Abstract
Introduction
This study investigated the long-term visual and optical quality changes after small incision lenticule extraction (SMILE) for the correction of moderate to high myopia.
Methods
Forty-one eyes of 41 patients with a mean spherical equivalent (SE) of − 6.74 ± 1.45 D undergoing SMILE were enrolled. Preoperative and 1-month, 3-month, 1-year and 5-year postoperative follow-up examinations were performed including visual acuity, manifest refraction, corneal aberrations and contrast sensitivity. An optical quality analysis system was used to measure objective scatter index (OSI), Strehl ratio (SR) and modulation transfer function cutoff frequency (MTFcutoff).
Results
The safety and efficacy indices were 1.09 ± 0.12 and 1.03 ± 0.17, respectively, at the 5-year follow-up. No significant changes in SE from 1 month to 5 years postoperatively were found. The OSI significantly increased at 1 and 3 months postoperatively (p < 0.01 and p < 0.01) and declined at 1 and 5 years (p = 0.81 and p = 0.87). MTFcutoff and SR showed similar trends. Coma, spherical aberration and total higher-order aberration significantly increased after SMILE (p < 0.01) and remained stable from 1 month to 5 years after surgery (p > 0.05). Contrast sensitivity in the photopic and mesopic condition showed no significant changes during 5-year follow-up (p > 0.05).
Conclusion
The SMILE procedure is satisfactory in terms of optical quality for correcting moderate and high myopia in the long-term period.
Trial Registration
ChiCTR-ONRC-13003114.
Keywords: SMILE, Corneal aberrations, Objective scattering, Optical quality, Contrast sensitivity
Key Summary Points
| Why carry out this study? |
| SMILE (small incision lenticule extraction) for the correction of myopia and myopic astigmatism has provided good visual and refractive results in many patients in the last decade. |
| It was previously reported that intraocular scattering shows a tendency to increase temporarily, then gradually declines to preoperative levels in 3 months and remains stable at 18 months after surgery. |
| However, longer-term optical quality outcomes have not been well investigated. |
| What was learned from the study? |
| This study was the first to provide new information about the long-term (5 years) optical quality changes after SMILE. |
| SMILE showed stable visual and refractive outcomes with unaffected contrast sensitivity for moderate and high myopia in this 5-year follow-up study. |
| Intraocular scattering and retinal image quality temporarily changed and then recovered to preoperative levels within the 5 years of follow-up. |
Introduction
Small incision lenticule extraction (SMILE) was first reported by Sekundo et al. [1] and Shah et al. [2] for the correction of myopia and myopic astigmatism in 2011. As a flapless minimally invasive procedure that allows the relative preservation of the anterior stromal lamellae, SMILE could in theory maintain the strength of the cornea postoperatively [3, 4]. This procedure has provided good results to many satisfied patients in the past decade [5–9].
Blum et al. [10] were the first to report that SMILE is a safe, effective and stable procedure for the treatment of myopia and myopic astigmatism in a 10-year follow-up. Similarly, our previous studies [11, 12] investigated the 7-year outcomes after SMILE, including corneal wavefront aberrations and posterior elevation. Our team has long been focusing on optical quality and intraocular scattering after SMILE. In our previous studies, it was found that intraocular scattering first showed a tendency to increase temporarily and then gradually declined to preoperative levels in 3 months and remained stable at 18-month follow-up, while retinal image quality was barely influenced and remained stable at 18 months after surgery [13–15].
The purpose of this study was to evaluate visual and refractive outcomes within 5 years after SMILE for treating moderate to high myopia and to analyze the long-term changes in corneal aberrations, contrast sensitivity, intraocular scattering and retinal image quality of the procedure. To our knowledge, this prospective study is the first to provide detailed information about long-term visual and optical quality changes, including intraocular scattering and contrast sensitivity after SMILE.
Methods
Subjects
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of our Hospital. Written informed consent was obtained from each subject after giving them an explanation of the nature and possible consequences of the study, and all the procedures followed the HIPAA (Health Insurance Portability and Accountability Act) regulations for patients.
All subjects in the present study were recruited from a pool of patients who underwent SMILE for myopia correction at our hospital. Criteria for inclusion were as follows: ages from 18 to 40 years, spherical error of − 3.00 to − 9.00 D and cylindrical error of 0 to − 3.00 D. Exclusion criteria were as follows: suspicious of keratoconus, a history of other ocular diseases besides myopia and astigmatism, or previous ocular surgeries. Contact lens wearers were asked to discontinue lens wear for at least 2 weeks.
