Abstract
Introduction
Not much is known regarding the disparities in cancer care between women with and without disabilities.
Objectives
The aim of this study was to investigate the potential disparities in the diagnosis, treatment, and survival of women with cervical cancer with and without disabilities.
Methods
We performed a retrospective cohort study and linked the National Disability Database, Korean Central Cancer Registry, and Korean National Health Insurance claims database. Charlson comorbidity index was used for adjusting the comorbidity. The study population comprised 3 185 women with disabilities (physical/brain, communication, mental, cardiopulmonary, and other impairment) who were diagnosed with cervical cancer and 13 582 age- and sex-matched women without disability who were diagnosed with cervical cancer for comparison.
Results
Distant metastatic stage (7.7% vs 3.7%) and unknown stage (16.1% vs 7.0%) were more common in cervical cancer women with grade 1 disabilities, compared with women without disabilities. Women with cervical cancer with disabilities were less likely to undergo surgery (adjusted odds ratio (aOR) 0.81, 95% confidence interval (CI) 0.73–0.90) or chemotherapy (aOR 0.86, 95% CI 0.77–0.97). Lower rate of surgery was more evident in patients with physical/brain impairment (aOR 0.46, 95% CI 0.37–0.58) and severe mental impairment (aOR 0.57, 95% CI 0.41–0.81). The overall mortality risk was also higher in patients with disabilities (adjusted hazard ratio (aHR) 1.36, 95% CI 1.25–1.48).
Conclusion
Women with cervical cancer with disabilities, especially with severe disabilities, were diagnosed at later stages, received less treatment, and had higher mortality rates, compared with patients who lacked disabilities. Social support and policies, along with education for women with disabilities, their families, and healthcare professionals, are needed to improve these disparities.
Keywords: cervical cancer, disability, stage, treatment, survival
Introduction
Cervical cancer was the fourth most common cancer in women in 2020, with 604 127 new cases occurring worldwide. 1 Cervical cancer incidence and mortality were 2 to 4 times higher in low resource countries than in high resource countries. 2 In Korea, cervical cancer was the eighth most common cancer in women in 2018, with 3 500 new cases. 3 It is well established that cervical cancer is almost completely preventable with the detection and treatment of precancerous lesions (via Pap smear). 4 Mortality can be significantly reduced by early detection through cervical cancer screening. Surgery is typically reserved for early-stage, smaller lesions. Chemo-radiotherapy is the primary treatment for larger, localized, or advanced cervical cancers, with no significant differences in survival. 5 Surgery and concurrent chemo-radiotherapy for early-stage cervical cancers (stages I–II) have 5-year survival rates of 80–90%.6,7 The 5-year survival rate is 10–40% for stages III–IV. 8 In Korea, cervical cancer screening began in 1999 for low-income Medicaid recipients under the Korea National Cancer Screening Program. Since then, the target population has expanded to include all Korean women ≥20 years of age. 9 Because of these screening programs, cervical cancer incidence (per 100 000 individuals) decreased from 16.4 in 1999 to 8.8 in 2018, and the mortality rate (per 1 000 000 individuals) decreased from 2.6 in 1999 to 1.7 in 2018. 3
Generally, persons with disabilities are more likely to experience barriers in accessing medical services.10-13 People with disabilities experience greater socioeconomic problems than do people without disabilities. 14 Transportation barriers make timely visits to a clinic or physician’s office difficult. 15 Healthcare institutions often lack equipment that enables access for people with disabilities. 16 Many healthcare providers feel uncomfortable while treating people with intellectual disabilities. 17 A neglectful attitude toward health among disabled people has also been reported as a barrier. 18
Various studies have explored disparities in cancer screening between people with and without disabilities. One study found that deaf women had reduced rates of cervical cancer screening. 19 Shin et al. 12 reported that the cervical cancer screening rate of Korean women was reported to be 54.1% in women without disabilities and only 29.8% in women with severe disabilities as of 2015. Significant disparities were also found in breast cancer screening, especially in women with severe and mental disabilities. 20 Significant disparities were reported in gastric cancer screening in Korea, especially among people with severe disabilities, renal failure, or mental disabilities. 21 Fujiwara et al. 22 reported low rates of cancer screening in schizophrenic patients.
Few studies have reported disparities in cancer diagnosis and treatment between people with and without disabilities. According to one report, people with disabilities were more likely to have advanced cancer at the time of diagnosis. 23 Another study demonstrated that gastric cancer patients with disabilities were diagnosed at later stages, received fewer staging evaluations and treatments, and had worse overall survival rates. 24 Shin et al. 25 reported that disabled lung cancer patients underwent fewer staging work-ups and treatments; they also had lower survival rates. People with disabilities had lower rates of multiple myeloma diagnosis, received less treatment, exhibited lower survival rates, and compared with people who lacked disabilities. 26 However, there is no study on disparities with respect to the presence or absence of disabilities in patients with cervical cancer.
It is important to investigate these disparities to improve cancer care for people with disabilities. In Korea, the National Disability Registration System collects and manages the data of almost persons with disabilities along with their medical records, according to the disability type and severity. The nationwide cancer registry system also collects medical information for use by the Korean National Health Insurance Service (KNHIS).
In this study, our research question was “Do potential disparities exist in the diagnosis, treatment, and survival of cervical cancer patients according to disability status?” We examined this issue by using linked administrative databases.
