Summary
Introduction: Arterio-venous fistula (AVF) is the first-choice vascular access for hemodialysis (HD). Hemodialysis catheter (KT) may be a temporary or permanent alternative.
Aim: To evaluate indications of KT and AVF and their predictive factors of complications.
Methods: It's a retrospective multicentric study interesting KT and AVF in patients treated by hemodialysis, in the Kef Governorate in north-western Tunisia, during the period from 01/07/18 to 31/12/18.
Results: We included 288 AVF and 148 KT that were created on 205 patients. The average age was 58.14 years, the sex ratio was 1.5. Hypertensive patients and diabetics represented respectively 83.9% and 27.3% of the population. Diabetic nephropathy was the most common (25.9%). For the KT, the main indication was the wait for AVF creation (68.9%). The overall incidence of immediate complications was 11.5%. Dysfunction was reported in 23.6% of cases with obesity and tunneled type of KT as contributing factors. KT infection was occuring in 39.2% of cases. It was promoted by prolonged duration of use and hemoglobin level < 8g/dl. The use of antiseptic lock reduced infections' risk (p=0.011). For AVF, the most common complications were thrombosis (36.2%), aneurysm (29.9%) and stenosis (22.6%). Survival rate was 60% at 2000 days. The AVF impairing factors were diabetes (p=0.05), obesity (p=0.05), anterior AVF creation (p=0.011), AVF grafts (p=0.016), and anticoagulant therapy (p=0.0001). Antiplatelet therapy improved AVF patency (p=0.02).
Conclusion Much remained to be done to reduce KT complications, creation of AVF on time and prevention of their complications.
Keywords: renal insufficiency, hemodialysis, arteriovenous fistula, central venous catheterization
Résumé
Introduction: La fistule artério-veineuse (FAV) est l’accès de choix pour hémodialyse (HD). Le cathéter central (KT) peut en être une alternative.
Objectif: Evaluer les indications des KT et des FAV et leurs facteurs prédictifs de complications.
Méthodes: C’est une étude rétrospective multicentrique s’intéressant aux abords vasculaires (KT et FAV) chez les hémodialysés, dans le gouvernorat du Kef, au nord-ouest de la Tunisie, pendant la période du 01/07/18 au 31/12/18.
Résultats: Nous avons inclus 288 AVF et 148 KT créés chez 205 patients. L’âge moyen était de 58,14 ans, le sex-ratio de 1,5. Les hypertendus et les diabétiques représentaient respectivement 83,9 % et 27,3 % de la population. La néphropathie diabétique était la plus fréquente (25,9 %). L’indication des KT était l’attente de création de FAV (68,9 %). L’incidence des complications était de 11,5 % avec des dysfonctionnements dans 23,6 % des cas, favorisés par l’obésité et la tunnélisation. L’infection était présente dans 39,2 % des cas ; favorisée par une durée d’utilisation prolongée et un taux d’hémoglobine < 8g/dl. Pour les FAV, les complications étaient la thrombose (36,2 %), l’anévrisme (29,9 %) et la sténose (22,6 %). La survie était de 60 % à 2 000 jours. Les facteurs de dysfonctionnement étaient le diabète (p=0,05), l’obésité (p=0,05), une FAV antérieure (p=0,011), une FAV prothétique (p=0,016) et le traitement anticoagulant (p=0,0001). Le traitement antiplaquettaire a amélioré la perméabilité (p=0,02).
Conclusion: Il faut agir pour réduire les complications des KT, créer des FAV à temps et prévenir leurs complications.
Mots-clés: insuffisance rénale, hémodialyse, fistule artério-veineuse, cathéter veineux central
Introduction
Chronic kidney disease is a major public health problem, its incidence and prevalence are constantly increasing. Hemodialysis requires good quality vascular access which is durable and reliable.
Two main types of vascular access are described : native or prosthetic arteriovenous fistula (AVF) and central venous catheter (CVC) simple or tunneled.
Type of vascular access affect the physical and mental health as well as the survival rate of patients undergoing HD 1, 2. Regardless of the type of initial vascular access, the total amount of time on a particular type of access is also important in mortality 3.
Significant progress has been made in the technical field for creation and maintenance of hemodialysis vascular accesses, like the contribution of the operating microscope, the use of microsurgical techniques, ultrasound and interventional radiology and new biochemical materials discoveries into medical application 4, 5.
Monitoring the vascular access in dialysis patients can help in earlier identification of developing complications and ppropriate, time intervention 6.
The first works on AVF were published by Brescia and Cimino7 over 30 years ago. Experience and hindsight confirm that AVF is currently the best vascular access for hemodialysis comparing to prosthetic bypass grafts and CVC.
The aim of this work is to study vascular access indications and to identify factors favoring catheter (KT) complications and interfering with AVFs survival.
