Abstract
Objective
To assess the effects of adding a workplace intervention to inpatient occupational rehabilitation on return-to-work self-efficacy, and whether changes in return-to-work self-efficacy were associated with future work outcomes.
Design
Randomized clinical trial.
Subjects
Individuals aged 18–60 years, sick-listed 2–12 months were randomized to multimodal inpatient rehabilitation with (n = 88) or without (n = 87) a workplace intervention.
Methods
Between-group differences for 4 months follow-up were assessed using linear mixed models. Associations between self-efficacy scores and future sickness absence days during 12 months of follow-up were assessed by linear regression.
Results
There were no statistically significant between-group differences in self-efficacy during follow-up. Participants with high or medium self-efficacy scores at the end of rehabilitation had fewer sickness absence days during follow-up compared with participants with low scores. Participants with consistently high scores or an increasing score throughout the programme showed fewer sickness absence days than those with reduced or consistently low scores.
Conclusion
Receiving an added workplace intervention did not increase return-to-work self-efficacy more than standard inpatient occupational rehabilitation alone. High scores and a positive development in return-to-work self-efficacy were associated with higher work participation. This suggests that return-to-work self-efficacy could be an important factor to consider in the return-to-work process.
LAY ABSTRACT
Return-to-work self-efficacy is related to a person’s beliefs about coping with challenges related to return-towork after sick leave. Several studies have suggested that having high return-to-work self-efficacy is associated with shorter time to return-to-work. This study assessed the effect of adding a workplace intervention to standard inpatient occupational rehabilitation on return-to-work self-efficacy, and whether changes in return-to-work self-efficacy were associated with future work outcomes. The results showed no difference in return-to-work self-efficacy between the participants receiving the added workplace intervention compared with the participants receiving only the standard inpatient occupational rehabilitation. However, participants with a high- or an increasing score in return-to-work self-efficacy had less sickness absence in the follow-up period. This suggests that return-to-work self-efficacy is important in the process of return-to-work after sickness absence.
Key words: sickness absence, randomized controlled trial, workplace intervention, sick leave, musculoskeletal disease, mental disorders
Musculoskeletal complaints and mental health disorders are the 2 leading diagnoses for long-term sick leave (1). However, the reasons for not returning to work are a result of several factors beyond the patient’s diagnosis (2, 3). Hence, the return-to-work (RTW) process for individuals on long-term sick leave is often complex. It has been suggested that a person’s perceptions and beliefs about their problems, together with expectations about RTW can incorporate this complexity and thus are important predictors for RTW (4–10).
Expectations and the concept of self-efficacy are closely related. Self-efficacy is described as the “belief in one’s abilities to organize and execute the courses of action required to produce given attainments” (11). Positive expectations about a situation can encourage action, while negative expectations may act as an obstacle. Self-efficacy also influences the goals individuals set for themselves, and with higher self-efficacy, they believe they can achieve more. Increased selfefficacy is associated with better outcomes if the selfefficacy beliefs are related to the same domain as the outcome (11). RTW self-efficacy (RTWSE) is related to a person’s beliefs about coping with challenges related to RTW. Several studies have suggested that having a high general self-efficacy (12, 13) or a more specific RTWSE (14), is associated with shorter time to RTW, and that RTWSE may be an important predictor of RTW (15, 16). In addition, a recent systematic review found a consistent and positive association between higher RTWSE scores and RTW status and work absence outcomes in individuals with musculoskeletal or mental health complaints (17). It has been proposed that future studies should explore ways to increase self-efficacy (17) and assess the relationship between RTWSE and RTW in different groups of patients and with long-term follow-up (18).
The RTWSE questionnaire (RTWSE-19) (18) measures self-efficacy specific to resumption of workplace activities. The questionnaire encompasses 3 domains of self-efficacy regarding challenges for RTW after sick leave: meeting job demands; modifying job tasks; and communicating needs to others. We recently reported no effect on sickness absence of adding a workplace intervention to traditional Inpatient Multimodal Occupational Rehabilitation (I-MORE) (19, 20). However, the choice of remaining on sickness absence or returning to work depends on several factors.
The present study reports secondary outcomes on whether I-MORE + workplace intervention (I-MORE+WI) increased RTWSE more than I-MORE alone. As the workplace intervention included a meeting with the employer to discuss barriers to RTW and possible job modifications, it was hypothesized that participants receiving the I-MORE+WI would increase their RTWSE more than those receiving only the I-MORE. Furthermore, this study assessed the association between: (i) RTWSE scores at the end of I-MORE, and (ii) changes in RTWSE during rehabilitation with number of sick leave days during 12 months’ of follow-up.