Materials and Methods
Study Setting and Data Source
Korean National Health Insurance Service
The Korean National Health Insurance Service (KNHIS) provides universal health insurance for virtually all Koreans except for Medicaid beneficiaries in the lowest income bracket (representing 3% of the population). 27 The KNHIS collects all data necessary for reimbursement to medical service providers, including disease codes, medical costs for inpatients and outpatients, and demographic data. The KNHIS also provides a free biennial cervical cancer screening program with the Papanicolaou test to all Korean women aged ≥20 years. 12
Disability Registration System in the Republic of Korea
The Korea National Disability Registration System was established in 1988 for the provision of welfare benefits based on the type and severity of disability.25,28 National disability registration involves 15 disability types and 6 levels of severity that are diagnosed by a specialist physician according to predefined government guidelines. 28 The 15 legally defined types of disability are limb, brain, visual, auditory, linguistic, facial, kidney, heart, liver, respiratory system, ostomy, epilepsy, intellectual, autistic, and mental disabilities. In our study, we reclassified the disability types as follows: (1) physical/brain impairment (limb and brain disability), (2) communication impairment (visual, auditory, or linguistic disability), (3) mental impairment (intellectual, autistic, or mental disability), (4) cardiopulmonary impairment (heart or lung disability), and (5) other impairment. The disability severity was graded from 1 (most severe) to 6 (least severe). This database is assumed to have covered 93.8% of the total population with disabilities in 2011. 29
Cancer Registration System in the Republic of Korea
The Korean Central Cancer Registry (KCCR), a government-sponsored, nationwide cancer registry, began in 1980. The KCCR collects data such as patients’ sex, age at diagnosis, date of diagnosis, cancer site, surveillance, epidemiology, and summary stage (in situ and local, regional, distant, and unknown). The completeness of cancer incidence data was estimated to be 98.2% as of 2015. 30
Study Patients
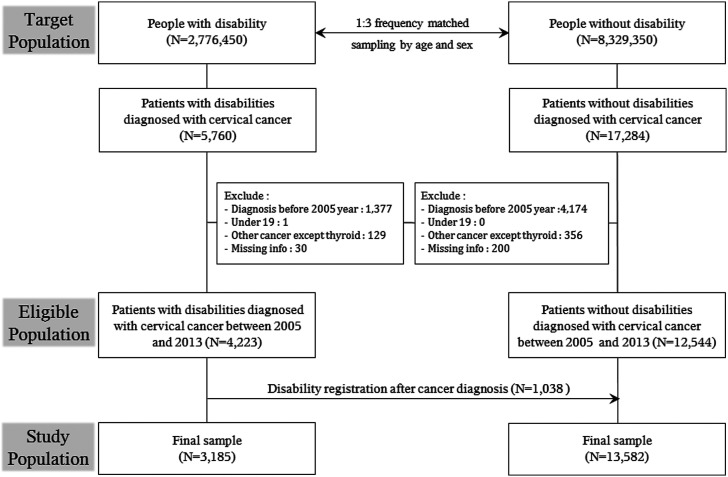
We selected 3 age- and sex-matched controls from the KNHIS, using frequency-matched random sampling, for each disabled patient registered in the national disability registry from 2009 to 2013 (2 776 450 people with disabilities; 8 329 350 people without disabilities; total of 11 105 800 individuals). Patients with newly diagnosed cervical cancer with International Classification of Diseases code D06, C53 were identified using KCCR data from January 1, 2005 to December 31, 2013 (n = 23 044). We excluded patients who (1) were diagnosed with cervical cancer before 2005 (n = 5 551), (2) were younger than 19 years at the time of diagnosis or index date (n = 1), (3) had a history of other cancers (except for thyroid cancer) before the cervical cancer diagnosis (n = 485), or (4) had missing data (n = 230). Among the eligible patients, we identified 1 038 patients who developed disabilities after the cervical cancer diagnosis and merged them with patients without disabilities. Thus, the study sample included 3 185 patients with disabilities and 13 582 patients without disabilities at the cervical cancer diagnosis. Further adjustments for smoking and body mass index were performed for patients who participated in a screening program within 2 years of cancer diagnosis. This screening subset comprised 1 104 people with disabilities and 5 078 people without disabilities (Figure 1). A subset of individuals who had localized disease treated with surgery was constructed to investigate the survival of cervical cancer patients who underwent surgery with curative intent. Of the 16 767 initially eligible individuals, the final subset had 11 687 patients (9 577 with disabilities and 2 110 without disabilities). Patients with heart and lung disabilities were also excluded because surgery may be contraindicated in these patients. Institutional review board approval was obtained from Chungbuk National University (no. CBNU-201708-ETC-504-01).
Figure 1.
Consort Diagram.
Statistical Analyses
Descriptive statistics were used to summarize the data based on the presence or absence of disabilities, as well as disability types and severities. The disease stage and treatment were analyzed using the chi-square test. Surgical procedures were categorized according to the extent of surgery (cone biopsy, hysterectomy, pelvic exenteration, and pelvic lymph node dissection). Owing to the complexity of the regimens, chemotherapy and radiotherapy were not further categorized. We assessed the relative probabilities of receiving a specific treatment (i.e., surgery, radiotherapy, and chemotherapy) through logistic regression analyses, adjusting for age, Charlson comorbidity index, income, place of residence, and cancer stage. The Charlson comorbidity index is a widely used measure of comorbidity, particularly among investigators conducting epidemiologic and outcomes research studies for administrative purposes.31,32 This measure comprises 19 comorbid conditions, each assigned a score based on its potential for causing mortality within 1 year. The index is the sum of the weighted comorbidities and assesses the risk of mortality. 33 Hazard ratios (HRs) for the overall mortality (not cancer specific mortality) of patients with disabilities (by grade, severity, and type), compared with patients who lacked disabilities, were calculated using Cox proportional hazard regression. We confined the survival time from diagnosis date of cervical cancer to the date of death or December 31, 2017 (date of censoring if still alive), whichever came first. We also performed separate Cox proportional hazard regression analyses for the surgery subgroups. All analyses were performed using the SAS statistical software (version 9.4; SAS Institute Inc., Cary, NC). P < .05 was considered statistically significant.
Results
Characteristics of the Study Patients
Cervical cancer patients with disabilities had more comorbidities and a higher Charlson comorbidity index score (1.55), compared with patients who lacked disabilities (1.00). In addition, patients with disabilities had lower income levels, higher body mass index, and were more likely to be smokers. According to the disability grade, patients with severe disabilities had a higher Charlson comorbidity index score (1.66), compared with patients who lacked disabilities (1.48). Severely disabled patients also had a greater proportion of individuals with a score of ≥4 (21.5%), compared with patients who had mild disabilities (14.3%) (Table 1).
Table 1.
Characteristics of Cervical Cancer Patients with and without Disabilities.
| Characteristics | People without disabilities | People with disabilities | P value | By disability grade | P value | |
|---|---|---|---|---|---|---|
| Grade 1-3 | Grade 4-6 | |||||
| All subject, N | 13 582 | 3 185 | 0.0011 | 1 105 | 2 080 | <.0001 |
| Age, years | ||||||
| Mean ± SD | 60.30 ± 14.12 | 60.68 ± 13.84 | 0.0011 | 58.13 ± 14.17 | 62.04 ± 13.47 | <.0001 |
