Abstract
We evaluated the impact of COVID-19 on cancer screening in Manitoba, Canada using an interrupted time series (ITS) design and data from Manitoba's population-based, organized cancer screening programs from April 2020 to August 2021. In June 2020 (breast screening was suspended during April and May 2020), there was a 54% decrease between the predicted (i.e., observed data produced from regression models) and expected (i.e., counterfactual values produced for the COVID-19 period by assuming COVID-19 did not occur) number of screening mammograms (ratio = 0.46, 95% Confidence Interval (CI) 0.28–0.64). By December 2020, there was no significant difference between predicted and expected number of screening mammograms (ratio = 0.95, 95% CI 0.80–1.10). In April 2020, there was an 83% decrease in the number of Pap tests (ratio = 0.17, 95% CI 0.04–0.30). By January 2021, there was no significant difference between predicted and expected number of Pap tests (ratio = 0.93, 95% CI 0.81–1.06). In April 2020, there was an 81% decrease in the number of screening program fecal occult blood tests (FOBTs) (ratio = 0.19, 95% CI 0.0–0.44). By September 2020, there was no significant difference between predicted and expected number of FOBTs (ratio = 0.95, 95% CI 0.65–1.24). The estimated cumulative deficit (i.e., backlog) from April 2020 to August 2021 was 17,370 screening mammograms, 22,086 Pap tests, and 5253 screening program FOBTs. Overall, screening programs adapted quickly to the COVID-19 pandemic. Additional strategies may be needed to address remaining backlogs.
Keywords: Cancer, COVID-19, Epidemiologic studies, Screening, Canada
Abbreviations: CCMB, CancerCare Manitoba; CI, Confidence interval; FOBT, Fecal occult blood test; ITS, Interrupted time series; NBCCEDP, National Breast and cervical Cancer early detection program
1. Introduction
Cancer screening is a key part of cancer control. The province of Manitoba, located in central Canada (1.35 million in 2021), has three publicly funded, population-based, organized cancer screening programs for breast (BreastCheck), cervical (CervixCheck), and colorectal (ColonCheck) cancer operated by CancerCare Manitoba (CCMB). Established in 1995, BreastCheck invites women 50 to 74 years of age for a bilateral, two-view mammogram every two years. Screening mammograms are provided by the program through four fixed sites and mobile mammography units that visit approximately 45 rural, northern, and First Nations communities each year. Breast cancer screening for average risk women is not offered outside of the screening program. Strategies such as charter flights or group trips to the nearest screening site are used to increase access to screening for women living in very remote northern communities. Women with an abnormal mammography result are directly referred by the screening program for a diagnostic mammogram, ultrasound, or core biopsy. From 2016 to 2017, 56% of eligible women had a screening or diagnostic mammogram (43,000 screening mammograms per year) (CancerCare Manitoba, 2019).
CervixCheck was established in 2001 to ensure that Manitoba women receive organized, high-quality cervical cancer screening. Program guidelines recommend screening every three years for women 21 to 69 years of age. Pap tests are performed by primary care physicians, nurses, midwives, and nurse practitioners. CervixCheck maintains a population-based registry of all Pap tests and colposcopies performed in the province and monitors Pap test results to ensure appropriate follow-up. The program also reminds women to be screened, facilitates awareness and education about the importance of Pap tests, works with health care professionals to increase screening access, and supports health care provider, laboratory, and colposcopy quality assurance. From 2015 to 2017, 65% of eligible women had a Pap test (84,000 women per year) (CancerCare Manitoba, 2019).
In 2007, Manitoba launched ColonCheck for average risk individuals 50 to 74 years of age using the guaiac-based fecal occult blood test (FOBT) Hemoccult II SENSA. ColonCheck mails an FOBT kit to eligible individuals every two years once they turn 50 years of age. Individuals with an abnormal FOBT are referred by the program for a colonoscopy. Individuals may also complete an FOBT provided by their primary care provider. In 2016–2017, 50,266 individuals completed a mailed FOBT from ColonCheck and from 2016 to 2017, 53% of the eligible population was up-to-date for screening (i.e., completed an FOBT in the previous two years, a flexible sigmoidoscopy in the previous five years, or colonoscopy in the previous five years) (CancerCare Manitoba, 2019).
