Abstract
Premature menopause can occur in women living with human HIV. In this study, we analyzed and reviewed published literature using the PubMed, Cochrane, and Embase databases since the year 1990 using a combination of MeSH terms such as “Early,” “Premature,” “Menopause,” “HIV,” and “Hormones.” Monitoring and implementation of targeted interventions for premature or early menopause among HIV-infected women might prevent or delay complications such as osteoporosis, cardiovascular diseases, and mental health issues.
Keywords: Endocrine, HIV/acquired immunodeficiency syndrome, menopause, osteoporosis, ovarian hormones, women
INTRODUCTION
Globally, over half of HIV-infected persons are reported to be women, and HIV is said to be associated with early onset of menopause. Menopause is linked with vasomotor symptoms such as night sweats, hot flashes, and sleep disturbance that also appears to correlate with the advancement of HIV or even the adverse effects of highly active antiretroviral medication.[1] In addition, menopause and HIV are found to be risk factors for bone mineral density loss and neurological and cardiovascular diseases.[1]
Gender difference in immune responses and cardiovascular diseases is primarily due to ovarian production of sex steroids such as estrogen, testosterone, and progesterone.[1] While it is known that with loss of ovarian steroids, there is an increase in bone demineralization, the impact of menopause in HIV disease progression and acquired immunodeficiency syndrome (AIDS) is not well known.[1,2] Some studies suggest that the onset of menopause is earlier in HIV-infected women when compared to the general population. However, these also differed about the number of women on combined antiretroviral therapy (cART), methodology, and suppressed virology.[2,3,4,5,6,7]
Although the mechanism of early menopause in HIV-infected women is not well known, the immune system which is affected by menopause leads to a lowering of CD4 cell count (<200 cells/[mu] L) and further disease progression occurs.[1,2] Plasma levels of the anti-Müllerian hormone (AMH) have been reported to be a biomarker of gonadal aging as well as an ovarian reserve in HIV-infected women. Although the relationship between levels of AMH and age of menopause has been studied in the general population, it is unknown in HIV-infected women.[2]
Menstrual and hormonal irregularities in HIV-infected women are multifactorial, and although common, the question that was raised by Kanapathipillai et al. (2013) remains as to whether it is appropriate to use the standard definitions of menopause in this particular population.[2]
This article reviewed the literature for early menopause among HIV-infected women, highlighting its age of onset, mechanisms, and its clinical consequences. It also drew the attention of the endocrinologists and HIV physicians to other possible factors of early menopause in HIV-infected women.
METHODS
Identification of relevant studies
Published literature was reviewed using the PubMed, Cochrane, and Embase databases since the year 1990 using a combination of MeSH terms such as “Early,” “Premature,” “Menopause,” “HIV,” and “Hormones.”
Selection of included studies
The search identified 21 studies (original and review articles), and these were independently reviewed using full text and abstract for inclusion. Included studies had to be on HIV-infected women, currently being treated or not, having experienced early or premature menopause or changes in hormone levels.
Menopause and early menopause: Age of onset of and frequencies among HIV-infected women
With better treatments for HIV and prolonged survival of patients, it is essential to look at the effect of HIV on women as they age. HIV has been linked with the early onset of menopause, and this can result in a significantly increased risk of cardiovascular conditions, osteoporosis, and neurological diseases.[1]
Premature menopause is when menopause occurs below the age of 40 years. Among the general population, it is found to affect 1% of women. Among HIV-infected women, determining the age at menopause is difficult due to the lack of consistency in the definition of menopause. Menopause is defined by the time of the final menstrual period, and ovarian follicular depletion is determined after 12 months of amenorrhea.[2]
On this note, advanced immune suppression (CD4 lymphocyte count <50 cells/[mu] L) and irregular bleeding are more common in HIV-infected women compared to the general population. A cohort study by Cejtin et al. found HIV-infected women to be associated with normal follicle-stimulating hormone (FSH) levels and secondary amenorrhea longer than 12 months, suggesting that HIV may not induce ovarian failure.[8] There was no association found between viral load, CD4 count or cART when adjusting for albumin, parity, and body mass index (BMI) although 47% of women in the study reported ever receiving cART.[2,8]
Several studies have looked at the age of onset of menopause in women infected with HIV. One such study showed that the age of the final menstrual period ranged from 45 to 52 years among HIV-infected women, whereas in women without HIV, it was between 49 and 55 years.[1] Another study showed that out of 667 HIV-infected women, 27% had early menopause, and the age of natural menopause ranged from 45 to 50.[9] A survey containing 102 women also found that the age of menopause in HIV-infected women ranged between 39 and 49 years (median age: 46), whereas in uninfected women, it was between 44.5 and 48 years (median age: 47).[6] This indicates that menopause seems to occur at least 4–5 years earlier in HIV-infected women compared to the general population. A case–control study performed in Burkina Faso involving 93 participants showed that the premature menopause rate among HIV-infected women was 5.5%, whereas among the general African population, it was just 1.4%.[10] It was also seen that the average age of menopause in women without HIV infection is 51 years among those of Hispanic and white ethnicity and 49 years among African-American ethnicity compared to the mean age of 47–48 years among HIV-infected women.[11]
