Abstract
In addition to concern about physical health consequences of COVID-19, many researchers also note the concerning impact on behavioral health and quality of life due to disruption. The purpose of this paper is to explore pathways of COVID-19 behavioral health and quality of life. We found increased anxiety, depression, and alcohol misuse and that the pandemic exacerbated prior problems. Further community indicators also lead to poorer behavioral health and overall decreased quality of life. The nature of COVID-19 and vast reach of the virus suggests that behavioral health concerns should take a primary role in pandemic recovery.
Subject terms: Risk factors, Signs and symptoms
Introduction
Decreased cases and death rates, along with increased vaccination coverage rates and lifted restrictions, are all markers that the COVID-19 pandemic is nearing the recovery phase of disaster response. While many are looking forward to their new normal or returning to pre-pandemic lifestyle, continued threat, vaccine uncertainties, and strain variation serve as cautionary reminders that the global pandemic is ongoing. Regardless of how long it takes for full recovery, more than a year of heightened fears, loneliness, economic consequences, and grief suggest that behavioral health will have longer term consequences1. In disaster mental health, when the threat has dissipated and individuals move out of survival mode, behavioral health problems become more apparent, and consequently services, such as psychoeducation, therapy and brief treatments, are needed2,3.
Limited research from previous pandemics suggest demographic indicators of poorer mental health, specifically for females, youth, and lower education levels4,5. Pandemic-related resource loss also contributed to mental health problems, including increased work, family, and financial stress coupled with decreased social support4,6,7. Direct exposure to the virus, including being a healthcare worker, being sick, or having sick family members, all had elevated symptomatology8–11. Whether it is a social determinant, exposure to SARs, H1N1, and Ebola help understand that pandemics can result in elevated and long lasting mental health symptoms6,9,12.
Early studies from the COVID-19 pandemic identify similar concerns to past pandemics regarding mental health5,13–15. Age appears to be a predictor of mental health problems—younger adults have more difficulty16–19. However, another study found that persons older than 85 years had worsened mental health, suggesting a potential U-shape distribution20. Female study participants also tend to report higher symptomatology21–23. Financial loss, lack of social interactions, and COVID-19 experiences also contribute to mental health concerns, which is consistent with past pandemics21,23,24. Overall studies point to increased mental health problems; yet there is limited information beyond demographics and COVID-19 disruption on factors that contribute to concerning outcomes.
Substance use
One particular concern is the increase in unhealthy coping mechanisms, such as alcohol misuse. Long-term disasters like the current pandemic place individuals and communities at increased risk for exhausting positive coping skills and turning to negative ones such as alcohol misuse25–27. Numerous studies report increases in stress, anger, anxiety, and depression, resulting in substance abuse and relapse post disaster28–31. For example, data from the National Survey on Drug Use and Health from 2007–2011 indicate that alcohol and marijuana use increased post disaster32, which may have resulted from perceived or real loss of income, loss of confidence in authorities, and loss of one's culture or way of life33. Given these experiences are likely to occur during the pandemic2,34, there is an emergent need to understand the magnitude and impact of these negative factors on alcohol misuse from COVID-19.
Physical health
Adverse physical health conditions (e.g. respiratory problems, headaches, musculoskeletal problems, and somatic complaints) are the most commonly reported symptomology among disaster survivors35,36. A study of Hurricane Ike survivors concluded that 45.1% of the study population exhibited functional impairment in performing essential daily living skills (e.g. maintaining social connectedness and academic and work-related responsibilities), 52.6% reported poor health (e.g. disability), and 74.9% experienced depression37. Similarly, the 2019 novel coronavirus disease (COVID-19) global pandemic is a disaster of unprecedented measure. Individuals have feared for self and family members' well-being, have been socially isolated from family and friends, and have endured interrupted, prolong, and unresolved grief2,38,39. Consequently, behavioral symptoms (e.g. depression, anxiety, and psychological distress) are increasingly prevalent among COVID-19 survivors, and behavioral health symptoms are also underdiagnosed, undertreated, and under researched40.
In addition to having an increased prevalence of behavioral health concerns, COVID-19 survivors have an increased prevalence of comorbid conditions that lead to worsened clinical outcomes41. Empirical evidence supports a bidirectional link between mental health and physical health, thereby increasing the risk of comorbid sequelae for disability, morbidity, and mortality, a frequent cause of emotional distress, and is associated with a diminished quality of life for COVID-19 survivors19,42.
Quality of life
Quality of life and overall well-being are highly attributed resources available and can be a protective factor for mental health. In studies following flu epidemics, those recovering reported decreased quality of life43,44. Recent COVID-19 studies have shown the interconnection of quality of life and mental health problems for recovery45. Liu and colleagues46 found that individuals with prior mental health problems had poorer health-related quality of life and reported more COVID-19-related disturbances. An early study found an increase in positive well-being since COVID-19, but it may have been due to looking at their past rather than future perceptions47. Other studies have shown significant declines in subjective well-being48 and quality of life49. Studies have shown that well-being may be beyond the individuals and influenced more by socio-environmental and community factors, such as GDP, healthcare access, and pandemic communication and response50,51. Quality of life and well-being are important to foster and are of great concern for individuals and for overall community recovery.
In a systematic review of recent studies regarding COVID mental health, common risk factors associated with mental distress during the COVID-19 pandemic include female sex, 40 years of age or younger, presence of mental or physical illnesses, and financial loss or unemployment12. However, only one study included U.S. participants, and more studies are needed to better inform local recovery plans regarding additional protective factors. Behavioral health is important for overall individual well-being, and also plays a role in collective prevention and risk52. The purpose of this paper is to explore pathways of COVID-19 behavioral health and quality of life. We hypothesize behavioral health indicators will have increased from 2019 population estimates and from participant perceived problems prior to COVID-19.
