Abstract
We systematically reviewed published research on dry eye disease and its association with higher order aberrations (HOAs). The purpose of this review was to first determine if an association between tear film metrics and HOAs exists and second to determine if the treatment of dry eyes can improve tear film metrics and HOAs together. A search was conducted in Entrez PubMed on 25 April 2021 using the keywords “higher order aberrations” and “dry eye”. The initial search yielded 61 articles. After publications were restricted to only original articles measuring HOA outcomes in patients with dry eye, the final yield was 27 relevant articles. Of these 27 papers, 12 directly looked at associations and correlations between dry eyes and HOA parameters. The remaining 15 studies looked at dry eye interventions and HOA outcomes and parameters. There is clear evidence demonstrating that dry eyes and HOAs have an association, and that the tear film is one of the most important factors in this relationship. There is also a direct correlation between tear film metrics and HOAs. Improvements in HOAs with dry eye interventions provide further evidence to support the intricate relationship between the two. Despite the clear association between HOAs and dry eye disease, further research is still required in the realm of clinical application as dry eye interventions vary depending on many factors, including patient severity and eye drop viscosity.
Keywords: Dry eye disease, Dry eye treatment, Higher order aberrations, Tear film
Key Summary Points
| The rationale for this review was to determine the association between tear film metrics and higher order aberrations (HOAs), and to also determine if treatment of dry eyes improves tear film metrics and HOAs. |
| The literature was systematically reviewed, in that the total of 60 search hits with our key terms were then curated by the authors on the basis of original research and a focus on tear film metrics and HOA parameters, leading to a total of 26 relevant articles for this review. |
| This review has shown clear associations and correlations between dry eyes and HOA parameters. |
| Improvements in HOAs with dry eye interventions provide further evidence to support the intricate relationship between the two. |
| However, despite the clear association between HOAs and dry eye disease, further research is still required in the realm of clinical application as many factors such as patient severity and eye drop viscosity can impact clinical outcomes. |
Introduction
The formation of optical images on the retina marks the beginning stages of vision processing [1]. However, there are many possible avenues of error either through diffraction, errors of focus, and wavefront aberrations [1, 2]. When optical systems are in “perfect” settings, rays emanating from an object are refracted to converge to the unique image point as expected from Gaussian theory [1]. However, when the system suffers from wavefront aberrations, the refracted rays no longer converge to the expected unique image point [1]. Therefore, the image is defocused or can be distorted. In particular, higher order aberrations (HOAs) have been of growing interest. Although most HOAs do not cause any noticeable degradation in visual acuity below 20/20 vision, laser and other refractive surgeries (including cataract-related ones) have left patients with symptomatic complaints of dry eye related to HOAs [1, 3].
Aberrometers are able to measure wavefront aberrations, i.e., the distance between an actual wavefront and the ideal spherical or “reference” wavefront on the ideal image point [1]. One of the most common designs is the Hartmann–Shack aberrometer which shoots a narrow beam of light into the eye to produce a reflection [1]. If the eye is free of aberrations, this ideally would result in a parallel ray leaving the eye and the existing wavefronts strike a Hartmann–Shack wavefront sensor comprising an array of identical converging micro lenses [1]. The overall ideal result is image points reflecting directly in a regular grid pattern. However, when aberrations are present, these image points are displaced by an amount and direction depending on the aberration, resulting in an irregular grid pattern [1].
An important factor that affects HOAs includes the tear film [2, 4, 5]. The tear film is the first refracting surface that light comes into contact with and thus has a crucial role in maintaining a smooth corneal surface [2, 4, 5]. Changes to the tear film thickness and regularity can introduce additional aberrations [4]. As the eyes remain open, the tear film eventually breaks up and this also causes irregularity and increased aberrations [2, 4, 5]. Dry eye can be defined as a tear deficiency disorder of the ocular surface [6]. Several studies have demonstrated that disruptions of tear film caused by dry eye increase HOAs compared with normal eyes which can result in impaired visual function and optical quality [4, 6–9].
One way to address the symptoms and reported impaired optical quality of dry eyes is to use lubricating eye drops that have been shown to improve optical quality and significantly decrease aberrations associated with irregular tear films and dry eyes [2, 10–12]. Another strategy or intervention for dry eyes is punctal plugs to block the puncta allowing for increased tear fluid accumulation, thus keeping the tear film intact [13].
Dry eyes are one of the most common ocular disorders and a complication of many common laser and refractive surgeries, including cataract surgeries [1, 2, 13]. Therefore, it is important to understand any potential association or pathophysiology of HOAs and dry eyes, as well as whether interventions that improve dry eyes reduce HOA severity.
Methods
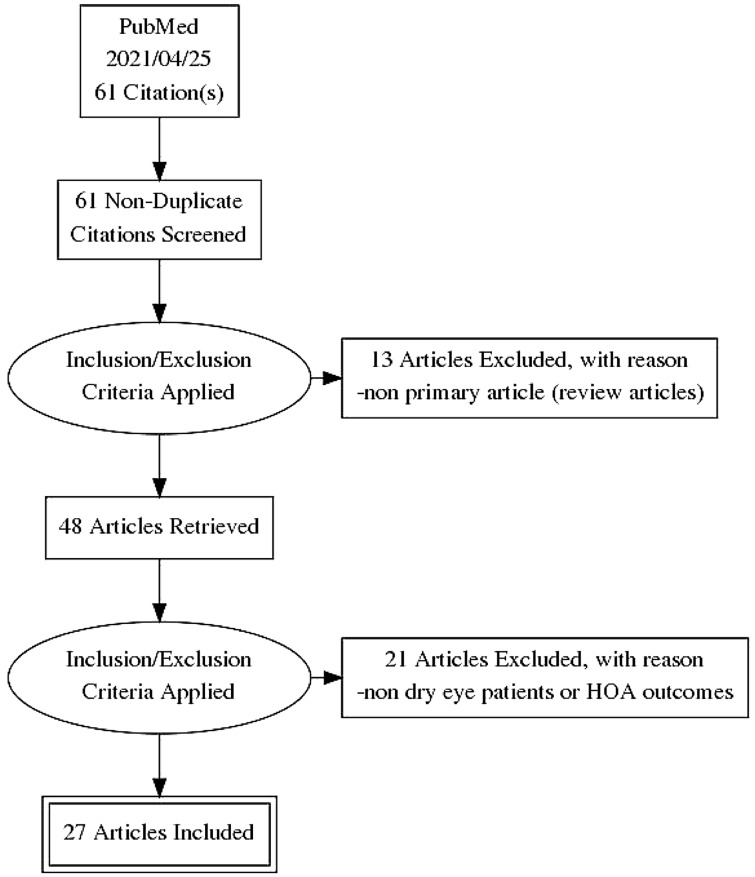
To determine the primary literature available focussing on HOAs and dry eye association as well as dry eye interventions and HOA outcomes, the following search strategy was used in Entrez PubMed on 25 April 2021. The key terms used were “higher order aberrations” and “dry eyes” with an “AND” between each keyword for a keyword search string of “higher order aberrations AND dry eyes”. No filters were set. This resulted in a total search hit of 61 articles. Figure 1 illustrates the screening process in a flowchart diagram. The articles were curated to determine whether they were original research articles; this excluded 13 articles as they were review articles. The second curation was based on subject relevance—if a paper did not look into dry eyes and HOAs as an outcome parameter, it would not be included. The second curation excluded 21 papers leaving a total of 27 relevant articles for this review (Fig. 1).
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) flowchart illustrating the selection process of articles
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
The search criteria and curation process yielded 27 relevant papers that looked at the primary outcome of HOAs in patients with dry eye. Of these 27 papers, 12 directly looked at any association and correlation of dry eyes and HOAs and HOA parameters. The remaining 15 studies looked at dry eye interventions and HOA outcomes and parameters. The main results of each paper are summarized in Tables 1 and 2.
Table 1.
