Abstract
BACKGROUND
Bedside needle arthroscopy of the ankle under local anesthesia has been proposed for intra-articular delivery of injectable agents. Accuracy and tolerability of this approach in the clinical setting–including patients with end-stage ankle pathology and/or a history of prior surgery–is not known.
AIM
To assess clinical accuracy and tolerability of bedside needle arthroscopy as a delivery system for injectable agents into the tibiotalar joint.
METHODS
This was a prospective study that included adult patients who were scheduled for an injection with hyaluronic acid to the tibiotalar joint. In our center, these injections are used as a last resort prior to extensive surgery. The primary outcome was injection accuracy, which was defined as injecting through the arthroscopic cannula with intra-articular positioning confirmed by a clear arthroscopic view of the joint space. Secondary outcome measures included a patient-reported numeric rating scale (NRS, 0-10) of pain during the procedure and willingness of patients to return for the same procedure. NRS of ankle pain at rest and during walking was collected at baseline and at 2-wk follow-up. Complications were monitored from inclusion up to a 2-wk control visit.
RESULTS
We performed 24 inspection-injections. Eleven (46%) participants were male, and mean age was 46.8 ± 14.5 years. Osteoarthritis was the indication for injection in 20 (83%) cases, of which 8 (33%) patients suffered from osteoarthritis Kellgren-Lawrence grade IV, and 10 (42%) patients from Kellgren-Lawrence grade III. An osteochondral defect was the indication for injection in 4 (17%) cases. A history of ankle surgery was present in 14 (58%) participants and a history of multiple ankle surgeries in 11 (46%) participants. It was possible to confirm accuracy in 21 (88%) procedures. The 3 (12%) participants where needle arthroscopy did not reach a clear view of the joint space all suffered from Kellgren-Lawrence grade IV osteoarthritis. Pain during the procedure was reported with a median of 1 [interquartile ranges (IQR): 0–2]. Willingness to return was 100%. Pain in rest decreased from a median NRS of 4 (IQR: 2–7) at baseline to a median of 3 (IQR: 1–5) at follow-up (P < 0.01). Pain during walking decreased from a median NRS of 8 (IQR: 6–9) to a median of 7 (IQR: 4–8) (P < 0.01). Infections or other complications were not encountered.
CONCLUSION
Clinical accuracy and tolerability of bedside needle arthroscopy of the ankle as a delivery system for injectable agents are excellent. Accuracy was 100% in patients without total ventral joint obliteration.
Keywords: Ankle arthroscopy, NanoScope, Needle arthroscopy, Injections, Proof of concept, Patient experience
Core Tip: Needle arthroscopy is rapidly attracting the interest of the orthopedic field, as recent technical innovation has increased image quality and improved surgical handling. Bedside needle arthroscopy under local anesthesia has been proposed as a possible use. In this study, we performed needle arthroscopic inspection-injections of the tibiotalar joint in the procedure room and using only local anesthesia. We found high accuracy of these guided injections, and excellent patient tolerability of the procedure. The results of this study may form the groundwork for further expansion of indications that merit needle arthroscopy of the ankle under local anesthesia, including operative procedures.
INTRODUCTION
Intra-articular injections play an important role in orthopedic surgery[1], and innovative injectable agents promise to further increase their importance as minimally invasive treatment[2,3]. Yet, accuracy of articular injections is often limited, which lowers the chance of a positive treatment effect[4]. In the tibiotalar joint, accuracy of injections ranges between a mere 67% and 77% when guided by palpation[4]. The effect of ultrasound guidance is highly variable, and often does not improve injection accuracy at all[5]. Inaccurate injections may be especially unacceptable in case of expensive biologic augments, slowly releasing delivery systems, or for injections that have a detrimental effect on soft tissue.
Needle arthroscopy was first introduced in the 1990s, yet was never adopted as standard modality due to low image quality and inconvenient machinery. However, recent innovation has led to a substantial increase in image quality and has reduced the size of supportive devices to the likes of a tablet computer[6]. In a cadaveric study, this improved version of needle arthroscopy provided easy and safe access to the ankle[6].
