Abstract
This analysis contrasts traditional not-for-profit academic with new corporate practices of reproductive medicine and offers an assessment of risks to quality of patient care with investors entering the for-profit reproductive medicine market. Large corporate enterprises may have a global impact on access to care while at the same time is putting at risk the training of the next generation of reproductive medicine specialists.
Keywords: Corporate versus traditional not-for-profit academic practices, REI training, Private equity in healthcare, Access to care
Introduction
The treatment of infertility has become big business around the world. A medical specialty that began as an academic, innovative, research activity has now evolved into an industrial and commercial service that has expanded well beyond the treatment of infertility. Treatment options originally aimed at infertile couples are now aggressively marketed to broader population of young fertile individuals. This marketing includes many promises, such as preserving future fertility with oocyte freezing, or having healthy children after relying on various forms of genetic preconception testing, including pre-implantation genetic testing for aneuploidy (PGT-A). A long list of “medical” interventions, referred to as “add-ons” have been introduced over the past decade [1, 2]. Surprisingly, many such interventions have, however, yet to be clinically validated to improve pregnancy chances in the context of current in vitro fertilization (IVF) treatments [2–4]. As a result, practice revenues have been enhanced while patient costs have escalated, further limiting access to care especially in states with no or limited insurance coverage for infertility and IVF services.
How did we get here and where is the field going? Why are increasing amounts of private investment dollars flowing into the IVF world? What will their impact be on the viability of academic reproductive medicine including basic and translational research? Is a rapid increase in treatment demands, as witnessed over recent years for fertile individuals, an ethical practice of reproductive medicine?
The first models for delivering IVF
Louise Brown, the first baby born after in vitro fertilization (IVF), celebrated her 40th birthday on July 25, 2018 [5]. Her birth at the Oldham General Hospital in Manchester (England) made headlines around the world while raising religious, ethical, and legal questions. Her mother, Lesley Brown, had suffered many years of infertility due to blocked fallopian tubes. In November 1977, she agreed to undergo the then experimental procedure of IVF and conceived Louise with the aid of Drs. Patrick Steptoe and Robert Edwards. During a natural cycle, an egg was harvested, fertilized in vitro in a petri dish, and, two days later, a single embryo was transferred into her uterus and resulted in the birth nine months later of Louise Brown. For the development of IVF, Dr. Edwards received the Nobel prize for Physiology and Medicine in 2010. Since then, millions of individuals battling infertility have enjoyed the opportunity of having children through IVF. Today, under the broader umbrella of assisted reproductive technologies (ARTs), IVF is considered mainstream treatment for infertility with over 8 million children born worldwide, and over 2.5 million cycles are being performed every year, resulting in over 500,000 deliveries [6].
The origins of IVF were rooted in the considerable prior research experience using animal models, but grave concerns remained that the technique might produce abnormal offspring. Some objected that the future offspring could not consent to the potential risks. Others noted that there were many children needing adoption making IVF unnecessary. Yet others worried that “manufacturing” human life outside the female body would break the natural bond between procreation and family. Research to advance IVF, involving creation as well as potential loss of embryos, was seen by many as inherently immoral. Because IVF was so ethically controversial, many governments decided to withhold public support and much-needed funding for research. Clinical IVF practice, therefore, quickly moved into private settings where new therapies were often introduced without proper validation. Within a few years, in the absence of insurance coverage (in the USA, to this day, insurance coverage for infertility treatments is still inconsistent), IVF largely became a fee-for-service paid by patients directly.
By now, IVF and the whole practice of ARTs have become thriving commercial businesses. In the process, the early fee for service model for infertility treatments has evolved toward highly integrated multicenter corporate businesses, driven by profits and not academic pursuits. Interestingly, and as reflection of these market changes, out of 34 REI fellows trained by one of the authors between 1996 and 2021, only 9 (26%) are currently employed in academic practices. The active “industrialization and commoditization of IVF,” defined as transition of IVF from a physician- to an investor-controlled business environment, could ultimately prove to be detrimental for patients and their quality of care [7, 8]. Between 2010 and 2017, the value of private equity deals involving the acquisition of healthcare–related companies (most involving physician practices and hospitals) increased 187% reaching $42.6 billion, while the number of healthcare deals increased by 48% [9].
In this paper, we examine the pros and cons of these developments and reflect on (i) the risks to the quality of patient’s care by investors (non-physicians), understandably interested in good returns on their investments, entering the reproductive medicine market; (ii) the threat that investor-driven corporate medicine poses for the academic base of infertility programs including the training of future generations of reproductive medicine and endocrinology specialists; and (iii) the global impact of corporate reproductive enterprises on access to care.
