Abstract
Objectives:
Research examining the relationship between loneliness and Complex Posttraumatic Stress Disorder (CPTSD) is scarce, particularly among older adults. CPTSD includes the core symptoms of PTSD along with additional symptoms reflecting ‘disturbances in self-organisation’ (DSO). This study examined the cross-sectional relationships between loneliness (emotional and social loneliness) and CPTSD symptoms (i.e., PTSD and DSO symptoms) in older adults.
Methods:
Structural equation modelling was used to examine these relationships in a nationally representative sample of United States adults aged 60–70 years (n = 456).
Results:
Controlling for covariates, emotional loneliness was associated with PTSD (β = .31) and DSO (β = .57) symptoms whereas social loneliness was only associated with DSO symptoms (β = .25). The model explained 35.0% of the variance in PTSD symptoms and 71.3% in DSO symptoms.
Conclusion:
These findings have important implications for treating and understanding PTSD/CPTSD and their correlates among older adults.
Keywords: Posttraumatic stress disorder (PTSD), complex posttraumatic stress disorder (CPTSD), loneliness, emotional loneliness, social loneliness
1. Introduction
Traumatic exposure can result in a range of mental health disorders including Posttraumatic Stress Disorder (PTSD) and Complex PTSD (CPTSD). In the eleventh version of the International Classification of Diseases (ICD-11; World Health Organization [WHO], 2018), PTSD is defined by three symptom clusters (‘re-experiencing in the here and now’, ‘avoidance’, and ‘sense of current threat’), and CPTSD is defined by these PTSD symptoms plus those reflecting ‘disturbances in self-organisation’ (DSO). These DSO symptoms are represented by three clusters (‘affective dysregulation’, ‘negative self-concept’, and ‘disturbances in relationships’), and reflect the psychiatric sequalae that often occur following multiple and prolonged trauma exposure from which escape is difficult or impossible (Shevlin, Hyland, Roberts et al., 2018). Across multiple countries, prevalence rates among the general adult population have been estimated to range between 3.4% and 6.7% for ICD-11 PTSD and between 3.8% and 7.7% for CPTSD (Cloitre et al., 2019; Hyland, Karatzias, et al., 2020; Hyland, Vallières, et al., 2020).
PTSD and CPTSD are relatively under-researched disorders among older adults (i.e., those aged 60 years and above) (WHO, 2017). Epidemiological research suggests that both lifetime and current traumatic-stress related disorders tend to decline with age (Gum et al., 2009; Kessler et al., 2005; Reynolds et al., 2016). However, recent research using a large, nationally representative sample of older adults from the United States (U.S.) indicates that a meaningful proportion of older adults are affected by ICD-11 PTSD symptoms (Fox et al., 2020a, 2020b), with 6.1% of adults aged 60 years and older meeting the lifetime symptom requirements of ICD-11 PTSD. As the global proportion of adults aged 60 years or older is expected to nearly double from 12% to 22% between the years 2015 and 2050 (WHO, 2017), it is important to examine variables that may be associated with PTSD and CPTSD in later life.
One variable of interest, common among older adults, is loneliness (Ong et al., 2016). Loneliness can be characterised as a ubiquitous, distressing experience that occurs when an individual’s social relationships are of insufficient quality (Peplau & Perlman, 1982). While loneliness is not unique to older adults (Qualter et al., 2015), older adults are disproportionately exposed to risk factors for loneliness such as retirement, the death of a loved one, development of a chronic illness, and impaired mobility (Aartsen & Jylhä, 2011; Cohen-Mansfield et al., 2016; Pinquart & Sörensen, 2001).
Loneliness is often conceptualised as a multidimensional construct (Weiss, 1973) consisting of ‘emotional loneliness’ - a perceived lack/absence of intimate relationships and close attachments - and ‘social loneliness’ - a perceived lack/absence of an engaging social network that can provide a sense of belonging and companionship (de Jong Gierveld & van Tilburg, 2006). When evaluating loneliness in later life, it can be helpful to disassemble it into social and emotional subtypes since these have different incidences and antecedents in this population (Ó’Luanaigh & Lawlor, 2008; Schnittger et al., 2012). For example, emotional loneliness has been found to have a greater effect on numerous psychopathologies compared to social loneliness (Hyland et al., 2019; McHugh & Lawlor, 2013; Peerenboom et al., 2015).
A prominent theory that aids in the understanding the contribution of loneliness towards the development of psychopathology, in general, is Hawkley and Cacioppo’s (2010) “loneliness loop”. According to this theory, individuals with the perception that they are socially isolated can often feel that they are unsafe, which triggers an implicit hypervigilance for threatening stimuli in the environment. This hypervigilance can then cause the individual to create cognitive biases such as the world is an unsafe place, therefore causing the individual to remain socially isolated, yet in turn, blaming this social isolation on the environment. The initial increase in loneliness leads to a reciprocal effect whereby loneliness is maintained through negative cognitive biases. This self-reinforcing loneliness loop can elicit feelings of hostility, stress, low self-esteem, anxiety and can also activate the neurobiological and behavioural mechanisms that contribute towards negative mental health outcomes (Hawkley & Cacioppo, 2010; Qualter et al., 2015). Given the existing longitudinal studies, although limited, on posttraumatic stress responses and loneliness, it is possible that this theory may extend to PTSD/CPTSD.
A wealth of data exists highlighting the association between PTSD, using the model of PTSD as outlined in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association [APA], 1994), and psychosocial variables such as loneliness among adults (Itzhaky et al., 2017; Kuwert et al., 2014; O’Connor, 2010; Shevlin et al., 2015; Solomon et al., 2015; Tsur et al., 2019). Moreover, longitudinal research has indicated that loneliness both predicts future (van der Velden et al., 2019) PTSD (DSM-5 model; APA, 2013), and is predicted by past (van der Velden et al., 2018) PTSD symptoms (DSM-IV model). In addition, longitudinal changes in both social and emotional loneliness are associated with longitudinal changes in DSM-IV PTSD symptoms (Fox et al., 2021) in older adults. However, there is a dearth of research regarding the association between CPTSD and loneliness. A longitudinal study of Israeli prisoners of war found that persons displaying symptoms of CPTSD were more likely to experience a general sense of loneliness later in their lives compared to those displaying symptoms of ICD-11 PTSD, or those who were asymptomatic (Zerach et al., 2019). Additionally, a general sense of loneliness has been noted among patients with CPTSD in clinical case studies (Dagan & Yager, 2019), and has been found to be associated with the three DSO symptom clusters of emotional dysregulation (Hawkley et al., 2009; Wong et al., 2016), negative self-concepts (Goswick & Jones, 1981; Hawkley & Cacioppo, 2010; Knoke et al., 2010), and disturbances in relationships (Knoke et al., 2010; Solomon & Dekel, 2008). It stands to reason, therefore, that loneliness may play an important role in contributing to, or maintaining, symptoms of CPTSD.
It is important to note that, given the recency of the release of the ICD-11 model of PTSD, the majority of the current research on the association between PTSD and loneliness was conducted using the DSM models of PTSD. The predominant differences between these models of PTSD and the ICD-11 model of PTSD are in terms of the number of symptoms and symptom clusters. For example, the DSM-IV model of PTSD consists of 17 symptoms across three symptom clusters and the DSM-5 model consists of 20 symptoms across four symptom clusters, compared to the ICD-11 PTSD model consisting of six symptoms across three clusters and CPTSD model consisting of 12 symptoms across six clusters. Research suggests that there is substantial overlap among these models of PTSD (Carmassi et al., 2013; Heeke et al., 2020; Hyland et al., 2016; O’Donnell et al., 2014; Rosellini et al., 2015), including substantial agreement between the ICD-11 and DSM-5 models of PTSD among older adults (Fox et al., 2020b). Nevertheless, it is important to be aware of these methodological differences and the discordance that may exist across PTSD diagnosis (Crespo & Gómez, 2016; Forbes et al., 2011; Hafstad et al., 2017; Hoge et al., 2014; Hyland et al., 2018; Schnyder et al., 2015; Shevlin, Hyland, Vallières et al., 2018; Weathers, 2017) when interpreting the current literature surrounding PTSD and loneliness, as the use of differing models may fail to fully capture the heterogeneous symptom profiles of the other models of PTSD (Galatzer-Levy & Bryant, 2013; Shevlin, Hyland, Vallières et al., 2018; Weathers, 2017). As such, further research is required to determine whether these findings using DSM models of PTSD can be extended to the ICD-11 model of PTSD and CPTSD.
The current study was conducted to assess the associations between social and emotional loneliness and CPTSD symptoms in a nationally representative sample of older adults from the U.S. aged 60–70 years. We chose to examine the ICD-11 model of PTSD/CPTSD rather than the DSM-5 model due to the lack of research pertaining to loneliness and both ICD-11 PTSD and CPTSD, particularly among older adults. As the ICD is the official world classification (Tyrer, 2014), it is important that this dearth of research is addressed to ensure adequate interventions can be developed to treat ICD-11 PTSD and CPTSD in older adults.
Although this age range is relatively restricted, Ogle and colleagues (2014) noted that adults in their 60s may be an ideal population for trauma-related research, as they are likely to have a wide trauma history yet are less likely to have been affected by age-related conditions such as cognitive decline and chronic illnesses.
Research has found that older adults exhibiting PTSD symptoms (across different models of DSM/ICD PTSD) are at an increased risk of experiencing future cognitive decline and physical health problems (Burri et al., 2013; Cook et al., 2017; Rafferty et al., 2018). For example, a large-scale, longitudinal study (n = 181,093) of military veterans found that older veterans with PTSD were approximately twice as likely to develop common types of dementia such as Alzheimer’s disease and vascular dementia, compared to older veterans without PTSD (Yaffe et al., 2010). Therefore, understanding the factors associated with PTSD/CPTSD symptoms in adults aged 60–70 years may have important health and clinical implications in reducing these symptoms and thereby reducing the likelihood of the future onset of conditions associated with age-related elevated risk, such as Alzheimer’s disease whereby an individual’s risk doubles every five years after the age of 65 (Qiu et al., 2009). Furthermore, given the increased impairment associated with CPTSD relative to ICD-11 PTSD (Elklit et al., 2014; Karatzias et al., 2017), understanding how different types of loneliness (i.e., social and/or emotional) are related to CPTSD symptoms may provide important information that could enhance clinical interventions.
This study had two objectives. The first was to determine the proportion of adults aged 60–70 years who met the diagnostic requirements for ICD-11 PTSD and CPTSD. For comparison, these diagnostic rates, among other key study variables, were compared to adults aged younger than 60. The second objective was to assess if social and emotional loneliness were cross-sectionally associated with PTSD symptoms and the additional DSO symptoms (of CPTSD), among adults aged 60–70 years. We hypothesised that social and emotional loneliness would be positively associated with PTSD and DSO symptoms after adjusting for a range of covariates.
