Abstract
Purpose
This case report represents poor nutritional intake and vomiting secondary to COVID-19 resulting in Wernicke's syndrome and blindness.
Observations
We report the case of a 36 year old with a post-COVID episode of acute-subacute onset bilateral blindness ultimately diagnosed as Wernicke's syndrome based on MRI findings and clinical response to high dose IV thiamine supplementation.
Conclusions and Importance
Given this patient's dramatic presentation of no light perception vision in both eyes and resolution of symptoms with treatment, it is reasonable to consider thiamine deficiency in any individual who presents with acute-subacute onset vision loss, particularly when the history is suggestive of potential nutritional deficiency.
Keywords: Neuro-ophthalmology, Neurology, COVID-19, SARS-CoV-2, Nutrition, Optic neuropathy
1. Introduction
Wernicke's Syndrome (WS) is a disorder that results from thiamine or vitamin B1 deficiency. In the United States, the most common etiology is alcoholism, however any cause of nutritional deficiency or malabsorption can also result in a thiamine deficit and thus the clinical presentation of WS. The classic presentation of WS consists of the triad of altered mental status, ophthalmoplegia, and ataxia. The single most common presentation of WS is some degree of altered mentation, which can range from mild apathy to coma.1
With regard to ocular findings associated with thiamine deficiency, nystagmus is the most common and usually presents as a horizontal gaze-evoked nystagmus followed by bilateral abducens palsy. Optic nerve and retinal hemorrhages have been reported and were described in Dr. Wernicke's initial publication in 1881. Disc edema alone is relatively uncommon, reported in 4% of cases reviewed by De Wardener et al.2 Vision loss is also a rare finding associated with Wernicke's syndrome and likely secondary to retinal hemorrhages and disc edema.3 When vision loss is reported it tends to be severe and bilateral.4 Severe vision loss to no light perception in both eyes is rare and has only been documented in individual case reports.
One study that compared alcohol-induced Wernicke's encephalopathy (WE) to non-alcohol induced WE found that both eye involvement and ataxia were significantly more common in alcohol-induced WS than in non-alcohol induced WE.5 Interestingly, ocular abnormalities related to thiamine deficiency show significant, rapid, and predictable improvement in response to high dose vitamin repletion.6 In one case report of alcohol-induced Wernicke Syndrome resulting in acute bilateral vision loss, extraocular movement abnormalities, and pathologic vertical nystagmus, administration of IV thiamine resulted in complete resolution of nystagmus and blindness within 12h along with significant improvement in extraocular movement abnormalities.7
2. Case report
We report the case of a post-COVID episode of acute-subacute onset bilateral blindness ultimately diagnosed as Wernicke's syndrome based on MRI findings and clinical response to high dose IV thiamine supplementation.
The patient is a 36-year-old previously healthy male with significant medical history only of recent SARS-COVID19 infection who presented with subacute onset painless bilateral blindness. He was initially diagnosed with COVID six weeks prior after presenting with fever, chills, diffuse myalgia, headache, nonproductive cough, and loss of smell and taste. The diagnosis was ultimately confirmed by PCR testing. He endured recurrent episodes of these symptoms as well as severe nausea, diarrhea, and odynophagia necessitating multiple hospitalizations at an outside facility and eventual diagnosis of concomitant oropharyngeal thrush which further limited his oral intake. During his hospitalizations, patient did not require intensive care unit admission and he was not intubated, sedated, proned; he did not require tube feedings. Of note, he complained of blurred vision during his prior hospitalization and noncontrast CT brain was performed and unrevealing: he was advised to follow up with ophthalmology; ophthalmology was not consulted during his admissions. Prior to COVID19 diagnosis, patient was slightly overweight but otherwise healthy. Per patient and wife, he regularly exercised, had well rounded diet and had normal annual exams with his primary care doctor.
Upon presentation to our institution, he endorsed vision gradually worsening with increasing blurriness over the 5 days prior to presentation. He had been able to see silhouettes the prior evening but awoke on day of presentation with vision completely dark bilaterally, unable to appreciate light or shapes. He denied pain, recent redness or irritation, headache, neck pain or stiffness, recent floaters or visual auras, rashes, or other focal neurologic deficits. He denied any personal or family history of seizure, stroke, or autoimmune disease, with no recent travel outside of Chicago or the United States. His wife noted that he had unintentional significant weight loss since his COVID-19 diagnosis (52lbs per chart review, or 20% of body weight). Of note, patient's starting weight prior to COVID-19 was 246 pounds and on presentation to ED he weighed 194 pounds. He had presented to an optometrist earlier in the morning and underwent dilated ophthalmologic examination; he did not recall the results but was advised to present emergently to a hospital.
