Abstract
Introduction
The massive spread of COVID-19 affected many aspects of medical and surgical services. Many patients with sacral neuromodulation (SNM) devices needed integrated follow-up and close communication regarding the programming of the device. In this study, we aimed to explore the effect of COVID-19 lockdown on patients with SNM devices.
Materials and Methods
This was a multicenter study designed and conducted in four centers performing SNM (Toronto Western Hospital, Toronto, Canada; King Abdulaziz University Hospital, Jeddah, Saudi Arabia; Al-Amiri Hospital, Kuwait City, Kuwait; and Austin and Western Health, University of Melbourne, Australia). An online questionnaire was created through Google Forms and circulated among patients with SNM devices in all four mentioned centers. The questionnaire was sent to patients during the forced lockdown period in each country.
Results
A total of 162 responses were received by September 2020. Data showed that most patients had their device implanted before the lockdown period (92.5%, 150/162). Most patients did not experience any contact difficulties (91.9%, 149/162). When patients were requested for their preference of programming, 89.5% (145/162) preferred remote programming. Correlation analysis did not show any significant relation between patient diagnosis and COVID-19–related difficulties or preferences.
Conclusion
The difficulties with access to care experienced during the pandemic and the patient’s expressed willingness to participate in virtual care should provide impetus for manufacturers of SNM devices to move forward with developing remote programming capabilities.
Keywords: COVID-19, lockdown, LUTS, sacral neuromodulation
Introduction
The dramatic outbreak of the novel COVID-19 affected many aspects of medical and surgical services. Substantial interruption of high quality of care was encountered in those hospitals that had been converted to dedicated facilities to manage these COVID-19 cases specifically.1 During the current pandemic, more extensive efforts were highly needed to overcome the unique challenges posed to the health care system. Many patients with sacral neuromodulation (SNM) devices needed integrated follow-up and close communication regarding the programming of the device, especially those who had been implanted recently. This study aimed to assess the impact of COVID-19 on patients with SNM devices and to determine their willingness for other alternative programming communication such as a virtual clinic visit. To the best of our knowledge, no studies have been conducted to investigate the effect of COVID-19 and the lockdown on patients with SNM devices.
Materials and Methods
This was a multicenter study designed and conducted in four centers performing SNM (Toronto Western Hospital, Toronto, Canada; King Abdulaziz University Hospital, Jeddah, Saudi Arabia; Al-Amiri Hospital, Kuwait City, Kuwait; and Austin and Western Health, University of Melbourne, Australia). An online questionnaire was created through Google Forms and circulated among patients with SNM devices in all four mentioned centers through their emails or social mobile applications by the clinic secretary. The questionnaire was sent to the patients during the forced lockdown period in each country. Local ethical committee approval was obtained. The survey, which consisted of 11 questions (Appendix 1), was designed by the main authors in English and translated into Arabic language for use in the Gulf region. The questionnaire was open for a period of one month; lockdown details in each country are available in Appendix 2. All data were extracted into Excel (Microsoft, Albuquerque, NM) and then analyzed using the SPSS program, version 19 (IBM Corp, Armonk, NY) for statistical analysis. The association between categorical variables was assessed using Fisher exact test or χ2 test. We considered p < 0.05 as statistically significant.
Results
A total of 162 responses were received by September 2020. More details of respondents’ demographics are in Table 1 . Of the patients who responded, 80 were from Canada, 20 from Kuwait, 33 from Kingdom of Saudi Arabia, and 29 from Australia. Data analysis showed that most patients had their device implanted before the lockdown period (92.5%, 150/162). Those who had COVID-19 constituted 1.5% of the patients (2/133) (status of infection of patients from Australia was not known at the time the questionnaire was collected), with mild to moderate symptoms not requiring intensive care unit admission. A high proportion of patients (74.6%, 121/162) did not experience any complications after implantation. Patients who complain of pain or device malfunction were further assessed for need of reprogramming.
Table 1.