Based on cadaveric experience, it has been suggested to use needle arthroscopy under local anesthesia as a means to inspect the ankle joint and to simultaneously deliver an injectable in a minimally invasive yet highly accurate manner[6]. Yet, feasibility of this approach has not been tested in a patient setting so far. The cadaveric setting may differ from clinical practice, as for example patient discomfort, time pressure, scar tissue and joint stiffness may hamper a successful procedure. Therefore, the aim of this study was to assess the accuracy and patient tolerability of bedside needle arthroscopy to deliver injectable agents to the ankle joint in a clinical setting, which may include participants with advanced pathology and a history of previous ankle surgery. We hypothesized that even in such a difficult patient group, we would be able to deliver injections with high accuracy, and that procedures would be well tolerated by patients.
MATERIALS AND METHODS
A prospective pilot study of consecutive patients was conducted in our academic hospital between December 2019 and December 2020. The study was approved by our institutional ethical review board with reference 2019_203 and conducted in agreement with the 1964 Helsinki Declaration and its later amendments. All patients provided written consent for their participation. The study was monitored by our institution’s monitoring board. Prior to the first inclusion, the study was registered at ToetsingOnline.nl with reference NL71185.018.19.
Patients
All patients between 18 years and 80 years of age that were planned for an injection with hyaluronic acid in the tibiotalar joint were potentially eligible for inclusion. In our center, these injections are used as a last resort of conservative management. Patients were excluded from the study who had concern for active local or systemic infection, known history of bleeding disorders, were unable to communicate informed consent, or were logistically unavailable at the time of planned needle arthroscopy.
Arthroscopic procedure
We used a 1.9-millimeter arthroscope (NanoScope, Arthrex, Naples, FL, United States) for procedures. Procedures were performed by two fellowship trained foot and ankle surgeons with extensive experience in ankle arthroscopy (SAS and GK) in an outpatient treatment room, suitable for small interventions. The patient was positioned in supine semi-sitting position on a standard operating chair. The ankle was disinfected with a chlorohexidine solution and standard surgical draping was applied. A standard anteromedial portal was utilized and located by palpation. The portal was locally anesthetized with lidocaine 2%, injected along the entire tract including the joint capsule. Once the anesthetic had taken effect, a 2-mm stab incision of the skin was made at the desired portal location. A 2.3-mm diameter cannula was positioned intra-articular, with help of a blunt obturator and slight non-invasive distraction. The obturator was removed and the arthroscope was inserted. Syringes with sterile saline could be connected to the cannula for improving visibility. If needed, the cannula was repositioned (with a maximum of three attempts) until a clear view of the intra-capsular joint space was obtained. No power tools were used and the joint capsule was not resected or debrided. Once the intra-articular view was confirmed, any injected saline was aspirated, after which the pre-packed syringe with hyaluronic acid was connected to the cannula, and the hyaluronic acid was delivered to the joint space through the cannula. The cannula was then flushed with 1cc of saline in order to deliver all the remaining hyaluronic acid. The arthroscope and cannula were removed and the 2-mm portal was closed with sterile wound closure strips. Standard post-treatment care–including 48 h of partial weightbearing–was advised. In the cases where a clear view of the joint space could not be obtained after three attempts, we converted to an intra-articular injection through a standard 21G (green) needle.
Outcome measures
The primary outcome measure was injection accuracy. An accurate injection was defined as injecting through the arthroscopic cannula with intra-articular positioning confirmed by a clear arthroscopic view of the intra-capsular joint space. As secondary outcome measures we collected intra-operative complications, need for conversion to a conventional injection, reason for conversion and procedure time (from patient entrance to patient departure from the procedure room). In addition, patient-reported outcome measures (PROMS) were collected at discharge and during a control visit 2 wk after the procedure. PROMS included numeric rating scales (NRS, 0–10) of pain at rest and during walking as experienced in the 2 wk prior to answering the questionnaire (i.e. in the 2 wk prior to either the intervention or the follow-up visit). At discharge, PROMS additionally included NRS of pain during the procedure, and a dichotomous promotor score, asking patients whether they would undergo the procedure again if needed. Complications (infection, neurovascular damage, pain or other complaints prompting contact with a physician) were monitored from inclusion up to study end upon completing the control visit. Follow-up and collection of PROMS was not performed by the orthopedic surgeon but by an independent PhD-fellow (TS) instead.