The onset of the COVID-19 pandemic and the subsequent need for physical distancing, the reallocation of health care resources, and implementation of new procedures to reduce the spread of COVID-19 necessitated immediate and significant changes to Manitoba's screening programs. In March 2020, BreastCheck operations were suspended, ColonCheck operations were reduced to processing returned FOBT kits, and CervixCheck operations were reduced to the follow-up of abnormal Pap test results. No screening invitations were mailed. Screening program staff were re-deployed to support new COVID-19 protocols such as patient and staff entry screening at CCMB. BreastCheck resumed limited operation at its primary location in June 2020 followed by other locations and the mobile screening units in July and August. In June 2020, screening program invitation letters were reinstated beginning with eligible individuals who had never been screened, were most due for screening, or were at potentially higher risk due to personal or family health history (i.e., a risk-based screening approach). BreastCheck mobile screening units began operations in geographically distant communities (most remote) and communities that had not had a screening clinic in the longest time. By September 2020, all three screening programs had resumed full operations. Full operations have continued throughout the subsequent waves of the pandemic. Screening programs also increased testing availability above usual levels beginning in September 2020, and provided more communication to the public and health care providers about the importance of cancer screening even during a pandemic and the policies and procedures that had been implemented to keep screening clients safe. To understand the full extent of the COVID-19 pandemic on breast, colorectal, and cervical cancer outcomes such as stage at diagnosis and survival, we must first understand and quantify the impact on cancer screening. Therefore, the objective of this study was to evaluate the impact of the COVID-19 pandemic on the number of screening mammograms, Pap tests, and screening program FOBTs completed each month from April 2020 to August 2021 in Manitoba, Canada.
2. Methods
2.1. Study design and data sources
We used an interrupted time series (ITS) study design, often used in the evaluation of natural experiments occurring in real-world settings (Lopez Bernal et al., 2017), to examine the number of screening mammogram, Pap test, and screening program FOBTs over time before COVID-19 (1 January 2015 until 15 March 2020) and after the start of COVID-19 and interventions implemented to mitigate its impact (16 March 2020 until 31 August 2021) on a monthly basis. We used data from BreastCheck, CervixCheck, and ColonCheck's population-based registries. BreastCheck includes women 50 to 74 years of age, ColonCheck includes individuals 50 to 74 years of age, and CervixCheck includes women 21 to 69 years of age in Manitoba. The study was approved by the University of Manitoba's Health Research Ethics Board (HS23979; H2020:264) and CCMB's Research and Resource Impact Committee (2020–14).
2.2. Outcomes
Outcomes included 1) the number of screening mammograms, Pap tests, and screening program FOBTs completed each month, 2) the cumulative deficit in the number of screening mammograms, Pap tests, and screening program FOBTs, and 3) the percent cumulative deficit in the number of screening mammograms, Pap tests, and screening program FOBTs. The cumulative deficit was defined as the difference between the monthly cumulative of the predicted number of screens and the monthly cumulative of the expected number of screens. The percent cumulative deficit was defined as the cumulative deficit in the predicted number of screens divided by the cumulative deficit in the expected number of screens.
2.3. Statistical analysis
Generalized linear models (Poisson, quasi-Poisson, negative binomial, gamma, inverse gaussian) were considered for the analyses. We evaluated model fit by plotting the predicted mean and variance of each model and the observed mean and variance in the data (Rodriguez, 2021). Scaled quantile residual plots were also used to evaluate the overall uniformity of residuals and dispersion (Hartig, 2021). A linear model was also considered. Model fit was evaluated using scaled residual plots. Each model included a binary intervention term that was equal to 0 during the pre-COVID-19 period and 1 during the COVID-19 period, a time term defined as the number of months since the start of the study period, and a month term that accounted for seasonality. Non-linear time and seasonality effects were accounted for using splines. Model building was performed by comparing the adjusted R-squared between subsequent models.
Predicted values to describe the observed data were produced for each outcome using regression models. Counterfactual predictions (or expected values) were also produced for the COVID-19 period by assuming COVID-19 did not occur. Plots were produced using the observed, predicted, and expected values. If plotted expected estimates were unrealistic (e.g., greatly above what would be expected from the baseline trend), the model was simplified until estimates were consistent with the baseline trend (i.e., the number of degrees of freedom for splines were reduced). COVID-19 by time interactions were considered if plotted predicted values in the COVID-19 period did not fit the observed data well when graphically evaluated (e.g., observed values were below predicted values during the early COVID-19 period but higher during the late COVID-19 period). March 2020 was excluded from the analyses because COVID-19 restrictions were implemented incrementally throughout March. April and May 2020 were excluded from the mammography analyses because BreastCheck ceased operations during this time. Likelihood ratio testing was used to produce p-values for the impact of COVID-19 by time interactions. Ratios between predicted values and expected estimates and 95% confidence intervals (CI; derived from contrast estimates) were calculated to complement the reported mean differences and 95% CIs. The cumulative deficit in the number of screening mammograms, Pap tests, and screening program FOBTs was calculated. The 95% CIs for the cumulative deficit were calculated with parametric bootstrapping and 1000 replications.