In total, 41 eyes of 41 patients (13 men and 28 women) with a mean age of 26.49 ± 4.68 years were included in this prospective longitudinal study. The baseline characteristics of the study population are summarized in Table 1.
Table 1.
Baseline characteristics of the patients
| Mean ± SD | Range | |
|---|---|---|
| Age (years) | 26.49 ± 4.68 | 19–40 |
| Sphere (D) | − 6.74 ± 1.45 | − 4.25 to − 9.00 |
| Cylinder (D) | − 0.84 ± 0.70 | 0 to – 2.25 |
| Spherical equivalent (D) | − 7.16 ± 1.51 | − 4.25 to – 10.00 |
| IOP (mmHg) | 15.35 | 11.5–20.1 |
D diopters, SE spherical equivalent, IOP intraocular pressure
Measurements
The preoperative and 1-month, 3-month, 1-year and 5-year postoperative ophthalmic examinations included slit-lamp biomicroscopy, uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction and optical quality assessment.
Wavefront aberrations were calculated by Zernike analysis using Pentacam HR (Oculus Optikgerate GmbH, Wetzlar, Germany). Coma, trefoil, spherical aberration (SA) and the root mean square (RMS) of total lower order aberration and higher order aberration (HOA) were observed for the 6-mm pupil diameter. A double-pass optical quality analysis system (OQAS, Visiometrics, Terrassa, Spain) was used to measure optical quality parameters, such as objective scatter index (OSI), modulated transfer function cutoff frequency (MTFcutoff) and Strehl ratio (SR) in two dimensions. The testing was conducted in a mesopic condition with a 4-mm artificial pupil. Contrast sensitivity (CS) was assessed with the CSV-1000 test chart (Vector Vision, Greenville, OH) in the mesopic (85 cd/m2) and photopic (3 cd/m2) conditions in four different spatial frequencies: 3, 6, 12 and 18 cycles per degree (cpd).
Surgical Procedure
All SMILE procedures were conducted in accordance with previous studies [12, 13] and performed by the same experienced surgeon (XZ) using the VisuMax femtosecond laser system (Carl Zeiss Meditec, Jena, Germany). Laser scanning was set to a pulse energy of 130 nJ and a repetition rate of 500 kHz. The intended thickness of the cap was 110 μm, and the diameter of the cap was 7.5 mm. The refractive lenticule was 6.5–6.9 mm based on refractive errors. The intrastromal lenticule was extracted through a 2-mm incision at the 12 o’clock position.
Prescriptions were given for levofloxacin eye drops, four times a day for 3 days; artificial tears, four times a day for 1 month; 0.1% fluorometholone eye drops, seven times daily initially, followed by a gradual reduction over 3 weeks.
Statistical Analysis
All statistical tests were performed using the Statistical Package for the Social Sciences (SPSS) version 25.0 (SPSS, Chicago, IL, USA). Continuous variables were expressed as mean ± standard deviation (SD). Normal distribution was evaluated by the Shapiro-Wilk test. Comparisons of the pre- and postoperative data were performed using the repeated measurement analysis of variance for normally distributed data and Friedman rank sum test for non-normally distributed data. A Bonferroni-based adjustment was made for multiple comparisons to control the family type I error at a level of 0.05. Significance was set at p < 0.05.
Results
Safety and Efficacy
All surgical procedures were completed successfully, without any intra- or postoperative adverse effects such as interface debris, diffuse lamellar keratitis, subconjunctival hemorrhage, epithelial ingrowth or corneal ectasia during the follow-up period. The safety index (ratio between postoperative CDVA and preoperative CDVA) was 1.09 ± 0.12 at 5 years after SMILE. A total of 41.46% eyes gained one line in CDVA after 5 years, 2.44% eyes gained two lines or more and no eye lost two or more lines.