Method
Sample selection for this cross-sectional study included responses from April 7, 2020, through July 26, 2020, and respondents ages 18–65. Electronic recruitment was conducted through Tulane University School of Social Work website and media promotions requesting voluntary participation through a Qualtrics link. Participants gave virtual consent by continuing the online survey and were informed they could skip any questions or stop at any time—there was no compensation for time. Adults (18 years of age or older) and access to the technological platform were the only limiting factors. The SAMHSA national hotline was provided at the end of the survey to connect participants with resources or if they incurred distress. Tulane University Institutional Review Board approved study protocol and were performed in accordance with relevant guidelines and regulations.
Measures
Demographics (age, race, marital status, and income) were collected, along with participants completed dichotomous pre-existing COVID items. Participants were asked if they experienced mental health, physical health, or alcohol problems prior to the COVID-19 pandemic. In addition, valid measures of behavioral health, quality of life, and COVID impact were used.
Behavioral health
Behavioral health was assessed by anxiety, depression and alcohol misuse. Anxiety was measured by the General Anxiety Disorder 2 item scale, which asks in the past 30 days, were participants bothered by 1) feeling nervous, anxious, or on edge; and 2) not being able to stop or control worrying53. The GAD2 cut point was 3 and 53% met the cut-off (M = 4.9, SD = 1.9; α = 0.88). Depression was measured with the 2-item Patient Health Questionnaire, which asks if, in the past 30 days, participants were bothered by 1) little interest or pleasure in doing things and 2) feeling down, depressed, or hopeless54. The PHQ2 cut point was 3 and 28% met the cut-off (M = 3.9, SD = 1.7; α = 0.86. Alcohol misuse was measured by the CAGE, which asks participants if, in the past 30 days, they have: 1) felt you should Cut down on drinking; 2) been Annoyed when people have commented on drinking; 3) felt Guilty or badly about your drinking; 3) had an Eye opener first thing in the morning to steady your nerves or get rid of a hangover55. The CAGE cut point was 1 and 14% met the cut-off; (M = 0.4, SD = 0.9; κ = 0.66.
Quality of life
Overall quality of life was measured with items selected from the World Health Organization WHOQOL-BREF quality of life assessment56. Participants were asked how good or satisfied they have felt over the last 2 weeks with their: quality of life, health, sleep, performance of daily living activities, capacity for work, conditions of your living place, and access to health services (M = 25.1, SD = 4.9; α = 0.74).
COVID-19
Impact was assessed through COVID experiences and COVID disruption. Participants were asked to respond to whether they had experienced the following as a result of COVID 19: loss of usual way of life, social isolation, work from home, children and adolescents being out of school, loss of income or revenue, personal health effects, participated in response or emergency services, and COVID-19 suspected or diagnosed, loss of job or business, COVID-19 diagnosis. A COVID experience index was created where 1 point was given for experiences listed. Items for the COVID disruption were adapted from the Sheena Disability Scales57. Participants were also asked to what degree the pandemic had disrupted their work/school life, social/leisure activities, and family/home responsibilities activities (M = 11.6, SD = 2.4; α = 0.61).
Community behavioral health
County-level data was accessed from the Robert Wood Johnson Better Health Data58. Data were matched to participants’ zip codes and included: percentage of excessive drinking, average number of mentally unhealthy days, and average number of physically unhealthy days. County-level COVID death and diagnosis rates through October 2020 were also accessed from the Center for Disease Control COVID Data Tracker59.
Participants
The participants (N = 296) represented many states, including Louisiana (55%), Texas (6%), California (5%), Florida (3%), Georgia (3%), Illinois (3%); 2% percent from Mississippi, Pennsylvania, Virginia, North Carolina, and Massachusetts; and 1% from New Jersey, New York, Arizona, Iowa, Maryland, Michigan, Missouri, Connecticut, South Carolina, Kentucky, Ohio, Minnesota, Oregon, Washington; and less than 1% (0.3%) representation from Rhode Island, Delaware, Alabama, Tennessee, Indiana, Wisconsin, Nebraska, Colorado, Wyoming, Alaska.
The minimum age was 19 and the maximum was 65 (M = 43.6, SD = 12.5); 85% identified as women, 14% as men, and 1% as nonbinary. Participants were allowed to select multiple racial/ethnic identities, the majority identified as White (86%); 8% identified Black or African American, 6% were Latinx, Latin@ or Hispanic, 3% identified as Asian, and 1% identified as Native American or Alaskan Native. The median 2019 income was $60,000– $69,999. All participants had at least a high school education (18%) and 72% had a 4-year or professional degree, 10% had a doctorate. The majority of participants (65%) were married or cohabitating; 26% were single, 8% were divorced or separated, and 1% were widowed.
Data analysis
Data analyses were conducted using Statistical Package for the Social Sciences (SPSS) version 27. Point biserial correlations were conducted among COVID-19 experiences and behavioral health variables. McNamara Chi square analyses were conducted to compare current cut-off scores (meeting cutoff for either anxiety or depression) or alcohol misuse cutoff with previous mental health and substance use problems. One sample Z tests were used to compare participant cut-off scores (anxiety, depression, and alcohol misuse) with 2019 population estimates. Zero order (Pearson product moment) correlations were conducted to assess associations among variables. The structural model was tested using SPSS analysis of moment structure (AMOS) version 27. Assumptions of normality and linearity were met; missing data was less than 5% and imputed using linear interpolation. Significant zero-order correlation paths were added to the model but did not reveal good fit (RMSE > 0.05). After reviewing regression weights, the dichotomized married versus nonmarried and minority versus nonminority were removed due to their lack of contribution to the model.
Results
Prior behavioral health concerns were asked and 30% noted physical (n = 88) health problems, 29% mental health problems, and 4% substance use problems. Results suggest an increase in current mental health concerns (33%), compared to preexisting problems (25%), Χ2 (1) = 37.61, p < 0.001. Current alcohol use (12%) was also increased over previous substance use (2%), Χ2 (1) = 16.42, p < 0.001. Increased levels of anxiety 53% compared to 16% for 2019 population estimates 60, Z (296) = 17.4, p < 0.001. Increased levels of depression 28% for moderate compared to 19% for the population estimates61, Z (296) = 4.4, p < 0.001. Alcohol misuse (14%) was also increased compared to 2019 population estimates (6%) of heavy alcohol use62, Z (296) = 5.6, p < 0.001.
