Abstract
Vertebrobasilar artery dissection is an uncommon cause of acute ischaemic stroke (AIS). Optimal endovascular management has not been established. This study aimed to share our experience with endovascular reperfusion therapy for vertebrobasilar artery occlusion due to vertebral artery dissection (VAD). We retrospectively reviewed 134 consecutive patients with AIS who received urgent endovascular reperfusion therapy between November 2017 and November 2019. Three patients diagnosed with VAD were investigated. The evaluation included mechanisms of vertebrobasilar artery occlusion due to VAD, variations in endovascular procedures, and functional outcomes. Dissections at the V3, V4 and extension of V3 to V4 segments were seen in one patient each. The mechanism of AIS was different in each patient: occlusion of the distal non-dissected artery due to an embolus from the dissection site (distal occlusion), haemodynamic collapse of the entire vertebrobasilar artery system due to the arterial dissection itself (local occlusion), or coexistence of distal occlusion and local occlusion (tandem occlusion). The endovascular reperfusion therapy was performed corresponding to the abovementioned mechanisms: mechanical thrombectomy for distal occlusion, stenting for local occlusion, and a combination of thrombectomy and stenting for tandem occlusion. In all three patients, effective recanalization and functional independence (modified Rankin Scale scores of 0–2 at 90 days after the onset) were achieved. Endovascular treatment corresponding to the individual mechanism of AIS may improve patient outcomes.
Keywords: vertebral artery dissection, acute ischaemic stroke, large vessel occlusion, endovascular treatment, thrombectomy
Introduction
Cervical-cranial artery dissection is identified in 1–5% of patients with acute ischaemic stroke (AIS) undergoing mechanical thrombectomy.1–4) The majority of previous reports concerned cervical carotid artery dissection and described the efficacy of mechanical thrombectomy with or without stenting.2,4–11) In contrast, it remains unclear if endovascular reperfusion therapy can be effective for AIS resulting from vertebrobasilar artery dissection (VBAD).
We report the cases of three patients with vertebrobasilar artery occlusion due to vertebral artery dissection (VAD) who underwent urgent endovascular reperfusion therapy.
Case series
To determine VBAD cases, an experienced neurointerventionalist retrospectively reviewed the imaging data of 134 consecutive patients with AIS who received urgent endovascular reperfusion therapy between November 2017 and November 2019. VBAD was diagnosed based on a modified version of a previously proposed diagnostic criteria.3,12–14) Our diagnostic criteria consist of six major requirements (Criteria I–VI). For a definitive diagnosis, at least one of the major requirements must be fulfilled. Criteria I (intimal flap) and II (double lumen) are independent definite findings of cervical–cranial artery dissection. Criteria III (string sign), IV (long irregular stenosis), V (tapered occlusion), and VI (pearl and string sign) are defined as non-specific findings and need to be combined with at least one of the three minor requirements: intramural haematoma defined as hyperintensity on T1-weighted magnetic resonance imaging (MRI), external calibre enlargement of the affected artery on basi-parallel anatomical scanning (BPAS)–MRI,15) or rapid change in arterial morphology.
Among the 134 patients, three patients were diagnosed with vertebrobasilar artery occlusion due to VAD. No patient with basilar artery dissection was found.
Ethical considerations
This study was conducted in accordance with the Declaration of Helsinki. The procedures followed in experiments on human subjects were conducted in accordance with “Ethical Guidelines for Medical and Health Research Involving Human Subjects (Provisional Translation as of March 2015)” and its later amendments. The relevant institutional review boards approved this study. All patients included in this study or their legal representatives provided written informed consent to receive endovascular treatment. As the study design was retrospective and included a non-interventional review, rather than obtaining a written informed consent from each patient for participation in this study, the opportunity to opt out was provided via a website. No patient made an objection to using his or her clinical data in this study.