Data analyses were performed in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and R version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria). The following R packages were used: haven, splines, Hmisc, lattice, MASS, ggplot2, car, DHARMa, multcomp, and lmtest.
3. Results
Linear models demonstrated better model fit than the generalized linear models and therefore were used to analyze the data. Significant time interactions were found within each screening outcome but still demonstrated poor fit (i.e., the predicted values did not fit the observed values well). Therefore, we created multiple COVID-19 dummy variables representing different periods during the pandemic to provide a slope for each period which enabled more accurate predictions (for screening mammograms, April 2020 to February 2021, March 2021 to August 2021; for Pap tests, April 2020 to November 2020, December 2020 to August 2021; for screening program FOBTs, April 2020 to June 2020, July 2020 to September 2020, October 2020 to March 2021, April 2021 to August 2021).
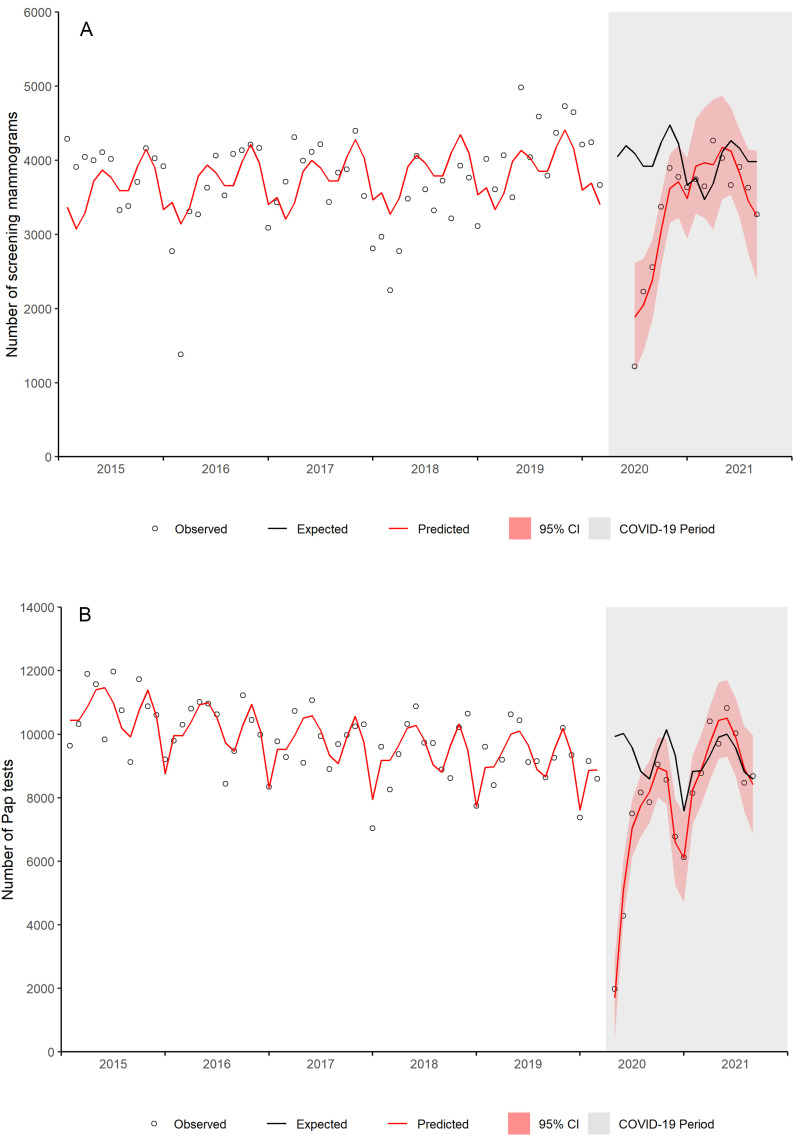
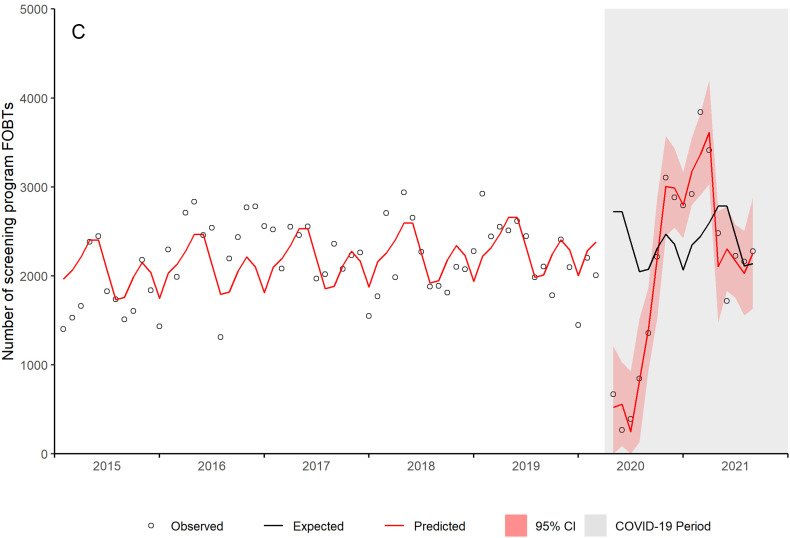
Linear regression results are provided in Table 1 (Supplementary material). Ratios between predicted and expected values and 95% CI for screening mammograms, Pap tests, and screening program FOBTs by month are provided in Table 2 (Supplementary material). Fig. 1a shows the observed number of screening mammograms, the predicted number of mammograms based on the regression model, and the expected number of mammograms (i.e., the number of mammograms expected in the absence of COVID-19) during the COVID-19 period (grey shaded area). The change in number of screening mammograms during the COVID-19 period demonstrated a significant time interaction (p value <0.001). When BreastCheck resumed limited operations at one location in June 2020, there was a 54% decrease in number of screening mammograms (ratio = 0.46, 95% CI 0.28–0.64). By December 2020, there was no significant difference between the predicted and expected number of screening mammograms (ratio = 0.95, 95% CI 0.80–1.10).