Analysis
We determined to include 24 patients which, applying the sample size calculation for pilot studies by Viechtbauer et al[7] (2015), gives 95% certainty to detect problems that arise with a probability of at least 12%. Descriptive statistics of primary and secondary outcome parameters were provided. Each variable was tested for normality with the Shapiro-Wilk test. Medians and interquartile ranges (IQR) were calculated in case of non-normally distributed data. Otherwise, means and standard deviations (SD) were provided. The Wilcoxon signed-rank test was used to compare preoperative and postoperative outcome scores. In case of a statistically significant difference in PROMS between discharge and follow-up, the number of patients that met the threshold for a minimal clinically important difference (MCID) was calculated[8]. For the NRS of pain, this MCID was set a minimal difference of three points on the 0–10 scale[9]. Data was collected using CASTOR EDC[10]. Analyses were conducted using Stata 12 (StataCorp, College Station, TX, United States).
RESULTS
Twenty-four patients were screened for eligibility and included in the study and received a needle arthroscopic injection. Eleven (46%) patients were male (Table 1). Mean age was 46.8 ± 14.5 years (range: 20–71 years). Twenty (83%) injections were performed as a temporizing biotribologic therapeutic for advanced osteoarthritis with near obliteration of the joint space. Kellgren-Lawrence grading was grade IV in 8 (33%) patients and grade III in 10 (42%) patients. Four (17%) injections were performed as a treatment modality for a talar osteochondral defect. Fourteen (58%) patients had a history of prior surgery–either open or arthroscopic–to the applicable ankle, and 11 (46%) had a history of multiple prior surgeries.
Table 1.
Patient demographics at the time of the intervention (mean ± SD)
|
Parameter
|
Value
|
| Age in yr (range) | 46.8 ± 14.5 (20–71) |
| Sex | |
| Male, n (%) | 11 (46%) |
| Female, n (%) | 13 (54%) |
| Indication for injection | |
| Osteoarthritis, n (%) | 20 (83%) |
| Kellgren-Lawrence Grade I (n) | 0 |
| Kellgren-Lawrence Grade II (n) | 2 |
| Kellgren-Lawrence Grade III (n) | 10 |
| Kellgren-Lawrence Grade IV (n) | 8 |
| (Osteo)chondral defect, n (%) | 4 (17%) |
| Prior ankle surgery | |
| None, n (%) | 10 (42%) |
| Any, n (%) | 14 (58%) |
| Multiple, n (%) | 11 (46%) |
Procedure
It was possible to perform an injection with arthroscopic confirmation of accuracy in 21 (88%) patients (Table 2 and Figure 1). Conversion to a conventional injection needle was needed in 3 (12%) patients, all on account of technical inability to achieve intra-articular positioning of the needle arthroscope within three attempts. All failures occurred in patients suffering from end-stage osteoarthritis with Kellgren-Lawrence grade IV. Two of the failed cases occurred in a patient with a history of prior ankle surgery, of which 1 patient had had multiple prior surgeries. There were no intra-operative complications. Mean intra-OR time was 17 ± 5 min. Sterile wound closure strips were sufficient for wound closure in all cases and sutures were never required.
Table 2.
Procedure and follow-up (mean ± SD)
|
Parameter
|
Value
|
| Accurate injections, n (%) | 21 (88%) |
| Accuracy by indication | |
| Kellgren-Lawrence Grade I [n accurate (% of subset)] | NA |
| Kellgren-Lawrence Grade II [n accurate (% of subset)] | 2 (100%) |
| Kellgren-Lawrence Grade III [n accurate (% of subset)] | 10 (100%) |
| Kellgren-Lawrence Grade IV [n accurate (% of subset)] | 5 (62.5%) |
| (Osteo)chondral defect [n accurate (% of subset)] | 4 (100%) |
| Accuracy by prior ankle surgery | |
| None [n accurate (% of subset)] | 9 (90.0%) |
| Any [n accurate (% of subset)] | 12 (85.7%) |
| Multiple [n accurate (% of subset)] | 10 (90.1%) |
| Procedure time (min) | 17 ± 5 |
| Completed follow-up, n (%) | 24 (100%) |
| Follow-up time (median days, IQR) | 14 (IQR, 14–16) |
| Complications, n (%) | 0 (0%) |
NA: Not applicable; IQR: Interquartile ranges.
Figure 1.
