Abstract
The long head of the biceps tendon is widely recognized as an important pain generator, especially in anterior shoulder pain and dysfunction with athletes and working individuals. The purpose of this review is to provide a current understanding of the long head of the biceps tendon anatomy and its surrounding structures, function, and relevant clinical information such as evaluation, treatment options, and complications in hopes of helping orthopaedic surgeons counsel their patients. An understanding of the long head of the biceps tendon anatomy and its surrounding structures is helpful to determine normal function as well as pathologic injuries that stem proximally. The biceps-labral complex has been identified and broken down into different regions that can further enhance a physician’s knowledge of common anterior shoulder pain etiologies. Although various physical examination maneuvers exist meant to localize the anterior shoulder pain, the lack of specificity requires orthopaedic surgeons to rely on patient history, advanced imaging, and diagnostic injections in order to determine the patient’s next steps. Nonsurgical treatment options such as anti-inflammatory medications, physical therapy, and ultrasound-guided corticosteroid injections should be utilized before entertaining surgical treatment options. If surgery is needed, the three options include biceps tenotomy, biceps tenodesis, or superior labrum anterior to posterior repair. Specifically for biceps tenodesis, recent studies have analyzed open vs arthroscopic techniques, the ideal location of tenodesis with intra-articular, suprapectoral, subpectoral, extra-articular top of groove, and extra-articular bottom of groove approaches, and the best method of fixation using interference screws, suture anchors, or cortical buttons. Orthopaedic surgeons should be aware of the complications of each procedure and respond accordingly for each patient. Once treated, patients often have good to excellent clinical outcomes and low rates of complications.
Keywords: Shoulder pathology, Long head of the biceps tendon, Biceps-labral complex, Biceps tenotomy, Biceps tenodesis, Superior labrum anterior to posterior lesions
Core Tip: Management of proximal pathologies involving the long head of the biceps tendon is evolving. While biceps tenotomy, biceps tenodesis, and superior labrum anterior to posterior repair can be used to treat these pathologic injuries, no consensus exists with regard to which procedure is best. This clinical review provides a current understanding of the long head of the biceps tendon anatomy and its surrounding structures, function, and relevant clinical information such as evaluation, treatment options, and complications in hopes of helping orthopaedic surgeons counsel their patients.
INTRODUCTION
While the role of the long head of the biceps tendon (LHBT) in shoulder pathology has been studied extensively, the management of such pathology has evolved. Recently, studies have demonstrated that biceps tenodesis can be used to treat individuals with symptomatic superior labrum anterior to posterior (SLAP) lesions[1-3]. As a result, the number of biceps tenodesis procedures performed each year has increased[4]. Despite this rise in volume, there is no consensus on which procedure-biceps tenotomy, biceps tenodesis, or SLAP repair is superior in terms of clinical outcomes. Typically, orthopaedic surgeons use their preference and specific patient factors to determine which procedure is ideal for each patient. Furthermore, in patients who undergo biceps tenodesis, there is controversy as to whether orthopaedic surgeons should utilize open vs arthroscopic techniques, the best method of fixation with interference screws, suture anchors, or cortical buttons, and the ideal location of tenodesis with intra-articular, suprapectoral, subpectoral, extra-articular top of groove, or extra-articular bottom of groove approaches. Regardless of this debate, researchers can agree that the LHBT is widely recognized as an important pain generator, especially in anterior shoulder pain and dysfunction[5-8].
The purpose of this review is to provide a current understanding of LHBT anatomy, function, and clinical information such as evaluation, nonsurgical management, surgical management, and complications in hopes of helping orthopaedic surgeons counsel their patients.
ANATOMY AND FUNCTION
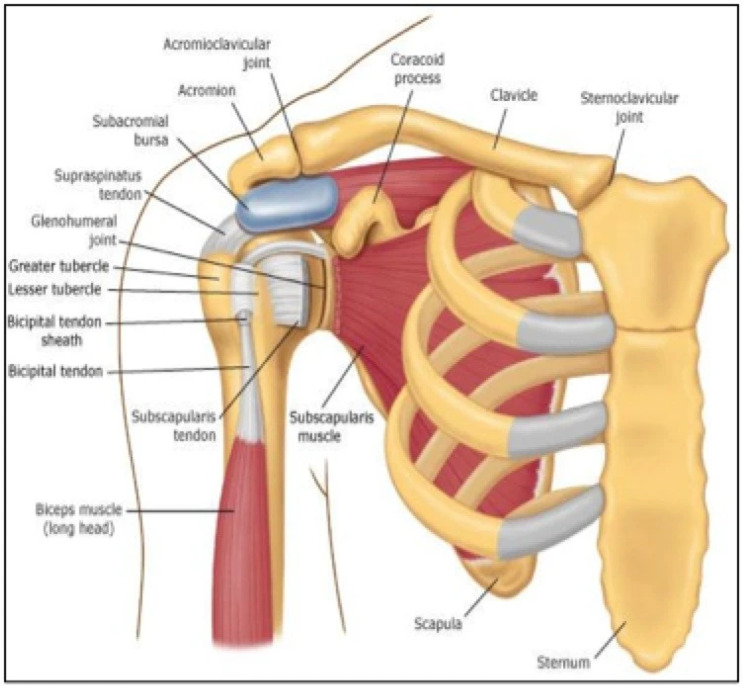
An appreciation of the LHBT anatomy and its surrounding structures is helpful to understand normal function as well as proximal pathologic injuries (Figures 1 and 2)[9,10]. The LHBT originates from the supraglenoid tubercle and the superior glenoid labrum and exits the glenohumeral joint through the bicipital groove[11]. The attachment point of the LHBT on the superior labrum is variable amongst patients: equal anterior and posterior attachment is the most common (37%), predominantly anterior is the least common (8%), and other variations such as entirely posterior (22%) or mostly posterior (33%) also exist[12,13]. As it exits the glenohumeral joint and before it enters the bicipital groove, the LHBT is stabilized by a capsule-ligamentous complex referred to as the biceps pulley, which consists of the subscapularis tendon, the supraspinatus tendon, the coracohumeral ligament, the pectoralis major tendon insertion, and the falciform ligament (Figure 1)[14,15]. The LHBT then travels distally into the bicipital groove along the anterior surface of the humerus through the osteoligamentous sheath which is formed by the transverse humeral ligament as well as the greater and lesser tuberosities (Figures 1 and 2)[16]. The LHBT and the short head of the biceps tendon, which originates from the coracoid process with the coracobrachialis, give rise to the muscle belly of the biceps brachii which externally rotates 90° before the tendons attach as a single tendinous insertion on the ulnar aspect of the bicipital tuberosity of the radius[6].
Figure 1.
Schematic illustration of anterior shoulder anatomy from Blum et al[9]. Citation: Blum K, Chen AL, Chen TJ, Waite RL, Downs BW, Braverman ER, Kerner MM, Savarimuthu SM, DiNubile N. Repetitive H-wave device stimulation and program induces significant increases in the range of motion of post operative rotator cuff reconstruction in a double-blinded randomized placebo controlled human study. BMC Musculoskelet Disord 2009; 10: 132. Copyright© The Authors 2009. Published by BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons CC BY license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure 2.
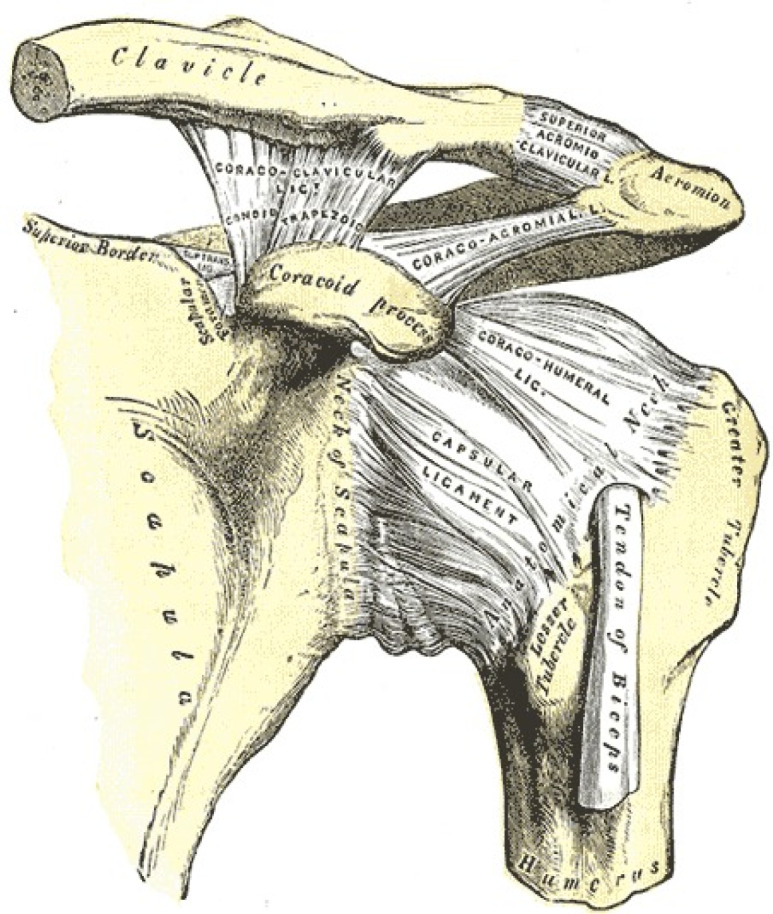
Anterior view of the left shoulder joint depicting tendons and ligaments from Miniato et al[10]. Citation: Miniato MA, Anand P, Varacallo M. Anatomy, Shoulder and Upper Limb, Shoulder. [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536933/. Copyright© The Authors 2021. Published by StatPearls Publishing LLC. This book is distributed under the terms of the Creative Commons Attribution 4.0 International License, which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license, and any changes made are indicated.
Furthermore, the long head of the biceps (LHB) and glenoid labrum have collectively been described as the “biceps-labral complex” (BLC) which can be categorized into three main parts: (1) The inside, which includes the superior labrum and the LHBT anchor at the supraglenoid tubercle; (2) The junction, which includes the intra-articular LHBT and its stabilizing pulley system; and (3) The bicipital tunnel, which includes the LHBT beginning at the articular margin of the humeral head adjacent to the pulley and extending to the subpectoral region (Figure 3)[17-19]. The bicipital tunnel, which houses the extra-articular biceps, is further divided into three clinically relevant zones. Zone 1 stretches from the articular margin to the distal margin of the subscapularis. Zone 2 extends from the distal margin of the subscapularis to the proximal margin of the pectoralis major. Lastly, zone 3 is the subpectoralis region[20].
Figure 3.