Participants were asked to report on COVID-19 experiences. Over one third of respondents reported COVID-19 experiences as social isolation, working from home, loss of income, and children and adolescents being out of school (see Table 1). Participants noting social isolation and personal health effects had higher anxiety and depression and lower quality of life. Participants with suspected or diagnosed COVID-19 reported more alcohol misuse and lower quality of life (see Table 1).
Table 1.
Frequency, Percentages and Correlation Coefficients on COVID-19 Experiences.
| Frequency | Percent | Point biserial Correlation Coefficients | ||||
|---|---|---|---|---|---|---|
| Anxiety | Depression | Alcohol Misuse | Quality of Life | |||
| Social isolation | 219 | 74% | .21** | .26** | −.10 | −.22** |
| Work from home | 181 | 61% | .09 | .05 | .09 | −.01 |
| Children and adolescents being out of school | 104 | 35% | −.02 | −.03 | .04 | −.02 |
| Loss of income | 103 | 35% | .06 | .05 | −.01 | −.13* |
| Personal health effects | 42 | 14% | .26** | .23** | .07 | −.33** |
| Participated in response or emergency services | 46 | 15% | .03 | −.03 | .07 | −.01 |
| COVID-19 suspected or diagnosed | 32 | 11% | .01 | .04 | .15* | −.12* |
Significant values are in bold.
Zero order correlations are presented in Table 2. COVID-19 experiences and disruption were associated with increases in anxiety and depression and decreased quality of life. Younger participants reported more COVID-19 experiences and prior mental health concerns. Anxiety and depression were positively associated, and both were negatively associated with quality of life, suggesting that as depression and anxiety increase, quality of life decreases. Current anxiety and depressive symptoms were associated with prior physical and mental health problems. Females and whites reported more anxiety, while higher income was associated with higher quality of life scores. Respondents with higher anxiety scores lived in communities with a higher number of physically unhealthy days.
Table 2.
Zero Order Coefficients and Descriptive Statistics.
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Anxiety | 4.9 | 1.9 | 1 | ||||||||||||||||
| 2 | Depression | 3.9 | 1.7 | .62** | 1 | |||||||||||||||
| 3 | Alcohol misuse | 0.4 | 0.9 | .04 | .12* | 1 | ||||||||||||||
| 4 | Quality of life | 25.1 | 4.9 | −.38** | −.45** | −.05 | 1 | |||||||||||||
| 5 | % Excessive Drinking | 20.4 | 2.2 | .07 | .01 | .08 | −.01 | 1 | ||||||||||||
| 6 |
# Mentally Unhealthy Days |
4.4 | 0.6 | .13* | .06 | .06 | −.04 | .20** | 1 | |||||||||||
| 7 |
# Physically Unhealthy Days |
4.1 | 0.6 | .12* | .09 | .04 | −.03 | .15* | .94** | 1 | ||||||||||
| 8 | Age | 43.6 | 12.6 | −.09 | −.09 | −.08 | .04 | −.01 | −.104 | −.14* | 1 | |||||||||
| 9 | 2019 income | 7.2 | 3.6 | −.05 | −.14* | −.07 | .21** | −.01 | −.21** | −.24** | .43** | 1 | ||||||||
| 10 | Minority | 0.8 | 0.4 | .13* | −.01 | −.09 | −.01 | .08 | −.01 | −.02 | .18** | .14* | 1 | |||||||
| 11 | Gender | 0.9 | 0.4 | .18** | .10 | −.01 | −.04 | −.02 | −.01 | −.01 | −.01 | −.02 | .17** | 1 | ||||||
| 12 | Married | 0.7 | 0.5 | −.05 | −.08 | .05 | .09 | .01 | −.03 | −.05 | .32** | .34** | .08 | −.01 | 1 | |||||
| 13 | Pre physical health problems | 0.3 | 0.5 | .14* | .12* | −.17** | −.16** | −.13* | .01 | −.01 | .16** | .08 | .01 | .04 | −.01 | 1 | ||||
| 14 |
Pre Mental health problems |
0.3 | 0.5 | .30** | .31** | .02 | −.25** | .08 | .03 | .08 | −.37** | −.25** | .04 | .02 | −.11* | .07 | 1 | |||
| 15 |
Pre alcohol problems |
0.0 | 0.2 | .01 | .09 | .29** | −.03 | .01 | −.04 | −.04 | −.11 | .01 | −.11 | −.11 | −.17** | .02 | .21** | 1 | ||
| 16 | COVID-19 rate | 12,201.3 | 5041.7 | .01 | .05 | .17** | −.03 | .21** | .36** | .24** | −.04 | −.08 | −.09 | −.05 | −.01 | −.08 | −.01 | −.02 | 1 | |
| 17 |
COVID-19 experiences |
2.5 | 1.2 | .22** | .19** | .09 | −.27** | .04 | −.02 | −.02 | −.11* | −.02 | −.01 | .06 | .08 | .05 | .22** | .02 | .03 | 1 |
| 18 | COVID-19 disruption | 11.6 | 2.4 | .31** | .28** | .02 | −.29** | −.01 | −.01 | −.04 | −.01 | −.07 | .04 | .01 | .05 | −.09 | .03 | −.02 | .01 | .40** |
Significant values are in bold.
*p < .05, **p < .001.
Respondents who reported prior physical health problems were older, had more alcohol misuse, had decreased quality of life, and were less likely to live in communities with excessive drinking. Respondents who reported prior mental health problems had lower quality of life, lower incomes, and were younger. As current alcohol misuse increased, depression increased, and respondents also tended to live in communities with higher COVID-19 rates. Individuals reporting prior substance use problems had higher alcohol misuse scores, were less likely to be married, and reported prior mental health problems. Communities with more physically unhealthy days also had increased percentages of excessive drinking. Respondents who were older lived in communities with higher numbers of physically unhealthy days. Respondents with lower 2019 income reported higher depression. They were more likely to live in communities with more physically and mentally unhealthy days. Communities with higher COVID-19 rates also had higher averages of mentally and physically unhealthy days and percentages of excessive drinking.
