Abstract
In the late 1990s, an estimated 75% of pregnant women in Nepal were anaemic. Although iron and folic acid (IFA) supplements were available free of charge, coverage among pregnant women was very low. In response, the Government of Nepal launched the Iron Intensification Programme (IIP) in 2003 to improve the coverage of IFA supplementation and anthelminthic treatment during pregnancy, as well as promote the utilization of antenatal care. This review examined how the IIP programme contributed to Nepal's success in increasing the consumption of IFA supplements during pregnancy. Nepal's cadre of Female Community Health Volunteers were engaged in the IIP to support the community‐based distribution of IFA supplements to pregnant women and complement IFA distribution through health facilities and outreach services. As a result, the country achieved a fourfold increase in the proportion of women who took IFA supplements during pregnancy between 2001 and 2016 (from 23% to 91%) and a 12‐fold increase in the proportion who took IFA supplements for at least 90 days during pregnancy (from 6% to 71%). The increase in coverage of IFA supplements accompanied an increase in the coverage of antenatal care during the same period. By 2016, the prevalence of anaemia in pregnant women decreased to 46%, highlighting the need to tackle other causes of anaemia and improve haemoglobin concentration before pregnancy, while maintaining the successful efforts to reach pregnant women with IFA supplements at the community level.
Keywords: anaemia, antenatal, anthelmintics, community health volunteer, community‐based distribution, iron and folic acid supplements, iron deficiency anaemia, Nepal, pregnancy, prenatal care, review
Key messages.
Following the launch of the Iron Intensification Programme in Nepal, the proportion of women who took iron and folic acid (IFA) supplements during pregnancy for at least 90 days increased from 6% in 2001 to 71% in 2016.
Female Community Health Volunteers contributed to the increase in IFA coverage by promoting early and regular antenatal care visits, distributing IFA supplements to women at the community level and counselling women to take them.
Despite this success, 46% of pregnant women were anaemic in 2016, highlighting the need to address other causes of anaemia and improve haemoglobin concentration before pregnancy, while sustaining community‐based distribution of IFA supplements.
1. INTRODUCTION
Anaemia affects an estimated 27% of the population worldwide, with developing countries accounting for more than 89% of the global burden (Kassebaum & GBD 2013 Collaborators, 2016). Iron deficiency is the most dominant cause of anaemia and is largely caused by insufficient dietary intake of iron to meet physiological needs and infections that cause intestinal blood loss or affect iron absorption or metabolism (World Health Organization [WHO], 2001). Iron deficiency and anaemia are public health concerns associated with an increased risk of maternal and perinatal mortality, low birthweight and inadequate cognitive growth and development in the first years of life (Black et al., 2008).
In South Asia, anaemia affects over half of women (Stevens et al., 2013) and is the second leading cause of maternal death in the region (Kassebaum et al., 2014). No country in South Asia is on track to achieve the World Health Assembly's target to halve the prevalence of anaemia in women of reproductive age by 2025 (Development Initiatives, 2018). However, effective interventions are available to prevent and control anaemia. A meta‐analysis found that daily iron supplementation during pregnancy reduces the incidence of anaemia at term by 73% (Yakoob & Bhutta, 2011).
In Nepal, the prevalence of anaemia was alarmingly high in the late 1990s, affecting 75% of pregnant women (MoH et al., 1998). The major causes of maternal anaemia at that time included iron deficiency, hookworm infection and malaria (Dreyfuss et al., 2000). To address this public health concern, the Government of Nepal launched the Iron Intensification Programme (IIP) in 2003 to improve the coverage of iron and folic acid (IFA) supplementation and anthelmintic treatment during pregnancy (Pokharel et al., 2011). The IIP set out to enhance the delivery mechanisms for IFA supplements by actively engaging Female Community Health Volunteers (FCHVs) to distribute IFA supplements to pregnant and post‐partum women at the community level. Over the course of 15 years, the proportion of women consuming any IFA supplements during pregnancy increased from 23% in 2001 to 91% in 2016.
A recent study examined socio‐demographic predictors of IFA supplementation during pregnancy in Nepal (Yadav et al., 2019). However, to our knowledge, no review has been conducted on the contribution of programme actions to increasing IFA consumption in Nepal between 2001 and 2016. The aim of the present study was to examine how community‐based distribution of IFA supplements through the IIP programme contributed to Nepal's success in increasing the consumption of IFA supplements during pregnancy and to discuss future directions for sustaining the coverage and achieving the World Health Assembly's target on anaemia reduction.
2. METHODS
This paper is based on a comprehensive review of policy and programme documents, published and unpublished reports, journal articles, and household survey reports published between 1991 and 2019. The documents were identified from PubMed (using the key words ‘Nepal’, ‘anaemia’, ‘iron deficiency anaemia’, ‘prenatal care’, ‘antenatal’ and ‘community‐based distribution’) and from the websites and document repositories of government ministries and development organizations. The review examined the evolution of the IIP, including an analysis of the successes and challenges of the actions taken to improve the coverage of IFA supplements and reduce anaemia during pregnancy.
The trends in the consumption of IFA supplements, coverage of anthelmintic treatment, antenatal care (ANC) utilization and prevalence of anaemia were examined using data extracted from the reports of five nationally representative surveys: the 1998 Nepal Micronutrient Status Survey (MoH et al., 1998), the Nepal Demographic and Health Surveys (NDHS) in 2001, 2006, 2011 and 2016 (MoH et al., 2002; MoHP et al., 2007, 2012) and the 2016 Nepal National Micronutrients Status Survey (NNMSS) (MoHP et al., 2018). In addition, to assess the performance of programmes that were designed to improve micronutrient status, data on the sources of IFA supplements and the reasons why pregnant women did not take IFA supplements were extracted from the reports of twice yearly or annual micronutrient surveys, which were conducted by the Nepali Technical Assistance Group (NTAG) between 2001 and 2010 in eight to 10 randomly selected districts.
The strategies used in Nepal to implement community‐based distribution of IFA supplements were described using the framework proposed by Proctor et al. (2013) that characterizes implementation strategies using a series of domains (actor, target of actions, skills required to deliver the actions, temporality, intensity/frequency, desired implementation outcome and justification).
Last, implications were drawn for sustaining and strengthening the community‐based distribution of IFA supplements in Nepal.
3. RESULTS AND DISCUSSION
3.1. Evolution of the IFA supplementation programme in Nepal
Table 1 describes the key milestones leading to the design of Nepal's IIP and its implementation until 2016.
Table 1.