| 19–40 | 1 353 (10.0) | 263 (8.3) | 123 (11.1) | 140 (6.7) | ||
| 41–65 | 6 525 (48.0) | 1 620 (50.9) | 628 (56.8) | 992 (47.7) | ||
| 66–75 | 3 812 (28.1) | 836 (26.2) | 224 (20.3) | 612 (29.4) | ||
| >75 | 1892 (13.9) | 466 (14.6) | 130 (11.8) | 336 (16.2) | ||
| Charlson comorbidity score | ||||||
| Mean ± SD | 1.00 ± 1.24 | 1.55 ± 1.45 | <.0001 | 1.66 ± 1.54 | 1.48 ± 1.40 | <.0001 |
| 0 | 6 512 (47.9) | 1 057 (33.2) | 372 (33.7) | 685 (32.9) | ||
| 1 | 3 387 (24.9) | 715 (22.4) | 213 (19.3) | 502 (24.1) | ||
| 2 | 1 767 (13.0) | 547 (17.2) | 166 (15.0) | 381 (18.3) | ||
| 3 | 915 (6.7) | 331 (10.4) | 116 (10.5) | 215 (10.3) | ||
| ≥4 | 1 001 (7.4) | 535 (16.8) | 238 (21.5) | 297 (14.3) | ||
| Comorbidity | ||||||
| Hypertension | 4 584 (33.8) | 1 451 (45.6) | <.0001 | 498 (45.1) | 953 (45.8) | 0.68 |
| Diabetes mellitus | 2 207 (16.2) | 736 (23.1) | <.0001 | 261 (23.6) | 475 (22.8) | 0.61 |
| Coronary heart disease | 901 (6.6) | 335 (10.5) | <.0001 | 137 (12.4) | 198 (9.5) | 0.01 |
| Stroke | 431 (3.2) | 226 (7.1) | <.0001 | 112 (10.1) | 114 (5.5) | <.0001 |
| COPD | 2 875 (21.2) | 800 (25.1) | <.0001 | 256 (23.2) | 544 (26.2) | 0.06 |
| Income | ||||||
| Medical aid | 833 (6.1) | 692 (21.7) | <.0001 | 384 (34.8) | 308 (14.8) | <.0001 |
| 1st quartile (lowest) | 2 841 (20.9) | 620 (19.5) | 187 (16.9) | 433 (20.8) | ||
| 2nd quartile | 2 618 (19.3) | 541 (17.0) | 157 (14.2) | 384 (18.5) | ||
| 3rd quartile | 3 211 (23.6) | 561 (17.6) | 161 (14.6) | 400 (19.2) | ||
| 4th quartile (highest) | 4 079 (30.0) | 771 (24.2) | 216 (19.5) | 555 (26.7) | ||
| Surgery | 10 127 (74.6) | 2 223 (69.8) | <.0001 | 707 (64.0) | 1 516 (72.9) | <.0001 |
| Conization | 6 721 (49.5) | 1 487 (46.7) | 0.0045 | 492 (44.5) | 995 (47.8) | 0.07 |
| Hysterectomy | 6 295 (46.3) | 1 319 (41.4) | <.0001 | 386 (34.9) | 933 (44.9) | <.0001 |
| Pelvic exenteration | 20 (.1) | 2 (.1) | 0.23 | 0 | 2 (.1) | 0.30 |
| Pelvic lymph node dissection | 79 (.6) | 13 (.4) | 0.23 | 2 (.2) | 11 (.5) | 0.14 |
| Chemotherapy | 3 001 (22.1) | 645 (20.3) | 0.02 | 215 (19.5) | 430 (20.7) | 0.41 |
| Radiotherapy | 4 084 (30.1) | 939 (29.5) | 0.51 | 354 (32.0) | 585 (28.1) | 0.02 |
| Treatment combination | ||||||
| Surgery only | 8 107 (59.7) | 1 817 (57.0) | <.0001 | 576 (52.1) | 1 241 (59.7) | <.0001 |
| Surgery + CT | 233 (1.7) | 51 (1.6) | 20 (1.8) | 31 (1.5) | ||
| Surgery + RT | 673 (5.0) | 149 (4.7) | 59 (5.3) | 90 (4.3) | ||
| Surgery + CT + RT | 1 114 (8.2) | 206 (6.5) | 52 (4.7) | 154 (7.4) | ||
| CT | 76 (.6) | 21 (.7) | 5 (.5) | 16 (.8) | ||
| RT | 719 (5.3) | 217 (6.8) | 105 (9.5) | 112 (5.4) | ||
| CT + RT | 1 578 (11.6) | 367 (11.5) | 138 (12.5) | 229 (11.0) | ||
| No treatment | 1 082 (8.0) | 357 (11.2) | 150 (13.6) | 207 (10.0) | ||
| Subgroup | 5 078 | 1104 | 243 | 861 | ||
| Smoking | ||||||
| Current | 173 (3.4) | 54 (4.9) | 0.04 | 17 (7.0) | 37 (4.3) | 0.14 |
| Past | 78 (1.5) | 20 (1.8) | 6 (2.5) | 14 (1.6) | ||
| None | 4 827 (95.1) | 1 030 (93.3) | 220 (90.5) | 810 (94.1) | ||
| BMI, kg/m2 | ||||||
| <18.5 | 172 (3.4) | 30 (2.7) | <.0001 | 6 (2.5) | 24 (2.8) | 0.05 |
| 18.5–23 | 1 963 (38.7) | 360 (32.6) | 98 (40.3) | 262 (30.4) | ||
| 23–25 | 1 253 (24.7) | 247 (22.4) | 53 (21.8) | 194 (22.5) | ||
| 2530 | 1 525 (30.0) | 406 (36.8) | 75 (30.9) | 331 (38.4) | ||
| >30 | 165 (3.2) | 61 (5.5) | 11 (4.5) | 50 (5.8) | ||
Abbreviation: BMI, body mass index; COPD, Chronic obstructive pulmonary disease; CT, chemotherapy; RT, radiotherapy; SD, standard deviation.
Stage at Diagnosis According to Disability
Overall, women with and without disabilities were diagnosed with similar distribution of stages of cervical cancer. However, the distribution of distant metastatic stage (7.7% vs 3.7%) and unknown stage (16.1% vs 7.0%) was more common in women with grade 1 disability. Among the various disability types, women with severe communication disabilities had a higher percentage of distant metastatic stage (6.7%) and unknown stage (10.9%) (Table 2). The unknown stage included cases for which sufficient evidence was not available to adequately assign a stage. Examples included patient death before workup could be completed, patient refusal for a diagnostic or treatment procedure, limited workup because of the patient’s age or condition, and lack of sufficient patient information (https://seer.cancer.gov/tools/ssm/ssm2000/).
Table 2.
Distribution of Cervical Cancer Stage by Disability Grade and Type.
| Characteristics | All | Localized | Locoregional | Distant | Unknown | P value |
|---|---|---|---|---|---|---|
| All subject, n | 16 767 | 12 479 (74.4) | 2 475 (14.8) | 615 (3.7) | 1 198 (7.1) | 0.34 |
| People without disabilities | 13 582 | 10 127 (74.6) | 1 995 (14.7) | 508 (3.7) | 952 (7.0) | |
| People with disability | 3 185 | 2 352 (73.8) | 480 (15.1) | 107 (3.4) | 246 (7.7) | |
| By disability grades | ||||||
| Severe (Grade 1–3) | 1 105 | 796 (72.0) | 172 (15.6) | 46 (4.2) | 91 (8.2) | 0.24 |
| Mild (Grade 4–6) | 2 080 | 1 556 (74.8) | 308 (14.8) | 61 (2.9) | 155 (7.5) | |
| Grade 1 | 143 | 88 (61.5) | 21 (14.7) | 11 (7.7) | 23 (16.1) | <.0001 |
| Grade 2 | 498 | 367 (73.7) | 75 (15.1) | 17 (3.4) | 39 (7.8) | |
| Grade 3 | 464 | 341 (73.5) | 76 (16.4) | 18 (3.9) | 29 (6.3) | |
| Grade 4 | 537 | 390 (72.6) | 87 (16.2) | 13 (2.4) | 47 (8.8) | |
| Grade 5 | 812 | 596 (73.4) | 112 (13.8) | 36 (4.4) | 68 (8.4) | |
| Grade 6 | 731 | 570 (78.0) | 109 (14.9) | 12 (1.6) | 40 (5.5) | |
| By disability types | ||||||
| Physical/brain | ||||||
| Grade 1–3 | 475 | 330 (69.5) | 82 (17.3) | 17 (3.6) | 46 (9.7) | 0.0017 |
| Grade 4–6 | 1 510 | 1 136 (75.2) | 220 (14.6) | 49 (3.2) | 105 (7.0) | |
| Communication | ||||||
| Grade 1–3 | 238 | 165 (69.3) | 31 (13.0) | 16 (6.7) | 26 (10.9) | |
| Grade 4–6 | 488 | 353 (72.3) | 81 (16.6) | 10 (2.0) | 44 (9.0) | |
| Mental | ||||||
| Grade 1–3 | 211 | 147 (69.7) | 41 (19.4) | 8 (3.8) | 15 (7.1) | |
| Grade 4–6 | 3 | 1 (33.3) | 2 (66.7) | 0 (0.0) | 0 (0.0) | |
| Heart/Lung | ||||||
| Grade 1–3 | 31 | 26 (83.9) | 4 (12.9) | 0 (0.0) | 1 (3.2) | |
| Grade 4–6 | 2 | 2 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Others | ||||||
| Grade 1–3 | 150 | 128 (85.3) | 14 (9.3) | 5 (3.3) | 3 (2.0) | |
| Grade 4–6 | 77 | 64 (83.1) | 5 (6.5) | 2 (2.6) | 6 (7.8) | |
Treatment Received According to Disability
Cervical cancer patients with disabilities were less likely to undergo surgery (adjusted odds ratio (aOR) 0.81, 95% confidence interval (CI) 0.73–0.90) and chemotherapy (aOR 0.86, 95% CI 0.77–0.97), especially those with severe disabilities (for surgery: aOR 0.56, 95% CI 0.48–0.66; for chemotherapy: aOR 0.74, 95% CI 0.62–0.90) (Table 3). Radiation therapy was not associated with the presence or absence of disabilities. Among women with severe disabilities, those with severe physical/brain impairment (aOR 0.46, 95% CI 0.37–0.58) and severe mental impairment (aOR 0.57, 95% CI 0.41–0.81) were less likely to undergo surgery. Severe communication disability was significantly associated with less surgery based on crude OR (0.57, 95% CI 0.43–0.74), whereas the aOR was 0.76 (95% CI 0.41–1.06). The proportion of patients with “no treatment” was higher in women with disabilities (11.2% vs 8.0%), especially severe disabilities (13.6%) (Table 1).