Background economic data: the US market and the international landscape
As of 2017, 498 clinics in the USA offered infertility services. The overwhelming majority (369, 74%) report outcome data both to the Society for Assisted Reproductive Technology (SART) and Center for Disease Control & Prevention (CDC), while 79 (16%) only report to the CDC. A few (50, 10%) do not report at all and, therefore, are non-compliant with federal law (in 1992, the Fertility Clinic Success Rate and Certification Act mandated data reporting) [https://www.sart.org/globalassets/__sart/infographics/number-of-clinics.png] [10].
According to the CDC’s 2006–2010 National Survey of Family Growth, 12% of American women of reproductive age (about 7 million women), or husbands/partners, had sought fertility treatment in their lifetimes. The fertility industry is growing. It proved resilient even during the Great Recession [11] and more recently during the COVID pandemic. Currently, the majority of IVF clinics are private, either owned by an individual or group of physicians or owned by private equity groups and often co-managed by physicians that have sold their practices to the investors (equity groups). Only a small minority of data-reporting clinics (< 15%) are currently within academic centers [12].
According to an international survey of the health economics of IVF, the global need for ART is estimated to be at least 1,500 cycles/million population per year [13]. The average cost of an IVF cycle in U.S. is $12,000 [14]. In addition, patients must pay for medications, adding approximately $3,000–$4,000 per cycle to the IVF costs. Very often, one treatment cycle is not successful, leading to the need for additional cycles. Each successive cycle accrues cumulative costs that can quickly run into tens of thousands of dollars and the success rate, even after three cycles, is still not 100%. Egg donation and gestational surrogacy costs are even more expensive, averaging between $22,000 and 30,000 for an egg donation cycle and between $80,000 and $100,000 for gestational surrogacy [15].
Insurance coverage in the USA remains spotty. Seventeen states—Arkansas, California, Connecticut, Delaware, Hawaii, Illinois, Louisiana, Maryland, Massachusetts, Montana, New Hampshire, New Jersey, New York, Ohio, Rhode Island, Texas, and West Virginia— have passed laws that mandate insurance to either cover (15 states) or offer some coverage (California and Texas) for infertility diagnoses and treatments. In some of these states however, the treatment of infertility stops before offering IVF and the burden of out-of-pocket payments for infertility treatment remains. According to research by Marketdata Enterprises, about 75% of potential clients are not using infertility services because of costs [16]. The same research found that “women who use infertility services are more likely to be Caucasian, college educated, older than 30 and have higher incomes” [16]. Some corporations (Google, Facebook, Apple) have started to offer fertility services as special recruitment incentives to retain “high-powered” female employees. A new, highly specialized insurance industry has also evolved, offering corporations tightly managed infertility services outside the usual health insurance packages that corporations purchase for their employees.
Fertility centers usually offer most, if not all, of their services and procedures including many laboratory tests on site. They can also sell company-branded products and supplements to patients; they can offer new services as soon as they become available and refer to in-house specialists rather than referring outside the company framework (e.g., andrologists, urologists, genetic counselors, social workers, acupuncturists, massage therapists), all of which serve as additional revenue streams for the corporation. Moreover, many so-called add-ons to IVF, often introduced into routine IVF practice, are offered to patients as adjuncts to standard ART treatments [1–4] despite a lack of proper validation. Some of these include pre-implantation genetic testing for aneuploidy screening (PGT-A), time-lapse embryo imaging, endometrial scratching; assisted hatching, freeze-only cycles, the “embryo glue,” and the endometrial receptivity assays. From a socio-economic standpoint, the IVF market is growing thanks also to an increase in the age of first-time mothers and to an increase in women having difficulty in finding partners [17].
So how did investors and private equity investment firms become interested in the IVF market? The main obvious answer is that IVF has become a thriving business with considerable growth potential. In 1992, according to the Biomedical Business International newsletter, infertility care in US was a $2 billion per year business; today, it is about 8-billion-a year business in gross revenues. According to Technavio’s latest report, globally the fertility services market was expected to have exceeded US$ 20 billion by 2021, growing at a compound annual growth rate (CAGR) of almost 9% [18]. Globally, the industry is estimated to be worth $25 billion and is predicted to grow to $41 billion by 2026 [19]. A detailed predictive analysis of the international markets [18] shows the following:
Europe Middle East and Africa: EMEA countries will boost growth and the fertility services were expected to have reached USD 8.9 billion by 2021, with a compounded annual growth rate of over 8%. In this market region, the UK, France, Germany, Italy, and Spain are the major contributors though birth rates are declining, and currently, most of the countries in the region have fertility rates of less than 1.5 children per woman. Many governments and non-governmental organizations are trying to educate the population in the region about fertility and associated treatment options through commercial and professional media. In 2012, the number of ART procedures conducted in Europe amounted to twice that in the USA. Countries such as Belgium, Israel, and the Czech Republic are fertility tourism hotspots due to favorable reimbursement scenarios and the availability of advanced medical techniques. The government of Israel subsidizes IVF costs until a family unit has three children. The country, therefore, has the highest utilization rate for IVF services in the world.