Case Presentation
Case 1
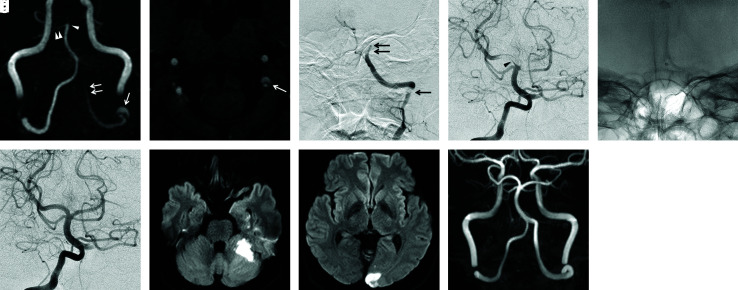
Case 1 was a 42-year-old man who experienced sudden onset headache, vertigo, truncal ataxia, and dysarthria. Initial diffusion-weighted imaging (DWI) showed no abnormality. Magnetic resonance angiography (MRA) revealed tandem occlusion of the left intracranial vertebral artery (VA) and basilar artery (BA) with intimal flap and double lumen at the left V3 segment (Fig. 1a and 1b). Digital subtraction angiography (DSA) immediately following MRI showed long irregular stenosis of the left V3 segment leading to the occluded V4 segment (Fig. 1c) and a thrombus in the top of the BA (Fig. 1d). The contralateral or right VA was intact and maintained antegrade blood flow to the BA (Fig. 1d). At this point, the mechanism of AIS was considered as a distal BA occlusion due to an embolus from the left VAD (V3–V4 segment). He underwent mechanical thrombectomy for an occluded distal BA by a direct aspiration first pass technique using Penumbra ACE68 (Penumbra, Inc., Alameda, CA, USA) via the non-dissected right VA (Fig. 1e). This resulted in recanalization with a modified thrombolysis in cerebral infarction (mTICI) score of 2b (Fig. 1f). DWI obtained a day after the treatment showed a small infarction in the territory of the left anteroinferior cerebellar artery (AICA) and left posterior cerebral artery (Fig. 1g and 1h). The endovascular parent artery occlusion for the dissected left V3–V4 segment was considered in order to prevent the repeated embolism, but it was not executed because the intentional V4 occlusion had the risk of perforator injury resulting in the severe medullary infarction. The dissected left VA was subsequently observed on repeat MRA. One month later, spontaneous recanalization and morphological normalization of the dissected left VA were confirmed by MRA. The left VA remained intact until the last MRA was obtained 6 months after the onset (Fig. 1i). His modified Rankin Scale (mRS) score at 3 months after the onset was 0, which was maintained until the last clinical follow-up carried out 6 months after the onset.
Fig. 1. Case 1. (a) Initial MRA. An abnormal hyperintense signal suggesting intramural thrombus is observed around the transposition part between the left V3 and V4 segments (arrow). The signal of the left VA is faint and interrupted at the V4 segment (double arrow). The top of the BA including the left SCA and the bilateral PCA is not depicted (arrowhead). Only the right SCA is preserved (double arrowheads). (b) Source image of initial MRA. The intimal flap and double lumen are demonstrated at the end of the V3 segment of the left VA (arrow). (c) Initial left vertebral angiogram. The left VA exhibits irregular long segment stenosis at the V3 segment (arrow), followed by irregular tapered occlusion (double arrow). (d) Initial right vertebral angiogram. A filling defect indicating a large clot (arrowhead) extends from the top of the BA to the left SCA and bilateral PCA. (e) Snapshot image of Penumbra ACE68. Penumbra ACE68 has already reached the occlusion site of the BA via the right VA. Afterward, thrombectomy by contact aspiration was performed. (f) Right vertebral angiogram after first pass of contact aspiration. Recanalization of the top of the BA is confirmed. (g and h) DWI obtained a day after the treatment. Small infarcts are observed in the territory of the left AICA and left PCA. (i) MRA obtained 6 months after the treatment. Left VA is spontaneously recanalized without any remaining findings of dissection. MRA: magnetic resonance angiography, VA: vertebral artery, BA: basilar artery, SCA: superior cerebellar artery, PCA: posterior cerebral artery, DWI: diffusion-weighted imaging, AICA: anteroinferior cerebellar artery.
