Abstract
COVID-19 vaccines have been granted emergency use authorization for children ages 5 years and older. To understand how racially and ethnically diverse parents of young children enrolled in Medicaid feel about a prospective COVID-19 vaccine for their children, we administered an online survey that included both close-ended and open-ended items to a statewide sample in Florida (n = 1951). We used quantitative responses to conduct a statistical audience segmentation analysis that identified five distinct sub-groups that varied widely in the likelihood that they would get a COVID-19 vaccine for their child. Qualitative responses were used to illustrate differences between the groups. The youngest Black and White mothers were least likely to vaccinate their child (24%), followed by Black and White mothers in their early 30s (36%), younger Hispanic and mixed-race or other race parents (45%), older mothers (48%) and older fathers (71%). Unique challenges to building vaccine confidence emerged for each group. The youngest Black and White mothers were more likely to report their lives being worse during the COVID-19 pandemic, were far more negative and less positive about a COVID-19 vaccine, and were more concerned about paying bills than preventing COVID-19. Younger Hispanic and mixed-race parents were less negative, but more likely to use emotional language (e.g., scared, nervous, worried) talking about a COVID-19 vaccine, and more likely to report that protecting their child's health was their top concern. Recommendations are made for applying the insights gained in outreach and education efforts.
Keywords: COVID-19, Vaccination, Medicaid, Children, Health communication
1. Introduction
Clinical trials testing the safety and effectiveness of COVID-19 vaccines for children as young as 6 months old are underway (Bever, 2021), and have been granted emergency use authorization for children age 5 years and older (U.S. Centers for Disease Control and Prevention, 2021; U.S. Food and Drug Administration, 2021). While hesitancy about adult COVID-19 vaccination is well documented (Khubchandani et al., 2021; AP-NORC Center for Public Affairs Research, 2020; AP-NORC Center for Public Affairs Research, 2021), less is known about parents' beliefs and intentions about vaccinating their young children. One in five children in the United States have a vaccine hesitant parent (Santibanez et al., 2020), and recent surveys among U.S. parents have found that about half plan to vaccinate their children against COVID-19 when a vaccine becomes available (Ruggiero et al., 2021; Teasdale et al., 2021). Low-income parents and parents of younger children have been found to be more vaccine hesitant (Santibanez et al., 2020; Ruggiero et al., 2021), and low-income parents are less likely to plan to vaccinate their child against COVID-19 (Teasdale et al., 2021). Therefore, this paper aims to provide actionable insights to increase confidence about COVID-19 vaccination among parents of young children in Medicaid by: (1) using classification tree analysis to detect easily identifiable sub-groups that vary in likelihood to vaccinate their young children; and (2) examining sources of hesitancy among the sub-groups that can be addressed in education, outreach, messaging and vaccine delivery strategies.
2. Methods
We developed and administered a cross-sectional online survey to all parents and guardians (hereafter, parents) of Florida Sunshine Health Medicaid members ages 0–5 years old. The survey focused on pediatric health care visits during COVID-19, and COVID-19 vaccination of children, the focus of this report. The survey also elicited qualitative responses. We sent e-mail invitations with a survey link to 32,761 members, and 1951 completed a survey (99 in Spanish) between January 13 and January 31, 2021. Respondents who provided contact information (n = 1698) were e-mailed a $9.99 Walmart e-gift card. Study materials and protocols were reviewed and approved by Washington University's IRB as exempt.
2.1. Measures
2.1.1. Survey items
Two items assessed intentions for vaccinating one's child for COVID-19. The first assessed likelihood: If an approved vaccine that protected your child from COVID-19 was available for free, how likely would you be to get it for your child? (highly likely/somewhat likely/somewhat unlikely/highly unlikely). The second assessed urgency: I would rush to get an approved vaccine to prevent COVID-19 for my child (strongly agree/agree/disagree/strongly disagree).
Two items assessed beliefs about the COVID-19 vaccine: Getting my child vaccinated to prevent COVID-19 is important; The benefits of an approved vaccine to prevent COVID-19 would outweigh any rare side effects (strongly agree/agree/disagree/strongly disagree).
To understand how the pandemic had affected their lives, participants were asked: Since the spread of COVID-19 in mid-March, how have things changed for you or people in your household? (much better/somewhat better/no change/somewhat worse/much worse). We assessed this in 16 separate areas: childcare, emotional health, getting food or other daily necessities, getting medical care, happiness, household relationships, housing, money, physical activity or exercise, physical health, sleep, social life, stress, taking care of older relatives, transportation, and work.
A single item assessed respondents greatest concern right now, allowing them to choose one answer from a list that included employment, childcare, caring for older relatives, paying bills, avoiding getting COVID-19, managing your current health conditions, protecting your child's health and other.