Summary of HOAs and its association with dry eyes
| Reference/study | Country | Study design | Groups and sample size | HOA measuring device | Level of evidence | Parameters for efficacy | Main result | Associations and remarks |
|---|---|---|---|---|---|---|---|---|
|
Corneal higher-order aberrations (HOAs) in eyes with chronic ocular graft-versus-host disease Shimizu et al. 2020 [14] |
Japan | Retrospective comparison study | 30 eyes from 15 chronic ocular graft-versus-host disease (GVHD) cases and 30 eyes from 15 non-GVHD cases | Measured using anterior segment optical coherence tomography (AS-OCT)—OCT device | Level 3 |
Corneal HOAs, spherical aberrations (SA), and coma aberrations Correlation of corneal HOAs and visual acuity Correlation of International Chronic Ocular (ICO) severity score and visual acuity Correlation of corneal HOAs and ICO severity scores |
The total and anterior HOAs at both 4- and 6-mm diameters in patients with GVHD were significantly higher than non-GVHD and healthy controls Total and anterior SA at both 4- and 6-mm diameters were significantly lower in patients with GVHD compared to control Total and anterior coma aberrations at 4-mm diameters were significantly higher in patients with GVHD vs without GVHD. Total coma aberrations at 6-mm was significantly higher in GVHD vs control Corneal HOAs were significantly higher in patients with GVHD compared to those without GVHD There was a statistically significant positive correlation between HOAs and visual acuity in all HOAs (total, anterior, and posterior) at 4 mm and 6 mm There was a statistically significant positive correlation between ICO severity score and visual acuity There was a statistically significant positive correlation between HOAs and ICO severity scores for all HOAs (total, anterior, and posterior) at 4 mm and 6 mm |
There was no significant difference in posterior HOAs between groups There was no significant difference in SA between patients with GVHD and patients without GVHD. There was also no significant difference in posterior SA The correlation between posterior HOAs and ICO severity was significant but not as strong as total or anterior correlations |
|
Wavefront analysis of higher order aberrations in dry eye patients Montes-Mico et al. 2004 [4] |
Spain | Prospective comparison study | 20 patients with dry eyes and 20 patients with normal eyes | Measured using a Zywave aberrometer (Bausch & Lomb, Irvine, CA) which is based on the Hartmann–Shack aberrometer—ray tracing device | Level 2 |
HOAs Hartmann–Shack and color-coded maps of total wavefront aberrations |
HOAs in the patients with dry eye were significantly higher than in normal eyes for 4- and 6-mm diameter. Coma, spherical, and total aberrations for both 4- and 6-mm diameters were significantly greater in patients with dry eye compared to normal eyes In a 6-mm pupil for a normal and dry eye, quantitative analysis of the Hartmann–Shack image indicates a significant change in wavefront pattern in the dry eye compared to the normal eye |
HOAs in general were found to be higher in patients with dry eye compared to normal eyes Statistical and quantitative analysis of the Hartmann–Shack image was not shown |
|
Serial measurements of higher-order aberrations after blinking in patients with dry eye Koh et al. 2008 [15] |
Japan | Prospective comparison study |
20 patients with dry eyes Group A: 7 patients with superficial punctate keratopathy (SPK) in the central cornea Group B: 13 patients with SPK over the pupil and inferior paracentral cornea |
Measured using the Hartmann–Shack wavefront aberrometer (Topcon Corp., Tokyo, Japan)—ray tracing | Level 2 |
Total HOAs, fluctuation index (FI), stability index (SI), coma, and spherical aberrations Serial changes in HOAs |
Total HOAs, coma, and spherical aberrations were significantly higher in group B compared to group A In a 6-mm pupil for a normal and dry eye, quantitative analysis of the Hartmann–Shack image indicates a significant change in wavefront pattern in the dry eye compared to the normal eye In group A, total HOAs remained constant at each blink over 9 measurements taken over 10 s. In spherical aberrations, the aberrations were significantly higher at 7 and 9 s compared to at 2 s In group B, total HOAs remained relatively stable. For spherical aberrations, it was significantly higher at 9 s compared to at 2 and 4 s |
There was no significant difference in FI and SI between groups There were no significant differences in coma aberrations in both groups over the 10 s |
|
Higher order aberrations of the corneal surface after laser subepithelial keratomileusis Jung et al. 2014 [16] |
South Korea | Prospective comparison study | 16 patients with dry eyes and 15 patients with non-dry eyes that all underwent laser subepithelial keratomileusis (LASEK) | Measured using the Pentacam (Oculus; Optikgerate GmbH, Wetzlar, Germany)—OCT device | Level 2 |
Baseline characteristics Wavefront HOAs after blinking Correlation between HOAs and eye parameters |
At baseline the dry eye group had significantly lower tear breakup time (TBUT), Schirmer test, and tear clearance rate (TCR) compared to the non-dry eye group. Ocular surface staining and ocular surface disease index (OSDI) scores were significantly higher in the dry eye group compared to non-dry eye group Ten seconds after blinking, there was a significant decrease in total HOAs RMS, coma, and trefoil aberrations in the non-dry eye group compared to the dry eye group Total HOA root mean square (RMS), coma, and trefoil aberrations were significantly higher 10 s after blinking compared to immediately after in the dry eye group only There was a significant negative correlation with total HOA RMS, coma, and trefoil aberrations with TBUT. There was a significant positive correlation with total HOA RMS, coma, and trefoil aberrations with OSDI |
There was no significant difference in spherical aberrations between both groups. There was also no significant difference immediately after blinking for total HOA RMS, coma, trefoil, and spherical aberrations between both groups Lower TBUT scores were correlated with higher HOA RMS, coma, and trefoil aberrations. Higher OSDI scores were correlated with higher HOA, coma, and trefoil aberrations |
|
Dynamic wavefront aberrations and visual acuity in normal and dry eyes Wang et al. 2009 [17] |
China | Prospective comparison study | 30 dry eyes and 27 normal controls | Measured using a WASCA system (Model 1369–202, Carl Zeiss Meditec, Germany)—ray tracing device | Level 2 |
Changes in wavefront aberrations Changes in visual acuity Mean instability of tRMS and hoRMS of wavefront aberrations |
In general, wavefront aberrations changed and were more dynamic in patients with dry eye than normal eye patients Visual acuity changes were much more volatile patient to patient but changes in visual acuity on a logMAR scale had smaller amplitude changes in normal eyes The mean instability of tRMS and hoRMS in patients with dry eye was significantly greater than in the normal group The mean instability of visual acuity was also found to be higher in the dry eye group compared to the normal group |
The changes in right and left eye differed in patients with dry eye. The RMS value tended to increase during periods of open eyes and returned to minimum after a blink. In the left eye, decreased about 4–5 s before returning to minimum after a blink There was no significant difference in post-LASIK eyes |
|
Effect of tear film break-up on higher order aberrations of the anterior cornea in normal, dry, and post-LASIK eyes Lin et al. 2005 [18] |
Taiwan | Prospective comparison study | 40 post-LASIK eyes, 40 dry eyes, and 40 normal eyes | Measured using videokeratography—OCT device | Level 2 |
TBUT Corneal Topographies HOAs |
TBUT was significantly less for dry eyes compared to post-LASIK and normal eyes Patients with normal and dry eyes showed a significant pattern of increased aberrations from post-blink through BUT There was a significant decrease in coma, trefoil, 3rd to 6th order aberrations after saline addition in both patients with normal and dry eyes |
There was no significant difference in post-LASIK eyes |
|
Tear film aberration dynamics and vision-related quality of life in patients with dry eye disease Denoyer et al. 2012 [19] |
France | Prospective comparison study | 40 patients with Sjögren syndrome/dry eyes and 40 patients with normal eyes | Measured using the KR-1 aberrometer (Topcon, Clichy, France)—dual OCT and ray tracing | Level 2 |
Baseline characteristics Aberration dynamics by group Area under the curve of modulation transfer function (aucMTF) Correlations |
OSDI was significantly higher in dry eye vs normal eyes. TBUT and Schirmer test values were significantly lower in dry eye vs normal eyes There was a significant increase in total HOAs, coma, and trefoil aberrations in dry eyes compared to control eyes AucMTF was significantly decreased in patients with dry eye from 7 to 10 s after blinking compared to normal control A significant and negative correlation between TBUT and HOA progression index was found A significant and positive correlation between OSDI scores and HOA progression index was found |
|
|
The impact of dysfunctional tear films and optical aberrations on chronic migraine Shetty et al. 2017 [20] |
India | Prospective comparison study | 30 patients with migraines and 30 control patients | Measured using the Optical Path Difference (OPDIII, Nidek, Japan)—dual OCT and ray tracing | Level 2 | Baseline characteristics |
Total aberrations, HOAs, coma, spherical, and objective scatter index (OSI) were significantly higher in the control group compared to the migraine group Lipiview interferometric coloric units (ICU) were significantly lower in the control group compared to the migraine group |
There was no significant difference in trefoil aberrations and TBUT between the groups |
|
Corneal fluorescein staining correlates with visual function in dry eye patients Kaido et al. 2011 [7] |
Japan | Prospective comparison study | 10 patients with Sjögren’s and SPK, 12 patients with Sjögren’s but no SPK, 10 control patients | Measured using the Hartmann–Shack wavefront aberrometer (Topcon Corp., Tokyo, Japan)—ray tracing device | Level 2 |
Tear function and vital staining scores Visual acuity parameters Ocular HOA parameters Serial changes in HOAs Correlation between visual acuity and HOAs |
Schirmer value, fluorescein score, rose bengal score, and BUT were significantly different in the SPK+ group compared to control. Only Schirmer value was significantly lower in the SPK− group compared to control Visual maintenance ratio (VMR) was significantly lower in the SPK+ group compared to both SPK− and control groups. Variation of visual acuity was significantly higher in SPK+ group compared to both SPK− and control groups There was also a significant negative correlation between VMR and severity of epithelial damage. There was a significant positive correlation between variation of visual acuity and severity of epithelial damage Coma and total HOAs were significantly higher in the SPK+ group compared to the SPK− and control groups There was no significant change over the 10 s in coma, spherical, and total HOAs There were significant negative correlations between VMR and coma and total HOA |
No statistical analysis between the SPK+ and SPK− groups were assessed There was no significant difference in spherical, FI, and SI between all groups The SPK+ was the only group with fluctuation during the measurement period but this was not significant |
|
The impact of dry eye disease on visual performance while driving Deschamps et al. 2013 [21] |
France | Prospective comparison study | 20 patients with dry eyes and 20 patients with normal eyes | Measured using the dynamic aberrometer KR-1 (Topcon, Clichy, France)—dual OCT and ray tracing | Level 2 | Driving test scores |
The percentage of targets missed and average response time were significantly higher in patients with dry eye compared to control The progression index of total HOAs and trefoil aberrations were significantly higher in patients with dry eye compared to control There was a significantly positive correlation between response time and the progression index for HOAs as well as between response time and OSDI “symptom” subscale |
|
|
Paradoxical increase of visual impairment with punctal occlusion in a patient with mild dry eye Koh et al. 2006 [22] |
Japan | Case report | Patient with dry eye | Measured using the Hartmann–Shack wavefront aberrometer (Topcon Corp., Tokyo, Japan)—ray tracing device | Level 3 | HOAs | There was an increase in HOAs post-blink after punctal plug placement | The change in HOAs corresponded to coma aberrations but not spherical aberrations |
|
Effects of suppression of blinking on quality of vision in borderline cases of evaporative dry eye Koh et al. 2008 [23] |
Japan | Case report |
10 patients with short TBUT Normal stable group: stable pattern and small fluctuation pattern from normal eyes Normal-sawtooth group: sawtooth pattern of normal eyes Short TBUT group |
Measured using the Hartmann–Shack wavefront aberrometer (Topcon Corp., Tokyo, Japan)—ray tracing device | Level 3 |
Serial changes in HOAs Total HOAs, FI, and SI |
Total HOAs and coma aberrations were significantly higher from 5 to 9 s after a blink compared to those immediately after a blink Spherical aberrations were significantly higher from 6 to 9 s after a blink compared to immediately after The FI and SI in the short TBUT group were significantly higher than those in the normal-stable group |
There was no significant difference in FI and SI between the short TBUT group and the normal-sawtooth group |
Table 2.