Structural model
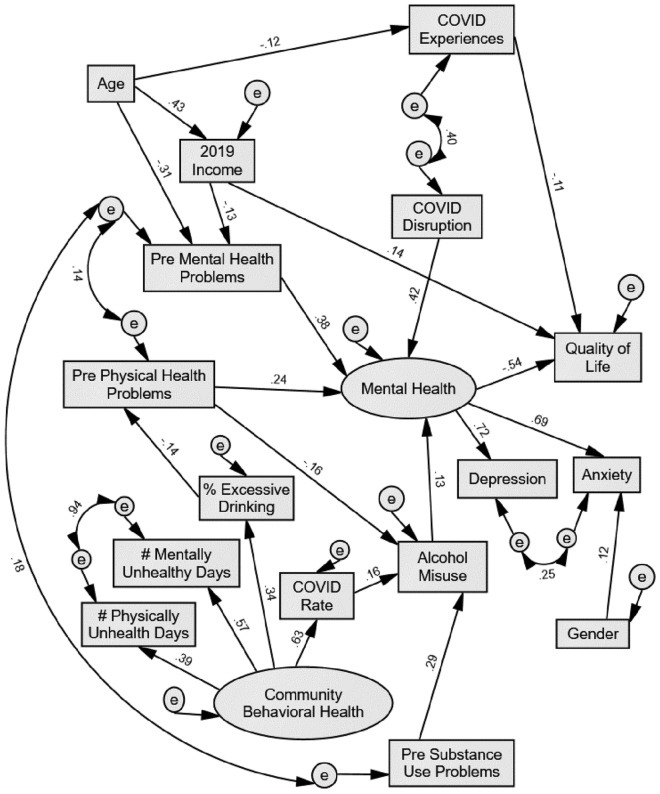
The final model was acceptable given the smaller sample size and use of dichotomous pre COVID-19 behavioral health variables, χ2 (93) = 123.7, p = 0.018, CFI = 0.976, RMSEA = 0.033 (lower 0.15, upper 0.48); PNFI of 0.623, suggests the overall model accounts for approximately 62% of the variance in behavioral health and quality of life. Table 3 presents the path coefficients and model estimates. The largest contributors to the model are as follows: mental (β = 0.39, p < 0.001) and physical health (β = 0.24, p < 0.001) problems prior to COVID-19 were predictive of current mental health (latent variable including anxiety and depression). Mental health was predictive of quality of life (β = -0.55, p < 0.001). Younger age was predictive of prior mental health problems (β = -0.31, p < 0.001). Prior substance use problems were predictive of current alcohol misuse (β = 0.29, p < 0.001) and COVID-19 disruption was predictive of mental health (β = 0.42, p < 0.001). Figure 1 presents the final model, where significant standardized estimates are shown next to each path, and the coefficient for each variable’s contribution to the model is also included.
Table 3.
Path Coefficients.
| Estimate | SE | CR | p | Standardized Estimates | |||
|---|---|---|---|---|---|---|---|
| % Excessive Drinking | ← | Community behavioral health | 3.47 | 1.14 | 3.04 | .002 | 0.34 |
| Pre physical health problems | ← | % Excessive Drinking | −0.03 | 0.01 | −2.50 | .012 | −0.14 |
| Income | ← | Age | 0.12 | 0.02 | 8.10 | *** | 0.43 |
| COVID-19 rate | ← | Community behavioral health | 14,612.88 | 4837.86 | 3.02 | .003 | 0.63 |
| Pre Mental health problems | ← | Income | −0.02 | 0.01 | −2.13 | .033 | −0.13 |
| Pre Mental health problems | ← | Age | −0.01 | 0.00 | −5.30 | *** | −0.31 |
| Alcohol misuse | ← | Pre substance use problems | 1.29 | 0.24 | 5.40 | *** | 0.29 |
| Alcohol misuse | ← | Pre physical health problems | −0.30 | 0.10 | −2.91 | .004 | −0.16 |
| Alcohol misuse | ← | COVID-19 rate | 0.00 | 0.00 | 2.92 | .003 | 0.16 |
| Mental Health | ← | Pre physical health problems | 0.70 | 0.18 | 3.83 | *** | 0.24 |
| COVID-19 Experience | ← | Age | −0.01 | 0.01 | −2.18 | .029 | −0.12 |
| Mental Health | ← | COVID-19 disruption | 0.23 | 0.04 | 6.41 | *** | 0.42 |
| Mental Health | ← | Pre Mental health problems | 1.12 | 0.19 | 5.87 | *** | 0.39 |
| Mental Health | ← | Alcohol misuse | 0.19 | 0.09 | 2.04 | .041 | 0.13 |
| Quality of Life | ← | COVID-19 Experiences | −0.46 | 0.21 | −2.21 | .027 | −0.11 |
| Quality of Life | ← | Mental Health | −2.02 | 0.33 | −6.04 | *** | −0.55 |
| # Physically Unhealthy Days | ← | Community behavioral health | 1.00 | 0.39 | |||
| # Mentally Unhealthy Days | ← | Community behavioral health | 1.49 | 0.14 | 10.62 | *** | 0.57 |
| Anxiety | ← | Gender | 0.64 | 0.24 | 2.72 | .007 | 0.12 |
| Anxiety | ← | Mental Health | 1.00 | 0.69 | |||
| Quality of Life | ← | Income | 0.19 | 0.07 | 2.81 | .005 | 0.14 |
| Depression | ← | Mental Health | 0.94 | 0.09 | 10.31 | *** | 0.72 |
***p < .001.
Figure 1.
COVID-19 Behavioral Health Model.
Discussion
Increased anxiety during a pandemic has led to preventative behaviors, such as increased handwashing and following safety restrictions, demonstrating a protective factor of mild anxiety52. However, ongoing stressors become cumulative and can lead to longer-term mental health problems64. Biological disasters like the COVID-19 pandemic create a large amount of disruption, uncertainty, and public fear—globally impacting communities for over a year. There is a significant gap in the literature regarding behavioral health and quality of life during global pandemics. Overall results of this study suggest complex pathways to COVID-19 behavioral health and subsequent quality of life.
