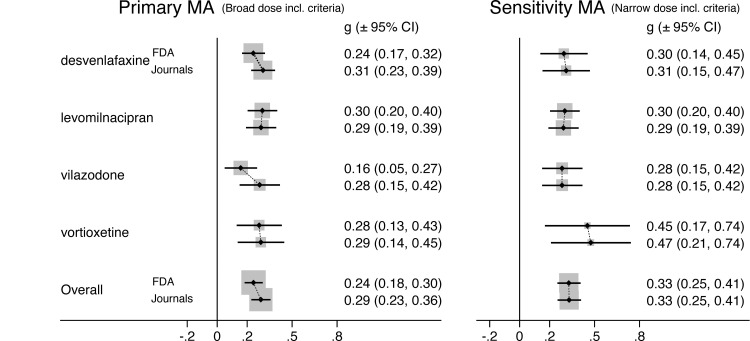
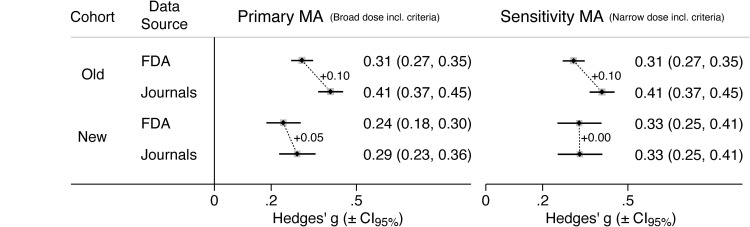
We also conducted and contrasted FDA- and journal-based meta-analyses. For newer antidepressants, FDA-based effect size (ESFDA) was 0.24 (CI95% 0.18 to 0.30), while journal-based effect size (ESJournals) was 0.29 (CI95% 0.23 to 0.36). Thus, effect size inflation, presumably due to reporting bias, was 0.05, less than for older antidepressants (0.10).
Limitations of this study include a small number of trials and drugs—belonging to a single class—and a focus on efficacy (versus safety).
Conclusions
Reporting bias persists but appears to have diminished for newer, compared to older, antidepressants. Continued efforts are needed to further improve transparency in the scientific literature.
Author summary
Why was this study done?
➢ Clinicians and researchers depend on the peer-reviewed literature for accurate assessments of drug efficacy and safety, but this depends on whether the outcomes of all trials—negative, as well as positive—are reported transparently.
➢ In an earlier study, using Food and Drug Administration (FDA) review documents as a gold standard, we found that many negative trials had been misreported in the published literature as having positive outcomes or had simply not been published.
➢ Since then, reporting bias has been the subject of additional studies and policy changes, raising the question, Is the antidepressant literature now being reported more transparently?
What did the researchers do and find?
➢ Using FDA reviews on 4 newer antidepressants, we identified 30 trials, half with positive, and half with negative, outcomes.
➢ Among the 15 negative trials, 6 were unpublished and 2 others were misreported as positive. Seven other negative trials (47%) were reported transparently (as negative), an improvement over the low (11%) rate found earlier with the older antidepressants.
➢ Statistical comparison of the newer and older drug datasets indicated that transparent reporting had improved overall, mainly among negative trials. Yet compared to positive trials, the rate of transparent reporting for negative trials remains low.
➢ Using meta-analysis to compare drug efficacy based on FDA versus published data, we found less inflation of drug efficacy among newer, compared to older, antidepressants.
What do these findings mean?
➢ Reporting bias persists but appears to have diminished for newer, compared to older, antidepressants.
➢ We do not know whether these results extend to drugs beyond the antidepressants studied here, nor do we know whether they extend to drug safety, as opposed to efficacy.
➢ Reporting bias remains a significant impediment to researchers and medical decision-makers, so further efforts are needed to improve transparent reporting in the scientific literature.
Introduction
Reporting bias can lead to overestimates of efficacy and/or underestimates of harms and thus undermine the evidence base regarding drugs and other interventions. Reporting bias takes several forms, including study publication bias and outcome reporting bias [1]. With study publication bias, entire studies are published or not depending on their results; with outcome reporting bias, studies are published but their outcomes are reported selectively depending on their results.
One of the early studies on reporting bias in antidepressant trials was published by our group [2]. Examining 12 second-generation antidepressants approved by the Food and Drug Administration (FDA) between 1986 and 2004, we found strong evidence for both study publication bias and outcome reporting bias. Because drug companies must report results of all Phase II/III trials to the FDA in order to gain approval for a new drug, FDA review documents can be considered a gold standard, an unbiased sample of all studies undertaken. Compared to trial results in FDA review documents, results published in journals inflated the apparent efficacy of antidepressants over placebo both in terms of proportion of positive trials and effect size (ES).
Using similar methodology, evidence for reporting bias has also been found among drugs for the treatment of schizophrenia [3] and of anxiety disorders [4], although not to the extent observed in antidepressant trials. Nor is reporting bias limited to psychotropic drugs—it has been documented for both pharmacological and nonpharmacological interventions across medical indications [5–9], and it appears to exist in social, biological, and physical sciences, as well [10].
An examination of papers published in all disciplines between 1990 and 2007 suggested an increase in reporting bias over time [10]. Since then, however, there have been important transparency-related policy changes, such as requirements for registration of clinical trials in 2005 [11,12] and for reporting of the trial results mandated by the Food and Drug Administration Amendments Act (FDAAA) of 2007 [13], and recent work suggests that the level of transparency has improved [14,15].
This raises the question, has the level of transparency of clinical trials changed specifically for the drugs for which reporting bias has perhaps been best described, namely antidepressants? Since our 2008 publication, several new antidepressant drugs have entered the United States market. Using the earlier study of older antidepressants for comparison, the current study aims to similarly determine whether, and to what degree, the apparent efficacy of the newer drugs has been inflated in published journal articles. More specifically, it asks, does trial outcome (positive or not) still influence whether and how the trial is reported? And does reporting bias still inflate ES?
Methods
Data procurement
FDA-registered trials
This study extends the methodology of a previously published study of reporting bias, which examined 74 trials of 12 older antidepressants [2]. Using medical and statistical reviews within FDA drug approval packages (https://www.accessdata.fda.gov/scripts/cder/daf/) [16], we identified all Phase II or Phase III double-blind placebo-controlled acute monotherapy trials for major depressive disorder on 4 newer antidepressants (Table 1).
Table 1. List of antidepressants included in the older and newer cohorts of RCTs.
| Drug group and cohort of RCTs | Approval date | Generic name | Brand name |
|---|---|---|---|
| Older [2] | December 1987 | fluoxetine | Prozac |
| December 1992 | paroxetine | Paxil | |
| December 1993 | venlafaxine | Effexor | |
| December 1994 | nefazodone | Serzone | |
| June 1996 | mirtazapine | Remeron | |
| October 1996 | bupropion sustained release | Wellbutrin SR | |
| July 1997 | sertraline | Zoloft | |
| October 1997 | venlafaxine extended release | Effexor XR | |
| July 1998 | citalopram | Celexa | |
| December 1999 | paroxetine controlled release | Paxil CR | |
| August 2002 | escitalopram | Lexapro | |
| Newer | February 2008 | desvenlafaxine | Pristiq |
| January 2011 | vilazodone | Viibryd | |
| July 2013 | levomilnacipran | Fetzima | |
| September 2013 | vortioxetine | Trintellix |
RCT, randomized controlled trial.
Literature search
Having identified the inception cohort of premarketing trials registered with the FDA, we used PubMed to search for matching publications reasonably discoverable by clinicians. Example search syntax for one drug was “desvenlafaxine[title] placebo (“major depressive disorder” OR “major depression”).” From the search output, titles and abstracts were screened to include journal articles focused on the overall efficacy of the drug in question for major depressive disorder; thus, we excluded articles focused on other indications, subsets with specific comorbid conditions, particular symptom clusters, safety (as opposed to efficacy), specific demographic samples, trials lacking a parallel design (add-on, open-label, crossover), trials that were not placebo controlled, trials not involving acute treatment (long-term trials, including maintenance trials), and trials involving other routes of administration. A literature search for the FDA-registered trials was also carried out independently by author YD in the context of a separate publication [17]. Separately, TF and YO identified the trials in ClinicalTrials.gov using the “Other Study ID Numbers” field and identified corresponding publications using the “Publication of Results” field. Matching of FDA-registered trials to publications was confirmed using trial design, duration, drugs used (study drug, placebo, active comparator), and number of participants randomized to each treatment arm. The preferred publication type was a stand-alone article, an article reporting on a single trial, with exceptions allowed as previously described [3].