Table 3.
Received Treatment by Disability Grade and Type.
| n | Surgery | Radiotherapy | Chemotherapy | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Received n (%) | Crude OR (95% CI) | Adjusted OR* (95% CI) | Received n (%) | Crude OR (95% CI) | Adjusted OR (95% CI) | Received n (%) | Crude OR (95% CI) | Adjusted OR* (95% CI) | ||
| People without disabilities | 13 582 | 10 127 (74.6) | Ref | Ref | 4 084 (30.1) | Ref | Ref | 3 001 (22.1) | Ref | Ref |
| People with disability | 3 185 | 2 223 (69.8) | 0.78 (0.72–0.85) | 0.81 (0.73–0.90) | 939 (29.5) | 0.97 (0.89–1.05) | 0.95 (0.85–1.05) | 645 (20.3) | 0.89 (0.81–0.98) | 0.86 (0.77–0.97) |
| By disability grades | ||||||||||
| Severe (Grade 1–3) | 1 105 | 707 (64.0) | 0.60 (0.53–0.68) | 0.56 (0.48–0.66) | 354 (32.0) | 1.09 (0.96–1.25) | 1.16 (0.98–1.36) | 215 (19.5) | 0.85 (0.73–0.99) | 0.74 (0.62–0.90) |
| Mild (Grade 4–6) | 2 080 | 1 516 (72.9) | 0.91 (0.82–1.01) | 0.99 (0.87–1.12) | 585 (28.1) | 0.91 (0.82–1.00) | 0.86 (0.76–0.97) | 430 (20.7) | 0.91 (0.82–1.02) | 0.92 (0.81–1.06) |
| Grade 1 | 143 | 79 (55.2) | 0.42 (0.30–0.58) | 0.49 (0.33–0.73) | 41 (28.7) | 0.93 (0.64–1.34) | 0.74 (0.48–1.15) | 24 (16.8) | 0.71 (0.45–1.10) | 0.49 (0.29–0.81) |
| Grade 2 | 498 | 315 (63.3) | 0.58 (0.48–0.70) | 0.51 (0.40–0.64) | 161 (32.3) | 1.11 (0.91–1.34) | 1.29 (1.02–1.63) | 82 (16.5) | 0.69 (0.54–0.88) | 0.60 (0.45–0.80) |
| Grade 3 | 464 | 313 (67.5) | 0.70 (0.58–0.86) | 0.66 (0.52–0.83) | 152 (32.8) | 1.13 (0.93–1.38) | 1.19 (0.93–1.51) | 109 (23.5) | 1.08 (0.87–1.34) | 1.03 (0.79–1.34) |
| Grade 4 | 537 | 371 (69.1) | 0.76 (0.63–0.91) | 1.01 (0.81–1.27) | 182 (33.9) | 1.19 (0.99–1.43) | 1.07 (0.86–1.33) | 121 (22.5) | 1.02 (0.83–1.26) | 1.04 (0.81–1.32) |
| Grade 5 | 812 | 587 (72.3) | 0.89 (0.76–1.04) | 1.05 (0.87–1.28) | 209 (25.7) | 0.80 (0.68–0.94) | 0.69 (0.57–0.84) | 155 (19.1) | 0.83 (0.69–0.99) | 0.80 (0.65–0.99) |
| Grade 6 | 731 | 558 (76.3) | 1.10 (0.92–1.31) | 0.89 (0.73–1.10) | 194 (26.5) | 0.84 (0.71–0.99) | 0.91 (0.74–1.11) | 154 (21.1) | 0.94 (0.78–1.12) | 0.98 (0.79–1.21) |
| By disability types | ||||||||||
| Physical/brain | ||||||||||
| Grade 1–3 | 475 | 282 (59.4) | 0.49 (0.41–0.60) | 0.46 (0.37–0.58) | 166 (35.0) | 1.24 (1.03–1.51) | 1.21 (0.96–1.54) | 102 (21.5) | 0.96 (0.77–1.20) | 0.84 (0.64–1.10) |
| Grade 4–6 | 1 510 | 1121 (74.2) | 0.98 (0.87–1.11) | 1.07 (0.93–1.24) | 422 (28.0) | 0.90 (0.80–1.01) | 0.84 (0.73–0.97) | 315 (20.9) | 0.92 (0.81–1.05) | 0.93 (0.80–1.09) |
| Communication | ||||||||||
| Grade 1–3 | 238 | 149 (62.6) | 0.57 (0.43–0.74) | 0.76 (0.55–1.06) | 73 (30.7) | 1.02 (0.77–1.35) | 0.90 (0.65–1.26) | 46 (19.3) | 0.84 (0.61–1.16) | 0.74 (0.50–1.08) |
| Grade 4–6 | 488 | 327 (67.0) | 0.69 (0.57–0.84) | 0.77 (0.61–0.98) | 152 (31.1) | 1.05 (0.86–1.27) | 0.96 (0.76–1.21) | 105 (21.5) | 0.96 (0.77–1.20) | 0.93 (0.72–1.20) |
| Mental | ||||||||||
| Grade 1–3 | 211 | 140 (66.4) | 0.67 (0.50–0.89) | 0.57 (0.41–0.81) | 66 (31.3) | 1.05 (0.78–1.41) | 1.20 (0.82–1.74) | 55 (26.1) | 1.24 (0.91–1.69) | 0.98 (0.66–1.45) |
| Grade 4–6 | 3 | 2 (66.7) | 0.68 (0.06–7.52) | 0.68 (0.05–8.97) | 2 (66.7) | 4.65 (0.42–51.31) | 3.94 (0.28–54.59) | 2 (66.7) | 7.05 (0.63–77.79) | 4.66 (0.32–67.68) |
| Heart/lung | ||||||||||
| Grade 1–3 | 31 | 22 (71.0) | 0.83 (0.38–1.81) | 0.58 (0.24–1.39) | 6 (19.4) | 0.55 (0.22–1.36) | 0.57 (0.20–1.63) | 4 (12.9) | 0.52 (0.18–1.49) | 0.53 (0.16–1.77) |
| Grade 4–6 | 2 | 2 (100.0) | - | - | 0 (.0) | - | - | 0 (.0) | - | - |
| Others | ||||||||||
| Grade 1–3 | 150 | 114 (76.0) | 1.08 (0.74–1.57) | 0.64 (0.41–0.99) | 43 (28.7) | 0.93 (0.65–1.33) | 1.69 (1.11–2.57) | 8 (5.3) | 0.19 (0.09–0.40) | 0.19 (0.08–0.42) |
| Grade 4–6 | 77 | 64 (83.1) | 1.68 (0.92–3.05) | 1.00 (0.50–2.02) | 9 (11.7) | 0.30 (0.15–0.61) | 0.42 (0.19–0.96) | 8 (10.4) | 0.40 (0.19–0.85) | 0.53 (0.23–1.22) |
Abbreviation: CI, confidence interval; OR, odds ratio; Ref, reference.