Behavioral health
The current study revealed that COVID-19 disruption to participants’ work, family, or social life uniquely contributed to poorer mental health. Specifically, participants noting social isolation and personal health effects exhibited worsened mental health. These findings are in line with existing research on pandemic contributors to mental health concerns, including loneliness1 and direct exposure10. As one study noted, increased experiences of COVID-19 at the height of the pandemic produced occurrences of psychological distress that created or increased mental illness in China64. Our study found that COVID-19 experiences likely exacerbated existing problems, where prior mental and physical health were predictive of current anxious and depressive symptoms. Similarly, Young and colleagues65 found those who experienced mental health symptoms in the past were at an increased risk for severe mental health diagnoses. Further, early studies and our results support the growing literature of concerns for longer-term mental health problems due to COVID-1917.
In a systematic review of recent literature surrounding COVID-19 Xiong and colleagues12, found that increases in depression, anxiety, and PTSD symptoms were associated with certain risk factors. Similarly, our study found indirect pathways to mental health, where younger participants reported prior mental health problems and older participants reported prior physical health problems. In the current study, younger participants also had more indirect stressors associated with the pandemic16 and reported more COVID-19 experiences. Females and whites reported more anxiety, although this association did not hold in the structural model. Similar results have been found in other studies regarding females20, but the opposite regarding race and ethnicity22,66. Discrepancies are likely due to the significant association among older participants identifying as members of a minority grouping.
Another contributor to poor behavioral health is substance use. Early COVID-19 studies estimate over 10% started or increased substance misuse as a coping mechanism67. Our study supports the increase of substance due to COVID-19, where current alcohol misuse was associated with prior substance use. Further, prior substance use was associated with prior mental health problems; this connection was continued for current usage, where alcohol misuse was also associated with depression. Following the Ebola outbreak, one risk factor identified was increased substance use, which can exacerbate negative mental health outcomes68. In the current study, participants with suspected or diagnosed COVID-19 or who lived in communities with higher rates reported higher alcohol misuse, suggesting use of alcohol as a potential negative coping mechanism.
Quality of life
Most would expect quality of life to be challenged during a global pandemic; however, when we assessed behavioral health as a component of overall quality of life, longer term outcomes became concerning. Both past and current mental health were strong predictors of quality of life. Other studies have demonstrated this connection for individuals recovering from COVID-1945,46,69. COVID-19 experiences play a large role in quality of life, where participants who felt socially isolated reported personal health effects, or COVID-19 suspected or diagnosed participants reported lower quality of life. Similar to a large international study by Alzueta and colleagues13, the number of experiences related to COVID-19 played a role in overall well-being. Specifically, we found that increased COVID-19 experiences predicted lower quality of life, demonstrating an allostatic load effect and the accumulation of pandemic-related stressors toward negative health outcomes63. Individuals who do not adapt well to taxing life events tended to experience increased rates of anxiety and depression, which lowers quality of life.
Place matters
Place matters with regards to COVID-19, where behavioral health and community factors contributed to overall health. A community consists of individuals one can identify with. Specifically, the community is place-based or labeled as a locality where individuals who comprise the community interact to share social capital. The social capital theory contends that social connectedness is a resource that guides the growth and accumulation of interpersonal relationships70. Community-based findings from this study found that participants with higher anxiety scores and who were older lived in communities with more physically unhealthy days. Respondents with lower 2019 income were less likely to live in communities with more physically and mentally unhealthy days. Respondents who reported prior physical health were less likely to live in communities with excessive drinking. Yet communities with overall poorer health also had increased percentages of excessive drinking. Communities with higher COVID-19 rates also had higher averages of mentally and physically unhealthy days and percentages of excessive drinking. Similar results demonstrated that higher individual and community stressors result in poor mental health and inadvertently decrease quality of life12,71,72. Communities' social capital works as a protective factor against the accumulative effects of COVID-19 (e.g. social isolation, depression, psychological distress, and deaths)73,74.
Limitations and future research
Future studies are needed to understand protective factors (e.g. self-care, technology-aided connectedness) that can buffer more negative effects. Researchers from Turkey observed a reduction in COVID-19 anxiety and depression symptomology following physical activity programs to increase optimal health functioning, social connectedness, decreased anxiety and depression symptoms75. Similar programs and studies are needed to understand buffering effects on U.S. populations. Respondents were largely female (85%) and while consistent with existing studies that more females respond to surveys76, this may impact results. Timing is a major consideration for this study, as behavioral health needs and concerns are likely to change over the course of the pandemic2. Future studies are also needed to understand longer term behavioral health implications, social media effects, and family impacts, including parenting, adult caregiving, and youth77.
Summary and impact
The nature of COVID-19 and vast reach of the virus suggest that behavioral health concerns should take a primary role in pandemic recovery. While we can expect many individuals with elevated symptoms or substance use problems to remit over time, the ongoing nature of the current pandemic is likely to yield longer-term reactions5,6,78,79. The continued direct and indirect effects of the pandemic alludes to the pandemic hindering improvements in people’s health and overall well-being. This study supports the urgent need for enhanced behavioral health service capacity moving into the recovery phase of the pandemic80. Based on past disasters, brief services such as Skills for Psychological Recovery81 are still needed to normalize mental health symptoms and awareness of risk factors and acknowledge problematic coping, such as alcohol use. Brief interventions may be necessary to boost coping skills that may be diminished due to COVID-19. At this point in the disaster, more intensive treatments should also be made available82, especially for those who exhibit specific risk factors, such as young and middle-aged adults, those with limited income and prior behavioral health concerns, and those living in communities with poorer health. Perhaps some of the gains made toward telehealth over the past year83 can continue and increase access and capacity to support improved behavioral health and quality of life.
