Abstract
Background
The prevalence of shoulder disorders has been reported to range from seven to 36% of the population (Lundberg 1969) accounting for 1.2% of all General Practitioner encounters in Australia (Bridges Webb 1992). Substantial disability and significant morbidity can result from shoulder disorders. While many treatments have been employed in the treatment of shoulder disorders, few have been proven in randomised controlled trials. Physiotherapy is often the first line of management for shoulder pain and to date its efficacy has not been established. This review is one in a series of reviews of varying interventions for shoulder disorders, updated from an earlier Cochrane review of all interventions for shoulder disorder.
Objectives
To determine the efficacy of physiotherapy interventions for disorders resulting in pain, stiffness and/or disability of the shoulder.
Search methods
MEDLINE, EMBASE, the Cochrane Clinical Trials Regiter and CINAHL were searched 1966 to June 2002. The Cochrane Musculoskeletal Review Group's search strategy was used and key words gained from previous reviews and all relevant articles were used as text terms in the search.
Selection criteria
Each identified study was assessed for possible inclusion by two independent reviewers. The determinants for inclusion were that the trial be of an intervention generally delivered by a physiotherapist, that treatment allocation was randomised; and that the study population be suffering from a shoulder disorder, excluding trauma and systemic inflammatory diseases such as rheumatoid arthritis.
Data collection and analysis
The methodological quality of the included trials was assessed by two independent reviewers according to a list of predetermined criteria, which were based on the PEDro scale specifically designed for the assessment of validity of trials of physiotherapy interventions. Outcome data was extracted and entered into Revman 4.1. Means and standard deviations for continuous outcomes and number of events for binary outcomes were extracted where available from the published reports. All standard errors of the mean were converted to standard deviation. For trials where the required data was not reported or not able to be calculated, further details were requested from first authors. If no further details were provided, the trial was included in the review and fully described, but not included in the meta‐analysis. Results were presented for each diagnostic sub group (rotator cuff disease, adhesive capsulitis, anterior instability etc) and, where possible, combined in meta‐analysis to give a treatment effect across all trials.
Main results
Twenty six trials met inclusion criteria. Methodological quality was variable and trial populations were generally small (median sample size = 48, range 14 to 180). Exercise was demonstrated to be effective in terms of short term recovery in rotator cuff disease (RR 7.74 (1.97, 30.32), and longer term benefit with respect to function (RR 2.45 (1.24, 4.86). Combining mobilisation with exercise resulted in additional benefit when compared to exercise alone for rotator cuff disease. Laser therapy was demonstrated to be more effective than placebo for adhesive capsulitis (RR 8, 95%CI 2.11 to 30.34) but not for supraspinatus tendinitis (RR 2, 95%CI 0.98 to 4.09). Both ultrasound and pulsed electromagnetic field therapy resulted in improvement compared to placebo in pain in calcific tendinitis (RR 1.81 (1.26, 2.60) and RR 19 (1.16, 12.43) respectively). There is no evidence of the effect of ultrasound in shoulder pain (mixed diagnosis), adhesive capsulitis or rotator cuff tendinitis. When compared to exercises, ultrasound is of no additional benefit over and above exercise alone. There is some evidence that for rotator cuff disease, corticosteroid injections are superior to physiotherapy and no evidence that physiotherapy alone is of benefit for adhesive capsulitis
Authors' conclusions
The small sample sizes, variable methodological quality and heterogeneity in terms of population studied, physiotherapy intervention employed and length of follow up of randomised controlled trials of physiotherapy interventions results in little overall evidence to guide treatment. There is evidence to support the use of some interventions in specific and circumscribed cases. There is a need for trials of physiotherapy interventions for specific clinical conditions associated with shoulder pain, for shoulder pain where combinations of physiotherapy interventions, as well as, physiotherapy interventions as an adjunct to other, non physiotherapy interventions are compared. This is more reflective of current clinical practice. Trials should be adequately powered and address key methodological criteria such as allocation concealment and blinding of outcome assessor.
Plain language summary
Some physiotherapy interventions are effective for shoulder pain in some cases.
There is a high prevalence of shoulder disorders in the community. Shoulder disorders can result in considerable pain and disability. Physiotherapy is often the first line of treatment for shoulder disorder. Twenty‐six trials presented sufficient data to be included in meta‐analysis. There is some evidence from methodologically weak trials to indicate that some physiotherapy interventions are effective for some specific shoulder disorders. The results overall provide little evidence to guide treatment. There is a clear need for further high quality trials of physiotherapy interventions, including trials using combinations of modalities, in the treatment of shoulder disorders.
Background
Conditions causing shoulder pain are common and contribute substantially to the musculoskeletal morbidity of the community (Bjelle 1989). The prevalence of shoulder disorders has been reported to range from seven to 36% of the general population (Lundberg 1969). Shoulder disorders account for 1.2% of all general practice encounters in Australia, being third only to back and neck complaints as musculoskeletal reasons for primary care consultation (Bridges Webb 1992). In Dutch general practice the incidence of shoulder disorders has been estimated to be 11.2 per 1000 registered patients per year (van der Windt 1995). The shoulder is frequently injured, particularly in competitive sports. Eight to 13% of athletic injuries involve the shoulder (Hill 1983).
Prevalence of shoulder disorders has been shown to increase with age (Badley 1992). This finding has implications for the provision of health care in view of the aging of the population as a whole. In contrast, others (Allander 1974, Ingemar 1993) have demonstrated a decline in both the prevalence and incidence of shoulder pain with age, the peak prevalence occurring in the 56 ‐ 60 year age group.
Substantial disability may result from shoulder disorders. Moving the shoulder allows placement of the hand, hence compromised shoulder mobility impacts substantially on the performance of tasks essential to daily living (e.g. dressing, personal hygiene, eating and work). In addition, shoulder pain is often associated with impaired ability to sleep, so affecting mood and concentration. People with shoulder pain have been shown to score substantially less than normal values on the SF‐36 (a standardised measure of general health) for physical function, social function, physical role function, emotional role function and pain (Beaton 1996;Gartsman 1998). Shoulder disorders are often recalcitrant with some studies demonstrating persisting pain and disability from 12 months (van der Windt 1995) to 18 months (Chard 1991) in up to 50% of cases.
There are many commonly employed forms of treatment for shoulder disorders, including, non‐steroidal anti‐inflammatory drugs, glucocorticosteroid injections, oral glucocorticosteroid medication, manipulation under anaesthesia, physical therapy, hydrodilatation (distension arthrography) and surgery. A previous version of this systematic review of randomised controlled trials investigated all these treatments and concluded that there was very little evidence to either support or refute the efficacy of interventions commonly used to treat shoulder pain. Furthermore, the interpretation of results of studies that have been performed is hampered by the fact that these disorders are labelled and defined in diverse and often conflicting ways. (Green 1998) In a review of the diagnostic labels and/or definitions of the study populations, we concluded that most trials can be broadly categorised as studying adhesive capsulitis (specific diagnoses also including periarthritis and frozen shoulder) and/or rotator cuff tendonitis disease Green 1998. Shoulder pain and disorder may be caused by varying underlying pathologies, and the diagnostic criteria for defining these disorders are not consistently nor reliably applied. No standardised definitions are used and often there are conflicting criteria defining the same condition in different trials.
Since our original review (Green 1999), many new clinical trials, studying a diverse range of interventions, have been performed. In order to update and simplify the review, it has been subdivided into a series of reviews investigating the evidence for efficacy of single interventions. The review has also been broadened by including all randomised or pseudo‐randomised clinical trials regardless of whether outcome assessment was blinded.
This review examines the evidence for efficacy and safety of physiotherapy for the treatment of adults with shoulder pain. Physiotherapy encompasses a broad range of interventions. This group of interventions are often the first line of management for shoulder pain. The aim is to relieve pain, promote healing, reduce muscle spasms, increase joint range and strengthen weakened muscles and ultimately to prevent and treat functional impairment (Lee 1973). Physiotherapy interventions include manual physical therapy where passive joint mobilisation is employed to mobilise and stretch the soft tissue. Supervised and prescribed exercises aim to improve range of movement and muscle function by restoring shoulder mobility and stability. Physiotherapy interventions also include a number of electrotherapeutic modalities including Laser Therapy, Ultrasound, Bipolar Interferential Current, Transcutaneous Electromagnetic Stimulation, and Pulsed Electromagnetic Field Therapy. Laser therapy is light amplification by stimulated emission of radiation. This results in a beam of light of a single frequency with little divergence, thought to reduce inflammation and improve circulation (England 1989). Ultrasound is used as a physiotheray intervention for its physiological effects which include argumentation of blood flow, increased capillary permeability and tissue metabolism, enhancement of tissue extensibility, elevation of pain threshold, and alteration of neuromuscular activity leading to muscle relaxation (Downing 1986). Bipolar Interferential Current is believed to promote recovery by elevation of the pain threshold and promotion of muscle relaxation (van der Heijden 1996).Transcutaneous Electromagnetic Stimulation (TENS) uses analgesic currents and while its mechanism of action is not completely understood it is thought that it serves to release endogenous opiates in specific areas of the Central Nervous System (Herrera‐Lasso 1993). Pulsed Electromagnetic Field Therapy is thought to improve vascularisation, so promoting healing (Binder 1984). In practice, patients with shoulder pain seldom receive a single treatment intervention in isolation.
This review will specifically address the effectiveness of physiotherapy interventions alone or in combination for relief of pain and dysfunction of the shoulder.
Objectives
To determine the efficacy of physiotherapy interventions for shoulder pain and dysfunction.
Methods
Criteria for considering studies for this review
Types of studies
a) Randomised or pseudo‐randomised controlled trials. Studies where participants were not randomised into intervention groups were excluded from the review. b) Trials in which allocation to treatment or control group was not concealed from the outcome assessor were included but recorded as such in the table of included studies. c) Studies in all languages were translated into English and considered for inclusion in the review.
Types of participants
Inclusion in this review was restricted to trials with participants meeting the following criteria:
a) Adults >16 years of age. b) Shoulder pain or disorder for greater than 3 weeks. Studies that included various soft tissue disorders were considered if the results for shoulder pain were presented separately or if 90% or more of participants in the study had shoulder pain. c) Studies of participants suffering a history of significant trauma or systemic inflammatory conditions such as rheumatoid arthritis, hemiplegic shoulders, post‐operative and peri‐operative shoulder pain and pain in the shoulder region as part of a complex myofacial neck/shoulder arm pain were excluded.
Trials were sub grouped into type of shoulder disorder for analysis (see methods section).
Types of interventions
All randomised controlled comparisons of a physiotherapist delivered intervention versus placebo, no treatment, another intervention, or of varying physiotherapy interventions compared to each other were included.
Types of outcome measures
No studies were excluded on the basis of outcome measure used. The clinically relevant outcomes of interest in shoulder disorder are pain, range of motion (active and passive), function/ disability and quality of life, strength, return to work, participants' perception of overall effect, global preference, physicians' preference and adverse effects.
Search methods for identification of studies
MEDLINE, EMBASE, CINAHL (includes all major physiotherapy and occupational therapy journals from U.S.A., Canada, England, Australia and New Zealand), and Science Citation Index (SCISEARCH) were searched 1966 to June 2002 .
1 Shoulder Pain/ 2 Shoulder Impingement Syndrome/ 3 Rotator Cuff/ 4 exp Bursitis/ 5 ((shoulder$ or rotator cuff) adj5 (bursitis or frozen or impinge$ or tendinitis or tendonitis or pain$)).mp. 6 rotator cuff.mp. 7 adhesive capulitis.mp. 8 or/1‐7 9 exp Rehabilitation/ 10 exp Physical Therapy Techniques/ 11 exp Musculoskeletal Manipulations/ 12 exp Exercise Movement Techniques/ 13 exp Ultrasonography, Interventional/ 14 (rehabilitat$ or physiotherap$ or physical therap$ or manual therap$ or exercis$ or ultrasound or ultrasonograph$ or TNS or TENS or shockwave or electrotherap$ or mobili$). mp. 15 or/9‐14 16 Clinical trial.pt 17 random$.mp. 18 ((single or double) adj (blind$ or mask$)).mp. 19 placebo$.mp. 20 or/16‐19 21 8 and 15 an 20
In addition, the Cochrane Controlled Trials Register (CCTR) Issue 2, 2002 was searched.
Data collection and analysis
Following identification of potential trials for inclusion by the previously outlined search strategy, the methods sections of all identified trials were reviewed independently according to predetermined criteria (see selection criteria), by two reviewers. All articles were coded and details of source, intervention, population and funding recorded. Where the two reviewers disagreed, discussion was facilitated in order to reach consensus. If this was to fail, the trial was sent to a third reviewer for arbitration.
Trials meeting inclusion criteria were collated, and the methods and results sections re‐sent to the same two reviewers for assessment of trial validity and data extraction.
ASSESSMENT OF VALIDITY Validity of included trials was assessed by comment on whether they met key criteria (including appropriate randomisation, allocation concealment, blinding, number lost to follow up and intention to treat analysis). These criteria were based on the PEDro scale specifically designed and validated for the assessment of validity for trials of physiotherapy interventions (http://ptwww.cchs.usyd.edu.au/pedro/). Trials were not scored numerically. The only quantitative scoring was given for allocation concealment, ranked as:
A: adequate B: unclear, or C: inadequate.
Whether or not trials met the key methodological criteria was recorded on a pre‐piloted data extraction sheet and later transposed into the "Characteristics of Included Studies" table. Validity of trials was assessed in this qualitative way as opposed to using a numerical or summary scale. There are concerns regarding the validity of such scales and a lack of information about whether all the criteria included in such scales impact on the overall outcome of the trial (Juni 1999).
DATA EXTRACTION AND ANALYSIS In order to assess efficacy, raw data for outcomes of interest, specifically means and standard deviations for continuous outcomes and number of events for binary outcomes were extracted where available from the published reports. All standard errors of the mean were converted to standard deviation. Wherever reported data was converted or imputed, this was recorded in the notes section of the included studies table. For trials where the required data was not reported or not able to be calculated, further details were requested from first authors. If no further details were provided, the trial was included in the review and fully described, but not included in the meta‐analysis. An entry to that effect was made in the notes section of the included studies table.
When trial results were not normally distributed and so reported as median and range, the trial was not included in the meta‐analysis but results presented in Additional Tables. Meta‐analysis was facilitated by RevMan 4.1. The following choices of statistic and 95% confidence intervals were presented for all outcomes. CONTINUOUS OUTCOMES: Weighted mean difference using a fixed effect model was selected when outcomes were measured on standard scales. When outcomes were reported on non standard scales, using differing units and methods of assessment (for example disability scales), a standardised mean difference was selected. Possible clinical reasons for heterogeneity were explored, and in the presence of significant heterogeneity, trial results were not combined.
DICHOTOMOUS OUTCOMES: Relative risk using a fixed effects model was selected for interpretation of dichotomous outcome measures in this review as we believe that this is the most appropriate statistic for interpretation when the event is common . Reasons for heterogeneity were evaluated and in the event of significant heterogeneity trial results were not pooled.
SUBGROUP ANALYSIS Shoulder pain and disorder may be caused by varying underlying pathologies, and the diagnostic criteria for defining these disorders are not consistent nor reliably applied. In general, adhesive capsulitis was defined as the presence of pain with restriction of active and passive glenohumeral joint movements, and rotator cuff tendonitis was defined by the presence of painful arc and pain with resisted movements, and/or normal passive range of motion. However there were no standardised definitions used in the included trials and often there were conflicting criteria defining the same condition in different trials. For example, "pain with resisted movements of the shoulder and loss of passive abduction" was used to define rotator cuff tendonitis in one trial, whereas another trial used "pain on resisted abduction and full passive range of motion". Based upon review of the diagnostic labels and/or definitions of the study populations (Green 1998), most trials could be broadly categorised as studying adhesive capsulitis (specific diagnoses also including periarthritis and frozen shoulder) and/or rotator cuff tendonitis disease. For the purposes of subgroup analysis rotator cuff disease was categorised as tendinitis (specific diagnoses also including supraspinatus, infraspinatus and subscapularis tendonitis) or full rotator cuff tear. Results for each intervention were analysed within each diagnostic subgroup where described. If not described by the trialist, the population was labelled as general shoulder pain. This was planned a priori.
Results
Description of studies
Individual studies are fully described in the table of included studies. Sixty seven potentially eligible trials were identified by the search strategy. There was agreement in all cases between reviewers on inclusion of studies. A total of twenty‐six trials fulfilled the inclusion criteria. The reasons for exclusion of the other 41 trials are listed in the table of excluded studies. The 26 included studies are described below.
PHYSIOTHERAPY MODALITIES COMPARED WITH PLACEBO OR NO TREATMENT Fourteen studies compared a physiotherapy modality to placebo (one study included two different modalities and placebo). The physiotherapy modalities studied were bipolar interferential current (one trial) (van der Heijden 1999), ultrasound (five trials) (van der Heijden 1999; Ebenbichler 1999; Berry 1980; Downing 1986; Nykanen 1995), laser (three trials) (Taverna 1990; Saunders 1995; England 1989) pulsed electromagnetic field (two trials) (Dal Conte 1990; Binder 1984), combined iontophoresis of acetic acid plus ultrasound (one trial) (Perron 1997), supervised exercises (two trials) (Brox 1993/7; Ginn 1997) and mobilisation (one trial) (Bulgen 1984).
COMPARISONS OF ONE TYPE OF PHYSIOTHERAPY MODALITY TO ANOTHER Eight trials compared one type of physiotherapy modality to another.
Electrotherapeutic agents compared to non electrotherapeutic interventions: One trial compared electrotherapy plus exercise to mobilisation and manipulation (Winters 1997/9) and one trial compared physiotherapy including electromagnetic therapy to an identical intervention without electromagnetic therapy (Leclaire 1991). One type of electrotherapeutical agent to another: One trial compared bipolar interferential current to ultrasound (van der Heijden 1999) and two compared transcutaneous nerve stimulation (TENS) to ultrasound (Herrera‐Lasso 1993; Shehab 2000)
Manual interventions: Three trials compared mobilisation plus exercise to exercise alone (Nicholson 1985; Conroy 1998; Bang 2000)
Exercise interventions: One trial investigated the effect of isokinetic resisted exercise compared to biofeedback (Reid 1996).
PHYSIOTHERAPY MODALITIES COMPARED TO OTHER, NON PHYSIOTHERAPY TREATMENT INTERVENTIONS Seven trials compared injection to physiotherapy. These comprised two trials comparing intra‐articular corticosteroid injection with a combined physiotherapy intervention (van der Windt 1998; Berry 1980), two trials comparing intra‐articular and subacromial corticosteroid injection to electrotherapy and exercises (Winters 1997/9; Lee 1973), and three comparing injections to mobilisation and manipulation (Winters 1997/9; Bulgen 1984; Dacre1989).