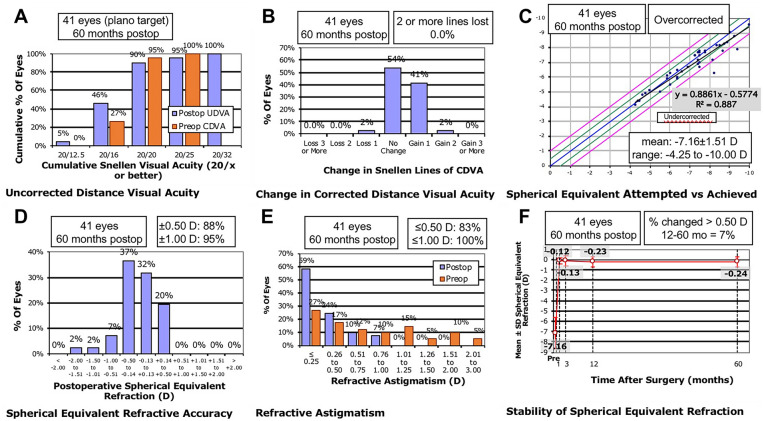
The efficacy index (ratio between postoperative UDVA and preoperative CDVA) was 1.03 ± 0.17 at 5 years postoperatively. As shown in Fig. 1, 90.24% of the eyes achieved a UDVA of 20/20 or better, 95.12% eyes achieved an UDVA of 16/20 or better, 95.12% eyes achieved a CDVA of 20/20 or better, and all eyes achieved a CDVA of 16/20 or better.
Fig. 1.
Visual and refractive outcomes at 5 years postoperatively for 41 eyes treated with small incision lenticule extraction (UDVA uncorrected distance visual acuity, CDVA corrected distance visual acuity, Preop preoperatively, Postop postoperatively, D diopters)
Predictability and Stability
Spherical equivalent (SE) was − 0.12 ± 32, − 0.13 ± 0.48, − 0.23 ± 0.50 and − 0.28 ± 0.55 D at 1, 3, 12 and 60 months after SMILE, respectively. There was no significant difference in SE between postoperative time points spanning the 5-year follow-up (p > 0.05). The average refractive regression rate was − 0.03 D per year. After 5 years, 87.80% of eyes were within ± 0.50 D and 95.12% of eyes were within ± 1.00 D of target refraction (Fig. 1).
Corneal Aberration
As shown in Table 2, an increase of HOA RMS was observed from a preoperative value of 0.38 ± 0.25 μm to 0.97 ± 0.29 μm at 3 months postoperatively and finally to 0.95 ± 0.31 μm at the last follow-up. Coma, SA and the RMS of low- and high-order aberrations showed significant increases at each point in time after SMILE compared with those measured before the surgery (p < 0.01), whereas no significant difference was found between 1 month and 5 years postoperatively (p > 0.05). Besides, no significant difference was found in pre- and postoperative trefoil at any point in time after surgery during the 5-year follow-up (p > 0.05).
Table 2.
Corneal aberrations at each time point before and after SMILE (mean ± SD)
| Preoperative | 3 months | 1 year | 5 years | p value | |
|---|---|---|---|---|---|
| Coma (Z1 3) | 0.11 ± 0.08 | 0.34 ± 0.24* | 0.33 ± 0.23* | 0.33 ± 0.24* | < 0.01# |
| Coma (Z-1 3) | 0.14 ± 0.10 | 0.59 ± 0.38* | 0.61 ± 0.34* | 0.60 ± 0.37* | < 0.01# |
| Coma | 0.20 ± 0.09 | 0.74 ± 0.35* | 0.73 ± 0.34* | 0.72 ± 0.38* | < 0.01# |
| Trefoil (Z3 3) | 0.08 ± 0.08 | 0.13 ± 0.10 | 0.11 ± 0.09 | 0.12 ± 0.10 | 0.18 |
| Trefoil (Z-3 3) | 0.08 ± 0.07 | 0.12 ± 0.10 | 0.12 ± 0.09 | 0.13 ± 0.10 | 0.76 |
| Trefoil | 0.12 ± 0.10 | 0.18 ± 0.14 | 0.17 ± 0.12 | 0.18 ± 0.14 | 0.63 |
| SA (Z0 4) | 0.22 ± 0.07 | 0.40 ± 0.17* | 0.41 ± 0.16* | 0.41 ± 0.17* | < 0.01# |
| LOA RMS | 1.55 ± 0.51 | 2.43 ± 0.72* | 2.38 ± 0.67* | 2.27 ± 0.81* | < 0.01# |
| HOA RMS | 0.38 ± 0.25 | 0.97 ± 0.29* | 0.98 ± 0.26* | 0.95 ± 0.31* | < 0.01# |
SA spherical aberration, LOA RMS root mean square of total lower order aberration, HOA RMS root mean square of total higher order aberration
*Versus preoperative values of statistical significance (p < 0.05)
#Intra-group difference of statistical significance (p < 0.05)
Optical Quality Analysis System
Table 3 shows time courses of the OSI, the MTFcutoff and the Strehl2D ratio after SMILE during the 5-year follow-up. Postoperative OSI showed a temporary increasing trend within 1 and 3 months (p < 0.01, p < 0.01) and then returned to the preoperative level at 1 to 5 years (p > 0.05) after SMILE. In addition, MTFcutoff significantly decreased at 1 and 3 months postoperatively (p < 0.01, p = 0.03) and increased with time at 1 to 5 years (p > 0.05). The SR showed similar trends as MTFcutoff during the 5-year follow-up.
