Abstract
Objective
To characterize differences in disposition arrangement among rehab-eligible stroke patients at a Comprehensive Stroke Center before and during the COVID-19 pandemic.
Materials and Methods
We retrospectively analyzed a prospective registry for demographics, hospital course, and discharge dispositions of rehab-eligible acute stroke survivors admitted 6 months prior to (10/2019-03/2020) and during (04/2020-09/2020) the COVID-19 pandemic. The primary outcome was discharge to an inpatient rehabilitation facility (IRF) as opposed to other facilities using descriptive statistics, and IRF versus home using unadjusted and adjusted backward stepwise logistic regression.
Results
Of the 507 rehab-eligible stroke survivors, there was no difference in age, premorbid disability, or stroke severity between study periods (p>0.05). There was a 9% absolute decrease in discharges to an IRF during the pandemic (32.1% vs. 41.1%, p=0.04), which translated to 38% lower odds of being discharged to IRF versus home in unadjusted regression (OR 0.62, 95%CI 0.42-0.92, p=0.016). The lower odds of discharge to IRF persisted in the multivariable model (aOR 0.16, 95%CI 0.09-0.31, p<0.001) despite a significant increase in discharge disability (median discharge mRS 4 [IQR 2-4] vs. 2 [IQR 1-3], p<0.001) during the pandemic.
Conclusions
Admission for stroke during the COVID-19 pandemic was associated with a significantly lower probability of being discharged to an IRF. This effect persisted despite adjustment for predictors of IRF disposition, including functional disability at discharge. Potential reasons for this disparity are explored.
Key Words: Ischemic stroke, Rehabilitation, COVID-19, Recovery of function
Background
The coronavirus disease 2019 (COVID-19) pandemic has led to an unprecedented healthcare demand with hospital admissions at an all-time high and discharge options at an all-time low. The dramatic rise in hospitalizations for COVID-19 has been met with a commensurate demand in acute inpatient rehabilitation facility (IRF) bed availability. Therefore, the depletion of available inpatient beds will mirror the scarcity of IRF units. IRFs are being overrun by COVID-19 survivors, while other facilities have been repurposed into intensive care units to accommodate the surge of patients.1 Previously, we found that half as many patients admitted to our center during the COVID-19 pandemic were being discharged to IRFs.2 This observation has since been validated in a larger multicenter study which showed a 28% decline in discharges to IRFs,3 and a 40% decline in IRF discharges among patients with severe strokes who underwent thrombectomy.4 The decline in discharge rates to IRFs remains unexplained, and may be the consequence of many patient-level and system-wide factors which warrant further exploration. The implications of a 30-50% loss in rehab-eligible patients receiving aggressive physical, speech, and occupational therapy are tremendous.
Therefore, we sought to more specifically evaluate discharge planning and long-term outcomes of stroke patients treated during the COVID-19 pandemic who were recommended for discharge to an IRF. We hypothesized that a significant proportion of rehab-eligible patients were not being discharged to inpatient facilities. Furthermore, we hypothesize that missed opportunities in inpatient rehab care for these patients may ultimately impact their long-term functional outcome.
Materials and methods
Study design and participants
Data will be made available to any qualified investigator upon reasonable request. We conducted a retrospective analysis of a prospective observational cohort of all consecutive adult patients 18 years of age or older admitted to a Comprehensive Stroke Center diagnosed with acute ischemic stroke from 03/13/2019-09/12/2020. At our center, the diagnosis of an acute ischemic stroke is confirmed by a vascular neurologist. Patients in this study were eligible for inclusion if they developed acute stroke symptoms, or were last known well, within 2 weeks. Patients were included in the analysis on the basis of eligibility for discharge to an IRF. Rehab-eligible patients were defined qualitatively as medically stable patients with a functional deficit, and who were deemed able to learn and participate in rehabilitation activities based on the evaluation of our multidisciplinary discharge planning team. Therefore, patients were excluded if they did not survive hospitalization, if they were discharged to hospice, or if they were discharged to any other acute care facility (e.g., long-term acute care or other acute healthcare facility).