For all of the above items, “not sure” and/or “prefer not to answer” were also response options. For items about children, respondents with more than one child age 0–5 years were instructed to respond about their youngest child. The survey also assessed respondents' age, gender, race, ethnicity, and education level.
2.1.2. Qualitative responses
Immediately following the COVID-19 survey items, respondents were asked: Is there anything else you would like to share with us about vaccines and your child? Participants entered qualitative responses in free text. Responses in Spanish were translated to English, and all responses were content analyzed.
2.2. Analyses
2.2.1. Audience segmentation
We used the CTree function of the partykit package in R, version 3.6.1, to create a conditional inference tree identifying sub-groups of survey respondents that were similar in their likelihood of getting their child vaccinated for COVID-19. Classification and regression tree methods divide a population into sub-groups that are increasingly similar with respect some outcome variable of interest, based on a predetermined set of predictor variables (Biggs et al., 1991). This process continues until no further splits are possible; each final sub-group is considered a terminal node. CTree analysis uses a statistical approach to recursive partitioning, with splits based on significance testing. First, all predictor variables are compared to the outcome and the predictor variable most strongly associated with the outcome (smallest statistically significant p-value) is selected. Second, an optimal binary split of the predictor variable is created to maximize goodness-of-fit for the resulting sub-groups. These two steps are repeated recursively until there are no more statistically significant splits (α = 0.05) (Hothorn et al., 2006).
The outcome variable of the conditional inference tree was dichotomized as “highly likely” and “somewhat likely” to get the COVID-19 vaccine for my child vs. “highly unlikely,” “somewhat unlikely” and “not sure.” Seven survey items were used as predictor variables in the CTree analysis: age (continuous, 18–71), race/ethnicity (non-Hispanic White/ non-Hispanic Black/ Hispanic/ mixed or other race), gender (female/male), education (≤ high school or GED/ some trade school or college/ ≥ college degree), number of children under age 5 years (continuous, range: 1–4+ children), greatest current concern (“protecting your child's health” / all other concerns), and number of life domains that had become “much worse” during the COVID-19 pandemic (continuous, range: 0–16). Missing data were handled with listwise deletion. Most participants (80%, n = 1553) had complete data on all predictor and outcome variables.
2.2.2. Content analysis of qualitative responses
Qualitative responses were coded for expressions of concern about the vaccine, plans to wait for or delay vaccination until later, and desire for more information about the vaccine. These were selected because at the time of the survey, one-in-three Americans were taking a wait-and-see approach to the adult vaccine, concerns about side effects were the top reasons for vaccine hesitancy, and those opposed to the vaccine cited its newness and not having enough information about it as major reasons for not getting vaccinated (Kaiser Family Foundation, 2021). Because Americans were expressing strong feeling and opinions about the vaccine – both pro and con – we also coded each qualitative response for polarity (Cacioppo et al., 1981) and emotional language.
To reduce potential bias, pairs of trained coders independently evaluated qualitative responses, then resolved discrepancies through discussion and consensus. Coders first determined whether each qualitative response addressed COVID-19 vaccination. Responses that did were then coded for polarity (positive, negative or neutral/mixed); concerns about the vaccine (presence or absence of comments about side effects, rushed vaccine development/newness); wanting more information about the vaccine (presence or absence); waiting until later to decide about or get the vaccine (presence or absence); and use of emotional language, such as feeling scared, nervous, worried, stressed or conflicted (presence or absence). A single response could express more than one of these variables; for example, “Kinda scared about the side effects it may cause” would be coded as present for concern about side effects and emotional language.
Descriptive statistics are reported for the full survey sample and for each of the terminal nodes resulting from the CTree analysis. These include demographic characteristics of participants, survey item responses and coding categories for qualitative responses.
3. Results
3.1. Sample
Nearly all respondents were women (96%), evenly distributed among African American, Hispanic and White race/ethnicity. The mean age of the sample was 31.9 years, and 30% reported completing 12 or fewer years of education (Table 1 ). Comparing respondents to non-respondents among those for whom race/ethnicity was known by the health plan, the proportions of Hispanics (33% vs. 32%, respectively) and Whites (31% vs. 28%) were similar, but African Americans were underrepresented among respondents (29% vs. 38%).
Table 1.