Summary of dry eye interventions and impact on HOAs
| Reference/study | Country | Study design | Intervention | Follow-up period | HOA measuring device | Level of evidence | Parameters for efficacy | Main result | Remarks |
|---|---|---|---|---|---|---|---|---|---|
|
A preliminary investigation into the effects of ocular lubricants on higher order aberrations in normal and dry eye subjects McGinnigle et al. 2013 [24] |
UK | Randomized controlled trial (RCT) | Unpreserved Hypromellose drops vs Tears Again™ liposome spray vs combination in normal and dry eyes | 60 min after instillation | Measured using Nidek OPD-Scan III (Nidek Technologies, Gamagori, Japan)—dual OCT and ray tracing | Level 1 |
Strehl ratio for HOAs Total aberrations Spherical aberrations Coma |
Hypromellose drops led to a significant decrease in HOAs immediately after but no difference 1 h post intervention in both normal and dry eyes. Liposome spray caused no significant difference at any time point in both eyes. Combination has no significant difference at any point in both eyes Hypromellose drops increased total aberrations immediately after but decreased proportionally after an hour for both eye types. Liposome spray had no effect on total aberrations for each eye type. Combination had no effect for each eye type There were no significant changes in spherical aberrations for each intervention type (drops, spray, and combination) for each eye type There were no significant changes in coma for each intervention type (drops, spray, and combination) for each eye type |
HOAs were higher at baseline in the dry eye group The increase in total aberrations with Hypromellose drops was insignificant compared to baseline |
|
Effects of 3% diquafosol sodium ophthalmic solution on higher-order aberrations in patients diagnosed with dry eye after cataract surgery Inoue et al. 2016 [3] |
Japan | RCT | 3% diquafosol sodium (DQS) ophthalmic solution vs artificial tears (ATs) in dry eyes after cataract surgery | 4 weeks | Measured using a wavefront analyzer (KR-1 W; Topcon Corp, Tokyo, Japan)—dual OCT and ray tracing | Level 1 |
Tear film metrics: tear breakup time (TBUT), fluorescein staining, and Schirmer test scores HOA Fluctuation index (FI) and stability index (SI) |
TBUT was significantly decreased in both DQS and AT groups compared to preoperative BUT baseline values. BUT was significantly increased after 4 weeks of DQS instillation Corneal and conjunctival fluorescein staining was significantly increased in both groups postoperatively. DQS significantly reduced fluorescein staining after 4 weeks of instillation There was no significant change 4 weeks after cataract surgery in both groups HOAs trends showed upward curves in both groups 4 weeks after surgery. DQS treatment stabilized the pattern whereas AT treatment continued to have an upward curve pattern FI was significantly lower in the DQS group compared to the AT group SI was significantly lower in the DQS group compared to the AT group |
4 weeks of AT instillation did not significantly increase BUT 4 weeks of AT instillation did not significantly reduce fluorescein staining There was no significant difference in the FI before and after 4 weeks of instillation for both DQS and AT groups There was no pre- and postoperative difference in SI for the DQS group but the AT group showed a significant increase in SI postoperatively after 4 weeks of instillation |
|
Effects of sodium hyaluronate on wavefront aberrations in dry eye patients Lekhanont et al. 2014 [25] |
Thailand | RCT |
100 eyes from 50 patients 0.18% sodium hyaluronate (SH) vs 0.9% sodium chloride in patients with dry eye |
1 min, 10 min, 30 min, 1 h, and 2 h after instillation | Measured using a Zywave II aberrometer (Bausch & Lomb, Irvine, CA, USA)—ray tracing device | Level 1 |
Baseline characteristics HOAs Coma and spherical aberrations Eye symptoms Adverse events |
No significant differences in baseline characteristics of Schirmer test value, TBUT, corneal fluorescein staining, pupil diameter, HOAs, and severity of dry eye symptoms At baseline, HOAs were not significantly different in both treatment and control eyes There was a significant decrease from baseline in spherical aberrations in the treatment group 1 min after instillation but this gradually increased back to baseline at later time points The treatment group showed significant reductions in visual analogue scale (VAS) for 6/12 symptoms: scratchiness, dryness, grittiness, burning, ocular fatigue, and photophobia No reported ocular or systemic adverse events or complications with treatment |
No patient had associated rheumatic disease There was no significant difference in HOA at any time point in both eye groups There was no significant difference in coma aberrations after treatment compared to baseline This was a double-blind study and significant improvement was found at all time points for treated eyes |
|
The short term effect of trehalose and different doses of sodium hyaluronate on anterior corneal aberrations in dry eye patients Yildirim et al. 2021 [26] |
Turkey | Prospective comparison study | 0.15% SH vs 0.2% SH vs trehalose + 0.15% SH in patients with dry eye | Immediately after and 10 min after instillation | Measured using a Pentacam Tomography imaging (PTC, Oculus Inc, Lynnwood, WA, USA; version: 1.21r41)—OCT device | Level 2 |
Baseline characteristics Total root mean square (RMS), lower order aberration (LOA), HOAs, and spherical aberrations |
No significant differences in baseline characteristics of Schirmer test value and TBUT Total RMS, LOA, HOAs, and spherical aberrations after each treatment group were significantly decreased compared to baseline. In 0.15% SH and 0.2% SH groups, vertical trefoil was significantly increased after treatment compared to baseline. Horizontal coma was increased after treatment in all groups compared to baseline |
Protection and prevention of histological changes caused by NMDA There was no significant difference between different treatment groups |
|
The effect of lifitegrast on refractive accuracy and symptoms in dry eye patients undergoing cataract surgery Hovanesian et al. 2020 [27] |
USA | Prospective comparison study | 5% lifitegrast ophthalmic solution in patients with dry eye undergoing cataract surgery | 28-day course of intervention | Measured using the Zeiss Atlas topographer (Dublin, California, USA)—OCT device | Level 2 |
Anterior corneal power measurements HOAs Standardized patient evaluation of eye dryness (SPEED) questionnaire Corneal staining TBUT Conjunctival redness |
Eyes treated with 5% lifitegrast for 28 days had more significantly accurate predicted spherical equivalent (SE) refraction for the lens actually implanted when measured There was a significant improvement in HOAs in 65% (44/77) of patients after the first course of treatment. There was a significant improvement in HOAs in 54% (27/77) of patients after the full course of treatment measured postsurgery and compared to baseline There was a significant improvement in SPEED questionnaire from baselines scores of 8.1 ± 6.6 to 4.0 ± 3.2 after preoperative treatment and second round postsurgery Corneal staining measured with the Oxford scale was significantly reduced after pre- and postoperative courses of treatment There was a significant improvement in TBUT after the pre- and postoperative courses of treatment Conjunctival redness was measured with the Schulze scale and there was significant improvement after the pre- and postoperative courses of treatment |
There was also a significant increase in HOAs in 26% (13/77) of patients after the full course of treatment measured postsurgery and compared to baseline SPEED scores > 10 are considered symptomatic of dry eye disease |
|
Clinical effects and safety of 3% diquafosol ophthalmic solution for patients with dry eye after cataract surgery: a randomized controlled trial Park et al. 2016 [28] |
South Korea | RCT | 3% DQS vs 0.1% SH in patients with dry eye after cataract surgery | 12 weeks | Measured using a KR-1W wavefront analyzer (Topcon Medical System, Inc, Tokyo, Japan)—dual OCT and ray tracing | Level 1 |
Mean changes in ocular surface disease index (OSDI) TBUT Schirmer test Fluorescein staining Conjunctival lissamine (LG) staining HOAs Trefoil, coma, tetrafoil, and second astigmatism Uncorrected distance visual acuity (UDVA) Anterior chamber inflammation |
OSDI scores were significantly lower in both treatment groups compared to baseline after 12 weeks TBUT was significantly longer in the DQS group than in the SH group Schirmer test values with DQS treatment were significantly higher compared to SH treatment Corneal fluorescein staining was significantly lower in the DQS group than in the SH group but both groups showed significant improvement compared to baseline after 12 weeks LG staining was significantly lower in the DQS group than in the SH group but both groups showed significant improvement compared to baseline after 12 weeks SH treatment significantly lowered HOAs compared to DQS treatment after 12 weeks There was no significant difference between the two groups for trefoil, coma, tetrafoil, and second astigmatism Both groups significantly improved UDVA by the 1-week mark postsurgery and sustained this improvement There was no significant difference in anterior chamber inflammation pre- and postoperatively and at any time points |
There was no significant difference between the treatment groups and at the 1-week postsurgery there was an increased OSDI score that recovered towards baseline by 4 weeks TBUT at postoperative week 12 was significantly longer than at baseline for DQS treatment whereas SH treatment returned to baseline by 12 weeks There was no significant difference between pre- and postoperative measurements in the DQS group but the SH group never returned to baseline after 12 weeks There was no significant difference in pre- and postoperative HOAs for both groups There was no significant difference between the two groups though inflammation reached its peak 1-week postsurgery and declined to baseline by 12 weeks for both groups |
|
Effectiveness and optical quality of topical 3.0% diquafosol versus 0.05% cyclosporine A in dry eye patients following cataract surgery Lee et al. 2016 [29] |
South Korea | RCT | 3% DQS vs 0.05% cyclosporine A in patients with dry eye after cataract surgery | 3 months | Measured using a Hartmann–Shack wavefront aberrometer (WASCA; Carl Zeiss Meditec, Oberkochen, Germany)—ray tracing device | Level 1 |
TBUT Schirmer test Corneal staining OSDI HOAs Vertical coma |
The DQS group had significantly better TBUT results at 1 and 3 months compared to the cyclosporine A group There was a significant improvement in Schirmer test scores at 2 and 3 months for the DQS group and 1 and 3 months for the cyclosporine A group compared to baseline There was a significant improvement ocular staining at all time points for both treatments compared to baseline All OSDI scores showed a decreasing trend but was not significant for either treatment group compared to baseline There was a significant improvement in HOAs in the cyclosporine A group at 2 and 3 months compared to baseline. Cyclosporine A treatment at 3 months was also significantly better than DQS Vertical coma significantly improved in the cyclosporine A group at 3 months compared to baseline and significantly compared to DQS treatment at 2 and 3 months |
There was a significant difference in TBUT results compared to baseline at 1, 2, and 3 month time points in the DQS group but only at 2 months for the cyclosporine A group There was no significant difference in improvements between the two groups There was no significant difference between the two groups SPEED scores > 10 are considered symptomatic of dry eye disease There was no significant difference in DQS treatment compared to baseline All other optical aberration values showed no significant difference |