Data collection
The baseline demographic information, including age, sex, race, pre-morbid disability according to the modified Rankin Scale (mRS), pertinent past medical history, National Institutes of Health Stroke Scale (NIHSS) at presentation, transfer status, acute inpatient treatment, discharge recommendations by physical therapy/occupational therapy/speech and language pathology (PT/OT/SLP), final discharge disposition, length of hospital stay (LOS), and mRS at discharge and 90 days were abstracted from the electronic medical record. Diagnosis of COVID-19 was made by nasopharyngeal polymerase chain reaction at the time of admission, or within 2 weeks prior to stroke diagnosis. Missing data were not imputed. The primary outcome was discharge to IRF (versus any other disposition).
As per our institutional protocol, patients with an acute stroke are evaluated by licensed PT/OT/SLP therapists and physical medicine and rehabilitation (PM&R) staff as a means of facilitating stroke recovery, advising as to discharge readiness and providing recommendations for disposition among patients who are able to tolerate such an evaluation. Unless desired by the patient and/or legally authorized representative, patients recommended for IRF are typically discharged to such a facility. Our center's transitional navigator and social work team ensure that all patients, irrespective of insurance status, are referred for their medically recommended discharge disposition. For patients without insurance, the transitional navigator and social workers collaborate with the patient and/or representative in order to apply for insurance such that the most appropriate medical care can be delivered.
Statistical analysis
Descriptive statistics were used to compare baseline demographic, treatment, and outcome data between patients admitted in the 6-month period prior to COVID-19 being declared a national emergency (Pre-COVID-19: 10/2019 - 03/2020) and the first six months of the COVID-19 pandemic (COVID-19: 04/2020-10/2020). The COVID-19 period was chosen to begin in April of 2020 as that is the month when the state of New Jersey saw a significant rise in COVID-19 cases and COVID-19-associated hospital discharges. The 6-month COVID-19 admission period terminated in October 2020 due to availability of 3-month follow-up data at the time of data consolidation and analysis. Non-normally distributed continuous data were compared using the Wilcoxon Rank Sum test, with categorical data compared using the Chi square test, or Fisher's exact test when contingency table cell counts were less than 5. Unadjusted logistic regression was used to estimate the effect of admission during the COVID-19 period and all candidate variables on the primary outcome. A multivariable logistic regression model was then generated to estimate the effect of admission during the pandemic on discharge to IRF, including all variables significant to p<0.2 in univariate regression as fixed effects, and retaining only variables that remained associated with discharge to IRF using the backward stepwise method.
All tests were performed at the two-sided level with a significance level set at 0.05. No adjustments were made for multiple hypothesis testing. No sample size calculations were made as all analyses were exploratory. P-values are provided for convention and should be interpreted with caution. STATA 15.0 (College Station, TX) was used for all analyses. This study was approved with waiver of informed consent by the local Institutional Review Board and is reported in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Resuts
Of the 627 patients admitted during this study period, 8 admitted during the COVID-19 period had not been discharged at the time of analyses and were excluded, 105 (17.0%) expired or were discharged to hospice, and 7 were discharged to a long-term acute care facility (1.1%), leaving 507 patients included in this analysis (258 pre-COVID-19 and 249 during COVID-19).
The median age of included patients was 67 years (IQR 57-77), 229 (44.5%) were female, and 266 (52.3%) were White (Table 1 ). Compared to rehab-eligible stroke survivors admitted prior to the pandemic, patients admitted during COVID-19 had similar pre-morbid disability according to the modified Rankin Scale, and less frequently had hypertension and dyslipidemia (p≤0.05 for both; Table 1). Healthcare-associated infections (HCAI) were twice as common during the pandemic when compared to the preceding months (20.8% vs. 11.1%, p=0.01), but were not entirely accounted for by infection with SARS-CoV-2 (5.1% infection rate among tested persons), rates of pneumonia (3.9% vs. 4.3%, p=0.83), or infections of the urinary tract (4.7% vs. 5.0%, p=0.85). Numerically more infections were observed in the bloodstream (bacteremia: 4.7% vs. 1.9%, p=0.07) and the heart (endocarditis: 3.1% vs. 0.8%, p=0.06) during the pandemic months when compared to prior months. Only 1 out of 9 rehab-eligible survivors who experienced pneumonia had COVID-19.