Table 3.
Intraocular scattering and retinal image quality before and after SMILE (mean ± SD)
| Preoperative | 1 month | 3 months | 1 year | 5 years | p value | |
|---|---|---|---|---|---|---|
| OSI | 0.64 ± 0.40 |
1.33 ± 0.90* (p < 0.01) |
1.04 ± 0.51* (p < 0.01) |
0.84 ± 0.47 (p = 0.81) |
0.84 ± 0.44 (p = 0.87) |
< 0.01# |
| MTFcutoff (cpd) | 38.60 ± 8.13 |
31.29 ± 9.17* (p < 0.01) |
33.72 ± 9.34* (p = 0.03) |
37.43 ± 8.06 (p = 0.99) |
37.15 ± 8.17 (p = 0.99) |
< 0.01# |
| Strehl2D ratio | 0.22 ± 0.05 |
0.18 ± 0.05* (p < 0.01) |
0.18 ± 0.05* (p < 0.01) |
0.19 ± 0.04* (p = 0.01) |
0.20 ± 0.04 (p = 0.21) |
< 0.01# |
OSI objective scatter index, MTFcutoff modulation transfer function cutoff frequency, cpd cycles per degree, Strehl2D ratio Strehl ratio in two dimensions
*Versus preoperative values of statistical significance (p < 0.05)
#Intra-group difference of statistical significance (p < 0.05)
Contrast Sensitivity
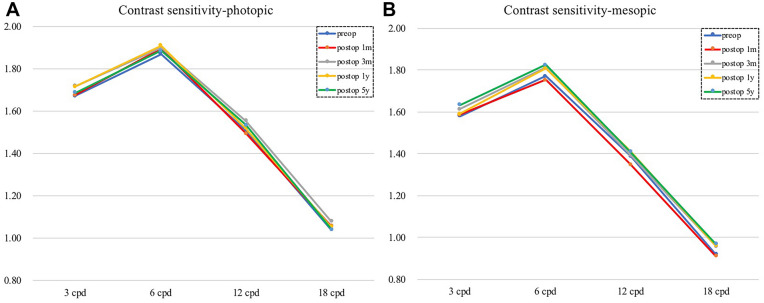
Figure 2 shows the log CS value changes in four spatial frequencies over time. The log CS values in the photopic and mesopic condition were not significantly different from the preoperative values throughout the whole follow-up period (p > 0.05).
Fig. 2.
Photopic (A) and mesopic (B) contrast sensitivities at four spatial frequencies at each time point before and after small incision lenticule extraction during 5-year follow-up (cpd cycles per degree). Horizontal axis corresponds to different spatial frequencies. Vertical axis corresponds to log10 contrast sensitivity
Discussion
SMILE procedures have been performed globally, and multiple studies have proved their safety, efficacy, predictability and stability. It is apparent that a long-term optical quality assessment following SMILE, which correlates to patient satisfaction, would be of great value. No previous study to our knowledge has comprehensively evaluated the long-term changes of optical quality after SMILE. In the current study, we investigated the visual outcomes and optical quality (including corneal aberrations, intraocular scattering and contrast sensitivity) at 5 years after SMILE.
At the 5-year follow-up, the safety and efficacy indices were 1.09 ± 0.12 and 1.03 ± 0.17, respectively, indicating that SMILE had good safety and efficacy for the correction of moderate and high myopia. The visual outcomes of this study are superior to those previously reported by Blum et al. [7] and Agca et al. [16] in 5-year follow-up studies, which might contribute to the differences of baseline age and SE of the study population.