Central and South Americas: The fertility services market in the Americas were expected to have generated revenue of US$ 6.6 billion by 2021, growing at a compounded rate of over 8%. Due to the expense of ART procedures in this region, many people cannot afford fertility treatments. Availability of egg donors is limited, and gestational surrogacy is commercially not available. Unavailability and expense of services drive many people to seek medical treatments in other countries [20]. Latin America has a high fertility rate. However, still by many considered morally and religiously unacceptable, fertility treatments are not as popular as in other regions of the world. In addition, as governments and insurance companies in the region do not offer coverage for these services, only wealthy people can afford fertility treatments or medical tourism.
Asia Pacific regions: The fertility services market in these areas were expected to have exceeded US$ 5.3 billion by 2021, growing at a compounded rate of over 9% per year. Because this market includes China, after removing of the one-child-policy, it is expected to grow at a rapid pace. Many countries in the region are improving their healthcare infrastructure and adopting sophisticated technologies, while also employing increasingly skilled medical professionals to keep up with their Western counterparts. Many Asian countries such as Thailand, Hong Kong, and India are major hotspots for fertility tourism. These countries offer services at much lower cost in comparison to developed countries. Regulations pertaining to infertility treatments are also less stringent in these countries. Australia’s fertility industry, alone, is projected to generate revenues of A$630 million by 2022.
The rise of the IVF Industry
Provision of infertility and especially IVF treatments are increasingly viewed as an industry. Facilitated by the accelerating development of the ART’s, strategic cooperative ventures between private and, recently, even some academic institutions with investors are becoming more frequent. Investors (private equity, venture capital, and other financing sources) and several already existing physician groups striving for further national expansion have been racing towards establishment of large national chains of fertility clinics [21]. The same economic forces driving consolidation in other medical specialties (dermatology, dentistry, orthopedics, radiology) and in other industries (airline, internet and media) are now shaping the future of the infertility field [7, 9, 21, 22].
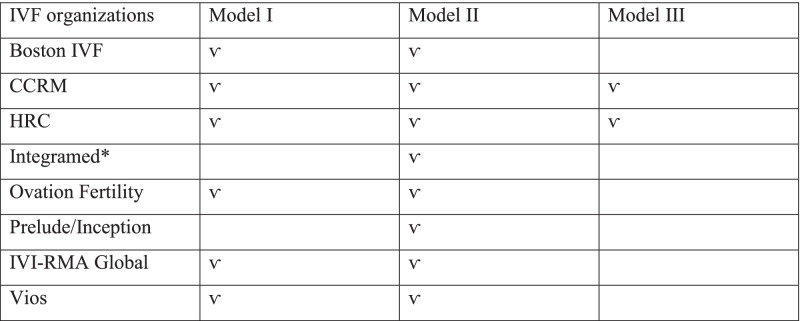
In the following section, we present the currently leading efforts in consolidating the IVF field of some US companies, understanding that the pace of change in the ART field continues to be a moving target with respect to recent exit/entry transitions. They in principle follow three types of business models (see Table 1): (a) progressive practice growth and expansions owned by physicians (type I model); (b) private investment firms entering the IVF market through acquisition of existing IVF practices and merging them into networks (type II model) with physicians remaining employed and becoming shareholders after their “cash out”; and (c) establishment of new independent IVF clinics, fully financed by investors hiring reproductive endocrinologists to run them profitably under a variety of incentive programs (type III model).
Table 1.
List of leading IVF organizations according to the three business models
CCRM Colorado Center Reproductive Medicine, HRC Huntington Reproductive Center, IVI-RMA Instituto Valenciano Infertilidad-Reproductive Medicine Associates. *Filed for bankruptcy in 2020
Boston IV
Initially a type I model, it since turned into a type II model, comprising of clinics mostly in the Northeast (Massachusetts, Maine, Vermont, New Hampshire, and Rhode Island but also in upstate NY, Arizona and Alabama). In 2019, Boston IVF was acquired by the NMC Eugin group and became a type II business model, with senior physicians of Boston IVF becoming shareholders in the NMC Eugin US corporation. Eugin group was a company founded by a wealthy Indian billionaire residing in Dubai, who had been consolidating infertility clinics across Europe before entering the US market. Since its inauguration in Barcelona in 1999, the group has treated thousands of patients worldwide. By 2019, Eugin reached about 36,000 treatment cycles, placing them as a European leader within the sector, with a team comprising over 1,000 specialists. In 2020, the NMC Eugin group was sold for €430 million to a German company, Fresenius Helios, one of the largest in-hospital and ambulatory services operators in Europe with properties in Germany, Spain, and Latin America. At the time of the sale, the Eugin group’s network comprised 31 IVF clinics and 34 additional sites across 9 countries in 3 continents (Fresenius.com, accessed December 30, 2020).