On examination, the patient was in no acute distress and jocular about his condition, subjectively disoriented according to his wife but nevertheless mental status was normal with intact arousal, orientation, fund of knowledge, concentration, recall, and language. Initially his pupils were mydriatic and nonreactive to light bilaterally, likely due to residual pharmacologic dilation from his optometrist. Upon ophthalmology examination his pupils were small, 2mm and still nonreactive to light. His visual acuity was without light perception or blink to threat in both eyes. His volitional extraocular movements were mildly restricted in adduction and abduction. He also had abnormal saccades present on smooth pursuit. His sclerae were white and quiet without obvious signs of inflammation. He underwent a full dilated exam with indirect ophthalmoscopy which was significant for mild nasal fullness on the optic nerves but no true papilledema; there were no vessel obscurations, hemorrhages, or blurring of the disc margins. The posterior pole and peripheral retina were overall normal. The remainder of his cranial nerve, strength, sensory, coordination and reflex exams were normal. He appeared unsteady on his feet but without clear deficits in equilibrium beyond that caused by visual loss. A white coating on his tongue consistent with his history of oral thrush was noted.
With concern for bilateral optic neuritis, he underwent lumbar puncture in the emergency department and was admitted to the neurology service. Cerebrospinal fluid studies demonstrated mildly elevated protein to 38mg/dL (reference normal 7–35), no leukocytosis, negative Gram stain and aerobic culture, and negative testing for oligoclonal bands and myelin oligodendrocyte glycoprotein. Serum HIV and sarcoid studies were negative. While the initial plan was to empirically treat with 500 mg of IV solumedrol, imaging results were obtained as described below prior to steroid administration so the patient received IV thiamine in lieu of steroids.
MRI brain and MRI orbits without and with contrast (Fig. 1) revealed FLAIR hyperintensity of the medial thalami, mammillary bodies and periaqueductal gray matter and associated enhancement with restricted diffusion of the medial thalami bilaterally consistent with Wernicke's syndrome. Based upon MRI findings, treatment with intravenous thiamine 500 mg was initiated within 5 hours of patient's presentation to the Emergency Department and within an hour of the MRI results. Vision improved to 20/25 binocular acuity on bedside evaluation with near card after first dose of thiamine. A thiamine level was not drawn prior to supplementation. He was evaluated by dietary specialists and extensive workup for other vitamin and nutritional deficiencies was done. Specifically, his Vitamin B12 and folate levels were within normal limits. His electrolytes were mildly deranged but quickly resolved with oral supplementation and fluid resuscitation. The patient received a total of three days of 500 mg of intravenous thiamine with continued resolution of symptoms until day of discharge, and was advised to continue prescribed oral supplementation 100 mg three times a day for one week then 100 mg daily.
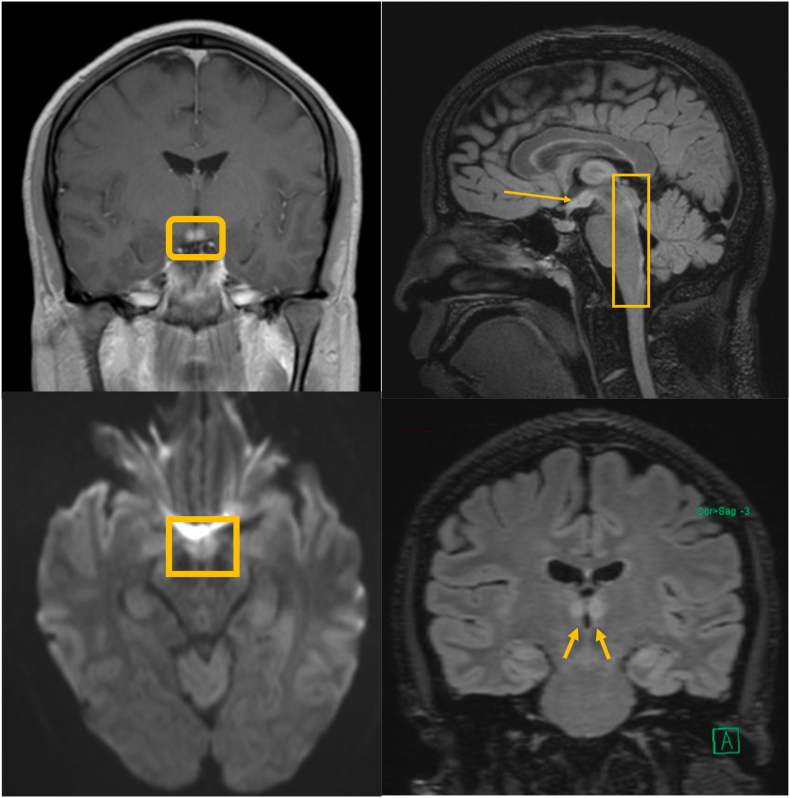
Fig. 1.