2. Methods
2.1. Design, Participants and Recruitment Strategy
Participants in this study were drawn from a larger, nationally representative sample of non-institutionalised adults from the U.S., details of which can be found elsewhere (Cloitre et al., 2019). These data were collected in March 2017 by the survey research company GfK, a world-wide market research company. GfK use a nationally representative panel system of the U.S. population who are willing to participate in survey-based research. Participants were selected from the nationally representative research panel using random probability-based sampling methods. The survey design oversampled females and ethnic minorities, both at approximately a 2:1 ratio. To adjust for this oversampling, and to ensure that the data remained nationally representative, the data were weighted to represent adults aged 18–70 years in the U.S. Poststratification weights were used to account for probabilities of selection, nonresponse, and potential shortcomings in the sampling frame on the basis of age (18–29, 30–44, 45–59, 60–70), region, education, household income, and urban dwelling. The use of random probability-based sampling and poststratification weights help facilitate population-based inferences and ensure that this sample remained nationally representative.
Inclusion criteria were that respondents had to be between 18 and 70 years of age and had experienced at least one traumatic experience in their lifetime. Participants were presented with a list of 17 traumatic events that may have occurred during childhood and 14 traumatic events that may have occurred during adulthood (traumatic event types are listed in Table 1). If a participant endorsed any of the traumatic events, then they were considered to have met the inclusion criterion of experiencing at least one traumatic experience in their lifetime. In total, 3,953 individuals were contacted to take part, and 1,839 (response rate = 46.5%) volunteered and met the inclusion criteria. The survey was conducted entirely online with a median completion time of 18 minutes. Panel members received financial reimbursement for their participation in the GfK panel, and participants were incentivised to participate in this survey through entry into a raffle for prizes. Protocols of this survey received ethical approval from the research ethics committee at the National College of Ireland1, and all participants provided their informed consent. Approval for secondary analysis was granted by the ethical review board of the first author’s affiliated institution.
Table 1.
Frequency of exposure to each type of traumatic event, and whether they occurred in childhood, adulthood, or both.
| Traumatic event | Childhood %a (n)b | Adulthood %a (n)b | Both %a (n)b |
|---|---|---|---|
| Natural disaster | 7.4 (34) | 24.0 (113) | 24.0 (110) |
| Fire or explosion | 9.4 (42) | 14.2 (63) | 1.4 (11) |
| Transportation accident | 6.6 (30) | 40.3 (181) | 20.7 (86) |
| Serious accident | 3.4 (17) | 17.7 (79) | 5.5 (26) |
| Exposure to toxic substance | 1.8 (7) | 9.2 (38) | 1.5 (7) |
| Physical assault NOT by parent or caregiver | 9.5 (42) | 12.0 (68) | 8.7 (41) |
| Assault with a weapon NOT by parent or caregiver | 2.6 (10) | 11.3 (50) | 1.4 (8) |
| Sexual assault NOT by parent or caregiver | 7.5 (39) | 4.8 (29) | 3.2 (20) |
| Combat or exposure to a war-zone | 0.2 (1) | 6.7 (20) | 0.6 (5) |
| Captivity | 0.5 (4) | 0.6 (4) | 0.3 (2) |
| Serious or life-threatening illness or injury | 3.4 (14) | 30.9 (142) | 5.5 (25) |
| Witnessed a violent death | 1.3 (6) | 5.7 (24) | 0.9 (6) |
| Sudden, unexpected death of someone close to you | 3.6 (18) | 41.4 (189) | 22.4 (118) |
| Serious injury, harm or death you caused to someone else | 0.3 (3) | 2.8 (11) | 1.8 (8) |
| Childhood sexual abuse | 19.2 (100) | - | - |
| Childhood physical abuse | 17.4 (75) | - | - |
| Childhood physical neglect | 4.6 (20) | - | - |
Note:
Percentages are adjusted for the weighting of the sample;
sample size is based on the unweighted data.
All reported parameter estimates were adjusted for the weighting of the study population, whereas sample size was based on the unweighted data. Consequently, reported proportions may not correspond to the reported sample sizes. The current sample (n = 456) included respondents who were aged 60–70 from the original survey. The weighted sample included more females (54.4%, n = 317) than males (45.6%, n = 139), and the average age was 65.04 years (SD = 3.33). Most were living in a metropolitan area (82.9%, n = 391). Moreover, 29.2% (n = 129) reported that their highest level of education attained was a bachelor’s degree or higher, 33.0% (n = 136) had some college education, 29.6% (n = 160) finished high school, and 8.2% (n = 31) had not finished high school. Regarding annual household income, 44.4% (n = 172) earned $75,000 or above, 23.2% (n = 99) earned $50,000–$74,999, 18.6% (n = 104) earned $25,000-$49,999, and 13.8% (n = 81) earned less than $25,000 per year. The vast majority experienced multiple lifetime traumatic events (89.9%, n = 405) compared to a single lifetime traumatic event (10.1%, n = 50).
2.2. Measures
2.2.1. ICD-11 PTSD and CPTSD
PTSD and DSO symptoms were assessed using the International Trauma Questionnaire (ITQ; Cloitre et al., 2018). The ITQ includes 18 items and is the only validated measure of PTSD and CPTSD, as per the ICD-11 diagnostic guidelines. Six items measure each past-month PTSD symptom, and six items measure the DSO symptoms. All items are answered in relation to the participant’s most distressing traumatic event. Six items measure functional impairment including social impairment, occupational impairment, and impairment in other important areas of life (e.g., parenting or college) in relation to the PTSD and DSO symptoms, respectively. All items were rated using a five-point Likert scale (‘not at all’ = 0, ‘extremely’ = 4), and total scores for PTSD and DSO symptoms range from 0–24 with higher scores reflecting greater symptomatology.
For diagnostic purposes, a symptom was deemed to be endorsed if scored ≥ 2 (‘Moderately’), as recommended by Cloitre and colleagues (2018) based on standard practice in trauma research. In order to meet the diagnostic requirements of an ICD-11 PTSD diagnosis, an individual must endorse the presence of at least one of two ‘re-experiencing in the here and now’ symptoms, one of two ‘avoidance’ symptoms, and one of two ‘sense of current threat’ symptoms. Endorsement of at least one functional impairment indicator is also required. To meet the diagnostic requirements of an ICD-11 CPTSD diagnosis, all of the PTSD criteria must be met, and at least one of two ‘affective dysregulation’ symptoms, one of two ‘negative self-concept’ symptoms, and one of two ‘disturbances in relationships’ symptoms must be endorsed. Endorsement of at least one functional impairment indicator relating to the DSO symptoms is also required. According to the diagnostic rules outlined in the ICD-11, an individual can meet the requirements for a diagnosis of PTSD or CPTSD, but not both. Moreover, it is important to note that PTSD/CPTSD prevalence was assessed using the ICD-11 guidelines from a self-reported measure, however, to receive an official PTSD or CPTSD diagnosis, the assessment must be carried out by a clinically trained professional. The psychometric properties of the ITQ in the full sample have previously been supported (Ben-Ezra et al., 2018; Cloitre et al., 2018; Hyland et al., 2017; Vallières et al., 2018).
2.2.2. Loneliness
Emotional and social loneliness were assessed using the six-item de Jong Gierveld Loneliness Scale (de Jong Gierveld & van Tilburg, 2006). This multidimensional scale is comprised of three negatively phrased items that assess ‘emotional loneliness’ (e.g., “I experience a general sense of emptiness”) and three positively phrased items that assess ‘social loneliness’ (e.g., “there are many people I can trust completely”). Items are scored on a three-point Likert scale (‘no’ = 1, ‘more-or-less’ = 2, ‘yes’ = 3). The ‘more-or-less’ response option is merged with ‘no’ for the positive items, and ‘yes’ for the negative items (i.e., responding ‘more-or-less’ indicates loneliness), thereby dichotomising the items (0 = ‘absence of loneliness item’, 1 = ‘presence of loneliness item’). Scores on the positively phrased items are then reversed so that higher scores suggest greater levels of loneliness. Possible scores on the emotional and social loneliness dimensions respectively range from 0–3. The psychometric properties of this measure have previously been supported in large-scale epidemiological studies (de Jong Gierveld & van Tilburg, 2010).
2.2.3. Covariates
A number of sociodemographic variables were measured including age, sex (0 = male, 1 = female), urban dwelling (0 = not living in a metropolitan area, 1 = living in a metropolitan area), education, and household income. Education information was assessed using 14 categories ranging from “no formal education” to “professional or doctorate degree”. Household income was measured using 21 categories that ranged from “less than $5,000” to “$250,000 or more”. A large number of categories were used for the education and income covariates to ensure that sufficient information/variance could be obtained from the demographic variables.
Exposure to traumatic events was measured using a modified version of the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013). Participants were presented with a list of 14 common traumatic events (e.g., “natural disaster [for example, flood, hurricane, tornado, or earthquake]” or “sudden, violent death [for example, homicide; suicide]”) and indicated ‘yes’ or ‘no’ to whether each event occurred to them in ‘childhood’ (i.e., before age of 18) and in ‘adulthood’ (i.e., at or after age 18). This created a measure of 28 potential traumatic events (i.e., 14 that may have occurred during childhood and 14 during adulthood). An additional three items were extracted from the Adverse Childhood Experiences questionnaire (ACE; Felitti et al., 1998) reflecting childhood neglect, childhood physical abuse, and childhood sexual abuse. Items were summed to create three trauma variables denoting those that occurred solely during childhood, solely during adulthood, or occurred during both childhood and adulthood. This allowed us to determine the effect of the recency of the trauma (whether it occurred during childhood or adulthood) and the chronicity of the trauma (whether it occurred throughout the lifespan). The total number of traumatic events that occurred solely during childhood could range from 0–17 (consisting of 14 items from the LEC-5 and three items from the ACE); whereas the total number that occurred during adulthood or during both childhood and adulthood could range 0–14, with higher scores representing a greater number of traumatic events experienced (traumatic event types are listed in Table 1).
Following the guidelines set forth by VanderWeele (2019) these covariates were selected to control for potential confounding effects that they may have on the primary variables of interest (i.e., PTSD symptoms, DSO symptoms, emotional loneliness and/or social loneliness) (e.g., Drennan et al., 2008; Fox et al., 2020b; Gum et al., 2009; Hyland et al., 2019; Ogle et al., 2014; Tolin & Foa, 2006; Ventimiglia & Seedat, 2019; Victor & Yang, 2012).
2.3. Analytical Plan
First, the current sample of adults aged 60–70 years was compared to the remaining sample (i.e., aged 18–59 years) in relation to all study variables. PTSD symptoms, DSO symptoms, and total number of childhood, adulthood, or both childhood and adulthood trauma exposures were assessed using independent samples t-tests (and Cohen’s d as a measure of effect size; 0.2 is a small, 0.5 a medium, and 0.8 a large effect). Differences in sex, urban dwelling, PTSD, and CPTSD diagnostic rates were assessed using chi-square (χ2) test of independence with odds ratios (OR). Emotional loneliness, social loneliness, education, and household income differences were compared using Mann-Whitney U tests (with r as a measure of effect size; .1 is a small, .3 a medium, and .5 a large effect), given the ordinal nature of the variables.
Second, zero-order correlations were used to determine the bivariate associations among all observed study variables. Spearman’s rho (ρ) was used for bivariate associations that involved at least one categorical variable of more than two levels (i.e., social and emotional loneliness, education, and household income), whereas, Pearson’s r coefficient was used for the remaining bivariate associations.