In addition, 87.80% and 95.12% of the eyes were within ± 0.50 D and ± 1.00 D of target refraction after 5 years, and the average refractive regression rate was – 0.03 D per year. Similar results were obtained by Xia et al. [11] and Chen et al. [12] in recent studies of 7-year refractive outcomes of SMILE for moderate to high myopia. Li et al. [9] compared the 5-year outcomes between SMILE and femtosecond laser-assisted laser in situ keratomileusis (FS-LASIK) and found that the mean regression of the above two groups from 6 months to 5 years postoperatively was − 0.02 D and − 0.12 D, suggesting that SMILE maintained the stability of refraction better than FS-LASIK.
In this study, the coma, SA and total HOAs of corneal aberration increased after SMILE, but no statistically significant difference was found between 1 month and 5 years after surgery. Similar results were reported by Tulu et al. [17] on 5-year outcomes of SMILE. However, the literature is inconsistent regarding the corneal aberrations after SMILE. Li et al. [9] reported that the coma and HOA were higher at the 6-month follow-up than at the 3-month follow-up, and then remained stable from 6 months to 5 years postoperatively, while the SA remained stable from 3 months to 5 years after SMILE. In Pedersen et al.’s [18] study, the coma remained stable, but SA and HOA significantly decreased from 3 months to 3 years postoperatively. The possible reasons underlying these differences may be attributable to different preoperative SE of the target myopia population. Further investigations of aberrations with larger sample sizes and longer follow-up periods are needed to test these findings.
Aberration and scattering are two independent factors that affect retinal image quality. Intraocular scattering was quantitatively assessed using OSI by OQAS. In this study, postoperative OSI values increased significantly at 1 and 3 months and then attenuated to preoperative levels at 1 to 5 years after SMILE. Kamiya et al. [19] compared two femtosecond laser settings of SMILE and demonstrated that the OSI values were significantly increased with both settings within 3 months preoperatively. Our previous studies showed that the OSI value had a temporary increase at 20 and 40 days postoperatively [13] and then returned to normal from 3 to 18 months after SMILE [14]. The current 5-year outcomes further proved that intraocular scattering remained stable over long periods.
As described in previous studies, a two-dimensional MTF profile was calculated from the retinal image through Fourier transformation by OQAS [20–22], MTFcutoff and SR are both related to the MTF curve. Larger MTFcutoff and SR values indicate higher optical quality. Our study demonstrated that MTFcutoff values showed decrements at 1 and 3 months and then recovered to preoperative levels at 1 and 5 years. The decline in optical quality was possibly due to mild interface haze formation after SMILE, but these changes gradually recovered in the early postoperative period [23].
The contrast sensitivity is also a crucial parameter affecting patients’ satisfaction after the surgery. In our study, the CS values in the photopic and mesopic condition remained stable during 5-year follow-up. Numerous studies have demonstrated that CS function temporarily declines and generally recovers to preoperative levels within 3–12 months after LASIK [24–26]. A study by Sekundo et al. [27] of 1-year results after SMILE revealed that neither mesopic nor photopic CS showed any significant changes. However, Tan et al. [28] reported improvements in both photopic and mesopic CS in the pseudo SMILE group, which could persist through 1 year, while decreases were observed in photopic CS at 3 months postoperatively in the femtosecond lenticule extraction group. Currently, the literature concerning the long-term (> 3 years) evaluation of postoperative CS after SMILE is scarce. The CS reflects the subjective quality of vision from the patient’s perspective; therefore, it is worthwhile to observe the changes in CS over longer periods after SMILE.
The limitations of this study include the relatively small sample size and that patients with moderate and high myopia were not categorized into different groups. Furthermore, collecting information on the patients’ visual symptoms might have provided additional information on subjective optical quality; therefore, application of a standardized questionnaire should be considered in further studies.
Conclusions
In summary, SMILE showed stable visual and refractive outcomes for moderate and high myopia with unaffected contrast sensitivity at the long-term follow-up. The intraocular scattering and retinal image quality temporarily changed and then returned to preoperative levels and could persist through 5 years.
Acknowledgements
We thank the participants of the study.
Funding
This study, including the Journal’s Rapid Service Fee, was supported by the National Natural Science Foundation of China (grant no. 81770955), Joint Research Project of New Frontier Technology in Municipal Hospitals (grant no. SHDC12018103), Project of Shanghai Science and Technology (grant no. 20410710100), Clinical Research Plan of SHDC (grant no. SHDC2020CR1043B) and Project of Shanghai Xuhui District Science and Technology (grant no. 2020-015).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization: Xingtao Zhou; Methodology: Mi Tian and Weijun Jian; Formal analysis and investigation: Mi Tian Huamao Miao and Weijun Jian; Writing—original draft preparation: Mi Tian and Weijun Jian; Writing—review and editing: Huamao Miao and Fei Xia; Funding acquisition: Xingtao Zhou; Resources: Xingtao Zhou; Supervision: Xingtao Zhou.