The rate of premature menopause among HIV-infected women has also been shown to be around 8% to up to 12%.[7,12] A study looking at ovarian function among HIV-infected women found that approximately 23% of them had abnormal AMH levels, 57% had abnormal FSH levels, and 63% had abnormal antral follicular count. This suggests that being HIV positive is linked to premature ovarian insufficiency.[13]
The age at natural menopause varies according to the ethnicity of women. The age of menopause among white women ranges from 50 to 52 years, which is similar to Asian women (except Thai and Filipino Malay women who experience it 2–3 years earlier).[14] However, it has been shown that African American and Latino women reach menopause about 2 years earlier than white women. There has also been a geographical influence, wherein women in rural areas have menopause earlier than those in urban areas. Living at high altitudes also seems to contribute to menopause occurring about 1–1.5 years earlier.[11,14] Importantly, 55.9% of 1422 Canadian women living with HIV reported menstrual disturbance, and risk factors were the use of ART, genetic, smoking, province of residence, and hepatitis B coinfection.[15] Furthermore, a cross-sectional study in 229 Canadian women living with HIV showed that the median age of menopause was 48 years; 29.7% of women experienced menopause <45 years: 16.6% with early menopause and 13.1% with premature menopause. Factors that can be associated with menopause in those aged <45 years were white ethnicity, birth in Canada, low education, smoking, recreational drug use, and hepatitis C coinfection, while low education and hepatitis C coinfection were regarded as independent risk factors associated with menopause in those aged <45 years.[16] However, there was one study that found that the association between HIV infection and early menopause is weak, as protracted amenorrhea is quite common among HIV-infected women and can result in the misdiagnosis of early menopause. However, it did note that prolonged amenorrhea due to anovulatory cycles can have similar implications on health as early menopause does.[17]
From these studies, we can assume that the prevalence of early menopause is much higher (ranging from 5.5% to 27%) than the general population (only 1%). The age at menopause can also be as much as 5 years earlier than the general population[17] with an ethnic and geographical variation. Premature menopause can have short-term effects on cognition and mental health such as irritability, reduced concentration, sleep disturbances, and forgetfulness.[18] In the long term, it can cause over 7 years a 30% increased risk of reduced psychomotor speed and global cognitive function.[19]
Possible mechanisms of early menopause among HIV-infected women
Serum plasma levels of the AMH, a protein indicative of ovarian reserve, are highly predictive of the age onset of menopause.[1] In HIV-affected women, it is documented to be significantly lower, directly associated with the early onset of menopause. There are, however, other factors that can additionally cause early menopause such as smoking, or low CD4 cell count, hepatitis C virus coinfection, and history of AIDS. The mechanism of this correlation is multivariant.
During natural menopause, several hormonal changes occur. First, there is complete depletion of oocytes within the ovary, which then results in decreased levels of inhibin, which in turn increases the circulating levels of FSH.[14] These changes cause reduced ovarian production of estrogen and hence results in the features seen during menopause such as irregular bleeding, hot flushes, vaginal dryness, and mood changes.[13,14,15,16,17]
On the other hand, the most prevalent predictor of early onset of menopause is the use of tobacco. Smoking is common among HIV-infected women and is pervasive with the use of recreational drugs. Studies have shown that the practice of cocaine and heroin in 5 years before the onset of menopause is associated with early-onset menopause.[6]
For HIV-infected women, the proportion of women commencing symptoms indicative of menopause was inversely proportional to the CD4+ count, indicating an increased percentage of early-onset menopause in women with low lymphocyte counts <200 cells/mm3, defined as clinical AIDS.[1]
Clark et al. showed data suggesting that women with more advanced immunosuppression, including coinfection of seropositive hepatitis C, are less likely to ovulate.[12] Ultimately, reproductive health in HIV-affected women is associated with the extent of HIV morbidity. Recipients of antiretroviral therapy have decreased copies of HIV (ribonucleic acid) in serum plasma and are more likely to have normal CD4+ counts, resulting in normal reproductive function. Additional influences associated with earlier onset of menopause included low BMI.[20]
Interestingly, Yalamanchi et al. state that there is little evidence to suggest that HIV itself is associated with an earlier age at menopause, but instead, HIV and HIV-related comorbidities are associated with amenorrhea.[17] A prospective women's interagency HIV study published that >50% of HIV-infected women who reported >12 months of amenorrhea did not have FSH levels of >25 mIU/mL, indicating that amenorrhea was common in the absence of menopause.[8] Furthermore, the reproductive effects of HIV must be differentiated from the comorbidities and treatments that are predominant in HIV-affected women. Women with HIV are at a higher risk of early menopause due to the use of drugs associated with secondary amenorrhea including psychiatric, antiepileptic therapies, chemotherapeutic agents, immune-modulating drugs, and long-term opioids.[17]
In addition, there are several other causes for the onset of premature menopause, with the majority being idiopathic.[21] Genetic causes such as Turner's syndrome, Fragile X syndrome, and other mutations involving the X chromosome should be considered. Autoimmune diseases have also been seen to be associated with premature menopause. It can be part of the autoimmune syndrome, such as autoimmune polyglandular syndrome-1 (APS-1). The disease associations found in APS-1 are Addison's disease, hypoparathyroidism, hypogonadism, Graves’ disease or autoimmune thyroiditis, and Type 1 diabetes.