Fig. 1.
Number of (a) screening mammograms, (b) Pap tests, and (c) screening program FOBTs by month, Manitoba.
Fig. 1b shows the observed, predicted, and expected number of Pap tests each month, with a significant COVID-19 by time interaction (p value <0.001). In April 2020, there was an 83% decrease in the number of Pap tests (ratio = 0.17, 95% CI 0.04–0.30). The decrease was 49% for May 2020 (ratio = 0.51, 95% CI 0.42–0.60). By August 2020, there was no significant difference between the predicted and expected number of Pap tests (ratio = 0.95, 95% CI 0.84–1.07). The difference was again significant from October to December 2020 and then non-significant during 2021.
A significant COVID-19 by time interaction was also observed for screening program FOBTs (p value = 0.029) (Fig. 1c). In April 2020, there was an 81% decrease in the number of screening program FOBTs (ratio = 0.19, 95% CI 0.0–0.44). By September 2020, there was no significant difference between predicted and expected number of FOBTs (ratio = 0.95, 95% CI 0.65–1.24). By November 2020, the predicted number of screening program FOBTs was 27% higher than expected (ratio = 1.27, 95% CI 1.08–1.46).
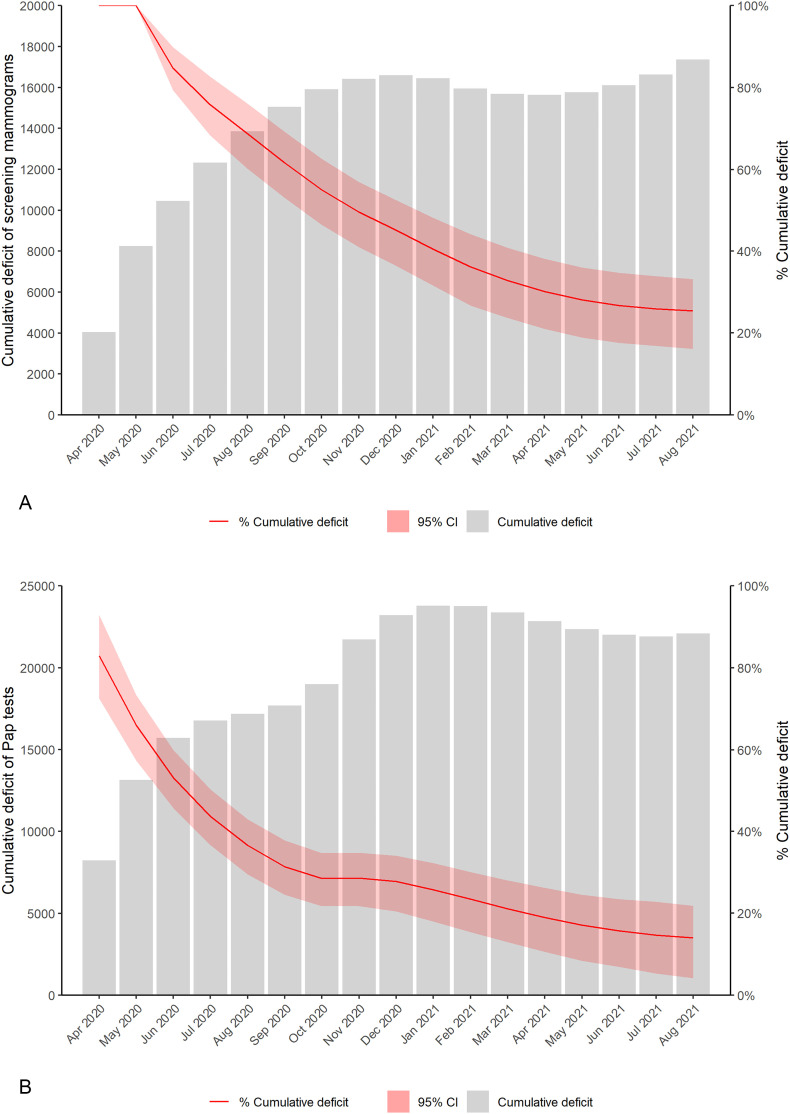
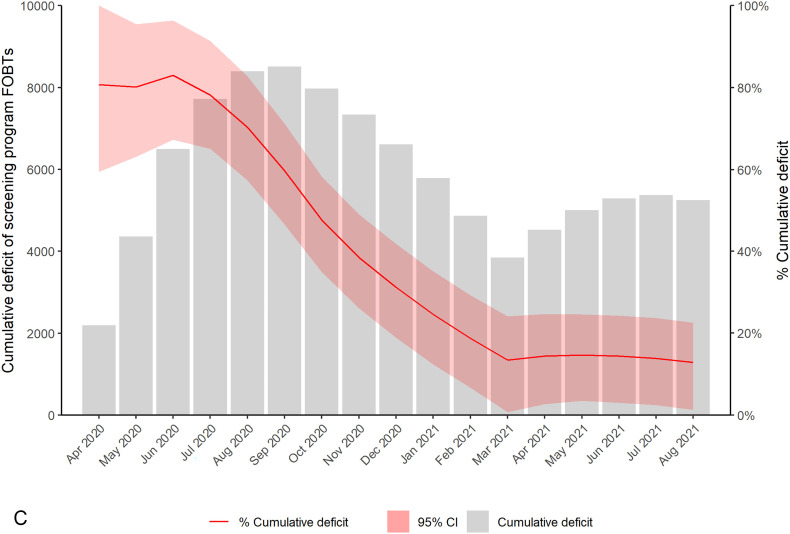
Fig. 2 and Table 3 (Supplementary material) show the cumulative deficit and percent cumulative deficit between the predicted and expected number of screening mammograms, Pap tests, and screening program FOBTs by month. By August 2021, the estimated cumulative deficit (i.e., the estimated backlog) was 17,370 for screening mammograms (25.5% fewer mammograms, 95% CI 16.1–33.2), 