|
The effect of punctal occlusion on wavefront aberrations in dry eye patients after laser in situ keratomileusis Huang et al. 2004 [30] |
USA | Prospective comparison study |
Punctal occlusion in patients with dry eyes post LASIK vs patients with non-dry eyes post LASIK |
1 month | Measured using a Hartmann–Shack wavefront sensor (Zywave; Bausch & Lomb, Rochester, New York, USA)—ray tracing device | Level 2 |
Total RMS wavefront error values, lower order wavefront errors, defocus, and astigmatism Higher order RMS wavefront errors Third, fourth, and fifth-order aberrations HOAs Visual acuity |
Dry eyes after 1 month post-punctal occlusion had significantly improved total RMS wavefront error values, lower order wavefront errors, defocus, and astigmatism compared to measurements pre-punctal occlusion There was a significant improvement in higher-order RMS wavefront error in patients after punctal plug insertion There was a significant reduction/improvement in RMS wavefront measures in the third, fourth, and fifth-order aberrations after punctal occlusion There was a significant reduction/improvement in coma and spherical aberration after punctal occlusion There was improvement in visual acuity in patients with punctal occlusion |
There were no significant changes in trefoil after punctal plug These results were not determined to be significant |
|
Effect of instillation of eyedrops for dry eye on optical quality Koh et al. 2013 [11] |
Japan | Prospective comparison study | 0.3% SH vs 3% DQS vs 2% rebamipide drops in healthy eyes | 1 min, 5 min, and 10 min after instillation | Measured using a custom-developed Hartmann–Shack wavefront aberrometer (Topcon Corp., Tokyo, Japan)—ray tracing device | Level 2 |
Coma-like aberrations, spherical-like aberrations, and total HOAs Forward light scatter |
There was a significant increase in coma, spherical, and total HOAs immediately after instillation for all 3 drops compared to baseline. SH had significantly higher values immediately after instillation compared to DQS, rebamipide, and control There was a significant increase in forward light scatter immediately after rebamipide instillation compared to baseline and compared to all other groups |
At 5 and 10 min after instillation, there were no significant differences in the HOA components among all groups At 5 and 10 min after instillation, there were no significant differences in forward light scatter among all groups |
|
Effects of lipid- versus sodium hyaluronate-containing eye drops on optical quality and ocular surface parameters as a function of the meibomian gland dropout rate Miháltz et al. 2018 [31] |
Austria | RCT | Artelac Lipid vs 0.2% SH in patients with dry eyes | 3 months | Measured using the iTrace VFA—ray tracing device | Level 1 |
Schirmer test, TBUT, ocular surface staining, symptom score, meibomian gland (MG) dropout rate, corneal higher order RMS (HORMS), HO Strehl ratio, and HO modulation transfer function (MTF) HO Strehl ratio based on MG loss severity HORMS values based on MG loss severity |
Both groups had significant improvement in Schirmer test, TBUT, ocular surface staining, and the symptom core after 3 months of treatment compared to baseline There was a significant improvement in SPEED questionnaire from baselines scores of 8.1 ± 6.6 to 4.0 ± 3.2 after preoperative treatment and second round postsurgery Corneal staining measured with the Oxford scale was significantly reduced after pre- and postoperative courses of treatment There was a significant increase in corneal HO Strehl ratio in patients with an MG dropout rate > 50% in the lipid group There was a significant decrease in corneal HORMS in patients with an MG dropout rate > 50% in the lipid group |
Both groups had no significant changes to MG dropout rate, corneal HORMS, the HO Strehl ratio, and HO MTF. There was no significant difference when comparing treatment groups There was no significant difference in HO Strehl ratio in patients with an MG dropout rate > 50% in the SH group There was no significant difference in corneal HORMS in patients with an MG dropout rate > 50% in the SH group |
|
Optical quality after instillation of eyedrops in dry-eye syndrome Montes-Mico et al. 2010 [32] |
Spain | Prospective comparison study | Lubricating eye drops (Blink Intensive Tears) in patients with dry eyes | Immediately after and 10 min after instillation | Measured by computerized videokeratography (PCT 200, Optopol Technology S.A.)—OCT device | Level 2 |
Mean TBUT Corneal wavefront aberration contour plots Retinal point-spread function (PSF) Higher-order, spherical-like, and coma-like aberrations |
TBUT was significantly lengthened the mean TBUT at 10 min compared to at 0 min (baseline) There was change in the number of contour lines between baseline and after artificial tear instillation There was an improvement in PSF after eye drop instillation Higher-order, spherical-like, and coma-like aberrations were all significantly decreased after drop instillation and this reduction was maintained and significant at 10 min |
At 5 and 10 min after instillation, there were no significant differences in the HOA components among all groups This change in wavefront aberration contour plots was not qualitative and not quantified This change in PSF was not qualitative and not quantified There was no significant difference in reduction at 0 and 10 min |
|
Effect of rebamipide ophthalmic suspension on optical quality in the short break-up time type of dry eye Koh et al. 2013 [33] |
Japan | Prospective comparison study | 2% rebamipide drops in patients with short breakup time (BUT) of the tear time type of dry eye | Baseline, 2 weeks, and 4 weeks | Measured using the KR-1W (Topcon, Tokyo, Japan)—dual OCT and ray tracing | Level 2 |
Tear film BUT Fluorescein staining scores Schirmer test scores HOAs—corneal, coma-like, and spherical-like Fluctuation index (FI) and stability index (SI) |
There was a significant increase in tear film BUT at 2 and 4 weeks after treatment when compared to baseline There was no significant difference in fluorescein staining scores at 2 and 4 weeks after treatment There was a significant decrease in Schirmer test scores at 4 weeks but not at 2 weeks after treatment HOAs were recorded for 10 s and there was a significant upward trend at baseline during the 10 s recording for corneal, coma-like, and spherical-like aberrations There was a significant variation/increase in spherical-like aberrations at the 2 week period during the 10 s recording The FI before treatment was significantly higher than at the 2- and 4-week time points. The SI before treatment was significantly higher only compared to the 4-week time point |
There were no significant changes at the 4-week period |
|
Effect of diquafosol ophthalmic solution on the optical quality of the eyes in patients with aqueous-deficient dry eye Koh et al. 2014 [34] |
Japan | Prospective comparison study | 3% DQS drops in patients with aqueous-deficient dry eyes | 15 min and 4 weeks after instillation | Measured using a custom-developed Hartmann–Shack wavefront aberrometer (Topcon Corp., Tokyo, Japan)—ray tracing device | Level 2 |
Dry eye symptoms Mean corneal staining scores Conjunctival staining Schirmer test scores Mean total HOAs, coma-like aberrations, spherical-like aberrations, FIs, and SIs |
There was a significant improvement in dry eye symptoms after treatment There was a significant decrease in corneal staining scores after treatment There was no significant change in conjunctival staining There was no significant change in Schirmer test scores There were significant decreases in mean total HOAs and spherical-like aberrations at 4 weeks compared to baseline |
There were no significant differences in mean total HOAs and spherical-like aberrations at 15 min compared to baseline. There were also no significant differences in coma-like aberrations, FIs, and SIs at any time points compared to baseline |
|
Effects of diquafosol tetrasodium administration on visual function in short break-up time dry eye Kaido et al. 2013 [35] |
Japan | Prospective comparison study | DQS drops in patients with symptomatic dry eye and short BUT vs patients without dry eye symptoms and short BUT | 1 month | Measured using the Hartmann–Shack wavefront aberrometer (Topcon Corp., Tokyo, Japan)—ray tracing device | Level 2 |
BUT values logMAR functional, minimal and maximal visual acuities, and HOAs |
There was a significant increase in BUT values in symptom-negative BUT patients treated with DQS Symptom-positive BUT patients treated with DQS had a significant decrease in logMAR functional, minimal and maximal visual acuities, and HOAs |
There was an increase trend in symptom-positive BUT patients treated with DQS but this was not significant There was no significant change in symptom-negative BUT patients |
|
Effects of preservative-free 3% diquafosol in patients with pre-existing dry eye disease after cataract surgery: a randomized clinical trial Jun et al. 2019 [36] |
South Korea | RCT | 3% DQS drops in patients with pre-existing dry eye disease after cataract surgery | 1 and 3 months | Measured using the iTrace (Tracey Technology, Texas, USA)—ray tracing device | Level 1 |
TBUT OSDI scores Meibomian gland dysfunction (MGD) HOAs |
TBUT was significantly improved in the preservative-free 3% DQS (group 1), and preservative-containing 3% DQS (group 2) groups compared to preoperative baseline after 1 month. Only group 1 remained significantly improved after 3 months OSDI scores were significantly improved in groups 1 and 2 at both 1 and 3 months MGD stage was significantly improved in group 2 compared to preoperative measurements after 1 month. However only group 1 showed significant improvement in MGD stage at 3 months HOAs were reduced for all 3 groups at all points throughout the study and there were no significant differences between the groups |
The preservative-free 0.15% SA (group 3) group had no significant improvement at both 1 and 3 months postoperatively compared to baseline MGD staging was significantly lower in groups 1 and 2 when compared to group 3 |
HOAs and Dry Eye Association
The first paper retrospectively reviewed patients with chronic ocular graft-versus-host disease (GVHD) after hematopoietic stem cell transplantation (HSCT) with dry eye disease [14]. Dry eye is the main and most common phenotype for GVHD in the eye. Although chronic ocular GVHD does not typically lead to visual loss and recipients generally have good visual acuity, the vision-related quality of life is impaired. The total and anterior HOAs at 4-mm and 6-mm diameters in patients with GVHD were significantly higher compared to both non-GVHD and healthy controls. Total and anterior spherical aberrations (SA) at both 4-mm and 6-mm diameters were significantly lower in patients with GVHD compared to healthy controls. Total and anterior coma aberrations at 4-mm diameters were significantly higher in patients with GVHD compared to patients without GVHD while total coma aberrations at 6-mm were significantly higher in GVHD compared to healthy controls. When the HOAs in the same patients were analyzed and compared to their contralateral eyes, patients with GVHD had significantly higher HOAs compared to patients without GVHD. A significantly positive correlation was found between HOAs and visual acuity (logMAR) as well. Although dry eye is the most common phenotype for GVHD in the eye, the increase in HOAs revealed could also be attributed to the inflammation on the ocular surface as opposed to a direct effect of dry eyes.
