Abstract
Introduction:
Obstructive sleep apnea (OSA) is a common condition in the United States that is strongly linked to metabolic disease, cardiovascular disease, and increased mortality. Uninsured populations experience sleep health disparities, including delayed recognition, diagnosis, and treatment of OSA due to barriers accessing and affording care. Partnerships between primary care clinics and sleep medicine specialists for sleep apnea management have the potential to increase screening, testing, and treatment among underserved populations. Here, we present an integrated and cost-effective model that is easier to navigate for patients while maintaining high quality care.
Methods:
We designed and implemented a specialty sleep clinic at Shade Tree Clinic, Vanderbilt’s student-run, free primary care clinic. Patients with signs and symptoms of OSA were identified at primary care appointments and screened using the STOP-BANG questionnaire. Clinic visits took place over telehealth with a medical student and sleep specialist. Patients were diagnosed using a home sleep test, and if indicated, were prescribed and given a CPAP device for treatment. CPAP adherence was monitored using a cloud-based remote monitoring system.
Results:
From December 2020 through August 2021, we hosted 6 telehealth Sleep Clinics, seeing a total of 28 patients across these visits. We have received a total of 37 referrals and have coordinated sleep evaluations and diagnostic testing for 18 of these patients so far. Prior to initiation of the sleep clinic, there were 17 patients on our primary care panel at Shade Tree with a diagnosis of OSA. These patients were using donated equipment and many had been lost to follow-up or had broken parts. We were able to replace 10 of these patient’s CPAP devices and plan to replace the remaining seven.
Conclusions:
We have created a model of integrated specialty care that is efficient and cost-effective. This paradigm can be replicated for the many specialties that are typically overlooked and undertreated when working with uninsured patients. As awareness of this sleep medicine program becomes more widespread at Shade Tree Clinic, we anticipate reaching more primary care patients with signs and symptoms of sleep apnea through student education, cost-effective diagnostics, and partnership with sleep specialists.
Keywords: cost effectiveness, access to care, disease management, medical cost, primary care, underserved communities
Introduction
Obstructive sleep apnea (OSA) is a common condition in the United States that is strongly linked to metabolic disease, cardiovascular disease, and increased mortality. Prevalence of OSA in men is 22% (range, 9%-37%) and 17% (range, 4%-50%) in women, 1 and 90% of all OSA cases go undiagnosed. 2 OSA is highly comorbid with hypertension, atrial fibrillation, stroke, and type 2 diabetes. 3 The consequences of untreated sleep apnea include increased all-cause mortality, 4 cognitive dysfunction, impaired productivity, increased risk of motor vehicle accidents, and mood disturbances. 5
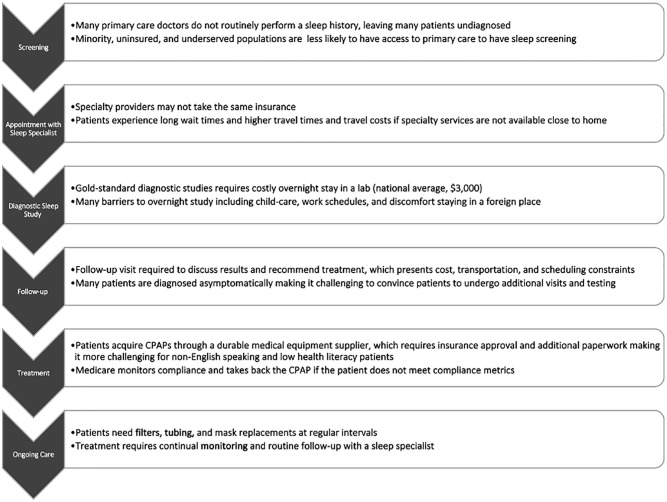
Access to sleep medicine services continues to be a problem for immigrants, racial minorities, and uninsured populations. 6 These populations experience sleep health disparities, including delayed recognition, diagnosis, and treatment of OSA (Figure 1). These groups are at greater risk of untreated OSA due to medical comorbidities and insufficient sleep due to stress, multiple jobs, long work hours, and shift work which leads to personal and public safety concerns. 7
Figure 1.