Timeline of milestones leading to the design of the Nepal's IIP and its implementation until 2016
| Year | IFA programme milestone |
|---|---|
| 1980s | IFA supplementation for pregnant and post‐partum women begins. |
| 1988 | FCHV programme begins, and the community‐based delivery platform that is later used by the IIP is established. |
| 1997 | Nepal Multiple Indicator Surveillance report identifies that only 10% of pregnant women consumed any IFA supplements and only 2% consumed at least 90 supplements. |
| 1998 | The Nepal Micronutrient Status Survey finds that 75% of pregnant women are anaemic. |
| 1999 | Operations research show that IFA coverage and compliance improve if Female Community Health Volunteers (FCHVs) are involved in the distribution of IFA supplements to pregnant women. |
| 1999–2010 | Micronutrient surveys conducted in eight to 10 districts following each round of twice yearly vitamin A supplementation report on the consumption of iron tablets by pregnant women. |
| 2001 | Nepal Demographic and Health Survey finds that only 23% of women take any IFA during pregnancy. |
| 2001 | Comprehensive review of the anaemia in Nepal (Malla, 2001) shows that a lack of awareness and limited accessibility to IFA supplements are the main factors that prevent pregnant women from taking IFA supplements. |
| 2003 | National strategy for controlling anaemia among women and children is formulated by the Ministry of Health and Population. The new strategy introduces community‐based distribution of IFA supplements to pregnant and post‐partum women through FCHVs, trained traditional birth attendants and community motivators. |
| 2003 | The findings of the 2001 review, combined with the (i) high prevalence of anaemia in 1998, (ii) low coverage of IFA supplementation in pregnancy in 2001, and (iii) evidence from operational research that FCHVs can effectively distribute IFA supplements at the community level, and (iv) 2003 National Strategy for Controlling Anaemia inform the design of the Iron Intensification Programme (IIP). |
| 2003 | The IIP is launched in five districts and involves FCHVs in community‐based distribution of IFA supplements. |
| 2004–2007 | The IIP is expanded to 38 districts (Phases II, III and IV). |
| 2005 | First five‐year Plan of Action for Anaemia Control commences and is aimed at expanding IIP coverage to all 75 districts by 2010. |
| 2008–2011 | The IIP is expanded to a further 27 districts (Phase V), covering 53 out of 75 districts. |
| 2012 | IIP is scaled‐up to cover 74 districts. |
| 2013 | Nepal's first Multi‐Sector Nutrition Plan (2013–17) begins implementation and includes a commitment to continue community‐based distribution of IFA supplements to pregnant and post‐partum women. |
| 2014 | IIP reaches its final district, covering all 75 districts. |
3.1.1. IFA supplementation in the 1990s
In the early 1990s, maternal and infant mortality, as well as deficiencies of iron and vitamin A, were major public health problems in Nepal (Government of Nepal, 1991). At that time, Nepal's policy of universal IFA supplementation for women included a daily dose of 60 mg of iron and 400 μg of folic acid, starting in the second trimester of pregnancy and ending 45 days post‐partum. Health workers were responsible for reaching pregnant and post‐partum women with IFA supplements at health facilities (health posts and subhealth posts), and in 1997, the distribution of IFA supplements was extended to outreach clinics (Pokharel et al., 2011).
By the late 1990s, it was clear that these health services were not effective in ensuring that pregnant women received and consumed IFA supplements or in reducing anaemia. The fifth cycle of the 1997 Nepal Multiple Indicator Surveillance showed that only 10% of women consumed any IFA supplements during pregnancy, and only 2% consumed daily supplements for at least 90 days (Central Bureau of Statistics, 1997). Meanwhile, the 1998 Nepal Micronutrient Status Survey showed that 75% of pregnant women were anaemic (MoH et al., 1998). The 2001 NDHS found improved IFA coverage, with 23% of pregnant women taking any IFA supplements. However, the proportion of women consuming supplements for at least 90 days was very low at 6% (MoH et al., 2002).
In the 1990s, Nepal's cadre of FCHVs were not involved in IFA supplementation, but had supported other community‐based health initiatives since 1988, including encouraging families to attend health clinics and promoting family planning. From 1993, FCHVs were also enlisted to support the distribution of vitamin A supplements to children at the community level twice a year. An operations research study conducted in two districts in eastern Nepal in 1999 established that FCHVs had effectively distributed IFA supplements and counselled pregnant women at the community level (Malla, 2001). In fact, the coverage of IFA supplements among pregnant women increased from 8% to 76% in the study area. These findings were crucial because they opened up the possibility to distribute IFA supplements to pregnant women at the community level, close to where they lived. At that time, pregnant women faced significant geographic barriers to accessing ANC at health facilities in Nepal: 67% of women took more than 1 h to reach the nearest health post our sub‐health post, and 10% took at least 3 h (UNICEF, 2000).
In 2011, a review of published and unpublished literature and reports on the causes of anaemia in Nepal and the efficacy of available interventions was conducted (Malla, 2001). The main reasons cited for the low consumption of IFA supplements included (1) the low awareness of health workers on anaemia and the health benefits of IFA supplementation, (2) the low access of pregnant women to IFA supplements (in particular, the reliance on IFA distribution by health workers at health facilities and outreach clinics), (3) inadequate education and counselling of pregnant women on the benefits of IFA supplementation, (4) common fear among pregnant women of giving birth to a ‘big baby’ and (5) the low demand of pregnant women for IFA supplements. The availability and supply of IFA supplements from central level to health facilities was not found to be a major bottleneck, though the review noted room for improvement. The review also recognized the multifactorial causes of anaemia and suggested that other interventions besides IFA supplementation were needed as part of a successful strategy to reduce anaemia, including anthelminthic treatment and malaria prevention.
3.1.2. Introduction and scale‐up of the Iron Intensification Programme (IIP)
Policy makers within the Ministry of Health revisited the strategies to address maternal anaemia in Nepal as a result of (1) the high prevalence of anaemia in pregnant women in 1998 (MoH et al., 1998), (2) the low consumption of IFA supplements in 2001 (MoH et al., 2002), (3) the findings of the review of anaemia and (4) the operational research on the effectiveness of IFA distribution by FCHVs (Malla, 2001). As a result, the Government of Nepal launched the IIP in five districts of the country in 2003.
The IIP was designed to improve access to and utilization of ANC and to enhance two key interventions to prevent and control anaemia during pregnancy: IFA supplementation and anthelmintic treatment. From the onset of the IIP, the Government of Nepal involved FCHVs in order to expand access to IFA from health facilities to the community and thereby bring IFA supplements much closer to the homes of pregnant and post‐partum women. Each FCHV was responsible for a ward—a catchment area of 80 to 100 households with approximately five pregnant women. As part of the overall IIP strategy, FCHVs were trained to build their knowledge and skills on how to distribute IFA supplements, counsel women on the benefits of IFA, emphasize the importance of taking supplements every day throughout pregnancy and for 45 days post‐partum, inform about the possibility of side effects and suggest ways to minimize side effects. The FCHVs distributed IFA supplements to pregnant women at monthly mother's group meetings (30 supplements per woman every month). In addition, FCHVs involved other family members, such as the woman's husband and mother‐in‐law, so that they could encourage and remind the pregnant women to take IFA supplements. To improve the acceptability of the supplements and to preserve their appearance and taste, the packaging was changed from newspaper wrapping to small clear plastic bottles, and blister packs were introduced in 2011. The FCHVs also encouraged mothers to attend ANC clinics to receive other ANC services that were only available in health facilities, including anthelmintic and malaria treatment.