Confirmation of nonpublication
For desvenlafaxine and vilazodone, we were unable to identify publications corresponding to all of the FDA-registered trials, so following a method reported previously [3], we searched for bibliographic information on said trials within recent review articles [18–23], whose authors made use of additional databases, including EMBASE [18,22], ClinicalTrials.gov [22,23], and Cochrane Central [18]. Additionally, the authors of one article contacted the sponsor [22], and the authors of another article were employees of the sponsor [20].
Data extraction
As with previous studies [2,3], we employed double data extraction and entry. Data were extracted and entered by 3 teams (ET with 3 assistants; YD; TF and YO), compared using Boolean formulas in Excel, and reconciled for any discrepancies. For each trial, we extracted the results on the primary outcome from the FDA reviews, including the summary statistics and the FDA reviewer’s judgment as to whether the trial was positive, i.e., whether it provided “substantial evidence of effectiveness” for purposes of marketing approval [24].
From the corresponding journal articles, consistent with our previous study of the apparent (to the average clinician-reader) efficacy of antidepressants [2],we extracted the summary statistics on the apparent primary outcome. This was defined as the drug–placebo comparison highlighted as the trial’s main result by virtue of its being reported first in the article’s results section.
Data analysis
Descriptive examination of trial results
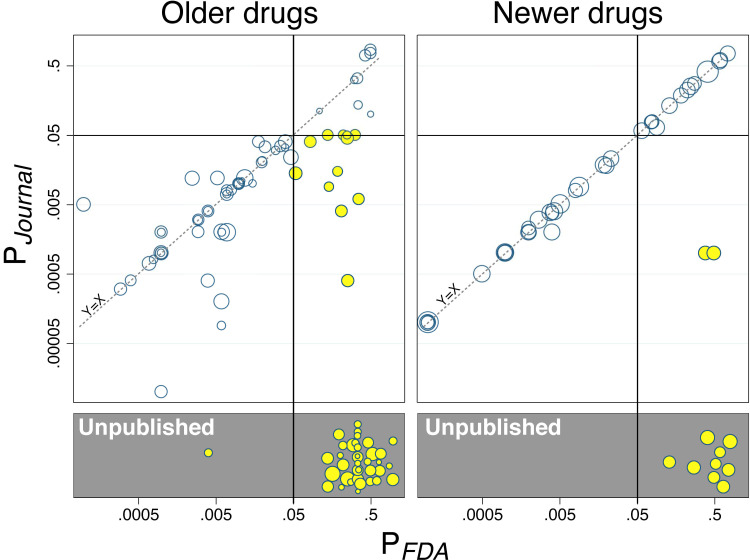
Many trials consisted of 2 or more treatment arms compared to a common placebo group, resulting in 2 or more P values. Treatment-arm-level P values reported by the FDA (PFDA) were compared to P values reported in corresponding journal articles (PJournal). Because of nonindependence (the same placebo group could be represented in 2 or more datapoints), they were examined descriptively in the form of scatterplots, one for each cohort of trials. The scatterplots necessarily excluded treatment arms whose results were not published (no PJournal values).
Transparent publication
We considered a trial to be published transparently if the trial was published in a way that was consistent with the FDA report of that trial. Transparent publication was deemed absent when (a) the trial results were not published (study publication bias) or (b) the results were published but in a way that conflicted with the FDA report (outcome reporting bias). For example, if a trial was reported by the FDA to be negative (nonsignificant on the primary outcome), but the publication conveyed a positive overall result by emphasizing statistically significant results in the beginning of the results section (see above re apparent primary outcome) and the abstract, that trial was deemed not transparently published.
We examined 2 predictors of transparent publication. The first was trial cohort (i.e., older versus newer antidepressants). The second was trial outcome according to the FDA report—positive (study drug clearly statistically superior to placebo on the primary outcome) or not positive. The main model also included a third variable for the interaction between the first 2 predictors. To estimate the associations, within Stata 11 [25], we employed Firth (penalized) logistic regression using the module firthlogit [25–27]. As a secondary analysis, we employed exact logistic regression [26] using the module exlogistic [25]. (These methods were chosen because, in the context of rare events, such as FDA-positive trials that are not transparently published, standard logistic regression fails. Please see S1 Text for elaboration.) We also undertook the following post hoc univariable analyses: Because transparent publication is arguably more likely to occur with positive than negative trials, we examined the effect of cohort within each of these subsets; similarly, we examined the effect of trial outcome within each cohort.
Meta-analysis of effect sizes
The meta-analysis portion of this study is reported as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guideline (S1 Checklist).
We examined whether reporting bias misinformed the public by comparing one meta-analysis (MA) using trial data obtained from FDA reviews to a second MA using data from the corresponding publications. The MAs were conducted using the metan module in Stata 11 [25], with random effects pooling and the DerSimonian–Laird estimator for heterogeneity. The resulting effect measures (standardized mean difference Hedges’ g ± 95% confidence interval) obtained by author ET were verified against those obtained independently by author YD. As in previous work [2–4], for each multiple-dose trial, we used fixed effects MA to obtain a single trial-level ES; to avoid a spuriously low standard error, each trial’s shared placebo n was counted once rather than redundantly for each dose group.
We then compared the results of the MAs, with effect size inflation (ESI), presumably due to reporting bias, calculated as journal-based ES (ESJournal) minus FDA-based ES (ESFDA). To facilitate visual comparison of these values, we exported the Stata-generated forest plots to vector-based graphics software (Intaglio version 3.9), which allowed corresponding ESFDA and ESJournal values to be placed alongside one another. Such pairwise forest plots were generated showing ES values at the level of trial, drug, and cohort.
Because journal-based ES and FDA-based ES are not independent (both derived from the same set of trials), we did not perform a formal statistical comparison through, for instance, meta-regression. As an exploratory method, we did perform multivariate MA, which is capable of handling such dependency, but it is limited in another respect. As explained further in the Supporting information, multivariate MA relies on the correlation between paired FDA-based and journal-based ES values, and complete pairs exist for published trials but not for unpublished trials. Because unpublished trials, compared to published trials, are much more likely to be negative and have systematically smaller ES values [2], journal-based ES values are missing not at random. Thus, the multivariate approach is less well suited to the examination of study publication bias than to outcome reporting bias. Because our dataset contains both of these forms of reporting bias, results of the multivariate MA are provided as Supporting information (S1 Text and S8 Fig).
We included only doses approved by the FDA, as reflected in the Dosage and Administration section of the product label. While this wording in this section was clear in many cases, in others, it was ambiguous; thus, for certain doses, arguments could be made for both inclusion and exclusion. We resolved this by conducting a primary MA using broad dose inclusion criteria and a sensitivity MA using narrow or restrictive dose inclusion criteria. For rationale and elaboration, please see legend to Table 2 and Table C in S1 Text. As explained in the latter, for dose reasons, one trial (vilazodone #244) was excluded from both MAs.