*Adjusted for age, Charlson comorbidity index, income, place of residence, and cancer stage.
Survival According to Disability
Cervical cancer patients with disabilities, especially patients with severe disabilities, had a higher overall mortality risk, compared with the control group (with disabilities: adjusted hazard ratio (aHR): 1.36; 95% CI 1.25–1.48 and with severe disabilities: aHR: 1.72; 95% CI: 1.52–1.95). The median survival time was shorter in cervical cancer patients with disabilities (73.9 months) than in patients without disabilities (85.2 months). Patients with grade 1 (aHR: 1.91; 95% CI: 1.43–2.55) and grade 2 disabilities (aHR: 2.09; 95% CI: 1.75–2.48) had a particularly high risk of overall mortality. By disability type, the aHR for the overall mortality risk was 1.44 (95% CI 1.20–1.73) for women with severe physical/brain impairment, 1.41 (95% CI 1.10–1.80) for those with severe communication impairment, and 2.46 (95% CI 1.83–3.31) for those with severe mental impairment (Table 4).
Table 4.
Mortality according to Disability in Patients with Cervical Cancer.
| All | No. of Death | Rate per 1000 | Crude HR (95% CI) | Adjusted HR (95% CI)* | |
|---|---|---|---|---|---|
| People without disabilities | 13 582 | 2 341 | 22.02 | Ref | Ref |
| People with disability | 3 185 | 691 | 31.06 | 1.37 (1.26–1.49) | 1.36 (1.25–1.48) |
| By disability grades | |||||
| Severe (Grade 1–3) | 1 105 | 296 | 39.68 | 1.75 (1.55–1.97) | 1.72 (1.52–1.95) |
| Mild (Grade 4–6) | 2 080 | 395 | 26.72 | 1.18 (1.06–1.31) | 1.19 (1.06–1.32) |
| Grade 1 | 143 | 48 | 52.68 | 2.30 (1.73–3.06) | 1.91 (1.43–2.55) |
| Grade 2 | 498 | 145 | 44.91 | 1.96 (1.66–2.32) | 2.09 (1.75–2.48) |
| Grade 3 | 464 | 103 | 31.03 | 1.38 (1.13–1.68) | 1.35 (1.10–1.65) |
| Grade 4 | 537 | 118 | 31.15 | 1.38 (1.15–1.66) | 1.18 (0.98–1.42) |
| Grade 5 | 812 | 164 | 29.21 | 1.28 (1.10–1.51) | 1.18 (1.00–1.38) |
| Grade 6 | 731 | 113 | 20.99 | 0.93 (0.77–1.12) | 1.21 (1.00–1.47) |
| By disability types | |||||
| Physical/brain | |||||
| Grade 1–3 | 475 | 126 | 38.65 | 1.710 (1.42–2.04) | 1.449 (1.20–1.73) |
| Grade 4–6 | 1 510 | 263 | 24.41 | 1.081 (0.95–1.22) | 1.113 (0.97–1.26) |
| Communication | |||||
| Grade 1–3 | 238 | 65 | 39.93 | 1.770 (1.38–2.26) | 1.411 (1.10–1.80) |
| Grade 4–6 | 488 | 117 | 34.54 | 1.530 (1.27–1.84) | 1.321 (1.09–1.59) |
| Mental | |||||
| Grade 1–3 | 211 | 48 | 34.49 | 1.516 (1.13–2.01) | 2.462 (1.83–3.31) |
| Grade 4–6 | 3 | 0 | - | - | - |
| Heart/lung | |||||
| Grade 1–3 | 31 | 12 | 53.14 | 2.372 (1.34–4.18) | 3.303 (1.86–5.83) |
| Grade 4–6 | 2 | 0 | - | - | - |
| Others | |||||
| Grade 1–3 | 150 | 45 | 47.20 | 2.049 (1.52–2.75) | 3.466 (2.55–4.70) |
| Grade 4–6 | 77 | 15 | 25.70 | 1.163 (0.70–1.93) | 2.829 (1.69–4.72) |
Abbreviation: CI, confidence interval; HR, hazard ratio; Ref, reference.
*Adjusted for age, Charlson comorbidity index, income, place of residence, cancer stage, surgery, chemotherapy, and radiotherapy.
Survival According to Disability in Patients with Localized Stage Treated with Surgery
Cervical cancer patients with severe disabilities had higher overall mortality risk than those without disabilities (aHR 1.55, 95% CI 1.20–2.00) (Table 5). The difference was not statistically significant between patients with mild disabilities and without disabilities (aHR: 0.97; 95% CI 0.80–1.18). Patients with grade 1 (aHR: 1.97; 95% CI: 1.08–3.61) and grade 2 disabilities (aHR: 2.05; 95% CI: 1.45–2.89) had a significantly higher risk of overall mortality. By disability type, survival was significantly lower in women with mental impairment (aHR 1.82, 95% CI 1.01–3.29). In addition, patients with mild communication impairment or other severe impairments had a significantly higher overall mortality risk. Overall, patients with disabilities had significantly higher overall mortality than those without disabilities, based on crude HR (1.26, 95% CI 1.08–1.48); however, the difference was not significant after adjusting for covariates (1.12, 95% CI 0.95–1.32).
Table 5.
Mortality according to Disability in Cervical Cancer Patients with Localized Stage Treated with Surgery.