22,086 for Pap tests (14.0% fewer Pap tests, 95% CI 4.2–21.9), and 5253 for screening program FOBTs (12.9% fewer screening program FOBTs, 95% CI 1.3–22.6). For all three screening programs, the percent cumulative deficit steadily decreased over time (i.e., the predicted number of screens began to exceed the expected number of screens).
Fig. 2.
Cumulative deficit and percent cumulative deficit between the predicted and expected number of (a) screening mammograms, (b) Pap tests, and (c) screening program FOBTs by month, Manitoba.
4. Discussion
4.1. Main findings
At the start of the pandemic, cancer screening programs in Manitoba were immediately affected. However, within a few months, screening programs adapted to the COVID-19 pandemic. By the end of 2020, the number of screening mammograms provided by BreastCheck reached pre-pandemic levels and the pattern of care for 2021 was similar to that observed for 2015 to 2019. The number of screening program FOBTs exceeded expected levels in late 2020 as ColonCheck increased the number of invitations and FOBTs mailed to the eligible population. Unlike breast and colorectal cancer screening, CervixCheck does not provide Pap tests directly to women but relies on health care providers to deliver the service. Therefore, the decrease in the number of Pap tests seen in April and May 2020 may have been related to limited primary health care provider accessibility as many moved to virtual care and lower levels of health care use by individuals. Studies found that individuals were often hesitant to seek medical care out of fear of COVID-19 infection early in the pandemic (Wong et al., 2020; Jeffery et al., 2020). However, primary care providers and women appeared to quickly adapt to the pandemic and by January 2021, there was no longer a significant difference in the number of expected and predicted Pap tests.