One group prospectively assessed HOAs in patients with normal and dry eyes [4]. The group was able to demonstrate that HOAs were significantly higher in patients with dry eye for both 4-mm and 6-mm diameters. This included coma, spherical, and total aberrations for both 4- and 6-mm diameters. Their quantitative analysis of the Hartmann–Shack images showed a significant change in the wavefront patterns in dry eyes compared to normal eyes. Specifically, these corresponded to reduced optical path length, which indicated relative thinning of the tear film compared to areas on the lateral sides of the cornea (left and right) and increased thickening of the tear film at the inferior portion of the cornea. Although differences in vertical and horizontal coma aberrations are expected as a result of gravitational effects on the tear layer and recovery from the effects of lid pressure after blinking, these expected differences were significantly higher in dry eyes compared to normal eyes. These changes in tear film in dry eyes may be responsible for the aberrations and irregularities of the corneal surface.
Another group prospectively assessed serial measurements of HOAs after blinking in patients with dry eyes with or without superficial punctate keratopathy (SPK) [15]. SPK occurs in patients with chronic dry eye disease in which small groups of cells are damaged as a result of inadequate tear production [37]. The total HOAs in the group with SPK were significantly higher than the group without SPK. Similarly, both coma- and spherical-like aberrations were significantly higher in the group with SPK compared to the group without SPK [15]. In the group without SPK, spherical aberrations were significantly higher at 7 and 9 s compared to 2 s after the blink. In the group with SPK, spherical aberrations were also higher at 9 s compared to at 2 and 4 s after the blink [15]. The increases in spherical-like aberrations over time between blinks found in both groups were also observed in normal eyes in a previous study by the same group [38]. These results suggest that HOAs in dry eye with SPK in the central cornea are higher than those in dry eye without SPK [15].
As mentioned before, laser and refractive surgeries have been shown to cause dry eyes and an increase in HOAs [1, 3, 16]. One group prospectively assessed HOAs in patients who underwent laser subepithelial keratomileusis (LASEK) [16] with and without dry eye. At baseline, the dry eye group had significantly lower tear breakup time (TBUT), Schirmer I test values, and tear clearance rate compared to the non-dry eye group [16]. The ocular surface staining and ocular surface disease index (OSDI) were significantly higher in the dry eye group compared to the non-dry eye group at baseline. Postoperatively, at 10 s after blinking, the dry eye group had significantly higher total HOA, coma, and trefoil aberrations compared to the non-dry eye group. The total HOA, coma, and trefoil aberrations were also significantly higher 10 s after a blink compared to immediately after in the dry eye group [16]. Correlation analysis also revealed that total HOA, coma, and trefoil aberrations had a significantly negative correlation with TBUT while the correlation was significantly positive with OSDI score. These results suggest that additional HOAs caused by tear film instability in patients with dry eye after LASEK may lead to a further reduction in optical quality [16]. Another group prospectively assessed HOAs in patients who underwent laser-assisted in situ keratomileusis (LASIK) and compared this to patients with dry eyes and normal eyes [18]. The TBUT was significantly lower for dry eyes compared to both post-LASIK and normal eyes [18]. There was a significant increase in HOAs from post-blink to BUT in patients with normal and dry eyes and a subsequent decrease in HOAs after saline addition [18]. Interestingly, post-LASIK eyes showed no significant differences between the phases [18].
The tear film is subject to dynamic changes and one group assessed the dynamic properties and changes of wavefront aberrations in patients with dry eye and normal eyes [17]. Overall, the group noted that changes in wavefront aberrations and visual acuity is dynamic and variable patient-to-patient (in both dry and normal eyes) [17]. However, the mean instability of total wavefront aberrations and HOAs were significantly greater in patients with dry eye than in normal patients. Similarly, the mean instability of visual acuity was significantly higher in patients with dry eye compared to the normal patients [17]. Interestingly, the instability of visual acuity was dependent on blink rate in the dry eye group, showing that patients with a higher blink rate had more stable visual acuity [17]. This could suggest that patients with dry eye may compensate for tear breakup with increased blinking to maintain stable vision [17]. Another group similarly assessed tear film aberration dynamics in patients with dry eye disease (Sjögren’s syndrome) and normal patients [19]. At baseline, they found that the patients with dry eye had significantly lower TBUT and Schirmer test values compared to the control group [19]. Meibomian dysfunction and ocular surface disease index (OSDI) scores were significantly higher for patients with dry eye compared to control [19]. After blinking, there was a significant increase in total HOAs, coma, and trefoil aberrations in patients with dry eye [19]. This increase in aberrations was not seen in the control eyes. Total HOAs, coma, and trefoil aberrations were also significantly higher in dry eyes compared to control eyes [19]. The area under the curve of modulation transfer function (aucMTF), where MTF is the measurement of the ability of an optical system to transfer various levels of detail from object to image, was found to be significantly lower in patients with dry eye disease than controls at 7, 8, 9, and 10 s after blinking [19]. There was also a significantly negative correlation between TBUT and HOA progression index, and a significantly positive correlation between OSDI scores and HOA progression index [19]. The study was able to demonstrate that the time course of tear film HOAs correlates with the clinical examination (TBUT) and patient-reported outcomes (OSDI scores) of dry eye [19].
Dry eye disease has been noted to be more frequent in patients with migraine [20]. One group assessed the impact of dysfunctional tear films and aberrations in patients with migraine and normal eyes [20]. Total aberrations, total HOAs, coma aberrations, spherical aberrations, and objective scatter index (OSI) were significantly higher in normal patients compared to the patients with migraine [20]. Trefoil aberrations and TBUT were not significantly different between the groups [20]. Patients with dry eyes as evaluated with a Schirmer test score < 10 mm/5 min were excluded [20]. The group’s rationale behind this was to prevent overestimation of aberration profile with patients with confirmed dry eyes [20]. On the basis of the results, patients with migraines do not have increased evidence of dry eyes or HOAs.
Another group assessed wavefront aberrations and functional visual acuity as the major causes of visual deterioration in patients with dry eye and Sjögren’s syndrome [7]. The group also specifically looked at patients with dry eye and Sjögren’s syndrome with and without SPK. The mean visual maintenance ratio (VMR) in the group with SPK was significantly lower than those without SPK and the normal group. The VMR was significantly lower in the group without SPK compared to the normal group [7]. The variation in visual acuity in the group with SPK was significantly higher than in the group without SPK and the normal group. Total HOAs and coma-like aberrations were significantly higher in the SPK group compared to those in the group without SPK and the normal group [7]. Serial changes in HOAs were also tracked and measured over 10 s; however, there were no significant changes in coma, spherical, and total HOAs in any of the groups. A significant negative correlation was found between VMR and both coma and total HOAs [7].
The impact of dry eye disease and functional visual impact in the context of driving was explored by another group [21]. The eyes of patients with dry eye and control patients were compared and total HOAs, coma, and trefoil aberrations varied significantly overtime in patients with dry eye, whereas this variation in aberrations was not found in control patients [21]. To assess the functional impact higher levels of HOA variations have on patients with dry eye, both groups underwent a driving visual performance assessment which required patients to identify targets. Patients with dry eye had a significantly longer response time to identify targets compared to control and were able to detect fewer targets compared to the control group. A significant positive correlation was also found between HOAs and the response time and OSDI symptom score.
In a unique case report, one group reported a woman with Sjögren’s syndrome who underwent punctal plug placement to improve her dry eye symptoms [22]. However, despite dry eye symptom improvements, the patient reported epiphora and blurred vision immediately after blinking [22]. The total HOAs during the few seconds after blinking were spiked higher than before the punctal plug insertion [22]. Although these HOAs gradually declined and stabilized, a paradoxical increase in HOAs was observed in this patient after punctal plug insertion [22]. The same group also looked into the effects of suppressing blinking on vision quality in 10 patients with no ocular disease but short TBUT [23]. This group was further divided into a normal stable, normal-sawtooth, and short TBUT group [23]. The total HOAs and coma-like aberrations were significantly higher from 5 to 9 s after a blink compared to immediately after a blink [23]. Spherical-like aberrations were significantly higher from 6 to 9 s after a blink compared to immediately after a blink [23]. When the three groups were compared in terms of HOAs, fluctuation index (FI), and stability index (SI), the short TBUT group had significantly higher FI and SI compared to the normal stable group. There were no significant differences in FI and SI between the normal-sawtooth and short TBUT group [23].
Overall, the published evidence provides a clear link between dry eye disease and HOAs, in which HOAs are increased with dry eye severity [4, 7, 14–16, 19, 39]. One of the most important factors to consider is the tear film in the context of dry eyes and HOAs, as many of the studies have demonstrated a significant decrease in TBUT in patients with dry eye [7, 16, 18, 19]. Tear film issues should be readily attenuated with lubricant drops, whereas punctate keratitis may not be so readily treated with lubricants. Showing improvements in HOAs after treating dry eyes helps strengthen the relationship and association of HOAs and dry eye severity. Therefore, it is also important to explore whether improvements in dry eye parameters impact HOA severity.