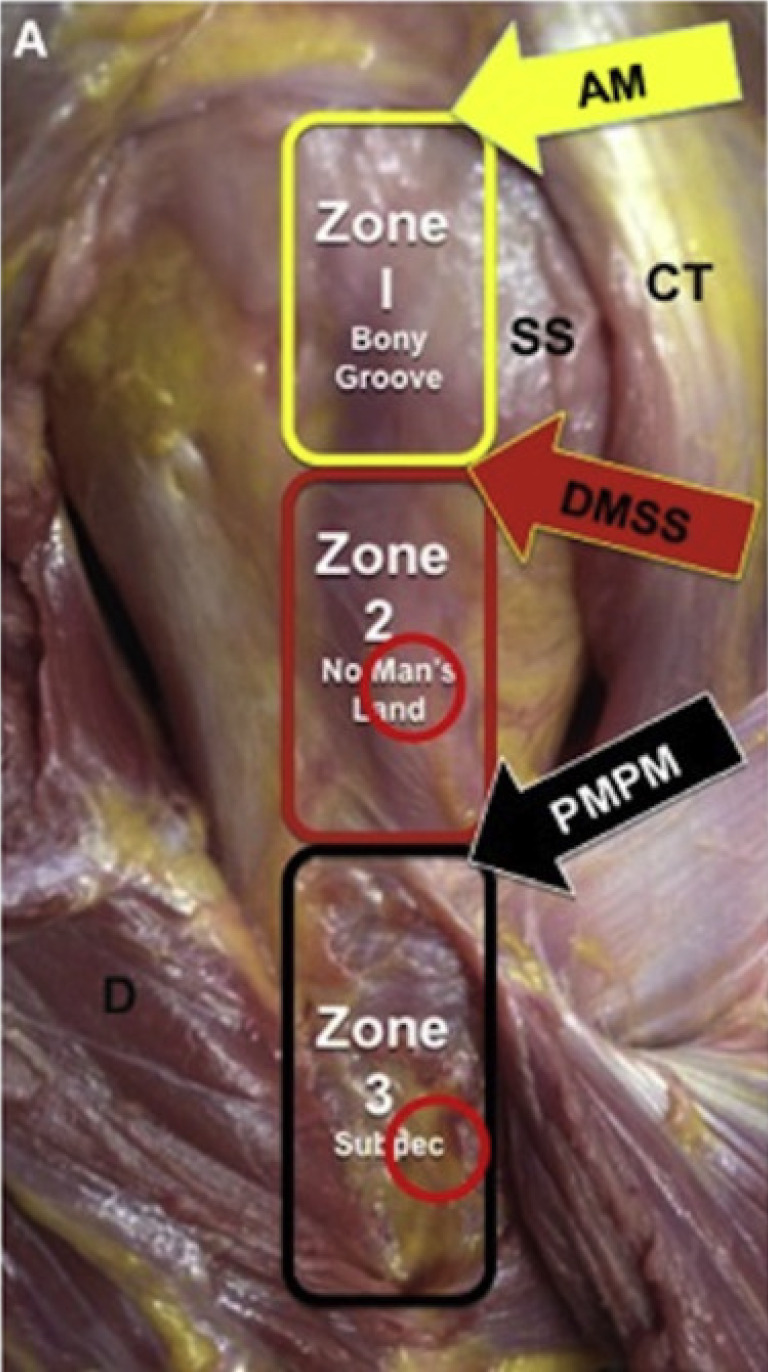
Visual depiction of biceps-labral complex with zone 2 red circle as site for arthroscopic suprapectoral tenodesis and zone 3 red circle as open subpectoral tenodesis location from Forsythe et al[120]. Citation: Forsythe B, Zuke WA, Agarwalla A, Puzzitiello RN, Garcia GH, Cvetanovich GL, Yanke AB, Verma NN, Romeo AA. Arthroscopic Suprapectoral and Open Subpectoral Biceps Tenodeses Produce Similar Outcomes: A Randomized Prospective Analysis. Arthroscopy 2020; 36: 23-32. Copyright© The Authors 2020. Published by Elsevier. The authors have obtained the permission for figure (Supplementary material). AM: Articular margin; CT: Conjoined tendon; d: Deltoid; DMSS: Distal margin of subscapularis tendon; PMPM: Proximal margin of pectoralis major; SS: Subscapularis.
The function of the LHBT still remains highly debated. Prior cadaveric studies have shown it may serve as a humeral head depressor, a stabilizer of the glenohumeral joint, or a stabilizer of the humeral head particularly in the anterosuperior and anterior directions of shoulder abduction[21-23]. Other authors consider the LHBT to be a vestigial structure that is not active during isolated shoulder movements and may have a larger role in proprioception of the shoulder[24,25]. Anatomically, there is consensus that the LHBT mainly functions as a forearm supinator while the short head of the biceps tendon mostly functions as an elbow flexor[6].
PROXIMAL BICEPS TENDON PATHOLOGY
The pathologic entities involving the LHBT can be classified into three general categories: inflammatory, instability, and traumatic[8]. Inflammation of the biceps tendon is commonly attributed to degenerative tendinopathy and overuse injuries. Additionally, rotator cuff tears and subacromial impingement can also lead to or be associated with bicipital tendinitis[26-30]. Some studies have found a prevalence as high as 93% in the association of LHBT inflammatory injuries and rotator cuff tears[31]. Instability of the tendon can create mechanical symptoms such as popping and clicking with range of motion. If the LHBT is unstable, the physician should highly suspect an associated subscapularis tendon tear or tears of the coracohumeral and/or superior glenohumeral complex[6,8]. Lastly, the LHBT is susceptible to traumatic injury, most commonly a complete rupture of the tendon, where pain resolves over time and function is typically reserved. These injury categories have been associated with other various shoulder conditions such as glenohumeral arthritis, labral lesions, and anterior or anterosuperior rotator cuff tears[1,32-35].
Anatomically, the three main parts of the BLC are associated with specific pathologic entities[17]. Injuries to the inside, which is predominantly associated with SLAP lesions, can be caused by superior migration of the humeral head, biceps tension, or peelback as a result of internal impingement[36]. Injuries to the junction include LHBT tears, LHBT incarceration, biceps chondromalacia, hourglass biceps, and pulley lesions[37-39]. The bicipital tunnel, specifically zones one and two, encompass LHBT tears, loose bodies, and tenosynovitis[18,40].
Evaluation
An in-depth history and physical examination must be done to differentiate biceps pain from other causes of referred shoulder pain[41]. This can be difficult because individuals with biceps pain can also have concomitant pathologies such as rotator cuff tears and may even have similar symptoms to patients with SLAP lesions[42-44]. As a result, physicians should utilize patient history, physical examination results, and imaging modalities to consider multiple differential diagnoses and help determine appropriate management.
A comprehensive history should be acquired when evaluating patients with LHBT injuries. A thorough history that documents the mechanism of injury can help the physician differentiate between various shoulder pathologies[45]. Obtaining information such as hand dominance, history of injury/trauma to the shoulder area, symptom exacerbation with overhead activities, pain at rest and/or pain at night, history or current overhead sport participation, history of current manual labor occupation or employment status, and any relevant surgical history can be incredibly useful in conjunction with the physical examination to determine the etiology of the pain[45].
Physical examination should start with assessment of range of motion as well as neurovascular examination that includes strength testing of all rotator cuff muscles. Common LHBT conditions that should be differentiated with an in depth physical examination include inflammatory injuries, instability, and rupture. LHBT inflammatory changes such as tenosynovitis or tendinitis often presents with pain in the anterior aspect of the shoulder that radiates to the anterior biceps[46]. Symptoms can be exacerbated by overhead activity or elbow flexion. LHBT instability will often present with reproducible clicking or tendon subluxation on physical examination[6]. For this type of injury, the physician should pay special attention to the subscapularis muscle as LHBT instability is associated with rotator cuff tears, especially those of the upper border of the subscapularis[17]. Therefore, physicians should also perform passive external rotation, lift-off, belly-press, and bear hug test for the subscapularis (Figure 4)[8,17,47]. LHBT rupture often occurs with a tearing sensation anteriorly and presents with swelling and ecchymosis. Some patients may have a Popeye deformity or sagging biceps muscle belly which can be exaggerated by having the patient flex his biceps (Figure 5)[6,17,48]. For these patients, muscle belly cramping has also been reported[49]. In patients with symptomatic proximal biceps pathology, pain will often be localized to the bicipital groove. This pain can be elicited on direct palpation of the area 7 cm below the acromion with the arm adducted, internally rotated 10°, and the elbow flexed[50]. To assist in proper palpation and pain elicitation, the shoulder should be internally and externally rotated in this position.
Figure 4.
Special tests for subscapularis from Jain et al[47]. Citation: Jain NB, Wilcox RB 3rd, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R 2013; 5: 45-56. Copyright© The Authors 2013. Published by John Wiley and Sons. The authors have obtained the permission for figure (Supplementary material). Top left: Lift-off test; Top right: Belly-press test; Bottom: Bear hug test.
Figure 5.

Lateral view showing Popeye deformity from José et al[48]. Citation: José AG, Luís Felipe HFS, Gabriel RSM, Fernando MI. Treatment of the Distal Biceps Brachii Tendon Rupture Using the Three Mini-Incisions Technique: Evaluation through MEPS and DASH. Ortho Rheum Open Access J. 2019; 14: 555888. Copyright© The Authors 2019. Published by Juniper Publishers INC. This work is licensed under Creative Commons Attribution 4.0 License.
While specific examinations in patients with biceps-related pathology and SLAP tears can be utilized to differentiate etiologies of shoulder pain, these maneuvers often lack specificity[51,52]. For example, the Speed test, which is used to elicit anterior shoulder pain with resisted elbow flexion has overall sensitivity of 57% and specificity of 52% in diagnosing biceps tendon disorders and SLAP lesions (Figure 6)[47,52-55]. Similarly, the Yergason test, which is used to elicit anterior shoulder pain with resisted forearm supination, has been shown to be an unreliable predictor of biceps pathology or SLAP tears with a reported sensitivity of 43% and specificity of 79%[54-56]. Physical examination maneuvers specific for SLAP pathology, such as the O’Brien active compression test and the O’Driscoll dynamic labral shear test, have demonstrated reasonable diagnostic utility, but are still controversial (Figure 7)[57]. While some studies initially reported excellent results for the diagnostic utility of the O’Brien active compression test, recent meta-analyses have suggested that it is not diagnostic of SLAP tears[58,59]. The O’Driscoll dynamic labral shear test was also found to have excellent initial results in terms of diagnostic utility for SLAP tears, but was questioned by further studies[60-62]. Furthermore, examination maneuvers for SLAP pathology are limited by shoulder pathology that is often observed in individuals with SLAP tears, such as Bankart lesions and partial-thickness rotator cuff tears[63-65].
Figure 6.
Speed test from Jain et al[47]. Citation: Jain NB, Wilcox RB 3rd, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R 2013; 5: 45-56. Copyright© The Authors 2013. Published by John Wiley and Sons. The authors have obtained the permission for figure (Supplementary material).
Figure 7.
O’Driscoll dynamic labral shear test from Myer et al[57]. Citation: Myer CA, Hegedus EJ, Tarara DT, Myer DM. A user's guide to performance of the best shoulder physical examination tests. Br J Sports Med 2013; 47: 903-907. Copyright© The Authors 2013. Published by BMJ Publishing Group Ltd. The authors have obtained the permission for figure (Supplementary material).
Imaging and diagnostic injections
With the lack of specificity in physical examination maneuvers, imaging studies are often used to differentiate LHBT pathology. Unfortunately, this too has its faults. While radiographs can be useful in assessing bony anomalies and ruling out concomitant osseous disorders, they often appear normal[7,52]. Advanced imaging studies such as MRI demonstrate reasonable sensitivity and specificity for the diagnosis of SLAP tears, LHBT rupture, and other inside lesions of the BLC; however, junctional and bicipital tunnel lesions are poorly identified[66-70]. Additionally, ultrasonography is a fast, cost-effective, and radiation-free diagnostic method for shoulder and has been used for LHBT instability, dynamic examination of the tendon, examination of hypoechogenic areas, and increased tendon diameter[71,72]. While ultrasound techniques are useful in detecting LHBT pathology with a sensitivity between 50%-96% and a sensitivity of 98%-100%, it is less helpful in diagnosing partial-thickness tears[71,73,74]. Regardless of its faults, ultrasonography techniques should be used in conjunction with MRI when examining LHBT pathology.
Diagnostic injections could also be utilized in patients with anterior shoulder pain as peritendinous or sheath injections are often used to clinically diagnose and treat biceps tendinopathy[75,76]. Injections into the tendon sheath can be diagnostic and therapeutic by providing the physician information about the patient’s pathology based on their pain response post-treatment[77,78]. It is important to note that injections should not be directly inserted into tendons as it can lead to tendon rupture[79]. Improved injection accuracy through ultrasound guidance has proven to be effective compared to blind injection techniques. In a recent study by Hashiuchi et al[80], ultrasound-guided injections resulted in 87% accuracy while blind injections were accurate only 27% of the time.
TREATMENT OPTIONS
The treatment of LHBT pathology can be separated into nonsurgical and surgical management. Initially, LHBT injuries should be treated conservatively followed by surgery when all conservative treatments fail.
Nonsurgical management
Nonsurgical management of LHBT disorders is largely driven by individual surgeon experience. Typically, management begins with nonsteroidal anti-inflammatory drugs, physical activity, activity modifications, and ultrasound-guided corticosteroid injections into the biceps sheath[56,80,81]. Although physical therapy improves overall shoulder strength, range of motion, and function, limited research has been done that analyzes the outcomes of physical therapy as a nonoperative management option for LHBT pathologies. As mentioned earlier, the corticosteroid injection should be carefully placed as accidentally guiding the injection into the biceps tendon may cause rupture[82]. If correctly placed, ultrasound-guided corticosteroid injections have shown to cause lower patient discomfort as well as superior accuracy compared to palpated and blind injections[83]. Unfortunately, corticosteroid injections were found only to be beneficial in the short term, but may be worse than other treatment options in the intermediate and long terms[84]. Regardless of technique, research on the effectiveness of corticosteroid injections is inconclusive[85].