CCRM
The Colorado Center for Reproductive Medicine (CCRM), founded in 1987, has gone from a type I to type II and III business model. Originally owned by a physician founder (type I model), after receiving private investment funds (type II), it further expanded into 10 new markets around the US (type III model). The CCRM received investments from TA (a private equity firm) and opened new IVF clinics in Atlanta, New York, Boston, San Francisco, Dallas, Houston, Minneapolis, Orange County (CA), Northern Virginia, and Maryland and also opened a clinic in Toronto, Canada. In June 2021, the Unified Women’s Healthcare, a practice management platform in women’s healthcare backed by Atlas Partners, with funds managed by the Private Equity Group of Ares Management Corporation and Oak HC/FT, announced that it had entered into an agreement to partner with CCRM. As part of the transaction, the CCRM founder was to remain Medical Director. In addition, TA Associates, which were the strategic investor in CCRM since 2015, sold its stake in the company [23].
Huntington Reproductive Centers (HRC) (type I and II models)
Huntington Reproductive Centers opened the first practice in 1988 and now has nine offices throughout the California Southland (Encino, Fullerton, Laguna Hills, Newport Beach, Oceanside, Pasadena, Rancho Cucamonga, Westlake Village, and West Los Angeles). In 2018, a Chinese investment company, Jinxin Fertility, acquired HRC. The new round of financing was led by Warburg Pincus and CNCB (Hong Kong) Investment Limited [24]. The press release of the acquisition [Oct. 10, 2018 /PRNewswire/Hong Kong] read “With a potential market size of more than RMB100 billion (about 11.5 billion US$), assisted reproduction has become one of the fastest growing markets among the healthcare industry in China.” This promising prospect has attracted a flood of capital. Among interested parties, the Sichuan Jinxin Fertility Company Limited (Jinxin Fertility), which recently announced the completion of a major financing round. In 2016, the National Health and Family Planning Commission of the government reported that “China's licensed assisted reproductive institutions had completed 700,000 assisted reproductive operations annually, while the number of infertile patients was over 40 million, indicating the severe inadequacy of supply.”
Chinese investors have many legitimate business reasons to be interested in American fertility clinics. In the years before COVID-19 pandemic, large numbers of wealthy Chinese flocked to American clinics, which are seen as among the best in the world. With the acquisition of the US-based HRC Fertility, which has had 30 years of history in the USA, Jinxin Fertility expanded their international market.
IntegraMed Fertility (type II model)
IntegraMed Fertility was a division of IntegraMed America, one of the largest networks of providers offering fertility services with 39 centers in 153 locations across 39 States. It also included Shady Grove Fertility centers (type I and II models). IntegraMed America was a privately held company of the Sagard capital group, and it was the first so-called physician management company in the IVF arena, starting management of IVF clinics in 1990. As one of the largest and most sophisticated chains of infertility clinics in the USA, Shady Grove Fertility Centers were IntegraMed’s largest client until the company filed for bankruptcy in early May 2020 after most US IVF clinics had shut down for several months. Many IVF clinics under management by IntegraMed found themselves in difficult circumstances when their management company shut down [19, 25].
Shady Grove
The Shady Grove (type I and II models) enterprise is now one of the largest chains of fertility clinics in the country, present in 8 states, acquiring or opening de novo a number of clinics in District of Columbia, Georgia, Pennsylvania, Virginia, Florida, New York, Colorado, and Connecticut. They also have a presence in Santiago, Chile. The plans to open center in China in 2020 had to be put on hold. Shady Grove first attracted attention when one of its founders in 1992 started promoting a then highly controversial Shared Risk Program, which offered refunds to selected, good prognosis, patients who paid upfront double the IVF treatment price, but then get refunded their money if all the treatments allowed were unsuccessful. As a model, this program became the forerunner to multiple cycle packages, nowadays a marketing tool at many IVF clinics. After the departure of IntegraMed, Shady Grove has remained in a close relationship with a smaller chain of fertility centers in Chicago, IL, The Fertility Centers of Illinois (FCI), which also used to be managed by IntegraMed.