Author contributions
T.C.H., L.Y.S., and P.S.B. designed the study. All authors contributed to the writing of the main manuscript. T.C.H. conducted analyses and prepared tables and figures; L.Y.S. reviewed analyses.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Saltzman LY, Hansel TC, Bordnick PS. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol. Trauma Theory Res. Pract. Policy. 2020;1:1. doi: 10.1037/tra0000703. [DOI] [PubMed] [Google Scholar]
- 2.Hansel TC, Saltzman LY, Bordnick PS. Behavioral health and response for COVID-19. Disaster Med. Public Health Prepared. 2020;1:1–23. doi: 10.1017/dmp.2020.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Titov N, Staples L, Kayrouz R, Cross S, Karin E, Ryan K, Dear B, Nielssen O. Rapid report: Early demand, profiles and concerns of mental health users during the coronavirus (COVID-19) pandemic. Internet Interv. 2020;21:100327. doi: 10.1016/j.invent.2020.100327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lau JT, Yang X, Pang E, Tsui HY, Wong E, Wing YK. SARS-related perceptions in Hong Kong. Emerg. Infect. Dis. 2005;11(3):417. doi: 10.3201/eid1103.040675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, Kontopantelis E, Webb R, Wessely S, McManus S, Abel KM. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sprange G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7:105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- 8.Luyt CE, Combes A, Becquemin MH, Beigelman-Aubry C, Hatem S, Brun AL, Zraik N, Carrat F, Grenier PA, Richard JCM, Mercat A. Long-term outcomes of pandemic 2009 influenza A(H1N1)- associated severe ARDS. Chest. 2012;142(3):583–592. doi: 10.1378/chest.11-2196. [DOI] [PubMed] [Google Scholar]
- 9.Wing Chit Mak I, Chu CM, Pan PC, Chung Yiu MG, Ho SC, Chan VL. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen. Hosp. Psychiatry. 2010;32:590–598. doi: 10.1016/j.genhosppsych.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerg. Infect. Disease. 2005;11(8):1297–1300. doi: 10.3201/eid1108.041083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu J, Zheng Y, Wang M, Zhao J, Zhan Q, Fu M, Wang Q, Xiao J, Cheng Y. Predictors of symptoms of posttraumatic stress in Chinese university students during the 2009 H1N1 influenza pandemic. Med. Sci. Monit. 2011;17(7):60–64. doi: 10.12659/MSM.881836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alzueta E, Perrin P, Baker F, Caffarra S, Ramos-Usuga D, Yuksel D, Arango-Lasprilla J. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. J. Clin. Psychol. 2021;77(3):556–570. doi: 10.1002/jclp.23082. [DOI] [PubMed] [Google Scholar]
- 14.Robillard R, Daros AR, Phillips JL, Porteous M, Saad M, Pennestri M-H, Kendzerska T, Edwards JD, Solomonova E, Bhatla R, Godbout R, Kaminsky Z, Boafo A, Quilty LC. Emerging new psychiatric symptoms and the worsening of pre-existing mental disorders during the COVID-19 pandemic: A Canadian multisite study. Can. J. Psychiat. 2021;1:1. doi: 10.1177/0706743720986786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, Di Marco A, Rossi A, Siracusano A, Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psych. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elezi F, Tafani G, Sotiri E, Agaj H, Kola K. Assessment of anxiety and depression symptoms in the Albanian general population during the outbreak of COVID-19 pandemic. Indian J. Psychiatry. 2020;62(Suppl 3):S470. doi: 10.4103/psychiatry.IndianJPsychiatry_842_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Minahan J, Falzarano F, Yazdani N, Siedlecki K. The COVID-19 pandemic and psychosocial outcomes across age through the stress and coping framework. Gerontologist. 2020;61(2):228–239. doi: 10.1093/geront/gnaa205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reading TM, Grossman L, Myers A, Pathak J, Creber R. Correlates of mental health symptoms among US adults during COVID-19, March–April 2020. Public Health Rep. 2021;136(1):97–106. doi: 10.1177/0033354920970179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE. 2020;15(12):e0244630. doi: 10.1371/journal.pone.0244630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cigiloglu A, Ozturk Z, Efendioglu E. How have older adults reacted to coronavirus disease 2019? Psychogeriatrics. 2021;21(1):112–117. doi: 10.1111/psyg.12639. [DOI] [PubMed] [Google Scholar]
- 21.Hyland P, Shevlin M, McBride O, Murphy J, Karatzias T, Bentall R, Martinez A, Vallières F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020;142(3):249–256. doi: 10.1111/acps.13219. [DOI] [PubMed] [Google Scholar]
- 22.Kujawa A, Green H, Compas B, Dickey L, Pegg S. Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depress. Anxiety. 2020;37(12):1280–1288. doi: 10.1002/da.23109. [DOI] [PubMed] [Google Scholar]
- 23.Lahav Y. Psychological distress related to COVID-19 – The contribution of continuous traumatic stress. J. Affect. Disord. 2020;277:129–137. doi: 10.1016/j.jad.2020.07.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Griffiths D, Sheehan L, van Vreden C, Petrie D, Grant G, Whiteford P, Sim MR, Collie A. The impact of work loss on mental and physical health during the COVID-19 pandemic: Baseline findings from a prospective cohort study. J. Occup. Rehabil. 2021;1:1–8. doi: 10.1007/s10926-021-09958-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorder in systematically studied survivors of 10 disasters. Arch. Gen. Psychiatry. 2011;68(2):173–180. doi: 10.1001/archgenpsychiatry.2010.131. [DOI] [PubMed] [Google Scholar]
- 26.Sinha R, Fox HC, Hong KA, Hansen J, Tuit K, Kreek MJ. Effects of adrenal sensitivity, stress- and cue-induced craving, and anxiety on subsequent alcohol relapse and treatment outcomes. Arch. Gen. Psychiatry. 2011;68(9):942–952. doi: 10.1001/archgenpsychiatry.2011.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Brown BL, Kopak AM, Hinkel HM. A critical review examining substance use during the disaster life cycle. Disast. Prevent. Manag. 2019;28(2):171–182. [Google Scholar]
- 28.Fergusson DM, Hormwood J, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. J. Am. Medical Assoc. Psychiatry. 2014;71(9):1025–1031. doi: 10.1001/jamapsychiatry.2014.652. [DOI] [PubMed] [Google Scholar]
- 29.Pfefferbaum B, Doughty DE. Increased alcohol use in a treatment sample of Oklahoma City bombing victims. Psychiatry. 2001;64(40):296–303. doi: 10.1521/psyc.64.4.296.18598. [DOI] [PubMed] [Google Scholar]
- 30.Vetter S, Rossegger A, Rossler W, Bisson JI, Endrass J. Exposure to the tsunami disaster, PTSD symptoms and increased substance abuse – an Internet based survey of male and female residents of Switzerland. BMC Public Health. 2008;8(92):1–6. doi: 10.1186/1471-2458-8-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vlahov D, Galea S, Ahern J, Resinck H, Boscarino JA, Gold J, Bucivalas M, Kilpatrick D. Consumption of cigarettes, alcohol and marijuana among New York residents six months after September 11 terrorist attacks. Am. J. Drug Alcohol Abuse. 2004;30(2):385–407. doi: 10.1081/ada-120037384. [DOI] [PubMed] [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration, & Centers for Disease Control and Prevention. (2013). Behavioral Health in the Gulf Coast Region Following the Deepwater Horizon Oil Spill, HHS Publication No. (SMA) 13–4737.