METHODS
This study is based on data from a randomized clinical trial with 2 parallel groups (19). The trial compared I-MORE and I-MORE+WI for individuals on sick leave due to musculoskeletal complaints, unspecific or common metal health disorders. Primary outcome was sickness absence days (20). The study protocol and the primary outcome are published in previous papers, and the methods sections is partly overlapping (19, 20). The study was approved by the Regional Committee for Medical and Health Research Ethics in Central Norway (number 2014/2279), and the trial is registered at clinicaltrials. gov (NCT02541890). The results are presented according to the Consolidated Standards of Reporting Trials (CONSORT) statement (21).
Participants
Participants were living in Trøndelag County, Norway. Inclusion criteria were: age 18–60 years, sick-listed 2–12 months, employed in at least a 20% position (e.g. minimum one day per week), had an employer, sick leave status of at least 50% off work, anticipated at least 4 more weeks of sick leave, and a diagnosis within the musculoskeletal, psychological or general and unspecified chapters of the International Classification of Primary Care, second edition (ICPC-2) (22). Participants were recruited in 2 ways: (i) identified in registers from the Norwegian Labor and Welfare Administration (NAV) and invited through a letter, or (ii) referred by their general practitioner. A physician, psychologist, and a physiotherapist assessed eligibility at the outpatient clinic. Exclusion criteria were any of the following: being self-employed, having or being under consideration of a serious somatic or mental health/substance abuse disorder, currently undergoing rehabilitation, having significant problems with working in a group, insufficient comprehension of Norwegian language to participate in group sessions and to complete questionnaires, scheduled for surgery within the next 6 months, or being pregnant.
Rehabilitation programmes
The rehabilitation programmes lasted 4 weeks; 2 weeks at the rehabilitation centre, one week at home and one week at the centre. Important parts of the I-MORE programme were acceptance and commitment therapy (ACT) (23), physical exercise training, work-related problem solving and creating a RTW plan. The programme was provided from an interdisciplinary team consisting of a psychologist, physiotherapist, exercise physiologist, nurse, physician and welfare caseworker. Each participant was appointed a primary rehabilitation therapist who designed the RTW plan together with the participant.
The workplace intervention consisted of (i) preparations before the workplace meeting, (ii) the workplace meeting, and (iii) summary meetings and writing of a report after the workplace meeting. Preparations included both individual preparations and a group meeting with other participants. The main aim of the individual preparations was to discuss important challenges and resources for RTW to choose the most important topics to address in the meeting. The group meeting was an open discussion about work and RTW to share experiences. The workplace meeting took place at the workplace during the week at home, and also included a tour at the workplace. The workplace meeting was scheduled for 2 h and included the participant, the employer and the primary rehabilitation therapist from the rehabilitation centre, and aimed to address obstacles, possibilities and progress for RTW. The rehabilitation therapist led the meeting and ensured that all participants in the meeting were given time to share their thoughts about the RTW process. The meeting should result in a realistic plan for RTW that all parties agreed upon. A report from the meeting was sent to all those who participated in the meeting and also included in the RTW plan. A more detailed description of the programmes was published previously (19).
Outcomes
Questionnaires
Participants completed the RTWSE questionnaire (RTWSE-19) (18, 24) at arrival and departure from the rehabilitation centre and at 4 months follow-up. The RTWSE-19 questionnaire is a self-report measure of beliefs and expectations to execute job responsibilities. Participants are asked to report their level of confidence on a scale from 1 (not at all confident) to 10 (totally confident) to overcome several RTW barriers. The total score is obtained by summing all items and dividing them by 19, where a higher score indicates higher self-efficacy. In addition to the total score, the questionnaire has 3 subscales: “meeting job demands” (7 questions about expectations of the demands at work); “modifying tasks” (7 questions about the experience of contributing to customizing the workday); and “communicating needs” (5 questions about the expectations of being able to communicate with employer and colleagues). The subscales are scored similarly to the total score, i.e. scores on a 1–10 scale are summed and divided by the number of items in the subscale, and a higher score indicates a higher self-efficacy (18). To make the questionnaire usable for participants with complaints other than pain, the word “injury” was removed from item 7 (the Norwegian version of this item include the words “injury/worsening”) and the word “complaints” replaced “pain” in item 12. Information on factors such as sex, age, education, pain level (measured by numerical rating scale), and anxiety and depression (measured using the Hospital Anxiety and Depression scale (HADS) (25)) was obtained at inclusion.
Sick leave data were obtained from the National Social Security System Registry, where all legal residents are included. The data consisted of all individual registrations of periods with any medical benefits. Number of sickness absence days was calculated for 12 months of follow-up after the rehabilitation programme and was adjusted for graded sick leave, employment fraction and calculated as a 5-day working week.
Randomization
Eligible individuals who passed the outpatient screening were randomized to either I-MORE or I-MORE+WI. The block randomization with unknown sizes were delivered through a web-based programme, by the Unit for Applied Clinical Research at the Norwegian University of Science and Technology.