Other options for nonsurgical management include iontophoresis, phonophoresis, ultrasonography, extracorporeal shock wave therapy, and laser therapy. Unfortunately, these have shown conflicting results in the literature[86,87]. Furthermore, promising yet inconclusive clinical outcomes have been shown for treatment options such as regenerative injection therapy which includes platelet-rich plasma[88,89]. If all nonsurgical treatment options fail, then patients should consider surgical treatment options.
Surgical management
While surgical management of LHBT pathologies is reserved for individuals who have failed all previously performed nonsurgical treatment options or individuals with acute injuries, the optimal surgical treatment is still up for debate[17]. The three options include biceps tenotomy, biceps tenodesis, and SLAP repair.
Biceps tenotomy: Biceps tenotomy is a viable option to surgically manage LHBT pathology and involves cutting the LHBT at its origin and maintaining the integrity of the labrum (Table 1)[49]. While numerous studies have shown excellent outcomes, pain relief, and improved patient-reported outcomes in individuals who undergo biceps tenotomy, there are a few complications shown in Table 1[46,90-92]. Other cited complications include stiffness, infection, transient nerve injuries, complex regional pain syndrome, and stroke secondary to cerebral hypoperfusion[93]. In recent studies, surgeons have tried to address some of these complications by testing arthroscopic techniques to limit distal migration of the LHB after tenotomy to minimize and even eliminate the occurrence of the Popeye deformity[94-97]. Other studies have reported ways to improve the efficiency of arthroscopic biceps tenotomy by using a biceps squeeze maneuver[98]. This is a simple method that entails manually squeezing the biceps muscle belly while performing the arthroscopic biceps tenotomy in order to shorten and tension the intra-articular portion of the tendon. In doing so, this technique improves the efficiency and safety of the procedure without adding additional cost.
Table 1.
Comparison of biceps tenotomy versus biceps tenodesis
|
|
Biceps tenotomy
|
Biceps tenodesis
|
| Timing and cost | Quicker, shorter procedure with a lower cost | Technically more challenging with a longer surgical and rehabilitation time as well as a higher cost |
| Patient population | Symptomatic patients with biceps tenosynovitis > 60 yr of age, individuals with lower demand occupations, those with minimal cosmesis concerns | Symptomatic athletic patients, individuals with higher demand occupations, those with cosmesis concerns |
| Complications | Postoperative Popeye deformity, muscle belly cramping, discomfort and fatigue | Risk of infection, loss of fixation and recurrence of Popeye deformity, implant failure |
Biceps tenodesis: Biceps tenodesis is increasingly used to treat individuals with LHBT pathology (Table 1). It involves releasing the LHBT from its origin and attaching it at one of four locations: (1) Within the glenohumeral joint to the intact rotator cuff; (2) To the conjoint tendon or the transverse humeral ligament; (3) Proximal to or within the bicipital groove in a suprapectoral fashion; or (4) Distally in a subpectoral fashion (mini-open approach)[6]. Current areas of debate include whether orthopaedic surgeons should perform biceps tenodesis open or arthroscopically, the best method of fixation (interference screw, suture anchor, or cortical button), and the ideal location of tenodesis (intra-articular, suprapectoral, subpectoral, and other positions such as extra-articular top of groove or extra-articular bottom of groove)[99].
Open vs arthroscopic: Biceps tenodesis can be performed via an open or arthroscopic approach; both methods have excellent clinical outcomes[100,101]. While a comparison between approaches is difficult due to concomitant pathology and different types of fixation, a comparison highlighting timing and cost, functional outcomes, range of motion, and complications can be seen in Table 2[102-105]. With no consensus over which method is superior, surgeons should take into account their own preference and technical experience when deciding on the proper approach for their patients.
Table 2.
Comparison of open biceps tenodesis versus arthroscopic biceps tenodesis
|
|
Open approach
|
Arthroscopic approach
|
| Timing and cost | Lower cost with slightly longer operation time | Higher cost with slightly lower operation time |
| Functional outcomes | No significant difference found between ASES, Constant, UCLA, DASH, or SST scores | |
| Range of motion | Similar in both approaches, forward range of motion slightly higher in arthroscopic approach | |
| Complications | Higher overall rate of complications such as wound healing issues, hematoma/seroma formation, nerve injury, deep vein thrombosis, and general anesthetic complications | Lower overall rate of complications, but higher incidence of postoperative stiffness and bicipital groove tenderness in early stages of recovery |
ASES: American shoulder and elbow surgeons; DASH: Disabilities of the arm, shoulder and hand; SST: Simple shoulder test.
A number of studies have analyzed open biceps tenodesis procedures in patients without rotator cuff tears and demonstrated improved patient reported outcome measures as well as pain and functional outcome scores[106-110]. Even though fewer studies have been identified for arthroscopic biceps tenodesis procedures in isolated LHB pathology, the patient reported outcome measures, pain scores, and objective outcomes are satisfactory in 98%-99% of patients with low rates of revision (0.4%) for biceps related problems[111-113].
Some studies have compared open LHB tenodesis to arthroscopic LHB tenodesis in order to determine which is superior. Abraham et al[100] and Green et al[114] found excellent outcomes with both methods and low complication rates. Gombera et al[115] compared forty-six patients who underwent arthroscopic or open biceps tenodesis and found no significant differences in American Shoulder and Elbow Surgeons (ASES) scores, patient satisfaction scores, return to sports activity, pain levels at night, pain levels with heavy activity, or Popeye deformities. In terms of complications, arthroscopic biceps tenodesis mirrors open biceps tenodesis. Complications following arthroscopic biceps tenodesis include residual postoperative groove pain, injury to the surrounding neurovascular structures, and increased risk of early postoperative stiffness[116]. Additionally, complications can be dependent on the fixation strategy. For example, open biceps tenodesis can be associated with fracture when using an interference screw and can also cause neurovascular injury in the subpectoralis region due to association with brachial plexus palsy and musculocutaneous nerve injury[117-119]. From these studies, no difference in outcomes can be found between open and arthroscopic biceps tenodesis.
Tenodesis placement: Biceps tenodesis is mainly done with intra-articular, suprapectoral, or subpectoral placement; other possible positions include extra-articular top of the groove and extra-articular bottom of the groove placement. In the intra-articular approach, the LHBT is cut and reattached within the intertubercular groove. While the clinical outcomes of this approach are excellent, patients may have persistent bicipital groove pain and tendinopathy with a portion of the tendon within the bicipital groove[120,121]. In the suprapectoral approach, the LHBT is cut and reattached distally to the bicipital groove and proximally the pectoralis major tendon. Even though this approach avoids the inflammation from the tendon remaining in the bicipital groove and sheath, it may be a longer and thus more costly approach compared to the subpectoral method and has thinner bone stock for hardware fixation[120,122,123]. Furthermore, in intra-articular and suprapectoral approaches, residual pain has been described[100,124].
In patients with significant inflammation in the biceps groove or patients where the suprapectoral part of the biceps is of poor quality or significantly injured, the subpectoral approach is the preferred method[125]. Subpectoral tenodesis is advantageous because it eliminates the pain created from reattachment within the groove, it is associated with stronger bone for fixation in the humerus, and it can potentially lead to a quicker recovery[126-128]. Like the other approaches, the subpectoral method has its disadvantages. The main disadvantages include scar formation, elongation of the biceps, biceps asymmetry, and partial detaching and reattaching of the pectoralis major to the humerus[126,128,129]. Compared to the suprapectoral approach, the subpectoral approach has more residual tenderness and spasm initially following the procedure[120]. Furthermore, fracture has been described as a complication particularly with the use of interference screws[130,131].
In a study by Godshaw et al[121], authors compared forty-three patients who had undergone intra-articular tenodesis to fifty-six patients who had undergone suprapectoral tenodesis. While both groups showed improvement in all outcome measures, there was no difference between the groups in functional outcomes for physical and mental component scores as well as ASES scores. Werner et al[128] compared arthroscopic suprapectoral biceps tenodesis in nine cadavers to open subpectoral biceps tenodesis in nine cadavers. They found that the arthroscopic suprapectoral biceps tenodesis group had a significantly decreased load to failure compared to the open subpectoral biceps tenodesis group. Additionally, the arthroscopic suprapectoral technique over-tensioned the biceps tendon. Despite these findings, other individuals did not know if there would be similar results in live patients. To further test this idea, Werner et al[132] compared thirty-two patients who underwent arthroscopic suprapectoral biceps tenodesis to fifty patients who underwent open subpectoral biceps tenodesis patients. There was no significant difference reported in Constant, ASES, Single Assessment Numeric Evaluation, Simple Shoulder Test (SST), LHB, and Veterans RAND 36-Item Health Survey scores. Furthermore, there were no range of motion or strength deficits in either group. These studies prove that regardless of associated complications for intra-articular, suprapectoral, and subpectoral biceps tenodesis placement, all three approaches have excellent and similar clinical outcomes.
Fixation strategies: The two types of fixations that can be used in intra-articular, suprapectoral, and subpectoral approaches include inlay and onlay. With inlay fixation, the biceps tendon is inserted perpendicularly into the bicipital groove. This technique is less technically challenging to perform, but can result in tenodesis failure in patients with poor tendon quality or osteoporosis at the screw insertion site[133,134]. For the onlay technique, the biceps tendon lays parallel to the bicipital groove. Onlay fixation with a suture anchor may be technically challenging and require longer operative times, but may have superior clinical and functional outcomes compared to the inlay technique[135,136].
Within inlay and onlay strategies, the different fixation techniques include interference screw and suture anchor, which are the most common, as well as cortical button and all-suture suture anchor constructs. Arthroscopic intra-articular biceps tenodesis has historically utilized an inlay technique in which the tendon is docked into a bone socket perpendicular to the bicipital groove and secured with an interference screw[113,137]. In open subpectoral tenodesis, the onlay technique is used with a suture anchor meant to heal the tendon to the cortical surface of the humerus[138-141].
The various types of interference screws include titanium, polyether ether ketone (PEEK), and bioresorbable screws. Titanium interference screws are infrequently used as they have an increased risk of tendon laceration during screw insertion and can make postoperative assessment challenging due to significant artifact on MRI[142,143]. PEEK interference screws have become more popular for several reasons: (1) They are chemically inert and insoluble; (2) They have a modulus of elasticity similar to human cortical bone; and (3) They are compatible with MRI and have a higher resistance to radiation[144,145]. Suture anchors require a smaller bone socket compared to interference screws and as previously mentioned secure the tendon to the humeral cortex. Furthermore, all-suture suture anchors allow for even less violation of the cortex.
While all constructs have been studied and proven to be effective, there is no consensus on which fixation strategy provides the most superior fixation[141,146-148]. In a study by Buchholz et al[147], researchers compared intramedullary cortical button fixation to interference screw usage and found similar results in regard to stiffness and ultimate failure loads. In Chiang et al[149], interference screws and all-suture suture anchors were found to have similar failure loads and stiffness which correlates to an increased likelihood of tenodesis failure. Likewise, Tashjian et al[141] found failure loads to be similar when comparing interference screws to dual-anchor all-suture suture anchors. Despite these results, additional studies have concluded contrary findings. In Richards et al[148], authors analyzed eleven cadaveric humerus specimens in which biceps tenodesis was performed with interference screw fixation or double suture anchor fixation. Authors reported consistent failure at the anchor or anchor eyelet in the suture anchor cadaver models and concluded that interference screw fixation had superior fixation strength. On the other hand, Golish et al[133] found interference screws to have a higher failure load and stiffness compared to all-suture suture anchors. With mixed results from these studies, there is no consensus on which fixation strategy provides the greatest advantage.
Supporters of the interference screw technique argue that it creates more surface area contact between the tendon and cancellous bone and thus results in greater exposure to marrow-derived endogenous stem cells[150-153]. However, this comes at a cost, as securing the tendon within a bone socket can result in local deformations in the tendon[140,154]. In Tan et al[150], researchers used a rabbit model of bicep tenodesis and compared tendon healing within the bone socket to healing on the cortical surface. Histologic analysis showed similar healing profiles between the two groups which allowed authors to conclude that the creation of large bone sockets with interference screws, which can lead to increased fracture risk, may be unnecessary. Furthermore, the interference screw technique has been associated with additional complications such as persistent pain and bioabsorbable screw reactions[119,155,156].