Table 1.
Demographics.
| Pre-COVID-19 (n=258) | COVID-19 (n=249) | p-value | |
|---|---|---|---|
| Age, median y (IQR) | 68 (58-77) | 66 (57-75) | 0.18 |
| Female, no. (%) | 110 (42.6%) | 119 (46.3%) | 0.40 |
| Race, no. (%) | 0.57 | ||
| White | 137/257 (53.3%) | 129/252 (51.2%) | |
| Black | 75/257 (29.2%) | 84/252 (33.3%) | |
| Other/unk | 45/257 (17.5%) | 39/252 (15.5%) | |
| Hispanic, no. (%) | 31/248 (12.5%) | 31/252 (12.3%) | 0.95 |
| Pre-morbid mRS, median (IQR) | 0 (0-2) (n=257) | 0 (0-1) (n=222) | 0.19 |
| Pre-morbid mRS >2, no. (%) | 33/257 (12.8%) | 26/222 (11.7%) | 0.71 |
| Medical history, no. (%) | |||
| Hypertension | 220/258 (85.3%) | 194/255 (76.1%) | 0.01 |
| Dyslipidemia | 161/258 (62.4%) | 138/256 (53.9%) | 0.05 |
| Tobacco use | 133/252 (52.8%) | 134/242 (55.4%) | 0.56 |
| Diabetes | 110/258 (42.6%) | 91/256 (35.6%) | 0.10 |
| Prior stroke | 72/257 (28.0%) | 69/256 (27.0%) | 0.79 |
| Coronary artery disease | 65/257 (25.3%) | 48/256 (18.8%) | 0.07 |
| Atrial fibrillation | 48/256 (18.9%) | 41/256 (16.0%) | 0.41 |
| Congestive heart failure | 52/256 (20.3%) | 38/256 (14.8%) | 0.10 |
| Peripheral artery disease | 20/257 (7.8%) | 19/256 (7.4%) | 0.88 |
| Baseline NIHSS, median (IQR) | 3 (1-7) (n=255) | 2 (1-6) (n=223) | 0.17 |
| LVO*, no. (%) | 35 (13.6%) | 34 (13.2%) | 0.91 |
| Intravenous thrombolysis | 32 (12.4%) | 25 (9.7%) | 0.33 |
| Symptomatic ICH**, no. (%) | 2 (0.8%) | 1 (0.4%) | 0.57 |
| Healthcare-associated infection, no. (%) | 30 (11.6%) | 50 (20.8%) | 0.01 |
| COVID-19, no. (%) | 0/1 (0%) | 11/217 (5.1%) | n/a |
*LVO is defined as intracranial occlusion affecting the internal carotid, proximal middle cerebral (M1), or basilar arteries.
**Symptomatic ICH defined as a parenchymal hematoma type 2 associated with 4 or more point worsening in NIHSS.
COVID denotes coronavirus 2019 disease, IQR interquartile range, EMS emergency medical services, NIHSS National Institutes of Health Stroke Scale, LVO large vessel occlusion, and ICH intracerebral hemorrhage.