Demographics and survey responses for full sample and five segmentation sub-groups.
| Five sub-groups from audience segmentation analysis |
|||||||
|---|---|---|---|---|---|---|---|
| All (n = 1951) | ≤ 30 Black, white (n = 470) | 31–34 Black, white (n = 266) | ≤ 34 Hispanic, mixed, other (n = 461) | > 34 Female (n = 498) | > 34 Male (n = 48) | p-value | |
| Mean age in years (n = 1951) | 31.9 | 26.3 | 32.5 | 28.0 | 39.2 | 44.9 | <0.001 |
| % female (n = 1737) | 96% | 99% | 99% | 99% | 100% | 0% | <0.001 |
| Race/ethnicity (n = 1720) | |||||||
| % non-Hispanic white | 31% | 46% | 54% | 0% | 34% | 42% | <0.001 |
| % non-Hispanic black or African American | 29% | 55% | 46% | 0% | 23% | 10% | |
| % Hispanic, Latino, Latina (any race) | 33% | 0% | 0% | 84% | 35% | 33% | |
| % another race or mixed race | 7% | 0% | 0% | 16% | 7% | 15% | |
| Education (n = 1733) | |||||||
| % ≤ high school/GED | 30% | 40% | 25% | 31% | 24% | 13% | <0.001 |
| % some technical/trade school or some college | 39% | 38% | 39% | 39% | 37% | 34% | |
| % ≥ college degree | 32% | 21% | 37% | 30% | 39% | 53% | |
| COVID-19 vaccine beliefsa | |||||||
| Getting my child vaccinated is important (n = 1630) | 47% | 35% | 44% | 54% | 53% | 75% | <0.001 |
| Benefits of vaccine outweigh rare side effects (n = 1666) | 32% | 23% | 30% | 34% | 37% | 68% | <0.001 |
| Intention to get an approved, free COVID-19 vaccine | |||||||
| % likely/very likely to get it for my child (n = 1731) | 38% | 23% | 34% | 44% | 46% | 69% | <0.001 |
| % agree/strongly agree would rush to get it for my child (n = 1672) | 35% | 24% | 30% | 42% | 40% | 67% | <0.001 |
| COVID-19 made life “much worse” in these ways…b | |||||||
| % social life (n = 1732) | 41% | 38% | 44% | 40% | 41% | 43% | 0.596 |
| % money (n = 1727) | 35% | 40% | 31% | 35% | 31% | 28% | 0.016 |
| % stress (n = 1734) | 34% | 38% | 31% | 36% | 30% | 28% | 0.045 |
| % work (n = 1712) | 26% | 29% | 25% | 28% | 23% | 26% | 0.195 |
| % childcare (n = 1714) | 23% | 31% | 24% | 23% | 16% | 21% | <0.001 |
| % emotional health (n = 1731) | 17% | 19% | 17% | 15% | 15% | 19% | 0.556 |
| % happiness (n = 1718) | 17% | 20% | 16% | 14% | 16% | 21% | 0.212 |
| % physical activity or exercise (n = 1740) | 16% | 17% | 13% | 17% | 17% | 9% | 0.518 |
| % sleep (n = 1737) | 16% | 21% | 13% | 14% | 15% | 11% | 0.010 |
| % housing (n = 1727) | 16% | 20% | 15% | 16% | 12% | 9% | 0.007 |
| % taking care of older relatives (n = 1672) | 14% | 18% | 14% | 11% | 13% | 14% | 0.033 |
| % household relationships (n = 1724) | 12% | 14% | 13% | 11% | 9% | 13% | 0.182 |
| % getting food or other daily necessities (n = 1735) | 10% | 13% | 9% | 10% | 7% | 9% | 0.049 |
| % getting medical care (n = 1735) | 9% | 10% | 8% | 9% | 8% | 4% | 0.622 |
| % physical health (n = 1738) | 9% | 10% | 8% | 9% | 9% | 9% | 0.943 |
| % transportation (n = 1740) | 8% | 10% | 7% | 8% | 8% | 4% | 0.508 |
| Mean sum of “much worse” items (n = 1771) | 2.9 | 3.4 | 2.8 | 2.9 | 2.6 | 2.6 | 0.022 |
| Greatest concern right now (n = 1795) | |||||||
| Paying bills | 27% | 32% | 29% | 18% | 27% | 15% | 0.002 |
| Protecting child's health | 27% | 25% | 29% | 30% | 25% | 38% | |
| Avoiding getting COVID-19 | 19% | 14% | 17% | 18% | 27% | 15% | |
| Employment | 8% | 8% | 8% | 9% | 6% | 4% | |
| Childcare | 6% | 8% | 8% | 6% | 5% | 10% | |
| Managing current health conditions | 2% | 3% | 2% | 1% | 3% | 2% | |
| Caring for older relatives | 1% | 1% | 0% | 1% | 1% | 2% | |
| Other | 5% | 4% | 5% | 5% | 4% | 2% | |
Note: Ns from subgroups sum to 1743, 208 respondents could not be classified due to missing demographic data.
Percent “agree” or “strongly agree”.
Percent “much worse”.