Third, structural equation modelling (SEM) techniques were applied to examine the relationships between social and emotional loneliness, and PTSD and DSO symptoms, while controlling for exogenous covariates (age, sex, urban dwelling, education, household income, and total number of traumatic events experienced in childhood, adulthood, or both). SEM is advantageous as it can parse out measurement error thereby yielding more accurate parameter estimates (Bollen, 1989). Furthermore, multiple outcomes can be measured simultaneously, reducing Type I errors associated with multiple comparisons. Prior to evaluating the structural model, it was first necessary to evaluate the fit of the measurement models (i.e., the specification of the latent variables only) (Anderson & Gerbing, 1988). Model fit was determined using several goodness-of-fit indices (Hu & Bentler, 1999): A non-significant χ2 indicates excellent model fit; however, this test becomes limited in its use at larger sample sizes, therefore, a significant result (p < .05) should not lead to the rejection of a model (Tanaka, 1987). In addition, Comparative Fit Index (CFI; Bentler, 1990) and Tucker-Lewis Index (TLI; Tucker & Lewis, 1973) values ≥ .90 indicate adequate model fit. Additionally, Root Mean Square Error of Approximation (RMSEA; Steiger, 1990) values ≤ .08 suggest adequate model fit.
Due to the nonnormality of the data, as indicated by significant Mardia’s multivariate normality tests (all p < .001), the second-order measurement model of CPTSD was estimated using the robust maximum likelihood (MLR) estimator as this estimator is robust to non-normally distributed data and can account for concerns of multivariate non-normality. Given the dichotomous nature of the loneliness items, the two-factor loneliness (social and emotional) measurement model was estimated using the robust weighted least squares estimator (WLSMV) estimator, as this estimator performs best with categorical data (Brown, 2006). A one-factor model of loneliness, consisting of a general loneliness latent variable, was compared to a two-factor loneliness model whereby we distinguished between social loneliness and emotional loneliness. The models were compared using change (Δ) in the model fit indices, whereby ΔCFI and ΔTLI ≥ .010, and ΔRMSEA ≥ .015 indicate significant change in model fit (Chen, 2007; Cheung & Rensvold, 2002; Putnick & Bornstein, 2016). Moreover, the structural model was estimated using the WLSMV estimator. All analyses were conducted in Mplus 8.2 (Muthén & Muthén, 2018).
We used composite reliability (ρc) to estimate the internal reliability of the PTSD, DSO, and emotional and social loneliness items. Composite reliability is superior to Cronbach’s alpha as it estimates the reliability of items without the strict assumption of tau-equivalence (Graham, 2006; Raykov, 1997). Bagozzi and Yi (1988) suggest that composite reliability values ≥ .60 are acceptable. In order to estimate the composite reliabilities of the emotional and social loneliness measures, we used the method outlined by Raykov and colleagues (2010) for estimating composite reliability for measures with dichotomous items.
Missing data were minimal, with the proportion of missingness on all variables ranging from 0% to 3.9%, with a mean of 0.81%. Missing data were handled using full information maximum likelihood (FIML) when a model was estimated using the MLR estimator; whereas models estimated using the WLSMV estimator handled missing data using the default (Mplus) pairwise deletion method.
3. Results
3.1. Comparison of Adults aged 60–70 to those under 60
Among the study variables, adults aged 60–70 years reported significantly (t[659.76] = 4.30 p <.001, d = 0.22) lower PTSD symptoms (M = 2.88, Mdn = 1.00, SD = 3.86) compared to adults aged under 60 years (M = 3.95, Mdn = 2.00, SD = 5.15). Similarly, older adults (M = 3.33, Mdn = 2.00, SD = 3.91) reported significantly lower DSO symptoms (t[650.85] = 6.14 p <.001, d = 0.32) symptoms compared to adults aged younger than 60 years (M = 4.95, Mdn = 3.00, SD = 5.24). There were significant differences in the number of individuals who met the diagnostic requirements for ICD-11 PTSD (χ2 [1, n = 1,818] = 6.72, p = .010, OR = 0.28 [95% CI 0.10, 0.78]) with 1.2% (n = 11; 95% CI = 0.1%, 2.4%) of adults aged 60–70 years meeting the diagnostic requirements for PTSD, compared to 3.9% (n = 62; 95% CI = 2.9%, 4.9%) of those aged younger than 60 years. A similar trend was observed for CPTSD (χ2 [1, n = 1,818] = 5.23, p = .021, OR = 0.38 [95% CI 0.17, 0.89]), with an additional 1.6% (n = 5; 95% CI = 0.0%, 3.0%) of those aged 60–70 years meeting the diagnostic requirements of CPTSD, compared to 4.4% (n = 75; 95% CI = 3.3%, 5.4%) of adults aged below 60 years. Older adults (M = 0.99, Mdn = 1.00, SD = 1.17) reported experiencing significantly fewer traumatic events that occurred solely in childhood (t[610.05] = 4.19 p < .001, d = 0.22), compared to adults aged younger than 60 years (M = 1.29, Mdn = 1.00, SD = 1.40). Older adults (M = 2.21, Mdn = 2.00, SD = 1.73) reported experiencing a higher number of traumatic events that occurred solely in adulthood (t[465.97] = −8.09 p < .001, d = −0.54), compared to adults aged younger than 60 years (M = 1.41, Mdn = 1.00, SD = 1.41). There was no difference between the number of traumatic events experienced in both childhood and adulthood (t[1,837] = 0.25 p = .804, d = 0.01) in older adults (M = 0.98, Mdn = 1.00, SD = 1.32) compared to adults aged younger than 60 years (M = 1.00, Mdn = 0.00, SD = 1.59). Older adults (M = 1.61, Mdn = 2.00, SD = 1.32) reported lower scores on social loneliness (Z = 2.28, p = .023, r = .05) compared to adults aged younger than 60 years (M = 1.77, Mdn = 2.00, SD = 1.31). Similarly, older adults (M = 0.90, Mdn = 1.00, SD = 1.03) reported lower scores on emotional loneliness (Z = 3.28, p = .001, r = .08) compared to adults aged younger than 60 years (M = 1.16, Mdn = 1.00, SD = 1.16). However, the effect sizes were very small. There were no significant differences regarding sex (χ2 [1, n = 1,839] = 1.027, p = .311, OR = 1.13 [95% CI 0.93, 1.43]), urban dwelling (χ2 [1, n = 1,839] = 3.65, p = .056, OR = 0.74 [95% CI 0.54, 1.01]), education (Z = 1.15, p = .250, r = .03), or household income (Z = 1.18, p = .240, r = .03).
3.2. Bivariate Correlations
The bivariate association between DSO symptoms and emotional loneliness was strong (ρ = .56, p < .001) and social loneliness was moderate-strong (ρ = .48, p < .001). The associations between PTSD symptoms and emotional loneliness (ρ = .19, p < .001) and social loneliness (ρ = .17, p = .001) were both weak. See Table 2 for all correlations.
Table 2.
Zero-order correlations between all observed study variables.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PTSD symptoms | – | |||||||||||
| 2. DSO symptoms | .47*** | – | ||||||||||
| 3. Emotional loneliness | .19*** | .56*** | – | |||||||||
| 4. Social loneliness | .17** | .48*** | .36*** | – | ||||||||
| 5. Age | .03 | .01 | .04 | −.20*** | – | |||||||
| 6. Sexa | .02 | .08 | .10 | −.05 | .01 | – | ||||||
| 7. Urban dwellingb | .05 | −.09 | −.13* | .02 | −.05 | .10 | – | |||||
| 8. Education | −.02 | .09 | −.06 | .01 | .02 | .01 | .04 | – | ||||
| 9. Household income | −.10 | −.16** | −.25*** | −.08 | −.13* | −.15** | .12* | .38*** | – | |||
| 10. Trauma (childhood only) | .40*** | .26*** | .25*** | .25*** | −.01 | −.03 | .09 | −.01 | −.12* | – | ||
| 11. Trauma (adulthood only) | .22*** | .15** | .08 | −.04 | .11* | −.01 | .00 | .07 | −.09 | .04 | – | |
| 12. Trauma (childhood and adulthood) | .24*** | .15** | .17** | .13** | .14** | −.08 | −.03 | .04 | −.07 | .28*** | −.04 | – |
Note: PTSD = posttraumatic stress disorder; DSO = disturbances in self-organisation;
sex coded as 0 = male, 1 = female;
urban dwelling coded as 0 = not living in a metropolitan area, 1 = living in a metropolitan area.
Statistical significance:
p < .05;
p < .01;
p < .001.
3.3. Measurement Model: PTSD and DSO Two-factor Second-order Model
The latent structure (see Figure 1) of PTSD and DSO was represented using a two factor (PTSD and DSO) second-order model, where PTSD explains the variance/co-variance between the three first-order factors of ‘Re-experiencing in the here and now’, ‘Avoidance’, and ‘Sense of Current Threat’ and DSO explains the variance/co-variance between the three first order factors of ‘Affective Dysregulation’, ‘Negative Self-concept’, and ‘Disturbances in Relationships’. This model initially produced a Heywood case (factor loading greater than one) between the DSO second-order factor and the ‘affective dysregulation’ first-order factor producing a negative residual variance. An exceptionally large factor loading between DSO and ‘affective dysregulation’ has been noted previously (e.g., Karatzias et al., 2016). As this residual variance was non-significant, the model was re-evaluated with the residual variance fixed to zero (Chen et al., 2001), which also constrains the factor loading to one. The re-specified model demonstrated excellent statistical fit to the data (χ2[48] = 71.42, p = .016; CFI = .981; TLI = .974; RMSEA = .033 [90% CI .015, .048]). The inter-factor correlation between PTSD and DSO was .63, and all factor loadings were positive and significant (p < .001) ranging from .59–1.00. Composite reliability estimates for the PTSD (ρc = .87) and DSO (ρc = .93) factors demonstrated satisfactory internal reliability.
Figure 1.