Case 2
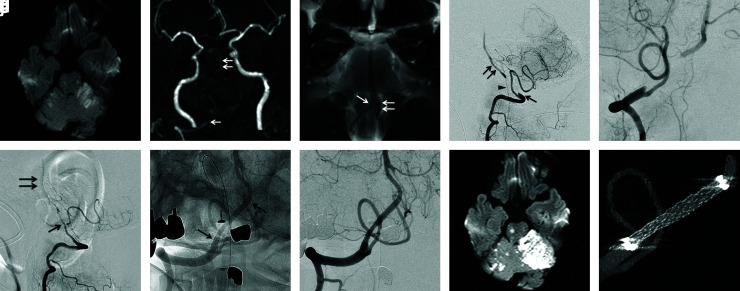
Case 2 was a 69-year-old man who experienced severe headache, right facial palsy, and dysarthria followed by mild tetraparesis. The spotty acute multiple infarcts in the territory of bilateral AICA and pons were confirmed on initial DWI (Fig. 2a). Bilateral intracranial VA occlusion with tubular enlargement of the external vessel calibre was shown on MRA and BPAS–MRI (Fig. 2b and 2c). The discrepancy between the inner shape on MRA and outer shape on BPAS–MRI strongly suggested the bilateral VAD. DSA revealed long segment tapered occlusion of the right V4 segment (Fig. 2d and 2e) and long segment irregular pseudo-occlusion of the left V4 segment (Fig. 2f). Inadequate reconstitution of the distal right V4 and BA was indicated by collateral flow via the anterior spinal artery (Fig. 2d). Based on the clinical course and the findings of imaging examination, the mechanism of cerebral ischaemia was considered as hypoperfusion resulting from the bilateral VA dissection. The occluded right VA was considered more suitable for recanalization by stenting rather than the left VA because the affected segment of the right VA was shorter than the left VA in length (Fig. 2d and 2f) and the assumed landing zone for the stent was clearer in the right VA (Fig. 2e). A loading dose of dual antiplatelet therapy (DAPT) with 300 mg of clopidogrel and 200 mg of aspirin was administered prior to the endovascular treatment. It was difficult challenge to secure the occluded true lumen. However, it happened so that the intact right V4 segment at the distal side of the occlusion was visible owing to collateral flow via the anterior spinal artery (Fig. 2e). This angioarchitecture made it possible to recognize the proximal and distal true lumen at both sides of the occlusion. CHIKAI black 14 soft tip microwire (Asahi Intecc, Aichi, Japan) was carefully advanced with slight rotation through the occluded dissection site to the visible distal left V4 segment. The operator sought the route in which the microwire straightly moved forward in the biplane road map images without friction transmitted to his or her fingers. When the slightest bending of the microwire was seen on the monitor or the subtle resistance was sensed by the operator’s fingers, the microwire was slightly pulled back and the lesion cross was retried by seeking the correct route. After crossing the lesion, it was confirmed that the tip of microwire was in the true lumen by biplane DSA. The Excelsior SL-10 microcatheter (Stryker, Kalamazoo, MI, USA) was advanced along the microwire to the BA followed by superselective injection to reconfirm securing the true lumen. SL-10 microcatheter was exchanged to Gateway percutaneous transluminal angioplasty (PTA) balloon 2.0 × 12 mm (Stryker) using CHIKAI 315 EXC microwire (Asahi Intecc). Subsequently to the modest PTA, Gateway was exchanged with Prowler Select Plus microcatheter (Johnson & Johnson, Miami, FL, USA) for stenting. Stenting was performed using Enterprise 2 Vascular Reconstruction Device (VRD; Johnson & Johnson Cerenovus) (Fig. 2g). Complete recanalization of the right VA was achieved, and antegrade blood flow to the BA was re-established (Fig. 2h). Although the expansion of left cerebellar infarction was observed on DWI obtained two days after the treatment (Fig. 2i), he reached functional independence with an mRS score of 2 by three months after the onset. Maintenance DAPT with 75 mg of clopidogrel and 100 mg of aspirin was continued for three months followed by life-long monotherapy with 75 mg of clopidogrel. The angiographic cure of the right VA dissection (Fig. 2j) and functional independence (mRS 2) was confirmed at the 12-month follow-up.