Clockwise from top left: Coronal MRI post-contrast with mamillary body enhancement (box) (a), sagittal FLAIR with mamillary body (arrow) and periaqueductal gray matter (box) hyperintensity(b), coronal FLAIR with bilateral thalamic (arrows) hyperintensity(c), and axial diffusion restriction of the periaqueductal gray matter (box) (d).
Follow up exam in the eye clinic four days after discharge from the hospital was significant for visual acuity of 20/25 at distance with pinhole. Dilated exam remained normal. Static perimetry, 24–2, (Fig. 3) was significant for paracentral depression. Initial ocular coherence tomography of the optic nerves (Fig. 2) showed mild edema in sectors which subsequently showed atrophy. These findings are consistent with metabolic optic neuropathy. The patient reports his vision is about 95% back to his baseline.
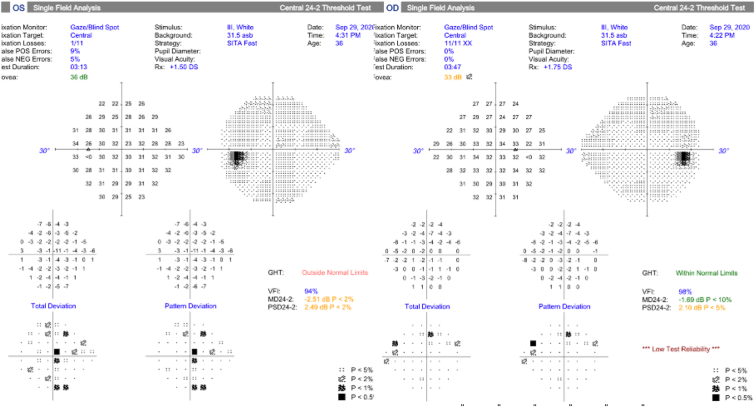
Fig. 3.
Humphrey visual field of left eye (on the right) and right eye (on the left) after thiamine treatment. The test is poorly reliable in the left eye. There is a possible paracentral scotoma present in the right eye.
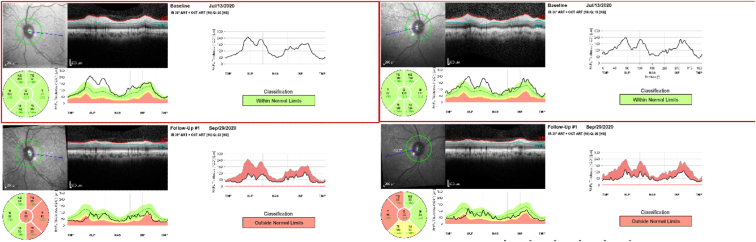
Fig. 2.
OCT nerve of patient at presentation and comparison at follow up. At presentation there is fullness to the nerve but no frank edema, consistent with pseudoedema. After treatment with thiamine there is severe temporal thinning noted on the OCT nerves symmetrically in both eyes which can be seen in metabolic optic neuropathy. Global thickness 136 at presentation to 70 at follow up in the right eye, and 131 at presentation to 66 at follow up in the left eye.
3. Discussion
The diagnosis of WS is made clinically and can be supported either with a low serum thiamine level or with characteristic imaging findings. While CT scan is usually unremarkable in individuals with WS, an MRI can identify typical WS lesions in about two-thirds of individuals with WS. In our patient, an MRI scan was obtained given the concern for optic neuritis and ultimately was consistent with WS. These findings most frequently include T2 and FLAIR hyperintensity with associated diffusion restriction symmetrically in the bilateral medial thalami and surrounding the third ventricle. Additional MRI changes are commonly seen in the periaqueductal region, mammillary bodies, and in the tectal plate.5 Interestingly, these more characteristic MRI changes involving thalamic and mamillary body contrast enhancement are more commonly seen in WS induced by chronic alcoholism, as opposed to the more atypical imaging findings seen more often in non-alcohol induced WS including cranial nerve nuclei involvement, as was described in one retrospective WS imaging study that involved 56 patients.5
Wernicke's Syndrome has been well documented in patient's after gastric bypass and other bariatric surgeries leading to rapid weight loss. Thiamine deficiency is also seen in patients during intensive care unit stays and when critically ill due to hypermetabolism and increased thiamine demand.8 However there are no published reports discussing Wernicke's syndrome after recovery from COVID-19. Early during the pandemic there were contradictory opinions on pausing tube feeds while in the proned position. Currently, it is recommended to continue feeds while proned as long as can be tolerated by the patient. We suspect as more patients recover from COVID-19, we are likely to encounter complications from prolonged hospital stays, repeated proning, post-viral syndromes and poor nutrition. Ensuring proper nutrition during inpatient stays not only allows the patient proper nutrients to heal but also decreases longer term complications such as those seen in our patient.