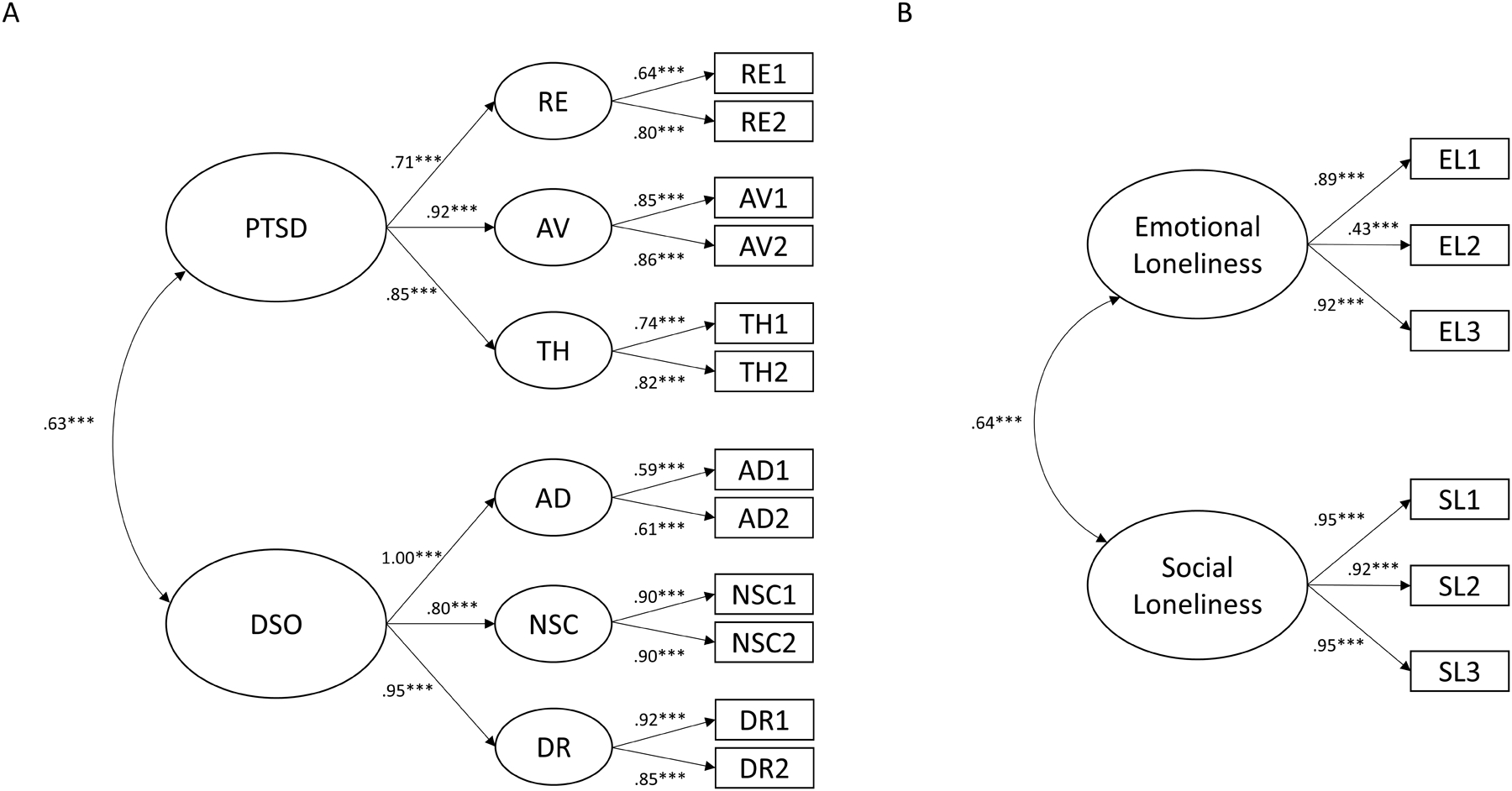
Two-factor higher-order model of CPTSD (PTSD and DSO) and two-factor model of loneliness (social loneliness and emotional loneliness). PTSD = posttraumatic stress disorder; DSO = disturbances in self-organisation; RE = re-experiencing in the here and now; AV = avoidance; TH = sense of current threat; AD = affective dysregulation; NSC = negative self-concept; DR = disturbances in relationships; EL = emotional loneliness; SL = social loneliness.
Statistical significance: *p < .05; **p < .01; ***p < .001.
3.4. Measurement Model: Social and Emotional Loneliness
A one-factor model of loneliness provided adequate fit to the data (χ2[9] = 94.53, p < .001; CFI = .963; TLI = .939; RMSEA = .145 [90% CI .119, .172]). However, a two-factor model (social and emotional loneliness) of loneliness provided excellent statistical fit (χ2[8] = 14.57, p = .068; CFI = .997; TLI = .995; RMSEA = .042 [90% CI .000, .077]). Additionally, as the ΔCFI and ΔTLI values > .010, and ΔRMSEA > .015, this suggests that the two-factor model provided superior statistical fit to the data. The inter-factor correlation between social and emotional loneliness was .64, and all factor loadings were positive and significant (p < .001) ranging from .43–.95 (see Figure 1 for all parameter estimates). Composite reliability estimates for the social (ρc = .86) and emotional (ρc = .67) loneliness factors demonstrated acceptable internal reliability.
3.5. Structural Model: PTSD, DSO, and Social and Emotional Loneliness
The SEM model (see Figure 2) demonstrated satisfactory fit to the data (χ2[252] = 482.39, p < .001; CFI = .924; TLI = .910; RMSEA = .045 [90% CI .039, .051]) and explained 35.0% of the variance in PTSD symptoms and 71.3% of the variance in DSO symptoms.
Figure 2.
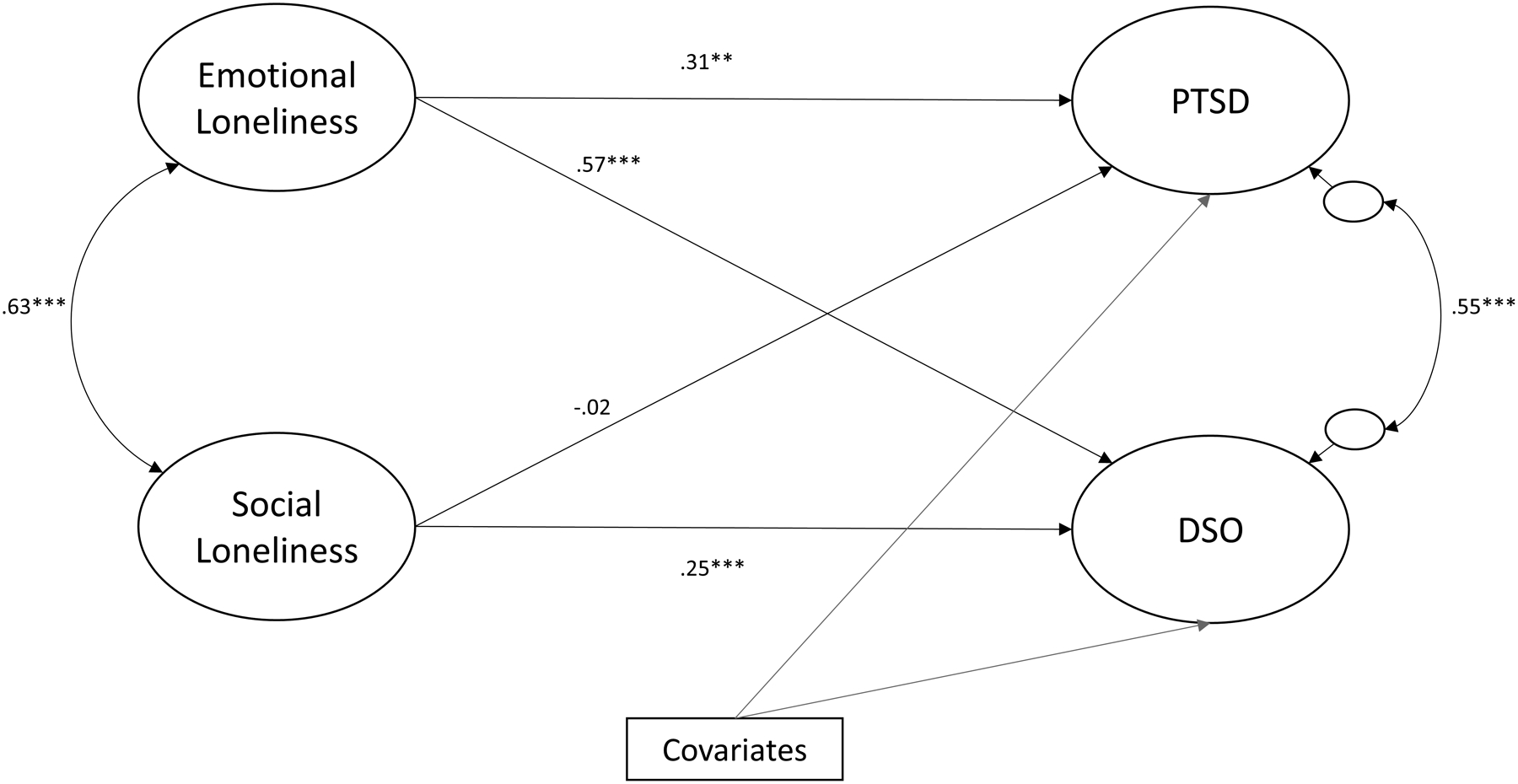
Structural model illustrating the relationship (standardised estimates) between loneliness (emotional and social loneliness), and PTSD symptoms and DSO symptoms. Individual exogenous covariate pathways are omitted for visual clarity. PTSD = posttraumatic stress disorder; DSO = disturbances in self-organisation.
Statistical significance: *p < .05; **p < .01; ***p < .001.
While controlling for the exogenous covariates, emotional loneliness (β = .31, p = .001), but not social loneliness (β = −.02, p = .817), was associated with PTSD symptoms. Emotional loneliness (β = .57, p < .001) and social loneliness (β = .25, p < .001) were associated with DSO symptoms. Of the covariates in the model, the total number of childhood trauma exposures (β = .39, p < .001), adulthood trauma exposures (β = .21, p < .001), and both childhood and adulthood trauma exposures (β = .14, p = .001) were associated with PTSD symptoms. The total number of childhood trauma exposures (β = .28, p < .001), adulthood trauma exposures (β = .13, p = .028), both childhood and adulthood trauma exposures (β = .09, p = .049), and living in a rural area (β = −.14, p = .027) were associated with DSO symptoms (see Table 3 for full details).
Table 3.
SEM model of PTSD, DSO, and social and emotional loneliness.
| PTSD | DSO | |||
|---|---|---|---|---|
| B (SE) | β (SE) | B (SE) | β (SE) | |
| Latent variables | ||||
| Emotional loneliness | .11** (.04) | .31 (.10) | .31*** (.05) | .57 (.06) |
| Social loneliness | −.01 (.03) | −.02 (.09) | .13*** (.04) | .25 (.06) |
| Covariates | ||||
| Age | .00 (.01) | −.02 (.05) | −.01 (.01) | −.05 (.06) |
| Sexa | .04 (.04) | .06 (.06) | .08 (.06) | .08 (.06) |
| Urban dwellingb | .01 (.05) | .01 (.07) | −.18* (.08) | −.14 (.06) |
| Education | −.01 (.01) | −.04 (.06) | .02 (.02) | .09 (.06) |
| Household income | .00 (.00) | −.04 (.06) | −.01 (.01) | −.07 (.06) |
| Trauma (childhood only) | .10*** (.02) | .39 (.04) | .12*** (.03) | .28 (.05) |
| Trauma (adulthood only) | .04*** (.01) | .21 (.05) | .04* (.02) | .13 (.06) |
| Trauma (childhood and adulthood) | .03** (.01) | .14 (.04) | .04* (.02) | .09 (.05) |
Note: PTSD = posttraumatic stress disorder; DSO = disturbances in self-organisation; B = unstandardised estimates; β = standardised estimates; SE = standard error;
sex coded as 0 = male, 1 = female;
urban dwelling coded as 0 = not living in a metropolitan area, 1 = living in a metropolitan area.
Statistical significance:
p < .05;
p < .01;
p < .001.