Statistical analysis
Linear mixed-effects models were used to estimate differences in change in RTWSE over time between I-MORE and I-MORE+WI, both for the total RTWSE-19 score and the 3 subscales. A random intercept for person was included in the model, to allow the participants to start at individual levels. In addition to programme and time, an interaction term between programme and the 3 time-points was included in the analyses to assess whether the effects of the programmes differed over time. The estimates from the analyses (fixed effects) were used to predict RTWSE at different time-points for the 2 groups. The analyses were performed unadjusted and adjusted for age (continuous variable), sex (man, woman) and education (variable dichotomized as high (college/university) or low).
Linear regression was used to assess the association between RTWSE-19 scores at the end of the programme and mean number of sickness absence days during 12 months of follow-up. RTWSE scores were categorized as low (< 5), medium (5–7.5) or high (> 7.5), using cut-offs from previous studies (18, 26). To assess the association between changes in RTWSE during rehabilitation and future work participation, the RTWSE score was dichotomized at the start and the end of the programme as low or medium/high self-efficacy using 5 as a cut-off. The cut-off value of 5 was chosen based on results from previous studies (18), and as it was close to the median. To increase statistical power, medium and high score values were collapsed. Based on the 2 categories at the start and the end of the programme, we classified participants into 4 groups: (i) consistently low self-efficacy, (ii) reduced self-efficacy, (iii) increased self-efficacy, or (iv) consistently high self-efficacy.
In a third analysis, the change in RTWSE was categorized as “increased” (a positive change ≥ 0.5), “no change” (positive or negative change < 0.5) or a “reduced” RTWSE score (a negative change ≥ 0.5).
For the analysis assessing the association between RTW selfefficacy RTWSE and number of sick leave days, participants from both intervention programmes were included as a single cohort. All these analyses were performed for the total RTWSE score and for the 3 subscales. In addition to unadjusted analyses, the associations were adjusted for age (continuous variable), sex (man, woman), education (variable dichotomized as high (college/university) or low) and intervention group (I-MORE or I-MORE+WI).
All analyses were done using STATA 14 (StataCorp, 2015, Stata Statistical Software: Release 14, College Station, TX: StataCorp LP).
RESULTS
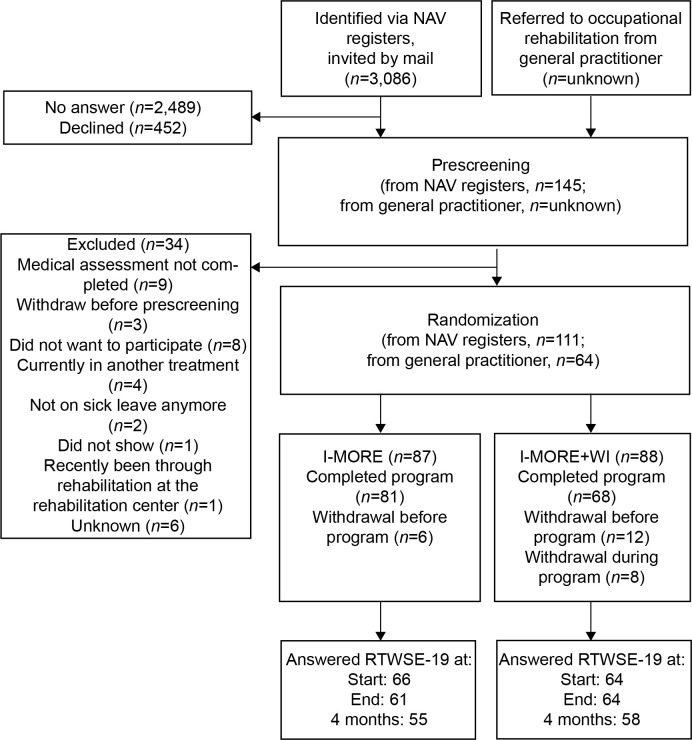
The flow of participants in the study is presented in Fig. 1. After the screening, 175 participants were randomized to either I-MORE (n = 87) or I-MORE+WI (n = 88). The number of participants answering the questionnaires decreased throughout the study (Fig. 1). However, 90% of participants contributed with some data in the analyses, i.e. answered the questionnaire at least once (I-MORE; n = 80, I-MORE+WI; n = 78).
Fig. 1.
Participation flow through the study. NAV: social security register from the Norwegian Labor and Welfare Administration; I-MORE: Inpatient Multimodal Occupational Rehabilitation; I-MORE+WI: I-MORE with Workplace Intervention. Data on the number of participants referred from general practitioners were not available.