Premature menopause with HIV/AIDS can be due to other endocrine diseases such as APS, Addison's disease, hypothyroidism, hypoparathyroidism, and diabetes also increases the risk of suffering from premature ovarian failure. Cushing's syndrome can cause amenorrhea. The menstrual abnormalities correlated with increased serum cortisol and decreased serum estradiol concentrations but not with serum androgen concentrations. Because both luteinizing hormone and FSH levels are low, the menstrual irregularities appear to be due to suppression of secretion of gonadotropin-releasing hormone by hypercortisolemia. Furthermore, it can also be due to nonendocrine conditions such as rheumatoid arthritis, systemic lupus erythematosus, vitiligo, chronic hepatitis, Sjogren's syndrome, and Crohn's disease. Infections such as mumps, tuberculosis, Shigella, malaria, and cytomegalovirus have also been seen to cause premature menopause. Iatrogenic causes and environmental toxins also seem to contribute to early menopause. It is imperative to note, however, that the clinical consequences of amenorrhea and menopause are mostly similar.
The importance of understanding the impact of HIV has on reproductive function, and aging in HIV-infected women is vital. The crucial component of reproduction in women is the ovarian function; however, standard methods to assess this are limited in women with HIV.[17]
Among HIV-infected women, early menopause is frequent. High rates of premature and early menopause could suggest a virus attacking ovarian function.[17,22] AMH and FSH hormones have also been shown to be predictive factors for HIV-infected women when it comes to age at the final menstrual period.[1,23] Measuring this hormone may enable the prediction of early menopause and, as such, allow the implementation of individualized treatment plans to reduce comorbidities related to early menopause in HIV-infected women.[9]
In conclusion, there seems to be an association between early menopause and factors reported in HIV-infected women.[12] Thus, we must monitor and implement targeted interventions for premature or early menopause among HIV-infected women to effectively prevent or delay the onset of resulting conditions such as osteoporosis, cardiovascular diseases, and mental health illnesses.[22,23] Figure 1 illustrates a summary of possible mechanisms involved in premature menopause.
Figure 1.
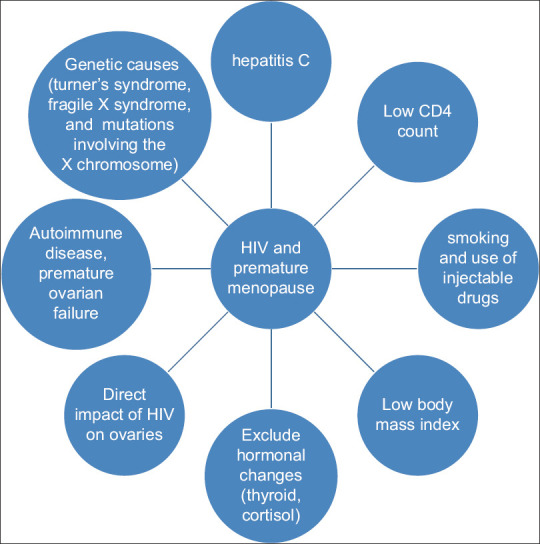
Possible mechanisms of early menopause among HIV-infected women
Consequences of early menopause on HIV-infected women
The onset of menopause in HIV-associated women has increased long-term clinical adversities, including bone demineralization, diabetes, cardiovascular disease, and the emergence of urogenital symptoms.