4. Discussion
The primary objectives of this study were to determine the proportion of older adults who met the diagnostic requirements for PTSD and CPTSD, and to determine the relationship between social and emotional loneliness and CPTSD symptoms. We hypothesised that both social and emotional loneliness would be positively associated with PTSD and DSO symptoms, while controlling for a number of covariates. The main study hypothesis was partially supported in that emotional loneliness was associated with PTSD and DSO symptoms; however, social loneliness was associated with DSO symptoms but not PTSD symptoms. Moreover, we found that adults aged 60–70 years were approximately 3.5 times less likely to meet the diagnostic requirements for PTSD and 2.5 times less likely to meet the diagnostic requirements for CPTSD, compared to adults aged younger than 60 years.
These findings align with the wider PTSD literature which has consistently demonstrated a decline in PTSD prevalence among adults aged 60 years and older (Gum et al., 2009; Kessler et al., 2005; Reynolds et al., 2016), and an association between loneliness and PTSD (Itzhaky et al., 2017; Kuwert et al., 2014; O’Connor, 2010; Shevlin et al., 2015; Solomon et al., 1991, 2015; Tsur et al., 2019; van der Velden et al., 2018, 2019), and adds to a small-but-growing literature that loneliness is related to symptoms of CPTSD (Dagan & Yager, 2019; Zerach et al., 2019). To the best of our knowledge, this is the first study to examine the relationship between subtypes of loneliness and CPTSD symptoms. The large effect of emotional loneliness and small-moderate effect of social loneliness on DSO symptoms suggest that these subtypes of loneliness may play an important role in the development of CPTSD. However, given the cross-sectional nature of this study, it is also possible that the reverse relationship is true, in that CPTSD symptoms may induce feelings of loneliness. Future longitudinal research will be required to determine the temporal relationship between these variables.
Loneliness may be associated with increased PTSD/CPTSD symptoms through a number of different pathways. For instance, loneliness is associated with sleep problems in older adults (Matthews et al., 2017; McHugh & Lawlor, 2013) which have also been found to be associated with both ICD-11 PTSD and CPTSD symptomatology (Dagan & Yager, 2019; Elklit et al., 2014; Grossman et al., 2019). It has been posited that loneliness and a lack of a secure social environment is associated with sleep problems due to an increase in hypervigilance for threat (Cacioppo & Cacioppo, 2014; Hom et al., 2017). This increase in hypervigilance for threat within one’s environment results in the individual remaining alert and prepared to fight threats while they are trying to sleep (Cacioppo & Cacioppo, 2014; Hom et al., 2017) and, thus, results in poorer sleep quality and sleep problems. Grossman and colleagues (2019) found, within a female sample of captivity survivors, that 95% of those who met the diagnostic requirements for CPTSD, also presented with insomnia. The authors proposed that a loneliness-induced sense of hypervigilance at night might partially explain the observed relationship between CPTSD symptoms and loneliness. Furthermore, following trauma exposure, hyperarousal has been hypothesised to be an important factor that leads to trauma-induced insomnia that results in the development of PTSD symptomatology (Sinha, 2016). As such, it is possible that increasing one’s risk for hyperarousal (due to loneliness) may contribute towards the development of risk factors, such as sleep problems, that increase the likelihood of developing PTSD/CPTSD symptomatology.
Loneliness is also associated with increased negative cognitive biases (Cacioppo & Hawkley, 2009) which can predict future PTSD symptoms and treatment outcomes (Brown et al., 2019). The relationship between PTSD/CPTSD and loneliness may also be bidirectional (Fox et al., 2021). For example, increased DSM-IV PTSD symptoms, namely avoidance symptoms (Fredman et al., 2017), are associated with relational difficulties that may induce loneliness (Solomon et al., 2015; Solomon & Dekel, 2008). Moreover, as social withdrawal can be used as a form coping with DSM-IV PTSD symptoms (Thompson et al., 2018), this behaviour may also lead to increased feelings of loneliness among older adults (Hawkley & Cacioppo, 2010; McHugh Power et al., 2019). Additionally, it is plausible that the DSO symptoms may lead to increased difficulty in maintaining close relationships and thus result in increased feelings of loneliness.
These findings provide a useful addition to the trauma literature by highlighting the different associations that social and emotional loneliness have with the DSO symptoms of CPTSD. Specifically, while social loneliness had a small-to-moderate sized effect on DSO symptoms, emotional loneliness had a large effect on these symptoms. This suggests that emotional loneliness, in particular, may be especially important in the conceptualization and treatment of CPTSD among older adults. As older adults may become more vulnerable to emotional loneliness as they age (Ó’Luanaigh & Lawlor, 2008), finding ways to help these people build and maintain close attachments is an important social and clinical objective. This finding is in line with the wider loneliness literature noting a greater association between emotional loneliness and poorer outcomes, compared to social loneliness. For instance, emotional loneliness had been found to be more predictive of both psychiatric and physical health concerns such as increased anxiety and depressive symptoms, poorer psychological wellbeing and sleep quality, and all-cause mortality (Hyland et al., 2019; McHugh & Lawlor, 2013; OʼSúilleabháin et al., 2019; Peerenboom et al., 2015).
These results may aid in identifying qualitative differences between PTSD and CPTSD. Exposure to trauma can lead to feelings of alienation from others and a disconnect from society (DePrince et al., 2011; Solomon et al., 2015; Solomon & Dekel, 2008). These feelings of alienation and disconnect from close relationships, and also from the wider community may, in theory, contribute to the self-concept and relational difficulties that are inherent to CPTSD. Indeed, prior to the formulation of CPTSD in ICD-11, Herman (1992) wrote that feelings of emptiness, aloneness, and disconnection from others are common features of individuals who have experienced repeated, prolonged, and interpersonal forms of trauma. Notably, CPTSD most typically emerges from prolonged and multiple forms of trauma (i.e., complex trauma) but also can result from single incidents, such as an event in which there is a social/attachment loss (e.g., the unexpected or violent death of a loved one).
As this study used a cross-sectional design, it is not possible to infer the direction of effects. As such, it is possible that CPTSD symptoms engender feelings of loneliness, and not vice-versa, and thus have no impact on the treatment of CPTSD. Nevertheless, while evidence synthesis attempts reveal limited effectiveness of interventions aimed at reducing loneliness, the largest effects are observed for those aimed at reducing maladaptive social cognitions (Cacioppo et al., 2015; Jarvis et al., 2020; Mann et al., 2017; Masi et al., 2011). Evidence has also been found for behavioural and social interventions to reduce loneliness, such as volunteer-based interventions among veterans (Matthieu et al., 2017). Alternatively, technology-based interventions have been found to be effective in alleviating loneliness, among older adults (Poscia et al., 2018). If it is the case that the association between loneliness and CPTSD arises because loneliness causes or exacerbates CPTSD symptomatology, then intervening on loneliness may exert an ameliorative effect on CPTSD. Given the effectiveness of interventions targeting maladaptive social cognitions in reducing loneliness, and the association between reducing negative post-trauma cognitions and positive PTSD treatment outcomes (Brown et al., 2019), these types of interventions may be particularly beneficial. As our findings indicate a strong relationship between emotional loneliness and CPTSD symptoms, distinguishing between subtypes of loneliness in order to specifically target emotional loneliness may be particularly beneficial for adapting existing treatment protocols for CPTSD in older adults. Furthermore, as there was no effect observed between social loneliness and PTSD symptomatology, it is possible that ICD-11 PTSD interventions may benefit from focusing on assuaging emotional loneliness, rather than social loneliness, during treatment. Of course, further, longitudinal research is required before any definitive conclusions can be drawn regarding treatment.
In contrast, meta-analytic findings (Karatzias et al., 2019) suggest that standard PTSD interventions may be effective in reducing symptoms of CPTSD, most notably the ‘negative self-concept’ and ‘disturbances in relationships’ symptom clusters. As such, if it is the case that the reverse-association is true, in that CPTSD/PTSD symptoms cause or exacerbate loneliness, then effective interventions for CPTSD/PTSD may aid in alleviating loneliness, such as cognitive behavioural therapies (CBT). For example, Cognitive Processing Therapy (CPT; Resick & Schnicke, 1992), a type of CBT, aims to address dysfunctional thinking patterns associated with trauma, such as negative beliefs about the world and others, and teach individuals to develop healthy and adaptive thinking styles. It is possible that addressing negative cognitions associated with trauma, such as the distrust of others, may also address feelings of loneliness. Similar approaches are taken in some loneliness interventions, including those that aim to address maladaptive social cognitions about others and negative automatic thoughts regarding social interactions (Cacioppo et al., 2015; Mann et al., 2017; Masi et al., 2011). As CBT treatments are effective at reducing PTSD symptoms and appear to be somewhat effective at reducing the additional DSO symptoms of CPTSD (Karatzias et al., 2019), it is possible that CBT style interventions may be useful in reducing feelings of loneliness. This might be particularly relevant for alleviating emotional loneliness, given the strong and moderate relationships found with the DSO symptoms and core PTSD symptoms, respectively. As such, targeting the negative cognitions associated with intimate relationships and close attachments (i.e., those associated with emotional loneliness) may be particularly beneficial in preventing, or mitigating, the development of emotional loneliness in older adults, following trauma exposure. In addition, given the association with PTSD symptoms and risk factors of loneliness, such as relational difficulties (Fredman et al., 2017; Solomon et al., 2015; Solomon & Dekel, 2008) and social withdrawal (Hawkley & Cacioppo, 2010; McHugh Power et al., 2019; Thompson et al., 2018), reducing the symptoms of PTSD may lead to a reduction in these risk factors of loneliness, thereby preventing feelings of loneliness from developing. This is, of course, speculative with future longitudinal research being needed to accurately parse the relationship between PTSD/CPTSD and loneliness.
Symptoms of PTSD have been found to fluctuate and re-emerge in later life (Chopra et al. 2014). This might be possibly due to age-related normative events such as retirement, bereavements, and worsening physical health (Pless Kaiser et al., 2019). For example, retired individuals might have more opportunity to reflect on their life and may, therefore, recall early traumatic memories (Solomon et al., 2012) or veterans who begin to suffer from impaired mobility may re-experience the sense of vulnerability they felt when injured in combat (Pless Kaiser et al., 2019), leading to PTSD re-emerging in later life. It is possible that loneliness may precede the re-emerging of symptoms in later life, highlighting the importance of identifying and treating loneliness in later life. Similarly, if PTSD/CPTSD symptoms precede loneliness, then it is also possible that re-emerging symptoms in later life might also lead to increased loneliness, which is associated with numerous forms of psychopathology (Beutel et al., 2018; Luo et al., 2012; Wang et al., 2018), further highlighting loneliness as a clinically meaningful construct among trauma-exposed older adults.