Participants’ characteristics
There was a higher proportion of women than men (79% women), mean age was 46 years (SD 9 years) and approximately half (55%) had higher education. Prior to sick leave, 71% worked full time, 28% part time and one participant had a graded disability pension. During the 12 months before inclusion, the median length of sick leave was 184 days (interquartile range (IQR) 139–255 days). Participants’ sick leave diagnoses were mainly within the musculoskeletal (44%) and psychological (43%) chapters of ICPC-2, while 13% were diagnosed with a general and unspecified diagnosis (chapter A). The baseline characteristics for the participants in the 2 programmes were similar (Table I).
Table I.
Participants’ baseline characteristics
| Variables | I-MORE+WI (n = 88) | I-MORE (n = 87) |
|---|---|---|
| Age mean (SD) | 45 (9) | 46 (8) |
| Female n (%) | 68 (77) | 70 (80) |
| Education n (%)a | 43 (52) | 49 (58) |
| Diagnosis | ||
| A-general and unspecified, n (%) | 13 (15) | 9 (11) |
| L-musculoskeletal, n (%) | 36 (43) | 39 (46) |
| P-psychological, n (%) | 35 (42) | 37 (44) |
| HADS | ||
| Anxiety (0–21), mean (SD) | 8.4 (4.5) | 7.6 (4.4) |
| Depression (0–21), mean (SD) | 6.6 (4.2) | 6.8 (4.2) |
| Length of sick leave, median (IQR)b | 184 (137 to 242) |
184 (144 to 268) |
| Pain level (0–10), mean (SD) | 6.9 (5.2) | 6.9 (4.2) |
| Work status before sick leave | ||
| Full job, n (%) | 61 (70) | 63 (73) |
| Part-time, n (%) | 26 (30) | 22 (26) |
| Partly on disability, n (%) | 0 (0) | 1 (1) |
| RTWSEc | ||
| Total score, mean (SD) | 4.8 (2.3) | 4.9 (2) |
| Meeting job demands, mean (SD) | 4.3 (2.6) | 4.7 (2.6) |
| Modify job task, mean (SD) | 4.6 (2.5) | 4.4 (2.2) |
| Comunicating needs to others, mean (SD) | 6.0 (2.7) | 6.1 (2.3) |
Higher education: college or university.
Number of days on sick leave during the last 12 months prior to inclusion. Measured as calendar days, not adjusted for partial sick-leave. Based on data from the National Social Security System Registry.
Measured at start of rehabilitation (I-MORE+WI; n = 83, I-MORE; n = 84). RTWSE: return to work self-efficacy; HADS: Hospital Anxiety and Depression scale; SD: standard deviation; IQR: interquartile range.
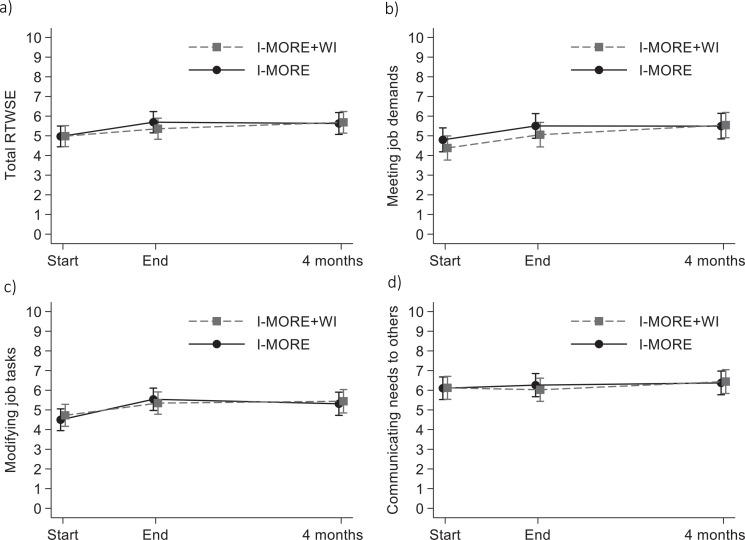
Comparison of RTWSE over time between I-MORE and I-MORE+WI
There was no difference in total RTWSE scores over time between I-MORE and I-MORE+WI (0.04, 95% confidence interval (95% CI) –0.69 to 0.78) (Fig. 2). The I-MORE group increased their total RTWSE score with 0.66 (95% CI 0.13–1.18), while the I-MORE+WI group had an increase in total RTWSE of 0.70 (95% 0.19–1.22). Two of the subscales did not show any differences between groups over time (“modifying job tasks” –0.1, 95% CI –0.93 to 0.73; “Communicating needs to others” 0.05, 95% CI –0.68 to 0.78). The subscale “meeting job demands” showed a difference of 0.47 between groups (95% CI –0.38 to 1.31), but the difference was not statistically significant.
Fig. 2.