Barriers encountered at each stage of OSA diagnosis and treatment.
Continuous Positive Airway Pressure (CPAP) devices are an effective therapy and can prevent the negative sequelae of OSA. Treatment requires high patient engagement, lifestyle modifications, and frequent follow-up. A multicenter randomized trial highlighted disparities in CPAP adherence among African American patients and patients from lower socioeconomic areas even with standardized access to diagnosis, treatment, and follow-up. 8 Medicare and Medicaid criteria require adherence for at least 4 h of use per night on greater than 70% of nights. 8 Loss of CPAP coverage due to stringent adherence criteria can further exacerbate these health disparities.
There are currently not enough Sleep Medicine professionals to serve all those in need. In the United States, the estimated patient to physician ratio among sleep medicine doctors is 43 000 to 1. 9 With increasing obesity rates in the US, the number of people living with sleep apnea is expected to increase. Creating an integrated system between primary care and sleep medicine can reduce access barriers, improve health outcomes, and begin to address gaps in care. 10
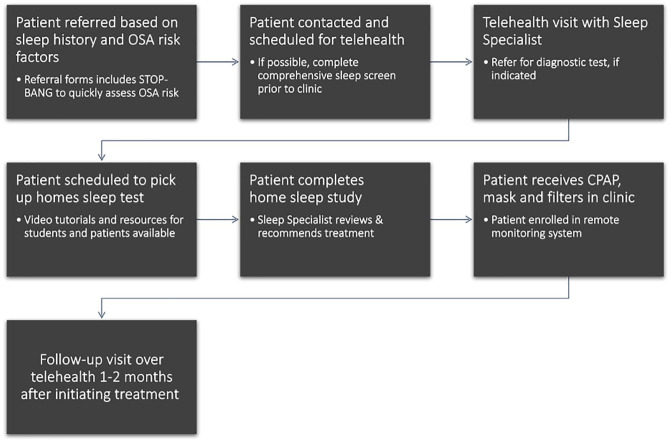
The Shade Tree Clinic (STC) is Vanderbilt University’s student-run, free primary care clinic that provides healthcare and social services free-of-charge to over 280 patients. Within our patient population, 46% have obesity with a BMI >30, 45% have hypertension, and 36% have diabetes, resulting in a large portion of our patient population at-risk for developing OSA (Figure 2).
Figure 2.
Shade Tree Clinic patient demographics and chronic conditions.
Partnerships between primary care clinics and sleep medicine specialists have the potential to increase screening, testing, and treatment among underserved populations. This integrated and cost-effective model makes the system easier to navigate for patients while maintaining high quality care. Here, we present our approach to addressing sleep medicine needs via a primary care-sleep medicine partnership at STC, including our methods for screening, diagnosing, and treating patients with OSA.
Methods
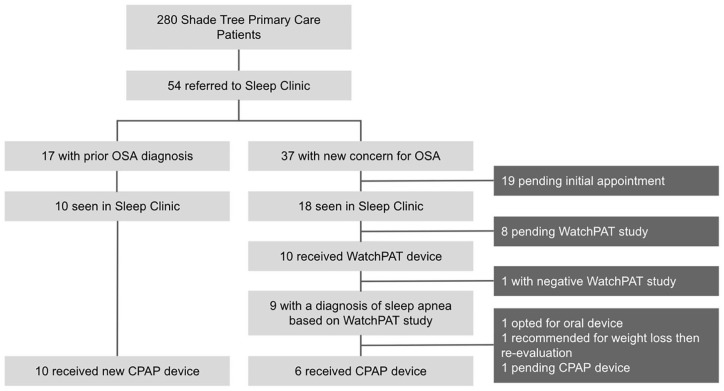
Historically, STC was unable to provide comprehensive treatment for sleep apnea due to lack of sleep medicine specialists involved at STC, access to CPAP machines, and cost of testing and treatment. Over the past year, we outlined a plan and designed a dedicated Sleep Clinic at STC. We partnered with 1 sleep medicine specialist at Vanderbilt who volunteered to oversee our process. With guidance from our medical directors and sleep specialist, we outlined a plan to provide comprehensive sleep services for our patients (Figure 3). Designing this clinic involved 4 major steps:
Figure 3.