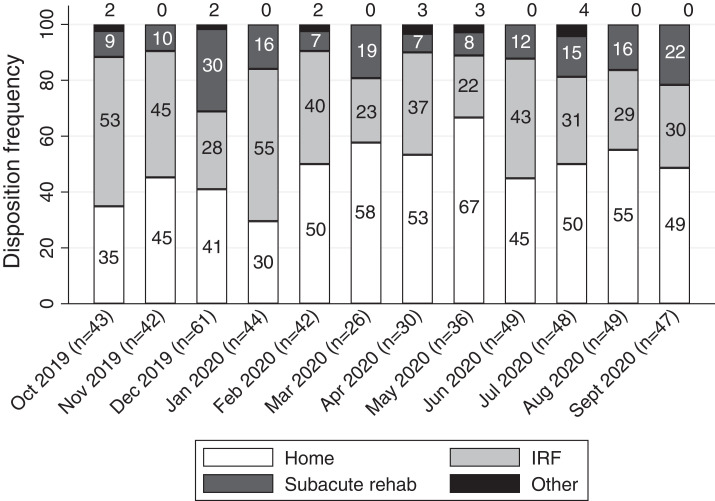
There was a 9% absolute decrease in discharges to IRF among rehab-eligible patients during the COVID-19 period when compared to the preceding months (Table 3), which translated to a 38% lower odds of being discharged to IRF versus home in unadjusted regression (OR 0.62, 95%CI 0.42-0.92, p=0.016). The lower rates of discharge to IRF peaked in May of 2020, then declined thereafter ( Fig. 1), but remained significantly different during the COVID-19 period when compared to preceding months. In univariate modeling, White race, greater stroke severity, presence of a proximal large vessel occlusion, healthcare-associated infection, and disability at discharge were all associated with discharge to IRF over home (Table 3). After adjustment for these variables in backward stepwise regression, the relationship between admission during the pandemic and discharge to IRF was strengthened (ORadj 0.16, 95%CI 0.09-0.31, p<0.001). In that model, White race (ORadj 1.91, 95%CI 1.16-3.14, p=0.01), more severe baseline deficits (ORadj 1.31, 95%CI 0.92-1.86, p=0.13), and higher discharge mRS (ORadj per point 3.46, 95%CI 2.63-4.55, p<0.001) remained associated with discharge to IRF over home.
Table 3.
Univariate and multivariable model for predicting discharge to IRF.
| Unadjusted OR for d/c to rehab vs. home (95%CI) | p-value | Adjusted OR for d/c to rehab (95%CI) | p-value | |
|---|---|---|---|---|
| Admission during pandemic | 0.62 (0.42-0.92) | 0.016 | 0.16 (0.09-0.31) | <0.001 |
| Age, per decade | 1.08 (0.94-1.23) | 0.26 | ||
| Female sex | 0.88 (0.60-1.30) | 0.52 | ||
| White race vs. other | 1.34 (0.92-1.98) | 0.13 | 1.91 (1.16-3.14) | 0.01 |
| Hispanic ethnicity | 0.67 (0.36-1.26) | 0.21 | ||
| Pre-morbid mRS | 0.98 (0.82-1.19) | 0.86 | ||
| Discharge mRS | 2.49 (2.06-3.01) | <0.001 | 3.46 (2.63-4.55) | <0.001 |
| Hypertension | 1.22 (0.75-1.98) | 0.42 | ||
| Dyslipidemia | 1.07 (0.73-1.57) | 0.74 | ||
| Tobacco use | 0.85 (0.58-1.26) | 0.42 | ||
| Diabetes | 1.05 (0.70-1.56) | 0.81 | ||
| Prior stroke | 1.13 (0.74-1.73) | 0.58 | ||
| Coronary artery disease | 0.94 (0.61-1.57) | 0.92 | ||
| Congestive heart failure | 1.17 (0.70-1.97) | 0.55 | ||
| Peripheral artery disease | 1.52 (0.72-3.20) | 0.27 | ||
| NIHSS* | 2.22 (1.67-2.95) | <0.001 | 1.31 (0.92-1.86) | 0.13 |
| LVO** | 2.53 (1.44-4.46) | 0.001 | 0.62 (dropped) | |
| Intravenous thrombolysis | 1.22 (0.69-2.17) | 0.49 | ||
| Healthcare-associated infection | 2.46 (1.33-4.55) | 0.004 | 0.64 (dropped) |
*NIHSS binned by 0-6, 7-14, and >14.