Table 2. FDA-registered trials and corresponding publications for cohort of 4 newer antidepressants.
| Drug | Trial Number | Registry Identifier | Total N | Dose Groups[n] | Comparator [n] | Trial Outcome per FDA | Publication |
|---|---|---|---|---|---|---|---|
| Desvenlafaxine | 223 | n/a | 213 | 200 mg1 [63], 400 mg1[72], pbo[78] | — | Negative | |
| 304 | NCT00063206 | 234 | ’100 mg or 200 mg’ 1[120], pbo[114] | — | Negative | Liebowitz 2007 [47] | |
| 306 | NCT00072774 | 461 | 100 mg1[114], 200 mg1[116], 4001[113], pbo[118] | — | Positive | DeMartinis 2007 [48] | |
| 308 | n/a | 369 | 200 mg1[121], 4001[124], pbo[124] | — | Positive | Septien-Velez 2007 [49] | |
| 309 | NCT00090649 | 364 | ’200 or 400 mg’ 1[110], pbo[120] | Venlafaxine “75 or 150 mg” [127] | Negative | Lieberman 2008 [27] | |
| 317 | NCT00087737 | 350 | ’200 or 400 mg’ 1[110], pbo[125] | Venlafaxine “150 or 225 mg” [115] | Negative | ||
| 320 | n/a | 235 | ’200 or 400 mg’ 1[117], pbo[118] | — | Negative | Feiger 2009 [50] | |
| 332 | NCT00277823 | 447 | 50 mg2[150], 100 mg1[147], pbo[150] | — | Positive | Liebowitz 2008 [51] | |
| 333 | NCT00300378 | 483 | 50 mg2[164], 100 mg1[158], pbo[161] | — | Positive | Boyer 2008 [52] | |
| Levomilnacipran | F02695 LP 202 | EudraCT 2006-002404-3 | 553 | 75 mg-100 mg2[277],pbo[276] | __ | Positive | Montgomery 2013 [53] |
| Levomilnacipran (cont’d) | LVM-MD-01 | NCT00969709 | 713 | 40 mg2[178],80 mg2[179],120 mg2[180],pbo[176] | __ | Positive | Asnis 2013 [54] |
| LVM-MD-02 | NCT00969150 | 357 | 40 mg-120 mg2[175],pbo[182] | __ | Negative | Gommoll 2014 [55] | |
| LVM-MD-03 | NCT01034462 | 434 | 40 mg-120 mg2[222],pbo[220] | __ | Positive | Sambunaris 2014 [56] | |
| LVM-MD-10 | NCT01377194 | 562 | 40 mg2[188],80 mg2[188],pbo[186] | __ | Positive | Bakish 2014 [57] | |
| Vilazodone | CLDA-07-DP-02 | NCT00683592 | 468 | 40 mg2[235],pbo[233] | __ | Positive | Khan 2011 [58] |
| GNSC-04-DP-02 | NCT00285376 | 409 | 40 mg2[205],pbo[204] | __ | Positive | Rickels 2009 [59] | |
| 244 | n/a | 289 | 20 mg-100 mg0[86], pbo[95] |
Fluoxetine 20 mg [89] | Negative | Not published | |
| 245 | n/a | 517 | 10–20 mg1[104],40–60 mg1[97],80–100 mg0[93],pbo[99] | Fluoxetine 20 mg [92] | Negative | Not published | |
| 246 | n/a | 483 | 10 mg0[119],20 mg1[121],pbo[128] | Citalopram 20 mg [115] | Negative | Not published | |
| 247 | n/a | 228 | 5 mg-20 mg1[113],pbo[115] | __ | Negative | Not published | |
| 248 | n/a | 533 | 20 mg1[132],10 mg0[133],5 mg0[140],pbo[128] | __ | Negative | Not published | |
| Vortioxetine | 303 | NCT00672958 | 597 (tx’d) | 5 mg1[299],Pbo[298] | — | Negative | Jain 2013 [60] |
| 304 | NCT00672620 | 611 (tx’d) | 2.5 mg0[153], 5 mg1[153], pbo[153] | Duloxetine 60 mg [152] | Negative | Mahableshwarkar 2013 [61] | |
| 305 | NCT00735709 | 560 | Pbo[140], 1 mg0[140], 5 mg1[140], 10 mg1[140] | — | Positive | Henigsberg 2012 [62] | |
| 315 | NCT01153009 | 591 | 15 mg1[145],20 mg2[147],pbo[153] | Duloxetine 60 mg [146] | Positive | Mahableshwarkar 2015(a) [63] | |
| 316 | NCT01163266 | 457 | 10 mg1[154],20 mg2[148],pbo[155] | — | Positive | Jacobsen 2015 [64] | |
| 317 | NCT01179516 | 434 (tx’d) | 10 mg1[143],15 mg1[142],Pbo[149] | — | Negative | Mahableshwarkar 2015(b) [65] | |
| 11492A | NCT00839423 | 425 | 5 mg1[108], 10 mg1[100], pbo[105] | Venlafaxine 225 mg [112] | Positive | Alvarez 2012 [66] | |
| 11984A | NCT00635219 | 766 (tx’d) | 2.5 mg0[155], 5 mg1[155], 10 mg1[151] | Duloxetine 60 mg [149] | Negative | Baldwin 2012 [67] | |
| 13267A | NCT01140906 | 604 | 15 mg1[149],20 mg2[151],pbo[158] | Duloxetine 60 mg [146] | Positive | Boulenger 2014 [68] |
Sample sizes (N/n) are number randomized unless specified as treated (“tx’d”). Superscripts in Dose Groups column correspond to dose inclusion levels explained in Table C in S1 Text.
0Dose group included in neither MA (excluded from both).
1Dose group included in primary MA.
2Dose group included in both primary and sensitivity MAs.
FDA, Food and Drug Administration; MA, meta-analysis.
Results
The FDA-registered trials and their corresponding publications are listed in Table 2. For the cohort of 4 newer antidepressants, there were 30 applicable trials with 13,747 participants, while for the cohort of older antidepressants, there were 74 applicable trials with 12,564 participants. Median trial sample sizes for the newer and older cohorts were 439.5 and 147.5, respectively (Z = 6.72, P < 0.001 by Wilcoxon rank-sum test), different by a factor of 3.
Results at level of treatment arm
The total number of treatment arms was 149, with 101 and 48 in the older and newer cohorts, respectively. Fig 1 plots the P values of all these arms against placebo as reported in the journals versus as confirmed in FDA reviews: It shows, among the 104 published treatment arms, a greater proportion of treatment arms lying along the Y = X (PJournal = PFDA) diagonal in the newer cohort, i.e., greater concordance between journal- and FDA-based data. The proportion of unpublished treatment arms (gray boxes) was 36% (36/101, CI95% 26% to 45%) for the older cohort versus 19% (9/48, CI95% 8% to 30%) for the newer cohort.
Fig 1. Reporting of P values in publications vs. FDA reviews for older and newer cohorts of antidepressant drugs.
P values reported by the FDA (PFDA, horizontal axes) are compared to those in corresponding journal articles (PJournal, vertical axes). The older and newer antidepressants are shown in the left and right plots, respectively. Each data point represents a drug treatment arm compared to placebo, with area proportional to the sum of their sample sizes. Dashed diagonal represents concordance between PFDA and PJournal, i.e., an absence of reporting bias. Cases of outcome reporting bias, where PFDA is NS but PJournal is reported as significant, are highlighted in yellow. (The 2 yellow circles far off the Y = X diagonal in the right-hand panel represent desvenlafaxine trials 309 and 317 (please see text).) Unpublished treatments arms, with PFDA values but no corresponding PJournal values, are shown in the gray boxes and highlighted in yellow. FDA, Food and Drug Administration; NS, not significant.
Transparent publication
For the 4 newer antidepressants, Table 2 and S1 Fig show each trial’s overall outcome, as determined by the FDA, and its corresponding publication status. Of these 30 trials, the FDA deemed 15 (50%) to be positive, i.e., statistically significant on the prespecified primary outcome, consistent with the proportion previously reported for the older cohort [2]. Among these 15 FDA-positive trials, all were published in agreement with the FDA (transparently reported as positive). Among the 15 not-positive trials, 7 (47%) were transparently published (as nonsignificant), a higher proportion than that observed for the older cohort (4/37 = 11%) [2]. The remaining 8 (53%) FDA-negative trials in the newer cohort were not transparently published.
Six of these were simply not published. One desvenlafaxine trial was referred to in one review publication as “an unpublished report with the code name Des 223” [18]; in a second review publication authored by employees of the sponsor, it was referred as “data on file” [20]. Regarding vilazodone, one review publication referred to 5 trials (#244 to 248) as “astonishingly unfavorable” and cited the FDA drug approval package and no publications; a second review publication listed them in a paragraph and a data table devoted to unpublished trials.