Return-to-work self-efficacy (RTWSE) scores (1–10) for Inpatient Multimodal Occupational Rehabilitation (I-MORE) (n = 80) and I-MORE with added Workplace Intervention (I-MORE+WI) (n = 78). Data are estimated means with 95% confidence intervals (95% CI) for: (a) total RTWSE score, (b) scores of subscale “meeting job demands”,(c) scores of subscale “modifying job tasks”, (d) scores of subscale “communicating needs to others”.
Associations between RTWSE scores and number of sick leave days
There was a positive association between RTWSE scores at the end of rehabilitation and number of sickness absence days during 12 months of follow-up (Table II). Compared with participants having a low RTWSE score (< 5) at the end of the programme, those with a medium score (≥ 5 and ≤ 7.5) had 42 fewer days of sick leave (95% CI –76 to –8), while participants with a high RTWSE score (> 7.5) had 85 fewer days (95% CI –133 to –37). The same positive association between high RTWSE scores and number of sickness absence days was seen for 2 of the subscales, but with less strength than the total score. The subscale “meeting job demands” differed from the other subscales, as participants with a medium score had the fewest number of sickness absence days (Table II).
Table II.
Associations between scores on the return-to-work self-efficacy (RTWSE) questionnaire at the end of the rehabilitation and number of sick leave days during 12 months of follow-up
| Number of sick leave daysa |
||||||
|---|---|---|---|---|---|---|
| n | Crude mean | Crude mean differenceb | Adjusted mean differenceb,c | 95% CI for adjusted mean difference | ||
| Total RTWSE score | Low < 5 | 51 | 158 | 0 (ref.) | 0 (ref.) | 0 (ref.) |
| Medium 5–7.5 | 48 | 109 | –49 | –42 | –76 to –8 | |
| High > 7.5 | 26 | 68 | –90 | –85 | –133 to –37 | |
| Meeting job demands | Low < 5 | 64 | 151 | 0 (ref.) | 0 (ref.) | 0 (ref.) |
| Medium 5–7.5 | 40 | 96 | –55 | –36 | –70 to –1 | |
| High > 7.5 | 29 | 94 | –57 | –28 | –72 to 17 | |
| Modifying job tasks | Low < 5 | 54 | 153 | 0 (ref.) | 0 (ref.) | 0 (ref.) |
| Medium 5–7.5 | 49 | 112 | –41 | –31 | –65 to 2 | |
| High > 7.5 | 29 | 73 | –80 | –70 | –112 to –28 | |
| Communicating needs to others | Low < 5 | 39 | 151 | 0 (ref.) | 0 (ref.) | 0 (ref.) |
| Medium 5–7.5 | 45 | 132 | –19 | –22 | –59 to 16 | |
| High > 7.5 | 47 | 78 | –73 | –86 | –131 to –42 | |
RTWSE measured by RTWSE-19. It was scored as a total score and as 3 subscales (meeting job demands, modifying job tasks and communicating needs to others).
Estimated from linear regression analyses.
Mean difference: difference in number of sick leave days relative to the reference group.
Adjusted for age, sex, education, rehabilitation programme and baseline score on the RTWSE questionnaire; CI: Confidence Interval.
There was also a positive association between the change in RTWSE and number of sickness absence days during 12 months of follow-up (Table III). Participants who had an increase in their score during the rehabilitation programme had 35 fewer sick leave days (95 % CI –77 to 8) compared with the “consistently low” group, while participants with consistently high score had 84 fewer sick leave days (95% CI –118 to –50). The association between the subscales of RTWSE and number of sick leave days showed the same strength and direction as the total RTWSE, except for “meeting job demands”, where the participants with a reduced score had a similar number of sickness absence days as participants with an increase in RTWSE scores (Table III).
Table III.
Associations between changes in return-to-work self-efficacy (RTWSE) using cut-off values and number of sick leave days for 12 months of follow-up.
| Number of sick leave daysa |
||||||
|---|---|---|---|---|---|---|
| n | Crude mean | Crude mean differenceb | Adjusted mean differenceb,c | 95% CI for adjusted mean difference | ||
| Total RTWSE score | Consistently low | 37 | 169 | 0 (ref.) | 0 (ref.) | 0 (ref.) |
| Reduced | 9 | 158 | –11 | –7 | –63 to 48 | |
| Increased | 19 | 133 | –37 | –35 | –77 to 8 | |
| Consistently high | 43 | 82 | –88 | –84 | –118 to –50 | |
| Meeting job demands | Consistently low | 49 | 164 | 0 (ref.) | 0 ref. | 0 (ref.) |
| Reduced | 11 | 126 | –38 | –39 | –88 to 10 | |
| Increased | 23 | 131 | –32 | –31 | –72 to 10 | |
| Consistently high | 39 | 79 | –85 | –81 | –113 to –49 | |
| Modifying job tasks | Consistently low | 39 | 160 | 0 (ref.) | 0 (ref.) | 0 (ref.) |
| Reduced | 13 | 146 | –14 | –16 | –67 to 34 | |
| Increased | 31 | 122 | –38 | –36 | –75 to 3 | |
| Consistently high | 35 | 81 | –79 | –77 | –112 to –41 | |
| Communicating needs to others | Consistently low | 25 | 159 | 0 (ref.) | 0 (ref.) | 0 (ref.) |
| Reduced | 11 | 168 | 9 | 7 | –50 to 63 | |
| Increased | 16 | 131 | –28 | –15 | –67 to 38 | |
| Consistently high | 66 | 105 | –54 | –50 | –88 to –12 | |
RTWSE measured by the RTWSE-19. It was scored as a total score and as 3 subscales (meeting job demands, modifying job tasks and communicating needs to others). A cut-off of 5 was used to categorize scores at the start and end of rehabilitation as high or low. Based on this information a new varible was created categorizing self-efficacy as: (i) consistently low, (ii) reduced from high to low, (iii) increasing from low to high, or (iv) consistently high.