- 33.Gould DW, Teich JL, Pemberton MR, Pierannunzi C, Larson S. Behavioral health in the Gulf Coast region following the Deepwater Horizon oil spill: Findings from two federal surveys. J. Behav. Health Serv. Res. 2015;42(1):6–22. doi: 10.1007/s11414-014-9441-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stein JY, Tuval-Mashiach R. Loneliness and isolation in life-stories of Israeli veterans of combat and captivity. Psychol. Trauma Theory Res. Pract. Policy. 2015;7(2):122. doi: 10.1037/a0036936. [DOI] [PubMed] [Google Scholar]
- 35.Karaye IM, Ross AD, Perez-Patron M, Thompson C, Taylor N, Horney JA. Factors associated with self-reported mental health of residents exposed to Hurricane Harvey. Progress Disast. Sci. 2019;2:100016. doi: 10.1016/j.pdisas.2019.100016. [DOI] [Google Scholar]
- 36.Osofsky HJ, Hansel TC, Osofsky JD, Speier A. Factors contributing to mental and physical health care in a disaster-prone environment. Behav. Med. 2015;41(3):131–137. doi: 10.1080/08964289.2015.1032201. [DOI] [PubMed] [Google Scholar]
- 37.Lowe SR, Joshi S, Pietrzak RH, Galea S, Cerdá M. Mental health and general wellness in the aftermath of Hurricane Ike. Soc. Sci. Med. 2015;124:162–170. doi: 10.1016/j.socscimed.2014.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern. Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 39.Raker EJ, Zacher M, Lowe SR. Lessons from Hurricane Katrina for predicting the indirect health consequences of the COVID-19 pandemic. Proc. Natl. Acad. Sci. 2020;117(23):12595–12597. doi: 10.1073/pnas.2006706117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo Q, Zheng Y, Shi J, Wang J, Li G, Li C, Yang Z. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Egede J, Campbell JA, Walker RJ, Garacci E, Dawson AZ, Egede LE. Relationship between physical and mental health comorbidities and COVID-19 positivity, hospitalization, and mortality. J. Affect. Disord. 2021;283:94–100. doi: 10.1016/j.jad.2021.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fragaszy EB, Warren-Gash C, White PJ, Zambon M, Edmunds WJ, Nguyen-Van-Tam JS, Hayward AC. Effects of seasonal and pandemic influenza on health-related quality of life, work and school absence in England: Results from the Flu Watch cohort study. Influenza Other Respirat. Viruses. 2018;12(1):171–182. doi: 10.1111/irv.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van Hoek AJ, Underwood A, Jit M, Miller E, Edmunds WJ. The impact of pandemic influenza H1N1 on health-related quality of life: A prospective population-based study. PLoS ONE. 2011;6(3):17030. doi: 10.1371/journal.pone.0017030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma YF, Li W, Deng HB, Wang L, Wang Y, Wang PH, Xiang YT. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020;275:145–148. doi: 10.1016/j.jad.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu CH, Stevens C, Conrad RC, Hahm HC. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among US young adults with suspected and reported psychiatric diagnoses. Psychiatry Res. 2020;292:113345. doi: 10.1016/j.psychres.2020.113345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O'Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL, O'Carroll RE, O'Connor DB, Platt S, Scowcroft E, Watson B. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2021;218(6):326–333. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zacher H, Rudolph CW. Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. Am. Psychol. 2020;76(1):50–62. doi: 10.1037/amp0000702. [DOI] [PubMed] [Google Scholar]
- 49.Ping W, Zheng J, Niu X, Guo C, Zhang J, Yang H, Shi Y. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS ONE. 2020;15(6):e0234850. doi: 10.1371/journal.pone.0234850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Blanton RE, Mock NB, Hiruy HN, Schieffelin JS, Doumbia S, Happi C, Samuels R, Oberhelman RA. African resources and the promise of resilience against COVID-19. Am. J. Trop. Med. Hyg. 2020;103(2):539–541. doi: 10.4269/ajtmh.20-0470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fernández-Prados JS, Lozano-Díaz A, Muyor-Rodríguez J. Factors explaining social resilience against COVID-19: The case of Spain. Eur. Soc. 2020;1:1–11. [Google Scholar]
- 52.Betancourt, T. S., Brennan, R. T., Vinck, P., VanderWeele, T. J., Spencer-Walters, D., Jeong, J., Akinsulure-Smith, A. M., & Pham, P. Associations between mental health and Ebola-related health behaviors: A regionally representative cross-sectional survey in Post-conflict Sierra Leone. 9; 13(8):e1002073 (2016). 10.1371/journal.pmed.1002073 [DOI] [PMC free article] [PubMed]
- 53.Sapra A, Bhandari P, Sharma S, Chanpura T, Lopp L. Using generalized anxiety disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020;12(5):e8224. doi: 10.7759/cureus.8224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: Validity of a two-item depression screener. Med. Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 55.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am. J. Med. 1987;82(2):231–235. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- 56.Whoqol Group Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 1998;28(3):551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 57.Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. Int. Clin. Psychopharmacol. 1996;11:89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- 58.Robert Wood Johnson Foundation. Better health data (2018). https://www.rwjf.org/en/library/collections/better-data-for-better-health.html
- 59.Centers for Disease Control and Prevention. Coronavirus disease 2019 data tracker (2020). https://covid.cdc.gov/covid-data-tracker/#mobility.