A major strength of this study is the use of a nationally representative sample of adults aged 60–70 in conjunction with a validated and reliable questionnaire for assessing CPTSD symptoms (ITQ; Cloitre et al., 2018). Moreover, the use of SEM allows us to estimate more accurate parameter estimates in examining the relationship between loneliness and PTSD/CPTSD symptoms. To our knowledge, this is the first study to examine the relationship between loneliness and CPTSD using an older adult-specific sample. However, there are a number of limitations associated with this study that should be acknowledged. First, the current study used a nationally representative household sample of older adults residing in the U.S., therefore, these inferences may not be generalisable to older adults in other nations, or to those in clinical settings. Second, participants were incentivised to take part in this study through entry into a raffle. This may affect the generalisability of the findings by resulting in a biased sample, with disadvantaged participants being more likely to volunteer to participate (Cleary et al., 2008). Third, it is also important to note that the multidimensional structure of the loneliness measure used (de Jong Gierveld Loneliness Scale; de Jong Gierveld & van Tilburg, 2006) has previously been criticised to reflect, at least in part, a method effect associated with the wording of the positively phrased items, compared to the negatively phrased items (Penning et al., 2014). This type of method effect can lead to biased estimates. Furthermore, negatively worded items have been found to yield less item information which can lead to less precise estimates (Sliter & Zickar, 2013). Fourth, as this study used a cross-sectional design it was not possible to infer the temporal ordering among the observed relationships.
Future studies should aim to further examine the relationship between social and emotional loneliness and PTSD/CPTSD symptomatology. Using additional waves of data, the precise pathways explaining this relationship can be delineated. Moreover, identifying the temporal relationship (i.e., whether it is unidirectional or bidirectional) has important implications for the development of effective interventions to target PTSD/CPTSD symptoms among older adults. Moreover, studies should also attempt to examine the impact of loneliness-based interventions (such as those designed to treat maladaptive cognitions) on PTSD/CPTSD symptoms. In this study, we have demonstrated an association between social and emotional loneliness and CPTSD symptomatology in a sample of older adults. Moreover, our findings highlight a potential difference between social and emotional loneliness regarding PTSD and DSO symptoms, with emotional loneliness being associated with both PTSD and DSO symptoms, whereas social loneliness was only related to the DSO symptoms. These findings have important implications for understanding the qualitative differences between PTSD and CPTSD, and potential clinical implications for the treatment of PTSD and CPTSD among older adults.
Acknowledgements:
Funding for the data used in this study was supported by the National Institutes of Mental Health (Grant number R01 MH08661). The funding source did not have any role in the study design, analysis or interpretation of the data, writing of the manuscript, or in the decision to submit this manuscript for publication.
Footnotes
Conflict of interest: On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics statement: Protocols for the collection of data that was used in this study received ethical approval from the research ethics committee at the National College of Ireland, and all participants provided their informed consent. Approval for secondary analysis was granted by the ethical review board at Maynooth University.
National College of Ireland was a secondary affiliation to the authors: R. Fox, P. Hyland, and J. McHugh Power.
References
- Aartsen M, & Jylhä M (2011). Onset of loneliness in older adults: Results of a 28 year prospective study. European Journal of Ageing, 8(1), 31–38. 10.1007/s10433-011-0175-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Anderson JC, & Gerbing DW (1988). Structural Equation Modeling in Practice: A Review and Recommended Two-Step Approach. Psychological Bulletin, 103(3), 411–423. 10.1037/0033-2909.103.3.411 [DOI] [Google Scholar]
- Bagozzi RP, & Yi Y (1988). On the evaluation of structural equation models. Journal of the Academy of Marketing Science, 16(1), 74–94. 10.1007/BF02723327 [DOI] [Google Scholar]
- Ben-Ezra M, Karatzias T, Hyland P, Brewin CR, Cloitre M, Bisson JI, Roberts NP, Lueger-Schuster B, & Shevlin M (2018). Posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) as per ICD-11 proposals: A population study in Israel. Depression and Anxiety, 35(3), 264–274. 10.1002/da.22723 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, Wiltink J, Wild PS, Münzel T, Lackner KJ, & Tibubos AN (2017). Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry, 17(1), 97. 10.1186/s12888-017-1262-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA (1989). Structural equations with latent variables. Wiley. [Google Scholar]
- Brown LA, Belli GM, Asnaani A, & Foa EB (2019). A Review of the Role of Negative Cognitions About Oneself, Others, and the World in the Treatment of PTSD. Cognitive Therapy and Research, 43(1), 143–173. 10.1007/s10608-018-9938-1 [DOI] [Google Scholar]
- Brown TA (2006). Confirmatory factor analysis for applied research. Guilford Press. [Google Scholar]
- Burri A, Maercker A, Krammer S, & Simmen-Janevska K (2013). Childhood Trauma and PTSD Symptoms Increase the Risk of Cognitive Impairment in a Sample of Former Indentured Child Laborers in Old Age. PLoS ONE, 8(2), e57826. 10.1371/journal.pone.0057826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, & Cacioppo S (2014). Social relationships and health: The toxic effects of perceived social isolation. Social and Personality Psychology Compass, 8(2), 58–72. 10.1111/spc3.12087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, & Hawkley LC (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13(10), 447–454. 10.1016/j.tics.2009.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT (2015). Loneliness: clinical import and interventions. Perspectives on Psychological Science : A Journal of the Association for Psychological Science, 10(2), 238–249. 10.1177/1745691615570616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C, Akiskal HS, Yong SS, Stratta P, Calderani E, Massimetti E, Akiskal KK, Rossi A, & Dell’Osso L (2013). Post-traumatic stress disorder in DSM-5: Estimates of prevalence and criteria comparison versus DSM-IV-TR in a non-clinical sample of earthquake survivors. Journal of Affective Disorders, 151(3), 843–848. 10.1016/j.jad.2013.07.020 [DOI] [PubMed] [Google Scholar]
- Chen FF (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. 10.1080/10705510701301834 [DOI] [Google Scholar]
- Chen F, Bollen KA, Paxton P, Curran PJ, & Kirby JB (2001). Improper solutions in structural equation models: Causes, consequences, and strategies. Sociological Methods & Research, 29(4), 468–508. 10.1177/0049124101029004003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung GW, & Rensvold RB (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 9(2), 233–255. 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- Chopra MP, Zhang H, Pless Kaiser A, Moye JA, Llorente MD, Oslin DW, & Spiro III A (2014). PTSD is a chronic, fluctuating disorder affecting the mental quality of life in older adults. The American Journal of Geriatric Psychiatry, 22(1), 86–97. 10.1016/j.jagp.2013.01.064 [DOI] [PubMed] [Google Scholar]
- Cleary M, Walter G, & Matheson S (2008). The challenge of optimising research participation: Paying participants in mental health settings. Acta Neuropsychiatrica, 20(6), 286–290. 10.1111/j.1601-5215.2008.00346.x [DOI] [PubMed] [Google Scholar]
- Cloitre M, Hyland P, Bisson JI, Brewin CR, Roberts NP, Karatzias T, & Shevlin M (2019). ICD-11 posttraumatic stress disorder and complex posttraumatic stress disorder in the United States: A population-based study. Journal of Traumatic Stress, 32(6), 833–842. 10.1002/jts.22454 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Shevlin M, Brewin CR, Bisson JI, Roberts NP, Maercker A, Karatzias T, & Hyland P (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. 10.1111/acps.12956 [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Hazan H, Lerman Y, & Shalom V (2016). Correlates and predictors of loneliness in older-adults: A review of quantitative results informed by qualitative insights. International Psychogeriatrics, 28(4), 557–576. 10.1017/S1041610215001532 [DOI] [PubMed] [Google Scholar]
- Cook JM, McCarthy E, & Thorp SR (2017). Older Adults with PTSD: Brief State of Research and Evidence-Based Psychotherapy Case Illustration. American Journal of Geriatric Psychiatry, 25(5), 522–530. 10.1016/j.jagp.2016.12.016 [DOI] [PubMed] [Google Scholar]
- Crespo M, & Gómez MM (2016). Diagnostic concordance of DSM-IV and DSM-5 posttraumatic stress disorder (PTSD) in a clinical sample. Psicothema, 28(2), 161–166. 10.7334/psicothema2015.213 [DOI] [PubMed] [Google Scholar]
- Dagan Y, & Yager J (2019). Addressing Loneliness in Complex PTSD. The Journal of Nervous and Mental Disease, 207(6), 433–439. 10.1097/NMD.0000000000000992 [DOI] [PubMed] [Google Scholar]
- de Jong Gierveld J, & van Tilburg T (2006). A 6-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Research on Aging, 28(5), 582–598. 10.1177/0164027506289723 [DOI] [Google Scholar]
- de Jong Gierveld J, & van Tilburg T (2010). The De Jong Gierveld short scales for emotional and social loneliness: Tested on data from 7 countries in the UN generations and gender surveys. European Journal of Ageing, 7(2), 121–130. 10.1007/s10433-010-0144-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePrince AP, Chu AT, & Pineda AS (2011). Links between specific posttrauma appraisals and three forms of trauma-related distress. Psychological Trauma: Theory, Research, Practice, and Policy, 3(4), 430–441. 10.1037/a0021576 [DOI] [Google Scholar]
- Drennan J, Treacy M, Butler M, Byrne A, Fealy G, Frazer K, & Irving K (2008). The experience of social and emotional loneliness among older people in Ireland. Ageing and Society, 28(8), 1113–1132. 10.1017/S0144686X08007526 [DOI] [Google Scholar]
- Elklit A, Hyland P, & Shevlin M (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(SUPPL), 24221. 10.3402/ejpt.v5.24221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Forbes D, Fletcher S, Lockwood E, O’Donnell M, Creamer M, Bryant RA, McFarlane A, & Silove D (2011). Requiring both avoidance and emotional numbing in DSM-V PTSD: Will it help? Journal of Affective Disorders, 130(3), 483–486. 10.1016/j.jad.2010.10.032 [DOI] [PubMed] [Google Scholar]
- Fox R, Hyland P, McHugh Power J, & Coogan AN (2020a). Patterns of comorbidity associated with ICD-11 PTSD among older adults in the United States. Psychiatry Research, 290, 113171. 10.1016/j.psychres.2020.113171 [DOI] [PubMed] [Google Scholar]
