Abstract
We present the case of a 41-year-old male, suspected to have pulmonary thromboembolism with a history of coronavirus disease 2019 (COVID-19) infection 1 month ago. He presented with dyspnea and dry cough for 2 weeks. D-dimer was >776.70 mcg/L. Lung perfusion scan with Tc-99m macroaggregated albumin revealed multiple bilateral segmental perfusion defects with no mass lesion/consolidation on high-resolution computed tomography (CT) of lungs suggestive of pulmonary embolism (PE) present according to perfusion only modified PIOPED II criteria. CT pulmonary angiogram showed a large filling defect in the right pulmonary artery. The case emphasizes the prolonged sequelae following COVID-19 after recovery from the acute phase of the illness. Lung perfusion scintigraphy can play an important role in the screening of such patients who may be at risk for developing PE as post-COVID-19 sequelae.
Keywords: Coronavirus disease 2019, lung perfusion scintigraphy, pulmonary embolism
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) that causes a SARS, a characteristic hyperinflammatory response, vascular damage, microangiopathy, angiogenesis, and widespread thrombosis.[1] We present the case of a 41-year-old male with suspected pulmonary embolism (PE) post-COVID-19 infection 1 month ago. The patient was diagnosed with COVlD-19 on the basis of reverse transcription polymerase chain reaction analysis of rhinopharyngeal samples when he had the complaints of fever and dyspnea. He did not require hospital admission for the same. At present, he came with a history of dyspnea and dry cough for 2 weeks. His respiratory rate was 20/min and oxygen saturation 88%. D-dimer was >776.70 mcg/L. With a clinical suspicion of pulmonary thromboembolism, a lung perfusion scan was advised by the referring clinician for screening.[2] Lung perfusion scan [Figure 1] with Tc-99m macroaggregated albumin revealed severely reduced perfusion in the right lung, more prominently in the upper and lower lobe. Multiple wedge-shaped perfusion defects were seen in the left lung. Quantitative analysis of the perfusion scan, right lung (%) – upper zone – 2.3%, middle zone – 18.6%, lower zone – 2.3% (total right lung perfusion % – 23.2%), left lung (%) – upper zone – 22.8%, middle zone – 40.2%, and lower zone – 13.8% (total %–76.8%). There was no mass lesion or consolidation on high-resolution computed tomography (CT) of lungs suggestive of PE present according to perfusion only modified PIOPED II criteria.[3] The CT [Figure 2a] showed few areas of juxtapleural fibrosis, suggestive of postinfective changes. In these cases, V/Q scan may be the first scan to indicate the presence of thromboembolic disease and can be a good screening tool for the same. The patient was started on anticoagulation therapy at the earliest. CT chest with pulmonary angiography [Figure 2b and c] was done which confirmed the diagnosis with a large filling defect noted in the right pulmonary artery and its subsegmental branches. There are few studies showing PE in COVID-19 pneumonia[4,5] and few case reports of PE as post-COVID-19 sequelae.[6,7,8] The case emphasizes the prolonged sequelae following COVID-19 after recovery from the acute phase of the illness. More studies may be required to risk stratify thrombotic the patients and identify the role of thromboprophylaxis for the mild cases of COVID-19. Lung perfusion scintigraphy can play an important role in the screening of such patients who may be at risk for developing PE as post-COVID-19 sequelae.
Figure 1.
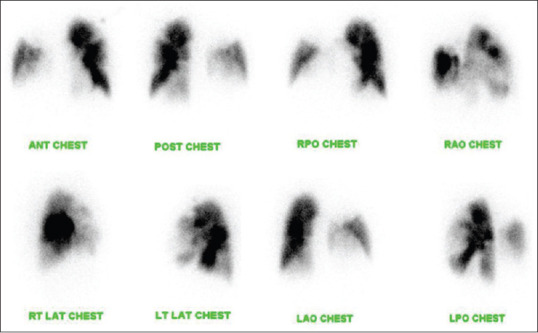
Tc-99m macroaggregated albumin reveal severely reduced perfusion in the right lung, more prominently in the upper and lower lobes. Multiple wedge-shaped perfusion defects seen in the left lung
Figure 2.
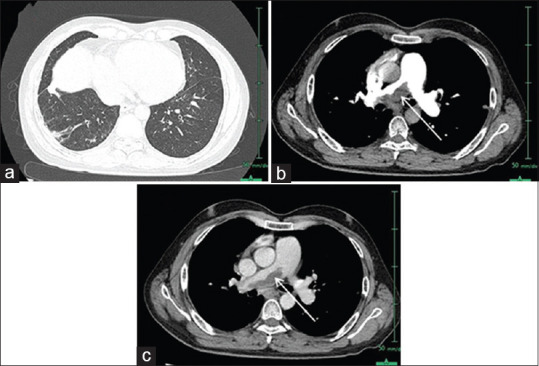
(a) High-resolution computed tomography lungs shows juxtapleural fibrosis, suggestive of postinfective changes in the middle lobe of the right lung. (b) (Thin arterial postcontrast pulmonary angiography) - shows a right main pulmonary artery thrombus (arrow) causing a narrowing of the vessels downstream. (c) (CTPA, delayed image)-shows similar findings
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stasi C, Fallani S, Voller F, Silvestri C. Treatment for COVID-19: An overview. Eur J Pharmacol. 2020;889:173644. doi: 10.1016/j.ejphar.2020.173644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: Management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001;135:98–107. doi: 10.7326/0003-4819-135-2-200107170-00010. [DOI] [PubMed] [Google Scholar]
- 3.Parker JA, Coleman RE, Grady E, Royal HD, Siegel BA, Stabin MG, et al. Society of Nuclear Medicine. SNM practice guideline for lung scintigraphy 4.0. J Nucl Med Technol. 2012;40:57–65. doi: 10.2967/jnmt.111.101386. [DOI] [PubMed] [Google Scholar]
- 4.Sakr Y, Giovini M, Leone M, Pizzilli G, Kortgen A, Bauer M, et al. Pulmonary embolism in patients with coronavirus disease-2019 (COVID-19) pneumonia: A narrative review. Ann Intensive Care. 2020;10:124. doi: 10.1186/s13613-020-00741-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bompard F, Monnier H, Saab I, Tordjman M, Abdoul H, Fournier L, et al. Pulmonary embolism in patients with COVID-19 pneumonia. Eur Respir J. 2020;56:2001365. doi: 10.1183/13993003.01365-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vadukul P, Sharma DS, Vincent P. Massive pulmonary embolism following recovery from COVID-19 infection: Inflammation, thrombosis and the role of extended thromboprophylaxis. BMJ Case Rep. 2020;13:e238168. doi: 10.1136/bcr-2020-238168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar MA, Krishnaswamy M, Arul JN. Post COVID-19 sequelae: Venous thromboembolism complicated by lower GI bleed. BMJ Case Rep. 2021;14:e241059. doi: 10.1136/bcr-2020-241059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Tano G, Moschini L, Loffi M, Testa S, Danzi GB. Late pulmonary embolism after COVID-19 pneumonia despite adequate rivaroxaban treatment. Eur J Case Rep Intern Med. 2020;7:001790. doi: 10.12890/2020_001790. [DOI] [PMC free article] [PubMed] [Google Scholar]