Disclosures
The authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Compliance with Ethics Guidelines
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Eye and ENT Hospital of Fudan University. Written consent was obtained from all the subjects after they were informed of the nature and possible consequences of the procedure.
Footnotes
Mi Tian and Weijun Jian contributed equally to this work and should be considered equal first authors.
References
- 1.Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011;95(3):335–339. doi: 10.1136/bjo.2009.174284. [DOI] [PubMed] [Google Scholar]
- 2.Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: all-in-one femtosecond laser refractive surgery. J Cataract Refract Surg. 2011;37(1):127–137. doi: 10.1016/j.jcrs.2010.07.033. [DOI] [PubMed] [Google Scholar]
- 3.Wu D, Wang Y, Zhang L, Wei S, Tang X. Corneal biomechanical effects: small-incision lenticule extraction versus femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg. 2014;40(6):954–962. doi: 10.1016/j.jcrs.2013.07.056. [DOI] [PubMed] [Google Scholar]
- 4.Spiru B, Kling S, Hafezi F, Sekundo W. Biomechanical properties of human cornea tested by two-dimensional extensiometry ex vivo in fellow eyes: femtosecond laser-assisted LASIK versus SMILE. J Refract Surg. 2018;34(6):419–423. doi: 10.3928/1081597X-20180402-05. [DOI] [PubMed] [Google Scholar]
- 5.Kamiya K, Shimizu K, Igarashi A, Kobashi H. Visual and refractive outcomes of femtosecond lenticule extraction and small-incision lenticule extraction for myopia. Am J Ophthalmol. 2014;157(1):128–134e122. doi: 10.1016/j.ajo.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology. 2014;121(4):822–828. doi: 10.1016/j.ophtha.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Blum M, Taubig K, Gruhn C, Sekundo W, Kunert KS. Five-year results of Small Incision Lenticule Extraction (ReLEx SMILE) Br J Ophthalmol. 2016;100(9):1192–1195. doi: 10.1136/bjophthalmol-2015-306822. [DOI] [PubMed] [Google Scholar]
- 8.Agca A, Cakir I, Tulu Aygun B, et al. Visual and refractive outcomes of small-incision lenticule extraction in high myopia: 5-year results. J Ophthalmol. 2018;2018:5893126. doi: 10.1155/2018/5893126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li M, Li M, Chen Y, et al. Five-year results of small incision lenticule extraction (SMILE) and femtosecond laser LASIK (FS-LASIK) for myopia. Acta Ophthalmol. 2019;97(3):e373–e380. doi: 10.1111/aos.14017. [DOI] [PubMed] [Google Scholar]
- 10.Blum M, Lauer AS, Kunert KS, Sekundo W. 10-year results of small incision lenticule extraction. J Refract Surg. 2019;35(10):618–623. doi: 10.3928/1081597X-20190826-02. [DOI] [PubMed] [Google Scholar]
- 11.Xia F, Shen Y, Han T, Zhao J, Xu H, Zhou X. Small incision lenticule extraction (SMILE) for moderate and high myopia: seven-year outcomes of refraction, corneal tomography, and wavefront aberrations. J Ophthalmol. 2020;2020:3825864. doi: 10.1155/2020/3825864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen Z, Zhao Y, Zhou X, Xia F, Zhao J, Zhou X. Seven-year observation of posterior corneal elevation after small-incision lenticule extraction in patients with moderate and high myopia. J Cataract Refract Surg. 2021;47:1398–1402. doi: 10.1097/j.jcrs.0000000000000631. [DOI] [PubMed] [Google Scholar]
- 13.Miao H, He L, Shen Y, Li M, Yu Y, Zhou X. Optical quality and intraocular scattering after femtosecond laser small incision lenticule extraction. J Refract Surg. 2014;30(5):296–302. doi: 10.3928/1081597X-20140415-02. [DOI] [PubMed] [Google Scholar]
- 14.Miao H, Tian M, Xu Y, Chen Y, Zhou X. Visual outcomes and optical quality after femtosecond laser small incision lenticule extraction: an 18-month prospective study. J Refract Surg. 2015;31(11):726–731. doi: 10.3928/1081597X-20151021-01. [DOI] [PubMed] [Google Scholar]