Sleep clinic flow diagram.
(1) Screening patients at risk of OSA
(2) Administering diagnostic sleep testing
(3) Treating with CPAP devices
(4) Monitoring CPAP adherence and replacing parts
Patient Screening
Symptoms of OSA include excessive daytime sleepiness, snoring, witnessed apnea, insomnia, morning headaches, depression, cognitive dysfunction, nocturia, and erectile dysfunction; however, many patients also present asymptomatically and are only diagnosed by screening. 11
According to the clinical practice guidelines for OSA sleep screening should begin with a sleep history, including questions about snoring and daytime sleepiness. 12 Once the structure was in place to provide treatment for OSA for our Shade Tree patients, we instructed clinical students to complete a sleep history, including questions about sleep schedule, sleep hygiene, snoring, and daytime sleepiness, as part of the exam. We educated our students to identify OSA risk factors including obesity, congestive heart failure, atrial fibrillation, hypertension, type 2 diabetes, stroke, and those being evaluated for bariatric surgery.
For patients with risk factors for OSA or with concerning symptoms, the clinical team completed a referral for Sleep Clinic using Research Electronic Data Capture (REDCap), a web-based application developed by Vanderbilt University to collect patient data. 13 The RedCAP referral included the STOP-BANG screening questions. The STOP-BANG is a validated screening tool used to evaluate patients for snoring, tiredness, observed apneic episodes, high blood pressure, body mass index (BMI), age, neck circumference, and male sex. Each “yes” receives 1 point; a STOP-BANG score of greater than 3 has a greater than 90% sensitivity and 49% specificity to detect moderate-severe OSA (apnea-hypopnea index [AHI] >15).14,15
Within the initial Red CAP referral form, we provided a link to a comprehensive sleep screening questionnaire with a full sleep history. This questionnaire could be done in a clinic visit or over the phone and took approximately 20 to 30 min to complete. From the comprehensive sleep screen, we calculated the Epworth Sleepiness Scale and STOP-BANG score. The sleep questionnaire also included questions to evaluate for comorbid sleep conditions, such as insomnia and restless leg syndrome, which can impact adherence and therapy outcomes.
Clinic Visits
Dedicated sleep clinics were held monthly via telehealth beginning in December 2020. We scheduled 4 to 5 patients per clinic. Patients were first contacted via phone or Zoom platform by a medical student. During this portion of the visit, the student reviewed sleep screening questionnaires and documented a comprehensive sleep history. The attending physician worked with the medical student and counseled the patient on sleep hygiene and diagnostic testing and treatment options. If a sleep study was indicated and the patient was interested in pursuing treatment, the clinical student met with the patient in clinic and provided the patient with a home sleep apnea testing device (WatchPAT) along with instructions on proper application.
Diagnostic Testing
Prior to the advent of this clinic, an STC patient with concern for OSA would need to be referred to the Vanderbilt Sleep Clinic and then scheduled for an overnight polysomnography at the Vanderbilt Sleep Lab. The patient would return to the sleep clinic to discuss results and therapy options, if indicated. Patients were often lost to follow-up during this process.