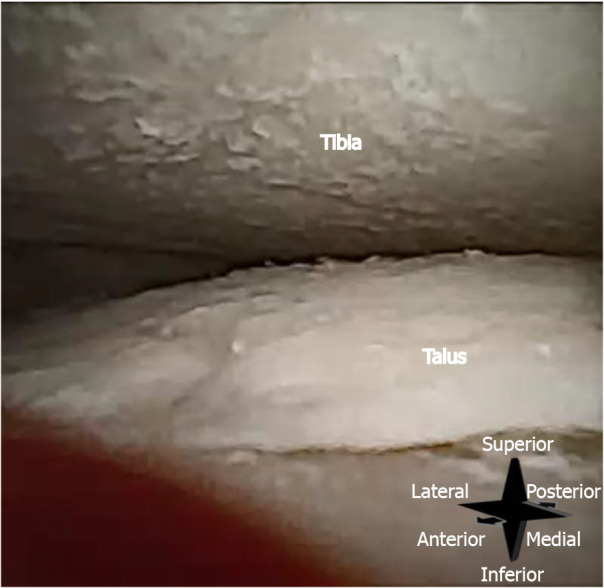
Intra-articular image of a right tibiotalar joint, taken with the 0° arthroscope inserted through the anteromedial portal. Substantial chondral wear can be seen on talus and tibia, with uncovered bone clearly visible.
Follow-up
All (100%) patients completed the follow-up visit and questionnaire (Table 2). The follow-up visit was performed at a median of 14 d (IQR: 14–16) after the intervention. Due to restrictions in the first wave of the COVID-19 pandemic, 2 follow-up visits were conducted by phone. All other visits were conducted in person. No infectious or neurovascular complications were found. No patient contacted a physician in the period between intervention and follow-up.
PROMS
The median NRS of pain during the arthroscopic procedure was 1 (IQR: 0–2) (Table 3). All (100%) patients were willing to return for another bedside needle arthroscopic injection if needed. Median NRS of pain in rest decreased from 4 (IQR: 2–7) in the 2 wk prior to the intervention, to 3 (IQR: 1–5) in the 2 wk prior to the follow-up visit (P < 0.01). In 6 patients, pain in rest decreased with at least 3 points (MCID) on the NRS scale. Pain during walking decreased from a median NRS of 8 (IQR: 6–9) to a median NRS of 7 (IQR: 4–8) (P < 0.01). In 7 patients, pain during walking decreased with at least 3 points (MCID) on the NRS scale.
Table 3.
Patient reported outcome
|
Activity
|
Intervention
|
Follow-up
|
Difference (P value)
|
| Willing to return, n (%) | 24 (100%) | NA | NA |
| NRS of pain (0–10) | |||
| During procedure (median, IQR) | 1 (0–2) | NA | NA |
| In rest (past 2 wk) (median, IQR) | 4 (2–7) | 3 (1–5) | < 0.01 |
| Walking (past 2 wk) (median, IQR) | 8 (6–9) | 7 (4–8) | < 0.01 |
NA: Not applicable; NRS: Numeric rating scale; IQR: Interquartile ranges.
DISCUSSION
Can bedside needle arthroscopy of the ankle be an accurate option for intra-articular delivery of injectable agents? Yes, but be aware that a difficult patient population with extensive scar tissue due to prior surgeries and severe joint space narrowing due to advanced osteoarthritic joint obliteration will not provide a 100% success rate. The main finding of this study was that 2-mm diameter needle arthroscopy of the ankle was able to achieve clear intra-articular positioning in 88% (21 out of 24) of cases. It was then possible to deliver hyaluronic acid in the joint space with absolute certainty in these 21 cases. The success rate was 100% in patients with less advanced osteoarthritis (Kellgren-Lawrence grade III) or lower and the success rate was 90% in patients without a history prior ankle surgery. Therefore, patient selection and counseling is important before considering inspection-injection through needle arthroscopy of the ankle. Procedures were well tolerated and there were no complications in this cohort, including a follow-up visit at 14 d.
A recent literature review by Hall[4] (2013) found that in a clinical setting, ankle injections are delivered with an accuracy ranging between 67% and 77%, if guided by palpation[4]. Although not statistically tested, the 88% accuracy this study found for needle arthroscopic injections is higher. This could be explained by the visual confirmation of the position of the arthroscope. In case of extra-articular positioning, the arthroscope was repositioned until correctly located in the joint. Repositioning of the needle in conventional procedures still could result in an extra-articular injection.