**LVO defined as intracranial occlusion affecting the internal carotid, proximal middle cerebral (M1), or basilar arteries.
Adjusted regression model was built using the backward stepwise method, including all candidate variables significant to p<0.2 in univariate regression, and retaining only variables which remained significant to p<0.2 after adjustment.
OR denotes odds ratio (with associated 95% confidence interval), mRS modified Rankin Scale, NIHSS National Institutes of Health Stroke Scale, LVO large vessel occlusion, and ICH intracerebral hemorrhage.
Fig. 1.
Month-by-month discharge disposition arrangements during the study period.
The lower odds of discharge to IRF were observed among rehab-eligible persons despite a significant increase in disability at discharge (median discharge mRS 4 [IQR 2-4] vs. 2 [IQR 1-3], p<0.001), which was in part driven by higher infection rates (other than COVID-19) during this period (median discharge mRS among patients with HCAI 4 [IQR 3-5] vs. 3 [IQR 1-4], p<0.001). This difference in disability among patients admitted during the COVID-19 period persisted at 3 months (p=0.009).
LOS was no different between the study periods (p=0.72; Table 2 ). Between the study periods, there was also no difference in median LOS among patients discharged to IRF (6d [IQR 3-12] vs. 5d [3-8], p=0.54) or to home (2d [IQR 1-4] vs. 2d [IQR 1-4], p=0.92), although LOS was generally longer among patients discharged to IRF versus home (6d [IQR 3-9] vs. 2d [IQR 1-4], p<0.001). Of the 11 patients with COVID-19 and stroke, 4 were discharged to IRF, 3 to a subacute inpatient rehabilitation facility, and 3 went home. The 11 patients with COVID-19 and stroke had a similar LOS when compared to stroke patients without COVID-19 who were admitted during the pandemic months (3d [IQR 2-14] vs. 3d [2-8], p=0.92).
Table 2.
Primary and secondary outcome measures.
| Pre-COVID-19 (n=258) | COVID-19 (n=249) | p-value | |
|---|---|---|---|
| Discharge to IRF, no. (%) | 106 (41.1%) | 80/249 (32.1%) | 0.04 |
| PT/OT recommendation for IRF, no. (%) | 118/257 (45.9%) | 92/246 (37.4%) | 0.05 |
| PT/OT recommendation for home services, no. (%) | 46/257 (17.9%) | 43/246 (17.5%) | 0.9 |
| mRS at discharge, median (IQR) | 2 (1-3) (n=258) | 4 (2-4) (n=229) | <0.0001 |
| Length of stay, median d (IQR) | 4 (2-7) (n=258) | 3 (2-8) (n=250) | 0.72 |
| mRS at 90 days, median (IQR) | 2 (1-3) (n=218) | 3 (1-4) (n=144) | 0.009 |
Discussion
In this follow-up analysis evaluating discharge planning among rehab-eligible patients with acute ischemic stroke, a smaller proportion were discharged to IRF during the COVID-19 pandemic when compared to the preceding 6-month period. Surprisingly, the effect of the pandemic on discharge to IRF persisted (and was strengthened) after adjustment for disability at the time of patient discharge. Importantly, there was no statistically significant difference in baseline stroke severity according to the NIHSS among rehab-eligible survivors before and during the pandemic, and length of hospital stay was no different between study periods. Therefore, we are left to conclude that the strokes that occurred during the pandemic left patients with greater functional disability, and yet numerically and proportionally fewer patients were being discharged to IRF. Furthermore, as we have shown previously,2 , 3 , 5 this decline in IRF discharges is met with a commensurate rise in discharge to home.