Ovation Fertility (type I and II models)
Ovation Fertility was created with money from a group of physicians from four REI/IVF practices. The group then hired a CEO and a CFO and raised money from MTS Health Investors, later renamed WindRose, an NY private equity firm, to further expand. The Ovation Fertility chain expanded their initial 4 clinics (from Southern California, Nevada, Tennessee, and Texas) to additional ones in Louisiana, Ohio, Indiana, and Washington DC. Recently, they entered in a partnership with the Penn Fertility Center at the University of Pennsylvania, IVF centers at the University of Alabama, and the University of Kansas to run their IVF/Andrology laboratories. Ovation Fertility differs in their operations from other players in the field in that both physicians and embryologists share in the ownership of the company, and, in principle, it only acquires and operates IVF and andrology laboratories. Selling physicians maintain 100% ownership of their clinical practices and 49% of their IVF laboratories. This structure facilitates alignment of incentives and ownership to the founders of the IVF practices. In addition, Ovation Fertility, like Inception (see below), has opened up a series of ancillary service chains as free-standing companies including ovation genetics, the Center for Surrogate Parenting, and ovation donor services (for both fresh and frozen donor egg services).
Prelude and Inception (type II model)
Supported by US$200 million from Lee Equity Partners, the serial entrepreneur M. Varsavsky established Prelude [26]. He first purchased the Reproductive Biology Associates of Atlanta, a large fertility clinic with an egg banking business, then bought Pacific Fertility Centers on the West coast and, recently, 22 clinics of the Vivere group as well as the prestigious IVF program of New York University Langone Medical Center, expanding Prelude’s reach across 23 States. More recently, Prelude merged with Inception, another investor-financed network of fertility brands including Pathways Fertility, My Egg bank, Inspire Rx, Inova, Haven Cryo, a centralized cryo storage company for the Prelude network, and also a multi-cycle fertility service bundling service company called Bundl. In the 2016 Forbes article [26], Varsavsky predicted a future fertility world where young women and men would cryopreserve gametes at peak fertility, thaw them when ready to parent, produce embryos in the laboratory, have them tested through preimplantation genetic testing for aneuploidy, and establish pregnancies through the transfer of only “normal” embryos. He predicted that companies like his Prelude, therefore, would have clients for many decades.
Reproductive Medicine Associates (RMA) (type I and II models)
RMA was founded by physicians in NJ and franchised the RMA brand mostly along the Northeastern corridor (New York, Connecticut, Pennsylvania) as well Florida and Texas. In Feb 2017, by becoming a minority partner, RMA sold out in a merger with the Instituto Valenciano Infertilidad (IVI) creating a global brand mostly on both sides of the Atlantic, the IVI-RMA [27]. IVI was founded in Valencia, Spain, in 1990 and owns many clinics in various regions of Spain and many other countries including Portugal, Turkey, Italy, Panama, Chile, Brazil, Argentina, and India. In addition, they own subsidiaries in genetic testing, IVF lab consulting, research and development, and stem cell banking. In 2016, IVI owned and operated 60 clinic locations in 11 countries and treated over 60,000 patients. In a translated press release, IVI reported that they own 70% of the new company, while RMA of New Jersey owns 30%. The company apparently has 2,400 employees, including 200 physicians and 300 research scientists across 70 clinics in 13 countries [27]. The 5-year plan of IVI-RMA global is to expand in the USA by opening additional sites.
Whether this plan can be executed remains to be seen since the founder of RMA, who after the merger of both companies served as CEO of the enterprise, has left the company.
Vios Fertility Institute (type I and II models)
Vios was founded by a physician formerly part of the previously mentioned Chicago-based chain of IVF clinics, Fertility Center of Illinois (FCI). This company has branched out to acquire existing IVF clinics and to open new ones in Chicago and St. Louis by now having a presence in 6 states.
Potential impact of mergers and acquisitions: a look at the cons and pros
Potential negative impacts (CONS)
The mergers and acquisitions of clinical practices will undoubtedly create competitive market advantages and pose new financial challenges to smaller, independent private practices and to not-for-profit academic centers. If they are unable to survive, practices may be forced to close or swallowed up, fostering a rise in regional monopolies, resulting in higher prices for services thereby decreasing both access to and the diversity of medical care available to patients. A good example for such a development has been Australia and New Zealand, where three mega network companies control two-thirds of the region’s IVF cycles [28]. Both of these countries have done pioneering work in the early days of IVF and have, for a number of years, maintained academic excellence in research. Yet, live births have been declining in strong correlation with increasing monopolization of IVF and with, in parallel, declining patient satisfaction, while costs have been increasing [22, 28].