Two primary options for diagnostic sleep apnea testing are in-lab polysomnography (PSG) and home testing. The main advantage of full-night PSG is the higher sensitivity and specificity of the test. However, in-lab PSG is not often practical for our patients due to cost (national average of about $3000), transportation, childcare, and work schedules. 16 Given the barriers to diagnostic testing among our uninsured patient population, we offered home sleep study testing using WatchPAT by Itamar Medical Ltd, an FDA-cleared portable home sleep study device that has been shown to reliably detect sleep apnea using the peripheral arterial signal. The disposable units cost $99 each. Patients wear the device around the wrist like a watch, slip on the finger probe, and attach a chest sensor. The WatchPAT device is clinically validated and has an 89% correlation to PSG. 17 The tests are straightforward to use, and medical students can teach patients after watching a 5-min instructional video. Patients who are not eligible to undergo home sleep studies due to respiratory or cardiovascular contraindications are offered PSG. Other reasons we would refer a patient for PSG instead of WatchPAT were use of alpha blockers, peripheral arterial disease, severe heart disease, central apnea, chronic obstructive pulmonary disease (COPD), and neuromuscular disorders. These recommendations are aligned with the OSA Practice Guidelines. 12
Treatment
Based on the results of the home sleep study, the sleep specialist would recommend treatment with CPAP. Our clinic was able to obtain the devices at a deep discount due to the charity nature of our clinic and our relationship with Vanderbilt. STC pays just $265 for each CPAP device. Having CPAPs available in our clinic streamlines the treatment process. Most sleep clinics are unable to directly provide CPAPs because of Stark Anti-kickback laws. Physicians cannot refer patients for certain health services paid for by Medicare if they have a financial relationship. Because we give these machines to our patients free of charge and do not bill insurance, we are able to provide machines directly from our clinic. Of note, this limits the generalizability of our approach, as it would not be possible to charge these patients for the devices if the patient is covered by Medicare or Medicaid.
Therapy data was tracked using a cloud-based data sharing system. This allowed the clinical team to monitor adherence, pressure requirements, and issues related to the device, such as leaks. After setting a patient up with a CPAP device, we saw the patient back in clinic 1 to 2 months later to review their CPAP usage with them.
Results
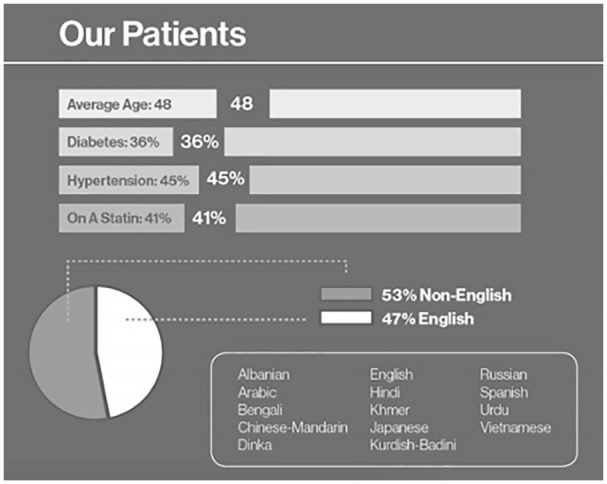
From December 2020 through August 2021, we hosted 6 telehealth Sleep Clinics seeing a total of 28 patients across these visits. Each clinic was a mix of newly referred patients and follow-up appointments. We have received a total of 37 referrals in the past 2 years and have coordinated sleep evaluations and diagnostic tests for 18 of these patients. Before the advent of this clinic, we had only diagnosed and treated 15 STC patients for OSA over the past 16 years (Figure 4).
Figure 4.
Consort diagram.
We administered 11 WatchPAT home sleep tests. One patient tested negative and 8 were confirmed to have OSA. One patient required a second home sleep test because of user error with the test the first time but tested positive for sleep apnea after a second test. We have 8 patients referred for home sleep testing and scheduled to pick up a WatchPAT device in the clinic.
Of the 8 newly diagnosed patients, 6 received new CPAP devices and are currently followed through our remote monitoring tool. One patient opted for mandibular advancement, and 1 opted for weight loss instead of CPAP. With each CPAP setup, a trained medical student met the patient in the clinic and taught the patient how to use the device. The medical student called each patient 2 and 4 weeks after setup to provide support and ask about mask fit, pressure tolerance, comfort, and usage. We then scheduled the patient for a follow-up with our sleep specialist 1 to 2 months after starting treatment to review patient adherence and provide additional education and support.
Prior to initiation of the sleep clinic, there were 17 patients on our primary care panel at STC with a diagnosis of obstructive sleep apnea. Two patients were diagnosed at outside institutions prior to becoming a STC patient. The remaining 15 patients were diagnosed between 2010 and 2018 via referral from STC to Vanderbilt Sleep Clinic. STC would pay for the cost of these appointments and for the in-lab sleep testing. These patients received CPAPs for treatment through donated supplies.