3.2. Survey responses
Interest in a COVID-19 vaccine for children was low: 47% of respondents agreed or strongly agreed that it is important to get their child vaccinated to prevent COVID-19, 38% reported being very likely or likely to get it for their child, and 32% agreed or strongly agreed that the benefits of an approved vaccine would outweigh any rare side effects (Table 1).
COVID-19 had a major impact on respondents' lives. Large proportions reported that COVID-19 made their life “much worse,” especially in terms of social life (41%), money (35%), stress (34%), work (26%) and childcare (23%) (Table 1). Respondents' greatest concerns were paying bills and protecting their child's health (both selected by 27% of respondents), followed by avoiding getting COVID-19 (19%), employment (8%) and childcare (6%).
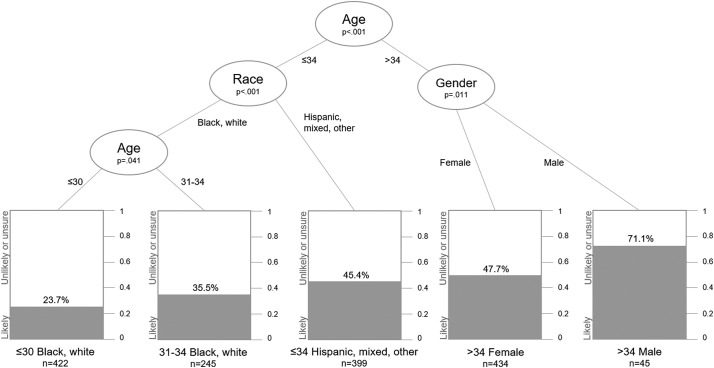
3.3. Audience segmentation
The CTree analysis resulted in five terminal nodes, or sub-groups, that varied widely in the proportion of members who reported being very likely or likely to get a COVID-19 vaccine for their child (Fig. 1 ). Analyses first split the sample into two groups, by age. The CTree analysis determined the optimal split occurred between those 34 and younger vs. those over 34. Younger parents were then split again by race/ethnicity, with Black and White parents forming one sub-group and Hispanic, mixed and other race parents forming the other. The sub-group of Black and White parents was then split again on age, creating one group age 30 and younger, and a second group age 31–34. Older parents also were split again, but on gender (female/male). The resulting groups and the proportion of each being very likely or likely to get their child vaccinated were:
-
•
Black and White parents, age 30 and younger (24% very likely or likely to vaccinate child);
-
•
Black and White parents, age 31–34 (36%);
-
•
Hispanic, mixed and other race parents, age 34 and younger (45%);
-
•
Female parents over age 34 (48%); and
-
•
Male parents over age 34 (71%).
Fig. 1.
Audience segmentation: Five sub-groups varying by likelihood of sub-group members getting the COVID-19 vaccination for their child under age 5.
Note: Listwise deletion resulted in a subsample of n = 1553 used in the CTree analysis.
3.4. Qualitative responses
Of the 1951 survey respondents, 1053 (54%) entered some text in response to the qualitative question, of which 51 were translated from Spanish to English. Most responses (n = 661) were not substantive (e.g., “thank you,” “not at this time,” “nothing else”) and were excluded from analysis. Of the 392 remaining responses, 60 were not about COVID-19 (e.g., “I don't want my child to get flu vaccine”) and also were excluded. This left a final sample of 332 qualitative responses.
Negative comments outnumbered positive comments 2:1 (Table 2 ). One in four comments (26%) mentioned vaccine side effects and 22% mentioned the vaccine being new or rushed. Among parents concerned about the vaccine being new or rushed, more parents expressed concern about it being new with little track record (75%) than concern about its development being rushed (44%). Roughly one in five comments mentioned waiting until sometime in the future to get the vaccine (18%) or wanting more information about the vaccine (21%); 17% of comments used emotional language (e.g., “It's scary because information is so limited”).
Table 2.
Content analysis of qualitative comments for full sample and five segmentation sub-groups.