- 60.Terlizzi, E.P., & Villarroel, M.A. Symptoms of generalized anxiety disorder among adults: United States, 2019. NCHS Data Brief, no 378. National Center for Health Statistics (2020). https://www.cdc.gov/nchs/products/databriefs/db378.htm [PubMed]
- 61.Villarroel, M.A., & Terlizzi, E.P. Symptoms of depression among adults: United States, 2019. NCHS Data Brief, no 379. National Center for Health Statistics. (2020) https://www.cdc.gov/nchs/products/databriefs/db379.htm [PubMed]
- 62.National Institute for Alcohol Abuse and Alcoholism. (2020). Alcohol facts and statistics. National Institute of Health. Updated: March 2021. Retrieved on May 7, 2021, from: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics
- 63.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 64.Ran L, Wang W, Ai M, Kong Y, Chen J, Kuang L. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: A study of the general population in China at the peak of its epidemic. Soc. Sci. Med. 2020;262:1161. doi: 10.1016/j.socscimed.2020.113261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Young K, Kolcz D, O'Sullivan D, Ferrand J, Fried J, Robinson K. Health care workers' mental health and quality of life during COVID-19: Results from a mid-pandemic, national survey. Psychiatr. Serv. 2021;72(2):122–128. doi: 10.1176/appi.ps.202000424. [DOI] [PubMed] [Google Scholar]
- 66.Browning MH, Larson LR, Sharaievska I, Rigolon A, McAnirlin O, Mullenbach L, Alvarez HO. Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS ONE. 2021;16(1):e0245327. doi: 10.1371/journal.pone.0245327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morb. Mortal. Wkly Rep. 2020;69(32):1049. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.James PB, Steel WA, Adams J. Post-Ebola psychosocial experiences and coping mechanisms among Ebola survivors: A systematic review. Trop. Med. Int. Health. 2019;24(6):671–691. doi: 10.1111/tmi.13226. [DOI] [PubMed] [Google Scholar]
- 69.Banna MHA, Sayeed A, Kundu S, Christopher E, Hasan MT, Begum MR, Khan MSI. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. Int. J. Environ. Health Res. 2020;1:1–12. doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- 70.Durant TJ., Jr The utility of vulnerability and social capital theories in studying the impact of Hurricane Katrina on the elderly. J. Fam. Issues. 2011;32(10):1285–1302. [Google Scholar]
- 71.Islam S, Sujan SH, Tasnim R, Sikder T, Potenza MN, Van Os J. Psychological responses during the COVID-19 outbreak among university students in Bangladesh. PLoS ONE. 2020;15(12):1–15. doi: 10.1371/journal.pone.0245083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lee S. Subjective well-being and mental health during the pandemic outbreak: Exploring the role of institutional trust. Res. Aging. 2020;1:1–12. doi: 10.1177/0164027520975145. [DOI] [PubMed] [Google Scholar]
- 73.Borgonovi F, Andrieu E. Bowling together by bowling alone: Social capital and Covid-19. Soc. Sci. Med. 2020;265:113501. doi: 10.1016/j.socscimed.2020.113501. [DOI] [PubMed] [Google Scholar]
- 74.Makridis CA, Wu C. How social capital helps communities weather the COVID-19 pandemic. PLoS ONE. 2021;16(1):e0245135. doi: 10.1371/journal.pone.0245135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ozdemir F, Cansel N, Kizilay F, Guldogan E, Ucuz I, Sinanoglu B, Colak C, Cumurcu HB. The role of physical activity on mental health and quality of life during COVID-19 outbreak: A cross-sectional study. Eur. J. Integrat. Med. 2020;40:1048. doi: 10.1016/j.eujim.2020.101248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cull WL, O'Connor KG, Sharp S, Tang SF. Response rates and response bias for 50 surveys of pediatricians. Health Serv. Res. 2005;40(1):213–226. doi: 10.1111/j.1475-6773.2005.00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Adıbelli D, Sümen A. The effect of the coronavirus (COVID-19) pandemic on health-related quality of life in children. Child Youth Serv. Rev. 2020;119:1–7. doi: 10.1016/j.childyouth.2020.105595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Reardon S. Ebola's mental-health wounds linger in Africa: Health-care workers struggle to help people who have been traumatized by the epidemic. Nature. 2015;519(7541):13. doi: 10.1038/519013a. [DOI] [PubMed] [Google Scholar]
- 79.Wang C, Chudzicka-Czupała A, Tee ML, Núñez MIL, Tripp C, Fardin MA, Habib HA, Tran BX, Adamus K, Anlacan J, García ME. A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans, Asians and Europeans. Sci. Rep. 2021;11(1):1–12. doi: 10.1038/s41598-021-85943-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shultz JM, Baingana F, Neria Y. The 2014 Ebola outbreak and mental health: Current status and recommended response. JAMA. 2015;313(6):567–568. doi: 10.1001/jama.2014.17934. [DOI] [PubMed] [Google Scholar]
- 81.Wade D, Crompton D, Howard A, Stevens N, Metcalf O, Brymer M, Ruzek J, Watson P, Bryant R, Forbes D. Skills for Psychological Recovery: Evaluation of a post-disaster mental health training program. Disaster Health. 2014;2(3–4):138–145. doi: 10.1080/21665044.2015.1085625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT) toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28(3):7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- 83.Zhou J, Liu L, Xue P, Yang X, Tang X. Mental health response to the COVID-19 outbreak in China. Am. J. Psychiatry. 2020;177(7):574–575. doi: 10.1176/appi.ajp.2020.20030304. [DOI] [PubMed] [Google Scholar]