Fig. 2. Case 2. (a) Initial DWI. The spotty acute multiple infarcts in the territory of bilateral AICA and pons are demonstrated. (b) Initial MRA. The signal of the right VA is faint and interrupted at the V4 segment (arrow). The left VA and proximal BA are not depicted. The middle to distal parts of the BA are faintly shown (double arrow). (c) BPAS–MRI. The outer shape of the bilateral VA and BA is shown. The outer diameter of the distal end of the right V4 segment is larger than that of the mid V4 (arrow). The left V4 segment presents tubular dilatation (double arrow). These findings indicate the outward dilatation of the bilateral V4 segment. The discrepancy between the inner lumen on MRA and the outer shape on BPAS strongly suggests dissection of the bilateral VA. (d) Initial right vertebral angiogram (lateral view). The right VA exhibits a tapered occlusion at the V4 segment (arrow). The BA is inadequately reconstituted (double arrow) by collateral flow via the anterior spinal artery (arrowhead). (e) Right vertebral angiogram before stenting (oblique view). The right V4 segment is occluded over a long distance. (f) Initial left vertebral angiogram (lateral view). The left VA exhibits long, irregular, severe stenosis through the V4 segment (arrow), followed by pseudo-occlusion. The BA is faintly depicted (double arrow). (g) Right vertebral angiogram after stenting (oblique view). Distal and proximal markers of Enterprise 2 VRD deployed in the affected segment are depicted (arrows). (h) Right vertebral angiogram after the stenting (oblique view). Complete recanalization and good dilatation of the affected right V4 segment are confirmed. (i) DWI obtained two days after the treatment. The expansion of the left cerebellar infarction is observed. (j) MIP image of 3D-DSA obtained 12 months after stenting. No in-stent restenosis is demonstrated. DWI: diffusion-weighted imaging, AICA: anteroinferior cerebellar artery, MRA: magnetic resonance angiography, VA: vertebral artery, BA: basilar artery, BPAS: basi-parallel anatomical scanning, VRD: Vascular Reconstruction Device, 3D-DSA: three-dimensional digital subtraction angiography.
Case 3
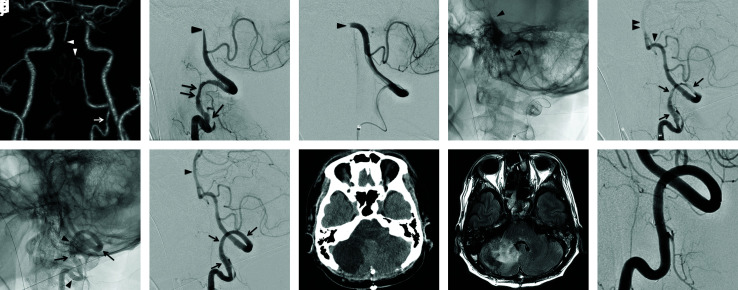
Case 3 was a 41-year-old man who presented with a sudden, severe occipital headache, deafness, vertigo, and rapidly deteriorating tetraparesis followed by respiratory arrest. Initial imaging and endovascular treatments were performed under artificial respiration. Computed tomography angiography (CTA) showed a long, irregular stenosis of the left V3 segment, a contrast filling defect extending from the left V4 segment to the proximal BA, and occlusion of the right VA (Fig. 3a). Immediately after CTA, DSA followed by endovascular treatment was started without MRI because of the patient’s critical condition and necessity of urgent endovascular reperfusion. DSA revealed an intimal flap with long and irregular stenosis at the left V3 segment, which were definitive findings of arterial dissection (Fig. 3b). The interruption of blood flow at the left V4 segment was also observed (Fig. 3b). Additional superselective angiography strongly suggested an embolic occlusion of the left V4 segment (Fig. 3c). On the basis of the angiographic findings, the patient was diagnosed as having a left VAD at the V3 segment causing a secondary embolic occlusion of the left V4 segment. Because the contralateral (right) VA was occluded (Fig. 3a), mechanical thrombectomy for the occluded left V4 segment was performed via the dissected left V3 segment. The first pass using Trevo XP ProVue 4 × 20 mm (Stryker) achieved recanalization of the left V4 segment (Fig. 3d and 3e). Even after complete recanalization of the left V4 segment, blood flow to the BA was still restricted due to severe stenosis of the dissected V3 segment (Fig. 3e). The contralateral (right) VA was occluded as mentioned earlier. In order to achieve patency of the left VA, two Enterprise 2 VRD were deployed to the affected left V3 segment in an overlapping manner (Fig. 3f) following the administration of a loading dose of DAPT (clopidogrel 300 mg and aspirin 200 mg). Good dilatation of the left V3 segment and restoration of antegrade blood flow were confirmed by the final DSA (Fig. 3g). The patient needed a decompression craniectomy two days after the treatment because of severe oedema in the right cerebellar hemisphere (Fig. 3h). Fluid-attenuated inversion recovery–MRI obtained 30 days after the treatment revealed haemorrhagic infarctions in the territory of the right posteroinfeior cerebellar artery and AICA that were not recanalized by the endovascular treatment (Fig. 3i). He regained functional independence (mRS 2) by three months after the onset. The morphological normalization of the left VA with no in-stent restenosis was confirmed by DSA obtained 12 months after the stenting (Fig. 3j).