FCHVs used a register to record the number of pregnant women who received IFA supplements each month. These data were forwarded to the nearest health post or subhealth post and subsequently added to Health Management Information System (HMIS) forms, together with data on anthelmintic treatment. The compiled data were then submitted by the District Health Office to the central HMIS and Child Health Division. FCHVs—supervised by health workers in the nearest health facility (health post or subhealth post)—participated in monthly meetings at health facilities, where they reported on activities, received supplies of IFA supplements and discussed any issues or concerns about the programme.
The IIP was gradually scaled up geographically in phases, starting with five priority districts in 2003 and expanding to all 75 districts in 2014.
3.2. Success factors and challenges to improving IFA coverage
Since the implementation of community‐based distribution began in 2003, the coverage of IFA supplements and anthelmintic treatment have increased considerably. Data from nationally representative NDHS show that the proportion of women taking any IFA supplements during pregnancy increased from 23% to 91% between 2001 and 2016, whereas the proportion of women consuming supplements for at least 90 days increased from 6% to 71% (Figure 1). Beginning in 2006, the NDHS revealed substantial increases in the proportion of women taking IFA supplements for at least 180 days during pregnancy (7% in 2006 to 42% in 2016) and the proportion who received anthelmintic treatment (20% in 2006 to 69% in 2016).
Figure 1.
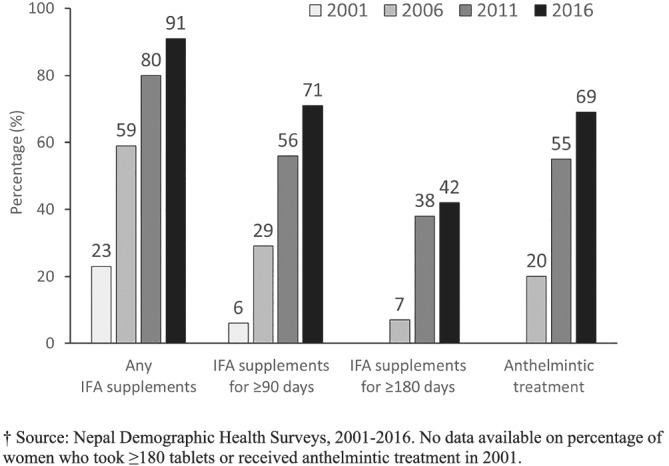
Percentage of women aged 15–49 years who consumed iron and folic acid (IFA) supplements and received anthelmintic treatment during their most recent pregnancy in Nepal, 2001–2016
Nepal's success in improving the coverage of IFA supplementation exceeds all other countries in South Asia, with the exception of Sri Lanka (UNICEF, 2019). The likely reasons for this success include (1) the increase in the number of ANC visits during pregnancy and proportion of women seeking ANC in the first trimester, which has increased opportunities for reaching pregnant women with IFA supplements at the health facility level and (2) the involvement of Nepal's >50,000 FCHVs, which has increased access to, demand for and adherence to IFA supplementation at the community level, as well as the uptake of earlier and more frequent ANC visits.
The larger the number of ANC visits, the greater the number of opportunities women have to receive IFA supplements and counselling during pregnancy at health facilities that are providing ANC. And the earlier ANC visits begin in pregnancy, the longer the period to improve iron stores and haemoglobin concentration. Results from the NDHS show that between 2001 and 2016 the proportion of women attending ANC increased from 49% to 94%, and the proportion attending ANC at least five times increased from 14% to 69% (Figure 2). During this period, there was a sharp increase in the proportion of women starting their ANC visits in the first trimester of pregnancy, from 16% in 2001 to 65% in 2016. Comparing Figures 1 and 2, it can be seen that the increase in the proportion of women who consumed any IFA supplements during pregnancy closely matches the increase in the coverage of any ANC visit. The difference between any IFA consumption and ANC coverage declined from 26 percentage points in 2001 to 3 percentage points in 2016, suggesting that there was a reduction in missed opportunities to reach women with IFA supplements during ANC. Similarly, the increase in the proportion of women who consumed IFA supplements for at last 90 days during pregnancy closely matches the coverage of at least four ANC visits and the proportion of women who had their first ANC visit in the first trimester.
Figure 2.
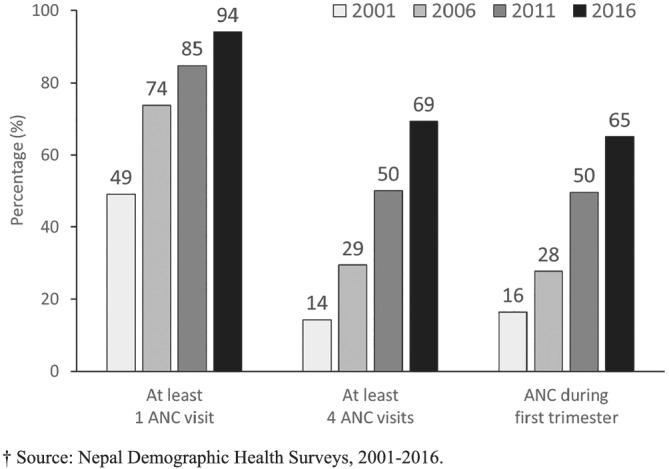
Percentage of women aged 15–49 years who received antenatal care (ANC) during their most recent pregnancy in Nepal, 2001–2016
Although these findings suggest that the increase in ANC coverage at the health facility level may explain the increase in IFA coverage in Nepal, there is compelling evidence that FCHVs play a key role. First, FCHVs are a leading source of information on IFA supplements among pregnant women. A survey conducted by the NTAG in November 2007 found that 65% of pregnant women received information on IFA supplements from FCHVs and only 39% from health workers. A recent literature review also found that community‐based approaches in low‐ and middle‐income countries increased awareness and knowledge of IFA supplementation (Kavle & Landry, 2018). Second, most NTAG surveys with available data find that at least 50% of pregnant women receive IFA supplements from FCHVs (Figure 3). And third, FCHVs are instrumental in increasing the demand for and uptake of ANC by pregnant women, countering a common concern that community‐based distribution of IFA discourages women from seeking health care at health facilities (MoHP, 2007). This is consistent with findings in other countries that show that community‐based distribution of IFA supplementation encourages earlier and consistent ANC visits (Aguayo et al., 2005; Ndiaye et al., 2009; Nisar et al., 2014).
Figure 3.