One trial compared laser to non‐steroidal anti‐inflammatory medication (England 1989).
Risk of bias in included studies
Included studies were of varying methodological quality. A full description of whether or not the methods of each trial met the predetermined quality assessment criteria can be found in the table of included studies. Trial populations were generally small (median sample size = 48, range 14 to 180) with many trials underpowered to demonstrate a difference between groups if one was present. Six of the 26 trials (23%) had adequate allocation concealment (Downing 1986; Ebenbichler 1999; Ginn 1997; Lee 1973; van der Heijden 1999; van der Windt 1998) (1 unclear and 19 inadequate), 19/26 (73%) trials had a blinded outcome assessor (Bang 2000; Berry 1980; Binder 1984; Brox 1993/7; Conroy 1998; Dacre1989; Ebenbichler 1999; England 1989; Ginn 1997; Leclaire 1991; Nicholson 1985; Nykanen 1995; Perron 1997; Saunders 1995; Shehab 2000; Taverna 1990; van der Heijden 1999; van der Windt 1998; Vecchio 1993) and 10/26 (38%) trials blinded the participants ( Binder 1984; Dal Conte 1990; Downing 1986; Ebenbichler 1999; England 1989; Leclaire 1991; Nykanen 1995; Saunders 1995; Taverna 1990; Vecchio 1993). In eight trials (8/26; 31%) there was greater than 20% loss to follow‐up (Brox 1993/7; Downing 1986; Lee 1973; Nicholson 1985; Reid 1996; Saunders 1995; Shehab 2000; Winters 1997/9) and in 6/26 (23%) the trialists described intention to treat analysis (Brox 1993/7; Saunders 1995; Shehab 2000; Taverna 1990; van der Heijden 1999; van der Windt 1998).
Twenty trials (20/26; 77%) presented sufficient data to be included in meta‐analysis, two presented data in a form which could not be included in meta‐analysis so these results are included as additional tables, and four trials did not present any data that could be included in the review.
Effects of interventions
PHYSIOTHERAPY MODALITIES COMPARED WITH PLACEBO OR NO TREATMENT
ELECTROTHERAPY INTERVENTIONS
One trial of 145 participants demonstrated bipolar interferential current to be no more beneficial than placebo in general (mixed population) shoulder disorders for the recovery or substantial improvement in pain in the short or long term (6 weeks to 12 month follow‐up) (van der Heijden 1999).
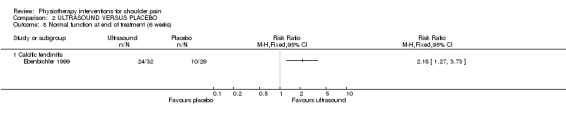
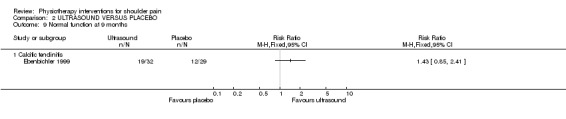
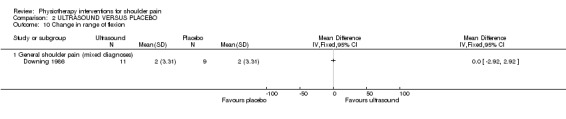
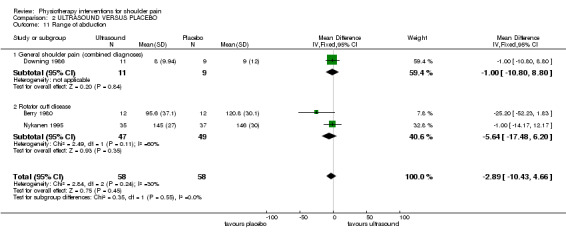
Based on the results of one trial (Ebenbichler 1999), ultrasound appears to have some significant benefit over placebo in calcific tendinitis (RR for recovery or substantial improvement in the short term (end of treatment) 1.81 (1.26, 2.60). In addition, the same trial demonstrated a significant effect in terms of improvement in radiological appearance of calcific tendinitis in the short term (end of treatment) (RR 4.53 (1.46, 14.07)) and long term (nine month follow‐up) (RR 3.74 (1.62, 8.66)). However, an additional trial investigating the effect of iontophoresis of acetic acid plus ultrasound (Perron 1997) found no significant benefit in calcific tendinitis. There is no evidence of effect of ultrasound in general shoulder pain or rotator cuff tendinitis. A pooled analysis of three trials assessing the effect of ultrasound on short term recovery or substantial improvement in three varying clinical conditions (van der Heijden 1999; Ebenbichler 1999; Berry 1980) demonstrated a very small but significant benefit over placebo (RR 1.41 (1.04,1.90)). This benefit was attributable to the trial in calcific tendinitis and was not supported by two additional trials, not included in the meta‐analysis, measuring the effect of ultrasound on pain (as opposed to recovery/ improvement). These trials demonstrated no benefit of ultrasound over placebo (Downing 1986; Nykanen 1995). Ultrasound had no significant effect demonstrated from pooled analysis of three trials on range of motion (WMD ‐2.89 (‐10.43, 4.66) (Downing 1986; Berry 1980; Nykanen 1995). No trial included in this review assessed adverse effects of ultrasound.
The effect of laser compared to placebo has been assessed by four trials, two included in meta‐analysis (Taverna 1990; Saunders 1995), one with results presented as single‐study forest plots (Vecchio 1993) and one with results presented as an additional table (England 1989). The pooled analysis demonstrates laser to be significantly more effective than placebo in bringing about a good or excellent result in the short term (RR 3.71, 95% CI 1.89 to 7.28). This analysis included a trial including participants with adhesive capsulitis (Taverna 1990) and a trial including participants with supraspinatus tendinitis (Saunders 1995). When looking at the results of each trial individually, the beneficial effect of laser therapy was only found for adhesive capsulitis. The trial including participants with rotator cuff tendinitis (Vecchio 1993) did not demonstrate statistically significant differences in outcomes between laser therapy and placebo. Finally, the fourth trial (England 1989), which included participants with supraspinatus or bicipital tendinitis, demonstrated a difference in medians of pain measured on a 10 cm VAS at 2 weeks to be 2.5cm (95% CI 2 to 3) (Table 1), however, the statistical significance of this difference could not be determined.
1. Results of included studies with data not appropriate for metaview.
| Study ID | Interventions | Outcome | Results |
| Shehab, 2000 | TENS VERSUS US | Pain post intervention | Median (Range) TENS 0(0‐.65) US 0.5(0‐2.75) Significantly better in US group |
| Flexion score post intervention | Median (Range) TENS 140 (120‐160) US 175 (115‐180) Significantly better in US group | ||
| Abduction score post intervention | Median (Range) TENS 130 (116.7‐156.5) US 180 (101.2‐180) Significantly better in US group | ||
| Brox, 1993 | ARTHROSCOPIC DECOPRESSION VERSUS EXERCISE | Pain at 3 months | Median Arthroscope 25 Median exercise 15 |
| Pain at 6 months | Median Arthroscope 25 Median exercise 25 | ||
| Pain at 2.5 years | Mean (SD) Arthroscope 24 (22) Mean (SD) exercise 22 (21) | ||
| Function at 3 months | Median Arthroscope 28 Median exercise 24 | ||
| Function at 6 months | Median Arthroscope 28 Median exercise 25 | ||
| Function at 2.5 years | Mean (SD) arthroscope 23 (20) Mean (SD) exercise 20 (19) | ||
| Overall change at 3 months | Median Arthroscope 84 Median exercise 74 | ||
| Overall change at 6 months | Median Arthroscope 87 Median exercise 86 | ||
| England 1989 | LASER VERSUS PLACEBO | Pain (10 cm VAS) at 2 weeks | Difference between medians (95% CI) 2.5cm (2,3) |
| Function (10cm VAS) at 2 weeks | Difference between medians (95%CI) 1.5cm (‐0.1,3.99) | ||
| Range of abduction (degrees) | Difference between medians (95% CI) 20 (10,40) | ||
| Range of flexion (degrees) | Difference between medians (95% CI) 15 (5,29) | ||
| LASER VERSUS NSAID | Pain (10 cm VAS) at 2 weeks | Difference between medians (95% CI) 2cm (1,3.5) | |
| Function (10cm VAS) at 2 weeks | No difference in medians | ||
| Range of abduction (degrees) | Difference between medians (95% CI) 20 (10,40) | ||
| Range of flexion (degrees) | Difference between medians (95% CI) 20 (10,40) | ||
Pulsed electromagnetic field (PEMF) has been shown in one trial to have a significantly beneficial effect on calcific tendinitis in both the short (RR 19, 95% CI 1.16 to 12.43) and medium (RR 39, 95% CI 2.46 to 617.84) term (Dal Conte 1990). A second trial assessing this intervention in general shoulder pain did not present quantitative analysis but concluded significant short term benefit (Binder 1984). PEMF resulted in more post treatment pain than placebo, but was not associated with increased adverse effect.
EXERCISES
A supervised exercise regime has been demonstrated to be of significant benefit in both the short and longer term. One trial of 56 participants with mixed shoulder disorders demonstrated significantly greater recovery (RR 7.74 (1.97, 30.32), function (RR 1.53 (0.98, 2.39)and range of abduction (RR for worsening range 0.33 (0.11, 0.96) than placebo at one month (Ginn 1997). A second trial, with a two and a half year follow up demonstrated sustained significant benefit with respect to function for exercise over placebo in rotator cuff disease (RR for good or excellent function 2.45 (1.24, 4.86) (Brox 1993/7).
MOBILISATION
Only one small trial of 42 participants with adhesive capsulitis divided into four groups assessed the effect of mobilisation compared to no treatment (and to ice and to intra‐articular corticosteroid injection) (Bulgen 1984). The data from this trial was not presented in a form allowing inclusion either in meta‐analyses or additional tables (presented graphically), but the authors concluded no significant differences between groups with respect to pain or range of motion.
COMPARISONS OF ONE TYPE OF PHYSIOTHERAPY MODALITY TO ANOTHER
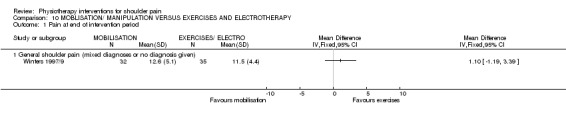
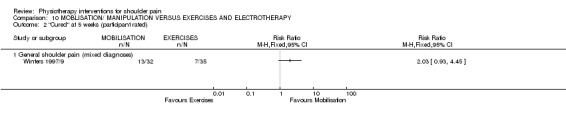
ELECTROTHERAPY INTERVENTIONS COMPARED TO NON ELECTROTHERAPY INTERVENTIONS.
One trial compared exercises and electrotherapy to mobilisation and manipulation and demonstrated no significant difference between the two groups in both the short or long term (Winters 1997/9). This trial contains no information about the benefits of either intervention over nothing. One trial demonstrated no additional benefit of electromagnetic therapy over physiotherapy alone (Leclaire 1991).
ONE TYPE OF ELECTROTHERAPEUTIC MODALITY COMPARED TO ANOTHER:
The effect of ultrasound was not significantly different to bipolar interferential current in the short or long term (van der Heijden 1999), however one trial showed significantly greater improvement with ultrasound than TENS (Shehab 2000). This was not supported by the results of a second trial (Herrera‐Lasso 1993).
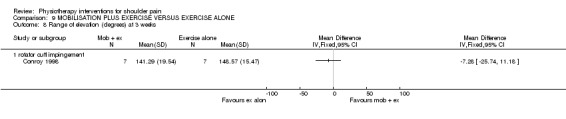
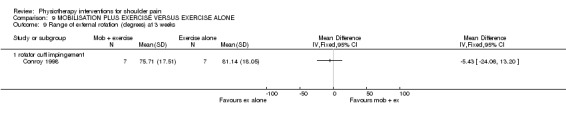
MANUAL INTERVENTIONS COMPARED TO EXERCISE
Based on three small trials it appears that mobilisation plus exercise is of greater benefit than exercise alone in rotator cuff disease, but not in adhesive capsulitis (Bang 2000; Conroy 1998; Nicholson 1985). Due to differences in scale and use of a combination of change scores and final value, results for pain could not be combined, however the two trials conducted in participants with rotator cuff disease both demonstrate a significant difference in reduction in pain at 3‐4 weeks for the exercise plus mobilisation group over the group performing exercise alone (WMD ‐186.23 (‐319.34, ‐53.12 (Bang 2000) and WMD ‐32.07 (‐58.04, ‐6.10)) (Conroy 1998) . The difference between groups with respect to range of motion, strength and function are based on only one of the three trials, but demonstrate benefit of adding mobilisation to exercise.
EXERCISE INTERVENTIONS COMPARED TO EACH OTHER
One trial with only 20 participants (Reid 1996) has shown no significant difference between a routine of isokinetic resistance exercises and use of electromyographic biofeedback for anterior instability. This was the only trial identified in a population with gleno‐humeral instability and tells us nothing about the benefit of exercise over no treatment.
PHYSIOTHERAPY MODALITIES COMPARED TO OTHER, NON PHYSIOTHERAPY,TREATMENT INTERVENTIONS
INJECTION
Seven trials compared injection to physiotherapy. These comprised two trials comparing intra‐articular corticosteroid injection with a combined physiotherapy intervention van der Windt 1998; Fernandes 1980, two trials comparing intra‐articular and subacromial corticosteroid injection to electrotherapy and exercises Winters 1997/9 Lee 1973, and three comparing injections to mobilisation and manipulation Winters 1997/9, Bulgen 1984, Dacre1989.
Several trials have compared the effect of physiotherapy to injection, however most have used differing physiotherapy modalities and injection sites making it not clinically sensible to combine the results of these trials in a meta‐analysis. One study with multiple outcomes assessed at many time points (van der Windt 1998) has demonstrated intra‐articular corticosteroid injection to be significantly more beneficial than a combination physiotherapy approach (mobilisation, exercise and electrotherapy) with respect to improvement in main complaint at 3 weeks, 7 weeks and 13 weeks, but not beyond. This benefit was maintained when combined with a second study assessing short term pain and demonstrating no significant difference between groups (Berry 1980). With respect to adverse effect, injection was associated with an increased risk of facial flushing (RR 9 (1.18, 68.74). These findings are supported by another trial comparing intra‐articular and subacromial cortico‐steroid injection to exercises and electrotherapy (Winters 1997/9) and demonstrating significant benefit of injection over physiotherapy in the short term (RR for 'cured' 3.72 (1.88, 7.37)), however in the longer term there was no difference between groups (RR for 'cured' 1.23 (0.47, 3.26). These results are consistent when injection is compared both to physiotherapy comprising mobilisation and manipulation (short term cure RR 1.83 (1.17, 2.88), long term cure RR 0.88 (0.36, 2.06).
A further study of injection compared to mobilisation presented results as a graph without numerical data but support the findings of the above trials, concluding no significant long term difference between injection and mobilisation, although some short term benefit with respect to pain in favour of injection (Bulgen 1984). In an old trial presenting their results graphically, no significant between group difference was reported for injection and exercise compared to heat and exercise at six weeks, but range of motion was the only outcome assessed (Lee 1973).
The only trial concluding no difference in short term benefit between physiotherapy and cortico‐steroid injection did not present results in a manner that could be included in the meta‐analysis, but was performed in a population with adhesive capsulitis (Dacre1989). All other trials were in a population with mixed shoulder disorders and rotator cuff disease.
MEDICATION
One trial compared laser to non‐steroidal anti‐inflammatory medication (England 1989) and demonstrated significant short term benefit in favour of laser with respect to pain, function and range of motion. The follow up for this trial however did not extend beyond the treatment period and hence little can be concluded about sustained effect (Table 1).
Discussion
While 26 trials are included in this review, there is substantial clinical heterogeneity with respect to the interventions tested and hence few trials could be combined in meta‐analysis to reach an overall conclusion about the effect of physiotherapy interventions for shoulder disorders. In addition, the results generated by this review are based on trials of very small numbers of participants and hence may be biased by Type II error (the failure to demonstrate a difference which is in truth present, or false negatives). Findings of no significant benefit are therefore consistent with no evidence to support or refute the use of the intervention.
Many of the trials included in this review were of poor methodological quality, with few concealing allocation or analysing results using intention to treat principles. Where possible, data was entered into the analysis section of the review as intention to treat, however the bias introduced by failure to conceal allocation, blind outcome assessors or obtain adequate follow up cannot be corrected in the review analysis and is likely to result in an overestimation of treatment effect.
Of major clinical concern is that few of the identified trials tested combinations of interventions, either more than one physiotherapy intervention or physiotherapy interventions combined with another intervetnion, despite this being the most common way in which shoulder disorders are treated by physiotherapists in practice. Shoulder disorders are difficult to diagnose and classify due to a common overlap of symptoms. Similarly, patients with shoulder disorders rarely receive a single treatment modality in isolation. Current clinical practice for shoulder disorders is likely to comprise not only a combination of physiotherapy intervetions, but also physiotherapy interventions combined with other medical treatments such as corticosteroid injection or medications. Very few trials have assessed combinations of treatments, with some directly comparing two interventions generally given together. This failure of trials to reflect actual practice in their tested interventions needs to be considered not only in interpreting the evidence available for the management of shoulder disorders using physiotherapy interventions, but also in planning future research. Trials should consider testing standardised methods of delivery of combination of physiotherapy interventions reflective of actual practice.
In many cases, included studies tested interventions in an ill‐defined or mixed population. It can be assumed from the selection criteria that these populations included a mix of diagnostic categories, for example adhesive capsulitis and rotator cuff disease. The same treatment modalities are rarely employed in clinical practice to treat people with varying shoulder disorders and it is likely that these trials were not able to accurately assess the effects of the intervention due to different subgroups of their populations responding in different ways. While the diagnosing of varying shoulder disorders is difficult and potentially unreliable , future trials would be of greater clinical benefit if performed in defined diagnostic categories.
Authors' conclusions
Implications for practice.
Further research, in particular larger trials of higher methodological quality, of well defined interventions and in specific populations need to be conducted. Furthermore, high quality trials more reflective of the current clinical practice of combined interventions using standardised methods of delivery need to be conducted before we can draw conclusions regarding the benefits and optimal use of physiotherapy interventions in the treatment of shoulder disorders. The evidence to date can be summarised as follows:
There is weak evidence from few, methodologically compromised trials to indicate:
Exercise for rotator cuff disease with additional benefit from exercise plus mobilisation (2 trials, Bang 2000; Conroy 1998).