The cause of our patient's vision loss was thought to be cortical in nature given overall normal ocular exam on presentation. The pupillary exam was muddled due to patient's recent pharmacological dilation at outside optometrist prior to arrival in the Emergency Department. On funduscopic exam were no signs of retinal or optic nerve pathology on exam. This is unlike previous reports of vision loss in Wernicke's encephalopathy caused by chronic alcoholism, which commonly describe optic nerve edema and retinal hemorrhages. A similar presentation as to the one described in this report was described by Desai et al. after gastric bypass surgery9. Their patient presented with mainly visual complaints and the conclusion from their case report was that the vision loss in their patient, who had normal pupil and fundoscopic exam, was due to post chiasm or cortical changes from thiamine deficiency. The OCT and the visual field testing do note optic nerve thinning and persistent paracentral scotomas which correlates with a retro-orbital process.
This case report represents poor nutritional intake and vomiting secondary to COVID-19 resulting in Wernicke's Syndrome and blindness.
4. Conclusion
We report an interesting case of acute-subacute onset bilateral vision loss in the setting of a recent COVID-19 infection that reversed rapidly and nearly completely with rapid administration of high dose IV thiamine 500 mg supplementation. Thus it is our recommendation that any individual who presents with acute-subacute onset vision loss, particularly when the history is suggestive of potential nutritional deficiency including but not limited to infection, critical illness, drug or alcohol use, or recent weight loss be evaluated for thiamine deficiency and be appropriately treated.
The following sections should appear just above the Reference section:
Patient consent
Consent to publish this case report has been obtained from the patient in writing.
Funding
No funding was required.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
No authors has any conflicts of interest.
Acknowledgements
None.
Contributor Information
Emily Shepherd, Email: Emily_a_shepherd@rush.edu.
David Smyth, Email: david_l_smyth@rush.edu.
Andrea Sterenstein, Email: Andrea_E_Sterenstein@rush.edu.
References
- 1.Sinha S., Kataria A., Kolla B.P., Thusius N., Loukianova L.L. Wernicke encephalopathy—clinical pearls. Mayo Clin Proc. 2019;94(6):1065–1072. doi: 10.1016/j.mayocp.2019.02.018. https://search.datacite.org/works/10.1016/j.mayocp.2019.02.018 [DOI] [PubMed] [Google Scholar]
- 2.De Wardener H.E., long mb, durh bl. Cerebral beriberi (wernicke's encephalopathy): review of 52 cases in a Singapore prisoner-of-war hospital. Lancet. 1947;249(6436):11–17. doi: 10.1016/S0140-6736(47)91272-5. http://www.sciencedirect.com/science/article/pii/S0140673647912725 [DOI] [PubMed] [Google Scholar]
- 3.Li J., Rucker J.C. Irreversible optic neuropathy in wernicke encephalopathy and leber hereditary optic neuropathy. J Neuro Ophthalmol. 2010;30(1):49–53. doi: 10.1097/WNO.0b013e3181ce80c6. [DOI] [PubMed] [Google Scholar]
- 4.Gratton S.M., Lam B.L. Visual loss and optic nerve head swelling in thiamine deficiency without prolonged dietary deficiency. Clin Ophthalmol. 2014;8:1021–1024. doi: 10.2147/OPTH.S64228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zuccoli G., Santa Cruz D., Bertolini M., et al. MR imaging findings in 56 patients with wernicke encephalopathy: nonalcoholics may differ from alcoholics. AJNR Am J Neuroradiol. 2009;30(1):171–176. doi: 10.3174/ajnr.A1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.(Eğitim tanrısı) ropper allan H., samuels martin A., joshua klein . McGraw hill education; 2019. Sashank Prasad Adams and Victor's Principles of Neurology. [Google Scholar]
- 7.Surges r, beck s, niesen w, weiller c, rijntjes m. Sudden bilateral blindness in wernicke's encephalopathy: case report and review of the literature. J Neurol Sci. 2007;260(1-2):261–264. doi: 10.1016/j.jns.2007.04.005. https://www-sciencedirect-com.ezproxy.rush.edu/science/article/pii/S0022510X07002742 [DOI] [PubMed] [Google Scholar]
- 8.Whitfield Kyly C., et al. Thiamine deficiency disorders: diagnosis, prevalence, and a roadmap for global control programs. Ann N Y Acad Sci. 2018;1430(1):3. doi: 10.1111/nyas.13919. [DOI] [PMC free article] [PubMed] [Google Scholar]