Abstract
Since the beginning of the COVID-19 pandemic in early 2020, global efforts to respond to and control COVID-19 have varied widely with some countries, including Australia, successfully containing local transmission, and minimising negative impacts to health and economies. Over this time, global awareness of climate variability due to climate change and the risk factors for emerging infectious diseases transmission has increased alongside an understanding of the inextricable relationship between the health of the environment, humans, and animals. Overall, the global response to the current pandemic suggests there is an urgent need for a One Health approach in controlling and preventing future pandemics, through developing integrated, dynamic, spatiotemporal early warning systems based on a One Health approach for emerging infectious diseases.
Keywords: COVID-19, One health, Early warning systems, Climate variability, Animals, Emerging infectious diseases
Australia is currently experiencing its largest outbreak of COVID-19 since the beginning of the pandemic in 2020 and pressure is now increasing to remove restrictions and co-exist with the virus. The lessons learned so far from the COVID-19 pandemic can contribute to future responses both in the short term, specifically informing the Australian public health response to COVID-19, and in the longer term, in dealing with other emerging infectious diseases. The knowledge gained can also be applied in a changed “post-COVID” world facing worsening climate change, where the health of vulnerable individuals and communities is disproportionately affected by the consequences of inadequate action on health and climate change. Australia had previously avoided the worst of the COVID-19 pandemic prior to the emergence of the Delta variant, enabling researchers and policymakers to learn from the global experience with COVID-19, to inform future public health response including the effectiveness of non-pharmaceutical interventions (NPI) for preventing and controlling COVID-19 transmission. Within Australia, the state-level responses have varied with differing levels of success, and there are lessons to be learned from this for both the future of COVID-19 and other infectious diseases and, more broadly, for improving early warning systems (EWS) and implementing a One Health approach to emerging infectious diseases and future COVID-19 outbreaks.
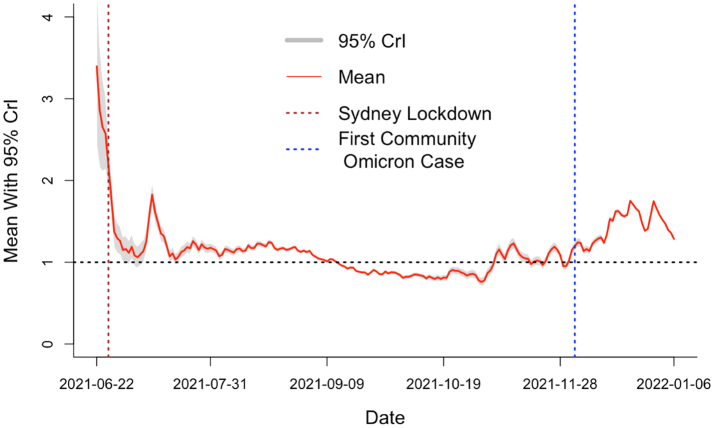
Following the emergence of the Delta variant, Australia was facing growing pressures on previously effective suppression strategies, with contact tracing in some states overwhelmed by the Delta outbreak, and limited vaccine supplies further complicated by inequitable access to vaccines between communities, with some populations such as regional Indigenous communities, with a high prevalence of underlying health conditions, remaining poorly protected [1]. The Delta outbreaks in New South Wales (NSW) and Victoria (VIC) from June 2021 proved a challenge to contain using previously successful strategies, the daily effective reproductive number (Reff) in NSW remained >1. After more than 14 weeks of strict stay-at-home orders and public health measures, NSW began trending below the Reff threshold following increased vaccination coverage (>80%) (Fig. 1). Following reports of a new highly transmissible SARS-CoV-2 strain (Omicron variant) with a high number of mutations in South Africa in mid-November 2021, locally transmitted cases were detected on 3rd December and as of January 2022, Omicron accounts for the majority of new infections in Australia. At the time of writing, daily case numbers in all states and territories are increasing (excluding WA), with record numbers of cases being recorded every day, though these numbers are likely undercounting the actual cases in the wider community as laboratory testing capacity is unable to process demand and rapid antigen tests are in limited supply. Hospitalisations and deaths are steadily increasing, mitigated by higher vaccination coverage compared with the previous Delta outbreak. On a global level, it is a similar situation following the emergence of Omicron variant as new cases are recorded at record levels and hospitalisations and deaths again increase, with more cases now being recorded in younger population groups and the unvaccinated compared with wild type SARS-CoV-2 infections [2].
Fig. 1.
Mean daily Effective Reproductive Number (Reff) curve in Great Sydney Area for the Delta Outbreak 16th June to 6th January 2022. The Great Sydney Area restrictions commenced on June 26th 2021, and first Omicron case detected on 3rd December 2021. Bayesian Estimation theory was used to estimate Reff with a 10-day averaging window [3].