There are several potential explanations for the relative decrease in discharge to IRF, and the corresponding increase in discharge to home during the pandemic. One major factor pertains to IRF bed availability. As many as 1 in 5 hospitalized COVID-19 patients will require invasive mechanical ventilation, and COVID-19 survivors regardless of ventilatory needs will suffer from a variety of extrapulmonary complications leading to deconditioning.6 That said, according to early data from a New York Health system, fewer than 6% of COVID-19 survivors are being discharged to IRF or other care facilities.7 As many stroke survivors are left with some disability, the majority of our COVID-19 patients were ultimately discharged to acute or subacute rehabilitation facilities (64%). Importantly, there was no delay in discharge to IRF among these patients when compared to their non-COVID-19 counterparts, which likely reflects the overall mildness of their COVID-19. Some centers have also taken measures to increase bed availability during this crisis,8 while other facilities have had to suspend rehabilitation services due to local spread of the infection on the premises or due to limited healthcare personnel.9 In order to accommodate the large influx of patients due to the pandemic, some rehabilitation facilities have been repurposed to acute care units.10 In addition, many hospital-based IRFs have begun to decline outside referrals due to the overwhelming internal demands.10 The duration and need of IRF beds and services among COVID-19 survivors is incompletely understood,11 , 12 but many of these reports indicate a general decline in available rehabilitation services. We hope that our experience will better illuminate the short-term consequences and highlight a critical need to this aspect of the pandemic.
A second factor may relate to patient preference. Patients have deliberately avoided acute care for medical emergencies,13 , 14 cancelled outpatient appointments,15 and are avoiding inpatient and outpatient rehabilitation services in order to reduce the risk of acquiring COVID-19. We have previously reported declines in stroke admissions at our center during the early phase of the pandemic,2 and similar declines across a network of Comprehensive Stroke Centers.3 The decrease in patient discharges from this study appeared to recover by June of 2020, however, in the experience of the investigators, some patients continue to exhibit reticence in seeking medical attention due to pandemic fears. By July 2020, half of all COVID-19-related deaths nationwide occurred in long-term care facilities.16 This can be partly explained by the vulnerable patients in these facilities, as well as severe shortage in personal protective equipment and staff. These shortages have perpetuated the cycle of infection, as they decreased adherence to infection control protocols leading to an increased infection rate and therefore more staff having to call out to quarantine.16 The immediate fear of contracting the virus is of greater concern than the relief that can be achieved with early and aggressive physical and occupational therapy. The perceived short-term benefits by patients of returning home rather than the likely long-term benefits of discharge to an IRF may be even more desired among elderly stroke survivors for whom long-term survival is not guaranteed. While infection with SARS-CoV-2 does not discriminate, the elderly population remains at the highest risk for developing symptoms and complications of this deadly disease.17 Regarding support mechanisms, family members may be more reluctant to send their loved ones to an inpatient facility–especially in light of visitation restrictions–however they are also less available to provide home support due to social distancing measures.18 In our experience, we have seen that many patients and caregivers prefer to be discharged to home, ideally with home or outpatient PT/OT/SLP services. This often requires formal recommendations and planning by the multidisciplinary treatment team, without which these services will not be provided or covered by insurance. Therefore, when a patient/family request discharge to home, the multidisciplinary discharge planning team must make the recommendation for discharge to home with PT/OT/SLP services. We believe this to be why fewer patients were recommended for discharge to IRF during the pandemic months, especially given that patients were being discharged to home with greater functional disability. It is critical that healthcare providers are aware of these social issues and appropriately counsel their patients on the short- and long-term risks and benefits of their immediate decision making.