Laser for adhesive capsulitis in the short term, but not for rotator cuff disease (4 trials, Taverna 1990; England 1989; Saunders 1995; Vecchio 1993)
Pulsed Electromagnetic Field for rotator cuff disease in the short term (1 trial, Binder 1984)
Ultrasound and Pulsed Electromagnetic Field for Calcific tendinitis. (2 trials Ebenbichler 1999; Dal Conte 1990)
In general, ultrasound is of no additional benefit over and above exercise alone (1 trial Winters 1997/9)
For rotator cuff disease, corticosteroid injections are superior to physiotherapy interventions (4 trials, van der Windt 1998; Berry 1980; Winters 1997/9; Bulgen 1984)
No evidence that physiotherapy interventions alone is of benefit for Adhesive Capsulitis (1 trial Dacre1989)
Supervised exercise regime is of benefit in the short and long term for mixed shoulder disorders and rotator cuff disease (Brox 1993/7; Ginn 1997)
Implications for research.
There is a clear need for trials of physiotherapy interventions, including trials of combinations of modalities, in the treatment of shoulder disorders. There is a need for validation studies of the inclusion and exclusion criteria used to define specific conditions which result in painful shoulder and trials should aim to use properly defined interventions. Trials should be adequately powered and address key methodological criteria (allocation concealment, blinding of participants and outcome assessors, adequate follow up and appropriate statistical reporting). Specifically, further research is needed before we can draw conclusions about:
Any physiotherapy intervention for Rotator Cuff tear
Physiotherapy interventions as an adjunct to medical interventions in any shoulder disorder.
Any physiotherapy intervention for instability or hypermobility of the glenohumeral joint.
What's new
| Date | Event | Description |
|---|---|---|
| 18 February 2013 | Amended | Minor revision made to the abstract and results section regarding the effect of laser therapy. In the previous version, the effect estimate and 95% confidence interval for the pooled result of laser therapy for adhesive capsulitis (AC) and rotator cuff disorders (RCD) was incorrectly reported to support the statement that laser therapy is effective for AC but not RCD. The appropriate effect estimates and 95% confidence intervals to support this statement have been inserted. The conclusion that laser therapy is effective for AC but not RCD has not been modified. |
History
Review first published: Issue 2, 2003
| Date | Event | Description |
|---|---|---|
| 1 May 2008 | Amended | Converted to RM5. CMSG ID C067‐R |
| 24 February 2003 | New citation required and conclusions have changed | Substantive amendment |
| 24 February 2003 | Amended | This review is based on the original review of 'Interventions for shoulder pain'. Please see published notes for further details. |
Notes
Since the original review which included all interventions for shoulder pain, many new clinical trials, studying a diverse range of intervetions, have been performed. In order to update the review, it has been subdivided into a series of reviews investigating the evidence for efficacy of single interventions. The review has also been broadened by including all randomised or pseudo‐randomised clinical trials regardless of whether outcome assessment was blinded.
This review will be split into separate reviews on updating: Physical therapies for shoulder pain due to adhesive capsulitis (frozen shoulder); Physical therapies for shoulder pain due to rotator cuff disoders; Electrotherapy modalities for shoulder pain due to adhesive capsulitis (frozen shoulder); and Electrotherapy modalities for shoulder pain due to rotator cuff disorders. Physiotherapy interventions for shoulder pain will be withdrawn from publication in The Cochrane Library, once the new reviews are published.
Acknowledgements
We are grateful to Steve McDonald from the Australasian Cochrane Centre for his help with the search strategy and to the Centre of Evidence‐based Physiotherapy at the University of Sydney for the use of the PEDro trial quality assessment method and database.
Data and analyses
Comparison 1. BIPOLAR INTERFERENTIAL CURRENT VERSUS PLACEBO.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recovery or substantial improvement at 6 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Recovery or substantial improvement (participant rated) at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Recovery or substantial improvement (participant rated) at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Recovery or substantial improvement (participant rated) at 9 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Recovery or substantial improvement (participant rated) at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
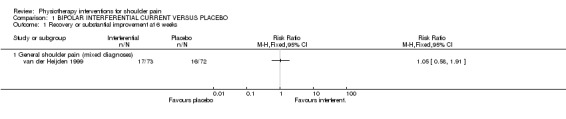
Comparison 1 BIPOLAR INTERFERENTIAL CURRENT VERSUS PLACEBO, Outcome 1 Recovery or substantial improvement at 6 weeks.
1.2. Analysis.
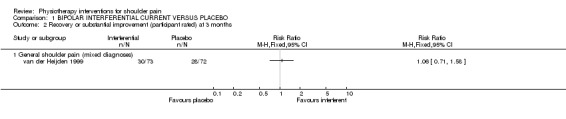
Comparison 1 BIPOLAR INTERFERENTIAL CURRENT VERSUS PLACEBO, Outcome 2 Recovery or substantial improvement (participant rated) at 3 months.
1.3. Analysis.
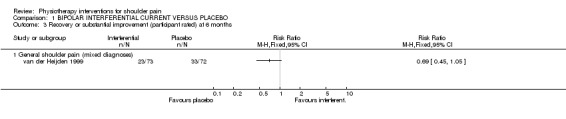
Comparison 1 BIPOLAR INTERFERENTIAL CURRENT VERSUS PLACEBO, Outcome 3 Recovery or substantial improvement (participant rated) at 6 months.
1.4. Analysis.
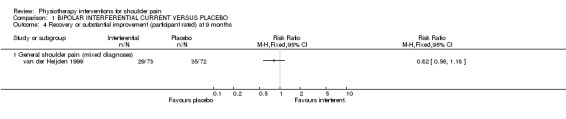
Comparison 1 BIPOLAR INTERFERENTIAL CURRENT VERSUS PLACEBO, Outcome 4 Recovery or substantial improvement (participant rated) at 9 months.
1.5. Analysis.
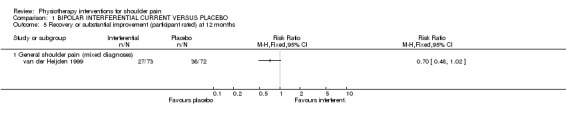
Comparison 1 BIPOLAR INTERFERENTIAL CURRENT VERSUS PLACEBO, Outcome 5 Recovery or substantial improvement (participant rated) at 12 months.
Comparison 2. ULTRASOUND VERSUS PLACEBO.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recovery or substantial improvement (participant rated) ‐ short term | 3 | 229 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [1.04, 1.90] |
| 1.1 General shoulder pain (combined diagnoses) | 1 | 145 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [0.77, 2.70] |
| 1.2 Calcific tendinitis | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.81 [1.26, 2.60] |
| 1.3 Rotator cuff disease | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.35, 1.28] |
| 2 Recovery or substantial improvement (participant rated) at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 General shoulder pain (combined diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Recovery or substantial improvement (participant rated) at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 General shoulder pain (combined diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Recovery or substantial improvement (participant rated) at 9 months | 2 | 206 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.78, 1.30] |
| 4.1 General shoulder pain (mixed diagnoses) | 1 | 145 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.60, 1.26] |
| 4.2 Calcific tendinitis | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.90, 1.77] |
| 5 Recovery or substantial improvement (participant rated) at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Resolution or improvement of radiological finding at end of treatment (6 weeks) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 Calcific tendinitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Resolution or improvement of radiological finding at 9 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Calcific tendinitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Normal function at end of treatment (6 weeks) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Calcific tendinitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Normal function at 9 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Calcific tendinitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Change in range of flexion | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 General shoulder pain (mixed diagnoses) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Range of abduction | 3 | 116 | Mean Difference (IV, Fixed, 95% CI) | ‐2.89 [‐10.43, 4.66] |
| 11.1 General shoulder pain (combined diagnoses) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.0 [‐10.80, 8.80] |
| 11.2 Rotator cuff disease | 2 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐5.64 [‐17.48, 6.20] |
| 12 Change in internal rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 General shoulder pain (combined diagnoses) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Change in external rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 General shoulder pain (combined diagnoses) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Pain (100mmVAS) at 4 weeks | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Rotator Cuff Disease | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Painfree at 4 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Pain (out of 20) at 4 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Rotator cuff disease | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Pain (out of 20) at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Rotator cuff disease | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Function (out of 14) at 4 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Rotator cuff disease | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Function (out of 14) at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Rotator cuff disease | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
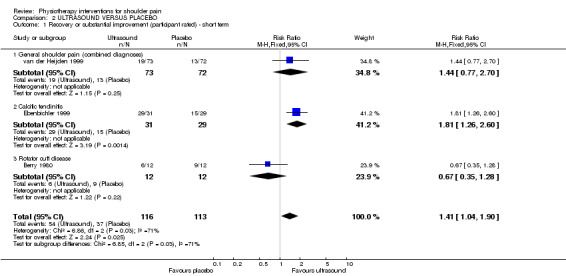
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 1 Recovery or substantial improvement (participant rated) ‐ short term.
2.2. Analysis.
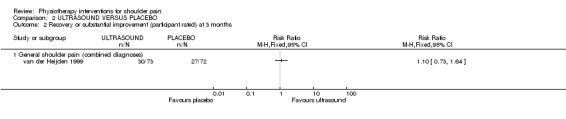
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 2 Recovery or substantial improvement (participant rated) at 3 months.
2.3. Analysis.
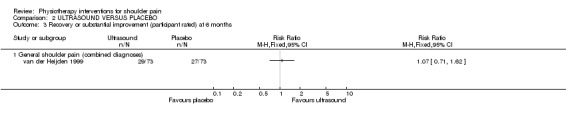
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 3 Recovery or substantial improvement (participant rated) at 6 months.
2.4. Analysis.
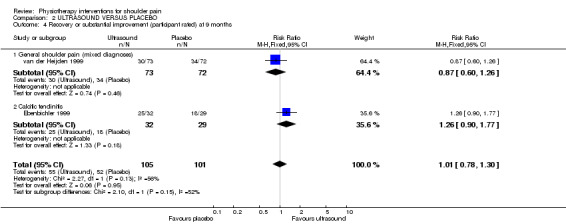
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 4 Recovery or substantial improvement (participant rated) at 9 months.
2.5. Analysis.
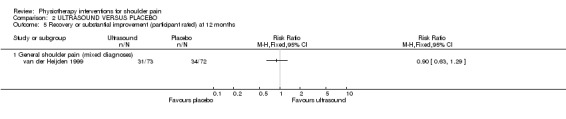
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 5 Recovery or substantial improvement (participant rated) at 12 months.
2.6. Analysis.
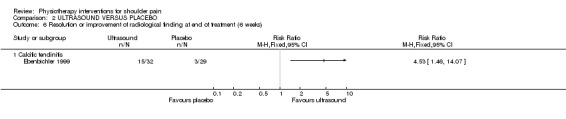
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 6 Resolution or improvement of radiological finding at end of treatment (6 weeks).
2.7. Analysis.
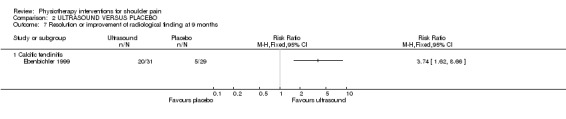
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 7 Resolution or improvement of radiological finding at 9 months.
2.8. Analysis.
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 8 Normal function at end of treatment (6 weeks).
2.9. Analysis.
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 9 Normal function at 9 months.
2.10. Analysis.
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 10 Change in range of flexion.
2.11. Analysis.
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 11 Range of abduction.
2.12. Analysis.
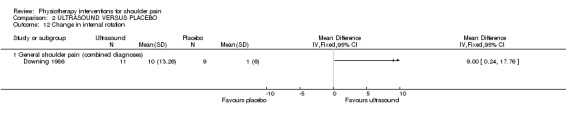
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 12 Change in internal rotation.
2.13. Analysis.
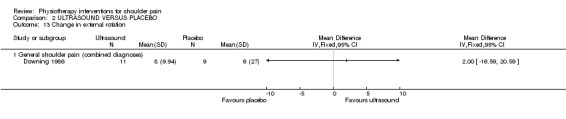
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 13 Change in external rotation.
2.14. Analysis.
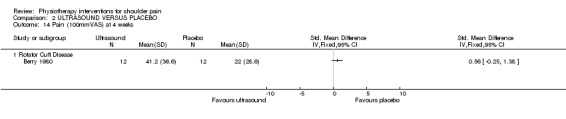
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 14 Pain (100mmVAS) at 4 weeks.
2.15. Analysis.
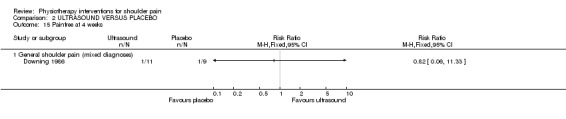
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 15 Painfree at 4 weeks.
2.16. Analysis.
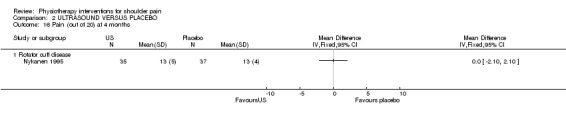
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 16 Pain (out of 20) at 4 months.
2.17. Analysis.

Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 17 Pain (out of 20) at 12 months.
2.18. Analysis.
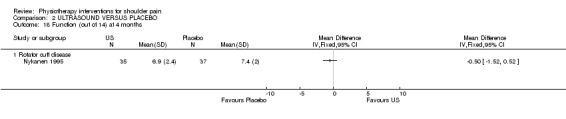
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 18 Function (out of 14) at 4 months.
2.19. Analysis.
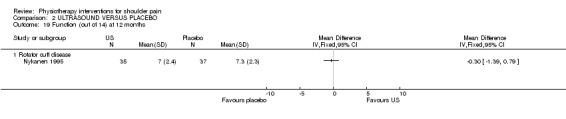
Comparison 2 ULTRASOUND VERSUS PLACEBO, Outcome 19 Function (out of 14) at 12 months.
Comparison 3. SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Good or excellent function (Neer score) at 2 and a half years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Rotator cuff disease | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 No pain on activity at 2 and a half years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 rotator cuff disease | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 No pain at rest at 2 and a half years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 rotator cuff disease | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 No pain at night at two and a half years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 rotator cuff disease | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Substantial improvement or recovered post treatment (1 month). Participant rated | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 No pain post treatment (1 month) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Good or excellent function post treatment (1 month) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Worsened range of abduction post treatment (1 month) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.
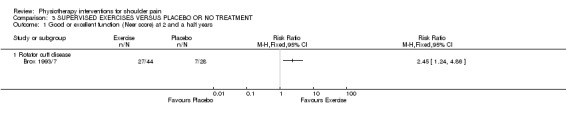
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 1 Good or excellent function (Neer score) at 2 and a half years.
3.2. Analysis.
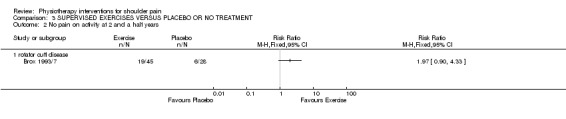
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 2 No pain on activity at 2 and a half years.
3.3. Analysis.
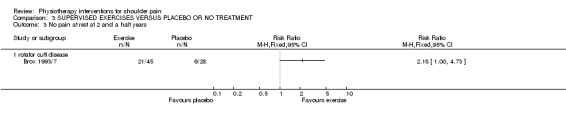
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 3 No pain at rest at 2 and a half years.
3.4. Analysis.
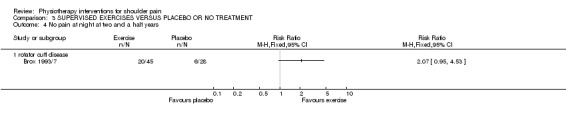
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 4 No pain at night at two and a half years.
3.5. Analysis.
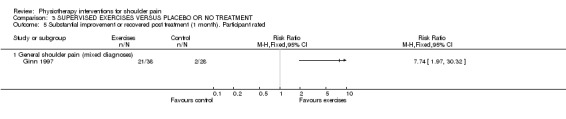
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 5 Substantial improvement or recovered post treatment (1 month). Participant rated.
3.6. Analysis.
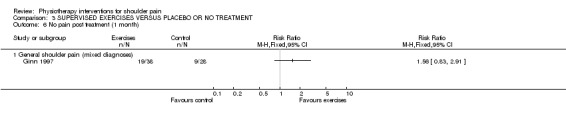
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 6 No pain post treatment (1 month).
3.7. Analysis.
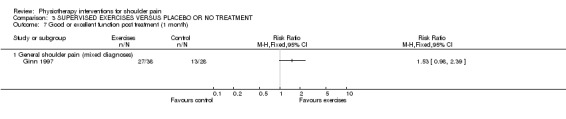
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 7 Good or excellent function post treatment (1 month).
3.8. Analysis.
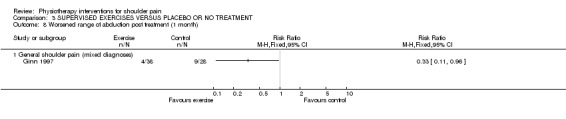
Comparison 3 SUPERVISED EXERCISES VERSUS PLACEBO OR NO TREATMENT, Outcome 8 Worsened range of abduction post treatment (1 month).
Comparison 4. LASER VERSUS PLACEBO.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Excellent or good result | 2 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.71 [1.89, 7.28] |
| 1.1 Periarthritis (adhesive capsulitis) | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.0 [2.11, 30.34] |
| 1.2 Supraspinatus tendinitis | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.98, 4.09] |
| 2 Change in Range of Movement at four weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐10.8 [‐40.76, 19.16] |
| 2.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐10.8 [‐40.76, 19.16] |
| 3 Change in night pain at four weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐1.06, 3.66] |
| 3.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐1.06, 3.66] |
| 4 Change in pain at rest at four weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐0.86, 2.46] |
| 4.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐0.86, 2.46] |
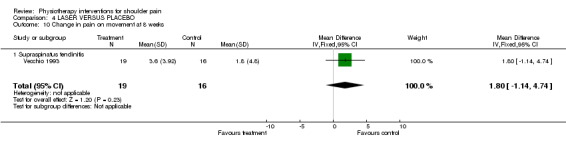
| 5 Change in pain on movement at four weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.50 [‐1.01, 4.01] |
| 5.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.50 [‐1.01, 4.01] |
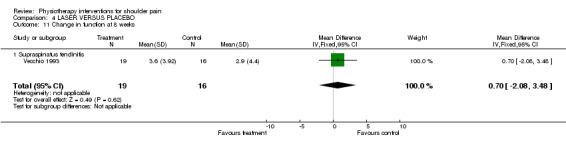
| 6 Change in function at four weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐1.06, 2.86] |
| 6.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐1.06, 2.86] |
| 7 Change in range of movement at 8 weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐25.2 [‐66.36, 15.96] |
| 7.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐25.2 [‐66.36, 15.96] |
| 8 Change in night pain at 8 weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐1.74, 4.14] |
| 8.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐1.74, 4.14] |
| 9 Change in pain at rest at 8 weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.7 [‐0.69, 4.09] |
| 9.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.7 [‐0.69, 4.09] |
| 10 Change in pain on movement at 8 weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.8 [‐1.14, 4.74] |
| 10.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.8 [‐1.14, 4.74] |
| 11 Change in function at 8 weeks | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐2.08, 3.48] |
| 11.1 Supraspinatus tendinitis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐2.08, 3.48] |
4.1. Analysis.
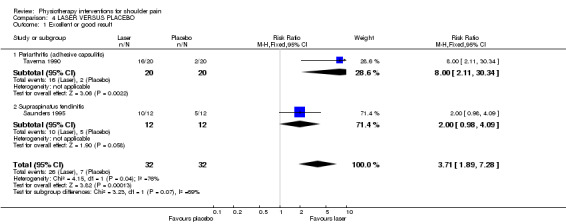
Comparison 4 LASER VERSUS PLACEBO, Outcome 1 Excellent or good result.