Fig. 3. Case 3. (a) Initial CTA. CTA shows a long, irregular stenosis of the left V3 segment (arrow), a contrast filling defect extending from the left V4 segment to the proximal BA (arrow heads), and occlusion of the right VA. The distal part of the BA is depicted with the collateral flow via the bilateral posterior communicating artery. (b) Initial left vertebral angiogram (lateral view). The intimal flap (arrow) followed by a long irregular stenosis (double arrow) is shown at the left V3 segment. The left VA is interrupted at the distal part of the V4 segment (arrowhead). (c) Superselective injection via the microcatheter (lateral view). A crescent-shaped filling defect suggesting embolic occlusion is demonstrated at the distal end of the V4 segment (arrowhead). (d) Mechanical thrombectomy for left V4 segment occlusion. Trevo XP 4 × 20 mm is deployed from the proximal BA to the distal left V4 segment (arrowhead). (e) Left vertebral angiogram after thrombectomy (lateral view). Although the left V4 segment is recanalized (arrowhead), blood flow to the BA is still restricted (double arrowhead) by severe stenosis of the left V3 segment resulting from dissection (arrows). (f) Left vertebral angiogram after the stenting (lateral view). Two Enterprise 2 VRDs were deployed at the dissected V3 segment in an overlapping manner. Markers of the distal stent (arrows) and proximal stent (arrowheads) are shown. (g) Left vertebral angiogram after the stenting (lateral view). Good dilatation of the left V3 segment (arrows) and complete restoration of blood flow to the BA (arrowhead) are confirmed. (h) CT immediately after the decompression craniectomy. The infarction and oedema in the right cerebellar hemisphere are observed. (i) FLAIR–MRI obtained 30 days after the treatment. The haemorrhagic infarction in the territory of the right PICA and AICA is revealed. (j) Left vertebral angiogram obtained 12 months after stenting (lateral view). The morphological normalization of the left V3 segment with no in-stent restenosis is demonstrated. CTA: computed tomography angiography, BA: basilar artery, VA: vertebral artery, VRD: Vascular Reconstruction Device, CT: computed tomography, FLAIR: fluid-attenuated inversion recovery, MRI: magnetic resonance imaging, AICA: anteroinferior cerebellar artery, PICA: posteroinfeior cerebellar artery.
Discussion
Incidence of VBAD in acute large vessel occlusions
In this case series, VBAD was retrospectively diagnosed in 3 of the 134 (2.2%) AIS cases who underwent urgent endovascular reperfusion therapy. Although the result is similar to previous reports that VBAD accounted for 0.2–2.0% of AIS cases needing mechanical thrombectomy,1,3) the accurate incidence of VBAD in AIS is still unclear because of a limited number of reported cases. As far as we have identified, 10 reports have described 15 patients with VBAD that resulted in AIS treated by urgent endovascular reperfusion therapy since 2010.1,3,16–23) The information regarding the reported 15 patients and the three cases from this report is summarized in Table 1.
Table 1. Reported AIS cases due to VBAD underwent endovascular reperfusion therapy.
| No. | Age | Sex | Angiographic findings | Aetiology of large vessel occlusion | Endovascular treatment | Outcomes | ||
|---|---|---|---|---|---|---|---|---|
| Dissection site | Distal artery occlusion | Dissection site | Occluded distal artery | |||||
| 117) | 11 | M | Left V4 | BA | Distal occlusion | – | LIF | mRS 4 |
| 218) | 6 | M | Left V3 | BA | Distal occlusion | – | MT | mRS 0 |
| 319) | 41 | F | Right V4 | BA | Distal occlusion | – | MT | mRS 0 |
| 420) | 1 | M | Left V2–V3 | BA | Distal occlusion | – | MT | mRS 0 |
| 521) | 17 | M | Left V4 | BA | Distal occlusion | – | MT | mRS 1 |
| 61) | 33 | N.A. | BA | – | Local occlusion | MT | – | mRS 2 |
| 71) | 47 | N.A. | Right V4–BA | – | Local occlusion | MT stenting | – | mRS 1 |
| 816) | 59 | F | BA | – | Local occlusion | MT stenting | – | mRS 1 |
| 93) | 64 | M | BA | – | Local occlusion | MT stenting | – | mRS 6 |
| 103) | 47 | F | V4–BA* | – | Local occlusion | Stenting | – | mRS 1 |
| 113) | 51 | M | V4–BA* | – | Local occlusion | Stenting | – | mRS 3 |
| 123) | 49 | M | V4–BA* | – | Local occlusion | MT | – | mRS 1 |
| 133) | 38 | F | BA | – | Local occlusion | MT, stenting | – | mRS 2 |
| 1422) | 37 | F | Bilateral V4 | BA | Tandem occlusion | PTA | MT | mRS 3 |
| 1523) | 64 | M | Right V4 | BA | Tandem occlusion | PTA | MT | mRS 3 |
| 16 (Present case no. 1) | 42 | M | Left V3–V4 | BA | Distal occlusion | – | MT | mRS 0 |
| 17 (Present case no. 2) | 69 | M | Bilateral V4 | – | Local occlusion | Stenting | – | mRS 2 |
| 18 (Present case no. 3) | 41 | M | Left V3 | Left V4 | Tandem occlusion | Stenting | MT | mRS 2 |
* Dissection side was not applicable.