Comparison of the effectiveness of COVID-19 public health responses between countries and states has many limitations as there are many contributing factors to the effectiveness of suppression methods, including climate, weather and air pollution; housing quality and workplace ventilation; global and localised patterns of human mobility and contact across regions and populations; crowding and urban density; sociocultural norms and economic factors including lifestyle, income disparity and access to healthcare [4]. Additional considerations are the willingness of individuals to comply with health directions and remain in quarantine or isolation. Anti-lockdown and anti-vaccination messaging on social media and from political figures locally and globally have influenced sectors of public opinion negatively towards lockdowns and achieving elimination or suppression of COVID-19 [5].
On a global level, the effect of worsening climate change leading to increasing weather variability will likely contribute to emerging infectious diseases and increased risks to health as human behaviour and our interactions with the environment are changing, such as access to clean air and water, which is vital to healthy living. Climate change contributes to the emergence of novel infectious diseases and the spread of existing infectious diseases through the health impacts of climate variability - temperature extremes, and extreme climate and weather events [6]. Previous research suggests weather, particularly variations in temperature and humidity, contributed to the transmission of COVID-19 [7]. Human activities contributing to environmental change, such as deforestation, intensive agricultural practices, biodiversity loss and increasing interactions with wild animals and live animal markets, increase the likelihood of emerging zoonoses and spillover events [8]. Air pollution, including high levels of particulate matter from burning fossil fuels, contribute to the development of chronic diseases such as cardiovascular disease, asthma and other respiratory diseases and increases the risk of mortality and hospitalization from COVID-19 and other respiratory infections [9]. Action to mitigate climate change is likely to decrease the risk of emerging infectious diseases and health risks contributing to poor health outcomes.
In the context of a changing climate, with increasing risks to human health through environmental stressors and emerging zoonoses, and the ongoing COVID-19 pandemic, the importance of a One Health approach for global action is more important than ever, particularly with emerging evidence of transmission of SARS-CoV-2 from humans to wild animal populations [10]. One Health, as defined by the World Health Organization (WHO), is an integrated, unifying approach that aims to sustainably balance and optimize the health of humans, animals, and ecosystems [11]. This approach requires communication, collaboration, capacity building and coordination of health response at the interface of human (doctors, epidemiologists, public health workers), environmental (ecologists, agricultural workers) and animal (veterinarians) health [12]. One Health requires global collaboration applied at the local level with the aim of achieving better public health outcomes, from addressing the impact of climate and environmental change through to the implementation of surveillance and EWS to detect COVID-19 variants of concern and other emerging pathogens with the potential to cause future pandemics [13]. Of particular importance is enhancing and building capacity in existing early notification systems based on localised surveillance and health system data for emerging infectious diseases, such as seasonal influenza strains, novel coronavirus (SARS, MERS) and future COVID-19 at the local, national, regional and global levels to enable the implementation of joint responses to health threats [14]. This is of great importance as prior to the detection of SARS-CoV-2, certain governments were trending towards reducing or defunding of pandemic preparedness. e.g. the Global Public Health Intelligence Network (GPHIN) in Canada [15], Pandemic Preparedness Plan in the USA, and reducing funding to the WHO [16]. The current COVID-19 pandemic has further highlighted the gaps in surveillance and risk communication.
For the future, enhancing the current surveillance methods in Australia must be a priority, to improve detection of community-level transmission of SARS-CoV-2 and detection of emerging variants in human and animal populations, and predict the magnitude of outbreaks for targeted and dynamic application of public health measures. Throughout the COVID-19 pandemic, ongoing genomic sequencing of COVID-19 variants has provided an up-to-date picture of the most prevalent strains across populations, though due to the increasing case numbers in Australia, widespread genomic sequencing has largely ended. To prepare for future COVID-19 variants and emerging zoonoses, genomic sequencing of human and animal populations must be prioritised. Spatiotemporal models have long played a key role in understanding the social and environmental determinants of infectious diseases. These models could be used to develop more accurate, viable and innovative EWS [17]. With the existing surveillance methods, EWS that integrate big data including internet-search queries, mobility data, socio-ecological factors, weather variability and other environmental factors [18] could be developed that would enable robust and dynamic models for timely infectious disease surveillance and public health action. This will refine current monitoring for ‘real-time’ COVID-19 surveillance in Australia and contribute to more effective surveillance for emerging infectious diseases.
In the short term, lessons from the COVID-19 response in Australia integrated with a One Health approach can be used to inform effective public health response. Identification of NPI's effectiveness in prevention and control of COVID-19 will likely contribute to the prevention of future respiratory diseases, vector-borne and intestinal infectious diseases; however, these measures need to be balanced against impacts on ecosystems and animals. As Australia has moved away from local elimination, public health responses should be targeted – such as localised restrictions on movement and interaction with the aim of preventing overburdening the public health system, and continued surveillance of human and animal populations for emerging variants. Now is the time to develop integrated dynamic spatiotemporal EWS based on socioenvironmental factors and other big data [19] for future emerging infectious disease outbreaks to improve detection and targeting of public health measures [20]. More broadly, integrating a One Health multidisciplinary approach to public health to address risk factors associated with COVID-19 and effects of climate and environmental change and for future pandemic preparedness is essential. Actions that limit climate change will also reduce the future risk of emerging infectious disease and the health impact of COVID-19.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Nunes-Vaz R., Macintyre C. Observations on the current outbreak of the SARS-CoV-2 Delta variant in Sydney. Global Biosecurity. 2021;3(1) [Google Scholar]
- 2.World Health Organisation Weekly epidemiological update on COVID-19 - 11 January 2022. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---11-january-2022 Available from.