Two other FDA-negative trials—desvenlafaxine EU trial 309 and US trial 317—were published but classified as not transparently published for 2 reasons. First, they were published solely in the form of a single positive “pooled analysis” paper [27]. (This form of reporting bias has been previously described in the antidepressant literature [28].) To be classified as transparently reported, the 2 trials should have been published in separate stand-alone papers highlighting their nonsignificant results, or published in a combined article highlighting the 2 nonsignificant results. Second, in the journal article, a nonprimary method of handling dropouts (MMRM instead of LOCF; Table D in S1 Text) was used, leading to statistically significant pooled results. (Although pooling trials increases statistical power, this alone would not have yielded a statistically significant result. Via post hoc MA of the FDA-reported primary results for these 2 trials, we calculated Hedges’ g = 0.10 (CI95% −0.08 to 0.28, P = 0.27).) These significant results were highlighted in the abstract and beginning of the results section. Meanwhile, the nonsignificant results from the individual trials were reported beginning on the fifth page of the results section and not in the abstract.
The effects of trial outcome and cohort on transparent reporting were examined using logistic regression. Please refer to Fig 2 for all counts and proportions, as well as odds ratios. (Further logistic regression results are available in Table A in S1 Text.) With respect to the variable for trial outcome, transparent reporting occurred more often for FDA-positive than for FDA-negative trials (OR 181, CI95% 26.9 to 1,219, P < 0.001). Post hoc univariable analyses showed significant effects of trial outcome within the older cohort (OR 181 CI95% 26.9 to 1,219, P < 0.001), consistent with findings reported earlier [2], and within the newer cohort (OR 35.1, CI95% 1.8 to 693, P = 0.019). Within the newer cohort, 15 of 15 (100%) positive trials were reported transparently versus 7 of 15 (47%) negative trials.
Fig 2. Interaction plot illustrating the effects of trial outcome and cohort (older vs. newer antidepressants) on transparent publication.
For all trials regardless of outcome (dashed oblique line), the proportion of transparently reported trials increased from 54% (older drugs) to 73% (newer drugs). Within the subset of FDA-positive trials (blue line), transparent reporting, which was already nearly 100% for the older cohort, showed no further increase. By contrast, within FDA-negative trials (green line), transparent reporting increased from 11% to 47%. FDA, Food and Drug Administration.
With respect to the variable for cohort, the overall proportion of transparently reported trials increased from 54% to 73%. Controlling for trial outcome, trials in the newer cohort were 6.6 times more likely to be transparently reported than trials in the older cohort (OR 6.6, CI95% 1.6 to 26.4, P = 0.008).
Post hoc analyses suggested that the higher rate of transparent publication in the newer cohort was limited to negative trials, which increased from 11% to 47%. Negative trials in the newer cohort were 6.6 times more likely to be transparently reported than negative trials in the older cohort (OR 6.6, CI95% 1.6, 26.4, P = 0.008), equal to the abovementioned main effect of cohort. By contrast, positive trials were transparently reported approximately 100% of the time for both cohorts; thus, the post hoc univariable analysis showed no effect (OR 1.3, CI95% 0.05 to 33, P = 0.88).
As shown in Table A in S1 Text, the multivariable model’s interaction effect was nonsignificant (OR 0.19, CI95% 0.006 to 6.7, P = 0.36); omitting the interaction term had little impact on the multivariable models’ 2 main effects. For all of the abovementioned analyses, similar results were obtained using exact logistic regression (S2 Fig and Table A in S1 Text).
Meta-analysis
Dose groups and trials included and excluded in the primary and sensitivity MAs are listed in Table C in S1 Text. Meta-analytic trial-level results from Stata, including forest plots, based on data from the FDA and the published literature, and for both primary and sensitivity MAs, are shown in S3–S6 Figs and Tables E-H in S1 Text.
S7 Fig is a forest plot comparing trial-level ES based on FDA versus journal data for each of the four newer antidepressants (using broad dose inclusion criteria). In S7 Fig, not-transparently published trials are highlighted for desvenlafaxine and vilazodone, which give rise to the observed (FDA- versus journal-based) ES differences at the level of drug (quantified below). For the other 2 drugs, levomilnacipran and vortioxetine, all trials were deemed transparently published (none highlighted otherwise); thus, their FDA- and journal-based ES values, at the level of both trial and drug, are virtually the same.
The abovementioned drug-level ES values are summarized and compared in Fig 3. In the primary MA (left panel), as mentioned above, ESI was largest for vilazodone (0.28 − 0.16 = 0.12), followed by desvenlafaxine (0.31 − 0.24 = 0.07). The overall FDA-based Hedges’ g for the 4 newer antidepressants was 0.24 (CI95% 0.18, 0.30), while the overall journal-based ES was 0.29 (CI95% 0.23, 0.36), for an ESI of +0.05.
Fig 3. Meta-analytic ES of 4 newer antidepressants derived from trial reports in FDA reviews vs. journal articles.
The primary (left panel) and sensitivity (right panel) MAs were based on broad and narrow/restrictive dose inclusion criteria, respectively, as described in text. For each antidepressant, 2 drug-level ES values are shown, one based on clinical trial data from FDA reviews and one based on data from the journal articles. ES, effect size; g, Hedges’s g; FDA, Food and Drug Administration; MA, meta-analysis.
In the sensitivity MAs (right panel of Fig 3),which employed restrictive/narrow dose inclusion criteria (see Methods), ES values were generally higher, especially for the FDA-based values, bringing them into closer alignment with the journal-based values. Thus, the abovementioned ESIs for vilazodone and desvenlafaxine decreased to nearly zero. The overall FDA-based Hedges’ g in these analyses was 0.33 (CI95%: 0.25, 0.41), while the overall journal-based value was 0.33 (CI95%: 0.25, 0.41), resulting in an ESI of approximately zero (+0.0).
Fig 4 compares the overall FDA- versus journal-based ES values for the newer versus the older cohort of antidepressants. As previously reported, the overall ESI for the older cohort was 0.10 (= 0.41 − 0.31), larger than the ESI found in the primary and sensitivity MA for the newer cohort. For additional context, ESI for individual drugs in the older cohort ranged from 0.03 (paroxetine controlled release) to 0.22 (mirtazapine), with a median of 0.10 [2].
Fig 4. Comparison of overall ES, derived from FDA reviews vs. journal articles, for older and newer antidepressants.
For the newer antidepressants, ESI was smaller than that previously reported for the older antidepressants. ES, effect size; ESI, effect size inflation; FDA, Food and Drug Administration; MA, meta-analysis.
Discussion
The data presented here suggest that reporting bias in the published literature on antidepressant drugs is still an important issue. Even within the cohort of newer antidepressants, statistical significance still has an undue influence on whether and how these trials are reported. Consistent with earlier work, we found that positive trials are much more likely to be transparently reported than negative trials, whether one looks within the newer cohort or at both cohorts combined. However, we also found evidence for improvement in reporting bias: Antidepressants trials, especially those deemed negative by the FDA, are more likely to be published transparently than they were previously. Regarding the meta-analytic results, though not the subject of formal statistical analysis, smaller ESI values for the newer, compared to the older, cohort also could be consistent with a decrease in reporting bias.
Comparison with previous findings
Our findings are consistent with at least 5 other recent studies: (1) A study [29] of Phase III randomized controlled trials (RCTs) in pediatric patients compared conference abstracts from 2008 to 2011 to subsequent publications and found evidence for “reduced but ongoing publication bias” as compared to a similar study from 15 years earlier [30]. (2) Another research group found evidence for improvements in some, though not all, measures of transparency (registration rates, results reporting, publication rates) for drugs approved in 2014, compared to drugs approved in 2012 [31]. (3) In an examination of trials of both pharmacological and nonpharmacological treatments for depression, the prevalence of proper registration and reporting was improved but still very low, despite the fact that registration and reporting had been mandatory for several years [32]. (4) Examining drugs approved for cardiovascular disease and diabetes mellitus [14], another group found a decrease in publication bias (as well as an increase in registration) among trials for drugs approved by the FDA after, compared to before, the FDAAA of 2007. (5) The same group applied similar methodology to drugs approved for several indications treated by neurologists and psychiatrists, as well as other indications (anesthesia, constipation, fibromyalgia, pain) [33]. The latter 2 studies were restricted to “pivotal” trials, a designation often assigned post hoc to trials with positive outcomes; by contrast, the current study covers all efficacy trials regardless of outcome, including so-called “failed trials” [34,35]. The current study differs from the 5 abovementioned studies in that it focuses on one drug class for one indication (major depressive disorder), thus enabling MA.