Despite meeting or exceeding pre-Covid-19 screening numbers by the end of the 2021 summer and the third wave of the pandemic, a deficit in the number of screening tests was evident. Microsimulation modeling estimating the impact of reduced breast and colorectal cancer screening in Canada found that interruptions in screening have the potential to lead to additional increases in cancer stage at diagnosis and more deaths (Yong et al., 2021). Therefore, strategies such as those implemented in Manitoba to mitigate interruptions in screening are important, particularly since the COVID-19 pandemic and its impact on screening may increase disparities that are already evident in the population such as lower cancer screening rates among First Nations individuals (Decker et al., 2015; Decker et al., 2014; Demers et al., 2015; Wentzensen et al., 2021). However, these strategies may also be constrained by program operating and human resource capacity limitations.
Screening programs in Manitoba have also been able to minimize the impact of the COVID-19 pandemic on follow-up procedures for individuals with an abnormal screening outcome because both BreastCheck and ColonCheck arrange for most diagnostic tests. We have recently shown that Manitoba has been able to minimize the impact on surgical cancer resections (Decker et al., 2021). However, there is an ongoing delay in diagnostic and procedural services performed outside of the screening program due to staff redeployment to support the critical care units. The magnitude of overall impact on cancer outcomes, such as stage, mortality, and survival, are being evaluated in analyses that build on these results.
4.2. Comparison to previous studies
Two Canadian studies have examined the impact of COVID-19 on cancer screening. Walker et al. examined cancer screening in Ontario from January 1, 2019 until December 31, 2020 (Walker et al., 2021). Compared to 2019, breast cancer screening for average risk women dropped by almost 100% in April, May, and June 2020, 54% in July, and 23% in December. Breast screening for higher risk women recovered more quickly and was 15% higher by July 2020 compared to 2019. Walker et al. also found that colorectal and cervical cancer screening in Ontario decreased by over 90% in the spring of 2020 compared to 2019; by December, fecal tests and Pap tests were 20% lower in 2020. Meggetto et al. found that Pap tests decreased by 63.8% in Ontario in the first six months of the pandemic compared to 2019 (Meggetto et al., 2021). The impact of COVID-19 on cancer screening in Ontario is similar to Manitoba's experience, although Manitoba was less severely impacted by the first wave of the pandemic. Screening programs in Manitoba are also more centrally organized and therefore, may have been able to pivot more quickly.
Other countries have reported a similar impact on cancer screening, particularly during the first months of the pandemic (Perin et al., 2021). Several studies used modeling simulations to estimate the impact on screening (Smith et al., 2021; Jen et al., 2021), although a few have published screening rates. Colorectal cancer screening participation in the Netherlands dropped to 66.7% and 64.7% in February and March 2020 respectively, compared to 71.7% and 71.5% in February and March 2018 and 2019 (Kortlever et al., 2021). In the United States, the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), which provides cancer screening services to women with low income and inadequate health insurance, found that the number of NBCCEDP-funded breast and cervical cancer screening tests declined by 87% and 84%, respectively, during April 2020 compared with previous 5-year averages for that month (DeGroff et al., 2021). In May and June 2020, NBCCEDP breast and cervical cancer screening test volumes were 39% and 40% below the 5-year average for those months. Basu et al. found that cervical cancer screening in Bangladesh was 14.1% lower in 2020 compared to 2019 with significant decreases in the two country divisions that were the most impacted by the pandemic (25.3% in Dhaka and 37.3% in Chattogram) (Basu et al., 2021).
Unlike our analyses, most prior studies did not examine rates over time using an ITS design but compared the observed number of cancer screens in 2020 to the observed number of screens in a prior year. This approach does not take into consideration baseline or seasonal trends in screening rates. For example, in Manitoba, as in other Canadian provinces, there has been a downward trend in the number of Pap tests over time (Decker et al., 2016). This can be seen clearly in Fig. 1b. Hence, a comparison of the number of Pap tests from year to year would overestimate the decrease during the pandemic.