Of these 17 total patients with prior diagnoses of OSA, we have replaced 10 patient’s old machines with CPAPs from our clinic. These patients are now remotely monitored in our system and followed by our sleep specialist. The other 7 patients with prior diagnoses are still using the old machines given to them by donations or the CPAP charity program. We plan to transition these 7 patients over to a new device that will allow for remote monitoring of therapy.
Therapy data was available for 13 patients with CPAP models compatible with our remote patient monitoring system. For the 13 patients with data recorded in our remote patient monitoring system, we analyzed compliance data for the last 30 days. This group of patients achieved average CPAP use of 4.3 ± 3.0 h per night when CPAP was used. CPAP use led to a decrease in average residual AHI to 4.8 across our patient population. Furthermore, we achieved usage of greater than 4 hours per night for 35% of days across patients. This data is preliminary, as patients new to CPAP take time before becoming accustomed to using the device for a whole night.
Conclusions
Creating a dedicated Sleep Clinic required coordination among physicians, patients, clinical students, and third-party vendors providing these kits and equipment. Given that 92% of our STC patients live under 200% of the federal poverty level and a majority of the patients are uninsured, it is challenging to coordinate OSA diagnosis and treatment, as it requires multiple follow-up appointments and expensive equipment and replacement parts.
In the process of getting treatment for OSA, patients historically had to go to a sleep clinic, sleep lab, and then to a durable medical equipment supplier for CPAP. Uninsured patients already face many barriers to care, and the more steps involved in the process, the greater the risk of patients being lost to follow-up and not receiving necessary care. Our process made the system easier to navigate for patients while providing high quality care. We designed a cost-effective program and taught our students to provide standard-of-care sleep medicine to high-risk patients. For screening, we utilized the STOP-BANG questionnaire because it is time-efficient and has a high sensitivity in patients at risk of moderate to severe sleep apnea. In terms of diagnostics, we selected a $99 home sleep test in place of costly in-lab polysomnography. In addition to its cost effectiveness, the home test allowed clinical students to take an active role in educating the patient, interpreting the results, and planning next steps.
CPAP treatment-related costs consisted of the device itself, accessories, and physician visits related to CPAP therapy. One study looking at the cost effectiveness of OSA treatment calculated the incremental cost-effectiveness ratio of CPAP therapy compared with no treatment to be $24K per life year gained and about $16K per quality of life year gained. 17 Kim et al 18 found that in 373 patients at risk for moderate-to-severe OSA, a home-based testing pathway resulted in significantly lower costs to the payer than a laboratory-based polysomnography pathway ($1575 vs $1840, P = .02).
Historically, 1 advantage of the laboratory-based testing was the necessity to perform a titration study for evaluation of the amount of pressure support a patient required. With the availability of auto-titrating CPAPs that sense airway resistance and provide appropriate pressure to maintain airway patency, in-lab titration studies are no longer required for most patients. Home sleep testing has the potential to increase access to diagnostic testing in underserved populations.
We acknowledge that our sample size is small and thus limits the generalizability of our experience. We also acknowledge that our initial PAP adherence rates are low on average, but we are confident that with further refinement of our model, for example by incorporating more in person mask refitting opportunities and utilizing motivational interviewing, we can achieve greater PAP adherence.
The telehealth clinic appointments allowed medical students leading the encounter to see how sleep disorders impact patients’ lives and to practice identifying the risk factors and symptoms of these diseases. Sleep medicine is a frequently overlooked part of medical education. Most medical schools in the U.S. devote only 2 to 4 hours to sleep education (0.06% of total classroom education). The lack of training in medical school contributes to the underdiagnosis of sleep disorders, with some studies estimating 90% of OSA cases go undiagnosed. 2
With our innovative program, we anticipate testing and treating 4 additional patients per month to meet the need of our sleep medicine referrals. For less than $400 per patient we have been able to screen, diagnose, and treat patients with OSA that previously did not have access to treatment. This program involved the support of 1 sleep specialist volunteering approximately 8 h per month at our primary care clinic. Given the high rate of OSA in the general population, the lack of sleep medicine care for uninsured patients and the scarcity of sleep specialists, partnership with primary care provides an effective and efficient alternative to the traditional method of treating sleep disorders.