In contrast, all-suture suture anchors provide the benefits of conventional interference screws while being less traumatic to the bone and thus having a lower risk of fracture[157,158]. Frank et al[157] compared torsional energy in humeri that underwent biceps tenodesis with all-suture suture anchors to humeri that underwent biceps tenodesis with interference screws. They found that humeri in the all-suture suture anchor group required greater torsional energy to fracture suggesting that this construct creates less of a stress riser than the interference screw construct.
Although many studies have compared the biomechanical qualities of these constructs, few have compared differences in clinical outcomes. Park et al[140] compared clinical and anatomic outcomes of the interference screw and suture anchor fixation techniques for biceps tenodesis and found that both methods improved functional outcomes. Additionally, there was no difference in patient-reported outcomes measured by the visual analog scale (VAS) for pain, ASES score, SST, Constant score, Korean shoulder score, and LHB score between the two groups. With that said, the authors did find interference screw fixation and more physically demanding work levels to be associated with tenodesis failure. In another study by Millett et al[159], no statistically significant differences were reported at thirteen months postoperatively in VAS, ASES, and modified Constant scores between individuals who underwent biceps tenodesis with interference screw fixation and individuals who underwent biceps tenodesis with all-suture suture anchor fixation.
From the various biomechanical studies described above, the decision on which fixation strategy to utilize can be rather nuanced. While some studies have cited no differences in regards to stiffness or ultimate failure load between fixation strategies, other studies have contradicted these findings declaring interference screw fixation as more superior in terms of fixation strength and more inferior in regards to failure load and stiffness[133,141,147-149]. Despite the lack of consensus amongst the ideal fixation technique regarding biomechanical data, there appears to be no difference between fixation techniques in terms of clinical outcomes.
Biceps tenotomy vs biceps tenodesis: Several studies have investigated the differences between biceps tenotomy and biceps tenodesis, but mainly for LHB tendinopathy with rotator cuff tears, which makes it difficult to determine the extent to which biceps management influences outcomes[160-162]. A comparison of the techniques can be found in Table 1. In a systematic review by Leroux et al[160], authors analyzed patients who underwent rotator cuff repair in combination with either biceps tenotomy or biceps tenodesis. They reported that patients who underwent biceps tenodesis had better Constant assessment scores (92.8 [tenodesis] vs 90.6 [tenotomy], P < 0.01) and decreased rates of biceps deformity compared to patients who underwent biceps tenotomy (3.8% [tenodesis] vs 15.5% [tenotomy], P < 0.01).
Another study compared the clinical results of biceps tenotomy and biceps tenodesis based on technique. In Shank et al[163], seventeen patients underwent biceps tenotomy, nineteen patients underwent suprapectoral biceps tenodesis with a double-loaded anchor fixation, and thirty-one control patients did not have any biceps surgery performed. Analysis showed no significant difference in either forearm supination nor elbow flexion strength among patients in all three groups.
One theory that has been challenged recently is the duration of postoperative rehabilitation. Zabrzyński et al[164] attempted to test different rehabilitation protocols in tenotomy vs tenodesis groups with the tenotomy group undergoing a personalized postoperative rehabilitation protocol. They found that patients who underwent tenotomy with a shortened postoperative rehabilitation protocol were able to achieve better clinical outcomes and ensure faster return to sports activity compared to those who underwent tenodesis[164].
The results described above demonstrate how challenging it can be to make direct comparisons between tenotomy and tenodesis in hopes of determining which is superior. Furthermore, the concern for cosmesis plays a role in determining whether a patient should undergo tenotomy or tenodesis. Typically, tenotomy is indicated in older patients as cosmesis is of minimal concern whereas tenodesis is indicated in younger more active patients where cosmesis tends to play a more significant role. Recent systematic reviews and meta-analyses by MacDonald et al[165], Zhou et al[166], and Kooistra et al[167] confirm the findings that there is no evidence-based difference in LHB tenodesis vs tenotomy when evaluating shoulder function, pain, or biceps-related strength.
SLAP lesion: Treatment recommendations for SLAP lesions are based on patient age as well as activity level and include nonsurgical management, arthroscopic debridement, arthroscopic repair, and biceps tenodesis. Over the last five years, orthopaedic literature has documented the growing trend to move away from SLAP repair due to an increased incidence of subsequent revision surgery[168,169]. Instead, literature has shown an increase in the frequency of biceps tenodesis, particularly in patients over the age of forty and athletes as return to activity after biceps tenodesis was significantly higher than the rate after revision SLAP repair[170,171].
SLAP tears are often categorized into Type I through Type X[172]. In a type II SLAP lesion, there is detachment of the superior labrum and the origin of the LHBT insertion from the glenoid[173,174]. Surgical techniques that can be used to repair a standard type II SLAP lesion include the use of a single suture anchor placed posterior to the biceps anchor or the use of two suture anchors with one suture anchor placed anterior and the other placed posterior to the biceps anchor[17]. A few studies have reported on outcomes regarding type II SLAP repair. Sayde et al included 506 patients who underwent repair of type II SLAP tear and reported excellent satisfaction in 83% of patients and return to previous level of play in 73% of patients; however, in the 198 patients who were overhead athletes, inferior outcomes were reported with only 63% able to return to previous level of play. Similar studies have assessed the outcomes of overhead athletes who have undergone arthroscopic SLAP lesion repair and report a return to preinjury level of sports activity between 22% and 85%[175-178]. In Frank et al[179], sixty-two patients underwent arthroscopic repair of a type II SLAP tear. Authors reported that patients aged twenty years and younger as well as overhead throwers were more likely to require revision surgery than patients greater than twenty years of age and non-overhead throwers. Furthermore, they concluded that patients greater than forty years of age were more likely to have inferior postoperative ASES scores compared to patients aged less than forty years of age.
An increasingly popular alternative to arthroscopic repair of SLAP lesions is biceps tenodesis as it has a significantly higher rate of return to activity following surgery[170,171]. Some studies have performed biceps tenodesis in combination with SLAP repair or performed biceps tenodesis in place of SLAP repair. For example, Boileau et al[1] compared ten patients with an isolated type II SLAP lesion who underwent repair with the use of suture anchors to fifteen patients with an isolated type II SLAP lesion who underwent arthroscopic biceps tenodesis with the use of an absorbable interference screw. Patients in the SLAP repair group had inferior outcomes including lower mean Constant assessment scores, lower satisfaction, and lower return to previous level of sports activity. On the other hand, some studies have reported similar outcomes in patients with a type II SLAP tear who undergo biceps tenodesis. In Denard et al[2], thirty-seven patients greater than thirty-five years of age with an isolated type II SLAP tear underwent arthroscopic biceps tenodesis or SLAP repair. Authors demonstrated that patients in the biceps tenodesis group had shorter postoperative recovery, higher satisfaction rates, and higher rates of return to normal activity. Similarly, Ek et al[3] compared twenty-five patients with an isolated type II SLAP lesion who underwent biceps tenodesis or SLAP repair and found that both groups had improved clinical outcomes with low failure rates and similar rates of return to sports. These studies demonstrate that patients who undergo biceps tenodesis for SLAP lesions experience a shorter postoperative recovery time, higher Constant assessment scores, higher satisfaction rates, higher rates of return to normal sports activity, and lower failure rates compared to patients who undergo SLAP repair.
While type II SLAP tears have seen an increase in biceps tenodesis as treatment, type III and type IV SLAP tears can be adequately treated with SLAP repair depending on the extent of the injury[172]. In a type III SLAP tear, a bucket-handle tear of the superior labrum occurs with potential displacement of the mobile labral fragment into the glenohumeral joint. In this case, the attachment of LHBT remains intact. Typically, type III SLAP lesions require resection of the unstable bucket-handle fragment with no further stabilization of the biceps anchor[172,180]. Some authors have also recommended refixation of the torn flap analogous to meniscal tears if the lesion is caused by trauma and located within a specific part of the shoulder[181]. For a type IV SLAP tear, there is a bucket-handle tear of the superior labrum that extends to the biceps tendon in a variable degree. Type IV SLAP lesion repair is reliant on biceps tendon stability after resection of the torn flap as at least half of the tendon should be intact to preserve stability of the labro-bicipital complex[172]. In an unstable biceps tendon where more than 50% of the tendon is affected, a tenotomy or tenodesis is preferred over a SLAP repair. With SLAP repairs demonstrating a wide variability in outcomes, specifically in rates of return to play and failure rates for older individuals, biceps tenodesis has shown a significant improvement in ASES scores and VAS scores[182].
The excellent outcomes and low rate of complications of biceps tenodesis for SLAP lesions have led to an increase in frequency of biceps tenodesis[119,183]. In a study by Patterson et al[4], trends in the management of SLAP lesions were reviewed and the proportion of SLAP repairs between 2002 and 2011 decreased from 69.3% to 44.8%, whereas the proportion of biceps tenodesis procedures increased from 1.9% to 18.8%. Furthermore, the proportion of SLAP repairs used to manage SLAP lesions in combination with rotator cuff repair decreased from 60.2% to 15.3%, whereas the proportion of biceps tenodesis or tenotomy procedures increased from 6% to 28%. In a more recent study by Cvetanovich et al[171], there was a 69.3% decrease in isolated SLAP repair from 2007 to 2016 and an increase of 370% in biceps tenodesis for the diagnosis of an isolated SLAP tear over the same period. With this knowledge, Chalmers et al[184] conducted a study with three groups: (1) Forty-five patients with a SLAP tear who underwent isolated SLAP repair; (2) Twenty-three patients with a SLAP tear who underwent isolated biceps tenodesis; and (3) Eighteen patients with a SLAP tear who underwent SLAP repair in combination with biceps tenodesis. Authors reported substantially worse postoperative ASES scores and visual analog scale pain scores in patients who underwent SLAP repair in combination with biceps tenodesis compared to either of the other categories. These studies demonstrate the utility and improved clinical outcomes in patients with SLAP lesions who undergo biceps tenodesis compared to patients with SLAP lesions who undergo arthroscopic repair. Furthermore, improved outcomes seen in biceps tenodesis for SLAP tears is supported by the increase in volume of biceps tenodesis procedures over the last five years or so.
CONCLUSION
LHBT is a common source of disease and shoulder pain with etiologies including inflammation, instability, and trauma. Although the anatomy can be easily digested, the decision to operate is a little more nuanced. Despite various physical examination maneuvers, the lack of specificity requires orthopaedic surgeons to rely on patient history as well as advanced imaging in order to best manage the patient’s condition. Nonsurgical treatment typically includes physical therapy, anti-inflammatory medications, and ultrasound-guided corticosteroid injections. If nonsurgical treatment fails, surgical techniques such as biceps tenotomy, biceps tenodesis, or SLAP repair can be used. In biceps tenodesis, differences between arthroscopic and open biceps tenodesis, type of fixation system, and location of tenodesis should be discussed with patients keeping in mind that no functional differences have been established. Furthermore, SLAP lesions can be treated with SLAP repair or biceps tenodesis depending on the categorization. While debridement has been used as the standard of treatment in the past for SLAP lesions, the increase in volume of biceps tenodesis for SLAP lesions indicates a transition to a treatment option with better functional and clinical outcomes.
Footnotes
Conflict-of-interest statement: Simon P Lalehzarian, Avinesh Agarwalla, and Joseph N Liu have no conflicts of interest to report.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: April 28, 2021
First decision: July 28, 2021
Article in press: December 25, 2021
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zabrzyński J S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
Contributor Information
Simon P Lalehzarian, The Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, IL 60064, United States.
Avinesh Agarwalla, Department of Orthopedic Surgery, Westchester Medical Center, Valhalla, NY 10595, United States.
Joseph N Liu, USC Epstein Family Center for Sports Medicine, Keck Medicine of USC, Los Angeles, CA 90033, United States. joseph.liu@med.usc.edu.