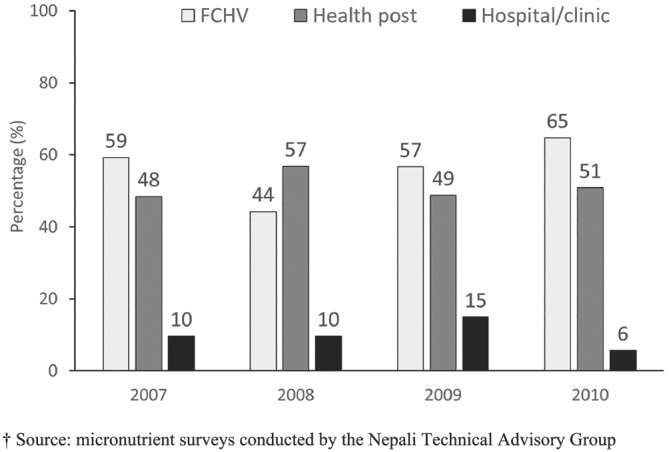
Percentage of pregnant women who received iron and folic acid supplements from Female Child Health Volunteers (FCHVs), health post and a hospital or clinic
Using a framework proposed by Proctor et al. (2013) to characterize implementation strategies, Table 2 describes the various dimensions of the strategies used in Nepal to engage FCHVs in increasing coverage, including the actors, the actions, the action targets, the temporality of actions and the intensity (frequency) of actions. These strategies are effective because they bring IFA supplements much closer to where pregnant women live and because IFA supplements are delivered by FCHVs—community members who have earned the trust and respect of households through their work in supporting the implementation of other health and nutrition interventions at the community level (Kandel & Lamichhane, 2019; Khatri et al., 2017). Close contact of FCHVs with community members, coupled with manageable catchment areas (80–100 households, which include approximately five pregnant women at any one time), has helped FCHVs identify newly pregnant women and ensure that they receive each monthly supply of supplements. FCHVs have also increased compliance by counselling pregnant women on side effects and enlisting other family members to remind and encourage pregnant women to take IFA supplements. Other studies have found that community‐based programmes help remind women to take IFA supplements, address side‐effects and increase compliance (Kavle & Landry, 2018). The success in involving FCHVs has been possible because the Government of Nepal invested in building the knowledge, counselling and reporting skills of FCHVs and ensured appropriate supportive supervision links with health workers at the nearest health facilities (Pokharel et al., 2011).
Table 2.
Implementation strategies to improve the coverage of IFA supplementation through community‐based distribution in Nepal
| Domain | Strategies |
|---|---|
| Actor | • female community health volunteers (FCHVs) |
| Actions |
• FCHVs identify pregnant women in their catchment area as early as possible in pregnancy. • FCHVs organize monthly mother's group meetings at the community level to raise awareness on anaemia, the benefits of IFA, the possibility of side effects and how to minimize them. • FCHVs distribute a monthly support of IFA to each pregnant mother and post‐partum mother at the monthly meetings and document the number of receiving supplies. • FCHVs attend monthly meetings at the health post or subhealth post to receive supplies of IFA, report on IFA distribution during the last month, and discuss any issues or challenges. |
| Targets of the action | • Pregnant women and post‐partum women (up to 45 days post‐partum) and their family members (husbands and mothers‐in‐law). |
| Skills required to deliver the actions |
• Knowledge of FCHVs on the benefits of IFA supplements during pregnancy and post‐partum, how to take IFA supplements, the possibility of side‐effects, and how to minimize side effects. • Group and individual counselling skills of the FCHVs to support women in understanding the importance of IFA supplements and addressing any barriers to adherence. • Reporting skills of the FCHVs to document the number of women who receive IFA each month. |
| Temporality | • FCHVs should identify and engage pregnant women as early as possible during pregnancy (ideally in first trimester) and until 45 days post‐partum. |
| Intensity/frequency |
• Monthly mother's group meetings of the FCHVs with pregnant and post‐partum women at the community level. • Monthly meetings of FCHVs with health workers at the health post or subhealth post. |
| Desired implementation outcome | • Proportion of pregnant women who take an adequate number of IFA supplements during pregnancy. |
| Justification | • Operations research show that IFA coverage and compliance improve in Nepal if FCHVs are involved in the distribution of IFA supplements to pregnant women. |
In spite of these notable improvements, challenges remain to the success of the IIP. First, the well‐being and motivation of FCHVs—who are central to community‐based distribution of IFA supplements—is an ongoing concern. Considered the ‘backbone of health care’ in Nepal, FCHVs are currently involved in a multitude of primary health care programmes, including family planning, immunization, maternal and child health and nutrition, as well as being first responders in emergencies, such as earthquakes and disease outbreaks (Kandel & Lamichhane, 2019; Khatri et al., 2017). Over the last three decades, their volunteer status has been maintained as a succession of additional responsibilities has been added. FCHVs report that they are overburdened and should receive pay for their work (Khatri et al., 2017; Panday et al., 2017). Although the case is often made to remunerate FCHVs, others argue that the volunteer status—which has earned them the trust and social respect of community members—is essential to the financial sustainability of the approach and that the low attrition of FHCVs is evidence of the continued viability of this volunteer model in Nepal (Glenton et al., 2010; Panday et al., 2017). Nevertheless, FCHVs should be recognized as key actors, and it is important that there are mechanisms to sustain their motivation.
Second, although IFA coverage has increased, many vulnerable pregnant women are still not taking sufficient IFA supplements. The 2016 NDHS found that although 91% of women took IFA supplements during pregnancy, only 71% took supplements for at least 90 days and only 42% for at least 180 days. Figure 4 shows that the proportion of women who took IFA supplements for at least 90 days during pregnancy was considerably lower in the Terai region than in the Hilly region (67% vs. 76%), in the lowest wealth quintile compared with the highest (67% vs. 84%) and in those with no education compared with those who had completed secondary school (56% vs. 88%). Khanal et al. (2014) analysed data from the 2011 NDHS and found that the odds of compliance during the post‐partum period (defined as taking IFA supplements for at least 45 days following delivery) were significantly lower in women who were less educated and had less antenatal and postnatal visits. These findings are consistent with other studies conducted in Nepal (Yadav et al., 2019) and elsewhere in South Asia (Nguyen et al., 2017; Nisar et al., 2014), which found that barriers acting at the individual (e.g. maternal education), household (e.g. wealth) and service delivery (e.g. access to ANC and PNC) levels affect IFA consumption during pregnancy and post‐partum. Nepal is already implementing many of the programme approaches that have been effective in addressing these barriers in South Asia, such as community‐based distribution of IFA supplements and engagement of family members (Goudet et al., 2018). However, more investment in the capacity, supervision, monitoring and motivation of FCHVs to provide information and counselling may assist in increasing IFA consumption, particularly among the most vulnerable and marginalized. A study in the Terai region found that ethnic minority groups are often reluctant to utilize the services of FCHVs because of a lack of trust and traditional beliefs and health care practices, suggesting that the volunteers should be trained to communicate effectively and deliver respectful care to women (Panday et al., 2019).
Figure 4.