Possible explanations
How might we explain this apparent increase in transparency? There have long been many incentives to engage in reporting bias [36]. In the past, there was little awareness within the research and clinical communities that the problem existed, and pharmaceutical companies (and others) could engage in reporting bias without fear of detection. Since then, however, there has been a cultural change, and what was once standard practice is no longer considered acceptable. Numerous policy changes have been implemented, summarized elsewhere [37]. ClinicalTrials.gov was launched in 2000, but registrations initially lagged. In 2004—the year the FDA approved duloxetine, the newest drug within the older cohort of antidepressants [2]—the International Committee of Journal Editors (ICMJE) announced that prospective registration would be a precondition for publication. The following year saw a 73% increase in the registration rate over a span of just 5 months [38]. In 2005, the WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/Default.aspx) was launched. In 2007, the FDAAA was enacted [13], which legally mandated public registration of applicable clinical trials and called for the augmentation of ClinicalTrials.gov with a basic results database; in 2010, FDAAA was clarified and expanded in scope to include all Phase II to IV drug and device trials, adverse events, and basic results [39].
It seems reasonable to conclude that these policy changes played a major role in bringing about the increase in transparency suggested by the current study and the others mentioned above. However, given the level of attention directed toward reporting bias with antidepressants, in the form of lawsuits [39], numerous key publications [2,40–43], and new incentives to increase transparency, for instance, the Good Pharma Scorecard [31], it is possible that substantial improvement would have occurred without these policy changes.
Implications, theoretical and practical
However, we must caution that, while the proverbial glass of transparency is now half full, it also remains half empty. Nothing less than full transparency should be considered acceptable in the realm of healthcare. Greater awareness of reporting bias is needed among researchers and clinicians so that they do not naively accept published research findings at face value.
The abovementioned policy changes should not be celebrated until compliance with them improves. In the case of FDAAA, apparently due to a lack of political will, enforcement has been lax, leading to over $5 billion in accrued fines remaining uncollected (http://fdaaa.trialstracker.net). Additionally, many journals that ostensibly support the ICMJE policy of preregistration continue to publish a substantial number of unregistered or belatedly registered trials [32].
Perhaps what is needed most is to eliminate reporting bias at its root. FDA reviews include the results of negative, as well as positive, studies, because the Agency receives study protocols before studies are undertaken, thus preventing drug companies from hiding the existence of studies or switching their outcomes. Although trial registries are intended to serve a similar purpose, they are separate from journals, in which the strength and direction of study results can continue to dictate submission and acceptance decisions. However, in an emerging peer review model known as Registered Reports [44], manuscripts are submitted and reviewed before studies are undertaken, leading to preliminary publication decisions based solely on the scientific question and methodological rigor. Registered Reports has been adopted, or offered as an option, by >300 journals in various fields (https://cos.io/rr/?_ga=2.192240618.1714708995.1570198509-367521697.1570198509, accessed November 20, 2021), but uptake among major medical journals has unfortunately lagged.
Limitations and suggestions for future research
Despite the above-referenced consistency with previous findings, this study has several limitations that may affect generalizability. The scope of this study is limited to drug efficacy, so future research could examine whether transparency has also improved with regard to safety issues. For instance, we previously found that reporting of serious adverse events in the older antidepressant trials is often incomplete and inconsistent with FDA information [45]. Another scope-related limitation is that, because this study is restricted to antidepressants, these findings may not extend to other drug classes, which likely vary in signal-to-noise ratio (efficacy), proportion of “negative” trials, “need” for reporting bias, and hence potential for increased transparency. Further, this report pertains to Phase II/III premarketing trials only; the extent of reporting biases for Phase IV postmarketing trials is yet to be examined.
The most recently approved drugs in our sample were approved by the FDA in 2013, making it difficult to draw inferences about more recent changes in transparency practices. On the other hand, this study is a follow-up to our earlier review, making the contrast before versus after 2008 the topic of research. In addition to 2008 being the year of approval for the newest antidepressant in the older cohort, it was the year FDAAA was enacted, a milestone event for addressing reporting bias [13]. In any case, it was not possible to include drugs approved after 2013. The sample of older drugs was limited to those FDA-approved as monotherapy for major depressive disorder, and newer such drugs do not exist. More recent FDA approvals exist only for drugs FDA-approved as adjunctive therapy and/or for other depression-related indications such as treatment-resistant depression and postpartum depression, and our findings may not extend to reporting practices on such drugs.
For the newer, compared to the older, cohort, although the sample size was larger in terms of overall number of patients, it was smaller in terms of the number of drugs (4 versus 12, respectively) and trials (30 versus 74). However, as noted above, the drugs and trials in our sample were dictated by the drug development/approval process. Additionally, selective reporting practices may be correlated among trials for the same treatment from the same sponsor. (This limitation also applies to our earlier study [2]; among the 12 older antidepressants, one company sponsored 3 drugs and 3 companies sponsored 2 each.)
There are also limitations with respect to the statistical approach. First, the dichotomization of drugs into older and newer cohorts is somewhat arbitrary in that it is based on the timing of the earlier publication on the older cohort [2]. Second, because pharmaceutical companies often have publication strategies [46], within any given company, decisions whether to transparently publish its trials likely do not occur independently of one another. Third, the logistic regression model’s interaction term was nonsignificant; however, due to a limited sample size, and because transparent reporting of positive trials in the older cohort was already approximately 100%, leaving no room for improvement, the model was underpowered to detect such an effect. Fourth, the nonindependence of journal-based and FDA-based ES precluded formally contrasting them via meta-regression, so we were unable to determine whether the observed ESI is statistically significant. Fifth and relatedly, in contrasting the proportion of unpublished treatment arms between the older and newer cohorts, because many studies compared 2 or more dose arms to a single placebo group, the assumption of independence was not fully met.
In the current study, we found no change in the (high) level of transparent publication within FDA-positive trials. This is unsurprising—regardless of cohort, it is hard to conceive of a positive trial going unreported or being reported as negative. Hence, it could be argued that positive trials are uninformative and may hamper reporting bias signal detection. Therefore, in future analyses of reporting bias datasets, researchers may wish to consider focusing primarily on (more informative) negative trials.
In the sensitivity MA, compared to the primary MA, the gap between ESJournals and ESFDA was diminished. The sensitivity MA employed narrow dose inclusion criteria, i.e., was limited to those doses unambiguously approved by the FDA. The FDA determines effective dose ranges based on how “successful” the various doses are in Phase II/III trials. In the narrowly defined dose range, the sample was limited to clearly successful (FDA-positive) data, which are associated with larger ES values and higher levels of transparent publication (less reporting bias).
Conclusions
In this study, we found a persistence of reporting bias within a cohort of newer antidepressants approved since 2008. However, compared to the cohort of older antidepressants, reporting bias in the newer cohort appeared to decrease, and neither study publication nor outcome reporting bias was found among trials for the 2 newest antidepressants (both approved in 2013). The observed improvement in transparency may be due to cultural and policy changes over the past decade. Further efforts and vigilance are needed to maintain and build upon these improvements.
Supporting information
Among 15 FDA-positive trials, all were published in agreement with the FDA (transparently reported as positive). Among 15 not-positive trials, 7 (47%) were transparently published (as nonsignificant), a higher proportion than that observed for the older antidepressants. FDA, Food and Drug Administration.
(EPS)
Above each line, the command for the primary method, penalized (Firth) logistic regression, is shown. Below each line, the command for the secondary method, exact logistic regression, is shown.
(EPS)
ES, effect size; FDA, Food and Drug Administration.
(EPS)
ES, effect size.
(EPS)
ES, effect size; FDA, Food and Drug Administration.
(EPS)
ES, effect size.
(EPS)
Red boxes indicate trials that were not transparently published. ES, effect size; FDA, Food and Drug Administration.
(EPS)
Blue asterisks and black plus signs represent trials of older and newer antidepressants, respectively. Blue and black ellipses indicate the 95% confidence regions for their respective summary effects. FDA, Food and Drug Administration; MA, meta-analysis; SMD, standardized mean difference.