References
- 1.Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37:929–936. doi: 10.1177/0363546508330127. [DOI] [PubMed] [Google Scholar]
- 2.Denard PJ, Lädermann A, Parsley BK, Burkhart SS. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37:e292–e297. doi: 10.3928/01477447-20140225-63. [DOI] [PubMed] [Google Scholar]
- 3.Ek ET, Shi LL, Tompson JD, Freehill MT, Warner JJ. Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tenodesis. J Shoulder Elbow Surg. 2014;23:1059–1065. doi: 10.1016/j.jse.2013.09.030. [DOI] [PubMed] [Google Scholar]
- 4.Patterson BM, Creighton RA, Spang JT, Roberson JR, Kamath GV. Surgical Trends in the Treatment of Superior Labrum Anterior and Posterior Lesions of the Shoulder: Analysis of Data From the American Board of Orthopaedic Surgery Certification Examination Database. Am J Sports Med. 2014;42:1904–1910. doi: 10.1177/0363546514534939. [DOI] [PubMed] [Google Scholar]
- 5.Krupp RJ, Kevern MA, Gaines MD, Kotara S, Singleton SB. Long head of the biceps tendon pain: differential diagnosis and treatment. J Orthop Sports Phys Ther. 2009;39:55–70. doi: 10.2519/jospt.2009.2802. [DOI] [PubMed] [Google Scholar]
- 6.Frank RM, Cotter EJ, Strauss EJ, Jazrawi LM, Romeo AA. Management of Biceps Tendon Pathology: From the Glenoid to the Radial Tuberosity. J Am Acad Orthop Surg. 2018;26:e77–e89. doi: 10.5435/JAAOS-D-17-00085. [DOI] [PubMed] [Google Scholar]
- 7.Hassan S, Patel V. Biceps tenodesis versus biceps tenotomy for biceps tendinitis without rotator cuff tears. J Clin Orthop Trauma. 2019;10:248–256. doi: 10.1016/j.jcot.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel KV, Bravman J, Vidal A, Chrisman A, McCarty E. Biceps Tenotomy Versus Tenodesis. Clin Sports Med. 2016;35:93–111. doi: 10.1016/j.csm.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Blum K, Chen AL, Chen TJ, Waite RL, Downs BW, Braverman ER, Kerner MM, Savarimuthu SM, DiNubile N. Repetitive H-wave device stimulation and program induces significant increases in the range of motion of post operative rotator cuff reconstruction in a double-blinded randomized placebo controlled human study. BMC Musculoskelet Disord. 2009;10:132. doi: 10.1186/1471-2474-10-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miniato MA, Anand P, Varacallo M. Anatomy, Shoulder and Upper Limb, Shoulder. [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536933/
- 11.Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581–592. doi: 10.1016/j.arthro.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Vangsness CT Jr, Jorgenson SS, Watson T, Johnson DL. The origin of the long head of the biceps from the scapula and glenoid labrum. An anatomical study of 100 shoulders. J Bone Joint Surg Br. 1994;76:951–954. [PubMed] [Google Scholar]
- 13.Habermeyer P, Magosch P, Lichtenberg S. Chapter 6: Classifications of pathology of long head of the biceps tendon. In: Habermeyer P, Magosch P, Lichtenberg S. Classifications and Scores of the Shoulder. Springer-Verlag Berlin Heidelberg, 2006: 35-47. [Google Scholar]
- 14.Walch G, Nové-Josserand L, Boileau P, Levigne C. Subluxations and dislocations of the tendon of the long head of the biceps. J Shoulder Elbow Surg. 1998;7:100–108. doi: 10.1016/s1058-2746(98)90218-x. [DOI] [PubMed] [Google Scholar]
- 15.Vap AR, Katthagen JC, Tahal DS, Horan MP, Fritz EM, Pogorzelski J, Millett PJ. Isolated Biceps Reflection Pulley Tears Treated With Subpectoral Biceps Tenodesis: Minimum 2-Year Outcomes. Arthroscopy. 2017;33:1788–1794. doi: 10.1016/j.arthro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 16.Sanders B, Lavery KP, Pennington S, Warner JJ. Clinical success of biceps tenodesis with and without release of the transverse humeral ligament. J Shoulder Elbow Surg. 2012;21:66–71. doi: 10.1016/j.jse.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 17.Thorsness RJ, Romeo AA. Diagnosis and Management of the Biceps-Labral Complex. Instr Course Lect. 2017;66:65–77. [PubMed] [Google Scholar]
- 18.Taylor SA, Khair MM, Gulotta LV, Pearle AD, Baret NJ, Newman AM, Dy CJ, O'Brien SJ. Diagnostic glenohumeral arthroscopy fails to fully evaluate the biceps-labral complex. Arthroscopy. 2015;31:215–224. doi: 10.1016/j.arthro.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 19.Taylor SA, Fabricant PD, Bansal M, Khair MM, McLawhorn A, DiCarlo EF, Shorey M, O'Brien SJ. The anatomy and histology of the bicipital tunnel of the shoulder. J Shoulder Elbow Surg. 2015;24:511–519. doi: 10.1016/j.jse.2014.09.026. [DOI] [PubMed] [Google Scholar]
- 20.Taylor SA, Newman AM, Dawson C, Gallagher KA, Bowers A, Nguyen J, Fabricant PD, O'Brien SJ. The "3-Pack" Examination Is Critical for Comprehensive Evaluation of the Biceps-Labrum Complex and the Bicipital Tunnel: A Prospective Study. Arthroscopy. 2017;33:28–38. doi: 10.1016/j.arthro.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 21.Kumar VP, Satku K, Balasubramaniam P. The role of the long head of biceps brachii in the stabilization of the head of the humerus. Clin Orthop Relat Res. 1989:172–175. [PubMed] [Google Scholar]
- 22.Pagnani MJ, Deng XH, Warren RF, Torzilli PA, O'Brien SJ. Role of the long head of the biceps brachii in glenohumeral stability: a biomechanical study in cadavera. J Shoulder Elbow Surg. 1996;5:255–262. doi: 10.1016/s1058-2746(96)80051-6. [DOI] [PubMed] [Google Scholar]
- 23.Warner JJ, Bowen MK, Deng X, Torzilli PA, Warren RF. Effect of joint compression on inferior stability of the glenohumeral joint. J Shoulder Elbow Surg. 1999;8:31–36. doi: 10.1016/s1058-2746(99)90051-4. [DOI] [PubMed] [Google Scholar]
- 24.Yamaguchi K, Riew KD, Galatz LM, Syme JA, Neviaser RJ. Biceps activity during shoulder motion: an electromyographic analysis. Clin Orthop Relat Res. 1997:122–129. doi: 10.1097/00003086-199703000-00017. [DOI] [PubMed] [Google Scholar]
- 25.Levy AS, Kelly BT, Lintner SA, Osbahr DC, Speer KP. Function of the long head of the biceps at the shoulder: electromyographic analysis. J Shoulder Elbow Surg. 2001;10:250–255. doi: 10.1067/mse.2001.113087. [DOI] [PubMed] [Google Scholar]
- 26.Wittstein J, Queen R, Abbey A, Moorman CT 3rd. Isokinetic testing of biceps strength and endurance in dominant versus nondominant upper extremities. J Shoulder Elbow Surg. 2010;19:874–877. doi: 10.1016/j.jse.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 27.Edwards TB, Walch G, Sirveaux F, Molé D, Nové-Josserand L, Boulahia A, Neyton L, Szabo I, Lindgren B. Repair of tears of the subscapularis. J Bone Joint Surg Am. 2005;87:725–730. doi: 10.2106/JBJS.D.02051. [DOI] [PubMed] [Google Scholar]
- 28.Boileau P, Baqué F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 29.Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. No advantages in repairing a type II superior labrum anterior and posterior (SLAP) lesion when associated with rotator cuff repair in patients over age 50: a randomized controlled trial. Am J Sports Med. 2008;36:247–253. doi: 10.1177/0363546507308194. [DOI] [PubMed] [Google Scholar]
- 30.Osbahr DC, Diamond AB, Speer KP. The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis. Arthroscopy. 2002;18:483–487. doi: 10.1053/jars.2002.32233. [DOI] [PubMed] [Google Scholar]
- 31.Vestermark GL, Van Doren BA, Connor PM, Fleischli JE, Piasecki DP, Hamid N. The prevalence of rotator cuff pathology in the setting of acute proximal biceps tendon rupture. J Shoulder Elbow Surg. 2018;27:1258–1262. doi: 10.1016/j.jse.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 32.Hsu SH, Miller SL, Curtis AS. Long head of biceps tendon pathology: management alternatives. Clin Sports Med. 2008;27:747–762. doi: 10.1016/j.csm.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 33.Barber FA, Field LD, Ryu RK. Biceps tendon and superior labrum injuries: decision making. Instr Course Lect. 2008;57:527–538. [PubMed] [Google Scholar]
- 34.Nho SJ, Frank RM, Reiff SN, Verma NN, Romeo AA. Arthroscopic repair of anterosuperior rotator cuff tears combined with open biceps tenodesis. Arthroscopy. 2010;26:1667–1674. doi: 10.1016/j.arthro.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 35.Habermeyer P, Magosch P, Pritsch M, Scheibel MT, Lichtenberg S. Anterosuperior impingement of the shoulder as a result of pulley lesions: a prospective arthroscopic study. J Shoulder Elbow Surg. 2004;13:5–12. doi: 10.1016/j.jse.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 36.Hwang E, Carpenter JE, Hughes RE, Palmer ML. Effects of biceps tension and superior humeral head translation on the glenoid labrum. J Orthop Res. 2014;32:1424–1429. doi: 10.1002/jor.22688. [DOI] [PubMed] [Google Scholar]
- 37.Verma NN, Drakos M, O'Brien SJ. The arthroscopic active compression test. Arthroscopy. 2005;21:634. doi: 10.1016/j.arthro.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 38.Byram IR, Dunn WR, Kuhn JE. Humeral head abrasion: an association with failed superior labrum anterior posterior repairs. J Shoulder Elbow Surg. 2011;20:92–97. doi: 10.1016/j.jse.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 39.Boileau P, Ahrens PM, Hatzidakis AM. Entrapment of the long head of the biceps tendon: the hourglass biceps--a cause of pain and locking of the shoulder. J Shoulder Elbow Surg. 2004;13:249–257. doi: 10.1016/j.jse.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 40.Mazzocca AD, McCarthy MB, Ledgard FA, Chowaniec DM, McKinnon WJ Jr, Delaronde S, Rubino LJ, Apolostakos J, Romeo AA, Arciero RA, Beitzel K. Histomorphologic changes of the long head of the biceps tendon in common shoulder pathologies. Arthroscopy. 2013;29:972–981. doi: 10.1016/j.arthro.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 41.Gerber C, Galantay RV, Hersche O. The pattern of pain produced by irritation of the acromioclavicular joint and the subacromial space. J Shoulder Elbow Surg. 1998;7:352–355. doi: 10.1016/s1058-2746(98)90022-2. [DOI] [PubMed] [Google Scholar]
- 42.Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9:382–385. doi: 10.1067/mse.2000.108386. [DOI] [PubMed] [Google Scholar]
- 43.Chen CH, Hsu KY, Chen WJ, Shih CH. Incidence and severity of biceps long head tendon lesion in patients with complete rotator cuff tears. J Trauma. 2005;58:1189–1193. doi: 10.1097/01.ta.0000170052.84544.34. [DOI] [PubMed] [Google Scholar]
- 44.Gurnani N, van Deurzen DF, Janmaat VT, van den Bekerom MP. Tenotomy or tenodesis for pathology of the long head of the biceps brachii: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24:3765–3771. doi: 10.1007/s00167-015-3640-6. [DOI] [PubMed] [Google Scholar]
- 45.Varacallo M, Seaman TJ, Mair SD. Biceps Tendon Dislocation and Instability. [Updated 2021 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534102/ [PubMed]
- 46.Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644–654. doi: 10.1016/s1058-2746(99)90105-2. [DOI] [PubMed] [Google Scholar]
- 47.Jain NB, Wilcox RB 3rd, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R. 2013;5:45–56. doi: 10.1016/j.pmrj.2012.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.José AG, Luís Felipe HFS, Gabriel RSM, Fernando MI. Treatment of the Distal Biceps Brachii Tendon Rupture Using the Three Mini-Incisions Technique: Evaluation through MEPS and DASH. Ortho Rheum Open Access J. 2019;14:555888. [Google Scholar]
- 49.Ding DY, Garofolo G, Lowe D, Strauss EJ, Jazrawi LM. The biceps tendon: from proximal to distal: AAOS exhibit selection. J Bone Joint Surg Am. 2014;96:e176. doi: 10.2106/JBJS.N.00032. [DOI] [PubMed] [Google Scholar]