Premature menopause is associated with an increased risk of earlier onset of osteoporosis fractures, low bone density, coronary artery disease, and impaired endothelial function which overall will result in increased morbidity and mortality.[18] Women with premature menopause also report having increased mental health illnesses such as anxiety and depression. Premature ovarian failure is commonly associated with autoimmune mechanisms, and hence, women with autoimmune who experienced early menopause can also suffer from thyroid disease, adrenal disease, and rheumatoid conditions.[18] In Table 1, we have included a summary of all the studies in relation to premature menopause and main findings.
Table 1.
Main summary of studies of HIV and early menopause
| Main findings | Reference |
|---|---|
| Early menopause can be associated with an increased cardiovascular risk, osteoporosis, and neurological condition | [1] |
| Menstruation can stop for >12 months despite normal plasma gonadotrophin level | [8] |
| HIV can be associated with abnormal AMH levels in 23% of women, 57% have abnormal FSH, and 63% abnormal antral follicular count | [13] |
| About 5%-30% of women with HIV may experience early menopause | [7,8,9,10,11,12] |
| Early menopause can occur 5 years early in women with HIV | [1,15,17] |
| Causes of early menopause with HIV can be due to chronic infection, hepatitis, depletion of estrogen, abnormal CD4 count, smoking, metabolic changes with HIV such as diabetes, other HIV-related diseases, and medication used for HIV or other related HIV illnesses | [12,13,14,15,16,17,18,19] |
AMH=Anti-Müllerian hormone; FSH=Follicle-stimulating hormone
CONCLUSIONS
HIV can be associated with early menopause. This is likely to occur 5 years earlier than in women without HIV. Early menopause can occur even in the presence of normal and abnormal hormonal levels. Different factors can be associated with early menopause in women living with HIV such as chronic infection, low education level, hepatitis, depletion of estrogen, abnormal CD4 count, smoking, metabolic changes with HIV such as diabetes, the use of injectable drugs, other HIV related disease and medication used for HIV or other related HIV illness. The issue of early menopause is not extensively researched yet, and currently, there are no randomized clinical trials about the management. Therefore, treatment can be individualized and may be addressed by a team of specialists in HIV, endocrinology, and psychology. Early treatment of any psychological illness may be needed. Future research is needed to address (i) the mechanisms involved in premature menopause with HIV, (ii) diagnostic criteria and whether it is different from the one used for women without HIV, (iii) management of premature menopause and the use of hormonal replacement, and (iv) role of specialist clinics in minimizing the mental health impact of premature menopause in women living with HIV.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Scherzer R, Greenblatt RM, Merhi ZO, Kassaye S, Lambert-Messerlian G, Maki PM, et al. Use of antimüllerian hormone to predict the menopausal transition in HIV-infected women. Am J Obstet Gynecol. 2017;216:46.e1–11. doi: 10.1016/j.ajog.2016.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanapathipillai R, Hickey M, Giles M. Human immunodeficiency virus and menopause. Menopause. 2013;20:983–90. doi: 10.1097/GME.0b013e318282aa57. [DOI] [PubMed] [Google Scholar]
- 3.Clark RA, Cohn SE, Jarek C, Craven KS, Lyons C, Jacobson M, et al. Perimenopausal symptomatology among HIV-infected women at least 40 years of age. J Acquir Immune Defic Syndr. 2000;23:99–100. doi: 10.1097/00126334-200001010-00016. [DOI] [PubMed] [Google Scholar]
- 4.Fantry LE, Zhan M, Taylor GH, Sill AM, Flaws JA. Age of menopause and menopausal symptoms in HIV-infected women. AIDS Patient Care STDS. 2005;19:703–11. doi: 10.1089/apc.2005.19.703. [DOI] [PubMed] [Google Scholar]
- 5.Ferreira CE, Pinto-Neto AM, Conde DM, Costa-Paiva L, Morais SS, Magalhães J. Menopause symptoms in women infected with HIV: Prevalence and associated factors. Gynecol Endocrinol. 2007;23:198–205. doi: 10.1080/09513590701253743. [DOI] [PubMed] [Google Scholar]