Patient Demographics According to Country.
| Variables | Canada (Toronto Western Hospital, Toronto, Canada) | Kuwait (Al-Amiri Hospital, Kuwait City, Kuwait) | Saudi Arabia (King Abdulaziz University, Jeddah, Saudi Arabia) | Australia (Austin and Western Health, University of Melbourne, Australia) | Total |
|---|---|---|---|---|---|
| Number of responders | 80 | 20 | 33 | 29 | 162 |
| Duration of InterStim | |||||
| • 1–3 mo | 4 (5%) | 2 (10%) | 1 (3%) | 5 (17%) | 12 (7.4%) |
| • >3 mo | 76 (95%) | 18 (90%) | 32 (96.9%) | 24 (82.7%) | 150 (92.5%) |
| Reason for SNM | |||||
| • OAB | 38 (47.5%) | 9 (45%) | 16 (48%) | 21 (72%) | 84 (51%) |
| • Retention | 27 (33.75%) | 9 (45%) | 11 (33%) | 7 (24%) | 54 (33%) |
| • IC | 8 (10%) | 2 (10%) | 5 (15%) | 1 (3%) | 16 (9%) |
| • Fecal incontinence | 5 (6.25%) | 0 (0%) | 1 (3%) | 0 (0%) | 6 (3%) |
| • OAB + fecal incontinence | 2 (2.5%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (1%) |
| Postoperative complication | |||||
| • None | 54 (67.5%) | 16 (80%) | 31 (93%) | 20 (69%) | 121 (74.6%) |
| • Pain | 13 (16.25%) | 3 (15%) | 0 (0%) | 4 (13.7%) | 20 (12.3%) |
| • Malfunction | 7 (8.75%) | 1 (5%) | 2 (6%) | 3 (10%) | 13 (8%) |
| • Bleeding | 1 (1.25%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.6%) |
| • Infection | 5 (6.25%) | 0 (0%) | 0 (0%) | 2 (6.8%) | 7 (4.3%) |
| Use the device easily | |||||
| • All the time | 64 (80%) | 16 (80%) | 23 (70%) | 19 (65%) | 122 (75%) |
| • Most of the time | 15 (18.75%) | 2 (10%) | 10 (30%) | 8 (27%) | 35 (21%) |
| • Sometimes | 1 (1.25%) | 1 (5%) | 0 (0%) | 1 (3.4%) | 3 (1.8%) |
| • No | 0 (0%) | 1 (5%) | 0 (0%) | 1 (3.4%) | 2 (1%) |
| Improvement rate | |||||
| • >80 | 28 (35%) | 14 (70%) | 0 (0%) | 1 (3.4%) | 43 (26%) |
| • <50 | 7 (8.75%) | 1 (5%) | 0 (0%) | 6 (20%) | 14 (8.6%) |
| • 50–80 | 45 (56.25%) | 5 (25%) | 33 (100%) | 22 (75%) | 105 (64%) |
| COVID-19 diagnosis | |||||
| • Positive | 0 (0%) | 0 (0%) | 2 (6%) | NA | 2 (1.23%) |
| • Negative | 80 (100%) | 20 (100%) | 31 (93.9%) | NA | 131 (80%) |
IC, interstitial cystitis; NA, not available; OAB, overactive bladder.
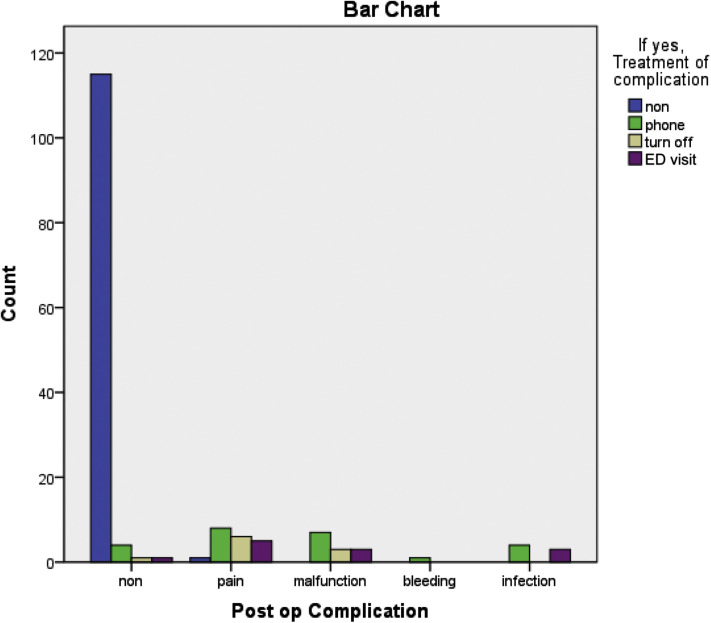
Most patients did not experience any difficulty contacting their surgeon (91.9%, 149/162). When patients were asked for their preferred method of contact if they developed any complications, phone communication was preferred by 24 patients, whereas ten patients chose to turn off the device and wait, and 12 patients preferred an emergency department (ED) visit (Fig. 1 ).