- 50.Matsen FA 3rd, Kirby RM. Office evaluation and management of shoulder pain. Orthop Clin North Am. 1982;13:453–475. [PubMed] [Google Scholar]
- 51.Chalmers PN, Verma NN. Proximal Biceps in Overhead Athletes. Clin Sports Med. 2016;35:163–179. doi: 10.1016/j.csm.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 52.Gill HS, El Rassi G, Bahk MS, Castillo RC, McFarland EG. Physical examination for partial tears of the biceps tendon. Am J Sports Med. 2007;35:1334–1340. doi: 10.1177/0363546507300058. [DOI] [PubMed] [Google Scholar]
- 53.Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg Am. 1995;77:366–372. doi: 10.2106/00004623-199503000-00006. [DOI] [PubMed] [Google Scholar]
- 54.Holtby R, Razmjou H. Accuracy of the Speed's and Yergason's tests in detecting biceps pathology and SLAP lesions: comparison with arthroscopic findings. Arthroscopy. 2004;20:231–236. doi: 10.1016/j.arthro.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 55.Parentis MA, Glousman RE, Mohr KS, Yocum LA. An evaluation of the provocative tests for superior labral anterior posterior lesions. Am J Sports Med. 2006;34:265–268. doi: 10.1177/0363546505279911. [DOI] [PubMed] [Google Scholar]
- 56.Nho SJ, Strauss EJ, Lenart BA, Provencher MT, Mazzocca AD, Verma NN, Romeo AA. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18:645–656. doi: 10.5435/00124635-201011000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Myer CA, Hegedus EJ, Tarara DT, Myer DM. A user's guide to performance of the best shoulder physical examination tests. Br J Sports Med. 2013;47:903–907. doi: 10.1136/bjsports-2012-091870. [DOI] [PubMed] [Google Scholar]
- 58.O'Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med. 1998;26:610–613. doi: 10.1177/03635465980260050201. [DOI] [PubMed] [Google Scholar]
- 59.Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, Wright AA. Which physical examination tests provide clinicians with the most value when examining the shoulder? Br J Sports Med. 2012;46:964–978. doi: 10.1136/bjsports-2012-091066. [DOI] [PubMed] [Google Scholar]
- 60.Cheung E, O’Driscoll , SW . The dynamic labral shear test for superior labral anterior to posterior tears of the shoulder. Paper presented at: AAOS annual meeting; February 2007; San Diego, CA. [Google Scholar]
- 61.Ben Kibler W, Sciascia AD, Hester P, Dome D, Jacobs C. Clinical utility of traditional and new tests in the diagnosis of biceps tendon injuries and superior labrum anterior and posterior lesions in the shoulder. Am J Sports Med. 2009;37:1840–1847. doi: 10.1177/0363546509332505. [DOI] [PubMed] [Google Scholar]
- 62.Cook C, Beaty S, Kissenberth MJ, Siffri P, Pill SG, Hawkins RJ. Diagnostic accuracy of five orthopedic clinical tests for diagnosis of superior labrum anterior posterior (SLAP) lesions. J Shoulder Elbow Surg. 2012;21:13–22. doi: 10.1016/j.jse.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 63.Keener JD, Brophy RH. Superior labral tears of the shoulder: pathogenesis, evaluation, and treatment. J Am Acad Orthop Surg. 2009;17:627–637. doi: 10.5435/00124635-200910000-00005. [DOI] [PubMed] [Google Scholar]
- 64.Knesek M, Skendzel JG, Dines JS, Altchek DW, Allen AA, Bedi A. Diagnosis and management of superior labral anterior posterior tears in throwing athletes. Am J Sports Med. 2013;41:444–460. doi: 10.1177/0363546512466067. [DOI] [PubMed] [Google Scholar]
- 65.Virk MS, Arciero RA. Superior labrum anterior to posterior tears and glenohumeral instability. Instr Course Lect. 2013;62:501–514. [PubMed] [Google Scholar]
- 66.Taylor SA, Newman AM, Nguyen J, Fabricant PD, Baret NJ, Shorey M, Ramkumar P, O'Brien SJ. Magnetic Resonance Imaging Currently Fails to Fully Evaluate the Biceps-Labrum Complex and Bicipital Tunnel. Arthroscopy. 2016;32:238–244. doi: 10.1016/j.arthro.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 67.Mohtadi NG, Vellet AD, Clark ML, Hollinshead RM, Sasyniuk TM, Fick GH, Burton PJ. A prospective, double-blind comparison of magnetic resonance imaging and arthroscopy in the evaluation of patients presenting with shoulder pain. J Shoulder Elbow Surg. 2004;13:258–265. doi: 10.1016/j.jse.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 68.Houtz CG, Schwartzberg RS, Barry JA, Reuss BL, Papa L. Shoulder MRI accuracy in the community setting. J Shoulder Elbow Surg. 2011;20:537–542. doi: 10.1016/j.jse.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 69.Reuss BL, Schwartzberg R, Zlatkin MB, Cooperman A, Dixon JR. Magnetic resonance imaging accuracy for the diagnosis of superior labrum anterior-posterior lesions in the community setting: eighty-three arthroscopically confirmed cases. J Shoulder Elbow Surg. 2006;15:580–585. doi: 10.1016/j.jse.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 70.Dubrow SA, Streit JJ, Shishani Y, Robbin MR, Gobezie R. Diagnostic accuracy in detecting tears in the proximal biceps tendon using standard nonenhancing shoulder MRI. Open Access J Sports Med. 2014;5:81–87. doi: 10.2147/OAJSM.S58225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gagat M, Zabrzyńska A, Zabrzyńska M, Zielińska W. The advances in diagnostic modalities of disorders of the long head of the biceps tendon-review. Med Stud Stud Med. 2021;37:83–90. [Google Scholar]
- 72.Zabrzyński J, Paczesny Ł, Zabrzyńska A, Grzanka D, Łapaj Ł. Sonography in the instability of the long head of the biceps tendon confronted with histopathologic and arthroscopic findings. Folia Morphol (Warsz) 2018;77:583–590. doi: 10.5603/FM.a2018.0012. [DOI] [PubMed] [Google Scholar]
- 73.Armstrong A, Teefey SA, Wu T, Clark AM, Middleton WD, Yamaguchi K, Galatz LM. The efficacy of ultrasound in the diagnosis of long head of the biceps tendon pathology. J Shoulder Elbow Surg. 2006;15:7–11. doi: 10.1016/j.jse.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 74.Skendzel JG, Jacobson JA, Carpenter JE, Miller BS. Long head of biceps brachii tendon evaluation: accuracy of preoperative ultrasound. AJR Am J Roentgenol. 2011;197:942–948. doi: 10.2214/AJR.10.5012. [DOI] [PubMed] [Google Scholar]
- 75.Stone TJ, Adler RS. Ultrasound-Guided Biceps Peritendinous Injections in the Absence of a Distended Tendon Sheath: A Novel Rotator Interval Approach. J Ultrasound Med. 2015;34:2287–2292. doi: 10.7863/ultra.15.02017. [DOI] [PubMed] [Google Scholar]
- 76.Gofeld M, Hurdle MF, Agur A. Biceps Tendon Sheath Injection: An Anatomical Conundrum. Pain Med. 2019;20:138–142. doi: 10.1093/pm/pny051. [DOI] [PubMed] [Google Scholar]
- 77.Lenz R, Kieb M, Diehl P, Grim C, Vogt S, Tischer T. Muscle, tendon and joint injections : What is the evidence? Orthopade. 2016;45:459–468. doi: 10.1007/s00132-016-3262-9. [DOI] [PubMed] [Google Scholar]
- 78.Barile A, La Marra A, Arrigoni F, Mariani S, Zugaro L, Splendiani A, Di Cesare E, Reginelli A, Zappia M, Brunese L, Duka E, Carrafiello G, Masciocchi C. Anaesthetics, steroids and platelet-rich plasma (PRP) in ultrasound-guided musculoskeletal procedures. Br J Radiol. 2016;89:20150355. doi: 10.1259/bjr.20150355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Unverferth LJ, Olix ML. The effect of local steroid injections on tendon. J Sports Med. 1973;1:31–37. doi: 10.1177/036354657300100404. [DOI] [PubMed] [Google Scholar]
- 80.Hashiuchi T, Sakurai G, Morimoto M, Komei T, Takakura Y, Tanaka Y. Accuracy of the biceps tendon sheath injection: ultrasound-guided or unguided injection? J Shoulder Elbow Surg. 2011;20:1069–1073. doi: 10.1016/j.jse.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 81.Schickendantz M, King D. Nonoperative Management (Including Ultrasound-Guided Injections) of Proximal Biceps Disorders. Clin Sports Med. 2016;35:57–73. doi: 10.1016/j.csm.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 82.Nichols AW. Complications associated with the use of corticosteroids in the treatment of athletic injuries. Clin J Sport Med. 2005;15:370–375. doi: 10.1097/01.jsm.0000179233.17885.18. [DOI] [PubMed] [Google Scholar]
- 83.Yiannakopoulos CK, Megaloikonomos PD, Foufa K, Gliatis J. Ultrasound-guided versus palpation-guided corticosteroid injections for tendinosis of the long head of the biceps: A randomized comparative study. Skeletal Radiol. 2020;49:585–591. doi: 10.1007/s00256-019-03315-9. [DOI] [PubMed] [Google Scholar]
- 84.Hart L. Corticosteroid and other injections in the management of tendinopathies: a review. Clin J Sport Med. 2011;21:540–541. doi: 10.1097/01.jsm.0000407929.35973.b9. [DOI] [PubMed] [Google Scholar]
- 85.Daniels EW, Cole D, Jacobs B, Phillips SF. Existing Evidence on Ultrasound-Guided Injections in Sports Medicine. Orthop J Sports Med. 2018;6:2325967118756576. doi: 10.1177/2325967118756576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Childress MA, Beutler A. Management of chronic tendon injuries. Am Fam Physician. 2013;87:486–490. [PubMed] [Google Scholar]
- 87.Andres BM, Murrell GA. Treatment of tendinopathy: what works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008;466:1539–1554. doi: 10.1007/s11999-008-0260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Moon JG. Clinical Application of Radial Head Prosthesis. Clin Shoulder Elbow. 2011;14:140–145. [Google Scholar]
- 89.Pogorzelski J, Fritz EM, Godin JA, Imhoff AB, Millett PJ. Nonoperative treatment of five common shoulder injuries: A critical analysis. Obere Extrem. 2018;13:89–97. doi: 10.1007/s11678-018-0449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Barber FA, Byrd JW, Wolf EM, Burkhart SS. How would you treat the partially torn biceps tendon? Arthroscopy. 2001;17:636–639. doi: 10.1053/jars.2001.24852. [DOI] [PubMed] [Google Scholar]
- 91.Gill TJ, McIrvin E, Mair SD, Hawkins RJ. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg. 2001;10:247–249. doi: 10.1067/mse.2001.114259. [DOI] [PubMed] [Google Scholar]
- 92.Kelly AM, Drakos MC, Fealy S, Taylor SA, O'Brien SJ. Arthroscopic release of the long head of the biceps tendon: functional outcome and clinical results. Am J Sports Med. 2005;33:208–213. doi: 10.1177/0363546504269555. [DOI] [PubMed] [Google Scholar]
- 93.Farmer KW, Wright TW. Shoulder arthroscopy: the basics. J Hand Surg Am. 2015;40:817–821. doi: 10.1016/j.jhsa.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 94.Lemos D, Esquivel A, Duncan D, Marsh S, Lemos S. Outlet biceps tenodesis: a new technique for treatment of biceps long head tendon injury. Arthrosc Tech. 2013;2:e83–e88. doi: 10.1016/j.eats.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Narvani AA, Atoun E, Van Tongel A, Sforza G, Levy O. The "anchor shape" technique for long head of the biceps tenotomy to avoid the popeye deformity. Arthrosc Tech. 2013;2:e167–e170. doi: 10.1016/j.eats.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cho NS, Cha SW, Rhee YG. Funnel tenotomy versus intracuff tenodesis for lesions of the long head of the biceps tendon associated with rotator cuff tears. Am J Sports Med. 2014;42:1161–1168. doi: 10.1177/0363546514523719. [DOI] [PubMed] [Google Scholar]