Estimated from linear regression analyses.
Mean difference: difference in number of sick leave days relative to the reference group.
Adjusted for age, sex, education, rehabilitation programme and baseline score on the RTWSE questionnaire; CI: Confidence Interval.
When assessing change (positive or negative change ≥ 0.5) in total RTWSE score, we found that participants who had an increased score had 12 fewer sickness absence days (95% CI –47 to 24) compared with those with no change in their score, while participants with a reduction in total RTWSE had 43 more sickness absence days (95% CI 1–85). The results for the 3 subscales were similar (see Table SI1).
Participants with missing questionnaires
The number of participants not completing the questionnaires in the 2 groups were similar at the end of the programme (I-MORE 30%, I-MORE+WI 27%), and at 4 months (I-MORE 37%, I-MORE+WI 34%). Participants with missing RTWSE questionnaires at the end of the programme had fairly similar age as responders (mean age 46 years (SD 9.2), vs 45 years (SD 7.8)), but were slightly more likely to be women (86% vs 78%), less likely to have higher education (47% vs 58%), and less likely to be working full time prior to sick leave (60% vs 75%). Baseline total RTWSE scores were similar for those responding and not responding at the end of programme (4.9 (SD 2.1) vs 4.9 (SD 2.2)).
Participants who did not respond to the questionnaire at the end of the programme had fewer sickness absence days during 12 months of follow-up compared with participants who answered at both time-points (mean 41 days (SD 75) vs 120 days (SD 82); median 0 days (IQR 0–58) vs 114 days (IQR 50–197)).
DISCUSSION
There was no difference in the change in RTWSE scores between I-MORE and I-MORE+WI during 4 months of follow-up. Having a moderate or high RTWSE score at the end of rehabilitation was associated with fewer sickness absence days during 12 months of follow-up compared with having a low score. Furthermore, increasing score or scoring consistently high during rehabilitation were associated with fewer sickness absence days during follow-up than decreasing score or scoring consistently low.
The lack of effect of the workplace intervention on RTWSE, compared with I-MORE alone, was contrary to our hypothesis. To our knowledge, only one previous study has used the RTWSE-19 to assess change in RTWSE (26), and no previous studies have investigated whether a workplace intervention increases RTWSE using this questionnaire. Previous studies evaluating changes in RTWSE have used a Dutch questionnaire developed for individuals with mental health problems (15, 16, 27). A possible explanation for the lack of difference in RTWSE between the programmes could be that the workplace intervention was too modest and insufficient to increase the participants’ beliefs in their own capabilities at the workplace. A more comprehensive workplace intervention, or more follow-up after the intervention could have been beneficial. However, it should also be noted that the workplace intervention was added to a comprehensive rehabilitation programme. Furthermore, the workplace intervention in this study had no effect on RTW compared with the traditional programme (20). However, both programmes showed only negligible changes in RTWSE, both for the total score and the 3 subscales. This is in line with a Danish validation study (26), which also reported no change in either of the scales between 2 measurement points (median 10 weeks). This could indicate a problem with the responsiveness of the questionnaire and should be evaluated in future studies. However, it is also possible that self-efficacy is a more enduring trait.
The results from the analysis assessing the association between RTWSE scores and future number of sickness absence days are in line with previous studies showing that higher RTWSE-19 scores are associated with better RTW outcomes (18, 26). The results of the current study support the previous knowledge in a broad target population on long-term sick leave. In addition to previous knowledge, this study assesses the association between both high scores and changes in RTWSE and future work participation. The results of the present study indicate that RTWSE is important in the RTW process and that future studies should investigate how RTW interventions can increase RTWSE. Furthermore, the RTWSE-19 questionnaire might be useful in assessing which patients will RTW on their own and who might need more support.