Low offerings of affordable treatment options. Large chains are expected to respond to investors, understandably, seeking returns on their investments. Profits, and not patients, emerge as a principal priority, often pushing aside in importance cycle outcomes and patient satisfaction. Industrialization inevitably leads to commoditization, incentivizing physicians to spend less time with patients, encouraging higher cost and more treatments, even when less expensive and less invasive options are also acceptable.
Employee health and job security in networks vs. independent clinics could become suboptimal. Young physicians, embryologists, nurses, etc., may have less bargaining power with corporations as they may be seen as commodity other than assets. Ownership and sense of community has disappeared from many corporate-owned fertility centers, having been replaced by profit/metrics-driven evaluation. Long-term career growth of employees is often viewed as low priority in these corporate entities.
In reproductive medicine, it is difficult to export success rates across multiple facilities (franchisee) since patients are diverse and team behaviors and practices vary widely. One, therefore, can foresee that, in attempts to streamlines services, large provider networks will select out better prognosis and avoid poorer prognosis patients, unless they can be directed towards third party egg donation cycles, which represent the most profitable IVF treatment in fertility centers, but will jeopardize comprehensive patient care.
Commercial interests may blur diagnostic needs and accuracy by offering non-validated tests called “adds on” which are unproven and costly. Some examples include the “embryo glue”; fertilome analysis; time-lapse imaging; routine freezing of all embryos and not doing fresh transfers; assisted hatching; and PGT/A for all [1–3]. US clinics, for example, offer PGT-A more frequently than the UK [29], and Australian IVF centers face a class action suit as a result of PGT-A [30]. Interestingly, already in 2017, based on CDC data, 6% of private clinics (22/375) used PGT in more than 30% of the IVF cycles, while only 0.5% (2/47) of academic centers did so [31].
Investors are also driven to enlarge markets. An example is the intense marketing campaign towards very young women about freezing eggs for elective reasons (Kindbody strategy), despite the fact that a number of studies have now demonstrated the low utilization rate and thus the unnecessary expenses that these young women incur to cryopreserve eggs and maintain them in storage [32–34].
Concentrating the care of the infertile in the hands of business entities provides different market leverages (buying disposables in bulk, medications in bulk), creating competitive advantages for these multi groups over non-merged, stand-alone clinics and academic programs.
Better suited to offer certain price discounts (IVF packages), payment plans, and offering free marketing to practices of referring physicians. Partial acquisition of referring physician practices will pose increased competition to the academic programs and to stand-alone clinics.
Fewer academic training programs—academic centers cannot compete, and if they do not adapt to these new business models, they will likely be on the brink of extinction. Who will train the next generation of reproductive endocrinologist and infertility practitioners? The establishment of a proper REI fellowship still requires an academic institution to request the fellowship as regulated by the American College for Graduate Medical Education (ACGME). At present, except for few of these private enterprises that are connected with academic institutions, the majority do not have fellows rotating through their private clinics.
The breadth and width of women’s health related to reproductive endocrinology, metabolic and hormonal disorders, would be marginalized.
Potential for rapid commercial expansion of services not yet scientifically and ethically validated (germline editing for disease repair, disease prevention, cosmetic genetics).
More direct to consumer (DTC) marketing.
Lobbying to keep insurance from covering infertility services so that it remains a treatment for rich and the middle class or lobbying insurance to cover infertility services with preferential contracts since they will “own” the majority of patients, putting academic centers out of business.
Potential to move patients or reproductive materials across national borders.
Making it harder for individual patients to sue deep pocket owners.
Elimination of inner city and rural service locations following the money to the right zip codes and neighborhoods and nations.
Merger of infertility services with other big health care corporations—investors selling to even bigger firms (e.g., Eugin sold the practice to Fresenius Health a mega health German company).
Potential positive impacts (PROS)
The inflow of investor capital has unquestionably accelerated the commercial development of IVF practice, especially facilitating an unprecedented expansion in numbers of IVF clinics, and thereby improving access to care.
Expanded marketing efforts provide more information to the public and, in the process, are likely to help in destigmatizing infertility.
At least theoretically (but still to be seen in practice), increased availability of services should lead to lower prices for treatment. These chains will have better leverage on buying products (bulk shopping), disposables, renting spaces, and overall lower overhead compared to academic centers. These costs reduction opportunities could be passed on to patients or payers.
In principle, these mega capital-strong industries could have more political power to lend their voice to support causes demanding insurance coverage for infertility services and convince legislators to enact bills.