- Fox R, Hyland P, McHugh Power J, & Coogan AN (2020b). Posttraumatic stress disorder among older adults: A differential item functioning analysis of PTSD in ICD-11 and DSM–5. Psychological Trauma: Theory, Research, Practice, and Policy. 10.1037/tra0000596 [DOI] [PubMed] [Google Scholar]
- Fox R, McHugh Power J, Coogan AN, Beekman ATF, van Tilburg TG, & Hyland P (2021). Posttraumatic stress disorder and loneliness are associated over time: A longitudinal study on PTSD symptoms and loneliness, among older adults. Psychiatry Research, 299, 113846. 10.1016/j.psychres.2021.113846 [DOI] [PubMed] [Google Scholar]
- Fredman SJ, Beck JG, Shnaider P, Le Y, Pukay-Martin ND, Pentel KZ, Monson CM, Simon NM, & Marques L (2017). Longitudinal associations between PTSD symptoms and dyadic conflict communication following a severe motor vehicle accident. Behavior Therapy, 48(2), 235–246. 10.1016/j.beth.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, & Bryant RA (2013). 636,120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science, 8(6), 651–662. https://doi.org/10.1177%2F1745691613504115 [DOI] [PubMed] [Google Scholar]
- Goswick RA, & Jones WH (1981). Loneliness, self-concept, and adjustment. Journal of Psychology, 107(2), 237–240. 10.1080/00223980.1981.9915228 [DOI] [Google Scholar]
- Graham JM (2006). Congeneric and (essentially) tau-equivalent estimates of score reliability: What they are and how to use them. Educational and Psychological Measurement, 66(6), 930–944. 10.1177/0013164406288165 [DOI] [Google Scholar]
- Grossman ES, Hoffman YSG, Shrira A, Kedar M, Ben-Ezra M, Dinnayi M, & Zivotofsky AZ (2019). Preliminary evidence linking complex-PTSD to insomnia in a sample of Yazidi genocide survivors. Psychiatry Research, 271, 161–166. 10.1016/j.psychres.2018.11.044 [DOI] [PubMed] [Google Scholar]
- Gum AM, King-Kallimanis B, & Kohn R (2009). Prevalence of mood, anxiety, and substance-abuse disorders for older Americans in the national comorbidity survey-replication. American Journal of Geriatric Psychiatry, 17(9), 769–781. 10.1097/JGP.0b013e3181ad4f5a [DOI] [PubMed] [Google Scholar]
- Hafstad GS, Thoresen S, Wentzel-Larsen T, Maercker A, & Dyb G (2017). PTSD or not PTSD? Comparing the proposed ICD-11 and the DSM-5 PTSD criteria among young survivors of the 2011 Norway attacks and their parents. Psychological Medicine, 47(7), 1283–1291. 10.1017/S0033291716002968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, & Cacioppo JT (2009). Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychology, 28(3), 354–363. 10.1037/a0014400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeke C, O’Donald A, Stammel N, & Böttche M (2020). Same same but different? DSM-5 versus ICD-11 PTSD among traumatized refugees in Germany. Journal of Psychosomatic Research, 134, 110129. 10.1016/j.jpsychores.2020.110129 [DOI] [PubMed] [Google Scholar]
- Herman JL (1992). Trauma and recovery: The aftermath of violence from domestic violence to political terrorism. Guilford Press. [Google Scholar]
- Hoge CW, Riviere LA, Wilk JE, Herrell RK, & Weathers FW (2014). The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: A head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. The Lancet Psychiatry, 1(4), 269–277. 10.1016/S2215-0366(14)70235-4 [DOI] [PubMed] [Google Scholar]
- Hom MA, Hames JL, Bodell LP, Buchman-Schmitt JM, Chu C, Rogers ML, Chiurliza B, Michaels MS, Ribeiro JD, Nadorff MR, Winer ES, Lim IC, Rudd MD, & Joiner TE (2017). Investigating insomnia as a cross-sectional and longitudinal predictor of loneliness: Findings from six samples. Psychiatry Research, 253, 116–128. 10.1016/j.psychres.2017.03.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hyland P, Karatzias T, Shevlin M, Cloitre M, & Ben-Ezra M (2020). A longitudinal study of ICD-11 PTSD and complex PTSD in the general population of Israel. Psychiatry Research, 286, 112871. 10.1016/j.psychres.2020.112871 [DOI] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, Brewin CR, Cloitre M, Downes AJ, Jumbe S, Karatzias T, Bisson JI, & Roberts NP (2017). Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the International Trauma Questionnaire. Acta Psychiatrica Scandinavica, 136(3), 313–322. 10.1111/acps.12771 [DOI] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, Cloitre M, Karatzias T, Vallières F, McGinty G, Fox R, & McHugh Power J (2019). Quality not quantity: loneliness subtypes, psychological trauma, and mental health in the US adult population. Social Psychiatry and Psychiatric Epidemiology, 54(9). 10.1007/s00127-018-1597-8 [DOI] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, Fyvie C, & Karatzias T (2018). Posttraumatic stress disorder and complex posttraumatic stress disorder in DSM-5 and ICD-11: Clinical and behavioral correlates. Journal of Traumatic Stress, 31(2), 174–180. 10.1002/jts.22272 [DOI] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, McNally S, Murphy J, Hansen M, & Elklit A (2016). Exploring differences between the ICD-11 and DSM-5 models of PTSD: Does it matter which model is used? Journal of Anxiety Disorders, 37, 48–53. 10.1016/j.janxdis.2015.11.002 [DOI] [PubMed] [Google Scholar]
- Hyland P, Vallières F, Cloitre M, Ben-Ezra M, Karatzias T, Olff M, Murphy J, & Shevlin M (2020). Trauma, PTSD, and complex PTSD in the Republic of Ireland: Prevalence, service use, comorbidity, and risk factors. Social Psychiatry and Psychiatric Epidemiology. 10.1007/s00127-020-01912-x [DOI] [PubMed] [Google Scholar]
- Itzhaky L, Stein JY, Levin Y, & Solomon Z (2017). Posttraumatic stress symptoms and marital adjustment among Israeli combat veterans: The role of loneliness and attachment. Psychological Trauma: Theory, Research, Practice, and Policy, 9(6), 655–662. 10.1037/tra0000259 [DOI] [PubMed] [Google Scholar]
- Jarvis MA, Padmanabhanunni A, Balakrishna Y, & Chipps J (2020). The effectiveness of interventions addressing loneliness in older persons: An umbrella review. International Journal of Africa Nursing Sciences, 12, 100177. 10.1016/j.ijans.2019.100177 [DOI] [Google Scholar]
- Karatzias T, Murphy P, Cloitre M, Bisson J, Roberts N, Shevlin M, Hyland P, Maercker A, Ben-Ezra M, Coventry P, Mason-Roberts S, Bradley A, & Hutton P (2019). Psychological interventions for ICD-11 complex PTSD symptoms: systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. 10.1017/S0033291719000436 [DOI] [PubMed] [Google Scholar]
- Karatzias T, Shevlin M, Fyvie C, Hyland P, Efthymiadou E, Wilson D, Roberts N, Bisson JI, Brewin CR, & Cloitre M (2016). An initial psychometric assessment of an ICD-11 based measure of PTSD and complex PTSD (ICD-TQ): Evidence of construct validity. Journal of Anxiety Disorders, 44, 73–79. 10.1016/j.janxdis.2016.10.009 [DOI] [PubMed] [Google Scholar]
- Karatzias T, Shevlin M, Fyvie C, Hyland P, Efthymiadou E, Wilson D, Roberts N, Bisson JI, Brewin CR, & Cloitre M (2017). Evidence of distinct profiles of Posttraumatic Stress Disorder (PTSD) and Complex Posttraumatic Stress Disorder (CPTSD) based on the new ICD-11 Trauma Questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. 10.1016/j.jad.2016.09.032 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Knoke J, Burau J, & Roehrle B (2010). Attachment styles, loneliness, quality, and stability of marital relationships. Journal of Divorce and Remarriage, 51(5), 310–325. 10.1080/10502551003652017 [DOI] [Google Scholar]
- Kuwert P, Knaevelsrud C, & Pietrzak RH (2014). Loneliness among older veterans in the United States: results from the National Health and Resilience in Veterans Study. American Journal of Geriatric Psychiatry, 22(6), 564–569. 10.1016/j.jagp.2013.02.013 [DOI] [PubMed] [Google Scholar]
- Luo Y, Hawkley LC, Waite LJ, & Cacioppo JT (2012). Loneliness, health, and mortality in old age: A national longitudinal study. Social Science and Medicine, 74(6), 907–914. 10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann F, Bone JK, Lloyd-Evans B, Frerichs J, Pinfold V, Ma R, Wang J, & Johnson S (2017). A life less lonely: The state of the art in interventions to reduce loneliness in people with mental health problems. Social Psychiatry and Psychiatric Epidemiology, 52(6), 627–638. 10.1007/s00127-017-1392-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi CM, Chen HY, Hawkley LC, & Cacioppo JT (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. 10.1177/1088868310377394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews T, Danese A, Gregory AM, Caspi A, Moffitt TE, & Arseneault L (2017). Sleeping with one eye open: Loneliness and sleep quality in young adults. Psychological Medicine, 47(12), 2177–2186. 10.1017/S0033291717000629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthieu MM, Lawrence KA, & Robertson-Blackmore E (2017). The impact of a civic service program on biopsychosocial outcomes of post 9/11 U.S. military veterans. Psychiatry Research, 248, 111–116. 10.1016/j.psychres.2016.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh Power JE, Steptoe A, Kee F, & Lawlor BA (2019). Loneliness and social engagement in older adults: A bivariate dual change score Analysis. Psychology and Aging, 34(1), 152–162. 10.1037/pag0000287 [DOI] [PubMed] [Google Scholar]
- McHugh JE, & Lawlor BA (2013). Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. British Journal of Health Psychology, 18(3), 546–555. 10.1111/j.2044-8287.2012.02101.x [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2018). Mplus User’s Guide (8th ed.). Muthén & Muthén. [Google Scholar]
- O’Connor M (2010). A longitudinal study of PTSD in the elderly bereaved: prevalence and predictors. Aging & Mental Health, 14(3), 310–318. 10.1080/13607860903228770 [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Alkemade N, Nickerson A, Creamer M, McFarlane AC, Silove D, Bryant RA, & Forbes D (2014). Impact of the diagnostic changes to post-traumatic stress disorder for DSM-5 and the proposed changes to ICD-11. British Journal of Psychiatry, 205(3), 230–235. 10.1192/bjp.bp.113.135285 [DOI] [PubMed] [Google Scholar]
- Ó’Luanaigh C, & Lawlor BA (2008). Loneliness and the health of older people. International Journal of Geriatric Psychiatry, 23(12), 1213–1221. 10.1002/gps.2054 [DOI] [PubMed] [Google Scholar]
- Ogle CM, Rubin DC, & Siegler IC (2014). Cumulative exposure to traumatic events in older adults. Aging & Mental Health, 18(3), 316–325. 10.1080/13607863.2013.832730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong AD, Uchino BN, & Wethington E (2016). Loneliness and health in older adults: A mini-review and synthesis. Gerontology, 62(4), 443–449. 10.1159/000441651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- OʼSúilleabháin PS, Gallagher S, & Steptoe A (2019). Loneliness, living alone, and all-cause mortality: The role of emotional and social loneliness in the elderly during 19 years of follow-up. Psychosomatic Medicine, 81(6), 521–526. 10.1097/PSY.0000000000000710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peerenboom L, Collard RM, Naarding P, & Comijs HC (2015). The association between depression and emotional and social loneliness in older persons and the influence of social support, cognitive functioning and personality: A cross-sectional study. Journal of Affective Disorders, 182, 26–31. 10.1016/j.jad.2015.04.033 [DOI] [PubMed] [Google Scholar]