The subscale “meeting job demands” showed a slightly different association with future sickness absences than the other 2 subscales (Tables II and III). For instance, participants with a reduced score in the subscale from start to end of the programme had a similar number of sickness absence days as participants with an increase in the subscale-score. In addition, participants with a medium score at the end of rehabilitation had a smaller number of sickness absence days than the participants with a higher score in the subscale. The items included in this subscale seem to be closely related to how well you can do your work (e.g. “keep up with the pace at work” and “meet your production requirements”), compared with the 2 other subscales, which are more related to communication and possible job modifications. The participants in this study had been sick-listed for a long time. Hence, it is possible that answering these specific questions about performing their job was difficult. Studies exploring sick-listed persons’ experiences with answering this part of the RWTSE-19 questionnaire could provide important knowledge on the use of this outcome measure.
Study strengths and limitations
A strength of the first part of this study is the randomized design and the use of registry data in the analysis. This study has some limitations that should be acknowledged. Of the 3,086 invitation letters, 145 people accepted, which limits the generalizability of the results. In addition, participants had to be willing to participate in a workplace meeting with their employer. Participants with a problematic relationship with their workplace or supervisor may have declined to participate in the study. This could explain why more participants withdrew from I-MORE+WI than I-MORE (20 vs 6). Another limitation is the response rate for the questionnaires, which decreased to approximately 65% at 4 months of follow-up. Although linear mixed models analyses were performed, which uses all available data, it nonetheless relies on the assumption of data missing at random. It cannot fully rule out possible bias due to loss to follow-up. Participants who did not complete the questionnaire at the end of the programme (not included in the association analyses) had considerably fewer days of sickness absence than those included in the analyses, suggesting that the included participants struggled more with their RTW process. This could have underestimated the association between the change in RTWSE and future work participation. Another limitation is the categorization of the RTWSE scores, which led to a loss of statistical power. However, the cut-off values for low/medium/high scores were suggested in previous studies (18), and were chosen for comparability and clinical usefulness. It should also be noted that the participants in the current study were sick-listed due to different diagnoses (musculoskeletal, psychological and general and unspecified disorders) and the RTWSE-19 questionnaire could have different properties or validity for the different diagnoses groups. However, considering the sample size and multiple testing, stratified analyses were not performed, due to the high risk of spurious findings.
CONCLUSION
In conclusion, adding a limited workplace intervention to an inpatient multimodal occupational rehabilitation programme did not increase RTWSE more than the standard rehabilitation programme alone. However, both high RTWSE scores at the end of rehabilitation and increased RTWSE during rehabilitation were positively associated with the future number of sickness absence days. The results suggest that RTWSE is important in the RTW process. Future studies should assess how interventions can increase RTWSE in sicklisted individuals.
AKNOWLEDGEMENTS
The authors thank everybody at Hysnes rehabilitation centre and the Norwegian Labor and Welfare Service (NAV) for help with collecting data and carrying out the study. We also thank project assistant Guri Helmersen for providing valuable assistance.
Footnotes
The authors have no conflicts of interest to declare.
Funding
The Norwegian government allocated funding through the Central Norway Regional Health Authority and St Olavs Hospital, Trondheim; and the Research Council of Norway.
REFERENCES
- 1.Organisation for Economic Co-operation and Development (OECD) . Reconsidering Norwegian sickness absence policies. In: Mental health and work. Paris: OECD Publishing; 2013. [Google Scholar]
- 2.Schultz IZ, Stowell AW, Feuerstein M, Gatchel RJ. Models of return to work for musculoskeletal disorders. J Occup Rehabil 2007; 17: 327–352. [DOI] [PubMed] [Google Scholar]
- 3.Andersen MF, Nielsen KM, Brinkmann S. Meta-synthesis of qualitative research on return to work among employees with common mental disorders. Scand J Work Environ Health 2012; 93–104. [DOI] [PubMed] [Google Scholar]
- 4.Løvvik C, Øverland S, Hysing M, Broadbent E, Reme SE. Association between illness perceptions and return-to-work expectations in workers with common mental health symptoms. J Occup Rehabil 2014; 24: 160–170. [DOI] [PubMed] [Google Scholar]