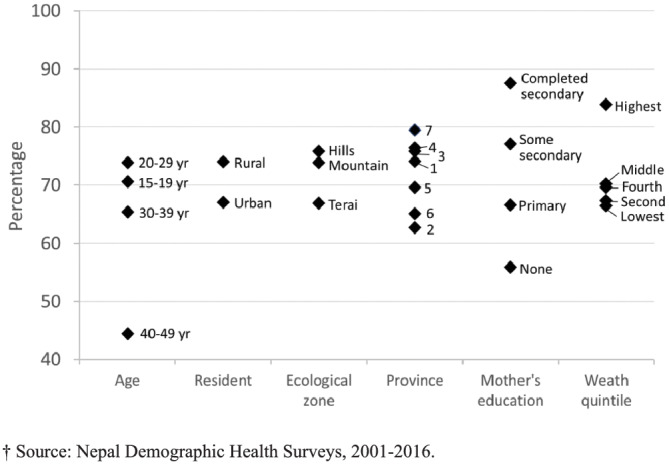
Percentage of women who consumed iron and folic acid supplements for at least 90 days during their most recent pregnancy by socio‐economic and demographic factors in Nepal, 2016
Third, the coverage or quality of counselling on IFA supplements is likely to be insufficient. The NTAG micronutrient surveys conducted between 2001 and 2010 found that pregnant women who did not take any IFA supplements reported four main reasons for non‐compliance: unaware of the benefits, were not advised to take them, did not want to take them or it was not a habit to take them. However, very few women reported that they did not receive IFA supplements (Appendix S1, Figure S1). These findings suggest that counselling actions were insufficient to address gaps in knowledge, attitudes and practices. Furthermore, the 2016 NDHS found that only 24% of women reported that they had received counselling to take IFA supplements for the recommended period (180 days) during their previous pregnancy. Elsewhere in South Asia, compliance with IFA supplementation is heavily dependent on access to and quality of counselling (Goudet et al., 2018).
3.3. Trends in the prevalence of maternal anaemia, low birthweight and child mortality
Given Nepal's success in improving the coverage of IFA supplementation over the last 15 years, we would expect to see a reduction in health conditions associated with iron deficiency during pregnancy. In this section, we review the data on the trends in maternal anaemia, low birthweight and neonatal and child mortality in Nepal.
3.3.1. Prevalence of anaemia during pregnancy
Data from the 1998 Nepal Micronutrient Status Survey and NDHS in 2006, 2011 and 2016 show that the prevalence of anaemia in pregnant women decreased from 75% in 1998 to 42% in 2006 and then plateaued at 48% in 2011 and 46% in 2016 (Figure 5). The prevalence of anaemia in non‐pregnant women also declined substantially between 1998 (67%) and 2006 (40% in breastfeeding women and 34% in non‐pregnant non‐breastfeeding women) but was slightly higher in 2016. The insufficient progress in reducing anaemia between 2006 and 2016—despite the high consumption of IFA supplements—suggests that other causes of anaemia, besides iron and folic acid deficiency, are important contributors to low haemoglobin concentrations in women of reproductive age. They include other micronutrient deficiencies, haemoglobinopathies (e.g. sickle cell diseases and thalassemia) and malaria. The 2016 Nepal National Micronutrient Status Survey (NNMS) found that 18.7% of non‐pregnant women had iron deficiency (ferritin <15 μg/L), whereas 4.5% had megaloblastic anaemia (a haematological indicator of folate deficiency), and 3% were vitamin A deficient (modified relative dose response ≥0.06) (MoHP et al., 2018). The low quality of women's diets in Nepal suggests that multiple micronutrient deficiencies are the norm rather than the exception. The 2016 NDHS reported that only 50% of women of reproductive age consumed foods from at least five different food groups in the last 24 h, and only 34% consumed either meat, poultry or fish. The 2016 NNMSS examined haemoglobinopathies in non‐pregnant women aged 15–49 years and found 0.7% with alpha‐thalassemia, 3.1% with beta‐thalassemia, and 0.7% with sickle cell, as well as 13.5% with glucose‐6‐phosphate dehydrogenase (G6PD) deficiency, which are all causes of anaemia. A recent study found that haemoglobinopathies and G6PD deficiency are associated with anaemia in non‐pregnant women in Nepal (Ford et al., 2022a). Nepal has made significant progress towards the goal of elimination of malaria by 2025, but importation along its southern border presents a major challenge (Smith et al., 2019) and could be a cause of anaemia in the region.
Figure 5.
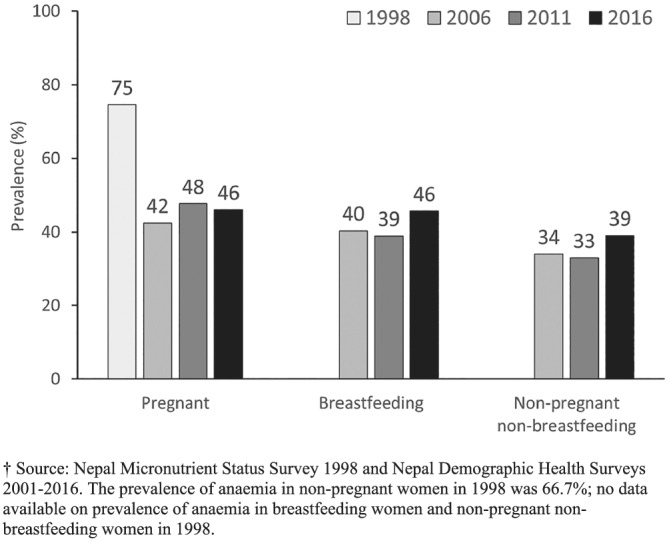
Prevalence of anaemia in women aged 15–49 years in Nepal, 1998–2016
3.3.2. Low birthweight
Low birthweight is a major public health challenge in Nepal. National household surveys in Nepal do not provide reliable estimates of low birthweight prevalence because home births are still a common practice, newborns are usually not weighed and home records of birthweight are often not available. UNICEF and WHO (2019) estimated the prevalence of low birthweight in Nepal using hierarchical regression and found that the prevalence decreased from 27% in 2000 to 22% in 2015. The increasing coverage of IFA between 2001 and 2016 might have contributed to the reduction in the prevalence of low birthweight. Epidemiological evidence from randomized controlled trials of pregnant women in Nepal indicate that iron supplementation during pregnancy, alone or combined with other micronutrients, improves weight at birth (Christian et al., 2003; Osrin et al., 2005).
3.3.3. Neonatal and under five mortality
The increase in IFA supplementation coverage over the past 15 years may have contributed to lowering neonatal and child mortality. Analyses of pooled data from the NDHS of 2001, 2006 and 2011, which controlled for potential confounders, indicated that early neonatal mortality (within 8 days of delivery), neonatal mortality (within 28 days of delivery), and childhood mortality (under 5 years of age) were lower among children whose mothers took IFA during pregnancy compared with children whose mothers did not (Nisar et al., 2014; Nisar et al., 2015). The greatest effect of IFA on neonatal and child survival was found in women who started IFA supplementation before the fourth month of pregnancy and took supplements for at least 150 days. Nisar et al. (2015) estimated that approximately 29,000 deaths of children under 5 years of age could be prevented in the next 5 years if all pregnant women took IFA supplements, and 38,000 child deaths could be prevented if all pregnant women started taking IFA supplement in the first 4 months of pregnancy and consumed at least 150 IFA supplements during pregnancy.