4.3. Strengths and limitations
This study includes several important strengths. First, we used of an ITS study design with a long pre-intervention period which permitted the evaluation of outcomes before the start of the COVID-19 pandemic, as well as the inclusion of seasonality and interactions between COVID-19 and time in the analysis. Second, we had access to timely, population-based, system-level screening data. Third, this study quantifies the impact of the COVID-19 pandemic on cancer screening. This is necessary to understand the impact of screening on potential changes in breast, colorectal, and cervical cancer stage at diagnosis and survival.
The results must also be interpreted within the Manitoba context of COVID-19 and therefore may not be generalizable to other jurisdictions. Manitoba experienced the easing of restrictions within six weeks of the start of the first wave with very few cases. The second (Nov 2020 to Jan 2021) and third (April 2021 to June 2021) waves of the pandemic were significantly more severe, but the screening programs had time to adjust and plan for modifications in service delivery. Finally, this analysis includes screening mammograms, Pap tests, and screening program FOBTs throughout three waves of the pandemic; the impact of the subsequent waves is yet to be measured.
5. Conclusions
In Manitoba, the COVID-19 pandemic resulted in decreases in breast, cervical, and colorectal cancer screening immediately after the implementation of COVID-19 restrictions. Within a few months, all screening programs adapted to the COVID-19 pandemic and one year later, the number of screening mammograms, Pap tests, and program FOBTs reached pre-pandemic levels. Although the deficit between the expected and predicted number of screening tests has decreased over time, additional strategies are needed to address the remaining backlog. The results from this analysis will now be used to assess the impact of COVID-19 shifts in the stage at diagnosis and survival for breast, cervical, and colorectal cancer.
Disclosure of funding and conflicts of interest
This work was supported by research grants from Research Manitoba and the CancerCare Manitoba Foundation. The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the University of Manitoba's Health Research Ethics Board (project code: HS23979, H2020:264), Manitoba Health's Health Information and Privacy Committee (2020/2021-16) and CancerCare Manitoba's Research and Resource Impact Committee (2020-14). Because data were de-identified, informed consent was not required.
Informed consent statement
Patient consent was waived because data were de-identified.
Data availability statement
The data that support the findings of this study are not publicly available to ensure and maintain the privacy and confidentiality of individuals' health information. Requests for data may be made to the appropriate data stewards (CancerCare Manitoba's Research and Resource Impact Committee).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We gratefully thank Natalie Biswanger and Kelly Bunzeluk from the Manitoba cancer screening programs for the provision of screening data and reviewing the draft manuscript, respectively.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2022.106961.
Appendix A. Supplementary data
Supplementary material: Table 1. Linear regression results; Table 2. Ratios and 95% confidence intervals between predicted and expected values; Table 3. Estimated cumulative deficit and percent cumulative deficit by month.
References
- Basu P., Lucas E., Zhang L., Muwonge R., Murillo R., Nessa A. Leveraging vertical COVID-19 investments to improve monitoring of cancer screening program - a case study from Bangladesh. Prev. Med. 2021;151:1–6. doi: 10.1016/j.ypmed.2021.106624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CancerCare Manitoba . Winnipeg; MB: 2019. Manitoba Cancer System Performance Report, 2019. [Google Scholar]
- Decker K.M., Demers A.A., Kliewer E.V., Biswanger N., Musto G., Elias B., et al. Pap test use and cervical cancer incidence in First Nations women living in Manitoba. Cancer Prev. Res. 2014;8(1):49–55. doi: 10.1158/1940-6207.CAPR-14-0277. [DOI] [PubMed] [Google Scholar]
- Decker K.M., Demers A.A., Kliewer E.V., Musto G., Shu E., Biswanger, et al. Colorectal cancer screening in First Nations people living in Manitoba. Cancer Epidemiol. Biomark. Prev. 2015;24(1):241–248. doi: 10.1158/1055-9965.EPI-14-1008. [DOI] [PubMed] [Google Scholar]
- Decker K.M., CM McLachlin, Group MaEW . Canadian Partnership Against Cancer; Toronto, ON: 2016. Cervical Cancer Screening in Canada: Monitoring and Evaluation of Quality Indicators. Special Feature: Cervical Cancer Screening in Young Women. [Google Scholar]