| Five sub-groups from audience segmentation analysis |
|||||||
|---|---|---|---|---|---|---|---|
| All (n = 332) | ≤ 30 Black, white (n = 71) | 31–34 Black, white (n = 44) | ≤ 34 Hispanic, mixed, other (n = 80) | > 34 Female (n = 121) | > 34 Male (n = 12) | p-value | |
| Spanish language (n = 332) | 5% | 0% | 0% | 4% | 9% | 17% | 0.006 |
| Polarity (n = 332) | 0.171 | ||||||
| Positive | 23% | 16% | 16% | 26% | 26% | 42% | |
| Neutral/mixed | 32% | 32% | 36% | 29% | 31% | 50% | |
| Negative | 46% | 52% | 48% | 45% | 44% | 8% | |
| Concerns about COVID-19 vaccine | |||||||
| Known or potential side effects (n = 332) | 26% | 23% | 27% | 30% | 24% | 33% | 0.838 |
| Rushed or new (n = 332) | 22% | 17% | 27% | 29% | 20% | 0% | 0.103 |
| It is new with little track record (n = 72) | 75% | 58% | 67% | 78% | 88% | NA | |
| Development was rushed (n = 72) | 44% | 50% | 50% | 39% | 42% | NA | |
| Wants more information about vaccine (n = 332) | 21% | 20% | 14% | 21% | 22% | 33% | 0.601 |
| Mentions waiting until future date for vaccine (n = 332) | 18% | 21% | 18% | 15% | 18% | 8% | 0.787 |
| Uses emotional languagea (n = 332) | 17% | 13% | 5% | 21% | 22% | 8% | 0.055 |
Note: Ns from subgroups sum to 328, four respondents could not be classified due to missing demographic data.
Emotional language = scared, nervous, worried, stressed, conflicted.
3.5. Understanding the sub-groups
Table 1, Table 2, respectively, also report survey and qualitative responses by the five sub-groups that emerged from the segmentation analysis in Fig. 1. These data provide an initial profile of the five groups.
The first sub-group, comprised of the youngest Black and White parents, had lower levels of education than all other groups. They were the least likely of any group to believe that getting their child vaccinated for COVID-19 was important, or that the benefits of an approved, free vaccine outweigh any rare side effects. More than the other groups, they reported that COVID had made their lives “much worse,” especially in the areas of money, stress, childcare, housing, getting food, sleep, and caring for older relatives. Their greatest concern was “paying bills,” which was selected twice as often as “avoiding getting COVID-19” (32% vs. 14%). In qualitative comments about the vaccine, they had the smallest percentage of positive comments (16%) and largest percentage of negative comments (52%) of any group.
The second sub-group, also Black and White parents but ages 31–34, were more educated and slightly less negative about a COVID-19 vaccine for kids than were younger Black and White parents. Still, less than half felt that getting their child vaccinated for COVID-19 was important. Their top concerns were paying bills and protecting their child's health, both cited by 29% of segment members. In qualitative responses, they were more concerned about the vaccine being rushed or new than were younger parents.
The third sub-group was comprised of parents 34 and younger who were Hispanic (84% of sub-group members) or mixed/other race (16%). Their greatest concern was protecting their child's health. They were more likely than other groups to use emotional language (e.g., scared, nervous, worried) in qualitative comments about the COVID-19 vaccine, and only one-third of members felt that the benefits of a vaccine outweighed any rare side effects. Their qualitative comments were more negative (45%) than positive (26%).
The sub-group of older (> age 34) female parents included a mix of Hispanic (35%), White (34%) and Black (23%) women. Although members of this sub-group were older with more years of education, their vaccine-related beliefs were generally similar to the sub-group of younger Hispanic and mixed or other race parents.
Male parents over age 34 made up a very small proportion of those responding to the survey (<3%), but were most favorable about getting the COVID-19 vaccine for their child. This sub-group was racially and ethnically diverse and had the largest proportion of members with a college degree (53%). Group members widely agreed (75%) that getting their child vaccinated for COVID-19 was important, the largest proportion of any sub-group. It was also the only group in which a majority of members (68%) felt that the benefits of a COVID-19 vaccine outweighed any rare side effects. Of all groups, they had the largest proportion of respondents (38%) report that protecting their child's health was their greatest concern. In qualitative responses provided by group members, positive comments outnumbered negative comments about the COVID-19 vaccine 5-to-1, the only group with a positive ratio. They were also the group least likely to report that COVID-19 had made their life much worse in terms of money, housing, or stress.
4. Discussion
In a racially- and ethnically-diverse sample of parents/guardians of children age 5 and younger in a Medicaid managed care plan in Florida, there was considerable resistance to the idea of getting a COVID-19 vaccination for their child. Fewer than half of respondents felt it was important, fewer than one-third believed the benefits would outweigh any rare side effects, and only 38% said it was very likely or likely that they would get an approved COVID-19 vaccine for their child. Content analysis of parents' qualitative comments about COVID-19 and vaccines found that 46% were negative and only 23% positive. Collectively, these findings suggest a sharply more vaccine-hesitant population than reported in studies of predominantly White college educated parents surveyed during the same time period (Ruggiero et al., 2021).