Intra-articular positioning of the arthroscope and cannula was not achieved in 3 patients (12%). All 3 patients suffered from Kellgren-Lawrence grade IV osteoarthritis, with complete obliteration of the ventral joint space. The joint space between their talus and tibia was less than 2 mm–too narrow for a safe introduction of the arthroscope, despite the use of non-invasive distraction. In addition, osteophytes narrowed the angle in which it was possible to navigate the arthroscope. As the needle arthroscope that was used has a 0° direction of view, changing the direction of view cannot be achieved by rotating the camera, as it can with for example conventional 30° arthroscopes. Instead, the direction of view can only be changed by tilting the entire arthroscope. Osteophytes limit the possibility for this tilting of the arthroscope, which may hamper visualization of the joint. Furthermore, the flexibility of the small diameter needle scope prevents using the barrel of the scope as a lever to gain access to the joint. We therefore recommend to carefully examine the patient’s radiological studies, which may constitute simple X-ray’s–in case of severe osteoarthritis, before considering needle arthroscopic injections. The amount of joint distraction that can be achieved with non-invasive distraction in patients with end-stage joint destruction under local anesthesia is a subject for further study.
Fourteen patients (58%) had a history of prior surgery. We noted difficulty with arthroscope introduction in 5 of them. In conventional arthroscopy, partial synovectomy is performed to obtain a clear view in these patients[11]. Needle arthroscopic synovectomy has been performed in the knee[12], and cadaveric studies have shown the feasibility of operative needle arthroscopy in the ankle[6]. In the knee, synovectomy under local anesthesia is well tolerated by most patients[13]. For the ankle, clinical feasibility of needle arthroscopic (partial) synovectomy under local anesthesia has yet to be established. Nevertheless, whether it is acceptable to perform a synovectomy may depend on the indication for needle arthroscopy, and may be excessively invasive for a simple injection. Extensive prior surgery may hence be a contraindication for bedside needle arthroscopy in these cases.
Procedures were well tolerated by patients and there were no complications up to a 2-wk follow-up. Although this is the first study to evaluate bedside needle arthroscopy of the ankle, needle arthroscopic procedures have been performed under local anesthesia in the knee and shoulder, and were well tolerated by patients in these joints as well[14]. That the procedure is well tolerated is further substantiated by 100% of participants being willing to return for another needle arthroscopic injection if needed. A recent cadaveric study showed that needle arthroscopy of the ankle does not pose a risk of damaging major neurovascular structures when using the anteromedial portal[6], which substantiates that our current study did not find any signs of neurovascular complications at 2-wk follow-up. Although this study cannot exclude that complications with a low prevalence (such as infection) may arise, a review of 1419 patients that underwent diagnostic needle arthroscopy of the knee or shoulder found no major complications[15], providing further assurance of the safety of the procedure.
This study is limited by its design as a pilot study. It does not offer a comparison with conventional injections, nor with conventional arthroscopy or more invasive forms of anesthesia. It should rather be interpreted as a proof of feasibility of bedside needle arthroscopy of the ankle and delivery of injectable agents under local anesthesia. Arthroscopy is difficult to perform in the ankle, especially with a 0° direction of view. In that sense, it is important to note that the study may have been underpowered to detect problems or events such as rare complications that occur with a frequency of less than 12%.
The basic procedure as reviewed in this study may be further augmented in order to increase benefit to patient and physician. A recent systematic review showed that compared to MRI, needle arthroscopy has higher accuracy in diagnosing knee osteoarthritis, anterior cruciate ligament insufficiency, meniscal tears, and osteochondral defects[14]. Needle arthroscopic diagnosis and delivery of an injectable treatment would be a beneficial combination. In general, the results of this study may form the groundwork for further expansion of indications that merit needle arthroscopy of the ankle under local anesthesia, including operative procedures.
CONCLUSION
In conclusion, in this clinical pilot study, needle arthroscopy of the ankle showed to be a procedure that is well tolerated by patients under local anesthesia. It is able to confirm intra-articular delivery of injectable agents with high accuracy. Accuracy may approach 100% by excluding patients with total ventral joint obliteration and patients with a history of extensive prior ankle surgery.
ARTICLE HIGHLIGHTS
Research background
Needle arthroscopy is rapidly attracting the interest of the orthopedic field, as recent technical innovation has increased image quality and improved surgical handling. Bedside needle arthroscopy of the ankle under local anesthesia has been proposed for intra-articular delivery of injectable agents.