4.2. Analysis.
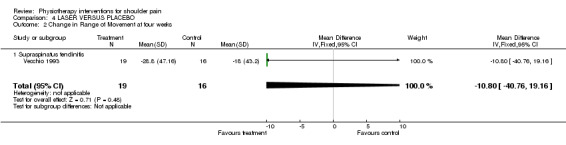
Comparison 4 LASER VERSUS PLACEBO, Outcome 2 Change in Range of Movement at four weeks.
4.3. Analysis.
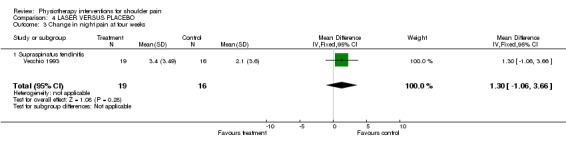
Comparison 4 LASER VERSUS PLACEBO, Outcome 3 Change in night pain at four weeks.
4.4. Analysis.
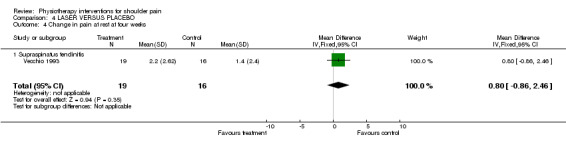
Comparison 4 LASER VERSUS PLACEBO, Outcome 4 Change in pain at rest at four weeks.
4.5. Analysis.
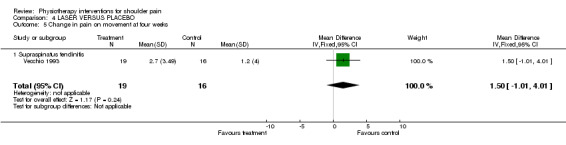
Comparison 4 LASER VERSUS PLACEBO, Outcome 5 Change in pain on movement at four weeks.
4.6. Analysis.
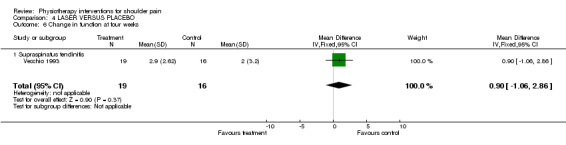
Comparison 4 LASER VERSUS PLACEBO, Outcome 6 Change in function at four weeks.
4.7. Analysis.
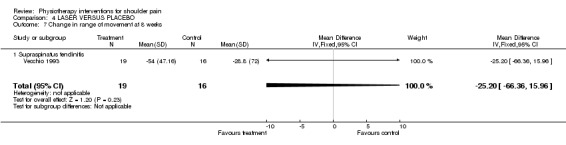
Comparison 4 LASER VERSUS PLACEBO, Outcome 7 Change in range of movement at 8 weeks.
4.8. Analysis.
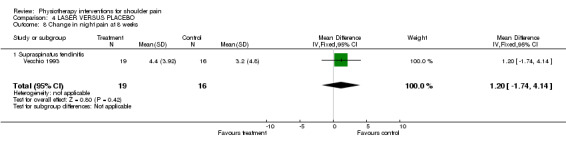
Comparison 4 LASER VERSUS PLACEBO, Outcome 8 Change in night pain at 8 weeks.
4.9. Analysis.
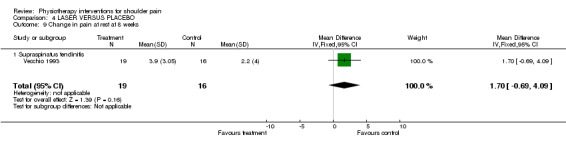
Comparison 4 LASER VERSUS PLACEBO, Outcome 9 Change in pain at rest at 8 weeks.
4.10. Analysis.
Comparison 4 LASER VERSUS PLACEBO, Outcome 10 Change in pain on movement at 8 weeks.
4.11. Analysis.
Comparison 4 LASER VERSUS PLACEBO, Outcome 11 Change in function at 8 weeks.
Comparison 5. PULSED ELECTROMAGNETIC FIELD VERSUS PLACEBO.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 No pain at end of treatment (6 days) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Calcific tendinitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 No pain at 4‐6 Weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Calcific tendinitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Adverse effects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Post treatment pain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Anxiety/ claustrophobia | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Headache | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Insomnia | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
5.1. Analysis.
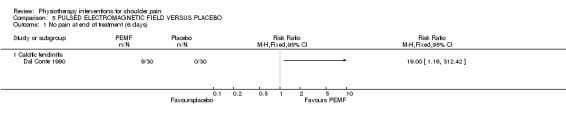
Comparison 5 PULSED ELECTROMAGNETIC FIELD VERSUS PLACEBO, Outcome 1 No pain at end of treatment (6 days).
5.2. Analysis.
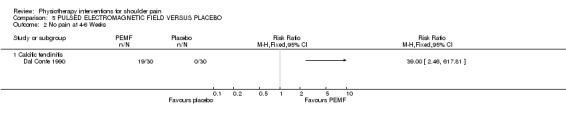
Comparison 5 PULSED ELECTROMAGNETIC FIELD VERSUS PLACEBO, Outcome 2 No pain at 4‐6 Weeks.
5.3. Analysis.
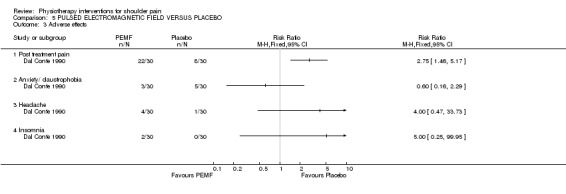
Comparison 5 PULSED ELECTROMAGNETIC FIELD VERSUS PLACEBO, Outcome 3 Adverse effects.
Comparison 6. IONTOPHORESIS WITH ACETIC ACID PLUS ULTRASOUND VERSUS NO TREATMENT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Percent change in size of calcium deposit | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Calcific tendinitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Percent improvement in abduction | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Calcific tendinitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
6.1. Analysis.
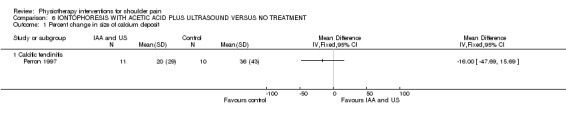
Comparison 6 IONTOPHORESIS WITH ACETIC ACID PLUS ULTRASOUND VERSUS NO TREATMENT, Outcome 1 Percent change in size of calcium deposit.
6.2. Analysis.
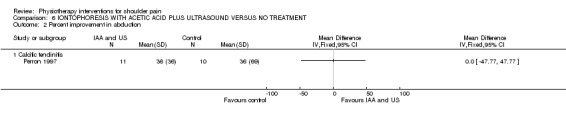
Comparison 6 IONTOPHORESIS WITH ACETIC ACID PLUS ULTRASOUND VERSUS NO TREATMENT, Outcome 2 Percent improvement in abduction.
Comparison 7. BIPOLAR INTERFERENTIAL CURRENT VERSUS ULTRASOUND.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recovery or substantial improvement (participant rated) at 6 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Recovery or substantial improvement (participant rated) at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Recovery or substantial improvement (participant rated) at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Recovery or substantial improvement (participant rated) at 9 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Recovery or substantial improvement (participant rated) at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
7.1. Analysis.
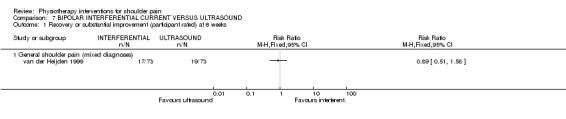
Comparison 7 BIPOLAR INTERFERENTIAL CURRENT VERSUS ULTRASOUND, Outcome 1 Recovery or substantial improvement (participant rated) at 6 weeks.
7.2. Analysis.
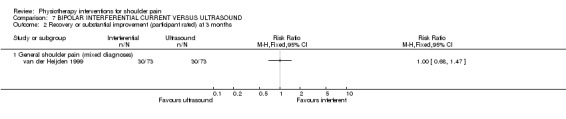
Comparison 7 BIPOLAR INTERFERENTIAL CURRENT VERSUS ULTRASOUND, Outcome 2 Recovery or substantial improvement (participant rated) at 3 months.
7.3. Analysis.
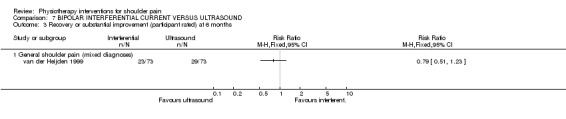
Comparison 7 BIPOLAR INTERFERENTIAL CURRENT VERSUS ULTRASOUND, Outcome 3 Recovery or substantial improvement (participant rated) at 6 months.
7.4. Analysis.
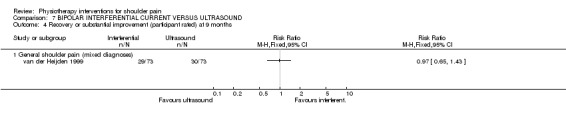
Comparison 7 BIPOLAR INTERFERENTIAL CURRENT VERSUS ULTRASOUND, Outcome 4 Recovery or substantial improvement (participant rated) at 9 months.
7.5. Analysis.
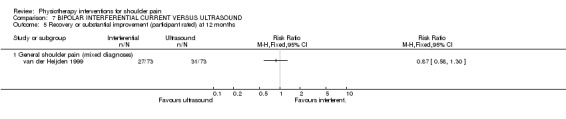
Comparison 7 BIPOLAR INTERFERENTIAL CURRENT VERSUS ULTRASOUND, Outcome 5 Recovery or substantial improvement (participant rated) at 12 months.
Comparison 8. TENS VERSUS ULTRASOUND.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain on VAS | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 General shoulder pain (mixed diagnoses) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
8.1. Analysis.
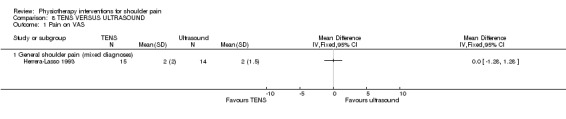
Comparison 8 TENS VERSUS ULTRASOUND, Outcome 1 Pain on VAS.
Comparison 9. MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Range of internal rotation at 3 to 4 weeks | 2 | 34 | Mean Difference (IV, Fixed, 95% CI) | 4.61 [‐0.99, 10.21] |
| 1.1 adhesive capsulitis | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 6.08 [0.06, 12.10] |
| 1.2 rotator cuff impingement | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | ‐4.71 [‐19.89, 10.47] |
| 2 Range of abduction at 3 to 4 weeks | 2 | 34 | Mean Difference (IV, Fixed, 95% CI) | 2.10 [‐10.03, 14.22] |
| 2.1 adhesive capsulitis | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 4.4 [‐9.02, 17.82] |
| 2.2 rotator cuff impingement | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | ‐8.15 [‐36.46, 20.16] |
| 3 Pain at 3 to 4 weeks | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 adhesive capsulitis (pain 10 cm VAS) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐2.20 [‐6.13, 1.73] |
| 3.2 rotator cuff impingement (pain composite several 100 mm scales) | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐186.23 [‐319.33, ‐53.13] |
| 3.3 rotator cuff impingement (mm on VAS) | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | ‐32.07 [‐58.04, ‐6.10] |
| 4 Range of passive abduction at 4 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Composite strength score at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 rotator cuff impingement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Function at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 rotator cuff impingement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain on subacromial compression (mm on VAS) at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 rotator cuff impingement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Range of elevation (degrees) at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 rotator cuff impingement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Range of external rotation (degrees) at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 rotator cuff impingement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
9.1. Analysis.
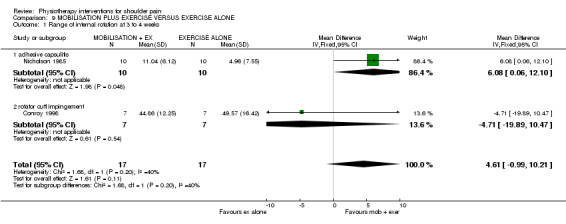
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 1 Range of internal rotation at 3 to 4 weeks.
9.2. Analysis.
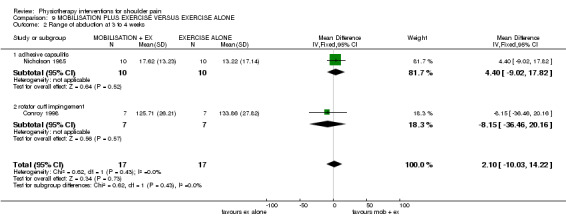
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 2 Range of abduction at 3 to 4 weeks.
9.3. Analysis.
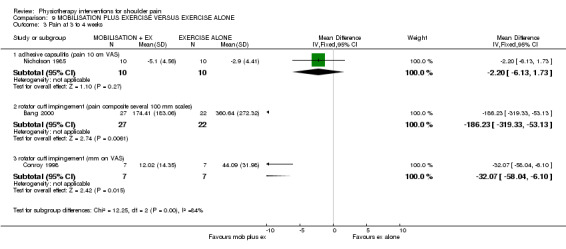
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 3 Pain at 3 to 4 weeks.
9.4. Analysis.
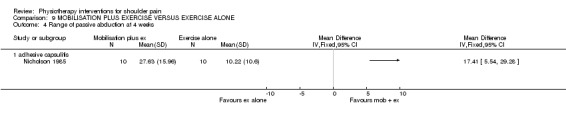
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 4 Range of passive abduction at 4 weeks.
9.5. Analysis.
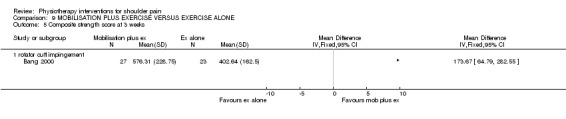
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 5 Composite strength score at 3 weeks.
9.6. Analysis.
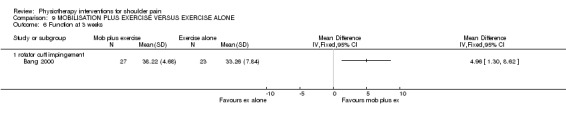
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 6 Function at 3 weeks.
9.7. Analysis.
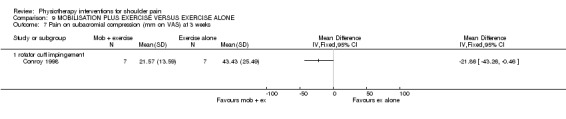
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 7 Pain on subacromial compression (mm on VAS) at 3 weeks.
9.8. Analysis.
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 8 Range of elevation (degrees) at 3 weeks.
9.9. Analysis.
Comparison 9 MOBILISATION PLUS EXERCISE VERSUS EXERCISE ALONE, Outcome 9 Range of external rotation (degrees) at 3 weeks.
Comparison 10. MOBLISATION/ MANIPULATION VERSUS EXERCISES AND ELECTROTHERAPY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain at end of intervention period | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 General shoulder pain (mixed diagnoses or no diagnosis given) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 "Cured" at 5 weeks (participant rated) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 "Not cured" (participant rated) at 2 and a half years (in those followed up) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
10.1. Analysis.
Comparison 10 MOBLISATION/ MANIPULATION VERSUS EXERCISES AND ELECTROTHERAPY, Outcome 1 Pain at end of intervention period.
10.2. Analysis.
Comparison 10 MOBLISATION/ MANIPULATION VERSUS EXERCISES AND ELECTROTHERAPY, Outcome 2 "Cured" at 5 weeks (participant rated).
10.3. Analysis.
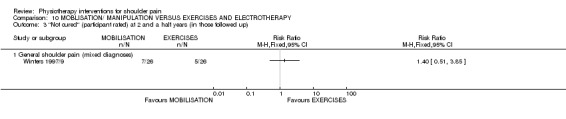
Comparison 10 MOBLISATION/ MANIPULATION VERSUS EXERCISES AND ELECTROTHERAPY, Outcome 3 "Not cured" (participant rated) at 2 and a half years (in those followed up).
Comparison 11. ISOKINETIC RESISTANCE EXERCISES VERSUS ELECTROMYOGRAPHIC BIOFEEDBACK.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 No functional limitation at work at 8 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Anterior instability | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 No functional limitation at work at 26 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Anterior instability | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 No functional limitation at work at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Anterior instability | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 No functional limitation at in sport at 8 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Anterior instability | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 No functional limitation in sport at 26 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Anterior instability | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 No functional limitation in sport at 1 year | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 Anterior instability | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
11.1. Analysis.
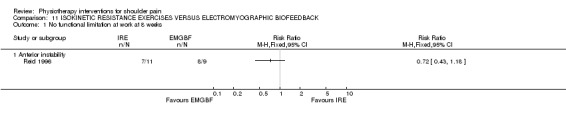
Comparison 11 ISOKINETIC RESISTANCE EXERCISES VERSUS ELECTROMYOGRAPHIC BIOFEEDBACK, Outcome 1 No functional limitation at work at 8 weeks.
11.2. Analysis.
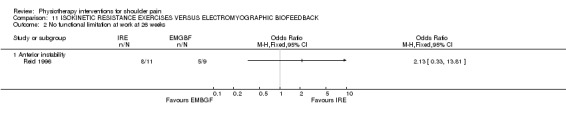
Comparison 11 ISOKINETIC RESISTANCE EXERCISES VERSUS ELECTROMYOGRAPHIC BIOFEEDBACK, Outcome 2 No functional limitation at work at 26 weeks.
11.3. Analysis.
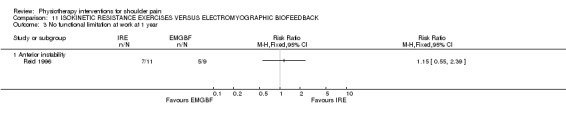
Comparison 11 ISOKINETIC RESISTANCE EXERCISES VERSUS ELECTROMYOGRAPHIC BIOFEEDBACK, Outcome 3 No functional limitation at work at 1 year.