| All | No. of death | Rate per 1000 | Crude HR (95% CI) | Adjusted HR* (95% CI) | |
|---|---|---|---|---|---|
| People without disabilities | 9 577 | 742 | 9.33 | Ref | Ref |
| People with disability | 2 110 | 190 | 11.79 | 1.26 (1.08–1.48) | 1.12 (0.95–1.32) |
| By disability grades | |||||
| Severe (Grade 1–3) | 659 | 70 | 13.98 | 1.50 (1.17–1.92) | 1.55 (1.20–2.00) |
| Mild (Grade 4–6) | 1 451 | 120 | 10.81 | 1.16 (0.95–1.40) | 0.97 (0.80–1.18) |
| Grade 1 | 74 | 11 | 20.38 | 2.18 (1.20–3.96) | 1.97 (1.08–3.61) |
| Grade 2 | 302 | 37 | 16.42 | 1.76 (1.27–2.45) | 2.05 (1.45–2.89) |
| Grade 3 | 283 | 22 | 9.94 | 1.06 (0.69–1.63) | 1.04 (0.68–1.60) |
| Grade 4 | 353 | 41 | 15.27 | 1.64 (1.19–2.24) | 1.09 (0.79–1.50) |
| Grade 5 | 558 | 43 | 10.22 | 1.10 (0.81–1.49) | 0.88 (0.64–1.20) |
| Grade 6 | 540 | 36 | 8.55 | 0.91 (0.65–1.28) | 0.98 (0.70–1.37) |
| By disability types | |||||
| Physical/brain | |||||
| Grade 1–3 | 273 | 25 | 11.70 | 1.25 (0.84–1.86) | 1.20 (0.80–1.79) |
| Grade 4–6 | 1 075 | 80 | 9.76 | 1.05 (0.83–1.32) | 0.82 (0.65–1.04) |
| Communication | |||||
| Grade 1–3 | 140 | 14 | 12.62 | 1.35 (0.79–2.30) | 1.41 (0.83–2.40) |
| Grade 4–6 | 312 | 34 | 14.29 | 1.53 (1.08–2.16) | 1.48 (1.04–2.09) |
| Mental | |||||
| Grade 1–3 | 132 | 12 | 12.56 | 1.35 (0.76–2.39) | 1.82 (1.01–3.29) |
| Grade 4–6 | 2 | 0 | - | - | - |
| Others | |||||
| Grade 1–3 | 114 | 19 | 23.61 | 2.54 (1.61–4.01) | 2.70 (1.68–4.34) |
| Grade 4–6 | 62 | 6 | 11.54 | 1.23 (0.55–2.75) | 2.08 (0.92–4.69) |
Abbreviation: CI, confidence interval; HR, hazard ratio; Ref, reference.
*Adjusted for age, Charlson comorbidity index, income, place of residence, cancer stage, chemotherapy, and radiotherapy.
Discussion
To our knowledge, this was the first study to analyze the disparities in diagnosis and mortality risks between cervical cancer patients with and without disabilities, considering individual characteristics. Our study showed that women with cervical cancer with disabilities, especially with severe disabilities, were diagnosed at later stages, received less treatment, and had higher overall mortality rates, compared with women who lacked disabilities. The strength of our study was that we used national disability registration, national cancer registration, and national health insurance corporation data, which are reliable data from large nationwide samples.
In this study, we found that cervical cancer was diagnosed at more advanced stages in patients with severe disability. This finding is consistent with the results of previous studies.23,24 People with disabilities have several barriers to medical care including inaccessibility of some facilities, lack of availability of transportation, poor knowledge and negative attitude of healthcare providers, and lack of knowledge of the patient or caregiver.13,34-36 In this study, severe communication and physical/brain disabilities were strongly associated with the stage at diagnosis. A recent study reported that the cervical cancer screening rate was markedly lower in women with severe disabilities in Korea (aOR 0.42, 95% CI 0.42–0.42). 12 Other studies have also reported similar findings regarding low rates of cancer screenings.15,19,22,37 We suspected that the low screening rates in disabled women may significantly contribute to the late diagnosis of cervical cancer in patients with severe disabilities. To overcome these barriers in medical care and cancer screening, there is a need to develop policy actions such as increasing the number of public screening facilities with accessible medical equipment, providing transportation support, addressing stereotyping by healthcare providers, and educating patients and caregivers about the importance of screening.34,35,38,39
In our study, women with disability were more likely to be diagnosed with an unknown stage of cervical cancer. “Unknown stage” means that there is insufficient information to determine the stage because of a lack of proper staging evaluation. This situation leads to patients with unknown-stage cancer to not receive proper treatment. A previous study showed that patients with older age, lower socioeconomic status, or residence in vulnerable areas were more likely to be diagnosed with unknown-stage cancer. 40 Disabilities should not lead to passivity in cancer diagnostic work up. Education on how to support patients with disabilities should be provided to healthcare professionals and families, to improve the observed disparities in cervical cancer diagnosis. In the United States, The Americans with Disabilities Act (ADA) mandates that healthcare providers offer reasonable accommodations to ensure that persons with disabilities have the same access to services as those without disabilities. 41 For example, “A guide to caring for people with disabilities” by center for disabilities studies, university of Delaware, provide various guidance such as “understanding medical information,” “positioning during a procedure,” and “A sign language interpreter.” 42
Women with disabilities were less likely to undergo surgery and chemotherapy and more likely to remain without treatment. This implies that disability seriously affects treatment decisions. Communication impairment can limit access to information about treatment or can limit conversations with healthcare professionals. 41 Patients with mental disability might have limitations in their understanding of the disease. 43 Therefore, healthcare professionals must maintain an encouraging attitude toward these patients by allowing adequate time for each patient and using repetition, precise explanations, and simple language. 42 It may be helpful to adjust the communication and decision-making process to fit the needs of cancer patients with disabilities. 43 In our analysis, there were no significant differences in radiation treatment (aOR 0.95, 95% CI 0.85–1.05) (Table 3) between patients with and without disabilities, even in those with localized disease. Radiation therapy might be more often selected for patients with disabilities with early-stage cancer because it is considered more tolerable.
Even after adjustment for factors (age, comorbidity, income, residence, stage, and treatment), the overall mortality risk from cervical cancer was higher in patients with disabilities (aHR 1.36). Specifically, among those with severe disabilities (aHR 1.72), the overall mortality risk was markedly higher in patients with severe mental disabilities (aHR 2.46) and severe cardiopulmonary disabilities (aHR 3.30). We suggest several reasons for these disparities, including less extensive surgery or lower dose of chemoradiation treatment, insufficient adjustment of comorbidity or poor health behavior in the current study, lack of self-care or low treatment compliance among patients, and lack of supportive care.44-46 Furthermore, previous data indicated that higher cervical cancer incidence and mortality rates are associated with lower socioeconomic status. 47 Women with disabilities are likely to have lower socioeconomic status, lower education level, and less medical use. Although the Medical-Aid program targets individuals with the lowest income levels in Korea, there remain low-income people who do not receive necessary medical services. 48 Therefore, economic support and social support for proper healthcare usage in women with disabilities are needed to improve the disparities.
According to the Surveillance, Epidemiology, and End Results (SEER), 49 localized stage means that the tumor is confined to the cervix uteri (stage 1A and 1B in the International Federation of Gynecology and Obstetrics (FIGO] classification). 50 Surgery for localized-stage cervical cancer is performed with a curative intent. In our study, the overall mortality risk of localized disease treated with surgery was significantly higher in patients with severe disabilities (aHR 1.55). We suggest several possible reasons for this result. It is possible that patients with severe disabilities underwent less extensive surgery or failed to undergo the proper routine follow-up schedule for determining recurrence. Further, adjuvant treatment may be necessary depending on the result of postoperative biopsy in early-stage cervical cancer; however, this may not have been done properly. Therefore, the importance of posttreatment care and follow-up, as well as diagnosis and treatment, should not be overlooked in patients with disabilities, especially those with severe disabilities.
Recent studies of disparities in lung and prostate cancer did not reveal any differences in cancer stages between patients with and without disabilities.25,51 On the other hand, in our study, the distant metastatic stage was more common in patients with cervical cancer with severe disabilities (grade 1). These differences reflect the importance of cervical cancer screening for early diagnosis. Cervical cancers can be screened effectively 52 and are preventable by using the human papillomavirus vaccine. 53 This may reduce disparities between cervical cancer patients with and without disabilities. The World Health Organization has set a target of cervical cancer elimination for all countries, through the scale-up of 90-70-90 targets: 90% of young women should be vaccinated, 70% of women should be screened, and 90% of women should receive adequate treatment, if required. 54 This could be a good strategy for reducing disparities between cervical cancer patients with and without disabilities.