Research motivation
Clinical accuracy and tolerability of this approach is not known.
Research objectives
To assess clinical accuracy and tolerability of bedside needle arthroscopy as a delivery system for injectable agents into the tibiotalar joint.
Research methods
A prospective clinical study was conducted. Adult patients who were scheduled for an injection to the ankle joint were included. The primary outcome was accuracy of bedside needle arthroscopic injections under local anesthesia. Additionally, a patient reported numeric rating scale (NRS, 0-10) of pain during the procedure and willingness of patients to return for a similar procedure if needed were recorded. Occurrence of complications was monitored from inclusion up to a 2-wk control visit.
Research results
Of 24 inspection-injections were performed. Osteoarthritis was the indication for injection in 20 (83%) cases–of which 8 cases (33%) were Kellgren-Lawrence grade IV, and 10 cases (42%) were Kellgren-Lawrence grade III. The indication was an osteochondral defect in 4 (17%) participants. Fourteen (58%) participants had a history of ankle surgery and 11 (46%) patients a history of multiple ankle surgeries. It was possible to confirm accuracy in 21 (88%) procedures. The 3 (12%) participants where this confirmation failed all suffered from Kellgren-Lawrence grade IV osteoarthritis. Participants reported a NRS of pain during the procedure with a median of 1 (interquartile ranges: 0–2), and a willingness to return of 100%. We did not encounter infections or other complications.
Research conclusions
Clinical accuracy and tolerability of bedside needle arthroscopy of the ankle as a delivery system for injectable agents are excellent. Accuracy was 100% in patients without total ventral joint obliteration.
Research perspectives
The results of this study may form the groundwork for further expansion of indications that merit needle arthroscopy of the ankle under local anesthesia, including operative procedures.
Footnotes
Institutional review board statement: The study was approved by our institutional ethical review board with reference 2019_203 and conducted in agreement with the 1964 Helsinki Declaration and its later amendments.
Clinical trial registration statement: Prior to the first inclusion, the study was registered at ToetsingOnline.nl with reference NL71185.018.19.
Informed consent statement: All patients provided written consent for their participation in the study prior to enrollment.
Conflict-of-interest statement: Dr. Kennedy reports consultancy fees from Arthrex, outside the submitted work.
CONSORT 2010 statement: The authors have read the CONSORT 2010 Statement, and the manuscript was prepared and revised according to the CONSORT 2010 Statement.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: May 8, 2021
First decision: October 16, 2021
Article in press: December 31, 2021
Specialty type: Orthopedics
Country/Territory of origin: Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li HY S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
Contributor Information
Tobias Stornebrink, Department of Orthopedic Surgery, Amsterdam UMC, University of Amsterdam, Amsterdam Movement Sciences, Amsterdam 1105AZ, Netherlands; Academic Center for Evidence based Sports Medicine, Amsterdam 1105AZ, Netherlands; Amsterdam Collaboration for Health and Safety in Sports, International Olympic Committee Research Center Amsterdam UMC, Amsterdam 1105AZ, Netherlands.
Sjoerd A S Stufkens, Department of Orthopedic Surgery, Amsterdam UMC, University of Amsterdam, Amsterdam Movement Sciences, Amsterdam 1105AZ, Netherlands; Academic Center for Evidence based Sports Medicine, Amsterdam 1105AZ, Netherlands; Amsterdam Collaboration for Health and Safety in Sports, International Olympic Committee Research Center Amsterdam UMC, Amsterdam 1105AZ, Netherlands.
Nathaniel P Mercer, Department of Orthopedic Surgery, NYU Langone Health, New York, NY 10010, United States.
John G Kennedy, Department of Orthopedic Surgery, NYU Langone Health, New York, NY 10010, United States.
Gino M M J Kerkhoffs, Department of Orthopedic Surgery, Amsterdam UMC, University of Amsterdam, Amsterdam Movement Sciences, Amsterdam 1105AZ, Netherlands; Academic Center for Evidence based Sports Medicine, Amsterdam 1105AZ, Netherlands; Amsterdam Collaboration for Health and Safety in Sports, International Olympic Committee Research Center Amsterdam UMC, Amsterdam 1105AZ, Netherlands. g.m.kerkhoffs@amsterdamumc.nl.