Using classification tree analysis – a recommended approach for audience segmentation to identify high risk sub-groups for public health outreach (Lemon et al., 2003) – we identified five mutually exclusive sub-groups of parents that varied widely in the likelihood that their child would get the COVID-19 vaccine. Only 24% of the youngest (age ≤ 30) African American and White parents reported being very likely or likely to vaccinate their child, followed by African American and White parents, 31–34 (36%). Hispanic or mixed race or other race parents 34 and younger (45%), and mothers 35 and older (48%) followed. In contrast, a large majority of fathers 35 and older (71%) reported being very likely or likely to vaccinate their child. These sub-groups align closely with findings from other recent studies showing that vaccine hesitancy is highest among parents who are younger and/or have fewer years of education (Teasdale et al., 2021; Reuben et al., 2020), and that male parents are more likely than female parents to report plans to vaccinate their child for COVID-19 (Teasdale et al., 2021).
The five sub-groups were different in important ways that can inform vaccination outreach and communication efforts in clinical and community settings. First, the segmentation findings help prioritize among sub-groups of parents. Younger parents were the least likely to intend to vaccinate their children. It would be very straightforward in most clinical health care settings to flag younger parents to receive additional explanation, discussion or information about the COVID-19 vaccination. Second, the findings identify parent beliefs and concerns that could delay or prevent vaccinating their child. The sub-group of young Black and White mothers were the least likely to believe it is important to vaccinate their child or that vaccine benefits outweighed rare side effects. Introducing new, positive themes about the COVID-19 vaccine could help counterbalance their strongly negative beliefs. In addition, recognizing the broader context of their challenging lives will also help communicators keep vaccination in proper perspective.
Third, the findings suggest potential messengers and partners for addressing vaccine hesitancy. Among the five sub-groups, COVID-19 made life worse in more ways for the sub-group of young Black and White mothers, who also reported that paying bills was a much higher priority to them than COVID-19 prevention. This detrimental impact of COVID-19 on working mothers has been described elsewhere (Bateman and Ross, 2021). Given the group's level of financial strain, there could be value in partnerships that deliver vaccination outreach and education through community social service agencies that assist people with the types of problems they are facing. For example, organizations taking requests for rent or utility payment assistance will likely assess whether there is a child in the household, and when there is, could provide information about vaccines.
Outreach to fathers might also be a priority in building vaccine confidence in low-income families. Although the proportion of men in this study is small, the findings are strong and consistent enough to merit further exploration. It is not clear, for example, how much influence fathers have on healthcare decisions about their children (Matoff-Stepp et al., 2014). Research suggests mothers are more likely than fathers to select their child's doctor, take the child to doctor appointments, assure the child receives doctor-recommended care, and care for a sick child (Kaiser Family Foundation, 2018). At the same time, fathers' attitudes about vaccines can be quite positive, despite having less knowledge about vaccines than mothers (Kornfeld et al., 2013). Understanding how best to leverage fathers' apparent support of child vaccination within the context of families' medical decision making is worth exploring. Our survey did not address this topic. Nor can we determine how well these data from a small, but diverse sample of fathers responding to a web survey generalize to other fathers of children receiving Medicaid.
Segmentation analysis is most useful when it identifies sub-groups that: (1) are large enough to justify focused attention in a campaign or outreach effort; (2) are easily identifiable within a larger population, thus making it more cost-effective to reach them; and (3) have distinctive attributes that can directly inform decisions about what, where and how information gets communicated to members of the group about an outcome of interest (Slater, 1996)Kreuter and Wray, 2003). Although we had a limited set of variables available for the segmentation analysis, our findings largely met these criteria, are consistent with conclusions from other emerging research on COVID-19 vaccine hesitancy in parents, and thus may be useful in guiding action in clinical and community settings. Future audience segmentation research could build upon this analysis by including a wider range of demographic, psychosocial, behavioral and health variables that collectively yield even more refined segments (Boslaugh et al., 2005).
The study has several important limitations, starting with the generalizability of findings from a sample of parents belonging to one Medicaid health plan in one state who responded to an online survey. As expected in a survey of households with children enrolled in Medicaid, our sample was disproportionately female and younger compared to adult populations in Florida and the U.S. (U.S. Census Bureau, 2020; U.S. Census Bureau, 2021), and was also more racially and ethnically diverse. Educational attainment, however, was similar between the study sample and state and national adult populations.
Content analysis of qualitative comments from hundreds of survey respondents is generally a strength of the study, especially because we found no differences in intention to vaccinate one's child when comparing those who provided a qualitative response focused on the COVID-19 vaccine to those who provided a response that was not about COVID-19 or who provided no response at all (37% vs. 39% vs. 36% intending to vaccinate their child respectively, p = .438). However, parents who were younger, Black, or had a high school degree or less were less likely to provide a qualitative response about the COVID-19 vaccine (data not shown), so it is possible that our descriptions of sub-groups that include such parents are disproportionately influenced by other group members (e.g., Whites). The sub-group of older fathers was more likely to provide qualitative comments than any other sub-group resulting from the segmentation analysis. Overall, though, the subset of participants providing qualitative responses was likely too small to observe statistically significant differences in the comments provided by the five subgroups of parents.