Dry Eye Interventions and Their Effects on Tear Film Metrics and HOA Severity
Artificial tears are the first-line treatment for dry eye and seem to have a lubrication effect [24]. However, the preservatives in artificial tears have been demonstrated to be detrimental to the ocular surface [24]. Therefore, unpreserved eye drops or alternatives such as liposome sprays are preferred options [24]. The first paper examined dry eye interventions and HOA outcomes using unpreserved Hypromellose drops, a liposome spray solution (Tears Again™), and the combination of the two in normal and dry eyes in an RCT of 48 participants [24]. There was a significant decrease in HOAs immediately after Hypromellose drop instillation compared to baseline in both normal and dry eyes [24]. However, this difference was no longer significant 1 h after intervention in both eye types. There was no significant difference in the liposome spray or combination intervention at any time point for both eye types [24]. Hypromellose drops significantly increased total aberrations immediately after instillation compared to baseline in both normal and dry eyes but there was a similarly sized and significant reduction 1 h after intervention in both eye types [24]. Liposome and combination intervention had no significant effect on total aberrations at any time point for both eyes [24]. There were no significant changes in spherical or coma-like aberrations with Hypromellose, liposome, or combination intervention for both eyes [24]. Despite insignificant and short-lived changes in HOAs, both eye type groups reported higher subjective comfort scores after combination treatment, followed by liposome spray, and Hypromellose drops last [24].
Diquafosol sodium ophthalmic solution (DQS) promotes the secretion of water and mucin from conjunctival cells and has been shown to be effective in treating dry eyes, improving visual function, and effective even in post-cataract dry eyes [3]. This group assessed the effects of 3% DQS and artificial tears (AT) in patients with dry eye after cataract surgery in an RCT of 42 participants [3]. Tear film breakup time was significantly decreased in both DQS and AT groups compared to preoperative TBUT baseline values [3]. After 4 weeks of DQS instillation there was a significant increase in TBUT, but no significant changes in TBUT were seen with AT [3]. Similarly, corneal and conjunctival fluorescein staining was significantly increased in both DQS and AT groups postoperatively but only DQS significantly reduced fluorescein staining after 4 weeks of instillation [3]. There were no significant changes in HOAs after 4 weeks post-cataract surgery in both groups, although DQS treatment stabilized HOA patterns, whereas AT treatment continued to have an upward curve pattern [3]. The FI and SI were significantly lower in the DQS group compared to the AT group [3]. DQS treatment was able to stabilize the pattern of HOAs, while AT treatment continued to show increasing sawtooth patterns [3]. Another group assessed the effects of 3% DQS on 16 patients with aqueous-deficient dry eyes in a prospective comparison study [34]. There were significant improvements in dry eye symptoms and corneal staining after treatment [34]. Schirmer test scores and conjunctival staining were not significantly changed after treatment though [34]. HOAs and spherical aberrations were significantly improved after 4 weeks of instillation when compared to baseline values [34]. However, no changes in coma-like aberrations, FIs, and SIs were seen when compared to baseline values [34]. DQS drops were also assessed in 11 patients with dry eye symptoms and short TBUT compared to patients without dry eye symptoms and short TBUT [35]. There was a significant improvement in TBUT in symptom-negative patients treated with DQS but not with symptom-positive patients [35]. The logMAR functional minimal, maximal, and visual acuities were significantly improved in symptom-positive patients, as were HOAs [35].
Sodium hyaluronate (SH) is a glycosaminoglycan that improves tear film stability and decreases washout from the ocular surface [25]. SH also binds water and resists dehydration to promote corneal epithelial wound healing [25]. One group assessed the effects of 0.18% SH drops and a 0.9% sodium chloride (NaCl) solution on 50 patients with dry eye in an RCT [25]. At baseline, there were no significant difference in HOAs in both SH- and NaCl-treated eyes [25]. HOA was measured over 2 h after SH or NaCl instillation and there was no significant difference in HOAs at any time point in both eye groups [25]. There was a significant decrease in spherical aberrations 1 min after SH instillation, but this gradually increased to baseline levels at later time points [25]. Reported dry eye symptoms were significantly reduced in SH-treated eyes compared to NaCl control [25]. Another group assessed SH at differing concentrations, 0.15% and 0.2%, along with a combination of 0.15% SH and trehalose in patients with dry eye in a prospective comparison study [26]. Trehalose provides a hypo-osmolar effect and has positive contributory effects on the corneal surface and cell survival by stabilizing membrane lipids and proteins during desiccation [26]. Trehalose and SH have also been shown to have synergistic action together in the context of dry eyes [26]. The total root mean square (RMS) values of lower order aberrations (LOAs), HOAs, and spherical aberrations were all significantly decreased compared to their respective baseline values for each treatment group (0.15% SH, 0.2% SH, and 0.15% SH + trehalose) [26]. However, there was no significant difference amongst the treatment groups [26]. Another group compared and assessed the effects of 0.2% SH and a lipid-based eye drop (Artelac Lipid) on 30 patients with dry eyes in an RCT [31]. There was a significant improvement in Schirmer test, TBUT, ocular staining, and symptom relief after 3 months in both SH- and lipid-treated groups compared to baseline values [31]. There was no significant change in HOAs compared to baseline values [31]. In patients with a meibomian gland (MG) dropout rate greater than 50%, lipid treatment was able to significantly improve higher order Strehl ratio and HOAs compared to baseline [31].
The effect of 3% DQS compared to 0.1% SH in 86 patients with dry eyes after cataract surgery was also assessed in an RCT [28]. Ocular surface disease index (OSDI) was significantly lower in both treatment groups compared to baseline after 12 weeks of treatment, but there was no difference between the treatment groups [28]. TBUT, Schirmer test, and fluorescein staining were significantly improved in the DQS group compared to the SH group [28]. HOAs were significantly lowered and stabilized earlier in the DQS group compared to the SH group, although both groups had no significant difference between pre- and postoperative measurements of HOAs [28]. There was no significant difference in trefoil, coma, tetrafoil, and second astigmatism in both groups after 12 weeks of treatment [28]. Uncorrected distance visual acuity was significantly improved by the 1-week mark postsurgery in both groups and sustained within the 12-week treatment period [28]. DQS treatment was superior to SH in improving TBUT, changes in HOAs, Schirmer values, and staining scores throughout a 12-week follow-up period [28]. Another study similarly assessed the effects of 3% DQS (with and without preservatives) compared to 0.15% SA in 150 patients with pre-existing dry eye disease after cataract surgery in an RCT [36]. TBUT was significantly improved for the preservative-free 3% DQS and preservative-containing 3% DQS group compared to baseline measurements 1 month postoperatively [36]. However, after 3 months, only the preservative-free 3% DQS group was significantly improved compared to baseline. OSDI scores were significantly improved at all time points throughout the study in both the preservative-free and preservative-containing 3% DQS groups. MGD stage was significantly reduced in the preservative-containing DQS group at 1 month postoperatively; however at 3 months, only the preservative-free DQS group had significantly improved MGD stage compared to group 3 [36]. HOAs were all significantly improved compared to baseline values for all treatment groups compared to baseline and there were no significant differences between DQS (preservative-free and containing) and SH [36].
The effects of 3% DQS, 0.3% SH, and 2% rebamipide solution were assessed on 15 healthy patients in a prospective comparison study [11]. Rebamipide stimulates mucous secretion on the ocular surface [11]. There was a significant increase in coma, spherical, and total HOAs immediately after instillation of all three drops (3% DQS, 0.3% SH, and 2% rebamipide) when compared to baseline values [11]. Immediately after instillation, SH led to the highest increase in coma, spherical, and total HOAs compared to DQS, rebamipide, and control [11]. However, 5 and 10 min after instillation, there were no significant differences in coma, spherical, or total HOAs among all groups and compared to baseline [11]. There was a significant increase in forward light scatter immediately after rebamipide instillation compared to baseline and compared to DQS and SH [11]. However, 5 and 10 min after instillation, there was again no significant difference in forward scatter among the groups and compared to baseline [11]. The same group assessed the effects of 2% rebamipide on 16 patients with short TBUT type of dry eye in a prospective comparison study [33]. TBUT was significantly increased at the measured 2- and 4-week time points after treatment when compared to baseline [33]. Fluorescein staining and Schirmer test scores were not significantly different at 2 and 4 weeks after treatment [33]. During 10-s recordings of HOAs, there was a significant upward trend at baseline for coma, spherical, and total HOAs [33]. At the 2-week time point, only spherical aberrations had a significant increase in during the 10-s recording period/post-blink change [33]. At 4 weeks, there were no significant changes in coma, spherical, or total HOAs, indicating stability in HOAs [33]. The FI was significantly improved at the 2- and 4-week periods, whereas SI was significantly improved only compared to the 4-week period [33].
Cyclosporine A is a calcineurin inhibitor and potent immunomodulatory agent that inhibits T cell activation and reduces surface inflammation in the context and usage as an eye drop [29]. This group assessed the effects of 3% DQS and 0.05% cyclosporine A (Restasis®) in 40 patients with dry eye after cataract surgery in an RCT [29]. DQS significantly improved TBUT at 1 and 3 months compared to the cyclosporine A group [29]. Schirmer test scores and corneal staining were significantly improved for both treatment groups, but there was no difference between the groups [29]. HOAs were significantly improved with cyclosporine at 2 and 3 months compared to baseline values and significantly better than DQS at 3 months after treatment [29]. Vertical coma was also significantly improved in the cyclosporine A group at 3 months compared to baseline and at both 2 and 3 months when compared to DQS [29]. DQS was more effective at increasing tear secretions and improving TBUT, but cyclosporine A was more effective at improving HOAs [29].
Lifitegrast 5% is a pharmacologic eye drop that inhibits the inflammation associated with dry eye disease by blocking T cell adhesion and migration through inhibition of lymphocyte function-associated antigen 1 (LFA-1) to intercellular adhesion molecule 1 (ICAM-1) binding [27, 40]. Lifitegrast is approved by the US Food and Drug Administration for treating both the signs and symptoms of dry eye disease [27, 40]. One group assessed the effects of 5% lifitegrast solution in 100 patients with dry eyes undergoing cataract surgery in a prospective comparison study [27]. Eyes that were treated with lifitegrast for 28 days had significantly more accurate predicted spherical equivalent refraction for the lens actually implanted [27]. There was also a significant improvement and reduction in HOAs in 65% (44/77) of patients after the first course of treatment and a significant improvement in HOAs in 54% (27/77) of patients after the full course of treatment when compared to baseline values [27]. Corneal staining, TBUT, and conjunctival redness were all significantly improved after treatment with lifitegrast [27]. Standardized patient evaluation of eye dryness questionnaire also revealed a significant improvement in dry eye symptoms after lifitegrast treatment [27].