Data sharing statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Vereniging FMS-NO. Conservatieve behandeling van artrose in heup of knie. 2018. [cited 10 May 2021]. Available from: https://richtlijnendatabase.nl/richtlijn/artrose_in_heup_of_knie/startpagina_-_heup-_of_knieartrose.html .
- 2.Repetto I, Biti B, Cerruti P, Trentini R, Felli L. Conservative Treatment of Ankle Osteoarthritis: Can Platelet-Rich Plasma Effectively Postpone Surgery? J Foot Ankle Surg. 2017;56:362–365. doi: 10.1053/j.jfas.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 3.Sandker MJ, Duque LF, Redout EM, Chan A, Que I, Löwik CWGM, Klijnstra EC, Kops N, Steendam R, van Weeren R, Hennink WE, Weinans H. Degradation, intra-articular retention and biocompatibility of monospheres composed of [PDLLA-PEG-PDLLA]-b-PLLA multi-block copolymers. Acta Biomater. 2017;48:401–414. doi: 10.1016/j.actbio.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Hall MM. The accuracy and efficacy of palpation vs image-guided peripheral injections in sports medicine. Curr Sports Med Rep. 2013;12:296–303. doi: 10.1097/01.CSMR.0000434103.32478.36. [DOI] [PubMed] [Google Scholar]
- 5.Gilliland CA, Salazar LD, Borchers JR. Ultrasound vs anatomic guidance for intra-articular and periarticular injection: a systematic review. Phys Sportsmed. 2011;39:121–131. doi: 10.3810/psm.2011.09.1928. [DOI] [PubMed] [Google Scholar]
- 6.Stornebrink T, Altink JN, Appelt D, Wijdicks CA, Stufkens SAS, Kerkhoffs GMMJ. Two-millimetre diameter operative arthroscopy of the ankle is safe and effective. Knee Surg Sports Traumatol Arthrosc. 2020;28:3080–3086. doi: 10.1007/s00167-020-05889-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viechtbauer W, Smits L, Kotz D, Budé L, Spigt M, Serroyen J, Crutzen R. A simple formula for the calculation of sample size in pilot studies. J Clin Epidemiol. 2015;68:1375–1379. doi: 10.1016/j.jclinepi.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Harris JD, Brand JC, Cote MP, Faucett SC, Dhawan A. Research Pearls: The Significance of Statistics and Perils of Pooling. Part 1: Clinical Versus Statistical Significance. Arthroscopy. 2017;33:1102–1112. doi: 10.1016/j.arthro.2017.01.053. [DOI] [PubMed] [Google Scholar]
- 9.Lee JS, Hobden E, Stiell IG, Wells GA. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med. 2003;10:1128–1130. doi: 10.1111/j.1553-2712.2003.tb00586.x. [DOI] [PubMed] [Google Scholar]
- 10.Castor EDC. Castor Electronic Data Capture. 2019. [cited 10 May 2021]. Available from: https://link.springer.com/referenceworkentry/10.1007/978-0-387-39940-9_2541 .
- 11.Guhl JF. New concepts (distraction) in ankle arthroscopy. Arthroscopy. 1988;4:160–167. doi: 10.1016/s0749-8063(88)80020-3. [DOI] [PubMed] [Google Scholar]
- 12.Lavender C, Patel T, Adil S, Blickenstaff B, Oliashirazi A. Incisionless Knee Synovectomy and Biopsy With Needle Arthroscope and Autologous Tissue Collector. Arthrosc Tech. 2020;9:e1259–e1262. doi: 10.1016/j.eats.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takahashi T, Tanaka M, Ikeuchi M, Sadahiro T, Tani T. Pain in arthroscopic knee surgery under local anesthesia. Acta Orthop Scand. 2004;75:580–583. doi: 10.1080/00016470410001457. [DOI] [PubMed] [Google Scholar]
- 14.Zhang K, Crum RJ, Samuelsson K, Cadet E, Ayeni OR, de Sa D. In-Office Needle Arthroscopy: A Systematic Review of Indications and Clinical Utility. Arthroscopy. 2019;35:2709–2721. doi: 10.1016/j.arthro.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 15.McMillan S, Chhabra A, Hassebrock JD, Ford E, Amin NH. Risks and Complications Associated With Intra-articular Arthroscopy of the Knee and Shoulder in an Office Setting. Orthop J Sports Med. 2019;7:2325967119869846. doi: 10.1177/2325967119869846. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