Data for this study were gathered early in 2021, and vaccine confidence in the U.S. has increased since then, at least as measured in the context of adult vaccination (AP-NORC Center for Public Affair’s Research, 2021). It is certainly possible that the rates of hesitancy we observed around child vaccination in January 2021 have also declined. However, the incremental improvement in population-level vaccine confidence among adults has not eliminated the gaps in confidence or uptake between racial, educational and other sub-groups (Sparks et al., 2021), and the same may be true of vaccine confidence related to children.
In the midst of a pandemic, pediatricians and public health officials who communicate with patients or the public to boost vaccine confidence among lower-income parents often must weigh the tradeoffs of acting on information of unknown generalizability vs. acting on no information vs. not acting at all. While this study's findings should be considered preliminary, have limitations, and would ideally be replicated in other datasets or explored further in local contexts before guiding outreach efforts, they do provide an initial set of actionable insights to consider as COVID-19 vaccination of children unfolds.
Credit author statement
Matthew W. Kreuter: Conceptualization, Methodology, Investigation, Supervision, Funding acquisition, Resources, Writing – Original Draft, Writing – review & editing. Rachel Garg: Methodology, Data curation, Formal analysis, Writing – Original Draft, Writing – review & editing. Alexis Marsh: Supervision, Data curation, Writing – review and editing. Tess Thompson: Conceptualization, Methodology, Investigation, Writing – review and editing. Charlene Caburnay: Supervision, Data curation, Writing – review and editing. Enguday Teshome: Conceptualization, Methodology, Writing – review and editing. Saneel Kulkarni: Conceptualization, Methodology, Supervision, Writing – review and editing. Thidaporn Tanpattana: Conceptualization, Methodology, Investigation, Writing – review and editing. Jennifer Wolff: Data curation, Writing – review and editing. Amy McQueen: Conceptualization, Methodology, Investigation, Supervision, Funding acquisition, Resources, Writing – review and editing.
Declaration of Competing Interest
Saneel Kulkarni declares employment at Centene Corporation no other potential competing financial interests or personal relationships. Thidaporn Tanpattana declares employment at Sunshine Health and no other potential competing financial interests or personal relationships. All other authors have no conflicts of interest to disclose. No funder was involved in the study design, collection, analysis, or interpretation of data, writing the report, or the decision to submit the report for publication.
Acknowledgments
This study was funded by the Centene Center for Health Transformation, a research collaboration between Washington University in St. Louis, Duke University, and Centene Corporation, as well as NIH/RADxUP (CA235773-02S1), NIH/CEAL (1OT2HL161614-01), and CDC/CBS-CVD (6U48 DP006395-02M001). The authors thank Andrea Chambers, Caitlin Smith, Jean Springsteen, Kaitlyn Stansbury, Sarah Thomas, and Jordyn Wartts for content analysis coding and training; Lourdes Balaez and Madeline Rogers for survey development and implementation assistance; and Brendan Kinnison for analysis of health plan data.
References
- AP-NORC Center for Public Affair’s Research Confidence in COVID-19 Vaccines Rises. 2021 May. apnorc.org/projects/confidence-in-covid-19-vaccines-rises/ cited 2021 Mar 17. Available from:
- AP-NORC Center for Public Affairs Research Many Remain Doubtful about Getting COVID-19 Vaccine. 2020 Dec. https://apnorc.org/projects/many-remain-doubtful-about-getting-covid-19-vaccine/ cited 2021 Mar 17. Available from:
- AP-NORC Center for Public Affairs Research Safety Concerns Remain Main Driver of Vaccine Hesitancy. 2021 Feb. https://apnorc.org/projects/safety-concerns-remain-main-driver-of-vaccine-hesitancy cited 2021 Mar 17. Available from:
- Bateman N., Ross M. Why has COVID-19 Been Especially Harmful for Working Women? The Brookings Institution. 2021 Jul 13. https://www.brookings.edu/essay/why-has-covid-19-been-especially-harmful-for-working-women/ Available from:
- Bever L. Washington Post; June 24, 2021. Should My Child Get a Coronavirus Vaccine? Is it Safe? Here what you Should Know. updated November 2, 2021. [Google Scholar]
- Biggs P., de Ville B., Suen K. A method of choosing multiway partitions for classification and decision trees. J. Appl. Stat. 1991;18:49–62. [Google Scholar]