Among our other findings, we observed that discharge disability remained a strong and independent predictor of discharge to IRF in multivariable modeling. This is unsurprising as stroke survivors with moderate disability are more likely to benefit from early and aggressive rehabilitation.19 , 20
The potential lack of inpatient rehabilitation beds coupled with patient (or family) fear of transfer to an IRF represent an opportunity for process improvement. Telemedicine and telerehabilitation services offer the means to reduce physical contact while at the same time providing reliable services despite patient transportation limitations and other constraints. Unfortunately, many of these services require support staff (or family assistance) in order to demonstrate and carry out range of motion exercises, assess power, tone, and sensory input, assist with gait training, and to monitor for recovery of swallow function. As we explore telemedicine as a growing resource in care delivery, we hope that outpatient care can be more effectively and conveniently delivered to patients who fear transfer to another inpatient facility, or are avoidant of any outpatient programs.
Limitations
While this study is the first to offer some insight into the discharge planning and rehabilitation concerns of survivors with acute stroke, it is not without limitation. The small sample size and single-center representation of patients may not be generalizable to other populations. Our tertiary care center provides medical services to a catchment of 2.5 million inhabitants of southern New Jersey and arranges discharge dispositions throughout a region spanning more than 4,000 square miles. Furthermore, our region was moderately impacted by the early phase of the pandemic, having hospitalized over 2500 patients with COVID-19 since March 2020. Centers which treat fewer patients with COVID-19 may not experience the same declines in IRF transfers. Additionally, the 5.1% infection rate among stroke patients during this period may have under- (or over-) estimated the true infection rate in our population, given only 85% of patients were tested within 2 weeks of stroke. It is possible that more patients suspected of COVID-19 were treated at our center, and this could have affected rehabilitation disposition planning. Furthermore, we are unable to definitively prove that declines in IRF transfers during the pandemic were directly tied to bed availability in our region. The available evidence cited here suggests a concerning scarcity in inpatient and outpatient rehabilitation resources. However, due to limitations in data availability and the retrospective nature of this investigation, we cannot conclude that bed availability is the only (or major) reason for this disparity in care during a time of crisis. Finally, we did not evaluate the effect of insurance status on discharge planning, which has the potential to confound the analysis. However, lack of available insurance is never a barrier to care delivery at our institution. Our multi-disciplinary team, inclusive of social workers, transitional navigators, and discharge planners begin to consider disposition arrangements early in the course of a stroke patient's hospitalization, and when appropriate, will assist in obtaining insurance coverage for our uninsured patients. While our hospital acts as a tertiary care referral center for southern New Jersey, it also treats a local population of largely uninsured, undomiciled individuals who benefit from these services.
Conclusions
The COVID-19 pandemic has affected all levels of patient care. In this observational cohort study, we observed a decline in the number of rehab-eligible patients being discharged to IRF during the pandemic when compared to the preceding 6-month period. This difference appears to correlate with a commensurate rise in discharges to home, despite an increase in functional disability at discharge among stroke survivors. Rehabilitation bed scarcity, patient avoidance of healthcare facilities, costs of rehabilitation care, and declines in outpatient rehabilitation services are all targets for process improvement interventions in order to optimize stroke recovery. Therefore, it is critical for providers to take into account resource availability, social barriers, as well as alternative services when discharge planning.
Acknowledgments
Sources of funding
None.
Disclosures
None.
Acknowledgments
None.