11.4. Analysis.
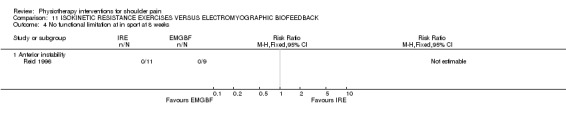
Comparison 11 ISOKINETIC RESISTANCE EXERCISES VERSUS ELECTROMYOGRAPHIC BIOFEEDBACK, Outcome 4 No functional limitation at in sport at 8 weeks.
11.5. Analysis.
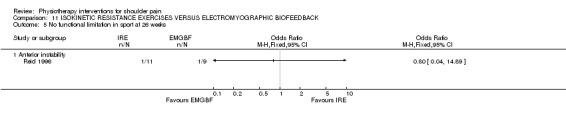
Comparison 11 ISOKINETIC RESISTANCE EXERCISES VERSUS ELECTROMYOGRAPHIC BIOFEEDBACK, Outcome 5 No functional limitation in sport at 26 weeks.
11.6. Analysis.
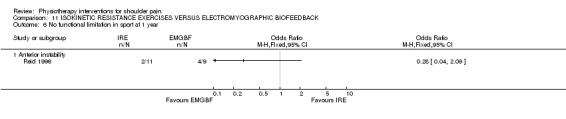
Comparison 11 ISOKINETIC RESISTANCE EXERCISES VERSUS ELECTROMYOGRAPHIC BIOFEEDBACK, Outcome 6 No functional limitation in sport at 1 year.
Comparison 12. PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Range of shoulder flexion at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Range of shoulder abduction at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Range of shoulder external rotation at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of shoulder internal rotation at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pain at rest at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Pain on movement at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain on lying at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
12.1. Analysis.
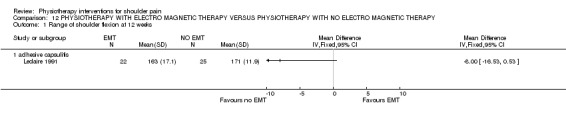
Comparison 12 PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY, Outcome 1 Range of shoulder flexion at 12 weeks.
12.2. Analysis.
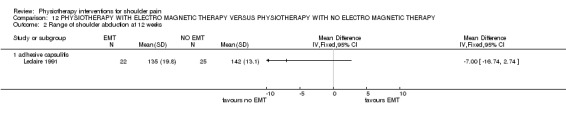
Comparison 12 PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY, Outcome 2 Range of shoulder abduction at 12 weeks.
12.3. Analysis.
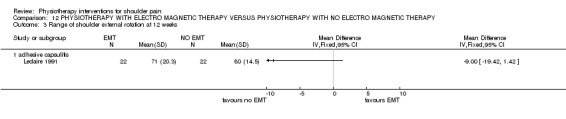
Comparison 12 PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY, Outcome 3 Range of shoulder external rotation at 12 weeks.
12.4. Analysis.
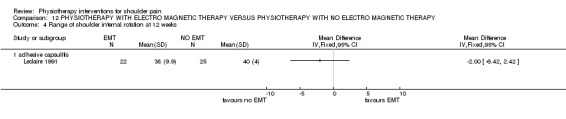
Comparison 12 PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY, Outcome 4 Range of shoulder internal rotation at 12 weeks.
12.5. Analysis.
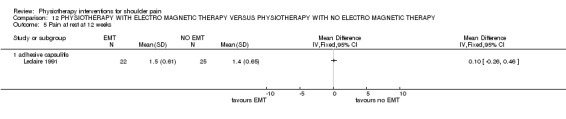
Comparison 12 PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY, Outcome 5 Pain at rest at 12 weeks.
12.6. Analysis.
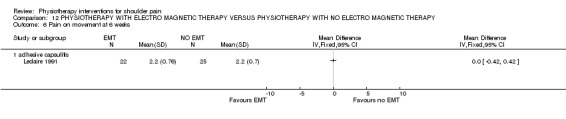
Comparison 12 PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY, Outcome 6 Pain on movement at 6 weeks.
12.7. Analysis.
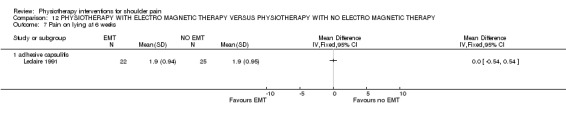
Comparison 12 PHYSIOTHERAPY WITH ELECTRO MAGNETIC THERAPY VERSUS PHYSIOTHERAPY WITH NO ELECTRO MAGNETIC THERAPY, Outcome 7 Pain on lying at 6 weeks.
Comparison 13. INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Improvement in severity of main complaint at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Improvement in severity of main complaint at 7 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Improvement in severity of main complaint at 13 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Improvement in severity of main complaint at 26 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Improvement in severity of main complaint at 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Pain at 2‐3 weeks (100cm VAS) | 2 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐12.18 [‐18.61, ‐5.75] |
| 6.1 Adhesive capsulitis | 1 | 109 | Mean Difference (IV, Fixed, 95% CI) | ‐10.00 [‐18.67, ‐5.33] |
| 6.2 Rotator cuff disease | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐14.60 [‐38.91, 9.71] |
| 7 Improvement in severity of day pain at 7 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Improvement in severity of day pain at 13 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Improvement in severity of day pain at 26 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Improvement in severity of day pain at 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Improvement in severity of night pain at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Improvement in severity of night pain at 7 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Improvement in severity of night pain at 13 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Improvement in severity of night pain at 26 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Improvement in severity of night pain at 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Improvement in severity as rated by observer at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Improvement in severity as rated by observer at 7 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Improvement in severity as rated by observer at 26 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Improvement in rating of shoulder disability at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Improvement in rating of shoulder disability at 7 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Improvement in rating of shoulder disability at 13 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 21.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Improvement in rating of shoulder disability at 26 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 22.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Improvement in rating of shoulder disability at 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Range of abduction (degrees) at 2‐3 weeks | 2 | 133 | Mean Difference (IV, Fixed, 95% CI) | 5.0 [0.36, 9.64] |
| 24.1 Adhesive capsulitis | 1 | 109 | Mean Difference (IV, Fixed, 95% CI) | 5.0 [0.31, 9.69] |
| 24.2 Rotator cuff disease | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 5.0 [‐24.93, 34.93] |
| 25 Improvement in degree of restriction of ROM of abduction at 7 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Improvement in degree of restriction of ROM of abduction at 26 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 Improvement in degree of restriction of ROM of ER at 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 27.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28 Improvement in degree of restriction of ROM of ER at 7 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 28.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29 Improvement in degree of restriction of ROM of ER at 26 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 29.1 Adhesive capsulitis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 30 Number needing additional treatment at 7 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 30.1 Adhesive capsulitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31 Frequency of adverse reactions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 31.1 pain after treatment > 2 days | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.2 facial flushing | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.3 irregular menstrual bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.4 fever | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.5 skin irritation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.6 overall | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32 Short term treatment success | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 32.1 Rotator cuff disease | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
13.1. Analysis.
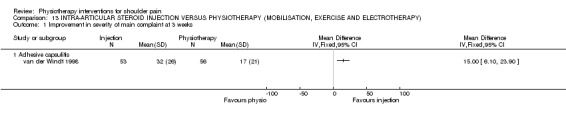
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 1 Improvement in severity of main complaint at 3 weeks.
13.2. Analysis.
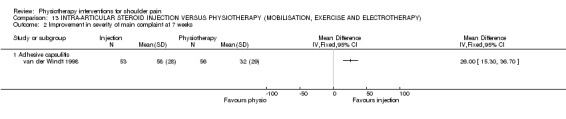
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 2 Improvement in severity of main complaint at 7 weeks.
13.3. Analysis.
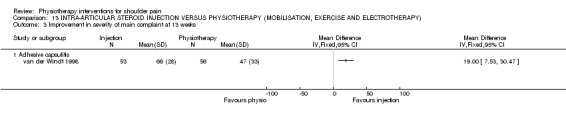
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 3 Improvement in severity of main complaint at 13 weeks.
13.4. Analysis.
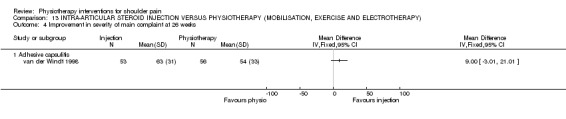
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 4 Improvement in severity of main complaint at 26 weeks.
13.5. Analysis.
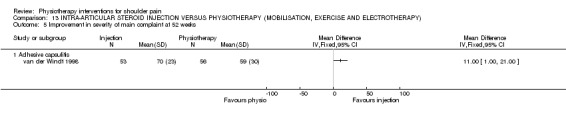
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 5 Improvement in severity of main complaint at 52 weeks.
13.6. Analysis.
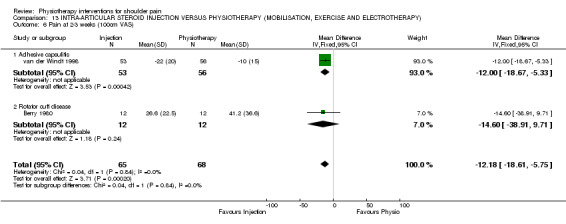
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 6 Pain at 2‐3 weeks (100cm VAS).
13.7. Analysis.
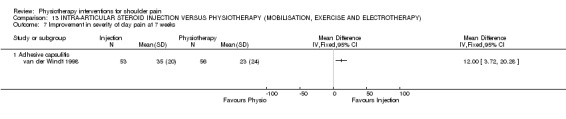
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 7 Improvement in severity of day pain at 7 weeks.
13.8. Analysis.

Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 8 Improvement in severity of day pain at 13 weeks.
13.9. Analysis.
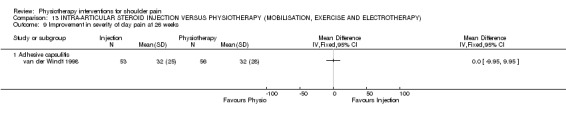
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 9 Improvement in severity of day pain at 26 weeks.
13.10. Analysis.
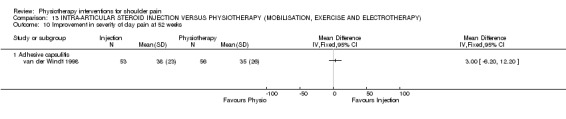
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 10 Improvement in severity of day pain at 52 weeks.
13.11. Analysis.
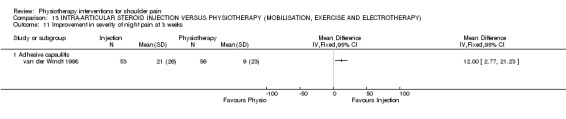
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 11 Improvement in severity of night pain at 3 weeks.
13.12. Analysis.
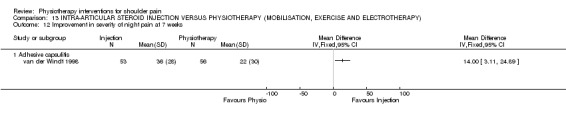
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 12 Improvement in severity of night pain at 7 weeks.
13.13. Analysis.
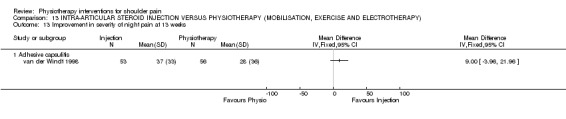
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 13 Improvement in severity of night pain at 13 weeks.
13.14. Analysis.
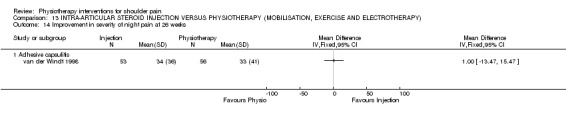
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 14 Improvement in severity of night pain at 26 weeks.
13.15. Analysis.
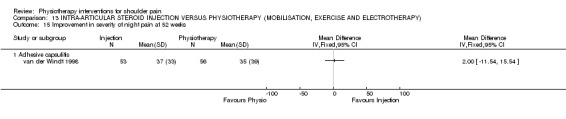
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 15 Improvement in severity of night pain at 52 weeks.
13.16. Analysis.
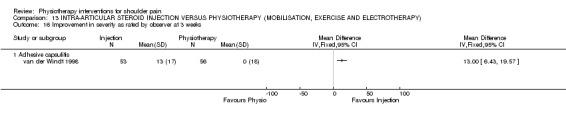
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 16 Improvement in severity as rated by observer at 3 weeks.
13.17. Analysis.
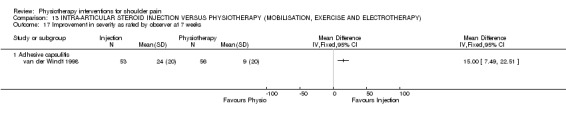
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 17 Improvement in severity as rated by observer at 7 weeks.
13.18. Analysis.
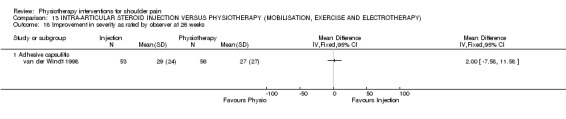
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 18 Improvement in severity as rated by observer at 26 weeks.
13.19. Analysis.
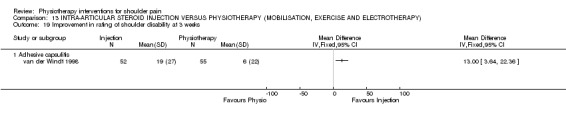
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 19 Improvement in rating of shoulder disability at 3 weeks.
13.20. Analysis.
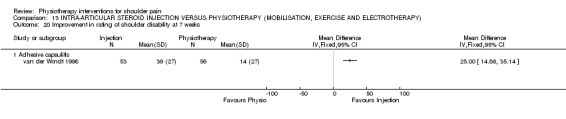
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 20 Improvement in rating of shoulder disability at 7 weeks.
13.21. Analysis.
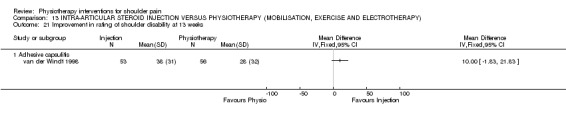
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 21 Improvement in rating of shoulder disability at 13 weeks.
13.22. Analysis.
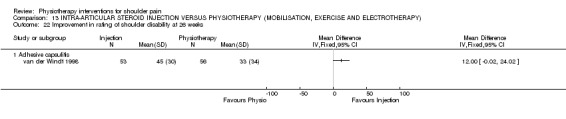
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 22 Improvement in rating of shoulder disability at 26 weeks.
13.23. Analysis.
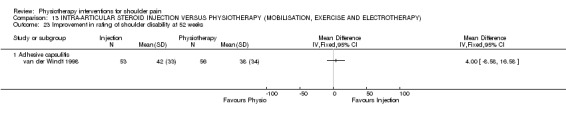
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 23 Improvement in rating of shoulder disability at 52 weeks.
13.24. Analysis.
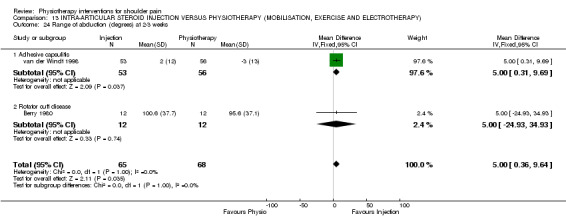
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 24 Range of abduction (degrees) at 2‐3 weeks.
13.25. Analysis.
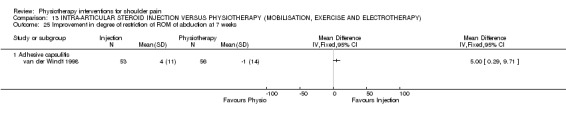
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 25 Improvement in degree of restriction of ROM of abduction at 7 weeks.
13.26. Analysis.
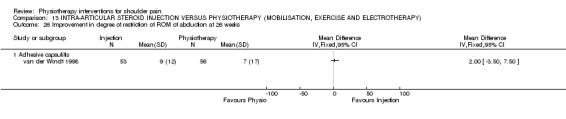
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 26 Improvement in degree of restriction of ROM of abduction at 26 weeks.
13.27. Analysis.
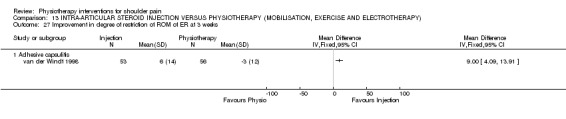
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 27 Improvement in degree of restriction of ROM of ER at 3 weeks.
13.28. Analysis.
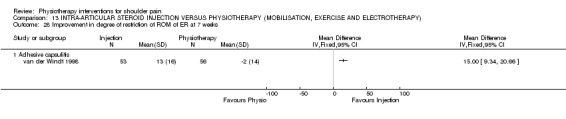
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 28 Improvement in degree of restriction of ROM of ER at 7 weeks.
13.29. Analysis.
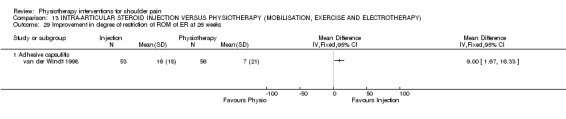
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 29 Improvement in degree of restriction of ROM of ER at 26 weeks.
13.30. Analysis.
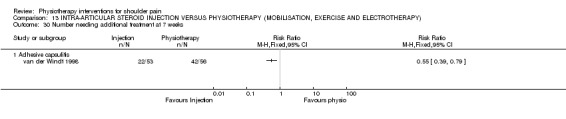
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 30 Number needing additional treatment at 7 weeks.
13.31. Analysis.
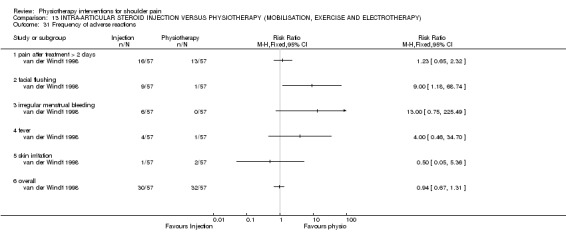
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 31 Frequency of adverse reactions.
13.32. Analysis.
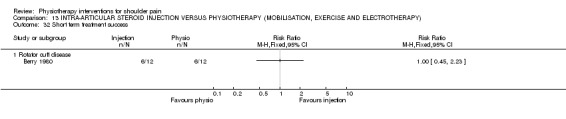
Comparison 13 INTRA‐ARTICULAR STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION, EXERCISE AND ELECTROTHERAPY), Outcome 32 Short term treatment success.
Comparison 14. INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (EXERCISES AND ELECTROTHERAPY).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain at end of intervention period | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 General shoulder pain (mixed diagnoses) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 "Cured" at 5 weeks (participant rated) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 "Not cured" (participant rated) at 2 and a half years (in those followed up) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
14.1. Analysis.
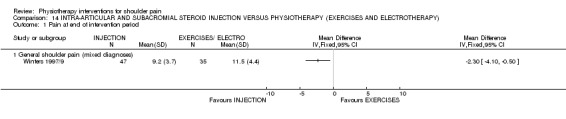
Comparison 14 INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (EXERCISES AND ELECTROTHERAPY), Outcome 1 Pain at end of intervention period.