Punctal plug procedures are another intervention for dry eyes that block the puncta which increases tear fluid accumulation, thus keeping the tear film intact [13]. One group assessed the effect of punctal plugs in eight patients with dry eye after LASIK in a prospective comparison study [30]. Patients with dry eye after 1 month of post-punctal occlusion had significantly improved RMS error values, lower order wavefront errors, defocus, and astigmatism compared to pre-punctal measurements [30]. There was also a significant improvement in the HOAs, spherical, and coma aberrations after punctal plug insertion [30].
One group assessed the effects of lubricating eye drops (Blink Intensive Tears) on 20 patients with dry eyes in a prospective comparison study [32]. The TBUT was significantly lengthened at 10 min after instillation when compared to baseline [32]. Spherical, coma, and HOAs were significantly decreased immediately after instillation of eye drops and were significantly maintained after 10 min [32].
Discussion
As mentioned before, several studies have demonstrated that disruptions in the tear film caused by dry eye increase HOAs compared to normal eyes which results in impaired visual function and optical quality [4, 6–9]. Of the 12 papers directly looking at dry eyes and HOA outcomes, eight have definitively shown that there is a significant difference and increase in HOAs in patients with dry eyes [4, 7, 14–17, 19, 21] and that with increasing dry eye severity, defined as patients with SPK, there is significant increase in HOAs as well [7, 15]. The other five papers had differing results in supporting the association of dry eyes and HOAs. In one paper, although the differences in HOAs between normal and dry eyes were not assessed, TBUT was significantly less in dry eyes compared to normal eyes and total HOAs were decreased after saline drops in both patients with normal and dry eyes [18]. Patients with migraines are reported to have more frequent dry eye disease [20] and this group was able to demonstrate that coma, spherical, and total HOAs were significantly higher in their control group compared to the migraine group [20]. This group specifically excluded patients with actual dry eye disease so as not to overestimate their measured parameters though [20]. The last two case reports by the same group showed an opposite phenomenon where HOAs were increased after blinking in post-punctal plug placement patients and in patients with short TBUT [22, 23]. HOAs tend to increase in normal patients and patients with dry eye post blink due to disruption and changes in the tear film [4, 8, 22, 41]. Before the tear film breaks up, the difference in tear film thickness of the thinner superior and thicker inferior cornea may lead to delayed wavefronts inferiorly and increased coma-like aberrations due to the longer optical path in the inferior tear film compared to the thinner superior tear film [22]. Similarly, punctal occlusion in some cases of mild dry eye may cause visual impairment due to the post-blink movement of excessive tear volume [22].
A significant negative correlation between HOAs and TBUT was also demonstrated, providing further evidence that as TBUT decreases, and consequently dry eye severity increases, HOAs increases [16, 19].
As the tear film and TBUT are crucial factors in dry eye disease and HOAs, tear film issues should be readily attenuated with interventions to improve TBUT or help stimulate lipid and aqueous secretions. Therefore, showing improvements in HOAs after treating dry eyes would help strengthen the relationship of HOAs and dry eye severity. From the 15 papers looking at dry eye interventions and HOA outcomes, 12 have shown improvements in HOAs to varying degrees [24–32, 34–36]. In particular, some papers did reveal improvements in HOAs but only for a short time period immediately after instillation of the intervention [25], or revealed an improvement in total HOAs but an increase in vertical trefoil and horizontal coma aberrations [26]. The variation in results can be a result of many factors, including the variation in patient dry eye severity as well as the type of eye drop and intervention used. The viscosity of eye drops plays an important role in the impact of aberrations and has been shown to impact aberration parameters [26, 33]. The type of intervention used also plays a role as one study was able to show that SH was able to significantly improve TBUT over DQS, but DQS was able to improve HOAs significantly more than SH [28]. Whereas, another study demonstrated that DQS and SH were both able to significantly improve HOAs without any significant difference between the two [36]. Another paper demonstrated that DQS significantly improved TBUT over cyclosporine A, but cyclosporine A was able to significantly improve HOAs over DQS [29]. In addition, DQS did not significantly change HOA outcomes and the group postulated that this may be due to 3% DQS causing excessive secretion of fluid that paradoxically disturbs tear film stability [29]. Related to the viscosity and makeup of the eye drops are the morphological changes and patterns that certain eye drops and artificial tears can produce on the ocular surface, which may be attribute to the variation in clinical success seen [42]. The turnover of tear film components, in particular the lipid components, plays an important role in the effectiveness of eye drops and is an important aspect to consider when utilizing lipid-based eye drop treatments [43].
The variation in dry eye disease in patients also played an important role when looking at HOA outcomes. For instance, in one study that assessed the effects of SH in their dry eye groups, HOAs were not significantly changed after instillation [25] while other studies have shown that SH improved HOAs [32, 44]. The researchers attributed this to their population group having both aqueous tear-deficient and evaporative dry eye with moderate to severe dry eye grading with some cases of SPK [25], compared to the patients with more mild dry eye in previous studies [32, 41].
One of the limitations of our paper includes the possibility that not all primary articles looking into patients with dry eye and HOAs were captured. However, we have tried to overcome these limitations by utilizing a very broad initial search strategy as mentioned in our “Methods” section and curated for relevant papers on the basis of Fig. 1.
Overall, there is evidence to show that an association between dry eyes and HOAs exists and that treating dry eye disease through interventions including eye drops, secretagogues, and punctal plugs can improve HOA outcomes. As dry eye disease is one of the most common ocular disorders and complications from many common laser and refractive surgeries, the clinical implications of improving HOAs are an important area of study. Factors such as patient variation in dry eye disease and severity as well as eye drop type and viscosity are a few of the many areas of study that need to be further elucidated for better clinical application.
Conclusion
On the basis of this systematically approached literature review, dry eyes and HOAs have a clear association with the tear film being one of the most important factors in this relationship between the two. Improvements in HOAs with dry eye treatment interventions such as artificial tears, secretagogues, and punctal plugs provide further evidence on this relationship between dry eyes and HOAs. However, there is still much more work to be done in the realm of clinical application as dry eye interventions vary depending on many factors including patient severity, intervention type, eye drop viscosity, and the mechanism of action of intervention. Therefore, although improving HOAs seems to be a viable clinical approach, further evidence and work are required for improved clinical application and outcomes.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Jess Rhee and Kendrick Co Shih were involved in study design, data collection, data analysis, manuscript writing and editing. Tommy Chung-Yan Chan, Sharon Shu-Wan Chow, Antonio Di Zazzo, Takenori Inomata and Louis Tong were involved in data collection, data analysis, manuscript writing and editing.
Disclosures
The following authors confirm that they have no relevant financial disclosures to declare: Jess Rhee, Tommy Chung-Yan Chan, Sharon Shu-Wan Chow, Antonio Di Zazzo, Takenori Inomata, Kendrick Co Shih, Louis Tong.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
This is a review article and, as such, does not generate new data. The authors agree to make all materials, data and associated protocols promptly available to readers without undue qualifications in material transfer agreements.