(EPS)
Table A. Results from penalized (Firth) logistic regression models. Effect of trial outcome and cohort on transparent reporting of trial outcome. Table B. Results from exact logistic regression models. Effect of trial outcome and cohort on transparent reporting of trial outcome. Table C. Rationale for inclusion of dosage groups in primary vs. sensitivity MA. Table D. Primary outcomes according to FDA review and journal articles. Table E. Numerical results (FDA-based MA; broad dose inclusion criteria). Table F. Numerical results (journal-based MA; broad dose inclusion criteria). Table G. Numerical results (FDA-based MA; narrow dose inclusion criteria). Table H. Numerical results (journal-based MA; narrow dose inclusion criteria). Table I. Results of the multivariate MAs. FDA, Food and Drug Administration; MA, meta-analysis
(DOCX)
(DOCX)
(DOCX)
(DTA)
(XLSX)
FDA, Food and Drug Administration; MA, meta-analysis.
(DTA)
MA, meta-analysis.
(DTA)
FDA, Food and Drug Administration; MA, meta-analysis.
(DTA)
MA, meta-analysis.
(DTA)
FDA, Food and Drug Administration; MA, meta-analysis.
(XLSX)
Acknowledgments
Kathryn Burrows assisted with Table 2. The following individuals assisted with double data extraction and entry: Sepideh Alavi, Ilya Ivlev, Ryan McKenna. Yusuki Ogawa assisted with the search for FDA-registered trials and corresponding publications and with data extraction and entry.
Abbreviations
- ES
effect size
- ESI
effect size inflation
- FDA
Food and Drug Administration
- FDAAA
Food and Drug Administration Amendments Act
- ICMJE
International Committee of Journal Editors
- MA
meta-analysis
- RCT
randomized controlled trial
Data Availability
All relevant data are within the manuscript, its Supporting Information files, in the database Drugs@FDA (https://www.accessdata.fda.gov/scripts/cder/daf/), in cited publications, in a previously published manuscript (https://www.nejm.org/doi/full/10.1056/nejmsa065779), and its supplemental appendix (https://www.nejm.org/doi/suppl/10.1056/NEJMsa065779/suppl_file/nejm_turner_252sa1.pdf).
Funding Statement
The authors received no specific funding for this work.
References
- 1.Dwan K, Altman DG, Arnaiz JA, Bloom J, Chan A-W, Cronin E, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS ONE. 2008;3:e3081. doi: 10.1371/journal.pone.0003081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective Publication of Antidepressant Trials and Its Influence on Apparent Efficacy. N Engl J Med. 2008;358:252–60. doi: 10.1056/NEJMsa065779 [DOI] [PubMed] [Google Scholar]
- 3.Turner EH, Knoepflmacher D, Shapley L. Publication Bias in Antipsychotic Trials: An Analysis of Efficacy Comparing the Published Literature to the US Food and Drug Administration Database. PLoS Med. 2012;9:e1001189. doi: 10.1371/journal.pmed.1001189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roest AM, Jonge d, Williams CD, Vries d YA, Schoevers RA, Turner EH. Reporting Bias in Clinical Trials Investigating the Efficacy of Second-Generation Antidepressants in the Treatment of Anxiety Disorders: A Report of 2 Meta-analyses. JAMA Psychiat. 2015;72:500–10. doi: 10.1001/jamapsychiatry.2015.15 [DOI] [PubMed] [Google Scholar]
- 5.Hart B, Lundh A, Bero L. Effect of reporting bias on meta-analyses of drug trials: reanalysis of meta-analyses. BMJ. 2012;344:d7202–2. doi: 10.1136/bmj.d7202 [DOI] [PubMed] [Google Scholar]
- 6.Omae K, Kataoka Y, Tsujimoto Y, Tsutsumi Y, Yamamoto Y, Fukuhara S, et al. Publication statuses of clinical trials supporting FDA-approved immune checkpoint inhibitors: a meta-epidemiological investigation. BMC Cancer. 2019;19:998. doi: 10.1186/s12885-019-6232-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rising K, Bacchetti P, Bero L. Reporting Bias in Drug Trials Submitted to the Food and Drug Administration: Review of Publication and Presentation. Ioannidis J, editor. PLoS Med. 2008;5:e217-discussion e217. doi: 10.1371/journal.pmed.0050217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGauran N, Wieseler B, Kreis J, Schüler Y-B, Kölsch H, Kaiser T. Reporting bias in medical research—a narrative review. Trials. 2010;11:37. doi: 10.1186/1745-6215-11-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ioannidis JPA, Karassa FB. The need to consider the wider agenda in systematic reviews and meta-analyses: breadth, timing, and depth of the evidence. BMJ. 2010;341:c4875. doi: 10.1136/bmj.c4875 [DOI] [PubMed] [Google Scholar]
- 10.Fanelli D. Negative results are disappearing from most disciplines and countries. Scientometrics. 2012;90:891–904. [Google Scholar]
- 11.DeAngelis CD, Drazen JM, Frizelle FA, Haug C, Hoey J, Horton R, et al. Clinical trial registration: a statement from the International Committee of Medical Journal Editors. JAMA. 2004;292:1363–4. doi: 10.1001/jama.292.11.1363 [DOI] [PubMed] [Google Scholar]
- 12.Zarin DA, Tse T, Williams RJ, Califf RM, Ide NC. The ClinicalTrials.gov results database—update and key issues. N Engl J Med. 2011;364:852–60. doi: 10.1056/NEJMsa1012065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zarin DA, Tse T. Moving toward transparency of clinical trials. Science. 2008;319:1340–2. doi: 10.1126/science.1153632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phillips AT, Desai NR, Krumholz HM, Zou CX, Miller JE, Ross JS. Association of the FDA Amendment Act with trial registration, publication, and outcome reporting. Trials. 2017;18:1518. doi: 10.1186/s13063-017-2068-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller JE, Korn D, Ross JS. Clinical trial registration, reporting, publication and FDAAA compliance: a cross-sectional analysis and ranking of new drugs approved by the FDA in 2012. BMJ Open. 2015;5:e009758. doi: 10.1136/bmjopen-2015-009758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turner EH. How to access and process FDA drug approval packages for use in research. BMJ. 2013;347:f5992–2. doi: 10.1136/bmj.f5992 [DOI] [PubMed] [Google Scholar]
- 17.Vries YA de, Roest AM, Jonge P de, Cuijpers P, Munafò MR, Bastiaansen JA. The cumulative effect of reporting and citation biases on the apparent efficacy of treatments: the case of depression. Psychol Med 2018;48:2453–2455. doi: 10.1017/S0033291718001873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laoutidis ZG, Kioulos KT. Desvenlafaxine for the acute treatment of depression: a systematic review and meta-analysis. Pharmacopsychiatry. 2015;48:187–99. doi: 10.1055/s-0035-1555879 [DOI] [PubMed] [Google Scholar]
- 19.Kornstein SG, McIntyre RS, Thase ME, Boucher M. Desvenlafaxine for the treatment of major depressive disorder. Expert Opin Pharmacother. 2014;15:1449–63. doi: 10.1517/14656566.2014.923403 [DOI] [PubMed] [Google Scholar]
- 20.Tourian KA, Jiang Q, Ninan PT. Analysis of the Effect of Desvenlafaxine on Anxiety Symptoms Associated with Major Depressive Disorder: Pooled Data from 9 Short-Term, Double-blind, Placebo-Controlled Trials. CNS Spectr. 2010;15:187–93. doi: 10.1017/s1092852900027450 [DOI] [PubMed] [Google Scholar]
- 21.Wang S-M, Han C, Lee S-J, Patkar AA, Masand PS, Pae C-U. Vilazodone for the Treatment of Depression: An Update. Chonnam Med J. 2016;52:91–100. doi: 10.4068/cmj.2016.52.2.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCormack PL. Vilazodone: a review in major depressive disorder in adults. Drugs. 2015;75:1915–23. doi: 10.1007/s40265-015-0490-y [DOI] [PubMed] [Google Scholar]
- 23.Citrome L. Vilazodone for major depressive disorder: a systematic review of the efficacy and safety profile for this newly approved antidepressant—what is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2012;66:356–68. doi: 10.1111/j.1742-1241.2011.02885.x [DOI] [PubMed] [Google Scholar]