AIS: acute ischaemic stroke, VBAD: vertebrobasilar artery dissection, BA: basilar artery, LIF: local intraarterial fibrinolysis, mRS: modified Rankin Scale, MT: mechanical thrombectomy, M: male, F: female, NA: not applicable, PTA: percutaneous transluminal angioplasty.
Mechanisms of AIS due to VBAD
In the present three and previously reported 15 patients, the mechanisms of AIS were investigated based on the morphology of dissection sites, status of non-dissected distal artery, and haemodynamic function of the contralateral VA.
The present three patients have respectively different mechanisms of AIS, which are provisionally divided into distal occlusion in case 1, local occlusion in case 2, and tandem occlusion in case 3. Distal occlusion was the occlusion of the distal non-dissected artery due to an embolus from the dissection site. Local occlusion was the haemodynamic collapse of the entire vertebrobasilar artery system due to the arterial dissection itself. Tandem occlusion was the coexistence of distal occlusion and local occlusion.
In the reported 15 cases, the mechanisms of AIS could be classified into three subtypes similar to the earlier. Five patients were classified as distal occlusion (no. 1–5 in Table 1), 8 patients as local occlusion (no. 6–13 in Table 1), and 2 patients as tandem occlusion (no. 14 and 15 in Table 1).
Endovascular treatment
In the present three cases, the endovascular reperfusion therapy was selected based on the mechanisms of AIS: the reperfusion therapy for the distal occluded artery (mechanical thrombectomy in case 1, as a case of distal occlusion), the reconstructive therapy for the dissected artery (stenting in case 2, as a case of local occlusion), and the combination of the two procedures (thrombectomy and stenting in case 3, as a case of tandem occlusion).
A similar tendency was seen in the reported 15 cases. Five patients classified as distal occlusion underwent reperfusion therapy (mechanical thrombectomy or local intra-arterial fibrinolysis [LIF]) for the occluded distal artery (no. 1–5 in Table 1). Seven of eight patients classified as local occlusion received reconstructive therapy for the dissection site by stenting (no. 7–13 in Table 1). The two patients classified as tandem occlusion was treated by the combination of mechanical thrombectomy and PTA (no. 14 and 15 in Table 1). Almost all of reported treatments are theoretically acceptable. However, LIF (no. 1 in Table 1) might be inadequate for the patients with intracranial arterial dissection because of risk of subsequent haemorrhage from the dissection site.
The assumed rationales of the endovascular procedure corresponding to the specific mechanism of AIS are discussed in the following.
In cases of distal occlusion, cerebral ischaemia is caused by the embolic occlusion of the distal artery. Even when a dissected VA is occluded or severely stenosed, a contralateral non-dissected VA can serve as the pathway for blood flow to the BA. Therefore, mechanical thrombectomy for an occluded distal artery is sufficient for reperfusion. Thrombectomy can be done via a VA of the non-dissected side. Urgent stenting for a dissected VA is neither necessary nor desirable because there is the possibility of acute in-stent thrombosis without appropriate antiplatelet therapy. The endovascular parent artery occlusion for the dissected VA is an effective option to prevent the repeated embolism, especially when the dissection site is extradural segment. However, when the dissection involves the V4 segment such as case 1, its benefit is controversial because the intentional V4 occlusion can cause severe medullary infarction affecting patients’ outcomes.24) Therefore, the propriety of carrying out of parent artery occlusion should be decided based on the location of the dissection site.