Figure 1.
Postoperative complications encountered by patients and their preferred response. ED, emergency department; non, none; Post-op, postoperative.
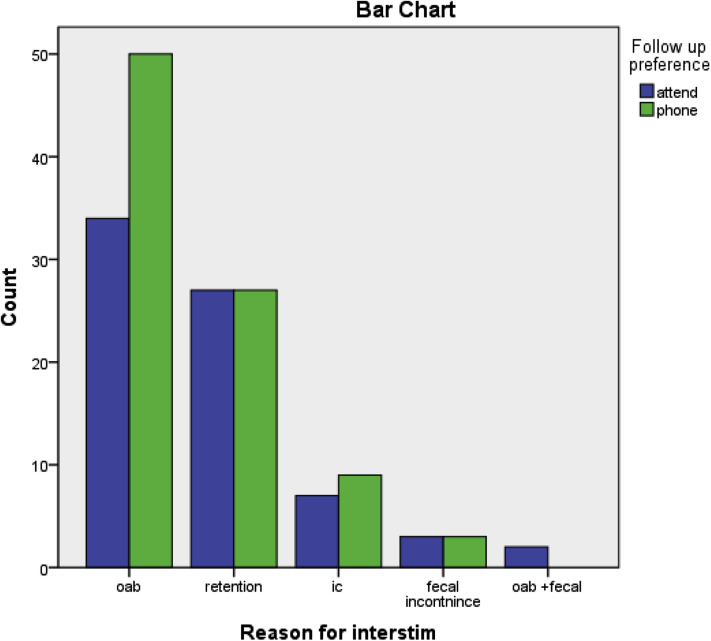
Patient follow-up preferences were as follows: 73 (45%) preferred to attend face-to-face, and 89 (55%) preferred virtual follow-up (Fig. 2 ). The need for changes to programming (putting several new programs into the patient programmer, which requires an in-person visit) was the main issue during COVID-19. When patients were requested for their preference of remote programming, 89.5% (145/162) preferred remote programming. This may be because a high proportion of patients (49%, 80/162) found that lockdown affected their ability to visit their urologist (Table 2 ).
Figure 2.
Patients’ follow-up preference categorized according to their functioning diagnosis (reason for InterStim therapy). IC, interstitial cystitis; OAB, overactive bladder.
Table 2.
Effect of COVID-19 and the Lockdown on Patients With SNM Devices.
| Variables | Canada (Toronto Western Hospital, Toronto, Canada) | Kuwait (Al-Amiri Hospital, Kuwait City, Kuwait) | Saudi Arabia (King Abdulaziz University, Jeddah, Saudi Arabia) | Australia (Austin and Western Health, University of Melbourne, Australia) | Total |
|---|---|---|---|---|---|
| Treatment of complications during lockdown, if developed | |||||
| • None | 49 (61%) | 16 (80%) | 31 (93.9%) | 20 (68.9%) | 116 (71.6%) |
| • Phone | 14 (17.5%) | 2 (10%) | 0 (0%) | 8 (27.5%) | 24 (14.8%) |
| • Turn off | 5 (6.25%) | 2 (10%) | 2 (6%) | 1 (3.44%) | 10 (7%) |
| • ED visit | 12 (15%) | 0 (0%) | 0 (0%) | 0 (0%) | 12 (7%) |
| Contact difficulties during lockdown | |||||
| • Yes | 7 (8.75%) | 0 (0%) | 3 (9%) | 3 (10%) | 13 (8%) |
| • No | 73 (91.25%) | 20 (100%) | 30 (0.9%) | 26 (89.6%) | 149 (91.9%) |
| Follow-up preference | |||||
| • Attend | 44 (55%) | 13 (65%) | 10 (30%) | 6 (20.6%) | 73 (45%) |
| • Phone | 36 (45%) | 7 (35%) | 23 (69.6%) | 23 (79%) | 89 (54.9%) |
| Lockdown affecting visit | |||||
| • Yes | 27 (33.75%) | 8 (40%) | 32 (96.9%) | 13 (44.8%) | 80 (49%) |
| • No | 53 (66.25) | 12 (60%) | 1 (3%) | 16 (55%) | 82 (50.6%) |
| Remote programming | |||||
| • Yes | 71 (88.75%) | 17 (85%) | 28 (84%) | 29 (100%) | 145 (89.5%) |
| • No | 9 (11.25%) | 3 (15%) | 5 (15%) | 0 (0%) | 17 (10%) |
Correlation analysis did not show any significant relation between patient diagnosis and COVID-19–related difficulties or preferences.