- Penning MJ, Liu G, & Chou PHB (2014). Measuring loneliness among middle-aged and older adults: the UCLA and de Jong Gierveld Loneliness Scales. Social Indicators Research, 118(3), 1147–1166. 10.1007/s11205-013-0461-1 [DOI] [Google Scholar]
- Peplau LA, & Perlman D (1982). Loneliness: A sourcebook of current theory, research, and therapy. Wiley. [Google Scholar]
- Pinquart M, & Sörensen S (2001). Influences on loneliness in older adults: A meta-analysis. Basic and Applied Social Psychology, 23(4), 245–266. 10.1207/S15324834BASP2304_2 [DOI] [Google Scholar]
- Pless Kaiser A, Cook JM, Glick DM, & Moye J (2019). Posttraumatic stress disorder in older adults: A conceptual review. Clinical Gerontologist, 42(4), 359–376. 10.1080/07317115.2018.1539801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poscia A, Stojanovic J, La Milia DI, Duplaga M, Grysztar M, Moscato U, Onder G, Collamati A, Ricciardi W, & Magnavita N (2018). Interventions targeting loneliness and social isolation among the older people: An update systematic review. Experimental Gerontology, 102, 133–144. 10.1016/j.exger.2017.11.017 [DOI] [PubMed] [Google Scholar]
- Putnick DL, & Bornstein MH (2016). Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Developmental Review, 41, 71–90. 10.1016/j.dr.2016.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu C, Kivipelto M, & Von Strauss E (2009). Epidemiology of Alzheimer’s disease: Occurrence, determinants, and strategies toward intervention. Dialogues in Clinical Neuroscience, 11(2), 111–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualter P, Vanhalst J, Harris R, Van Roekel E, Lodder G, Bangee M, Maes M, & Verhagen M (2015). Loneliness across the life span. Perspectives on Psychological Science, 10(2), 250–264. 10.1177/1745691615568999 [DOI] [PubMed] [Google Scholar]
- Rafferty LA, Cawkill PE, Stevelink SAM, Greenberg K, & Greenberg N (2018). Dementia, post-traumatic stress disorder and major depressive disorder: A review of the mental health risk factors for dementia in the military veteran population. Psychological Medicine, 48(9), 1400–1409. 10.1017/S0033291717001386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raykov T (1997). Scale reliability, Cronbach’s Coefficient Alpha, and violations of essential tau-equivalence with fixed congeneric components. Multivariate Behavioral Research, 32(4), 329–353. 10.1207/s15327906mbr3204_2 [DOI] [PubMed] [Google Scholar]
- Raykov T, Dimitrov DM, & Asparouhov T (2010). Evaluation of scale reliability with binary measures using latent variable modeling. Structural Equation Modeling: A Multidisciplinary Journal, 17(2), 265–279. 10.1080/10705511003659417 [DOI] [Google Scholar]
- Resick PA, & Schnicke MK (1992). Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology, 60(5), 748–756. 10.1037/0022-006X.60.5.748 [DOI] [PubMed] [Google Scholar]
- Reynolds K, Pietrzak RH, Mackenzie CS, Chou KL, & Sareen J (2016). Post-traumatic stress disorder across the adult lifespan: findings from a nationally representative survey. American Journal of Geriatric Psychiatry, 24(1), 81–93. 10.1016/j.jagp.2015.11.001 [DOI] [PubMed] [Google Scholar]
- Rosellini AJ, Stein MB, Colpe LJ, Heeringa SG, Petukhova MV, Sampson NA, Schoenbaum M, Ursano RJ, Kessler RC, & Army STARRS Collaborators. (2015). Approximating a DSM-5 diagnosis of PTSD using DSM-IV criteria. Depression and Anxiety, 32(7), 493–501. 10.1002/da.22364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittger RIB, Wherton J, Prendergast D, & Lawlor BA (2012). Risk factors and mediating pathways of loneliness and social support in community-dwelling older adults. Aging & Mental Health, 16(3), 335–346. 10.1080/13607863.2011.629092 [DOI] [PubMed] [Google Scholar]
- Schnyder U, Müller J, Morina N, Schick M, Bryant RA, & Nickerson A (2015). A comparison of DSM-5 and DSM-IV diagnostic criteria for posttraumatic stress disorder in traumatized refugees. Journal of Traumatic Stress, 28(4), 267–274. 10.1002/jts.22023 [DOI] [PubMed] [Google Scholar]
- Shevlin M, Hyland P, Roberts NP, Bisson JI, Brewin CR, & Cloitre M (2018). A psychometric assessment of Disturbances in Self-Organization symptom indicators for ICD-11 Complex PTSD using the International Trauma Questionnaire. European Journal of Psychotraumatology, 9(1), 1419749. 10.1080/20008198.2017.1419749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin M, Hyland P, Vallières F, Bisson J, Makhashvili N, Javakhishvili J, Shpiker M, & Roberts B (2018). A comparison of DSM-5 and ICD-11 PTSD prevalence, comorbidity and disability: An analysis of the Ukrainian Internally Displaced Person’s Mental Health Survey. Acta Psychiatrica Scandinavica, 137(2), 138–147. 10.1111/acps.12840 [DOI] [PubMed] [Google Scholar]
- Shevlin M, McElroy E, & Murphy J (2015). Loneliness mediates the relationship between childhood trauma and adult psychopathology: evidence from the adult psychiatric morbidity survey. Social Psychiatry and Psychiatric Epidemiology, 50(4), 591–601. 10.1007/s00127-014-0951-8 [DOI] [PubMed] [Google Scholar]
- Sinha SS (2016). Trauma-induced insomnia: A novel model for trauma and sleep research. Sleep Medicine Reviews, 25, 74–83. 10.1016/j.smrv.2015.01.008 [DOI] [PubMed] [Google Scholar]
- Sliter KA, & Zickar MJ (2013). An IRT examination of the psychometric functioning of negatively worded personality items. Educational and Psychological Measurement, 74(2), 214–226. 10.1177/0013164413504584 [DOI] [Google Scholar]
- Solomon Z, & Dekel R (2008). The contribution of loneliness and posttraumatic stress disorder to marital adjustment following war captivity: A longitudinal study. Family Process, 47(2), 261–275. 10.1111/j.1545-5300.2008.00252.x [DOI] [PubMed] [Google Scholar]
- Solomon Z, Bensimon M, Greene T, Horesh D, & Ein-Dor T (2015). Loneliness trajectories: The role of posttraumatic symptoms and social support. Journal of Loss and Trauma, 20(1), 1–21. 10.1080/15325024.2013.815055 [DOI] [Google Scholar]
- Solomon Z, Horesh D, Ein-Dor T, & Ohry A (2012). Predictors of PTSD trajectories following captivity: A 35-year longitudinal study. Psychiatry Research, 199(3), 188–194. 10.1016/j.psychres.2012.03.035 [DOI] [PubMed] [Google Scholar]
- Solomon Z, Mikulincer M, & Waysman M (1991). Delayed and immediate onset posttraumatic stress disorder: The role of life events and social resources. Journal of Community Psychology, 19(3), 231–236. [DOI] [Google Scholar]
- Steiger JH (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research, 25(2), 173–180. 10.1207/s15327906mbr2502_4 [DOI] [PubMed] [Google Scholar]
- Tanaka JS (1987). “How big is big enough?”: Sample size and goodness of fit in structural equation models with latent variables. Child Development, 58(1), 146. 10.2307/1130296 [DOI] [Google Scholar]
- Thompson NJ, Fiorillo D, Rothbaum BO, Ressler KJ, & Michopoulos V (2018). Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. Journal of Affective Disorders, 225, 153–159. 10.1016/j.jad.2017.08.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, & Foa EB (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959–992. 10.1037/0033-2909.132.6.959 [DOI] [PubMed] [Google Scholar]
- Tsur N, Stein JY, Levin Y, Siegel A, & Solomon Z (2019). Loneliness and subjective physical health among war veterans: Long term reciprocal effects. Social Science and Medicine, 234, 112373. 10.1016/j.socscimed.2019.112373 [DOI] [PubMed] [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. 10.1007/BF02291170 [DOI] [Google Scholar]
- Tyrer P (2014). A comparison of DSM and ICD classifications of mental disorder. Advances in Psychiatric Treatment, 20(4), 280–285. 10.1192/apt.bp.113.011296 [DOI] [Google Scholar]
- Vallières F, Ceannt R, Daccache F, Abou Daher R, Sleiman J, Gilmore B, Byrne S, Shevlin M, Murphy J, & Hyland P (2018). ICD-11 PTSD and complex PTSD amongst Syrian refugees in Lebanon: the factor structure and the clinical utility of the International Trauma Questionnaire. Acta Psychiatrica Scandinavica, 138(6), 547–557. 10.1111/acps.12973 [DOI] [PubMed] [Google Scholar]
- van der Velden PG, Oudejans M, Das M, Bosmans MWG, & Maercker A (2019). The longitudinal effect of social recognition on PTSD symptomatology and vice versa: Evidence from a population-based study. Psychiatry Research, 279, 287–294. 10.1016/j.psychres.2019.05.044 [DOI] [PubMed] [Google Scholar]
- van der Velden PG, Pijnappel B, & van der Meulen E (2018). Potentially traumatic events have negative and positive effects on loneliness, depending on PTSD-symptom levels: evidence from a population-based prospective comparative study. Social Psychiatry and Psychiatric Epidemiology, 53(2), 195–206. 10.1007/s00127-017-1476-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ (2019). Principles of confounder selection. European Journal of Epidemiology, 34(3), 211–219. 10.1007/s10654-019-00494-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventimiglia I, & Seedat S (2019). Current evidence on urbanicity and the impact of neighbourhoods on anxiety and stress-related disorders. Current Opinion in Psychiatry, 32(3), 248–253. 10.1097/YCO.0000000000000496 [DOI] [PubMed] [Google Scholar]
- Victor CR, & Yang K (2012). The prevalence of loneliness among adults: A case study of the United Kingdom. Journal of Psychology, 146(1–2), 85–104. 10.1080/00223980.2011.613875 [DOI] [PubMed] [Google Scholar]
- Wang J, Mann F, Lloyd-Evans B, Ma R, & Johnson S (2018). Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry, 18, 156. 10.1186/s12888-018-1736-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW (2017). Redefining posttraumatic stress disorder for DSM-5. Current Opinion in Psychology, 14, 122–126. 10.1016/j.copsyc.2017.01.002 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at http://www.ptsd.va.gov [Google Scholar]
- Weiss RS (1973). Loneliness: The experience of emotional and social isolation. In Loneliness: The experience of emotional and social isolation. MIT Press. [Google Scholar]
- Wong NML, Liu HL, Lin C, Huang CM, Wai YY, Lee SH, & Lee TMC (2016). Loneliness in late-life depression: Structural and functional connectivity during affective processing. Psychological Medicine, 46(12), 2485–2499. 10.1017/S0033291716001033 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017, December 12). Mental health of older adults. https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults
- World Health Organization. (2018). International statistical classification of diseases and related health problems (11th Revision). https://icd.who.int/browse11/l-m/en
- Yaffe K, Vittinghoff E, Lindquist K, Barnes D, Covinsky KE, Neylan T, Kluse M, & Marmar C (2010). Posttraumatic stress disorder and risk of dementia among US veterans. Archives of General Psychiatry, 67(6), 608–613. 10.1001/archgenpsychiatry.2010.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerach G, Shevlin M, Cloitre M, & Solomon Z (2019). Complex posttraumatic stress disorder (CPTSD) following captivity: A 24-year longitudinal study. European Journal of Psychotraumatology, 10(1), 1616488. 10.1080/20008198.2019.1616488 [DOI] [PMC free article] [PubMed] [Google Scholar]