- 3.Si X., Bambrick H., Zhang Y., Cheng J., McClymont H., Bonsall M.B., et al. Weather variability and transmissibility of COVID-19: a time series analysis based on effective reproductive number. Exp. Results. 2021;2 doi: 10.1017/exp.2021.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vardoulakis S., Sheel M., Lal A., Gray D. COVID-19 environmental transmission and preventive public health measures. Aust. N. Z. J. Public Health. 2020;44(5):333–335. doi: 10.1111/1753-6405.13033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bheekhun Z., Lee G., Camporesi S. Challenges of an ‘infodemic’: separating fact from fiction in a pandemic. Int Emerg Nurs. 2021;57:101029. doi: 10.1016/j.ienj.2021.101029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dennis S., Fisher D. Climate change and infectious diseases: the next 50 years. Ann. Acad. Med. Singap. 2018;47(10):401–404. [PubMed] [Google Scholar]
- 7.Si X., Bambrick H., Zhang Y., Cheng J., McClymont H., Bonsall M.B., et al. Weather variability and transmissibility of COVID-19: a time series analysis based on effective reproductive number. Exp. Results. 2021;2 doi: 10.1017/exp.2021.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tong S., Bambrick H., Beggs P.J., Chen L., Hu Y., Ma W., et al. Current and future threats to human health in the Anthropocene. Environ. Int. 2022;158 doi: 10.1016/j.envint.2021.106892. [DOI] [PubMed] [Google Scholar]
- 9.Wu X., Nethery R.C., Sabath M.B., Braun D., Dominici F. Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Sci. Adv. 2020;6(45):eabd4049. doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gryseels S., De Bruyn L., Gyselings R., Calvignac-Spencer S., Leendertz F.H., Leirs H. Risk of human-to-wildlife transmission of SARS-CoV-2. Mammal Rev. 2021;51(2):272–292. doi: 10.1111/mam.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu K., Wang T., Yang Z., Huang X., Milinovich G.J., Lu Y., et al. Using Baidu search index to predict dengue outbreak in China. Sci. Rep. 2016;6 doi: 10.1038/srep38040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doherty P.C. What have we learnt so far from COVID-19? Nat. Rev. Immunol. 2021;21(2):67–68. doi: 10.1038/s41577-021-00498-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Y., Bambrick H., Mengersen K., Tong S., Hu W. Using internet-based query and climate data to predict climate-sensitive infectious disease risks: a systematic review of epidemiological evidence. Int. J. Biometeorol. 2021;65(12):2203–2214. doi: 10.1007/s00484-021-02155-4. [DOI] [PubMed] [Google Scholar]
- 14.Solis A., Nunn C.L. One health disparities and COVID-19. Evolut. Med. Public Health. 2021;9(1):70–77. doi: 10.1093/emph/eoab003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dion M., AbdelMalik P., Mawudeku A. Big data and the global public health intelligence network (GPHIN) Can. Commun. Dis. Rep. 2015;41(9):209–214. doi: 10.14745/ccdr.v41i09a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilensky G. The importance of reestablishing a pandemic preparedness Office at the White House. JAMA. 2020;324(9):830–831. doi: 10.1001/jama.2020.15525. [DOI] [PubMed] [Google Scholar]
- 17.Milinovich G.J., Avril S.M.R., Clements A.C.A., Brownstein J.S., Tong S., Hu W. Using internet search queries for infectious disease surveillance: screening diseases for suitability. BMC Infect. Dis. 2014;14(1):690. doi: 10.1186/s12879-014-0690-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carleton T., Cornetet J., Huybers P., Meng K.C., Proctor J. Global evidence for ultraviolet radiation decreasing COVID-19 growth rates. Proc. Natl. Acad. Sci. 2021;118(1) doi: 10.1073/pnas.2012370118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milinovich G.J., Williams G.M., Clements A.C.A., Hu W. Internet-based surveillance systems for monitoring emerging infectious diseases. Lancet Infect. Dis. 2014;14(2):160–168. doi: 10.1016/S1473-3099(13)70244-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davis C., Murphy A.K., Bambrick H., Devine G.J., Frentiu F.D., Yakob L., et al. A regional suitable conditions index to forecast the impact of climate change on dengue vectorial capacity. Environ. Res. 2021;195 doi: 10.1016/j.envres.2021.110849. [DOI] [PubMed] [Google Scholar]