3.4. Future of anaemia prevention and control during pregnancy in Nepal
Although there has been considerable progress in scaling up interventions to prevent and control anaemia during pregnancy in Nepal, the prevalence remains one of the highest in South Asia (UNICEF, 2019). This sustained prevalence is most likely explained by one or more of the following: insufficient coverage of IFA supplements during pregnancy, other causes of anaemia that are not currently being adequately addressed and the high prevalence of anaemia in women of reproductive age before pregnancy.
Although there are gaps in the coverage of IFA supplements during pregnancy in Nepal, the country is performing considerably better than most other countries in South Asia (UNICEF, 2019). Much of the success is due to the effort and dedication of the FCHVs and the strong network of community support within villages and districts across the country. This valuable resource needs to be carefully protected to ensure continuity in the success of IFA supplementation coverage efforts. Ways to protect the work and dedication of FCHVs could include refresher training, reimbursement of expenses and other incentives (Panday et al., 2017). In particular, attention should be given to building or refreshing the counselling skills of FCHVs to encourage greater compliance with IFA supplementation and ensure that vulnerable and marginalized pregnant women are reached. Formative research on compliance with IFA supplements is planned under the current Multi‐Sector Nutrition Plan (2018–2022) and will inform this work.
Other potential causes of anaemia include non‐modifiable (G6PD and haemoglobinopathies) and modifiable (other micronutrient deficiencies and infectious diseases) conditions. As multiple micronutrient deficiencies are common among women in Nepal, and given the recent findings that multiple micronutrient supplements are more cost‐effective than IFA supplements during pregnancy (Kashi et al., 2019), policy makers in Nepal should consider replacing IFA supplements with multiple micronutrient supplements.
Earlier evidence from intervention studies suggested that anthelmintic treatment during pregnancy not only reduced anaemia in Nepal but also improved birthweight and infant survival (Christian et al., 2004). However, improvements in water, sanitation and hygiene have led to a substantial reduction in the annual incidence of soil‐transmitted helminths. The 2016 NNMSS found that <1% of non‐pregnant women were infected with Trichuris trichura or hookworm (MoHP et al., 2018), well below the 20% prevalence that justifies preventive chemotherapy during pregnancy (WHO, 2019). This evidence suggests that these infections are no longer endemic in Nepal and that routine anthelmintic treatment during pregnancy may no longer be justified.
When women enter pregnancy with a low haemoglobin concentration, it can be difficult to control anaemia due to the elevated iron requirements to support fetal growth. In Nepal, 39% of non‐pregnant and non‐breastfeeding women of reproductive age are anaemic (MoH et al., 2017). It is, therefore, important to implement approaches to prevent and control anaemia in adolescents and women of reproductive age so that they can enter pregnancy with an adequate haemoglobin concentration. These approaches include the fortification of staple foods and making sure that public health programmes promote dietary improvement and provide micronutrient supplements (Ford et al., 2022a; 2022b). Iron fortification of wheat flour has been mandatory in Nepal since 2011. A non‐controlled study found that the prevalence of anaemia in women of reproductive age was lower at post‐fortification (18%) than pre‐fortification (33%), but the statistical significance of this difference was not reported (Pachón et al., 2015). The 2016 NNMSS found that 45% of households purchased potentially fortified wheat flour from large scale producers, and 37% of purchased household wheat flour samples contained at least 60 mg/kg of iron, Nepal's standard for iron in wheat flour (MoHP et al., 2018)—suggesting that the coverage and quality of wheat flour fortification was inadequate. Interventions to improve the dietary intake of women in Nepal have predominantly focused on pregnant and breastfeeding women. However, these efforts should extend to non‐pregnant women and address the failures of multiple systems (notably the food, health, social protection and education systems) to increase access to and consumption of nutritious, safe, affordable and sustainable diets. There is currently no programme to supplement non‐pregnant women with iron supplements in Nepal, except school‐going adolescents. WHO recommends that adolescents and women of reproductive age take daily iron supplementation for 3 months a year in populations where the prevalence of anaemia is at least 40%. In Nepal, the prevalence of anaemia in non‐pregnant non‐breastfeeding women almost reaches this threshold (39%), thus supplementation of non‐pregnant women could be considered.
3.5. Limitations
A limitation of our study is that the quality of evidence included in the review was not graded. Another limitation is that the trends in anaemia prevalence and coverage of IFA supplements were based on data from different surveys, including the decline in anaemia prevalence between the 1998 Nepal Micronutrient Status Survey and 2016 NDHS. However, both of these surveys were nationally representative, had similar two‐stage sampling designs, and used HemoCue machines to measure blood haemoglobin concentration, with adjustments for altitude and smoking.
4. CONCLUSIONS
The Government of Nepal has achieved considerable success in increasing the coverage of and compliance with IFA supplementation during pregnancy nationwide. We argued that this was achieved by using respected and trusted FCHVs to reach pregnant women with IFA supplements at the community level, together with information and counselling to encourage adherence with IFA and early and regular ANC visits. The increase in the coverage of IFA supplements may partially account for the declines in anaemia, low birthweight and child mortality in Nepal. Despite the high consumption of IFA supplements during pregnancy, the decrease in anaemia prevalence has been slow since 2006. To make further progress in reducing maternal anaemia, policy makers should consider replacing IFA supplements with multiple micronutrient supplements, introducing or strengthening strategies to improve haemoglobin concentration in adolescents and women before pregnancy and strengthening and sustaining efforts to distribute IFA supplements and counsel pregnant women at the community level.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
NP conceptualized the review, and HT, SC and VGL prepared the manuscript. KRP provided overall guidance to the manuscript. SR supported the study design and data analysis. All authors, including RKA and MDD, reviewed and provided input into the manuscript.
Supporting information
FIGURE S1. Main reasons given by pregnant women who did not take any iron and folic acid supplements, 2001–2010
ACKNOWLEDGMENTS
The authors thank Mr. MR Maharjan, Programme Policy Officer‐ Rice Fortification Specialist, World Food Programme, who provided information on the evolution of the Iron Intensification Programme and flour fortification in Nepal. The research was funded by UNICEF Nepal.
Paudyal N, Parajuli KR, Garcia Larsen V, et al. A review of the maternal iron and folic acid supplementation programme in Nepal: Achievements and challenges. Matern Child Nutr. 2022;18(S1):e13173. 10.1111/mcn.13173
DATA AVAILABILITY STATEMENT
The data presented in the figures were extracted from survey reports. The following survey reports are available in the public domain: 1998 Nepal Micronutrient Status Survey (https://un.info.np/Net/NeoDocs/View/8446), 2016 Nepal National Micronutrient Status Survey (https://mohp.gov.np/downloads/NNMSS%20Report%202016-Final%20Report.pdf) and 2001–2016 Nepal Demographic Health Survey (https://dhsprogram.com/data/available-datasets.cfm). The reports of the micronutrient surveys conducted by the NTAG are available on request from the corresponding author.