In cases of local occlusion, stenting for a dissection site is the essential procedure for reperfusion because collapse of the dissection sites is the direct cause of ischaemia in the entire territory of the vertebrobasilar artery. In that case, a loading dose of DAPT must be administered prior to the stenting. We must be reminded the risk of perforation during crossing the lesion, especially when the dissection site is occluded. The operator must perceive the slightest bending of the microwire and the subtle resistance from the lesion. Although the various imaging modalities such as BPAS and three-dimensional DSA can support the endovascular procedures, the achievement of recanalization still depends on operator’s skills and penetration. It is controversial which type of stent is suitable for the reconstruction of the dissected artery. The closed cell or braided design stent with high metallic amount can not only facilitate the healing process theoretically but also accelerate acute in-stent thrombosis. We selected Enterprise stent because of its closed cell design and moderate metallic amount. The stenting is a reasonable solution for local occlusion; however, it must be noted that the stenting in acute VBAD is an emergency evacuation procedure for this life-threatening condition and is not covered by the public health insurance system in Japan.
In cases of tandem occlusion, the combination of thrombectomy and stenting is needed since this subgroup is under the composite pathological condition consisting of distal occlusion and local occlusion. In the present case 3, thrombectomy was performed by the stent retriever through the dissection site. There is an opinion that the stent retriever may aggravate the dissection, and the contact aspiration may be safer than the stent retriever. However, it is unclear whether the passing of large bore aspiration catheter is safer than that of the stent retriever. Further accumulation of experience and knowledge is needed.
Outcomes
In the present three cases and the reported 15 cases, the rate of functional independence defined as an mRS score of 0–2 at 90 days after the onset were 100% and 66.7%, respectively. Although the outcomes seem to be satisfactory, the efficacy of endovascular reperfusion therapy for VBAD cannot be proven yet. Because we could investigate only a limited number of patients having heterogeneous backgrounds, the outcomes were possibly affected by some bias.
Endovascular treatment corresponding to individual mechanism of AIS may improve patient outcomes. These findings should be further confirmed in a strict prospective study including a larger population.
Acknowledgments
We appreciate Keigo Naka as a physical therapist who contributed to the evaluation of patients’ outcomes.
Footnotes
Conflicts of Interest Disclosure
The authors declare that there are no conflicts of interest (COI). Five authors who are members of the Japan Neurosurgical Society (JNS) have registered online self-reported COI Disclosure Statement Forms through the website for JNS members. The remaining three authors who are members of the Japanese Society for Neuroendovascular Therapy (JSNET) have registered that through the website for JSNET members.
References
- 1). Fields JD, Lutsep HL, Rymer MR, et al. : Endovascular mechanical thrombectomy for the treatment of acute ischemic stroke due to arterial dissection. Interv Neuroradiol 18: 74– 79, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Hoving JW, Marquering HA, Majoie CBLM: Endovascular treatment in patients with carotid artery dissection and intracranial occlusion: a systematic review. Neuroradiology 59: 641– 647, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Labeyrie MA, Civelli V, Reiner P, et al. : Prevalence and treatment of spontaneous intracranial artery dissections in patients with acute stroke due to intracranial large vessel occlusion. J Neurointervent Surg 10: 761– 764, 2018 [DOI] [PubMed] [Google Scholar]
- 4). Compagne KCJ, Goldhoorn RB, Uyttenboogaart M, et al. : Acute endovascular treatment of patients with ischemic stroke from intracranial large vessel occlusion and extracranial carotid dissection. Front Neurol 10: 102, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Marnat G, Mourand I, Eker O, et al. : Endovascular management of tandem occlusion stroke related to internal carotid artery dissection using a distal to proximal approach: insight from the RECOST Study. AJNR Am J Neuroradiol 37: 1281– 1288, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Cohen JE, Leker RR, Eichel R, Gomori M, Itshayek E: Emergency endovascular revascularization of tandem occlusions: Internal carotid artery dissection and intracranial large artery embolism. J Clin Neurosci 28: 157– 161, 2016 [DOI] [PubMed] [Google Scholar]