- 6.Schoenbaum EE, Hartel D, Lo Y, Howard AA, Floris-Moore M, Arnsten JH, et al. HIV infection, drug use, and onset of natural menopause. Clin Infect Dis. 2005;41:1517–24. doi: 10.1086/497270. [DOI] [PubMed] [Google Scholar]
- 7.de Pommerol M, Hessamfar M, Lawson-Ayayi S, Neau D, Geffard S, Farbos S, et al. Menopause and HIV infection: Age at onset and associated factors, ANRS CO3 Aquitaine cohort. Int J STD AIDS. 2011;22:67–72. doi: 10.1258/ijsa.2010.010187. [DOI] [PubMed] [Google Scholar]
- 8.Cejtin HE, Kalinowski A, Bacchetti P, Taylor RN, Watts DH, Kim S, et al. Effects of human immunodeficiency virus on protracted amenorrhea and ovarian dysfunction. Obstet Gynecol. 2006;108:1423–31. doi: 10.1097/01.AOG.0000245442.29969.5c. [DOI] [PubMed] [Google Scholar]
- 9.Calvet G, Grinsztejn B, Quintana M, Derrico M, Jalil E, Cytryn A, et al. Predictors of early menopause in HIV-infected women: A prospective cohort study. Am J Obstetr Gynecol. 2015;212(765):e1–13. doi: 10.1016/j.ajog.2014.12.040. [DOI] [PubMed] [Google Scholar]
- 10.Willems N, Lemoine C, Liesnard C, Gervy C, Hien AD, Karama R, et al. Is ovarian function impaired in HIV patients? A clinical pilot study in Burkina Faso. Rev Med Bru×. 2013;34:397–404. [PubMed] [Google Scholar]
- 11.Kojic EM, Wang CC, Cu-Uvin S. HIV and menopause: A review. J Womens Health (Larchmt) 2007;16:1402–11. doi: 10.1089/jwh.2007.0345. [DOI] [PubMed] [Google Scholar]
- 12.Clark RA, Mulligan K, Stamenovic E, Chang B, Watts H, Andersen J, et al. Frequency of anovulation and early menopause among women enrolled in selected adult AIDS clinical trials group studies. J Infect Dis. 2001;184:1325–7. doi: 10.1086/323999. [DOI] [PubMed] [Google Scholar]
- 13.Ohl J, Partisani M, Demangeat C, Binder-Foucard F, Nisand I, Lang JM. Alterations of ovarian reserve tests in human immunodeficiency virus (HIV)-infected women. Gynecol Obstet Fertil. 2010;38:313–7. doi: 10.1016/j.gyobfe.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 14.Gold EB. The timing of the age at which natural menopause occurs. Obstet Gynecol Clin North Am. 2011;38:425–40. doi: 10.1016/j.ogc.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valiaveettil C, Loutfy M, Kennedy VL, Caddy S, Yudin M, Conway T, et al. High prevalence of abnormal menstruation among women living with HIV in Canada. PLoS One. 2019;14:e0226992. doi: 10.1371/journal.pone.0226992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andany N, Kaida A, de Pokomandy A, Yudin MH, Wang L, Kennedy VL, et al. Prevalence and correlates of early-onset menopause among women living with HIV in Canada. Menopause. 2020;27:66–75. doi: 10.1097/GME.0000000000001423. [DOI] [PubMed] [Google Scholar]
- 17.Yalamanchi S, Dobs A, Greenblatt RM. Gonadal function and reproductive health in women with human immunodeficiency virus infection. Endocrinol Metab Clin North Am. 2014;43:731–41. doi: 10.1016/j.ecl.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okeke T, Anyaehie U, Ezenyeaku C. Premature menopause. Ann Med Health Sci Res. 2013;3:90–5. doi: 10.4103/2141-9248.109458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ryan J, Scali J, Carrière I, Amieva H, Rouaud O, Berr C, et al. Impact of a premature menopause on cognitive function in later life. BJOG. 2014;121:1729–39. doi: 10.1111/1471-0528.12828. [DOI] [PubMed] [Google Scholar]
- 20.Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. Premature menopause or early menopause: Long-term health consequences. Maturitas. 2010;65:161–6. doi: 10.1016/j.maturitas.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ebrahimi M, Akbari Asbagh F. Pathogenesis and causes of premature ovarian failure: An update. Int J Fertil Steril. 2011;5:54–65. [PMC free article] [PubMed] [Google Scholar]
- 22.Samuel MI, Welch J, Tenant-Flowers M, Poulton M, Campbell L, Taylor C. Care of HIV-positive women aged 50 and over – Can we do better? Int J STD AIDS. 2014;25:303–5. doi: 10.1177/0956462413504553. [DOI] [PubMed] [Google Scholar]
- 23.Akl LD, Valadares AL, Moraes MJ, Pinto-Neto AM, Lagrutta B, Costa-Paiva L. Metabolic syndrome in HIV-infected middle-aged women on antiretroviral therapy: Prevalence and associated factors. Braz J Infect Dis. 2017;21:263–9. doi: 10.1016/j.bjid.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