Limitations
Our study has several limitations. First, information on the diagnosis and treatment decisions of the study patients was not available. We could not identify the reasons why some patients with unknown-stage cancer at diagnosis did not undergo diagnostic tests for staging, or why specific patients who remained without treatment did not undergo surgery, chemotherapy, or radiation treatment. Second, we were unable to identify the FIGO stage because we used the SEER staging of the KCCR. Therefore, it was unknown whether the patients were treated based on guidelines. Third, information on preoperative health conditions, postoperative care, and medical compliance, which affect the treatment outcome, was not available. Fourth, we excluded patients who became disabled after the cervical cancer diagnosis. However, some of these patients may not have developed disability because of cervical cancer. Furthermore, the use of national health insurance data excluded patients who paid directly for their treatment or participated in clinical trials. Therefore, our findings are not completely representative of the treatment approaches for patients with cervical cancer, although this was the first study to examine the effects of disabilities on the diagnosis and treatment of cervical cancer. Fifth, we used overall mortality, not cancer-specific mortality, because of limitations regarding the available data. Using overall mortality is a limitation because women with disabilities have a higher risk of death due to factors other than cervical cancer, and therefore we may be overestimating the impact in this analysis. In future studies, cancer-specific mortality should be investigated to improve the understanding of the effects of disabilities on the diagnosis and treatment of cervical cancer. Finally, because of limitations concerning data access, we could not obtain information regarding the number of disabilities present in each patient; only one major disability was analyzed for each patient. It is possible that patients with multiple disabilities had a worse prognosis for cervical cancer.
Conclusion
Women with cervical cancer with disabilities, especially severe disabilities, were diagnosed with more advanced stage or unknown stage of cervical cancer, received less treatment, and had higher overall mortality than those without disabilities. Women with disabilities, their families, and healthcare professionals need to be educated to improve their awareness of the diagnosis and treatment of diseases in this patient population. Social support and policies related to the healthcare for women with disabilities are also needed. Furthermore, efforts are important for prevention and cervical cancer screening.
Acknowledgments
We thank the Korean National Health Insurance Services for their provision of data.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the R&D grant (No. 2016007) on rehabilitation by Korea National Rehabilitation Center Research Institute, Ministry of Health & Welfare, and the National Research Foundation of Korea (NRF) grant funded by the Ministry of Education (No. 2019R1D1A3A03103862, 2020R1I1A1A01054268) and by the Korea government (MSIT) (No. 2019R1A2C1087507). Funders had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
ORCID iD
Jong Hyock Park https://orcid.org/0000-0003-3247-0827
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2021;71(3):209-249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. The Lancet Global Health. 2020;8(2):e191-e203. doi: 10.1016/S2214-109X(19)30482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hong S, Won Y-J, Lee JJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2018. Cancer Res Treat. 2021;53(2):301-315. doi: 10.4143/crt.2021.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell MF, Tortolero-Luna G, Cook E, Whittaker L, Rhodes-Morris H, Silva E. A randomized clinical trial of cryotherapy, laser vaporization, and loop electrosurgical excision for treatment of squamous intraepithelial lesions of the cervix. Obstet Gynecol. 1998;92(5):737-744. [PubMed] [Google Scholar]
- 5.Berek JS. Berek & Novak’s Gynecology. 15th ed.. Philadelphia, PA: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 6.Anderson DMLJ, Elkas JC. Berek & Novak’s Gynecology. 16th ed.. Alphen aan den Rijn, Netherlands: Wolters Kluwer; 2020:1048-1055. [Google Scholar]
- 7.Lim MC, Lee M, Shim SH, et al. Practice guidelines for management of cervical cancer in Korea: a Korean Society of gynecologic oncology Consensus Statement. J Gynecol Oncol. May 2017;28(3):e22. doi: 10.3802/jgo.2017.28.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quinn M, Benedet J, Odicino F, et al. Carcinoma of the cervix uteri. Int J Gynecol Obstet. 2006;95(suppl 1):S43-S103. doi: 10.1016/s0020-7292(06)60030-1. [DOI] [PubMed] [Google Scholar]
- 9.National Cancer Center . National Cancer Center Home Page [Internet]. Goyang, Korea: National Cancer Center. https://ncc.re.kr. [Google Scholar]
- 10.Horner-Johnson W, Dobbertin K, Iezzoni LI. Disparities in receipt of breast and cervical cancer screening for rural women age 18 to 64 with disabilities. Wom Health Issues. 2015;25(3):246-253. doi: 10.1016/j.whi.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Horner-Johnson W, Dobbertin K, Lee JC, Andresen EM. Disparities in health care access and receipt of preventive services by disability type: analysis of the medical expenditure panel survey. Health Serv Res. 2014;49(6):1980-99. doi: 10.1111/1475-6773.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shin DW, Lee J-W, Jung JH, et al. Disparities in cervical cancer screening among women with disabilities: a national database study in South Korea. J Clin Oncol. 2018;36(27):2778-2786. doi: 10.1200/jco.2018.77.7912. [DOI] [PubMed] [Google Scholar]
- 13.Wei W, Findley PA, Sambamoorthi U. Disability and receipt of clinical preventive services among women. Wom Health Issues. 2006;16(6):286-296. doi: 10.1016/j.whi.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosseinpoor AR, Williams JS, Jann B, et al. Social determinants of sex differences in disability among older adults: a multi-country decomposition analysis using the World Health Survey. Int J Equity Health. 2012;11(1):52-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park J-H, Lee J-S, Lee J-Y, et al. Disparities between persons with and without disabilities in their participation rates in mass screening. Eur J Publ Health. 2009;19(1):85-90. doi: 10.1093/eurpub/ckn108. [DOI] [PubMed] [Google Scholar]
- 16.Lee JY, Jeong J, Kim YK, et al. Has disabled access in healthcare institutions been increased? - A case study of Jongno-gu in Seoul, Korea -. Kor J Health Policy Admin. 2012;22(4):696-702. [Google Scholar]
- 17.Verger P, Aulagnier M, Souville M, et al. Women with disabilities. Am J Prev Med. 2005;28(2):215-220. doi: 10.1016/j.amepre.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 18.Scheer J, Kroll T, Neri MT, Beatty P. Access barriers for persons with disabilities. J Disabil Pol Stud. 2003;13(4):221-230. [Google Scholar]
- 19.Kushalnagar P, Engelman A, Simons AN. Deaf Women's Health: Adherence to Breast and Cervical Cancer Screening Recommendations. Am J Prev Med. 2019;57(3):346-354. doi: 10.1016/j.amepre.2019.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shin DW, Yu J, Cho J, et al. Breast cancer screening disparities between women with and without disabilities: a national database study in South Korea. Cancer. 2020;126(7):1522-1529. doi: 10.1002/cncr.32693. [DOI] [PubMed] [Google Scholar]