References
- 1.Charman WN. Wavefront technology: past, present and future. Cont Lens Anterior Eye. 2005;28:75–92. doi: 10.1016/j.clae.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Suliman A, Rubin A. A review of higher order aberrations of the human eye. Afr Vis Eye Heal. 2019;78:1. doi: 10.4102/aveh.v78i1.501. [DOI] [Google Scholar]
- 3.Inoue Y, Ochi S. Effects of 3% diquafosol sodium ophthalmic solution on higher-order aberrations in patients diagnosed with dry eye after cataract surgery. Clin Ophthalmol. 2017;11:87–93. doi: 10.2147/OPTH.S122542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Montés-Micó R, Cáliz A, Alió JL. Wavefront analysis of higher order aberrations in dry eye patients. J Refract Surg. 2004;20:243–247. doi: 10.3928/1081-597X-20040501-08. [DOI] [PubMed] [Google Scholar]
- 5.Koh S. Irregular astigmatism and higher-order aberrations in eyes with dry eye disease. Invest Ophthalmol Vis Sci. 2018;59:DES36–40. doi: 10.1167/iovs.17-23500. [DOI] [PubMed] [Google Scholar]
- 6.Goto E, Yagi Y, Matsumoto Y, Tsubota K. Impaired functional visual acuity of dry eye patients. Am J Ophthalmol. 2002;133:181–186. doi: 10.1016/S0002-9394(01)01365-4. [DOI] [PubMed] [Google Scholar]
- 7.Kaido M, Matsumoto Y, Shigeno Y, Ishida R, Dogru M, Tsubota K. Corneal fluorescein staining correlates with visual function in dry eye patients. Invest Ophthalmol Vis Sci. 2011;52:9516–9522. doi: 10.1167/iovs.11-8412. [DOI] [PubMed] [Google Scholar]
- 8.Montés-Micó R, Alió JL, Muñoz G, Pérez-Santonja JJ, Charman WN. Postblink changes in total and corneal ocular aberrations. Ophthalmology. 2004;111:758–767. doi: 10.1016/j.ophtha.2003.06.027. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Potvin R, Gong L. A study of the short-term effect of artificial tears on contrast sensitivity in patients with Sjögren’s syndrome. Invest Ophthalmol Vis Sci. 2013;54:7977–7982. doi: 10.1167/iovs.13-11798. [DOI] [PubMed] [Google Scholar]
- 10.Lu N, Lin F, Huang Z, He Q, Han W. Changes of corneal wavefront aberrations in dry eye patients after treatment with artificial lubricant drops. J Ophthalmol. 2016. 10.1155/2016/1342056. [DOI] [PMC free article] [PubMed]
- 11.Koh S, Maeda N, Ikeda C, et al. Effect of instillation of eyedrops for dry eye on optical quality. Invest Ophthalmol Vis Sci. 2013;54:4927–4933. doi: 10.1167/iovs.13-12409. [DOI] [PubMed] [Google Scholar]
- 12.Diaz-Valle D, Arriola-Villalobos P, García-Vidal SE, et al. Effect of lubricating eyedrops on ocular light scattering as a measure of vision quality in patients with dry eye. J Cataract Refract Surg. 2012;38:1192–1197. doi: 10.1016/j.jcrs.2012.02.040. [DOI] [PubMed] [Google Scholar]
- 13.Yellepeddi VK, Sheshala R, McMillan H, Gujral C, Jones D, Raghu Raj Singh T. Punctal plug: a medical device to treat dry eye syndrome and for sustained drug delivery to the eye. Drug Discov Today. 2015;20:884–889. doi: 10.1016/j.drudis.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Shimizu E, Aketa N, Yazu H, et al. Corneal higher-order aberrations in eyes with chronic ocular graft-versus-host disease. Ocul Surf. 2020;18:98–107. doi: 10.1016/j.jtos.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Koh S, Maeda N, Hirohara Y, et al. Serial measurements of higher-order aberrations after blinking in patients with dry eye. Invest Ophthalmol Vis Sci. 2008;49:133–138. doi: 10.1167/iovs.07-0762. [DOI] [PubMed] [Google Scholar]
- 16.Jung HH, Ji YS, Oh HJ, Yoon KC. Higher order aberrations of the corneal surface after laser subepithelial keratomileusis. Korean J Ophthalmol. 2014;28:285–291. doi: 10.3341/kjo.2014.28.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Xu J, Sun X, Chu R, Zhuang H, He JC. Dynamic wavefront aberrations and visual acuity in normal and dry eyes. Clin Exp Optom. 2009;92:267–273. doi: 10.1111/j.1444-0938.2009.00354.x. [DOI] [PubMed] [Google Scholar]
- 18.Lin Y-Y, Carrel H, Wang I-J, Lin P-J, Hu F-R. Effect of tear film break-up on higher order aberrations of the anterior cornea in normal, dry, and post-LASIK eyes. J Refract Surg. 2005;21:S525–S529. doi: 10.3928/1081-597X-20050901-21. [DOI] [PubMed] [Google Scholar]
- 19.Denoyer A, Rabut G, Baudouin C. Tear film aberration dynamics and vision-related quality of life in patients with dry eye disease. Ophthalmology. 2012;119:1811–1818. doi: 10.1016/j.ophtha.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Shetty R, Deshpande K, Jayadev C, et al. The impact of dysfunctional tear films and optical aberrations on chronic migraine. Eye Vis (Lond) 2017;4:4. doi: 10.1186/s40662-017-0070-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deschamps N, Ricaud X, Rabut G, Labbé A, Baudouin C, Denoyer A. The impact of dry eye disease on visual performance while driving. Am J Ophthalmol. 2013;156:184–189.e3. doi: 10.1016/j.ajo.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 22.Koh S, Maeda N, Ninomiya S, et al. Paradoxical increase of visual impairment with punctal occlusion in a patient with mild dry eye. J Cataract Refract Surg. 2006;32:689–691. doi: 10.1016/j.jcrs.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Koh S, Maeda N, Hori Y, et al. Effects of suppression of blinking on quality of vision in borderline cases of evaporative dry eye. Cornea. 2008;27:275–278. doi: 10.1097/ICO.0b013e31815be9c8. [DOI] [PubMed] [Google Scholar]
- 24.McGinnigle S, Eperjesi F, Naroo SA. A preliminary investigation into the effects of ocular lubricants on higher order aberrations in normal and dry eye subjects. Cont Lens Anterior Eye. 2014;37:106–110. doi: 10.1016/j.clae.2013.08.156. [DOI] [PubMed] [Google Scholar]
- 25.Lekhanont K, Chuckpaiwong V, Vongthongsri A, Sangiampornpanit T. Effects of sodium hyaluronate on wavefront aberrations in dry eye patients. Optom Vis Sci Off Publ Am Acad Optom. 2014;91:39–46. doi: 10.1097/OPX.0000000000000101. [DOI] [PubMed] [Google Scholar]
- 26.Yildirim Y, Ozsaygili C, Kucuk B. The short term effect of trehalose and different doses of sodium hyaluronate on anterior corneal aberrations in dry eye patients. Cutan Ocul Toxicol. 2021;40:14–20. doi: 10.1080/15569527.2020.1861001. [DOI] [PubMed] [Google Scholar]
- 27.Hovanesian J, Epitropoulos A, Donnenfeld ED, Holladay JT. The effect of lifitegrast on refractive accuracy and symptoms in dry eye patients undergoing cataract surgery. Clin Ophthalmol. 2020;14:2709–2716. doi: 10.2147/OPTH.S264520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park DH, Chung JK, Seo DR, Lee SJ. Clinical effects and safety of 3% diquafosol ophthalmic solution for patients with dry eye after cataract surgery: a randomized controlled trial. Am J Ophthalmol. 2016;163:122–131.e2. doi: 10.1016/j.ajo.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 29.Lee JH, Song IS, Kim KL, Yoon SY. Effectiveness and optical quality of topical 3.0% diquafosol versus 0.05% cyclosporine A in dry eye patients following cataract surgery. J Ophthalmol. 2016;2016:8150757. doi: 10.1155/2016/8150757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang B, Mirza MA, Qazi MA, Pepose JS. The effect of punctal occlusion on wavefront aberrations in dry eye patients after laser in situ keratomileusis. Am J Ophthalmol. 2004;137:52–61. doi: 10.1016/s0002-9394(03)00903-6. [DOI] [PubMed] [Google Scholar]
- 31.Miháltz K, Faschinger EM, Vécsei-Marlovits PV. Effects of lipid- versus sodium hyaluronate-containing eye drops on optical quality and ocular surface parameters as a function of the meibomian gland dropout rate. Cornea. 2018;37:886–892. doi: 10.1097/ICO.0000000000001523. [DOI] [PubMed] [Google Scholar]
- 32.Montés-Micó R, Cerviño A, Ferrer-Blasco T, García-Lázaro S, Ortí-Navarro S. Optical quality after instillation of eyedrops in dry-eye syndrome. J Cataract Refract Surg. 2010;36:935–940. doi: 10.1016/j.jcrs.2009.12.044. [DOI] [PubMed] [Google Scholar]
- 33.Koh S, Inoue Y, Sugmimoto T, Maeda N, Nishida K. Effect of rebamipide ophthalmic suspension on optical quality in the short break-up time type of dry eye. Cornea. 2013;32:1219–1223. doi: 10.1097/ICO.0b013e318294f97e. [DOI] [PubMed] [Google Scholar]
- 34.Koh S, Maeda N, Ikeda C, et al. Effect of diquafosol ophthalmic solution on the optical quality of the eyes in patients with aqueous-deficient dry eye. Acta Ophthalmol. 2014;92:e671–e675. doi: 10.1111/aos.12443. [DOI] [PubMed] [Google Scholar]
- 35.Kaido M, Uchino M, Kojima T, Dogru M, Tsubota K. Effects of diquafosol tetrasodium administration on visual function in short break-up time dry eye. J Ocul Pharmacol Ther. 2013;29:595–603. doi: 10.1089/jop.2012.0246. [DOI] [PubMed] [Google Scholar]
- 36.Jun I, Choi S, Lee GY, et al. Effects of preservative-free 3% diquafosol in patients with pre-existing dry eye disease after cataract surgery: a randomized clinical trial. Sci Rep. 2019;9:12659. doi: 10.1038/s41598-019-49159-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Su T, Ting P, Chang S, Chen D. Superficial punctate keratitis grading for dry eye screening using deep convolutional neural networks. IEEE Sens J. 2020;20:1672–1678. doi: 10.1109/JSEN.2019.2948576. [DOI] [Google Scholar]
- 38.Koh S, Maeda N, Hirohara Y, et al. Serial measurements of higher-order aberrations after blinking in normal subjects. Invest Ophthalmol Vis Sci. 2006;47:3318–3324. doi: 10.1167/iovs.06-0018. [DOI] [PubMed] [Google Scholar]
- 39.Wang H, Hu H, Zhang Q, et al. Dynamic transcriptomes of human myeloid leukemia cells. Genomics. 2013;102:250–256. doi: 10.1016/j.ygeno.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 40.Nichols KK, Donnenfeld ED, Karpecki PM, et al. Safety and tolerability of lifitegrast ophthalmic solution 5.0%: pooled analysis of five randomized controlled trials in dry eye disease. Eur J Ophthalmol. 2019;29:394–401. doi: 10.1177/1120672118791936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koh S, Maeda N, Kuroda T, et al. Effect of tear film break-up on higher-order aberrations measured with wavefront sensor. Am J Ophthalmol. 2002;134:115–117. doi: 10.1016/S0002-9394(02)01430-7. [DOI] [PubMed] [Google Scholar]
- 42.Napoli PE, Satta GM, Coronella F, Fossarello M. Spectral-domain optical coherence tomography study on dynamic changes of human tears after instillation of artificial tears. Invest Ophthalmol Vis Sci. 2014;55:4533–4540. doi: 10.1167/iovs.14-14666. [DOI] [PubMed] [Google Scholar]
- 43.Napoli PE, Coronella F, Satta GM, Fossarello M. A novel technique of contrast-enhanced optical coherence tomography imaging in evaluation of clearance of lipids in human tears. PLoS ONE. 2014;9:e109843. doi: 10.1371/journal.pone.0109843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Montés-Micó R, Cáliz A, Alió JL. Changes in ocular aberrations after instillation of artificial tears in dry-eye patients. J Cataract Refract Surg. 2004;30:1649–1652. doi: 10.1016/j.jcrs.2004.02.041. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This is a review article and, as such, does not generate new data. The authors agree to make all materials, data and associated protocols promptly available to readers without undue qualifications in material transfer agreements.