- 97.Goubier JN, Bihel T, Dubois E, Teboul F. Loop biceps tenotomy: an arthroscopic technique for long head of biceps tenotomy. Arthrosc Tech. 2014;3:e427–e430. doi: 10.1016/j.eats.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zalneraitis BH, Milam BP, Turner EK, Gasbarro G, Galvin JW. Biceps Squeeze Tenotomy: Technique to Improve Efficiency of Arthroscopic Biceps Tenotomy. Arthrosc Tech. 2020;9:e1851–e1853. doi: 10.1016/j.eats.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Corpus KT, Garcia GH, Liu JN, Dines DM, O'Brien SJ, Dines JS, Taylor SA. Long Head of Biceps Tendon Management: a Survey of the American Shoulder and Elbow Surgeons. HSS J. 2018;14:34–40. doi: 10.1007/s11420-017-9575-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Abraham VT, Tan BH, Kumar VP. Systematic Review of Biceps Tenodesis: Arthroscopic Versus Open. Arthroscopy. 2016;32:365–371. doi: 10.1016/j.arthro.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 101.Harris JD. Editorial Commentary: Open Versus Arthroscopic Biceps Tenodesis--You Choose. Arthroscopy. 2016;32:372–373. doi: 10.1016/j.arthro.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 102.Hurley DJ, Hurley ET, Pauzenberger L, Lim Fat D, Mullett H. Open Compared with Arthroscopic Biceps Tenodesis: A Systematic Review. JBJS Rev. 2019;7:e4. doi: 10.2106/JBJS.RVW.18.00086. [DOI] [PubMed] [Google Scholar]
- 103.Yeung M, Shin JJ, Lesniak BP, Lin A. Complications of Arthroscopic Versus Open Biceps Tenodesis in the Setting of Arthroscopic Rotator Cuff Repairs: An Analysis of the American Board of Orthopaedic Surgery Database. J Am Acad Orthop Surg. 2020;28:113–120. doi: 10.5435/JAAOS-D-19-00252. [DOI] [PubMed] [Google Scholar]
- 104.DeFroda SF, Li L, Milner J, Bokshan SL, Owens BD. Cost comparison of arthroscopic rotator cuff repair with arthroscopic vs. open biceps tenodesis. J Shoulder Elbow Surg. 2021;30:340–345. doi: 10.1016/j.jse.2020.05.031. [DOI] [PubMed] [Google Scholar]
- 105.Tu J, Xu B, Guo R. Open subpectoral vs. arthroscopic proximal biceps tenodesis: A comparison study of clinical outcomes. Exp Ther Med. 2020;19:428–434. doi: 10.3892/etm.2019.8232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mazzocca AD, Cote MP, Arciero CL, Romeo AA, Arciero RA. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36:1922–1929. doi: 10.1177/0363546508318192. [DOI] [PubMed] [Google Scholar]
- 107.Schoch C, Geyer M, Drews B. Suprapectoral biceps tenodesis using a suture plate: clinical results after 2 years. Arch Orthop Trauma Surg. 2017;137:829–835. doi: 10.1007/s00402-017-2664-4. [DOI] [PubMed] [Google Scholar]
- 108.Tahal DS, Katthagen JC, Vap AR, Horan MP, Millett PJ. Subpectoral Biceps Tenodesis for Tenosynovitis of the Long Head of the Biceps in Active Patients Younger Than 45 Years Old. Arthroscopy. 2017;33:1124–1130. doi: 10.1016/j.arthro.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 109.Ng CY, Funk L. Symptomatic chronic long head of biceps rupture: Surgical results. Int J Shoulder Surg. 2012;6:108–111. doi: 10.4103/0973-6042.106222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Euler SA, Horan MP, Ellman MB, Greenspoon JA, Millett PJ. Chronic rupture of the long head of the biceps tendon: comparison of 2-year results following primary versus revision open subpectoral biceps tenodesis. Arch Orthop Trauma Surg. 2016;136:657–663. doi: 10.1007/s00402-015-2393-5. [DOI] [PubMed] [Google Scholar]
- 111.Tangari M, Carbone S, Gallo M, Campi A. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20:409–413. doi: 10.1016/j.jse.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 112.Vitali M, Pedretti A, Naim Rodriguez N, Valenti M, Fraschini G. Our Totally Intra-Articular "Needle-Anchor" Tenodesis Technique Applied in Isolated Long Head of the Biceps Tendinopathy: Clinical and Functional Results in 60 Patients. Tech Hand Up Extrem Surg. 2016;20:26–31. doi: 10.1097/BTH.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 113.Brady PC, Narbona P, Adams CR, Huberty D, Parten P, Hartzler RU, Arrigoni P, Burkhart SS. Arthroscopic proximal biceps tenodesis at the articular margin: evaluation of outcomes, complications, and revision rate. Arthroscopy. 2015;31:470–476. doi: 10.1016/j.arthro.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 114.Green JM, Getelman MH, Snyder SJ, Burns JP. All-Arthroscopic Suprapectoral Versus Open Subpectoral Tenodesis of the Long Head of the Biceps Brachii Without the Use of Interference Screws. Arthroscopy. 2017;33:19–25. doi: 10.1016/j.arthro.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 115.Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43:1077–1083. doi: 10.1177/0363546515570024. [DOI] [PubMed] [Google Scholar]
- 116.Werner BC, Pehlivan HC, Hart JM, Carson EW, Diduch DR, Miller MD, Brockmeier SF. Increased incidence of postoperative stiffness after arthroscopic compared with open biceps tenodesis. Arthroscopy. 2014;30:1075–1084. doi: 10.1016/j.arthro.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 117.Provencher MT, LeClere LE, Romeo AA. Subpectoral biceps tenodesis. Sports Med Arthrosc Rev. 2008;16:170–176. doi: 10.1097/JSA.0b013e3181824edf. [DOI] [PubMed] [Google Scholar]
- 118.Rhee PC, Spinner RJ, Bishop AT, Shin AY. Iatrogenic brachial plexus injuries associated with open subpectoral biceps tenodesis: a report of 4 cases. Am J Sports Med. 2013;41:2048–2053. doi: 10.1177/0363546513495646. [DOI] [PubMed] [Google Scholar]
- 119.Nho SJ, Reiff SN, Verma NN, Slabaugh MA, Mazzocca AD, Romeo AA. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19:764–768. doi: 10.1016/j.jse.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 120.Forsythe B, Zuke WA, Agarwalla A, Puzzitiello RN, Garcia GH, Cvetanovich GL, Yanke AB, Verma NN, Romeo AA. Arthroscopic Suprapectoral and Open Subpectoral Biceps Tenodeses Produce Similar Outcomes: A Randomized Prospective Analysis. Arthroscopy. 2020;36:23–32. doi: 10.1016/j.arthro.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 121.Godshaw BM, Kolodychuk N, Browning BB, Williams G, Burdette R, Jones DG. Suprapectoral vs. Intra Articular Biceps Tenodesis: A Comparison of Clinical Outcomes. Orthop J Sports Med. :2018. [Google Scholar]
- 122.Lutton DM, Gruson KI, Harrison AK, Gladstone JN, Flatow EL. Where to tenodese the biceps: proximal or distal? Clin Orthop Relat Res. 2011;469:1050–1055. doi: 10.1007/s11999-010-1691-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Johannsen AM, Macalena JA, Carson EW, Tompkins M. Anatomic and radiographic comparison of arthroscopic suprapectoral and open subpectoral biceps tenodesis sites. Am J Sports Med. 2013;41:2919–2924. doi: 10.1177/0363546513503812. [DOI] [PubMed] [Google Scholar]
- 124.Denard PJ, Dai X, Hanypsiak BT, Burkhart SS. Anatomy of the biceps tendon: implications for restoring physiological length-tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28:1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 125.Levy DM, Meyer ZI, Campbell KA, Bach BR Jr. Subpectoral Biceps Tenodesis. Am J Orthop (Belle Mead NJ) 2016;45:68–74. [PubMed] [Google Scholar]
- 126.Gilmer BB, DeMers AM, Guerrero D, Reid JB 3rd, Lubowitz JH, Guttmann D. Arthroscopic versus open comparison of long head of biceps tendon visualization and pathology in patients requiring tenodesis. Arthroscopy. 2015;31:29–34. doi: 10.1016/j.arthro.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 127.Kolz CW, Suter T, Henninger HB. Regional mechanical properties of the long head of the biceps tendon. Clin Biomech (Bristol, Avon) 2015;30:940–945. doi: 10.1016/j.clinbiomech.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 128.Werner BC, Lyons ML, Evans CL, Griffin JW, Hart JM, Miller MD, Brockmeier SF. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of restoration of length-tension and mechanical strength between techniques. Arthroscopy. 2015;31:620–627. doi: 10.1016/j.arthro.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 129.Gupta AK, Chalmers PN, Klosterman EL, Harris JD, Bach BR Jr, Verma NN, Cole BJ, Romeo AA. Subpectoral biceps tenodesis for bicipital tendonitis with SLAP tear. Orthopedics. 2015;38:e48–e53. doi: 10.3928/01477447-20150105-60. [DOI] [PubMed] [Google Scholar]
- 130.Khalid MA, Morris RP, Black N, Maassen NH. Biomechanical Evaluation of Humerus Fracture After Subpectoral Biceps Tenodesis With Interference Screw Versus Unicortical Button. Arthroscopy. 2020;36:1253–1260. doi: 10.1016/j.arthro.2019.10.034. [DOI] [PubMed] [Google Scholar]
- 131.Sethi PM, Vadasdi K, Greene RT, Vitale MA, Duong M, Miller SR. Safety of open suprapectoral and subpectoral biceps tenodesis: an anatomic assessment of risk for neurologic injury. J Shoulder Elbow Surg. 2015;24:138–142. doi: 10.1016/j.jse.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 132.Werner BC, Evans CL, Holzgrefe RE, Tuman JM, Hart JM, Carson EW, Diduch DR, Miller MD, Brockmeier SF. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of minimum 2-year clinical outcomes. Am J Sports Med. 2014;42:2583–2590. doi: 10.1177/0363546514547226. [DOI] [PubMed] [Google Scholar]
- 133.Golish SR, Caldwell PE 3rd, Miller MD, Singanamala N, Ranawat AS, Treme G, Pearson SE, Costic R, Sekiya JK. Interference screw versus suture anchor fixation for subpectoral tenodesis of the proximal biceps tendon: a cadaveric study. Arthroscopy. 2008;24:1103–1108. doi: 10.1016/j.arthro.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 134.Slabaugh MA, Frank RM, Van Thiel GS, Bell RM, Wang VM, Trenhaile S, Provencher MT, Romeo AA, Verma NN. Biceps tenodesis with interference screw fixation: a biomechanical comparison of screw length and diameter. Arthroscopy. 2011;27:161–166. doi: 10.1016/j.arthro.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 135.Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of tenotomy versus tenodesis. Am J Sports Med. 2010;38:1584–1590. doi: 10.1177/0363546510364053. [DOI] [PubMed] [Google Scholar]
- 136.Scheibel M, Schröder RJ, Chen J, Bartsch M. Arthroscopic soft tissue tenodesis versus bony fixation anchor tenodesis of the long head of the biceps tendon. Am J Sports Med. 2011;39:1046–1052. doi: 10.1177/0363546510390777. [DOI] [PubMed] [Google Scholar]
- 137.Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;18:1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 138.Arora AS, Singh A, Koonce RC. Biomechanical evaluation of a unicortical button versus interference screw for subpectoral biceps tenodesis. Arthroscopy. 2013;29:638–644. doi: 10.1016/j.arthro.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 139.DeAngelis JP, Chen A, Wexler M, Hertz B, Grimaldi Bournissaint L, Nazarian A, Ramappa AJ. Biomechanical characterization of unicortical button fixation: a novel technique for proximal subpectoral biceps tenodesis. Knee Surg Sports Traumatol Arthrosc. 2015;23:1434–1441. doi: 10.1007/s00167-013-2775-6. [DOI] [PubMed] [Google Scholar]
- 140.Park JS, Kim SH, Jung HJ, Lee YH, Oh JH. A Prospective Randomized Study Comparing the Interference Screw and Suture Anchor Techniques for Biceps Tenodesis. Am J Sports Med. 2017;45:440–448. doi: 10.1177/0363546516667577. [DOI] [PubMed] [Google Scholar]
- 141.Tashjian RZ, Henninger HB. Biomechanical evaluation of subpectoral biceps tenodesis: dual suture anchor versus interference screw fixation. J Shoulder Elbow Surg. 2013;22:1408–1412. doi: 10.1016/j.jse.2012.12.039. [DOI] [PubMed] [Google Scholar]
- 142.Sawyer GA, Anderson BC, Paller D, Heard WM, Fadale PD. Effect of interference screw fixation on ACL graft tensile strength. J Knee Surg. 2013;26:155–159. doi: 10.1055/s-0032-1324808. [DOI] [PubMed] [Google Scholar]