REFERENCES
- Aguayo, V. M. , Koném, D. , Bamba, S. I. , Diallo, B. , Sidibé, Y. , Traoré, D. , Signé, P. , & Baker, S. K. (2005). Acceptability of multiple micronutrient supplements by pregnant and lactating women in Mali. Public Health Nutrition, 8, 33–37. 10.1079/PHN2004665 [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Allen, L. H. , Bhutta, Z. A. , Caulfield, L. E. , de Onis, M. , Ezzati, M. , Mathers, C. , Rivera, J. , & Maternal and Child Undernutrition Study Group . (2008). Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet, 371, 243–260. 10.1016/S0140-6736(07)61690-0 [DOI] [PubMed] [Google Scholar]
- Central Bureau of Statistics . (1997). Nepal multiple indicator surveillance 1997, fifth cycle. Kathmandu, Nepal: Central Bureau of Statistics. [Google Scholar]
- Christian, P. , Khatry, S. K. , Katz, J. , Pradhan, E. K. , LeClerq, S. C. , Shrestha, S. R. , Adhikari, R. K. , Sommer, A. , & West, K. P. Jr. (2003). Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: Double blind randomised community trial. British Medical Journal, 326(7389), 571. 10.1136/bmj.326.7389.571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian, P. , Khatry, S. K. , & West, K. P. Jr. (2004). Antenatal anthelmintic treatment, birthweight, and infant survival in rural Nepal. Lancet, 364(9438), 981–983. 10.1016/S0140-6736(04)17023-2 [DOI] [PubMed] [Google Scholar]
- Development Initiatives . (2018). 2018 global nutrition report: Shining a light to spur action on nutrition. Bristol, UK: Development Initiatives. [Google Scholar]
- Dreyfuss, M. L. , Stoltzfus, R. J. , Shrestha, J. B. , Pradhan, E. K. , LeClerq, S. C. , Khatry, S. K. , Shrestha, S. R. , Katz, J. , Albonico, M. , & West, K. P. Jr. (2000). Hookworms, malaria and vitamin A deficiency contribute to anemia and iron deficiency among pregnant women in the plains of Nepal. Journal of Nutrition, 130(10), 2527–2536. 10.1093/jn/130.10.2527 [DOI] [PubMed] [Google Scholar]
- Ford, N. D. , Bichha, R. P. , Parajuli, K. R. , Paudyal, N. , Joshi, N. , Whitehead, R. D. Jr. , Chitekwe, S. , Mei, Z. , Flores‐Ayala, R. , Adhikari, D. P. , Rijal, S. , & Jefferds, M. E. (2022a). Factors associated with anaemia in a nationally representative sample of nonpregnant women of reproductive age in Nepal. Maternal & Child Nutrition, 18(S1), e12953. 10.1111/mcn.12953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford, N. D. , Bichha, R. P. , Parajuli, K. R. , Paudyal, N. , Joshi, N. , Whitehead, R. D. , Chitekwe, S. , Mei, Z. , Flores‐Ayala, R. , Adhikari, D. P. , Rijal, S. , & Jefferds, M. E. (2022b). Factors associated with anaemia among adolescent boys and girls 10–19 years old in Nepal. Maternal & Child Nutrition, 18(S1), e13013. 10.1111/mcn.13013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenton, C. , Scheel, I. B. , Pradhan, S. , Lewin, S. , Hodgins, S. , & Shrestha, V. (2010). The female community health volunteer programme in Nepal: Decision makers' perceptions of volunteerism, payment and other incentives. Social Science & Medicine, 70(12), 1920–1927. 10.1016/j.socscimed.2010.02.034 [DOI] [PubMed] [Google Scholar]
- Goudet, S. , Murira, Z. , Torlesse, H. , Hatchard, J. , & Busch‐Hallen, J. (2018). Effectiveness of programme approaches to improve the coverage of maternal nutrition interventions in South Asia. Maternal & Child Nutrition, 14(Suppl 4), e12699. 10.1111/mcn.12699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Nepal . (1991). National health policy. Kathmandu, Nepal: Ministry of Health and Population, Government of Nepal. http://www.lawcommission.gov.np/en/wp-content/uploads/2018/09/national-health-policy-2048-1991.pdf [Google Scholar]
- Kandel, N. , & Lamichhane, J. (2019). Female health volunteers of Nepal: The backbone of health care. Lancet, 393(10171), e19–e20. 10.1016/S0140-6736(19)30207-7 [DOI] [PubMed] [Google Scholar]
- Kashi, B. , Godin, C. M. , Kurzawa, Z. A. , Verney, A. M. J. , Busch‐Hallen, J. F. , & De‐Regil, L. M. (2019). Multiple micronutrient supplements are more cost‐effective than iron and folic acid: Modeling results from 3 high‐burden Asian countries. Journal of Nutrition, 149(7), 1222–1229. 10.1093/jn/nxz052 [DOI] [PubMed] [Google Scholar]
- Kassebaum, N. J. , & Global Disease Burden 2013 Anemia Collaborators . (2016). The global burden of anemia. Hematology/Oncology Clinics, 30(2), 247–308. 10.1016/j.hoc.2015.11.002 [DOI] [PubMed] [Google Scholar]
- Kassebaum, N. J. , Jasrasaria, R. , Naghavi, M. , Wulf, S. K. , Johns, N. , Lozano, R. , Regan, M. , Weatherall, D. , Chou, D. P. , Eisele, T. P. , Flaxman, S. R. , Pullan, R. L. , Brooker, S. J. , & Murray, C. J. (2014). A systematic analysis of global anemia burden from 1990 to 2010. Blood, 123(5), 615–624. 10.1182/blood-2013-06-508325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavle, J. A. , & Landry, M. (2018). Community‐based distribution of iron‐folic acid supplementation in low‐ and middle‐income countries: A review of evidence and programme implications. Public Health Nutrition, 21(2), 346–354. 10.1017/S1368980017002828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanal, V. , Adhikari, M. , & Karkee, R. (2014). Low compliance with iron‐folate supplementation among postpartum mothers of Nepal: An analysis of Nepal Demographic and Health Survey 2011. Journal of Community Health, 39(3), 606–613. 10.1007/s10900-013-9806-6 [DOI] [PubMed] [Google Scholar]
- Khatri, R. B. , Mishra, S. R. , & Khanal, V. (2017). Female community health volunteers in community‐based health programs of Nepal: Future perspective. Frontiers in Public Health, 5, 181. 10.3389/fpubh.2017.00181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malla, S. (2001). Anaemia in Nepal, Review report. Kathmandu, Nepal, unpublished report.