- 24.Katz R. FDA: evidentiary standards for drug development and approval. NeuroRx. 2004;1:307–16. doi: 10.1602/neurorx.1.3.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 26.Mehta CR, Patel NR. Exact logistic regression: theory and examples. Stat Med. 1995;14:2143–60. doi: 10.1002/sim.4780141908 [DOI] [PubMed] [Google Scholar]
- 27.Lieberman DZ, Montgomery SA, Tourian KA, Brisard C, Rosas G, Padmanabhan K, et al. A pooled analysis of two placebo-controlled trials of desvenlafaxine in major depressive disorder. Int Clin Psychopharmacol. 2008;23:188–97. doi: 10.1097/YIC.0b013e32830263de [DOI] [PubMed] [Google Scholar]
- 28.Vries d YA, Roest AM, Turner EH, Jonge d PA. Hiding negative trials by pooling them: a secondary analysis of pooled-trials publication bias in FDA-registered antidepressant trials. Psychol Med. 2018;351:1–7. doi: 10.1017/s0033291718002805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crockett LK, Okoli GN, Neilson CJ, Rabbani R, Abou-Setta AM, Klassen TP. Publication of Randomized Clinical Trials in Pediatric Research: A Follow-up Study. JAMA Netw Open. 2018;1:e180156. doi: 10.1001/jamanetworkopen.2018.0156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klassen TP, Wiebe N, Russell K, Stevens K, Hartling L, Craig WR, et al. Abstracts of randomized controlled trials presented at the society for pediatric research meeting: an example of publication bias. Arch Pediatr Adolesc Med. 2002;156:474–9. doi: 10.1001/archpedi.156.5.474 [DOI] [PubMed] [Google Scholar]
- 31.Miller JE, Wilenzick M, Ritcey N, Ross JS, Mello MM. Measuring clinical trial transparency: an empirical analysis of newly approved drugs and large pharmaceutical companies. BMJ Open. 2017;7:e017917. doi: 10.1136/bmjopen-2017-017917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shinohara K, Tajika A, Imai H, Takeshima N, Hayasaka Y, Furukawa TA. Protocol registration and selective outcome reporting in recent psychiatry trials: new antidepressants and cognitive behavioural therapies. Acta Psychiatr Scand. 2015;132:489–98. doi: 10.1111/acps.12502 [DOI] [PubMed] [Google Scholar]
- 33.Zou CX, Becker JE, Phillips AT, Garritano JM, Krumholz HM, Miller JE, et al. Registration, results reporting, and publication bias of clinical trials supporting FDA approval of neuropsychiatric drugs before and after FDAAA: a retrospective cohort study. Trials. 2018;19:581. doi: 10.1186/s13063-018-2957-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ninan PT, Poole RM, Stiles GL. Selective publication of antidepressant trials. N Engl J Med. 2008;358:2181. PubMed PMID: author reply 2181–2. [PubMed] [Google Scholar]
- 35.Otto MW, Nierenberg AA. Assay sensitivity, failed clinical trials, and the conduct of science. Psychother Psychosom. 2002;71:241–3. doi: 10.1159/000064813 [DOI] [PubMed] [Google Scholar]
- 36.Turner EH. Publication bias, with a focus on psychiatry: causes and solutions. CNS Drugs. 2013;27:457–68. doi: 10.1007/s40263-013-0067-9 [DOI] [PubMed] [Google Scholar]
- 37.Dickersin K, Rennie D. The evolution of trial registries and their use to assess the clinical trial enterprise. JAMA. 2012;307:1861–4. doi: 10.1001/jama.2012.4230 [DOI] [PubMed] [Google Scholar]
- 38.Zarin DA, Tse T, Ide NC. Trial Registration at ClinicalTrials.gov between May and October 2005. N Engl J Med. 2005;353:2779–87. doi: 10.1056/NEJMsa053234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gibson L. GlaxoSmithKline to publish clinical trials after US lawsuit. BMJ. 2004;328:1513–3. doi: 10.1136/bmj.328.7455.1513-a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Melander H. Evidence b(i)ased medicine—selective reporting from studies sponsored by pharmaceutical industry: review of studies in new drug applications. BMJ. 2003;326:1171–3. doi: 10.1136/bmj.326.7400.1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whittington CJ, Kendall T, Fonagy P, Cottrell D, Cotgrove A, Boddington E. Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. Lancet. 2004;363:1341–5. doi: 10.1016/S0140-6736(04)16043-1 [DOI] [PubMed] [Google Scholar]
- 42.Jureidini J, McHenry L, Mansfield P. Clinical trials and drug promotion: Selective reporting of study 329. Int J Risk Saf Med. 2008;20:73–81. [Google Scholar]
- 43.Eyding D, Lelgemann M, Grouven U, Härter M, Kromp M, Kaiser T, et al. Reboxetine for acute treatment of major depression: systematic review and meta-analysis of published and unpublished placebo and selective serotonin reuptake inhibitor controlled trials. BMJ 2010;341:c4737. doi: 10.1136/bmj.c4737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chambers CD, Feredoes E, Muthukumaraswamy SD, Etchells P. Instead of “playing the game” it is time to change the rules: Registered Reports at AIMS Neuroscience and beyond. AIMS Neurosci. 2014;1:4–17. doi: 10.3934/neuroscience2014.1.4 [DOI] [Google Scholar]
- 45.Vries d YA, Roest AM, Beijers L, Turner EH, Jonge d P. Bias in the reporting of harms in clinical trials of second-generation antidepressants for depression and anxiety: A meta-analysis. Eur Neuropsychopharmacol. 2016;26:1752–9. doi: 10.1016/j.euroneuro.2016.09.370 [DOI] [PubMed] [Google Scholar]
- 46.Vedula SS, Goldman PS, Rona IJ, Greene TM, Dickersin K. Implementation of a publication strategy in the context of reporting biases. A case study based on new documents from Neurontin litigation. Trials. 2012;13:136. doi: 10.1186/1745-6215-13-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liebowitz MR, Yeung PP, Entsuah R. A randomized, double-blind, placebo-controlled trial of desvenlafaxine succinate in adult outpatients with major depressive disorder. J Clin Psychiatry. 2007;68:1663–72. doi: 10.4088/jcp.v68n1105 [DOI] [PubMed] [Google Scholar]
- 48.DeMartinis NA, Yeung PP, Entsuah R, Manley AL. A double-blind, placebo-controlled study of the efficacy and safety of desvenlafaxine succinate in the treatment of major depressive disorder. J Clin Psychiatry. 2007;68:677–88. doi: 10.4088/jcp.v68n0504 [DOI] [PubMed] [Google Scholar]
- 49.Septien-Velez L, Pitrosky B, Padmanabhan SK, Germain J-M, Tourian KA. A randomized, double-blind, placebo-controlled trial of desvenlafaxine succinate in the treatment of major depressive disorder. Int Clin Psychopharmacol. 2007;22:338–47. doi: 10.1097/YIC.0b013e3281e2c84b [DOI] [PubMed] [Google Scholar]
- 50.Feiger AD, Tourian KA, Rosas GR, Padmanabhan SK. A placebo-controlled study evaluating the efficacy and safety of flexible-dose desvenlafaxine treatment in outpatients with major depressive disorder. CNS Spectr. 2009;14:41–50. doi: 10.1017/s1092852900020046 [DOI] [PubMed] [Google Scholar]
- 51.Liebowitz MR, Manley AL, Padmanabhan SK, Ganguly R, Tummala R, Tourian KA. Efficacy, safety, and tolerability of desvenlafaxine 50 mg/day and 100 mg/day in outpatients with major depressive disorder. Curr Med Res Opin. 2008;24:1877–90. doi: 10.1185/03007990802161923 [DOI] [PubMed] [Google Scholar]
- 52.Boyer P, Montgomery S, Lepola U, Germain J-M, Brisard C, Ganguly R, et al. Efficacy, safety, and tolerability of fixed-dose desvenlafaxine 50 and 100 mg/day for major depressive disorder in a placebo-controlled trial. Int Clin Psychopharmacol. 2008;23:243–53. doi: 10.1097/YIC.0b013e32830cebed [DOI] [PubMed] [Google Scholar]
- 53.Montgomery SA, Mansuy L, Ruth A, Bose A, Li H, Li D. Efficacy and safety of levomilnacipran sustained release in moderate to severe major depressive disorder: a randomized, double-blind, placebo-controlled, proof-of-concept study. J Clin Psychiatry. 2013;74:363–9. doi: 10.4088/JCP.12m08141 [DOI] [PubMed] [Google Scholar]