- Boslaugh S.E., Kreuter M.W., Nicholson R.A., Naleid K. Comparing demographic, health status and psychosocial strategies of audience segmentation to promote physical activity. Health Educ. Res. 2005;20(4):430–438. doi: 10.1093/her/cyg138. [DOI] [PubMed] [Google Scholar]
- Cacioppo J.T., Harkins S.G., Petty R.E. In: Cognitive Responses in Persuasion. Petty R.E., Ostrom T.M., Brock T.C., editors. Erlbaum; Hillsdale, NJ: 1981. The nature of attitudes and cognitive responses and their relation to behavior; pp. 31–54. [Google Scholar]
- Hothorn T., Hornik K., Zeileis A. Unbiased recursive partitioning: a conditional inference framework. J. Comput. Graph. Stat. 2006;15(3):651–674. doi: 10.1198/106186006X133933. [DOI] [Google Scholar]
- Kaiser Family Foundation 2017 Kaiser Women's Health Survey and 2017 Kaiser Men's Health Survey. 2018 Mar 13. https://www.kff.org/womens-health-policy/issue-brief/women-work-and-family-health-key-findings-from-the-2017-kaiser-womens-health-survey/ cited 2021 Nov 9. Available from:
- Kaiser Family Foundation KFF COVID-19 Vaccine Monitor. 2021. https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/ January 11–18; February 15–23; March 15–22. [cited 2021 Nov 15]. Available from:
- Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J. Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfeld J., Byrne M.M., Vanderpool R., Shin S., Kobetz E. HPV knowledge and vaccine acceptability among Hispanic fathers. J. Prim. Prev. 2013;34(1–2):59–69. doi: 10.1007/s10935-013-0297-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter M.W., Wray R.J. Tailored and targeted health communication: strategies for enhancing information relevance. Am. J. Health Behav. 2003;27(1):S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- Lemon S.C., Roy J., Clark M.A., Friedmann P.D., Rakowski W. Classification and regression tree analysis in public health: methodological review and comparison with logistic regression. Ann. Behav. Med. 2003;26(3):172–181. doi: 10.1207/S15324796ABM2603_02. [DOI] [PubMed] [Google Scholar]
- Matoff-Stepp S., Applebaum B., Pooler J., Kavanagh E. Women as health care decision makers: implications for health care coverage in the United States. J. Health Care Poor Underserved. 2014;25(4):1507–1513. doi: 10.1353/hpu.2014.0154. [DOI] [PubMed] [Google Scholar]
- Reuben R., Aitken D., Freedman J.L., Einstein G. Mistrust of the medical profession and higher disgust sensitivity predict parental vaccine hesitancy. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0237755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero K.M., Wong J., Sweeney C.F., Avola A., Auger A., Macaluso M., Reidy P. Parents’ intentions to vaccinate their children against COVID-19. J. Pediatr. Health Care. 2021 doi: 10.1016/j.pedhc.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santibanez T.A., Nguyen K.H., Greby S.M., Fisher A., Scanlon P., Bhatt A., Srivastav A., Singleton J.A. Parental vaccine hesitancy and childhood influenza vaccination. Pediatrics. 2020;146(6) doi: 10.1542/peds.2020-007609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater M.D. Theory and method in health audience segmentation. J. Health Commun. 1996;1(3):267–284. doi: 10.1080/108107396128059. [DOI] [PubMed] [Google Scholar]
- Sparks G., Kirzinger A., Brodie M. KFF COVID-19 Vaccine Monitor: Profile of the Unvaccinated. 2021 Jun 11. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-profile-of-the-unvaccinated/ cited 2021 Jul 5. Available from:
- Teasdale C.A., Borrell L.N., Kimball S., Rinke M.L., Rane M., Fleary S.A., Nash D. Plans to vaccinate children for COVID-19: a survey of U.S. parents. medRxiv. 2021 doi: 10.1101/2021.05.12.21256874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau 2019 American Community Survey 1-Year Estimates. 2020. https://data.census.gov/cedsci/ [cited 2021 Nov 9] Available from:
- U.S. Census Bureau 2020 DEC Redistricting Data. 2021. https://data.census.gov/cedsci/ [cited 2021 Nov 9] Available from:
- U.S. Centers for Disease Control and Prevention CDC Recommends Pediatric COVID-19 Vaccine for Children 5 to 11 Years. 2021 Nov 2. https://www.cdc.gov/media/releases/2021/s1102-PediatricCOVID-19Vaccine.html cited 2021 Nov 15 Available at:
- U.S. Food and Drug Administration FDA Authorizes Pfizer-BioNTech COVID-19 Vaccine for Emergency Use in Children 5 through 11 Years of Age. 2021 Oct 29. https://www.fda.gov/news-events/press-announcements/fda-authorizes-pfizer-biontech-covid-19-vaccine-emergency-use-children-5-through-11-years-age cited 2021 Nov 15. Available at.