- 5.Aasdahl L, Pape K, Vasseljen O, Johnsen R, Fimland MS. improved expectations about length of sick leave during occupational rehabilitation is associated with increased work participation. J Occup Rehabil 2019; 29: 475–482. [DOI] [PubMed] [Google Scholar]
- 6.Nieuwenhuijsen K, Verbeek JH, de Boer AG, Blonk RW, van Dijk FJ. Predicting the duration of sickness absence for patients with common mental disorders in occupational health care. Scand J Work Environ Health 2006; 32: 67–74. [DOI] [PubMed] [Google Scholar]
- 7.Sampere M, Gimeno D, Serra C, Plana M, Lopez JC, Martinez JM, et al. Return to work expectations of workers on long-term non-work-related sick leave. J Occup Rehabil 2012; 22: 15–26. [DOI] [PubMed] [Google Scholar]
- 8.Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you’ll do? A systematic review of the evidence for a relation between patients’ recovery expectations and health outcomes. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne 2001; 165: 174–179. [PMC free article] [PubMed] [Google Scholar]
- 9.Reme SE, Hagen EM, Eriksen HR. Expectations, perceptions, and physiotherapy predict prolonged sick leave in subacute low back pain. BMC Musculoskel Dis 2009; 10: 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fleten N, Johnsen R, Førde OH. Length of sick leave – why not ask the sick-listed? Sick-listed individuals predict their length of sick leave more accurately than professionals. BMC Publ Health 2004; 4: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977; 84: 191–215. [DOI] [PubMed] [Google Scholar]
- 12.Brouwer S, Krol B, Reneman MF, Bültmann U, Franche R-L, van der Klink JJ, et al. Behavioral determinants as predictors of return to work after long-term sickness absence: an application of the theory of planned behavior. J Occup Rehabil 2009; 19: 166–174. [DOI] [PubMed] [Google Scholar]
- 13.Brouwer S, Reneman MF, Bultmann U, van der Klink JJ, Groothoff JW. A prospective study of return to work across health conditions: perceived work attitude, self-efficacy and perceived social support. J Occup Rehabil 2010; 20: 104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nieuwenhuijsen K, Noordik E, van Dijk FJ, van der Klink JJ. Return to work perceptions and actual return to work in workers with common mental disorders. J Occup Rehabil 2013; 23: 290–299. [DOI] [PubMed] [Google Scholar]
- 15.Lagerveld SE, Blonk RWB, Brenninkmeijer V, Schaufeli WB. Return to work among employees with mental health problems: development and validation of a self-efficacy questionnaire. Work Stress 2010; 24: 359–375. [Google Scholar]
- 16.Lagerveld SE, Brenninkmeijer V, Blonk RW, Twisk J, Schaufeli WB. Predictive value of work-related self-efficacy change on RTW for employees with common mental disorders. Occup Environ Med 2017; 74: 381–383. [DOI] [PubMed] [Google Scholar]
- 17.Black O, Keegel T, Sim MR, Collie A, Smith PJJoOR. The effect of self-efficacy on return-to-work outcomes for workers with psychological or upper-body musculoskeletal injuries: a review of the literature. J Occup Rehabil 2018; 28: 16–27. [DOI] [PubMed] [Google Scholar]
- 18.Shaw WS, Reme SE, Linton SJ, Huang YH, Pransky G. 3rd place, PREMUS best paper competition: development of the return-to-work self-efficacy (RTWSE-19) questionnaire--psychometric properties and predictive validity. Scand J Work Environ Health 2011; 37: 109–119. [DOI] [PubMed] [Google Scholar]
- 19.Rise MB, Skagseth M, Klevanger NE, Aasdahl L, Borchgrevink P, Jensen C, et al. Design of a study evaluating the effects, health economics, and stakeholder perspectives of a multi-component occupational rehabilitation program with an added workplace intervention - a study protocol. BMC Public Health 2018; 18: 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skagseth M, Fimland MS, Rise MB, Johnsen R, Borchgrevink PC, Aasdahl L. Effectiveness of adding a workplace intervention to an inpatient multimodal occupational rehabilitation program: a randomized clinical trial. Scand J Work Environ Health 2020; 46:3 56–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med 2010; 8: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WONCA International Classification Committee . International Classification of Primary Care ICPC-2-R. Oxford: Oxford University Press; 2005. [Google Scholar]
- 23.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther 2006; 44: 1–25. [DOI] [PubMed] [Google Scholar]
- 24.Nottingnes C, Fersum KV, Reme SE, Moe-Nilssen R, Morken T. Job-related self-efficacy in musculoskeletal disorders – a questionnaire. Tidsskrift for den Norske laegeforening 2019; 139. [DOI] [PubMed] [Google Scholar]
- 25.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 26.Momsen A-MH, Rosbjerg R, Stapelfeldt CM, Lund T, Jensen C, Johansen T, et al. Cross-cultural adaptation and validation of the Danish version of the 19-item return-to-work self-efficacy (RTWSE-19) questionnaire. Scand J Work Envir Health 2016; 42: 338–345. [DOI] [PubMed] [Google Scholar]
- 27.van Beurden KM, van der Klink JJ, Brouwers EP, Joosen MC, Mathijssen JJ, Terluin B, et al. Effect of an intervention to enhance guideline adherence of occupational physicians on return-to-work self-efficacy in workers sick-listed with common mental disorders. BMC Public Health 2015; 15: 796. [DOI] [PMC free article] [PubMed] [Google Scholar]