- Decker K.M., Lambert P., Feely A., Bucher O., Kim J.O., Hebbard P., et al. Evaluating the impact of the COVID-19 pandemic on new cancer diagnoses and oncology care in Manitoba. Curr. Oncol. 2021;28:3081–3090. doi: 10.3390/curroncol28040269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeGroff A., Miller J., Sharma K., Sun J., Helsel W., Kammerer W., et al. COVID-19 impact on screening test volume through the National Breast and Cervical Cancer early detection program, January-June 2020, in the United States. Prev. Med. 2021;2021:1–10. doi: 10.1016/j.ypmed.2021.106559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demers A.A., Decker K.M., Kliewer E.V., Musto G., Shu E., Biswanger N., et al. Mammography rates for breast cancer screening: a comparison of First Nations women and all other women living in Manitoba, Canada, 1999-2008. Prev. Chronic Dis. 2015;12(E82) doi: 10.5888/pcd12.140571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartig F. University of Regensberg; Regensberg, Germany: 2021. DHARMa: Residual Diagnostics for Hierarchical (Multi-level/Mixed) Regression Models.https://cran.r-project.org/web/packages/DHARMa/vignettes/DHARMa.html Available from: [Google Scholar]
- Jeffery M.M., D’Onofrio G., Paek H., Platts-Mills T.F., Soares W.E., III, Hoppe J.A., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first month of the COVID-19 pandemic in the US. JAMA Intern. Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jen G.H.-H., Yen A.M.-F., Hsu C.-Y., Chiu H.-M., Chen S.L.-S., Chen T.H.-H. Modelling the impacts of COVID-19 pandemic on the quality of population-based colorectal cancer screening. Prev. Med. 2021;151:1–10. doi: 10.1016/j.ypmed.2021.106597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortlever T.L., de Jonge L., Wisse Pieter H.A., Seriese Iris, Otto-Terlouw P., van Leerdam M.E., MCW Spaander, et al. The national FIT-based colorectal cancer screening program in the Netherlands during the COVID-19 pandemic. Prev. Med. 2021;151:1–6. doi: 10.1016/j.ypmed.2021.106643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez Bernal J., Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meggetto O., Jembere N., Gao J., Rey M., Rabeneck L., Murphy K.J., et al. The impact of the COVID-19 pandemic on the Ontario Cervical Screening Program, colposcopy and treatment services in Ontario, Canada: a population-based study. BJOG. 2021;128(9):1503–1510. doi: 10.1111/1471-0528.16741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perin D.M.P., Elfstrom K.M., Bulliard J.-L., Buron A., Campbell C., Flugelman A.A., et al. Early assessment fo the first wave of the COVID-19 pandemic on cancer screening services: the International Cancer Screening Network COVID-19 survey. Prev. Med. 2021;151:1–15. doi: 10.1016/j.ypmed.2021.106642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez G. Princeton University; Princeton, NJ: 2021. Generalized Linar Models. 4. A Model for Overdispersed Count Data.https://data.princeton.edu/wws509/r/overdispersion Available from: [Google Scholar]
- Smith M.A., Burger E.A., Castanon A., de Kok I.M.C.M., Hanley S.J.B., Rebolj M., et al. Impact of disruptions and recovery for establishing cervical screening programs across a range of high-income country program designs, using COVID-19 as an example: a modelled analysis. Prev. Med. 2021;151:1–15. doi: 10.1016/j.ypmed.2021.106623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker M.J., Meggetto O., Gao J., Espino-Hernandez G., Jembere N., Bravo C.A., et al. Measuring the impact of the COVID-19 pandemic on organized cancer screening and diagnostic follow-up in Ontario, Canada: a provincial, population-based study. Prev. Med. 2021;151:1–10. doi: 10.1016/j.ypmed.2021.106586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wentzensen N., Clarke M.A., Perkins R.B. Impact of COVID-19 on cervical cancer screening: challenges and opportunities to improve resilience and reduce disparities. Prev. Med. 2021;151:1–8. doi: 10.1016/j.ypmed.2021.106596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong L.E., Hawkins J.E., Langness S., Murrell K.L., Iris P., Sammann A. Where are all the patients? Addressing COVID-19 fear to encourage sick patients to seek emergency care. NEJM Catal. 2020;1:1–12. [Google Scholar]
- Yong J.H.E., Mainprize J.G., Yaffe M.J., Ruan Y., Poirier A.E., Coldman A., et al. The impact of episodic screening interruption: COVID-19 and population-based cancer screening in Canada. J. Med. Screen. 2021;28(2):100–107. doi: 10.1177/0969141320974711. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material: Table 1. Linear regression results; Table 2. Ratios and 95% confidence intervals between predicted and expected values; Table 3. Estimated cumulative deficit and percent cumulative deficit by month.
Data Availability Statement
The data that support the findings of this study are not publicly available to ensure and maintain the privacy and confidentiality of individuals' health information. Requests for data may be made to the appropriate data stewards (CancerCare Manitoba's Research and Resource Impact Committee).