Discussion
The COVID-19 crisis altered our health care system, society, and global economy. Because the degree of outbreak and its effect on urological services might vary significantly between different geographical locations, we aimed, in this study, to address this issue by assessing the impact of COVID-19 pandemic on patients with SNM devices in four different geographical areas. Health care centers from Canada, Kingdom of Saudi Arabia, Australia, and Kuwait participated in this study.
On March 11, 2020, the World Health Organization proclaimed COVID-19 as a global pandemic.2 , 3 Several international and local urological guidelines aimed to provide rapid guidance based on the best knowledge available to adapt to the current situation. Recommendations for diagnosis, surgical treatment, and follow-up of urological cases have been revised.4 , 5 In the European Association of Urology guidelines, patients were categorized into low, intermediate, and high priority, based on the potential of clinical harm.5 Most patients with functional urological diseases fell under the low priority category. These guidelines, however, might not have been based on the high quality of evidence in some instances. Several urological cases that were considered as elective cases or under the category of low priority were postponed, with unknown clinical outcome. From the respondents in this study, 74.6% of them did not experience any complication after operation. Fortunately, for those who had complications, 91.9% of them did not face any contact difficulties during the lockdown period.
The pandemic created an immediate need for virtual health care and telemedicine. Medical digital technology has been available for the past 20 years but was not used broadly until the past year, when it reached its peak of application in the health care system.6 For example, virtual clinic visits increased by 20-fold at the start of the lockdown period at the Cleveland Clinic.7 This increase also was seen in health care systems with higher pre–COVID-19 virtual care adoption; one clinic reported seeing <100 patients per day virtually pre–COVID-19 to >600 virtual patients per day during COVID-19.8 In other centers, demand for virtual health care increased from 1% to 70% during the first month of the crisis.8
Virtual care can be defined as “any interaction occurring remotely between patients and/or members of their circle of care, through any form of communication or information technology with the aim of facilitating or maximizing the quality and effectiveness of patient care.”9 , 10 Communication between the patient and their care provider in virtual care can be synchronous (such as video or phone call) or asynchronous (such as secure messaging or secure mails). Adopting virtual care was found to reduce barriers to care and wait times and also result in a significant reduction in cost.11 Most of our patients preferred virtual visit (by phone) when asked about the preferred way of communication if they developed any complication.
Remote reprogramming of implantable devices would be a greater expansion of virtual care for patients with SNM devices. While promoting social distancing, the patient’s data can be delivered to the health care provider in an informative and accurate way. However, remote programming is not yet initiated effectively among patients with SNM devices, in contrast to its successful use in monitoring patients with a cardiac pacemaker/defibrillator.12 Remote monitoring and programming technology is available for implanted cardiac devices but is not yet available for SNM devices. In this study, 89.5% of the respondents showed an interest and desire to be involved in remote programming care. A virtual visit where the patient's device can be interrogated and reprogrammed, if needed, would have been very beneficial during the restricted access of the lockdown period and would be a significant patient and provider satisfier in the post–COVID-19 era as well.
We believe a constructed pathway for virtual consultations would give the patient maximum benefit and better use of physician time. We suggest the virtual consultations would start as phone calls with the clinical fellow or senior resident to filter small, manageable issues, after which the patient would be directed to either further programming (adding new programs) or clinical physical visit.
Conclusion
The difficulties with access to care experienced during the pandemic and the patient’s expressed willingness to participate in virtual care should provide the impetus for manufacturers of SNM devices to move forward with developing remote programming capabilities.
Authorship Statements
Mai Ahmed Banakhar was responsible for the study design, statistical analysis, and data collection. Wadha Al-Qahtani was responsible for writing the manuscript draft. Tariq Faisal Al-Shaiji, Meshari Almutairi, and Johan Gani were responsible for revising the manuscript draft and data collection. Magdy Hassouna was responsible for the study design, ethical approval, revising the manuscript, and data collection. All authors approved the final version of the manuscript.
Footnotes
Source(s) of financial support: The authors reported no funding sources.
Conflict of Interest: Magdy Hassouna and Tariq Al-Shaiji received honorarium for Medtronic-sponsored lectures. The remaining authors reported no conflict of interest.
To access the supplementary material accompanying this article, visit the online version of Neuromodulation: Technology at the Neural Interface at www.neuromodulationjournal.org and at https://doi.org/10.1016/j.neurom.2021.12.001.