- 54.Asnis GM, Bose A, Gommoll CP, Chen C, Greenberg WM. Efficacy and safety of levomilnacipran sustained release 40 mg, 80 mg, or 120 mg in major depressive disorder: a phase 3, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2013;74:242–8. doi: 10.4088/JCP.12m08197 [DOI] [PubMed] [Google Scholar]
- 55.Gommoll CP, Greenberg WM, Chen C. A randomized, double-blind, placebo-controlled study of flexible doses of levomilnacipran ER (40–120 mg/day) in patients with major depressive disorder. J Drug Assess. 2014;3:10–9. doi: 10.3109/21556660.2014.884505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sambunaris A, Bose A, Gommoll CP, Chen C, Greenberg WM, Sheehan DV. A Phase III, Double-Blind, Placebo-Controlled, Flexible-Dose Study of Levomilnacipran Extended-Release in Patients With Major Depressive Disorder. J Clin Psychopharmacol. 2014;34:47–56. doi: 10.1097/JCP.0000000000000060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bakish D, Bose A, Gommoll C, Chen C, Nunez R, Greenberg WM, et al. Levomilnacipran ER 40 mg and 80 mg in patients with major depressive disorder: a phase III, randomized, double-blind, fixed-dose, placebo-controlled study. J Psychiatry Neurosci. 2014;39:40–9. doi: 10.1503/jpn.130040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khan A, Cutler AJ, Kajdasz DK, Gallipoli S, Athanasiou M, Robinson DS, et al. A randomized, double-blind, placebo-controlled, 8-week study of vilazodone, a serotonergic agent for the treatment of major depressive disorder. J Clin Psychiatry. 2011;72:441–7. doi: 10.4088/JCP.10m06596 [DOI] [PubMed] [Google Scholar]
- 59.Rickels K, Athanasiou M, Robinson DS, Gibertini M, Whalen H, Reed CR. Evidence for efficacy and tolerability of vilazodone in the treatment of major depressive disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2009;70:326–33. doi: 10.4088/jcp.08m04637 [DOI] [PubMed] [Google Scholar]
- 60.Jain R, Mahableshwarkar AR, Jacobsen PL, Chen Y, Thase ME. A randomized, double-blind, placebo-controlled 6-wk trial of the efficacy and tolerability of 5 mg vortioxetine in adults with major depressive disorder. Int J Neuropsychopharmacol. 2013;16:313–21. doi: 10.1017/S1461145712000727 [DOI] [PubMed] [Google Scholar]
- 61.Mahableshwarkar AR, Jacobsen PL, Chen Y. A randomized, double-blind trial of 2.5 mg and 5 mg vortioxetine (Lu AA21004) versus placebo for 8 weeks in adults with major depressive disorder. Curr Med Res Opin. 2013;29:217–26. doi: 10.1185/03007995.2012.761600 [DOI] [PubMed] [Google Scholar]
- 62.Henigsberg N, Mahableshwarkar AR, Jacobsen P, Chen Y, Thase ME. A randomized, double-blind, placebo-controlled 8-week trial of the efficacy and tolerability of multiple doses of Lu AA21004 in adults with major depressive disorder. J Clin Psychiatry. 2012;73:953–9. doi: 10.4088/JCP.11m07470 [DOI] [PubMed] [Google Scholar]
- 63.Mahableshwarkar AR, Jacobsen PL, Chen Y, Serenko M, Trivedi MH. A randomized, double-blind, duloxetine-referenced study comparing efficacy and tolerability of 2 fixed doses of vortioxetine in the acute treatment of adults with MDD. Psychopharmacology. 2015;232:2061–70. doi: 10.1007/s00213-014-3839-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jacobsen PL, Mahableshwarkar AR, Serenko M, Chan S, Trivedi MH. A randomized, double-blind, placebo-controlled study of the efficacy and safety of vortioxetine 10 mg and 20 mg in adults with major depressive disorder. J Clin Psychiatry. 2015;76:575–82. doi: 10.4088/JCP.14m09335 [DOI] [PubMed] [Google Scholar]
- 65.Mahableshwarkar AR, Jacobsen PL, Serenko M, Chen Y, Trivedi MH. A randomized, double-blind, placebo-controlled study of the efficacy and safety of 2 doses of vortioxetine in adults with major depressive disorder. J Clin Psychiatry. 2015;76:583–91. doi: 10.4088/JCP.14m09337 [DOI] [PubMed] [Google Scholar]
- 66.Alvarez E, Perez V, Dragheim M, Loft H, Artigas F. A double-blind, randomized, placebo-controlled, active reference study of Lu AA21004 in patients with major depressive disorder. Int J Neuropsychopharmacol. 2012;15:589–600. doi: 10.1017/S1461145711001027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baldwin DS, Loft H, Dragheim M. A randomised, double-blind, placebo controlled, duloxetine-referenced, fixed-dose study of three dosages of Lu AA21004 in acute treatment of major depressive disorder (MDD). Eur Neuropsychopharmacol. 2012;22:482–91. doi: 10.1016/j.euroneuro.2011.11.008 [DOI] [PubMed] [Google Scholar]
- 68.Boulenger J-P, Loft H, Olsen CK. Efficacy and safety of vortioxetine (Lu AA21004), 15 and 20 mg/day: a randomized, double-blind, placebo-controlled, duloxetine-referenced study in the acute treatment of adult patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29:138–49. doi: 10.1097/YIC.0000000000000018 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Among 15 FDA-positive trials, all were published in agreement with the FDA (transparently reported as positive). Among 15 not-positive trials, 7 (47%) were transparently published (as nonsignificant), a higher proportion than that observed for the older antidepressants. FDA, Food and Drug Administration.
(EPS)
Above each line, the command for the primary method, penalized (Firth) logistic regression, is shown. Below each line, the command for the secondary method, exact logistic regression, is shown.
(EPS)
ES, effect size; FDA, Food and Drug Administration.
(EPS)
ES, effect size.
(EPS)
ES, effect size; FDA, Food and Drug Administration.
(EPS)
ES, effect size.
(EPS)
Red boxes indicate trials that were not transparently published. ES, effect size; FDA, Food and Drug Administration.
(EPS)
Blue asterisks and black plus signs represent trials of older and newer antidepressants, respectively. Blue and black ellipses indicate the 95% confidence regions for their respective summary effects. FDA, Food and Drug Administration; MA, meta-analysis; SMD, standardized mean difference.
(EPS)
Table A. Results from penalized (Firth) logistic regression models. Effect of trial outcome and cohort on transparent reporting of trial outcome. Table B. Results from exact logistic regression models. Effect of trial outcome and cohort on transparent reporting of trial outcome. Table C. Rationale for inclusion of dosage groups in primary vs. sensitivity MA. Table D. Primary outcomes according to FDA review and journal articles. Table E. Numerical results (FDA-based MA; broad dose inclusion criteria). Table F. Numerical results (journal-based MA; broad dose inclusion criteria). Table G. Numerical results (FDA-based MA; narrow dose inclusion criteria). Table H. Numerical results (journal-based MA; narrow dose inclusion criteria). Table I. Results of the multivariate MAs. FDA, Food and Drug Administration; MA, meta-analysis
(DOCX)
(DOCX)
(DOCX)
(DTA)
(XLSX)
FDA, Food and Drug Administration; MA, meta-analysis.
(DTA)
MA, meta-analysis.
(DTA)
FDA, Food and Drug Administration; MA, meta-analysis.
(DTA)
MA, meta-analysis.
(DTA)
FDA, Food and Drug Administration; MA, meta-analysis.
(XLSX)
Data Availability Statement
All relevant data are within the manuscript, its Supporting Information files, in the database Drugs@FDA (https://www.accessdata.fda.gov/scripts/cder/daf/), in cited publications, in a previously published manuscript (https://www.nejm.org/doi/full/10.1056/nejmsa065779), and its supplemental appendix (https://www.nejm.org/doi/suppl/10.1056/NEJMsa065779/suppl_file/nejm_turner_252sa1.pdf).