- 143.Zantop T, Weimann A, Schmidtko R, Herbort M, Raschke MJ, Petersen W. Graft laceration and pullout strength of soft-tissue anterior cruciate ligament reconstruction: in vitro study comparing titanium, poly-d,l-lactide, and poly-d,l-lactide-tricalcium phosphate screws. Arthroscopy. 2006;22:1204–1210. doi: 10.1016/j.arthro.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 144.Shumborski S, Heath E, Salmon LJ, Roe JP, Linklater JP, Facek M, Pinczewski LA. A Randomized Controlled Trial of PEEK Versus Titanium Interference Screws for Anterior Cruciate Ligament Reconstruction With 2-Year Follow-up. Am J Sports Med. 2019;47:2386–2393. doi: 10.1177/0363546519861530. [DOI] [PubMed] [Google Scholar]
- 145.Kurtz SM, Devine JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials. 2007;28:4845–4869. doi: 10.1016/j.biomaterials.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Mazzocca AD, Bicos J, Santangelo S, Romeo AA, Arciero RA. The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis. Arthroscopy. 2005;21:1296–1306. doi: 10.1016/j.arthro.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 147.Buchholz A, Martetschläger F, Siebenlist S, Sandmann GH, Hapfelmeier A, Lenich A, Millett PJ, Stöckle U, Elser F. Biomechanical comparison of intramedullary cortical button fixation and interference screw technique for subpectoral biceps tenodesis. Arthroscopy. 2013;29:845–853. doi: 10.1016/j.arthro.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 148.Richards DP, Burkhart SS. A biomechanical analysis of two biceps tenodesis fixation techniques. Arthroscopy. 2005;21:861–866. doi: 10.1016/j.arthro.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 149.Chiang FL, Hong CK, Chang CH, Lin CL, Jou IM, Su WR. Biomechanical Comparison of All-Suture Anchor Fixation and Interference Screw Technique for Subpectoral Biceps Tenodesis. Arthroscopy. 2016;32:1247–1252. doi: 10.1016/j.arthro.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 150.Tan H, Wang D, Lebaschi AH, Hutchinson ID, Ying L, Deng XH, Rodeo SA, Warren RF. Comparison of Bone Tunnel and Cortical Surface Tendon-to-Bone Healing in a Rabbit Model of Biceps Tenodesis. J Bone Joint Surg Am. 2018;100:479–486. doi: 10.2106/JBJS.17.00797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Dovan TT, Gelberman RH, Kusano N, Calcaterra M, Silva MJ. Zone I flexor digitorum profundus repair: an ex vivo biomechanical analysis of tendon to bone repair in cadavera. J Hand Surg Am. 2005;30:258–266. doi: 10.1016/j.jhsa.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 152.Lim JK, Hui J, Li L, Thambyah A, Goh J, Lee EH. Enhancement of tendon graft osteointegration using mesenchymal stem cells in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy. 2004;20:899–910. doi: 10.1016/j.arthro.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 153.Soon MY, Hassan A, Hui JH, Goh JC, Lee EH. An analysis of soft tissue allograft anterior cruciate ligament reconstruction in a rabbit model: a short-term study of the use of mesenchymal stem cells to enhance tendon osteointegration. Am J Sports Med. 2007;35:962–971. doi: 10.1177/0363546507300057. [DOI] [PubMed] [Google Scholar]
- 154.Silva MJ, Thomopoulos S, Kusano N, Zaegel MA, Harwood FL, Matsuzaki H, Havlioglu N, Dovan TT, Amiel D, Gelberman RH. Early healing of flexor tendon insertion site injuries: Tunnel repair is mechanically and histologically inferior to surface repair in a canine model. J Orthop Res. 2006;24:990–1000. doi: 10.1002/jor.20084. [DOI] [PubMed] [Google Scholar]
- 155.Euler SA, Smith SD, Williams BT, Dornan GJ, Millett PJ, Wijdicks CA. Biomechanical analysis of subpectoral biceps tenodesis: effect of screw malpositioning on proximal humeral strength. Am J Sports Med. 2015;43:69–74. doi: 10.1177/0363546514554563. [DOI] [PubMed] [Google Scholar]
- 156.Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7–11. doi: 10.1016/j.jse.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 157.Frank RM, Bernardoni ED, Veera SS, Waterman BR, Griffin JW, Shewman EF, Cole BJ, Romeo AA, Verma NN. Biomechanical Analysis of All-Suture Suture Anchor Fixation Compared With Conventional Suture Anchors and Interference Screws for Biceps Tenodesis. Arthroscopy. 2019;35:1760–1768. doi: 10.1016/j.arthro.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 158.Mellano CR, Frank RM, Shin JJ, Jain A, Zuke WA, Mascarenhas R, Shewman E, Cole BJ, Romeo AA, Verma NN, Forsythe B. Subpectoral Biceps Tenodesis With PEEK Interference Screw: A Biomechanical Analysis of Humeral Fracture Risk. Arthroscopy. 2018;34:806–813. doi: 10.1016/j.arthro.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 159.Millett PJ, Sanders B, Gobezie R, Braun S, Warner JJ. Interference screw vs. suture anchor fixation for open subpectoral biceps tenodesis: does it matter? BMC Musculoskelet Disord. 2008;9:121. doi: 10.1186/1471-2474-9-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Leroux T, Chahal J, Wasserstein D, Verma NN, Romeo AA. A Systematic Review and Meta-analysis Comparing Clinical Outcomes After Concurrent Rotator Cuff Repair and Long Head Biceps Tenodesis or Tenotomy. Sports Health. 2015;7:303–307. doi: 10.1177/1941738114539627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zhang Q, Zhou J, Ge H, Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23:464–469. doi: 10.1007/s00167-013-2587-8. [DOI] [PubMed] [Google Scholar]
- 162.Oh JH, Lee YH, Kim SH, Park JS, Seo HJ, Kim W, Park HB. Comparison of Treatments for Superior Labrum-Biceps Complex Lesions With Concomitant Rotator Cuff Repair: A Prospective, Randomized, Comparative Analysis of Debridement, Biceps Tenotomy, and Biceps Tenodesis. Arthroscopy. 2016;32:958–967. doi: 10.1016/j.arthro.2015.11.036. [DOI] [PubMed] [Google Scholar]
- 163.Shank JR, Singleton SB, Braun S, Kissenberth MJ, Ramappa A, Ellis H, Decker MJ, Hawkins RJ, Torry MR. A comparison of forearm supination and elbow flexion strength in patients with long head of the biceps tenotomy or tenodesis. Arthroscopy. 2011;27:9–16. doi: 10.1016/j.arthro.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 164.Zabrzyński J, Huri G, Gryckiewicz S, Çetik RM, Szwedowski D, Łapaj Ł, Gagat M, Paczesny Ł. Biceps Tenodesis versus Tenotomy with Fast Rehabilitation Protocol-A Functional Perspective in Chronic Tendinopathy. J Clin Med. 2020;9 doi: 10.3390/jcm9123938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.MacDonald P, Verhulst F, McRae S, Old J, Stranges G, Dubberley J, Mascarenhas R, Koenig J, Leiter J, Nassar M, Lapner P. Biceps Tenodesis Versus Tenotomy in the Treatment of Lesions of the Long Head of the Biceps Tendon in Patients Undergoing Arthroscopic Shoulder Surgery: A Prospective Double-Blinded Randomized Controlled Trial. Am J Sports Med. 2020;48:1439–1449. doi: 10.1177/0363546520912212. [DOI] [PubMed] [Google Scholar]
- 166.Zhou P, Liu J, Deng X, Li Z. Biceps tenotomy versus tenodesis for lesions of the long head of the biceps tendon: A systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2021;100:e23993. doi: 10.1097/MD.0000000000023993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kooistra B, Gurnani N, Weening A, van Duerzen D, van den Bekerom M. Tenotomy or Tenodesis for Tendinopathy of the Long Head of the Biceps Brachii: An Updated Systematic Review and Meta-analysis. Arthrosc Sports Med Rehabil. 2021;3:e1199–e1209. doi: 10.1016/j.asmr.2021.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mollon B, Mahure SA, Ensor KL, Zuckerman JD, Kwon YW, Rokito AS. Subsequent Shoulder Surgery After Isolated Arthroscopic SLAP Repair. Arthroscopy. 2016;32:1954–1962.e1. doi: 10.1016/j.arthro.2016.01.053. [DOI] [PubMed] [Google Scholar]
- 169.Taylor SA, Degen RM, White AE, McCarthy MM, Gulotta LV, O'Brien SJ, Werner BC. Risk Factors for Revision Surgery After Superior Labral Anterior-Posterior Repair: A National Perspective. Am J Sports Med. 2017;45:1640–1644. doi: 10.1177/0363546517691950. [DOI] [PubMed] [Google Scholar]
- 170.Nadeem IM, Vancolen S, Horner NS, Leroux T, Alolabi B, Khan M. Management of Failed SLAP Repair: A Systematic Review. HSS J. 2020;16:261–271. doi: 10.1007/s11420-019-09700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Cvetanovich GL, Gowd AK, Agarwalla A, Forsythe B, Romeo AA, Verma NN. Trends in the Management of Isolated SLAP Tears in the United States. Orthop J Sports Med. 2019;7:2325967119833997. doi: 10.1177/2325967119833997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Popp D, Schöffl V. Superior labral anterior posterior lesions of the shoulder: Current diagnostic and therapeutic standards. World J Orthop. 2015;6:660–671. doi: 10.5312/wjo.v6.i9.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sullivan S, Hutchinson ID, Curry EJ, Marinko L, Li X. Surgical management of type II superior labrum anterior posterior (SLAP) lesions: a review of outcomes and prognostic indicators. Phys Sportsmed. 2019;47:375–386. doi: 10.1080/00913847.2019.1607601. [DOI] [PubMed] [Google Scholar]
- 174.Varacallo M, Tapscott DC, Mair SD. Superior Labrum Anterior Posterior Lesions. [Updated 2021 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538284/ [PubMed]
- 175.Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33:507–514. doi: 10.1177/0363546504269255. [DOI] [PubMed] [Google Scholar]
- 176.Brockmeier SF, Voos JE, Williams RJ 3rd, Altchek DW, Cordasco FA, Allen AA Hospital for Special Surgery Sports Medicine and Shoulder Service. Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Joint Surg Am. 2009;91:1595–1603. doi: 10.2106/JBJS.H.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fedoriw WW, Ramkumar P, McCulloch PC, Lintner DM. Return to play after treatment of superior labral tears in professional baseball players. Am J Sports Med. 2014;42:1155–1160. doi: 10.1177/0363546514528096. [DOI] [PubMed] [Google Scholar]
- 178.Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84:981–985. doi: 10.2106/00004623-200206000-00012. [DOI] [PubMed] [Google Scholar]
- 179.Frank RM, Nho SJ, McGill KC, Grumet RC, Cole BJ, Verma NN, Romeo AA. Retrospective analysis of arthroscopic superior labrum anterior to posterior repair: prognostic factors associated with failure. Adv Orthop. 2013;2013:125960. doi: 10.1155/2013/125960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Higgins LD, Warner JJ. Superior labral lesions: anatomy, pathology, and treatment. Clin Orthop Relat Res. 2001:73–82. [PubMed] [Google Scholar]
- 181.Lichtenberg S, Magosch P, Habermeyer P. Superior labrum-biceps anchor complex. Orthopade. 2003;32:616–626. doi: 10.1007/s00132-003-0491-5. [DOI] [PubMed] [Google Scholar]
- 182.Gottschalk MB, Karas SG, Ghattas TN, Burdette R. Subpectoral biceps tenodesis for the treatment of type II and IV superior labral anterior and posterior lesions. Am J Sports Med. 2014;42:2128–2135. doi: 10.1177/0363546514540273. [DOI] [PubMed] [Google Scholar]
- 183.Cvetanovich GL, Gowd AK, Frantz TL, Erickson BJ, Romeo AA. Superior Labral Anterior Posterior Repair and Biceps Tenodesis Surgery: Trends of the American Board of Orthopaedic Surgery Database. Am J Sports Med. 2020;48:1583–1589. doi: 10.1177/0363546520913538. [DOI] [PubMed] [Google Scholar]
- 184.Chalmers PN, Monson B, Frank RM, Mascarenhas R, Nicholson GP, Bach BR Jr, Verma NN, Cole BJ, Romeo AA. Combined SLAP repair and biceps tenodesis for superior labral anterior-posterior tears. Knee Surg Sports Traumatol Arthrosc. 2016;24:3870–3876. doi: 10.1007/s00167-015-3774-6. [DOI] [PubMed] [Google Scholar]