Supplementary Data
References
- 1.Teoh J.Y.C., Ong W.L.K., Gonzalez-Padilla D., et al. A global survey on the impact of COVID-19 on urological services. Eur Urol. 2020;78:265–275. doi: 10.1016/j.eururo.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometer. COVID-19 Coronavirus Pandemic. Accessed April 2, 2020. https://www.worldometers.info/coronavirus/
- 3.World Health Organization . World Health Organization; 2020. Coronavirus Disease (COVID-19) Pandemic. [Google Scholar]
- 4.American Urological Association Information Center Coronavirus disease 2019. https://www.auanet.org/covid-19-info-center/covid-19-info-center Accessed October 29, 2020.
- 5.European Association of Urology COVID19 resources for urologists. https://uroweb.org/covid19-resources-for-urologists/ Accessed October 29, 2020.
- 6.Mosnaim G.S., Stempel H., Van Sickle D., Stempel D.A. The adoption and implementation of digital health care in the post–COVID-19 era. J Allergy Clin Immunol Pract. 2020;8:2484–2486. doi: 10.1016/j.jaip.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fonda D. Coronavirus has ushered in the digital revolution in medicine. How investors can play it. https://www.barrons.com/articles/coronavirus-has-ushered-in-the-telehealth-revolution-which-stocks-to-play-it-51587169350?reflink¼article Accessed May 2, 2020.
- 8.Wosik J., Fudim M., Cameron B., et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaw J., Jamieson T., Agarwal P., Griffin B., Wong I., Bhatia R.S. Virtual care policy recommendations for patient-centred primary care: findings of a consensus policy dialogue using a nominal group technique. J Telemed Telecare. 2018;24:608–615. doi: 10.1177/1357633X17730444. [DOI] [PubMed] [Google Scholar]
- 10.Canadian Medical Association . Canadian Medical Association; 2020. Virtual Care Recommendations for Scaling Up Virtual Medical Services. [Google Scholar]
- 11.Appireddy R., Jalini S., Shukla G., Boissé Lomax L. Tackling the burden of neurological diseases in Canada with virtual care during the COVID-19 pandemic and beyond. Can J Neurol Sci. 2020;47:594–597. doi: 10.1017/cjn.2020.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller J.C., Skoll D., Saxon L.A. Home monitoring of cardiac devices in the era of COVID-19. Curr Cardiol Rep. 2020;23:1. doi: 10.1007/s11886-020-01431-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Comments
The COVID-19 pandemic has significantly affected virtually all aspects of medical care, and the field of sacral neuromodulation is no exception. As the authors note, unique issues arise when patients are not able to come in for in-person visits following the implantation of sacral neurostimulator devices, including physical examinations and reprogramming. Remote programming and virtual visits should be made more available to avoid situations such as these, when patients are not able to come to physician offices, whether it is because of a pandemic or other unusual scenarios.
Peter Rosenblatt, MD
Cambridge, MA, USA
∗∗∗
The effects of COVID-19 on medical care has been widely covered in the medical literature.1-6 Patients with sacral neuromodulation devices with functional diseases encountered several difficulties because of the necessity of periodic device programming. This multicenter study highlights the need that is remote programming. Furthermore, it makes evident the attitude of different centers to regularly take care of patients with implants.
Maria Paola Bertapelle, MD
Turin, Italy
References
1. Doná D, Torres Canizales J, Benetti E, et al. Pediatric transplantation in Europe during the COVID-19 pandemic: early impact on activity and healthcare. Clin Transplant. 2020;34:e14063.
2. Gomes CM, Favorito LA, Henriques JVT, et al. Impact of COVID-19 on clinical practice, income, health and lifestyle behavior of Brazilian urologists. Int Braz J Urol. 2020;46:1042–1071.
3. Togun T, Kampmann B, Stoker NG, Lipman M. Anticipating the impact of the COVID-19 pandemic on TB patients and TB control programmes. Ann Clin Microbiol Antimicrob. 2020;19:21.
4. Prayer-Galetti T, Motterle G, Morlacco A, et al. Urological care and COVID-19: looking forward. Front Oncol. 2020;10:1313.
5. Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database analysis. Gut. 2021;70:537–543.
6. Onesti CE, Rugo HS, Generali D, et al. Oncological care organisation during COVID-19 outbreak [Erratum in: ESMO Open. 2020;5:e000682corr1]. ESMO Open. 2020;5:e000853.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.