- 7). Gory B, Piotin M, Haussen DC, et al. : Thrombectomy in acute stroke with tandem occlusions from dissection versus atherosclerotic cause. Stroke 48: 3145– 3148, 2017 [DOI] [PubMed] [Google Scholar]
- 8). Marnat G, Bühlmann M, Eker OF, et al. : Multicentric experience in distal-to-proximal revascularization of tandem occlusion stroke related to internal carotid artery dissection. AJNR Am J Neuroradiol 39: 1093– 1099, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Li S, Zi W, Chen J, et al. : Feasibility of thrombectomy in treating acute ischemic stroke because of cervical artery dissection. Stroke 49: 3075– 3077, 2018 [DOI] [PubMed] [Google Scholar]
- 10). Dmytriw AA, Phan K, Maingard J, et al. : Endovascular thrombectomy for tandem acute ischemic stroke associated with cervical artery dissection: a systematic review and meta-analysis. Neuroradiology 62: 861– 866, 2020 [DOI] [PubMed] [Google Scholar]
- 11). Farouk M, Sato K, Matsumoto Y, Tominaga T: Endovascular treatment of internal carotid artery dissection presenting with acute ischemic stroke. J Stroke Cerebrovasc Dis 29: 104592, 2020 [DOI] [PubMed] [Google Scholar]
- 12). Montalvan V, Ulrich A, Wahlster S, Galindo D: Arterial dissection as a cause of intracranial stenosis: a narrative review. Clin Neurol Neurosurg 190: 105653, 2020 [DOI] [PubMed] [Google Scholar]
- 13). Debette S, Compter A, Labeyrie MA, et al. : Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol 14: 640– 654, 2015 [DOI] [PubMed] [Google Scholar]
- 14). Maruyama H, Nagoya H, Kato Y, et al. : Spontaneous cervicocephalic arterial dissection with headache and neck pain as the only symptom. J Headache Pain 13: 247– 253, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Nagahata M, Manabe H, Hasegawa S, Takemura A: Morphological change of unruptured vertebral artery dissection on serial MR examinations. Evaluation of the arterial outer contour by Basi-parallel anatomical scanning (BPAS)-MRI. Interv Neuroradiol 12: 133– 136, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16). Gao P, Gui L, Yang B, Krings T, Jiao L: Optical coherence tomography of spontaneous basilar artery dissection in a patient with acute ischemic stroke. Front Neurol 9: 858, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Devue K, Van Ingelgem A, De Keukeleire K, De Leeuw M: A vertebral artery dissection with basilar artery occlusion in a child. Case Rep Emerg Med 2014: 706147, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18). Huded V, Kamath V, Chauhan B, et al. : Mechanical thrombectomy using solitaire in a 6-year-old child. J Vasc Interv Neurol 8: 13– 16, 2015 [PMC free article] [PubMed] [Google Scholar]
- 19). Senda J, Nishikawa T, Iizuka H, et al. : Thrombectomy using Trevo ProVue stent retriever devices after recombinant tissue plasminogen activator thrombolysis for acute basilar artery occlusion during vertebral artery dissection. Intern Med 55: 985– 989, 2016 [DOI] [PubMed] [Google Scholar]
- 20). Nicosia G, Cicala D, Mirone G, et al. : Childhood acute basilar artery thrombosis successfully treated with mechanical thrombectomy using stent retrievers: case report and review of the literature. Childs Nerv Syst 33: 349– 355, 2017 [DOI] [PubMed] [Google Scholar]
- 21). Buonomo O, Caragliano AA, Tessitore A, Pitrone A, Vinci SL: A multidisciplinary approach in the management of a paediatric posterior fossa ischaemic stroke: a case report. Cureus 11: e6418, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22). Mikkelsen R, Dalby RB, Hjort N, Simonsen CZ, Karabegovic S: Endovascular treatment of basilar artery thrombosis secondary to bilateral vertebral artery dissection with symptom onset following cervical spine manipulation therapy. Am J Case Rep 16: 868– 871, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23). Otsuji R, Uno J, Motoie R, et al. : Basilar artery occlusion with “Seizures” as a presenting symptom: three cases treated using mechanical thrombectomy. World Neurosurg 117: 32– 39, 2018 [DOI] [PubMed] [Google Scholar]
- 24). Endo H, Matsumoto Y, Kondo R, et al. : Medullary infarction as a poor prognostic factor after internal coil trapping of a ruptured vertebral artery dissection. J Neurosurg 118: 131– 139, 2013 [DOI] [PubMed] [Google Scholar]