14.2. Analysis.
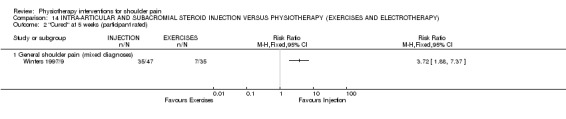
Comparison 14 INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (EXERCISES AND ELECTROTHERAPY), Outcome 2 "Cured" at 5 weeks (participant rated).
14.3. Analysis.
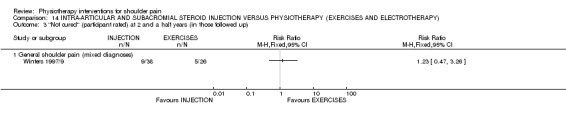
Comparison 14 INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (EXERCISES AND ELECTROTHERAPY), Outcome 3 "Not cured" (participant rated) at 2 and a half years (in those followed up).
Comparison 15. INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION AND MANIPULATION).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain at end of intervention period | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 General shoulder pain (mixed diagnoses) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 "Cured" at 5 weeks (participant rated) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 "Not cured" (participant rated) at 2 and a half years (in those followed up) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 General shoulder pain (mixed diagnoses) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
15.1. Analysis.
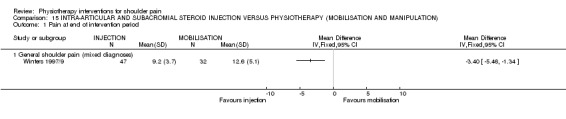
Comparison 15 INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION AND MANIPULATION), Outcome 1 Pain at end of intervention period.
15.2. Analysis.
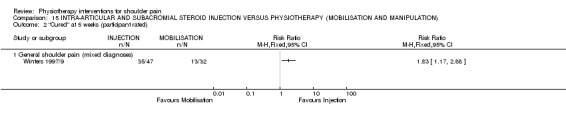
Comparison 15 INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION AND MANIPULATION), Outcome 2 "Cured" at 5 weeks (participant rated).
15.3. Analysis.
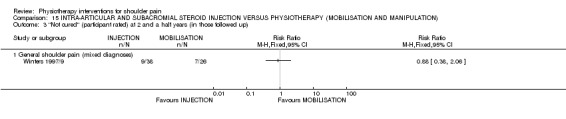
Comparison 15 INTRA‐ARTICULAR AND SUBACROMIAL STEROID INJECTION VERSUS PHYSIOTHERAPY (MOBILISATION AND MANIPULATION), Outcome 3 "Not cured" (participant rated) at 2 and a half years (in those followed up).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bang 2000.
| Methods | Random allocation: Yes;Concealed allocation: No;Baseline comparability: Yes;Blind assessors: Yes;Blind subjects: No;Blind therapists: No;Adequate follow‐up: Yes;Intention‐to‐treat analysis: No;Between‐group comparisons: Yes;Point estimates & variability: Yes;Eligibility criteria: Yes | |
| Participants | 52 participants (mean age treatment group 42, range 27‐65; mean age control group 45, range 24‐60) diagnosed with impingement syndrome | |
| Interventions | Both groups attended for 6 physiotherapy sessions over 3 weeksGroup 1: supervised flexibility and strength exercisesGroup 2: exercises as above plus mobilisation | |
| Outcomes | Assessed at 3 weeks and 2 months1. Isometric strength2. Pain on movement and resistance3. Function (questionnaire) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Berry 1980.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates and variability: Yes; Eligibility criteria: Yes | |
| Participants | 60 outpatients (mean age acupuncture group 52.3; mean age steroid plus placebo 54.1; mean age steroid plus tolmentin 51.2; mean age physiotherapy 55.1; mean age placebo 56.2) (with an uncomplicated rotator‐cuff lesion defined as pain on resisted movements of the shoulder with or without some loss of passive movement, mainly abduction | |
| Interventions | Four weeks of: Group 1: Acupuncture for 20 minutes weekly, using classical Chinese acupuncture with moxibustion Group 2: Steroid injection of 40 mg methylprednisolone with 2 ml 2% lignocaine using anterior appraoch to the shoulder joint plus placebo tolmentin (2 tablets 3 times daily) Group 3: Steroid injection plus active tolmetin sodium (a non steroidal anti‐inflamtory drug) (400 mg 3 times daily) Group 4: Physiotherapy of standardised ultrasound for 10 minutes for eight sessions Group 5: Placebo tolmetin plus placebo ultrasound | |
| Outcomes | Assessed at start of study and at 2 and 4 weeks on: 1. Pain measured by visual analogue scale and 4 point scale (none, mild, moderate, servere pain); 2. Active total shoulder abduction using a goniometer; 3. Comparative assessment by patient and assessor (much better, better, same, worse, much worse); 5. Success or failure of the treatment at the end of four weeks, defined as need for steroid injection; 6. Adverse outcomes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Binder 1984.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: No; Blind assessors: Yes; Blind subjects: Yes; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: No; Eligibility criteria: No | |
| Participants | 29 participants (mean age treatment group 54.4; mean age control group 53.2). Shoulder pain on resisted Abduction and ER, excluded "frozen shoulder" and cuff tears | |
| Interventions | Phase 1. Active treatment vs. placebo for 4 weeks.Phase 2. Without unblinding, all participants received active treatment for 4 weeks.Phase 3. 8 weeks of no active treatment Group 1: Pulsed electromagnetic field 4 weeks daily treatment (self administered).Group 2: Placebo | |
| Outcomes | Assessed at 4, 8 and 16 weeks.1. Pain VAS.2. Total range of active movement.3. Pain of resisted abduction, internal and external rotation (VAS).4. Painful arc on abduction. | |
| Notes | Met inclusion criteria of the review but did not report means, standard deviations, nor the means from which to calculate it (data presented graphically), and hence not included in meta analysis. In addition, placebo group all given active intervention at 4 weeks therefore longer term outcomes are not between group comparisons. The authors have been contacted in attempt to obtain 4 week data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Brox 1993/7.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: No; Intention‐to‐treat analysis: Yes; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: No | |
| Participants | 125 patients with pain in shoulder for at least 3 months. Pain resistant to physiotherapy and NSAIDS. Positive impingement test. | |
| Interventions | Group 1: Arthroscopic subacromial decompression.Group 2: 3 to 6 months of supervised low resistance exercises repeated many times. Group 3: Detuned (i.e. Placebo) laser. | |
| Outcomes | Assessed at 3 months, 6 months and 2.5 years.Success defined as a Neer shoulder score of >80. | |
| Notes | 3 and 6 month data given as medians with no ranges. Presented in additional tables. 2 and 1/2 year data as dicotomous data therefore in meta‐analysis and additional tables | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Bulgen 1984.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: No; Blind assessors: No;Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: No; Eligibility criteria: No | |
| Participants | 42 participants (mean age 55.8, range 44‐74) with "frozen shoulder"1.Pain in shoulder2.Night pain3.Inability to the affected side.4.Restriction of active and passive movements.5.Restriction of ER to at least 50%. | |
| Interventions | Group 1: intra‐articular steroid injection Group 2: mobilisation Group 3: ice therapyGroup 4: no treatment | |
| Outcomes | Assessed immediately post treatment and 8 months1.Pain: night pain, pain on movement, rest pain during the day (10cm VAS, and verbally "better", "worse", "the same").2.Passive movements: ER, total rotation, flexion, abduction, HBB (measured to the nearest 5°).3.Number of analgesics | |
| Notes | Met inclusion criteria for review, however no data reported to enable inclusion in meta‐analysis or additional tables. Authors contacted. Also authors noted that patients had difficulty using the visual analogue scales so relied on verbal reports of progress as they appeared more consistent and relaible. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Conroy 1998.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 14 participants with primary shoulder impingement syndrome. | |
| Interventions | Three treatments a week for 3 weeks.Group 1: Shoulder joint mobilisation and comprehensive treatment (hot packs, Active ROM, stretching, strengthening, soft tissue mobilisation, education). 3 times per week for 3 weeks.Group 2: Comprehensive treatment alone | |
| Outcomes | Measured at end of treatment course (3 weeks)1. 24 hour pain2. Pain on subacromial compression (VAS), 3. Mobility4. Function. | |
| Notes | Heat (hot packs) constant across both groups therefore analysed with studies of mobilisation plus exercise versus exercise alone | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Dacre1989.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: No; Point estimates & variability: No; Eligibility criteria: Yes | |
| Participants | 62 participants (mean age treatment group 58.8) 1.Pain and stiffness2.Restriction of movement3.Loss of full function4.Pain at night with inability to lie on the affected side. | |
| Interventions | Group 1: Four to six weeks of "physiotherapy thought most appropriate", performed by one therapist and mainly comprised of mobilisation.Group 2: Local steroid injections of 20,g triamcinolone with 1ml 2% lidocaine injected anteriorly around the shoulder joint by 1 physician.Group 3: Both physiotherapy and injection, as above. | |
| Outcomes | Assessed at baseline, 6 weeks & 6 months1.Day pain, night pain, pain on active movement and pain on passive movement (all assessed on individual 10cm visual analogue scales).2.Range of passive movement of abduction, external rotation and hand behind back.3.Treatment costs. | |
| Notes | While included in the review, data presented with no quantitative between group comparisons, and no measure of variance, hence not included in meta‐analysis. The authors have been contacted in an attempt to access their data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Dal Conte 1990.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: No; Blind subjects: Yes; Blind therapists: Yes; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: No; Eligibility criteria: Yes | |
| Participants | 60 participants with symptomatic unilateral calcific tendinitis of at least 3 months duration | |
| Interventions | Group 1: pulsed magnetic field 30 minutes a day for 6 consecutive daysGroup 2: sham PMF of the same time and number of treatments | |
| Outcomes | Assessed at 3 and 6 days, and 6 weeks.1. Pain (spontaneous and provoked)2. Range of motion | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Downing 1986.
| Methods | Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind assessors: No; Blind subjects: Yes; Blind therapists: Yes; Adequate follow‐up: No; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: No | |
| Participants | 20 participants (mean age 53, range 28‐75) with shoulder pain and limitation of movement for > 1 month and < 1 year.Pain on at least 1 activity and at end of range of at least one movement. Loss of range > 10° in at least 1 movement. | |
| Interventions | Group 1: Maximum tolerated dosage of ultrasound (mean 1.3 watts/cm squared 6 minutes, 3 times a week for 3 weeks.Group 2: Sham ultrasound at same frequency for three weeks | |
| Outcomes | Assessed at 0 and 3 weeks.1.Active and passive flexion, abduction and external rotation. 2.Pain on a descriptive scale3. Function4. Overall improvement (patient reported) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Ebenbichler 1999.
| Methods | Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: Yes; Blind therapists: Yes; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 54 participants (mean age treatment group 49; mean age control group 54) (61 shoulders) Radiographically verified calcific tendinitis.Mild‐mod pain for >4 weeks or restricted ROM | |
| Interventions | 24 treatment sessions (first 15 were daily then last 9 were 5 times weekly)Group 1: Ultrasound therapy (15 mins, .89MHz, 2.5w cm², pulsed 1:4, transducer size 5 cm²Group 2: Sham ultrasound | |
| Outcomes | Assessed following treatment course and at 9 months1. Assessment of change from baseline in calcium deposits on radiography2. 100 point Constant score (pain, AROM, strength, ADL's), 3. Pain (pain score and VAS and on abduction (4 point scale)4. QOL 10cm VAS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
England 1989.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: No; Blind assessors: Yes; Blind subjects: Yes; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 20 participants (mean age 48) with supraspinatus and biceps tendonitis, full range of passive movement with pain on resisted abduction and pain on resisted elbow flexion and supination. | |
| Interventions | Group 1:Active infrared laser therapy at 904nm 3 times a week for 2 weeks.Group 2: Placebo laser therapy at same frequency.Group 3: Naproxen sodium 550mg 2 times a day for 2 weeks. | |
| Outcomes | Outcomes (0 and 2 weeks)1.Active range of shoulder flexion, abduction and extension 2.Subjective rating of benefit with respect to pain, stiffness and function as measured on a 10cm VAS | |
| Notes | Results presented as difference between medians. Refer additional table | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Ginn 1997.
| Methods | Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 66 participants over the age of 18 (mean age 56.4; mean age control group 62.7) with unilateral shoulder pain of no specific diagnosis (i.e. mixed population). | |
| Interventions | Group 1: 1 month of physiotherapy, 4‐10 times, aimed at restoring function of shoulder muscles with a daily home exercise programme. Treatment individually determined by treating physiotherapist within the constraints of strengthening and stretching exercises as outlined on a training video. Group 2: No treatment (waiting list) | |
| Outcomes | Assessment at baseline & 1 month:1.Standardised interview and musculoskeletal assessment.2.Isometric muscle force: dynamometry.3.Pain intensity: visual analogue scale.4.ROM: measured from photographs.5.Functional impairment: 57‐point scale ‐ modified from Oswestry.6.Self‐perception of improvement: 5‐point scale. | |
| Notes | Data obtained from trial authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Herrera‐Lasso 1993.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: No; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates and variability: No; Eligibility criteria: Yes | |
| Participants | 30 participants (mean age US 56; mean age TENS 62) with bicipital or supraspinatus tendinitis, subdeltoid bursitis or periarthritis of the shoulder assessed clinically and radiologically | |
| Interventions | Group 1: Ultrasound to the glenohumeral joint for 10 minutes, 2‐5 times per week for 13 sessions, starting with 0.5W/cm squared and increasing by 0.1 W/cm squared each session to 1 W/cm squared for all subsequent sessions Group 2: Transcutaneous electrical nerve stimulation on the anterior and posterior aspects of the joint for 20 minutes for 2‐5 times per week for 13 sessions, with a mean frequency of 50Hz. All patients performed Codman (pendular) and stetching exercises and recieved superficial heat treatment | |
| Outcomes | Assessed before and after episode of treatment for: 1. range of movement (flexion and abduction) measured by standard goniomter; 2. pain on visual analogue scale | |
| Notes | Able to impute pain data from graph, but not range of motion. Authors contacted in attempt to retrieve range of motion data, awaiting response. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Leclaire 1991.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: Yes; Blind therapists: Yes; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: No | |
| Participants | 47 participants: 1.Pain 2.Limited active and passive movement >20%3.Pain on resisted abduction or rotation.4.Impaired glenohumeral joint motion. | |
| Interventions | Group 1: Electromagnetic therapy 3 times a week for 12 weeks or until complete resolution of symptoms (whichever was sooner).Group 2: Sham therapy. | |
| Outcomes | Assessed at 12 weeks1.Pain at rest, on motion and lying 2. Range of flexion, extension, abduction, adduction, ER, IR.3.Interference with daily activities.4.Adverse effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Lee 1973.
| Methods | Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: No; Blind assessors: No; Blind subjects: No; Blind therapists: No; Adequate follow‐up: No; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates and variability: No; Eligibility criteria: Yes | |
| Participants | 80 participants (mean age 58)with periarthritis of the shoulder with pain associated with limitation of passive movement of the shoulder joint | |
| Interventions | Treatment in each group lasted six weeks. Group 1: infra‐red irradiation to both anterior and posterior aspects of the shoulder region. Each exposure lasted 10 minutes. Together with a scheme of graduated active exercises according to patient's tolerance Group 2: intro‐articular injection of hydrocortisone acetate, 25 mg (anterior approach, below the coracoid process) followed by the same scheme of graduated exercises Group 3: injection of hydrocortisone acetate, 25 mg into the synovial sheath surrounding the bicipital tendon in the bicipital groove of the humerus, followed by the same scheme of graduated exercises Group 4: analgesics only | |
| Outcomes | Groups 1, 2 and 3 assessed at beginning of treatment and at weekly intervals throughout the six weeks. Group 4 was assessed at the beginning and end of the trial period. ROM only outcome assessed | |
| Notes | Composite score for range of motion graphed but no numerical data. Reported no significant differences between heat/exercise group and injection/exercise groups, all groups better than analgesia alone. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
Nicholson 1985.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No;Blind therapists: No; Adequate follow‐up: No; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 20 participants (mean age treatment group 51, range 31‐70; mean age control group 55, range 20‐77) with shoulder pain plus limited passive motion of the glenohumeral joint. | |
| Interventions | Group 1:Mobilisation and active exercise 2‐3 times a week for 4 weeks.Group 2: Active exercise only. | |
| Outcomes | Assessed at 4 weeks.Outcomes:1.Range of active internal rotation.2.Range of active abduction.3.Range of passive abduction4.Pain score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Nykanen 1995.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: Yes; Blind therapists: Yes; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 61 participants (aged 31 ‐ 81; mean age treatment group 66; mean age control group 67) with rotator cuff disease without tear for at least 2 months | |
| Interventions | Group 1: Pulsed ultrasound (frequency 1.0mHz, on: off ratio 1:4 & intensity 1.0w/cm², 10 minutes), 10‐12 treatments over 3‐4 weeks.Group 2: Placebo ultrasound as above. | |
| Outcomes | Assessment at baseline, completion & 4‐12 months follow‐up.1.Clinical assessment: active ROM abduction, pain (supraspinatus test ‐ 4 point scale)2.Questionaires answered re: pain, ADL's, medication, other treatment received. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Perron 1997.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 22 participants (mean age treatment group 43; mean age control group 40) with a confirmed diagnosis of symptomatic calcifying tendonitis of the shoulder, the area of the calcium deposit was to be 50mm or greater | |
| Interventions | Group 1: No treatment Group 2: 9 treatments including acetic acid iontophoresis (5% acetic acid solution via the negative electrode, 5mA galvanic current, 20 minutes) followed by continuous ultrasound (0.8w/cm², 1MHz, 5 minutes) | |
| Outcomes | Assessment at baseline, and after the 3rd, 6th, and 9th treatments.Outcomes: X‐ray of area (density of calcium deposit) and functional outcomes including passive shoulder abduction, ROM, pain intensity (present pain index scale ‐ 6pt scale). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Reid 1996.
| Methods | Random allocation: Yes;Concealed allocation: No;Baseline comparability: Yes;Blind assessors: No;Blind subjects: No;Blind therapists: No;Adequate follow‐up: No;Intention‐to‐treat analysis: No;Between‐group comparisons: No;Point estimates & variability: Yes;Eligibility criteria: Yes | |
| Participants | 20 male (mean age 22) university students with diagnosis of anterior instability (clinical history and positive apprehension test). Excluded if had history of voluntary or traumatic dislocation. | |
| Interventions | Group 1: Isokinetic resistance exercises, 2 times per week.Group 2: Electromyographic Biofeedback Re‐education Program, 2 times per week. Biofeedback provided to instruct dynamic control of humeral head in functional activity. | |
| Outcomes | Assessed at 8, 26 and 52 weeks1. Function (modified Constant score)2. Pain at rest and on activity (3 point scale)3. Isokinetic strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Saunders 1995.