- 21.Kim Y, Shin DW, Kim HW, et al. Disparities in gastric cancer screening among people with disabilities: a national registry-linkage study in South Korea. Gastric Cancer. 2020;23(3):497-509. doi: 10.1007/s10120-019-01017-8. [DOI] [PubMed] [Google Scholar]
- 22.Fujiwara M, Inagaki M, Nakaya N, et al. Cancer screening participation in schizophrenic outpatients and the influence of their functional disability on the screening rate: a cross-sectional study in Japan. Psychiatr Clin Neurosci. 2017;71(12):813-825. doi: 10.1111/pcn.12554. [DOI] [PubMed] [Google Scholar]
- 23.Park BR, Kim SY, Shin DW, Yang HK, Park JH. Influence of socioeconomic status, comorbidity, and disability on late-stage cancer diagnosis. Osg Public Health Res Perspect. 2017;8(4):264-270. doi: 10.24171/j.phrp.2017.8.4.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim HW, Shin DW, Yeob KE, et al. Disparities in the diagnosis and treatment of gastric cancer in relation to disabilities. Clin Transl Gastroenterol. 2020;11(10):e00242. doi: 10.14309/ctg.0000000000000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shin DW, Cho JH, Noh JM, et al. Disparities in the diagnosis and treatment of lung cancer among people with disabilities. J Thorac Oncol. 2019;14(2):163-175. doi: 10.1016/j.jtho.2018.10.158. [DOI] [PubMed] [Google Scholar]
- 26.Kwon J, Kim SY, Yeob KE, et al. The effect of disability on the diagnosis and treatment of multiple myeloma in Korea: a national cohort study. Cancer Res Treat. 2020;52(1):1-9. doi: 10.4143/crt.2018.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shin DW, Cho JH, Noh JM, et al. Disparities in the diagnosis and treatment of lung cancer among people with disabilities. J Thorac Oncol. 2019;14(2):163-175. [DOI] [PubMed] [Google Scholar]
- 28.Jeon B, Kwon S, Kim H. Health care utilization by people with disabilities: a longitudinal analysis of the Korea Welfare Panel Study (KoWePS). Disab Health J. 2015;8(3):353-362. [DOI] [PubMed] [Google Scholar]
- 29.Korean Statistical Information Service (KSIS) . National Survey on Persons with Disabilities. Daejeon, Republic of Korea: Korean Statistical Information Service; 2011. [Google Scholar]
- 30.Jung K-W, Won Y-J, Kong H-J, Lee ES. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. 2018;50(2):303-316. doi: 10.4143/crt.2018.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373-383. [DOI] [PubMed] [Google Scholar]
- 32.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258-1267. [DOI] [PubMed] [Google Scholar]
- 33.Klabunde CN, Legler JM, Warren JL, Baldwin L-M, Schrag D. A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol. 2007;17(8):584-590. [DOI] [PubMed] [Google Scholar]
- 34.Merten JW, Pomeranz JL, King JL, Moorhouse M, Wynn RD. Barriers to cancer screening for people with disabilities: a literature review. Disab Health J. 2015;8(1):9-16. doi: 10.1016/j.dhjo.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 35.Ramjan L, Cotton A, Algoso M, Peters K. Barriers to breast and cervical cancer screening for women with physical disability: a review. Women Health. 2016;56(2):141-156. doi: 10.1080/03630242.2015.1086463. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization . Promoting Sexual and Reproductive Health for Persons with Disabilities: WHO/UNFPA Guidance Note. Geneva. Switzerland: World Health Organization; 2009. [Google Scholar]
- 37.Shin DW, Chang D, Jung JH, et al. Disparities in the participation rate of colorectal cancer screening by fecal occult blood test among people with disabilities: a national database study in South Korea. Cancer Res Treat. 2020;52(1):60-73. doi: 10.4143/crt.2018.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iezzoni LI, Kurtz SG, Rao SR. Trends in pap testing over time for women with and without chronic disability. Am J Prev Med. 2016;50(2):210-219. doi: 10.1016/j.amepre.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen AQ, Mandigo M, Coleman JS. Cervical cancer screening for women with disabilities: time for a new approach? J Low Genit Tract Dis. 2018;22(4):318-319. [DOI] [PubMed] [Google Scholar]
- 40.Luo Q, Yu XQ, Cooke-Yarborough C, Smith DP, O’Connell DL. Characteristics of cases with unknown stage prostate cancer in a population-based cancer registry. Cancer Epidemiol. 2013;37(6):813-819. doi: 10.1016/j.canep.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 41.Withers J, Speight C. Health care for individuals with hearing loss or vision loss. N C Med J. 2017;78(2):107-112. doi: 10.18043/ncm.78.2.107. [DOI] [PubMed] [Google Scholar]
- 42.Riddle I, Romelczyk S, Sparling E. Effective Communication for Health Care Providers: A Guide to Caring for People with Disabilities. Newark, DE: Center for Disabilities Studies, University of Delaware; 2011. [Google Scholar]
- 43.Bailey R, Willner P, Dymond S. A visual aid to decision-making for people with intellectual disabilities. Res Dev Disabil. 2011;32(1):37-46. doi: 10.1016/j.ridd.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 44.Iezzoni LI, Ngo LH, Li D, Roetzheim RG, Drews RE, McCarthy EP. Treatment disparities for disabled medicare beneficiaries with stage I non-small cell lung cancer. Arch Phys Med Rehabil. 2008;89(4):595-601. doi: 10.1016/j.apmr.2007.09.042. [DOI] [PubMed] [Google Scholar]
- 45.Iglay K, Santorelli ML, Hirshfield KM, et al. Impact of preexisting mental illness on all-cause and breast cancer-specific mortality in elderly patients with breast cancer. J Clin Oncol. 2017;35(36):4012-4018. doi: 10.1200/jco.2017.73.4947. [DOI] [PubMed] [Google Scholar]
- 46.Alfred Haynes B M, Smedley D. The Unequal Burden of Cancer: An Assessment of NIH Research and Programs for Ethnic Minorities and the Medically Underserved. Washington, DC: The National Academies Press; 1999. [PubMed] [Google Scholar]
- 47.Singh GU, Miller BA, Hankey BF, Edwards BK. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975-2000. Cancer. 2004;101(5):1051-1057. doi: 10.1002/cncr.20467. [DOI] [PubMed] [Google Scholar]
- 48.Choi JW, Park EC, Chun SY, Han KT, Han E, Kim TH. Health care utilization and costs among medical-aid enrollees, the poor not enrolled in medical-aid, and the near poor in South Korea. Int J Equity Health. 2015;14(1):128-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.YoungJr JL, Roffers SD, Ries LAG, Fritz AG, Hurlbut AA, eds. SEER Summary Staging Manual - 2000: Codes and Coding Instructions. Bethesda, MD: National Cancer Institute, NIH Pub. No. 01-4969; 2001. [Google Scholar]
- 50.Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynecol Obstet. 2009;105(2):107-108. doi: 10.1016/j.ijgo.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 51.Shin DW, Park J, Yeob KE, et al. Disparities in prostate cancer diagnosis, treatment, and survival among men with disabilities: retrospective cohort study in South Korea. Disab Health J. 2021;14:101125. doi: 10.1016/j.dhjo.2021.101125. [DOI] [PubMed] [Google Scholar]
- 52.Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev. 2013;2:35. doi: 10.1186/2046-4053-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Angioli R, Lopez S, Aloisi A, et al. Ten years of HPV vaccines: state of art and controversies. Critic Rev Oncol Hematol J. 2016;102:65-72. doi: 10.1016/j.critrevonc.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 54.World Health Organization . Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Geneva, Switzerland: World Health Organization. 2020; [Google Scholar]