Theoretically, larger provider organizations also have better opportunities to conduct investigations to improve care. If they engage in research, it should be easier to carry out large randomized controlled clinical trials. Hypothesis testing with specimen archiving and appropriate data mining efforts should facilitate development of new products, protocols, and/or devices, faster than that of traditional small academic centers, while by-passing restrictions imposed by federal agencies. However, such an expectation awaits confirmation in practice because whether investors have enough long-term interests to direct capital towards research and development (R&D) is not certain.
Suggested responses
The American Board of Obstetrics and Gynecology (ABOG), the American Society of Reproductive Medicine (ASRM) with the help of the Society of Reproductive Endocrinology and Infertility (SREI), and the American College for Graduate Medical Education (ACGME) must cooperate for the future of REI training and credentialing.
Private enterprises and academic centers could form hybrid alliances to support REI training programs. Within such a hybrid framework, REI fellows would benefit from the opportunity to gain access to diverse models of leadership, business models, and large volumes of clinical care while still being assured time for academic scholarship and research projects.
ASRM ought to set marketing and advertising standards to control creation of demand for marginal services. Patient groups need to build websites with reliable, independent information about fertility treatment options, and costs.
Conclusions
In sum, the offering of infertility services is rapidly evolving into large commercial entities threatening patient care and the future of teaching and research in reproductive medicine. Private enterprises with increasingly aggressive sales techniques are fueling growth in this for-profit medical field; however, market values may not be the appropriate basis for creating families. More public fertility clinics and more insurance mandated coverage for fertility services might change the landscape. Such efforts might give women access to evidence-based treatments without running up huge bills and be less likely to be driven by the need to pay dividends to shareholders or return profits on private equity firms. Concurrently, academic centers need to be fully aware of these rapidly changing market dynamics and prepare plans for survival and for continuing teaching and training new generations of reproductive endocrinologist and infertility specialists.
Declarations
Conflict of interest
DFA receives stipend from Springer Nature Publishing. NG is the owner of a private fertility center. The other authors declare no conflicts.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
1/27/2022
A Correction to this paper has been published: 10.1007/s10815-022-02416-0
References
- 1.Harper J, Jackson E, Sermon K, Aitken RJ, Harbottle S, et al. Adjuncts in the IVF laboratory: where is the evidence for “add on” interventions? Hum Reprod. 2017;32(3):485–491. doi: 10.1093/humrep/dex004. [DOI] [PubMed] [Google Scholar]
- 2.Wilkinson J, Malpas P, Hammarberg K, Tsigdinos PM, Lensen S, Jackson E, Mol Harper J, BW. Do a’ la carte menus serve infertility patients? The ethics and regulation on in vitro fertility add-ons. Fertil Steril. 2019;112(6):973–77. doi: 10.1016/j.fertnstert.2019.09.028. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong S, Atkinson M, MacKenzie J, Pacey A, Farquhar C. Adds-on in the laboratory: hopeful but not always helpful. Fertil Steril. 2019;112:994–999. doi: 10.1016/j.fertnstert.2019.10.031. [DOI] [PubMed] [Google Scholar]
- 4.Macklon NS, Ahuja KK, Fauser BCJM. Building an evidence base for IVF “adds-on”. RBMO. 2019;38(6):853–6. doi: 10.1016/j.rbmo.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Steptoe PC, Edwards RG. Birth after the reimplantation of a human embryo. Lancet. 1978;2(8085):366. doi: 10.1016/S0140-6736(78)92957-4. [DOI] [PubMed] [Google Scholar]
- 6.Fauser BCJM. Towards the global coverage of a unified registry of IVF outcomes. RBMO. 2019;32(2):133–7. doi: 10.1016/j.rbmo.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Resneck JS. Dermatology practice consolidations fueled by private equity investments: potential consequences for the specialty and patients. JAMA Dermatol. 2018;154(1):13–4. doi: 10.1001/jamadermatol.2017.5558. [DOI] [PubMed] [Google Scholar]
- 8.Gleicher N, Kushnir V, Barad D. Worldwide decline of IVF birth rates and its probable causes. Hum Reprod Open. 2019;3:1–7. doi: 10.1093/hropen/hoz017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gondi S, Song Z. Potential implications of private equity investments in health care delivery. JAMA. 2019;321(11):1947–8. doi: 10.1001/jama.2019.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.https://www.sart.org/globalassets/_sart/infographics/number-of-clinics.png (accessed 9/1/2021).
- 11.www.SmartAsset.com, “The Economics of Fertility”, by Amelia Josephson, published Feb 2,2017, accessed Dec.26,2017).
- 12.www.CDC.gov >reproductivehealth, accessed 12/10/2021.