- MoH, New ERA, & ORC Macro . (2002). Nepal demographic and health survey 2001. Calverton, Maryland, USA: Family Health Division, Ministry of Health; New ERA; and ORC Macro. [Google Scholar]
- MoH, New ERA, MI, UNICEF, & WHO . (1998). Nepal micronutrient status survey 1998. Kathmandu, Nepal: Ministry of Health, New ERA, Micronutrient Initiative, UNICEF and WHO. [Google Scholar]
- MoHP . (2007). An analytical report on national survey of female community health volunteers of Nepal. Kathmandu, Nepal: Ministry of Health and Population, Government of Nepal. [Google Scholar]
- MoHP, New ERA, & ICF International Inc . (2012). Nepal. Demographic and health survey 2011. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland. [Google Scholar]
- MoHP, New ERA, & Macro International Inc . (2007). Nepal demographic and health survey 2006. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and Macro International Inc. [Google Scholar]
- MoHP, New ERA, & Macro International Inc . (2017). Nepal demographic and health survey 2016. Kathmandu, Nepal: Ministry of Health and Population. [Google Scholar]
- MoHP, New ERA, UNICEF, EU, USAID, & CDC . (2018). Nepal national micronutrient status survey, 2016. Kathmandu, Nepal: Ministry of Health and Population, Nepal. [Google Scholar]
- Ndiaye, M. , Siekmans, K. , Haddad, S. , & Receveuro, O. (2009). Impact of a positive deviance approach to improve the effectiveness of an iron‐supplementation program to control nutritional anemia among rural Senegalese pregnant women. Food and Nutrition Bulletin, 30, 128–136. 10.1177/156482650903000204 [DOI] [PubMed] [Google Scholar]
- Nguyen, P. H. , Sanghvi, T. , Kim, S. S. , Tran, L. M. , Afsana, K. , Mahmud, Z. , Aktar, B. , & Menon, P. (2017). Factors influencing maternal nutrition practices in a large scale maternal, newborn and child health program in Bangladesh. PLoS One, 12(7), e0179873. 10.1371/journal [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisar, Y. B. , Dibley, M. J. , Mebrahtu, S. , Paudyal, N. , & Devkota, M. (2015). Antenatal iron‐folic acid supplementation reduces neonatal and under‐5 mortality in Nepal. Journal of Nutrition, 145(8), 1873–1883. 10.3945/jn.114.206565 [DOI] [PubMed] [Google Scholar]
- Nisar, Y. B. , Dibley, M. J. , & Mir, A. M. (2014). Factors associated with non‐use of antenatal iron and folic acid supplements among Pakistani women: A cross‐sectional household survey. BMC Pregnancy and Childbirth, 14, 305. 10.1186/1471-2393-14-305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osrin, D. , Vaidya, A. , Shrestha, Y. , Baniya, R. B. , Manandhar, D. S. , Adhikari, R. K. , Filteau, S. , Tomkins, A. , & Costello, A. M. (2005). Effects of antenatal multiple micronutrient supplementation on birthweight and gestational duration in Nepal: Double‐blind: randomised controlled trial. Lancet, 365(9463), 955–962. 10.1016/S0140-6736(05)71084-9 [DOI] [PubMed] [Google Scholar]
- Pachón, H. , Spohrer, R. , Mei, Z. , & Serdula, M. K. (2015). Evidence of the effectiveness of flour fortification programs on iron status and anemia: A systematic review. Nutrition Reviews, 73(11), 780–795. 10.1093/nutrit/nuv037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panday, S. , Bissell, P. , Teijlingen, E. V. , & Simkhada, P. (2017). The contribution of female community health volunteers (FCHVs) to maternity care in Nepal: A qualitative study. BMC Health Services Research, 17(1), 623. 10.1186/s12913-017-2567-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panday, S. , Bissell, P. , Teijlingen, E. V. , & Simkhada, P. (2019). Perceived barriers to accessing Female Community Health Volunteers' (FCHV) services among ethnic minority women in Nepal: A qualitative study. PLoS One, 14(6), e0217070. 10.1371/journal.pone.0217070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokharel, R. K. , Maharjan, M. R. , Mathema, P. , & Harvey, P. W. J. (2011). Success in delivering interventions to reduce maternal anemia in Nepal: A case study of the intensification of maternal and neonatal micronutrient program. Washington: A2Z, the USAID Micronutrient and Child Blindness Project. [Google Scholar]
- Proctor, E. K. , Powell, B. J. , & McMillen, J. C. (2013). Implementation strategies: Recommendations for specifying and reporting. Implementation Science, 8, 139. 10.1186/1748-5908-8-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, J. L. , Ghimire, P. , Rijal, K. R. , Maglior, A. , Hollis, S. , Andrade‐Pacheco, R. , Das Thakur, G. , Adhikari, N. , Thapa Shrestha, U. , Banjara, M. R. , Lal, B. K. , Jacobson, J. O. , & Bennett, A. (2019). Designing malaria surveillance strategies for mobile and migrant populations in Nepal: A mixed‐methods study. Malaria Journal, 18(1), 158. 10.1186/s12936-019-2791-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens, G. A. , Finucane, M. M. , De‐Regil, L. M. , Paciorek, C. J. , Flaxman, S. R. , Branca, F. , Peña‐Rosas, J. P. , Bhutta, Z. A. , Ezzati, M. , & Nutrition Impact Model Study Group (Anaemia) . (2013). Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non‐pregnant women for 1995–2011: A systematic analysis of population‐representative data. The Lancet Global Health, 1(1), e16–e25. 10.1016/S2214-109X(13)70001-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2000). Between census household indicator monitoring evaluation system (BCHIMES). Kathmandu, Nepal: United Nations Children's Fund. [Google Scholar]
- UNICEF . (2019). Nutritional care of pregnant women in South Asia: Policy environment and programme action. Kathmandu, Nepal: United Nations Children's Fund Regional Office for South Asia. [Google Scholar]
- UNICEF & WHO . (2019). UNICEF‐WHO low birthweight estimates: Levels and trends 2000–2015. Geneva: World Health Organization. [Google Scholar]
- WHO . (2001). Iron deficiency anaemia. Assessment, prevention, and control. A guide for programme managers. Geneva: World Health Organization. [Google Scholar]
- WHO . (2019). Guideline: Preventive chemotherapy to control soil‐transmitted helminth infections in at‐risk population groups. Geneva: World Health Organization. [PubMed] [Google Scholar]
- Yadav, K. D. , Yadav, U. N. , Wagle, R. R. , Thakur, D. N. , & Dhakal, S. (2019). Compliance of iron and folic acid supplementation and status of anaemia during pregnancy in the Eastern Terai of Nepal: Findings from hospital based cross sectional study. BMC Research Notes, 12(1), 127. 10.1186/s13104-019-4167-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakoob, M. Y. , & Bhutta, Z. A. (2011). Effect of routine iron supplementation with or without folic acid on anemia during pregnancy. BMC Public Health, 11(Suppl 3), S21. 10.1186/1471-2458-11-S3-S21 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE S1. Main reasons given by pregnant women who did not take any iron and folic acid supplements, 2001–2010
Data Availability Statement
The data presented in the figures were extracted from survey reports. The following survey reports are available in the public domain: 1998 Nepal Micronutrient Status Survey (https://un.info.np/Net/NeoDocs/View/8446), 2016 Nepal National Micronutrient Status Survey (https://mohp.gov.np/downloads/NNMSS%20Report%202016-Final%20Report.pdf) and 2001–2016 Nepal Demographic Health Survey (https://dhsprogram.com/data/available-datasets.cfm). The reports of the micronutrient surveys conducted by the NTAG are available on request from the corresponding author.