References
- 1.Lew Henry L., Oh-Park Mooyeon, Cifu David X. The war on COVID-19 pandemic: role of rehabilitation professionals and hospitals. Am J Phys Med Rehabil /Assoc Acad Physiatrists. 2020;99(7):571–572. doi: 10.1097/PHM.0000000000001460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegler J.E., Heslin M.E., Thau L., et al. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29(8) doi: 10.1016/j.jstrokecerebrovasdis.2020.104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ortega-Gutierrez Santiago, Farooqui Mudassir, Zha Alicia, et al. Decline in mild stroke presentations and intravenous thrombolysis during the COVID-19 pandemic: the Society of Vascular and Interventional Neurology Multicenter Collaboration. Clin Neurol Neurosurg. 2021;201 doi: 10.1016/j.clineuro.2020.106436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czap Alexandra L., Zha Alicia M., Sebaugh Jacob, et al. Endovascular Thrombectomy Time Metrics in the Era of COVID-19: Observations from the Society of Vascular and Interventional Neurology Multicenter Collaboration. J Neurointervent Surg. 2021 doi: 10.1136/neurintsurg-2020-017205. [DOI] [PubMed] [Google Scholar]
- 5.Siegler James E., Zha Alicia M., Czap Alexandra L., et al. Influence of the COVID-19 pandemic on treatment times for acute ischemic stroke. Stroke. 2021;52(1):40–47. doi: 10.1161/STROKEAHA.120.032789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simpson Robert, Robinson Larry. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil /Assoc Acad Physiatrists. 2020;99(6):470–474. doi: 10.1097/PHM.0000000000001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richardson Safiya, Hirsch Jamie S., Narasimhan Mangala, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iannaccone Sandro, Castellazzi Paola, Tettamanti Andrea, et al. Role of rehabilitation department for adult individuals with COVID-19: the experience of the San Raffaele Hospital of Milan. Arch Phys Med Rehabil. 2020;101(9):1656–1661. doi: 10.1016/j.apmr.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bettger Prvu, Janet, Thoumi Andrea, Marquevich Victoria, et al. COVID-19: maintaining essential rehabilitation services across the care continuum. BMJ Global Health. 2020;5(5) doi: 10.1136/bmjgh-2020-002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stein Joel, Visco Christopher J., Barbuto Scott. Rehabilitation medicine response to the COVID-19 Pandemic. Am J Phys Med Rehabil /Assoc Acad Physiatrists. 2020;99(7):573–579. doi: 10.1097/PHM.0000000000001470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Falvey Jason R., Krafft Cindy, Kornetti Diana. The essential role of home- and community-based physical therapists during the COVID-19 pandemic. Phys Ther. 2020;100(7):1058–1061. doi: 10.1093/ptj/pzaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Biase Sarah, Cook Laura, Skelton Dawn A., et al. The COVID-19 Rehabilitation Pandemic. Age Ageing. 2020;49(5):696–700. doi: 10.1093/ageing/afaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhatt Ankeet S., Moscone Alea, McElrath Erin E., et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uchino Ken, Kolikonda Murali K., Brown Dena, et al. Decline in stroke presentations during COVID-19 surge. Stroke. 2020;51(8):2544–2547. doi: 10.1161/STROKEAHA.120.030331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mitchell Edith P. Declines in cancer screening during COVID-19 pandemic. J Natl Med Assoc. 2020;112(6):563–564. doi: 10.1016/j.jnma.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGarry Brian E., Grabowski David C., Barnett Michael L. Severe staffing and personal protective equipment shortages faced by nursing homes during the COVID-19 pandemic. Health Aff. 2020;39(10):1812–1821. doi: 10.1377/hlthaff.2020.01269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kunz Roland, Minder Markus. COVID-19 pandemic: palliative care for elderly and frail patients at home and in residential and nursing homes. Swiss Med Wkly. 2020;150:w20235. doi: 10.4414/smw.2020.20235. [DOI] [PubMed] [Google Scholar]
- 18.Keeney Tamra. Physical Therapy in the COVID-19 pandemic: forging a paradigm shift for rehabilitation in acute care. Phys Ther. 2020;100(8):1265–1267. doi: 10.1093/ptj/pzaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Musicco Massimo, Emberti Leonardo, Nappi Giuseppe, et al. Early and long-term outcome of rehabilitation in stroke patients: the role of patient characteristics, time of initiation, and duration of interventions. Arch Phys Med Rehabil. 2003;84(4):551–558. doi: 10.1053/apmr.2003.50084. [DOI] [PubMed] [Google Scholar]
- 20.Prescott R.J., Garraway W.M., Akhtar A.J. Predicting functional outcome following acute stroke using a standard clinical examination. Stroke. 1982;13(5):641–647. doi: 10.1161/01.str.13.5.641. [DOI] [PubMed] [Google Scholar]