- 15.Miao H, Liu X, Tian M, Zhao J, Fang X, Zhou X. Short-term observation of intraocular scattering and Bowman's layer microdistortions after SMILE-CCL. J Refract Surg. 2018;34(6):387–392. doi: 10.3928/1081597X-20180426-02. [DOI] [PubMed] [Google Scholar]
- 16.Agca A, Tulu B, Yasa D, Yildirim Y, Yildiz BK, Demirok A. Long-term (5 years) follow-up of small-incision lenticule extraction in mild-to-moderate myopia. J Cataract Refract Surg. 2019;45(4):421–426. doi: 10.1016/j.jcrs.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Tulu Aygun B, Cankaya KI, Agca A, et al. Five-year outcomes of small-incision lenticule extraction vs femtosecond laser-assisted laser in situ keratomileusis: a contralateral eye study. J Cataract Refract Surg. 2020;46(3):403–409. doi: 10.1097/j.jcrs.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 18.Pedersen IB, Ivarsen A, Hjortdal J. Three-year results of small incision lenticule extraction for high myopia: refractive outcomes and aberrations. J Refract Surg. 2015;31(11):719–724. doi: 10.3928/1081597X-20150923-11. [DOI] [PubMed] [Google Scholar]
- 19.Kamiya K, Shimizu K, Igarashi A, Kobashi H. Effect of femtosecond laser setting on visual performance after small-incision lenticule extraction for myopia. Br J Ophthalmol. 2015;99(10):1381–1387. doi: 10.1136/bjophthalmol-2015-306717. [DOI] [PubMed] [Google Scholar]
- 20.Saad A, Saab M, Gatinel D. Repeatability of measurements with a double-pass system. J Cataract Refract Surg. 2010;36(1):28–33. doi: 10.1016/j.jcrs.2009.07.033. [DOI] [PubMed] [Google Scholar]
- 21.Tomas J, Pinero DP, Alio JL. Intra-observer repeatability of optical quality measures provided by a double-pass system. Clin Exp Optom. 2012;95(1):60–65. doi: 10.1111/j.1444-0938.2011.00660.x. [DOI] [PubMed] [Google Scholar]
- 22.Tian M, Miao H, Shen Y, Gao J, Mo X, Zhou X. Intra- and intersession repeatability of an optical quality and intraocular scattering measurement system in children. PLoS ONE. 2015;10(11):e0142189. doi: 10.1371/journal.pone.0142189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kamiya K, Shimizu K, Igarashi A, Kobashi H. Time course of optical quality and intraocular scattering after refractive lenticule extraction. PLoS ONE. 2013;8(10):e76738. doi: 10.1371/journal.pone.0076738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mutyala S, McDonald MB, Scheinblum KA, Ostrick MD, Brint SF, Thompson H. Contrast sensitivity evaluation after laser in situ keratomileusis. Ophthalmology. 2000;107(10):1864–1867. doi: 10.1016/S0161-6420(00)00355-9. [DOI] [PubMed] [Google Scholar]
- 25.Chan JW, Edwards MH, Woo GC, Woo VC. Contrast sensitivity after laser in situ keratomileusis. One-year follow-up. J Cataract Refract Surg. 2002;28(10):1774–1779. doi: 10.1016/S0886-3350(02)01499-2. [DOI] [PubMed] [Google Scholar]
- 26.Yamane N, Miyata K, Samejima T, et al. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2004;45(11):3986–3990. doi: 10.1167/iovs.04-0629. [DOI] [PubMed] [Google Scholar]
- 27.Sekundo W, Gertnere J, Bertelmann T, Solomatin I. One-year refractive results, contrast sensitivity, high-order aberrations and complications after myopic small-incision lenticule extraction (ReLEx SMILE) Graefes Arch Clin Exp Ophthalmol. 2014;252(5):837–843. doi: 10.1007/s00417-014-2608-4. [DOI] [PubMed] [Google Scholar]
- 28.Tan DK, Tay WT, Chan C, Tan DT, Mehta JS. Postoperative ocular higher-order aberrations and contrast sensitivity: femtosecond lenticule extraction versus pseudo small-incision lenticule extraction. J Cataract Refract Surg. 2015;41(3):623–634. doi: 10.1016/j.jcrs.2014.07.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.