| Methods | Random allocation: Yes, stratified by gender; Concealed allocation: Unclear; Baseline comparability: Yes;Blind assessors: Yes; Blind subjects: Yes; Blind therapists: Yes; Adequate follow‐up: No;Intention‐to‐treat analysis: Yes;Between‐group comparisons: Yes;Point estimates & variability: Yes;Eligibility criteria: Yes | |
| Participants | 24 participants (mean age treatment group 49.8; mean age control group 50.7) with supraspinatus tendinitis of > 4 weeks duration. | |
| Interventions | All participants advised to rest arm from aggravating activity Group 1: 9 x 3 minute treatments with active laser over three weeks. Group 2: Identical regime with placebo laser | |
| Outcomes | Pain on VAS over 24 hours. Maximum voluntary contraction of abduction in internal rotation Tenderness. All assessed at end of intervention period. No long term follow up. | |
| Notes | Only general improvement in pain data presented in a format suitable for inclusion in the review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Shehab 2000.
| Methods | Random allocation: Yes;Concealed allocation: No;Baseline comparability: Yes;Blind assessors: Yes;Blind subjects: No;Blind therapists: No;Adequate follow‐up: No;Intention‐to‐treat analysis: Yes;Between‐group comparisons: Yes;Point estimates & variability: Yes;Eligibility criteria: Yes | |
| Participants | 50 female participants with painful shoulder movement of at least 1 month's duration. Diagnosis confirmed with provocative testing | |
| Interventions | Both groups treated 3‐5 times a week for 13 sessionsGroup 1: TNS 30 mins 50Hz to anterior and posterior shoulderGroup 2: US 0.5W for 10 mins, increased by 0.1W for each sessionBoth groups had ice and stretching | |
| Outcomes | Assessed after 13 visits 1. Pain on VAS2. Flexion and Abduction ROM | |
| Notes | Presented medians and ranges hence not included in meta‐analysis but in additional tables | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Taverna 1990.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: No; Blind assessors: Yes; Blind subjects: Yes; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: Yes; Between‐group comparisons: No; Point estimates & variability: No; Eligibility criteria: Yes | |
| Participants | 40 participants (age range 23 ‐ 79) with shoulder peri‐arthritis (trial also includes 40 participants with cervical osteoarthritis but results presented separately) | |
| Interventions | Group 1: Treated with Laser therapy (1000Hz, 24mWatt for 15 to 20 minutes) over 15 treatments. Group 2: Control group (sham laser therapy) | |
| Outcomes | Patient reported success or failure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
van der Heijden 1999.
| Methods | Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: Yes; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 180 participants aged over 18 years (mean age active ET 51; mean age placebo ET 50; mean age no ET and no US 54; mean age active US 50; mean age placebo US 51) with pain over deltoid on movement OR reduced GH ROM OR both and a standardised clinical assessment revealing soft tissue injury. | |
| Interventions | 5 groups who received 12 exercise therapy classes in 6 weeks as well as: Group 1: Active ET (Interferential electrotherapy) and US (Ultrasound)Group 2: Active ET and dummy USGroup 3: Dummy ET and active USGroup 4: Dummy ET and dummy USGroup 5: no additional adjuncts.ET: Bipolar interferential current (45Hz sinusoidal biphasis, amp module 60‐100Hz rampt fall 1 see each and constant phase 2 sec in between.US: 0.8MHz 4cm², pulsed 2:8. | |
| Outcomes | Assessed at 6 weeks and 3, 6, 9 and 12 months.1. Recovery (7 point Likert scale) 2. Functional status (shoulder disability questionnaire) 3. Chief complaint 4. Pain 5. Clinical status6. ROM. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
van der Windt 1998.
| Methods | Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: No; Blind therapists: No; Adequate follow‐up: Yes; Intention‐to‐treat analysis: Yes; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: Yes | |
| Participants | 108 participants (mean age corticosteroid 57.3; mean age physiotherapy 60.2). Painful restriction of GH joint and subjects 18 years and older | |
| Interventions | Group 1:Intraarticular corticosteroid injection (40mg triamcinolone acetonide 3 or less over 6 weeks, posterior route).Group 2: Physiotherapy (12 x 30 minute sessions of passive mobilisation, exercise and pain modalities). | |
| Outcomes | Assessed at 3, 7, 13, 26 and 52 weeks.Outcomes: 1. Improvement in main complaint and pain (6 point Likert scale, VAS scale), 2. Improvement in shoulder disability (shoulder disability questionnaire) 3. Adverse reactions, 4. Overall clinical severity (VAS), 5. Shoulder ROM. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Vecchio 1993.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind assessors: Yes; Blind subjects: Yes; Blind therapists: Yes; Adequate follow‐up: Yes; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates and variability: Yes; Eligibility criteria: Yes | |
| Participants | 35 participants (mean age 54.4, range 17‐77). Typical rotator cuff tendinitis with painful arc of abuction between 40‐120 degrees and painful restricted movement in at least oneof abduction external or internal rotation. NSAID therapy ceased with a one week washout before baseline assessment. Exclusion: participants with frozen shoulder, acromioclavicular arthritis or clinical rotator cuff tears; patients who were pregnant or breast feeding or who had received ultra‐articular or subacromial steroids in the three months prior to treatment; patients who had systemic disease or who had recieved physiotherapy for shoulder lesion | |
| Interventions | Group 1: Twice weekly low level laser treatment for eight weeks. EAch treatment 10 minutes consisting of three pulses (3J) to each of a maximum of five tender points with a wavelength of 830mn operated at 0 power. Group 2: same regimen but dummy laser operated at 0 power. Both groups performed exercises. | |
| Outcomes | Assessed at 2, 4 and 8 weeks. Outcomes: 1.Range of movement; 2. Painful arc score; 3. Resisted movement score; 4. Night, rest and movement pain (VAS); 5. Functional limitation (VAS) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Winters 1997/9.
| Methods | Random allocation: Yes; Concealed allocation: No; Baseline comparability: No; Blind assessors: No; \Blind subjects: No; Blind therapists: No; Adequate follow‐up: No; Intention‐to‐treat analysis: No; Between‐group comparisons: Yes; Point estimates & variability: Yes; Eligibility criteria: No | |
| Participants | 178 participants (mean age shoulder girdle manipulation group 43.9; mean age shoulder girdle physiotherapy group 46.4; mean age synovial corticosteroid group 53.5; mean age synovial manipulation group 46.7; mean age synovial physiotherapy group 53.1) with shoulder complaints presenting to general practice. Two populations reported in this trial, a "shoulder girdle group" where pain originated from the cervical and thoracic spine, and a "synovial group" where pain originated from shoulder joint (n=114). Shoulder joint population only reported in this statement. | |
| Interventions | First week: All received 50mg diclofenac sodium three times daily.Then, on the basis of reassessment they were divided into two groups: Group 1: Synovial group: Group 1: corticosteroid injection (1‐3 injections as needed at baseline, 1 week and after 2 weeks of 1 ml of 40 mg/ml triamcinolone acctonide with 9ml of 10mg.ml lidocaine), Group 2: "manipulation" (mobilisation/manipulation of cervical upper spine, upper thoracic spine, upper ribs, AC joint, GH joint once weekly with a maximum of 6 treatments), Group 3 "physiotherapy" (no mobes or manips, exercise and electrotherapy 2 times weekly). | |
| Outcomes | Assessment at baseline and 1, 2, 6 and 11 weeks.1. Pain level: Shoulder pain score, 6‐question scale and 101‐point numerical pain scale. . Weekly pain score 2. Active and passive ROM 3. Asked if they felt "cured" of if treatment had failed. 4. Duration of shoulder complaints analysed by survival analysis. | |
| Notes | Two groups of subjects reported in this trial, a "shoulder girdle group" where pain originated from cervical and thoracic spine, and a "synovial group" where pain originated from shoulder joint. Only data from "synovial group" included in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anderson 1996 | Population not included in this review: post‐operative shoulder surgery |
| Arciero 1994 | Population not included in this review: all patients had sustained trauma. |
| Arslan 2001 | Randomised controlled trial of corticosteroid injection versus combined physiotherapy and non‐steroiodal anti‐inflammatory. Not able to seperate out the effect of physiotherapy. Included in Cochrane Review of cortico‐steroid injection for shoulder disorders |
| Biswas 1979 | Not clear if randomised, 2/3 of participants lost to follow up and no between group comparisons |
| Chee 1986 | Population not included in this review: was neck and shoulder pain with no separately reported data. |
| Curtis 1999 | Population not included in this review: wheelchair users not necessarily with shoulder pain. Intervention was unsupervised exercise as prevention of pain and disability |
| Echternach 1966 | Intervention not included in this review: assessed the intervention of audioanalgesia as a way to better tolerate mobilisation, not whether mobilisation, nor audioanalgesia, was effective treatment |
| Gam 1998 | Population not included in this review: myofascial neck and shoulder region pain |
| Grossi 1986 | Population not included in this review: 73 patients with either lateral epicondylitis or adhesive capsulitis (numbers of each individual diagnosis not given). Not possible to seperate lateral epicondylitis and adhesive capsulitis data. |
| Hagberg 2000 | Population not included in this review: myofascial neck and shoulder region pain |
| Inaba 1972 | Population not included in this review: hemiplegia |
| Lastayo 1998 | Population not included in this review: post‐operative shoulder surgery |
| Leandri 1990 | Population not included in this review: hemiplegia |
| Leboeuf 1987 | Population not included in this review: repetitive strain injury of entire upper limb |
| Livesley 1992 | Population not included in this review: trauma |
| Lloyd‐Roberts 1959 | Not randomised. |
| Lundberg 1979 | Population not included in this review: humeral head fractures). Subjects sustained trauma and therefore excluded |
| Lundblad 1999 | Population not included in this review: included participants with neck and shoulder complaints with data from participants with shoulder complaints not presented seperately |
| Melzer 1995 | Not randomised |
| Meyer 1997 | Not randomised |
| Morgan 1995 | Is a randomised controlled trial of the use of TNS to control pain during a painful intervention for shoulder disorder, not of an intervention for the disorder. |
| Nash 1990 | Trail of high intensity TENS compared to low intensity TENS for analgesia during hydrodilatation (distension arthrography), not as a treatment for shoulder disorder |
| Partridge 1990 | Population not included in this review: hemiplegia |
| Philipson 1983 | Population not included in this review: chronic myofascial syndrome |
| Quin 1965 | Not randomised |
| Raab 1996 | Population not included in this review: post‐operative shoulder surgery |
| Rahme 1998 | Intervention is of surgery |
| Randlov 1998 | Population not included in this review: myofascial neck and shoulder region pain |
| Ritchie 1997 | Intervention is for post shoulder surgery pain relief, not treatment of shoulder disorder. |
| Rizk 1983 | Not randomised |
| Speer 1996 | Intervention is for post shoulder surgery pain relief, not treatment of shoulder disorder. |
| Spence 1995 | Population not included in this review: myofascial neck and shoulder region pain |
| Vasseljen 1998 | Population not included in this review: myofascial neck and shoulder region pain |
| Vecchini 1984 | Capsulitis data not presented seperately. Twelve of the 24 subjects in the study suffered adhesive capsulitis, the remaining 12 with lateral epicondylitis of the elbow. |
| Waldburger 1992 | Population not included in this review: post‐traumatic |
| Waling 2000 | Population not included in this review: myofascial neck and shoulder region pain |
| Williams 1986 | Population not included in this review: rheumatoid arthritis |
| Wolf 1996 | Population not included in this review: post‐operative shoulder surgery |
Contributions of authors
Sally Green and Rachelle Buchbinder modified the updated protocol. Sally Green and Rachelle Buchbinder identified trials and extracted study results. Sally Green and Sarah Hetrick entered study details and results. All reviewers wrote the review.
Sources of support
Internal sources
Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia.
Australasian Cochrane Centre, Australia.
External sources
No sources of support supplied
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
Bang 2000 {published data only}
- Bang M, Deyle G. [Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome]. Journal of Orthopeadic & Sports Physical Therapy 2000;30(3):126‐137. [DOI] [PubMed] [Google Scholar]
Berry 1980 {published data only}
- Berry H, Fernandes L, Bloom B, Clark RJ, Hamilton EB. [Clinical study comparing acupuncture, physiotherapy, injection and oral anti‐inflammatory treatment in shoulder‐cuff lesions]. Current Medical Research & Opinion 1980;7(121‐6). [DOI] [PubMed] [Google Scholar]
- Fernandes L, Berry H, Clark RJ, Bloom B, Hamilton EBD. [Clinical study comparing acupuncture, physiotherapy, injection and oral anti‐inflammatory therapy in shoulder cuff lesions]. Lancet 1980;Jan:208‐209. [DOI] [PubMed] [Google Scholar]
Binder 1984 {published data only}
- Binder A, Parr G, Hazleman B. [Pulsed electromagnetic field therapy of persistent rotator cuff tendonitis]. Lancet 1984;1(8379):695‐698. [DOI] [PubMed] [Google Scholar]
Brox 1993/7 {published data only}
- Bohmer A, Staff P, Brox J. [Supervised exercises in relation to rotator cuff disease (impingement syndrom stages I and II): a treatment regimen and its rationale]. Physiotherapy Theory & Practice 1998;14:93‐105. [Google Scholar]
- Brox J, Staff P, Ljunggren A, Brevik J. [Arthroscopic surgery compared with supervised exercises in patients with rotator cuff disease]. British Medical Journal 1993;307(6909):899‐903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brox JI, Gjengedal E, Uppheim G, Bohmer AS, Brevik JI, Ljuggren AE, Staff PH. [Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): A prospective, randomised, controlled study in 125 patients with a 2 1/2 year follow‐up]. Journal of Shoulder & Elbow Surgery 1999;8(2):102‐111. [DOI] [PubMed] [Google Scholar]
Bulgen 1984 {published data only}
- Bulgen D, Binder A, Hazleman B, Dutton J, Roberts S. [Frozen shoulder: prospective clinical study with an evaluation of three treatment regimes]. Annals of the Rheumatic Diseases 1984;43:353‐360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Conroy 1998 {published data only}
- Conroy DE, Hayes KW. [The effect of mobilization as a component of comprehensive treatment for primary shoulder impingement syndrome]. Journal of Orthopaedic & Sports Physical Therapy 1998;28(1):3‐14. [DOI] [PubMed] [Google Scholar]
Dacre1989 {published data only}
- Dacre J, Beeney N, Scott D. [Injections and physiotherapy for the painful, stiff shoulder]. Annals of the Rheumatic Diseases 1989;48(4):322‐332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dal Conte 1990 {published data only}
- Dal Conte G, Rivoltini P, Combi F. [Trattamento della periartrite calcarea di spalla con campi magnetici pulsanti: studio controllato]. La Riabilitazione 1990;23(1):27‐33. [Google Scholar]
Downing 1986 {published data only}
- Downing D, Weinstein A. [Ultrasound therapy of Subacromial Bursitis]. Physical Therapy 1986;66(2):194‐199. [DOI] [PubMed] [Google Scholar]
Ebenbichler 1999 {published data only}
- Ebenbichler GR, Erdogmus CB, Resch KL, Funovics MA, Kainberger F, Barisani G, et al. [Ultrasound therapy for calcific tendinitis of the shoulder]. New England Journal of Medicine 1999;340:1533‐8. [DOI] [PubMed] [Google Scholar]
England 1989 {published data only}
- England S, Farrell A, Coppock J, Struthers G, Bacon P. [Low laser therapy of shoulder tendonitis]. Scandanavian Journal of Rheumatology 1989;18:427‐43. [DOI] [PubMed] [Google Scholar]
Ginn 1997 {published data only}
- Ginn KA, Herbert RD, Khouw W, Lee R. [A randomized, controlled clinical trial of a treatment for shoulder pain]. Physical Therapy 1997;77(8):802‐811. [DOI] [PubMed] [Google Scholar]
Herrera‐Lasso 1993 {published data only}
- Herrera‐Lasso I, Moborak L, Fernandez‐Dominguez L, Cardiel M, Alarcon‐Segovia D. [Comparative effectiveness of packages of treatment including ultrasound or transcutaneous electrical nerve stimulation in painful shoulder syndrome]. Physiotherapy 1993;79(4):251‐253. [Google Scholar]
Leclaire 1991 {published data only}
- Leclaire R, Bourgouin J. [Electromagnetic treatment of shoulder periarthritis: a randomised controlled trial of efficiency and tolerance of magnetotherapy]. Archives of Physical Medicine & Rehabilitation 1991;72:284‐288. [PubMed] [Google Scholar]
Lee 1973 {published data only}
- Lee M, Haq A, Wright V, Longton E. [Periarthritis of the shoulder: A controlled trial of physiotherapy]. Physiotherapy 1973;59(10):312‐315. [PubMed] [Google Scholar]
Nicholson 1985 {published data only}
- Nicholson G. [The effects of passive joint mobilisation on pain and hypomobility associated with adhesive capsulitis of the shoulder]. Journal of Orthopaedic & Sports Physical Therapy 1985;6:238‐246. [DOI] [PubMed] [Google Scholar]
Nykanen 1995 {published data only}
- Nykanen M. [Pulsed ultrasound treatment of the painful shoulder: A randomized, double‐blind, placebo‐controlled study]. Scandinavian Journal of Rehabilotation Medicine 1995;27:105‐108. [PubMed] [Google Scholar]
Perron 1997 {published data only}