- 13.Collins JA. An international survey of the health economics of IVF and ICSI. Human Repro Update. 2002;8(3):266–277. doi: 10.1093/humupd/8.3.265. [DOI] [PubMed] [Google Scholar]
- 14.ASRM Disparities in access to effective treatment for infertility in the United States: an ethics committee opinion. Fertil Steril. 2021;116(1):54–61. doi: 10.1016/j.fertnstert.2021.02.019. [DOI] [PubMed] [Google Scholar]
- 15.Covington SN, Patrizio P. Gestational carriers and surrogacy. In: Sauer M, editor. Principle of oocyte and embryo donation. London: Springer Verlag; 2013. pp. 277–88. [Google Scholar]
- 16.https://www.marketresearch.com/Marketdata-Enterprises-Inc-v416/Fertility-Clinics-Infertility-Services-13236074/ accessed 10/1/2019.
- 17.Inhorn MC, Birenbaum-Carmeli D, Westphal LM, Doyle J, Gleicher N, Meirow D, Dirnfeld M, Seidman D, Kahane A, Patrizio P. Ten Pathways to Elective Egg Freezing and its underlying socio-demography: a binational analysis. J Asst Reprod Gen. 2018;35(8):1277–1283. doi: 10.1186/s12958-018-0389-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Technavio report Global IVF business (www. Businesswire.com April 2016, accessed Jan.26, 2018).
- 19.www.nbcnews.com/think/opinion/fertility-clinics-are-being-taken-over-profit-companies-selling-false-ncna1145671 (accessed10/2/2020).
- 20.De Mouzon J, Chambers GM, Zegers-Hochschild F, Mansour R, Ishihara O, Banker M, Dyer S, Kupka M, Adamson DG. International committee for monitoring assisted reproductive technologies world report: assisted reproductive technology 2012. Hum Reprod. 2020;35(8):1900–1913. doi: 10.1093/humrep/deaa090. [DOI] [PubMed] [Google Scholar]
- 21.Stern M. Healthcare- Fertility sector. In “Staying ahead of the curve” A Dresner Partners Newsletter, pages 1–8, published May 2021.
- 22.Gleicher N, Kushnir VA, Barad DH. Worldwide decline of IVF birth rates and its probable causes. Hum Reprod Open. 2019;1–7. [DOI] [PMC free article] [PubMed]
- 23.www.businesswire.com/news/home/20210618005302/en/Unified-Women’s-Healthcare-and-CCRM-Fertility-Establish-Strategic-Partnership (accessed 8/1/2021).
- 24.https://markets.businessinsider.com › News › Stock News- Warburg Pincus and CNCB (Hong Kong) Investment Limited (accessed July 28,2019).
- 25.Li, Mitchell MD (2021, July 17), Private equity is ruining American healthcare, MedpageToday, www.medpagetoday.com/opinion/second-opinions/93615.
- 26.Forbes Magazine, November 8, 2016, page 84.
- 27.IVI Press release. IVI arrives in America hand-in-hand with RMANJ and consolidates as the largest group of assisted reproduction in the world. February 16, 2017 wwwivi-fertility. com (accessed Dec. 19, 2017).
- 28.Blakely B, Williams J, Mayes C, Kerridge I, Lipworth W. Conflicts of interest in Australia’s IVF industry: an empirical analysis and call for action. Hum Fertil. 2017;22(4):230–237. doi: 10.1080/14647273.2017.1390266. [DOI] [PubMed] [Google Scholar]
- 29.Theobald R, SenGupta S, Harper J. The status of preimplantation genetic testing in the UK and USA. Hum Reprod. 2020;35(4):986–998. doi: 10.1093/humrep/deaa034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cunningham M. Class action lodged against Monash IVF over allegedly bungled screening. The Sydney Morning Herald; 2020.
- 31.https://www.cdc.gov › reproductivehealth (2017) Accessed (12/02/2021).
- 32.Barbey C. Evidence of biased advertising in the case of social egg freezing. New Bioethics. 2017;23(3):195–209. doi: 10.1080/20502877.2017.1396033. [DOI] [PubMed] [Google Scholar]
- 33.Hammarberg K, Kirkman M, Pritchard N, Hickey M, Peate M, McBain J, Agresta F, Bayly C, Fisher J. Reproductive experience of women who cryopreserved oocytes for non-medical reasons. Hum Reprod. 2017;32(3):575–5. doi: 10.1093/humrep/dew342. [DOI] [PubMed] [Google Scholar]
- 34.Ben RZ. The dilemma of social oocyte freezing: usage rate is too low to make it cost-effective. RBMO. 2018;37(4):443–8. doi: 10.1016/j.rbmo.2018.06.024. [DOI] [PubMed] [Google Scholar]