The model we have created here to increase access to treatment for OSA in uninsured and underserved populations can be replicated by other free clinics and Federally Qualified Health Centers (FQHCs). This paradigm can be replicated for the many specialties that are typically overlooked and undertreated when working with uninsured patients. We have demonstrated that high resource centers with specialists in every field can create a dedicated clinic to serve patients with minimal resources and relatively low total time input from specialists. As awareness of this sleep medicine program becomes more widespread at STC, we anticipate reaching more primary care patients with signs and symptoms of sleep apnea through student education, cost-effective diagnostics, and partnership with sleep specialists.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Olivia Henry  https://orcid.org/0000-0002-0753-3374
https://orcid.org/0000-0002-0753-3374
References
- 1. Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population—a review on the epidemiology of sleep apnea. J Thorac Dis. 2015;7(8):1311-1322. doi: 10.3978/j.issn.2072-1439.2015.06.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Finkel KJ, Searleman AC, Tymkew H, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009;10(7):753-758. doi: 10.1016/j.sleep.2008.08.007 [DOI] [PubMed] [Google Scholar]
- 3. Gottlieb DJ, Punjabi NM. Diagnosis and management of obstructive sleep apnea: a review. JAMA. 2020;323(14):1389-1400. doi: 10.1001/jama.2020.3514 [DOI] [PubMed] [Google Scholar]
- 4. Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6(8):e1000132. doi: 10.1371/journal.pmed.1000132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morsy NE, Farrag NS, Zaki NF, et al. Obstructive sleep apnea: personal, societal, public health, and legal implications. Rev Environ Health. 2019;34(2):153-169. doi: 10.1515/reveh-2018-0068 [DOI] [PubMed] [Google Scholar]
- 6. Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7-18. doi: 10.1016/j.sleep.2015.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hale L, Troxel W, Buysse DJ. Sleep health: an opportunity for public health to address health equity. Annu Rev Public Health. 2020;41(1):81-99. doi: 10.1146/annurev-publhealth-040119-094412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Billings ME, Thornton JD. The legacy of racial and ethnic segregation on health: the story of continuous positive airway pressure use. Am J Respir Crit Care Med. 2021;204:252-254. doi: 10.1164/rccm.202103-0649ED [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Collen JF, Wickwire EM, Capaldi V, Lettieri C. Losing sleep! Are we missing the future of sleep medicine? J Clin Sleep Med. 2020;16(4):473-474. doi: 10.5664/jcsm.8404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Watson NF, Rosen IM, Chervin RD. The past is prologue: the future of sleep medicine. J Clin Sleep Med. 2017;13(1):127-135. doi: 10.5664/jcsm.6406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cowie MR. Sleep apnea: state of the art. Trends Cardiovasc Med. 2017;27(4):280-289. doi: 10.1016/j.tcm.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 12. Epstein LJ, Kristo D, Strollo PJ, Jr, et al.; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-276. doi: 10.5664/jcsm.27497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Patridge EF, Bardyn TP. Research Electronic Data Capture (REDCap). J Med Libr Assoc. 2018;106(1):142-144. doi: 10.5195/jmla.2018.319 [DOI] [Google Scholar]
- 14. Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016;149(3):631-638. doi: 10.1378/chest.15-0903 [DOI] [PubMed] [Google Scholar]
- 15. Nagappa M, Liao P, Wong J, et al. Validation of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and meta-analysis. PLoS One. 2015;10(12):e0143697. doi: 10.1371/journal.pone.0143697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sleep study (Polysomnography) cost and procedure comparison. NewChoiceHealth.com. Accessed August 9, 2021. https://www.newchoicehealth.com/procedures/sleep-study-polysomnography
- 17. Pietzsch JB, Garner A, Cipriano LE, Linehan JH. An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep apnea. Sleep. 2011;34(6):695-709. doi: 10.5665/SLEEP.1030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim RD, Kapur VK, Redline-Bruch J, et al. An economic evaluation of home versus laboratory-based diagnosis of obstructive sleep apnea. Sleep. 2015;38(7):1027-1037. doi: 10.5665/sleep.4804 [DOI] [PMC free article] [PubMed] [Google Scholar]