- Perron M, Malouin F. [Acetic acid iontophoresis and ultrasound for the treatment of calcifying tendinitis of the shoulder: A randomized control trial]. Archives of Physical Medicine and Rehabilitation 1997;78:379‐384. [DOI] [PubMed] [Google Scholar]
Reid 1996 {published data only}
- Reid D, Saboe L, Chepeha J. [Anterior shoulder instability in athletes: comparison of isokinetic resistance exercises and an electromyographic biofeedback re‐education program ‐ a pilot program]. Physiotherapy Canada 1996;48(4):251‐256. [Google Scholar]
Saunders 1995 {published data only}
- Saunders L. [The efficacy of low level laser therapy in supraspinatus tendinitis]. Clinical Rehabilitation 1995;9:126‐34. [Google Scholar]
Shehab 2000 {published data only}
- Shehab D, Adham N. [Comparative effectiveness of ultrasound and transcutaneous electrical stimulation in treatment of periarticular shoulder pain]. Physiotherapy Canada 2000;52(3):208‐210, 214. [Google Scholar]
Taverna 1990 {published data only}
- Taverna E, Parrini M, Cabitza P. Laser therapy versus placebo in the treatment of some bone and joint pathology [Laserterapia IR versus placebo nel trattamento di alcune patologie a carcio dell'apparato locomotore]. Minerva Ortopedica E Traumatologica 1990;41:631‐6. [Google Scholar]
van der Heijden 1999 {published data only}
- Heijden GJMG, Leffers P, Wolters PJMC, Verheijden JJD, Mameren HHJP, Bouter LM, Knipschild PG. [No effect of bipolar interferential electrotherapy and pulsed ultrasound for soft tissue shoulder disorders: a randomised controlled trial]. Annals of Rheumatic Diseases 1999;58(9):530‐540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heijden GJMG, Windt DAWM. [Shoulder disorders in primary care: prognosis and management]. Dutch Journal of Physical Therapy 1999;May:19‐22. [Google Scholar]
van der Windt 1998 {published data only}
- Windt DAWM, Koes BW, Deville W, Boeke QAJP, Jong BA, Bouter LM. [Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care: randomised trial]. British Medical Journal 1998;317(7168):1292‐1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vecchio 1993 {published data only}
- Vecchio P, Cave C, King V, Adebajo AO, Smith M, Hazleman BL. [A double‐blind study of the effectiveness of low level laser treatment of rotator cuff tendinitis]. British Journal of Rheumatology 1993;32(740‐42). [DOI] [PubMed] [Google Scholar]
Winters 1997/9 {published data only}
- Winters JC, Jorritsma W, Groenier KH, Sobel JS, Meyboom‐de‐Jong B, Hans J. [Treatment of shoulder complaints in general practice: long term results of a randomised, single blind study comparing physiotherapy, manipulation, and corticosteroid injection]. British Medical Journal 1999;318(7195):1395‐1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters JC, Sobel JS, Groenier KH, Arendzen HJ, Meyboom‐de‐jong, B. [Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: Randomized, single blind study]. British Medical Journal 1997;314:1320‐1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters JC, Sobel JS, Groenier KH, et al. [Comparison of physiotherapy, manipulation and corticosteroid injection for treating shoulder complaints in general practice]. Journal of Family Practice (Journal Club) 1997;45(2):103‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Anderson 1996 {published data only}
- Anderson NH, Johannsen HV. Sneppen O. [Self‐training versus physiotherapist guided rehabilitation after arthroscopic deconmpression‐ a prospective randomized study]. Acta Orthopaedica Scandinavica 1996;Suppl 272:67. [Google Scholar]
Arciero 1994 {published data only}
- Arciero RA, Wheeler JH, Ryan JB, McBride JT. [Arthroscopic bankart repair versus non operative treatment for acute initial anterior shoulder dislocations]. American Journal of Sports Medicine 1994;22(5):589‐94. [DOI] [PubMed] [Google Scholar]
Arslan 2001 {published data only}
- Arslan S, Celiker R. [Comparison of the efficacy of local corticosteroid injection and physical therapy for the treatment of adhesive capsulitis]. Rheumatology International 2001;21(1):20‐23. [DOI] [PubMed] [Google Scholar]
Biswas 1979 {published data only}
- Biswas AK, Sur BN, Gupta CR. [Treatment of periarthritis shoulder]. Journal of the Indian Medical Association 1979;72:276‐7. [PubMed] [Google Scholar]
Chee 1986 {published data only}
- Chee E, Walton H. [Treatment of Trigger Points with Microamperage Transcutaneous Nerve Stimulation (TENS) ‐ (The Electro‐Acuscope 80)]. Journal of Manipulative & Physiological Therapeutics 1986;9(2):131‐134. [PubMed] [Google Scholar]
Curtis 1999 {published data only}
- Curtis K, Tyner T, Zachary L, Lentell G, Brink D, Didyk T, et al. [Effect of a standard exercise protocol on shoulder pain in long‐term wheelchair users]. Spinal Cord 1999;37(6):421‐429. [DOI] [PubMed] [Google Scholar]
Echternach 1966 {published data only}
- Echternach J. [Audioanalgesia as an adjunct to mobilization of the chronic frozen shoulder]. Physical Therapy 1966;46(8):839‐46. [DOI] [PubMed] [Google Scholar]
Gam 1998 {published data only}
- Gam A, Warming S, Larsen A. [Treatment of myofascial trigger‐points with ultrasound combined with massage and exercise: a randomised controlled trial]. Pain 1998;77(1):73‐79. [DOI] [PubMed] [Google Scholar]
Grossi 1986 {published data only}
- Grossi E, Monza GC, Pollavini S, Bona L. [NSAID ionisation in the management of soft‐tissue rheumatism: Role played by the drug, electrical stimulation and suggestion]. Clinical and Experimental Rheumatology 1986;4:265‐267. [PubMed] [Google Scholar]
Hagberg 2000 {published data only}
- Hagberg M, Harms‐Ringdahl K, Nisell R, Hjelm E. [Rehabilitation of neck‐shoulder pain in women industrial workers: a randomised trial comparing isometric shoulder endurance training with shoulder strength training]. Archives of Physical Medicine & Rehabilitation 2000;81(8):1051‐1058. [DOI] [PubMed] [Google Scholar]
Inaba 1972 {published data only}
- Inaba MK, Piorkowski M. [Ultrasound treatment of painful shoulders in patients with hemiplegia]. Physical Therapy 1972;52:737‐41. [DOI] [PubMed] [Google Scholar]
Lastayo 1998 {published data only}
- Lastayo P, Wright T, Jaffe R, Hartzel J. [Continuous passive motion after repair of the rotator cuff: A prospective outcome study]. Journal of Bone & Joint Surgery ‐ American Volume 1998;80(7):1002‐1011. [DOI] [PubMed] [Google Scholar]
Leandri 1990 {published data only}
- Leandri M, Parodi CI, Corrieri N. [Comparisons of TENS treatments in hemiplegic shoulder pain]. Scandinavian Journal of Rheumatology 1989;18:427‐31. [PubMed] [Google Scholar]
Leboeuf 1987 {published data only}
- Leboeuf C, Grant B, Maginnes GS. [Chiropractic treatment of repetitive strain injuries: A preliminary prospective outcome study of SMT versus SMT combined with massage]. Journal of Australian Chiropractors' Association 1987;17:11‐14. [Google Scholar]
Livesley 1992 {published data only}
- Livesley PJ, Mugglestone A, Whitton J. [Electrotherapy and the management of minimally displaced fractures of the neck of humerus]. Injury 1992;23:323‐327. [DOI] [PubMed] [Google Scholar]
Lloyd‐Roberts 1959 {published data only}
- Lloyd‐Roberts GC, French PR. [Periarthritis of the shoulder: A study of the disease and its treatment]. British Medical Journal 1959;1:1569‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lundberg 1979 {published data only}
- Lundberg BJ, Svenungsos‐Hartwig E, Wikmark R. [Independent exercises versus physiotherapy in non‐displaced proximal humeral head fractures]. Scandinavian Journal of Rehabilitation Medicine 1979;11:133‐136. [PubMed] [Google Scholar]
Lundblad 1999 {published data only}
- Lundblad I, Elert J, Gerdle B. [Randomized controlled trial of physiotherapy and feldenkrais interventions in female workers with neck‐shoulder complaints]. Journal of Occupational Rehabilitation 1999;9(3):179‐193. [Google Scholar]
Melzer 1995 {published data only}
- Melzer C, Wallny T, Wirth CJ, Hoffmann S. [Frozen shoulder, treatment and results]. Archives of Orthopaedic & Trauma Surgery 1995;114(2):87‐91. [DOI] [PubMed] [Google Scholar]
Meyer 1997 {published data only}
- Meyer M, Liebau C, Merk H. [Therapy for idiopathic frozen shoulder stages 2 and 3 ‐ Manipulation under anaesthesia versus arthroscopy: A prospective study]. The Journal of Bone and Joint Surgery ‐ British Volume (1997).;79B(supp. 2):202. [Google Scholar]
Morgan 1995 {published data only}
- Morgan B, Jones A, Mulcahy K, Finlay D, Collett B. [Transcutaneous electric nerve stimulation (TENS) during distension shoulder arthrography: a controlled trial]. Pain 1995;64:265‐267. [DOI] [PubMed] [Google Scholar]
Nash 1990 {published data only}
- Nash TP, Williams JD, Machin D. [TENS: Does the type of stimulus really matter?]. Pain Clinic 1990;3:161‐168. [Google Scholar]
Partridge 1990 {published data only}
- Partridge CJ, Edwards SM, Mee R, Langenberghe HVK van. [Hemiplegic shoulder pain: a study of two methods of physiotherapy treatment]. Clinical Rehabilitation 1990;4:43‐9. [Google Scholar]
Philipson 1983 {published data only}
- Philipson T, Haagensen N, Laumann V, Nies M, Thorup K, Hansen TI. [The effect of diadynamic current on chronic soft tissue pain in the neck and shoulder girdle]. Ugeskr Laeger 1983;145(7):479‐481. [PubMed] [Google Scholar]
Quin 1965 {published data only}
- Quin CE. [Frozen shoulder: Evaluation of tretment with hydrocortisone injections and exercises]. Annals of Physical Medicine 1965;8:22‐29. [PubMed] [Google Scholar]
Raab 1996 {published data only}
- Raab M, Rzeszutko D, O'Connor W, Greatting M. [Early results of continuous passive motion after rotator cuff repair: a prospective, randomised, blinded, controlled study]. American Journal of Orthopaedics 1996;25(3):214‐220. [PubMed] [Google Scholar]
Rahme 1998 {published data only}
- Rahme H, Solem‐Bertoft E, Westerberg CE, Lundberg E, Sorensen S, Hilding S. [The subacromial impingement syndrome. A study of results of treatment with special emphasis on predictive factors and pain‐generating mechanisms]. Scandinavian Journal of Rehabilitative Medicine 1998;30(4):253‐62. [DOI] [PubMed] [Google Scholar]
Randlov 1998 {published data only}
- Randlov A, Ostergaard M, Manniche C, Kryger P, et al. [Intensive dynamic training for females with chronic neck/ shoulder pain. A randomised controlled trial]. Clinical Rehabilitation 1998;12:200‐210. [DOI] [PubMed] [Google Scholar]
Ritchie 1997 {published data only}
- Ritchie, ED, Tong, D, Chung, F, Norris, A, Miniaci, A, & Vairavanathan, S. D. [Suprascapular nerve block ‐ A new technique for pain relief in arthroscopic shoulder surgery?]. The Journal of Bone and Joint Surgery ‐ British Volume 1997;79B(supp. 1):72‐73. [Google Scholar]
Rizk 1983 {published data only}
- Rizk T, Christopher R, Pinals R. [Adhesive Capsulitis (Frozen Shoulder): A new approach to its management]. Archives of Physical Medicine & Rehabilitation 1983;64:29‐33. [PubMed] [Google Scholar]
Speer 1996 {published data only}
- Speer K, Warren R, Horowitz. [The efficacy of cryotherapy in post‐operative shoulder]. Journal of Shoulder & Elbow Surgery 1996;5:62‐8. [DOI] [PubMed] [Google Scholar]
Spence 1995 {published data only}
- Spence SH, Sharpe L, Newton‐John T, Champion D. [Effect of EMG biofeedback compared to applied relaxation training with chronic, upper extremity cumulative trauma disorders]. Pain 1995;63:199‐206. [DOI] [PubMed] [Google Scholar]
Vasseljen 1998 {published data only}
- Vasseljen O, Johansen B, Westgaard R. [The effect of pain reduction on perceived tension and EMG recorded trapezius muscle activity in workers with shoulder and neck pain]. Scandinavian Journal of Rehabilitation Medicine 1995;27:243‐252. [PubMed] [Google Scholar]
Vecchini 1984 {published data only}
- Vecchini L, Grossi E. [Ionisation with diclofenac sodium in rheumatic disorders: A double blind placebo controlled trial]. Journal of International Medical Research 1984;12:346‐350. [DOI] [PubMed] [Google Scholar]
Waldburger 1992 {published data only}
- Waldburger M, Meirer JL, Gobelet C. [The frozen shoulder: Diagnosis and treatment. Prospective study of 50 cases of Adhesive capsulitis]. Clinical Rheumatology 1992;11(3):364‐368. [DOI] [PubMed] [Google Scholar]
Waling 2000 {published data only}
- Waling K, Sundelin G, Ahlgren C, Jarvholm B. [Perceived pain before and after three exercise program ‐ a controlled clinical trial of women with work related trapezius myalgia]. Pain 2000;85(1‐2):201‐207. [DOI] [PubMed] [Google Scholar]
Williams 1986 {published data only}
- Williams J, Harvey J, Tannenbaum H. [Use of superficial heat versus ice for rheumatoid arthritic shoulder. A pilot study]. Physiotherapy Canada 1986;38:8‐13. [Google Scholar]
Wolf 1996 {published data only}
- Wolf M, Gomez R. [Independent home therapy versus formal physical therapy following arthroscopic shoulder surgery]. American Academy of Orthopaedic Surgeons: Scientific Program. Abstract in Orthopaedic Transactions 1996;20:20. [Google Scholar]
References to studies awaiting assessment
Chard 1988 {published data only}
- Chard MD, Hazleman BL, Devereaux MD. Controlled trial to investigate dose‐response patterns to portable, pulsed electromagnetic fields in the treatment of rotator cuff tendinitis: a review trial. J Orthop Rheumatol 1988;1:33‐40. [Google Scholar]
Gudmundsen 1987 {published data only}
- Gudmundsen J, Vikne J. Laser treatment for epicondylitis humeri and rotator cuff syndrome. Nord Tidsskr Idrettsmed 1987;2:6‐15. [Google Scholar]
Knorre 1990 {published data only}
- Knorre, von B, Keitel, W. [Vergleichende Therapiestudie: Ultraschall, Kryotherapie und intraartikulare Kortisonoide bei Veranderungen des Schultergelenkes aus entzundlicher Ursache]. Z. Physiother. Jg. 1990;42:221‐225. [Google Scholar]
Additional references
Allander 1974
- Allander E. [Prevalence, incidence and remission rates of some common rheumatic diseases and syndromes]. Scandinavian Journal of Rheumatology 1974;3(3):145‐153. [DOI] [PubMed] [Google Scholar]
Badley 1992
- Badley EM, Tennant A. [Changing profile of joint disorders with age: Findings from a postal survey of the population of Calderdale, West Yorkshire, United Kingdom]. Annals of Rheumatic Diseases 1992;51(3):366‐371. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beaton 1996
- Beaton D, Richards L. [Measuring Function of the Shoulder]. The Journal of Bone and Joint Surgery 1996;78‐A:882‐90. [DOI] [PubMed] [Google Scholar]
Bjelle 1989
- Bjelle A. [Epidemiology of shoulder problems]. Balliere's Clinical Rheumatology 1989;3:437‐451. [DOI] [PubMed] [Google Scholar]
Bridges Webb 1992
- Bridges‐Webb CH, Britt D, Miles S, Neary A, Charles M. [Treatment in general practice in Australia]. Medical Journal of Australia 1992;Suppl(S1‐S56). [Google Scholar]
Chakravarty 1993
- Chakravarty K, Webley M. [Shoulder Joint Movement and Its Relationship to Disability in the Elderly]. Journal of Rheumatology 1993;20(8):1359‐1361. [PubMed] [Google Scholar]
Chard 1991
- Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. [Shoulder disorders in the elderly: a community survey]. Arthritis & Rheumatism 1991;34(6):766‐769. [DOI] [PubMed] [Google Scholar]
Gartsman 1998
- Gartsman GM, Brinker MR, Khan M, Karahan M. [Self assessment of general health status in patients with five common shoulder conditions]. Journal of Shoulder and Elbow Surgery 1998;7(3):228‐237. [DOI] [PubMed] [Google Scholar]
Goupille, 1996
- Goupille P, Sibillia J. [Local corticosteroid injections in the treatment of rotator cuff tendinitis (except for frozen shoulder and calcific tendinitis)]. Clinical & Experimental Rheumatology 1996;14(5):561‐6. [PubMed] [Google Scholar]
Green 1999
- Green S, Buchbinder R, Glazier R, Forbes A. The Cochrane Library 1999, Issue 1. [Google Scholar]
Hill 1983
- Hill JA. [Epidemiologic Perspective on Shoulder Injuries]. Clinics in Sports Medicine 1983;2(2):241‐246. [PubMed] [Google Scholar]
Ingemar 1993
- Ingemar‐Andersson H, Ejlertsson G, Leden I, Rosenberg C. [Chronic Pain In a Geographically Defined General Population: Studies of Differences in age, gender, social class, and pain localization]. Clinical Journal of Pain 1993;9(3):174‐182. [DOI] [PubMed] [Google Scholar]
Juni 1999
- Juni P, Witschi A, Bloch R, Egger M. [The hazards of scoring the quality of clinical trials for meta‐analysis]. Journal of the American Medical Association 1999;282(11):1054‐60. [DOI] [PubMed] [Google Scholar]
Lundberg 1969
- Lundberg B. [The frozen shoulder]. Acta Orthopaedica Scandinavia 1969;Suppl 119. [PubMed] [Google Scholar]
Pope 1997
- Pope D, Croft P, Pritchard C, Silman A. [Prevalence of shoulder pain in the community: the influence of case definition]. Annals Rheumatic Disease 1997;56:308‐312. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rekola 1993
- Rekola KE, Keinanen‐Kiukaanniemi S, Takala J. [Use of primary health services in sparsley populated country districts by patients with musculoskeletal symptoms: consultations with a physician]. Journal of Epidemiology & Commumity Health 1993;47(2):153‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
v der Heijden 1997
- Heijden GJMG, Windt DAWM, Winter SF. [Physiotherapy for patients with soft tissue shoulder disorders: a systematic review of randomised clinical trials]. British Medical Journal 1997;315(7099):25‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
van der Heijden 1996
- Heijden GJMG, Windt DAWM, Kleijnen J, Koes B, Bouter L. [Steroid injections for shoulder disorders: a systematic review of randomised clinical trials]. British Journal of General Practice 1996;46:309‐316. [PMC free article] [PubMed] [Google Scholar]
van der Windt 1995
- Windt DAWN, Heijden GJMG, Scholten RJPM, Koes BW, Bouter LM. [The efficacy of non‐steroidal anti‐inflammatory drugs (NSAIDs) for shoulder complaints: A systematic review]. Journal of Clinical Epidemiology 1995;48(5):691‐704. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Green 1998
- Green S, Buchbinder R, Glazier R, Forbes A. [Systematic review of randomised controlled trials of interventions for painful shoulder: selection criteria, outcome assessment and efficacy]. British Medical Journal 1998;316:354‐360. [DOI] [PMC free article] [PubMed] [Google Scholar]