Methods
This is a retrospective, descriptive, analytical and multicentric study of the hemodialysis vascular accesses : CVC and AVF, created in patients with end-stage renal disease (ESRD) during a period of 6 months : between 01/07/2018 and 31/12/2018.
This study included patients over 18 years old, prevalent in chronic hemodialysis for at least three months in one of the four hemodialysis centers in the Kef governorate in north-western of Tunisia : (one public department and three private department).
This study did not include patients having non-permanent femoral KTs or in acute renal failure with recovery in less than three months.
Are excluded from the study patients lost to follow-up during the study period.This study allowed to select 205 patients.
Data entry was carried out on an Excel database. The results were analyzed by SPSS version 25 software. The qualitative variables were expressed in number and in percentage. Quantitative variables were expressed as mean, standard deviation from the mean, and median with minimum and maximum value. The comparison of two means on independent series was carried out by means of Student's t test.
The comparison of percentages on independent series was carried out by Pearson's chi-squared test. If this test was not valid, comparisons were made by Fisher's two-tailed exact test.
The study of vascular access survival was carried out by calculating the survival rates with the date of origin of the creation of the vascular access until the end of the patency of the latter or until the date of the last news or the point date, chosen on 12/31/2018, for the still functional vascular accesses.
Death, loss to follow-up, and termination of study for vascular access that was still functional were not considered to be loss of patency events.
For the comparative study of the survival AVF, Kaplan-Meier survival curves were established with comparison by the Log Rank test.
A value of p <0 05 was considered significant
The diagnostic criteria for a catheter-related infection were those of the CDC's National Healthcare Safety Network (CDC-NHSN) published in 2014 8.Cumulative survival of AVF was defined by the time interval between the preparation of AVF and itsabandoning with or without recanalization intervention 9.
Results
Two hundred five patients were selected for this study among 223 patients prevalent in hemodialysis during the study period.
The mean age was 58.14±15.56 years with a peak frequency of 23.4% in the age group 65-74 years. The sex ratio (M/F) was 1.5. Eighty-three point nine percent were hypertensive, 32.2% dyslipidemic and 27.8% diabetic. A body mass index (BMI) ≥ 30 kg/m2 was found in 15.6% of cases.
Glomerular nephropathy was found on 47.8% of cases with diabetic nephropathy in 25.9% of cases. Tubulointerstitial nephropathy was observed on 20% of cases, vascular nephropathy on 16.1% of cases.
Nephrological management before the start of extra-renal purification lasting more than three months was found on 58.5% of patients.
The CVC in our population had the following characteristics: One hundred and forty-eight KTs were inserted on 108 patients, the most common indication was waiting for an AVF creation on 68.9% of patients ; frequent use of non-tunnel KTs on 68.3% of cases. The right internal jugular vein was used on 64.2% of cases. Ultrasound identification of the jugular vein before insertion was performed on 70.4% of cases. Hemoglobin level < 8 g/dl at the time of insertion was found on 34% of cases.
Immediate complication was observed on 17 cases (11.5%) with an insertion failure despite several attempts in six cases, a false venous path in three cases and a pneumothorax in one case.
Thirty-five catheters (23.6%) were complicated by dysfunction: 1.54 dysfunctions/1000 KT days. The most frequent dysfunctions were thrombosis (11 cases), fall (13 cases), and malpositioning (6 cases).
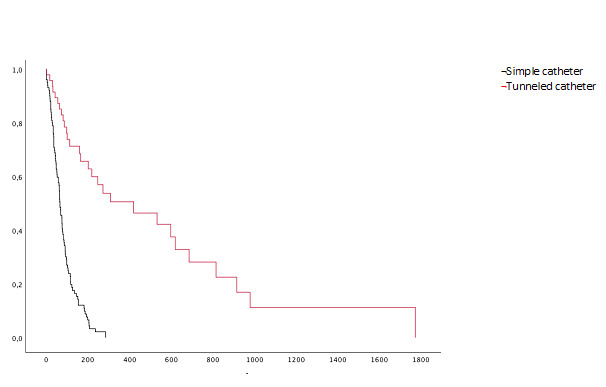
Fifty-eight catheters (39.1%) were complicated by infection: 2.54 infections/1000 KT days. These included 38 cases of bacteremia, 11catheter insertion site infection, seven cases of tunnelitis, and two cases of sepsis. The mean time to onset of infection was 177 days [3-1064 days]. The mean duration of catheter use was 77.5 days for non-tunnel catheters and 318 days for tunnel catheters Figure 1.
Figure 1. Catheter survival.
The most common cause of catheter ablation was AVF creation on 34.5% of cases, infection on 25% of cases and dysfunction on 17.6% of cases.
BMI ≥ 30 kg/m2 (p=0.035) and the use of a tunnel type catheter (p = 0.042) significantly increased the dysfunction risk.
Prolonged duration of catheter use (p = 0.041) and an hemoglobin level < 8g/dl (p = 0.039) significantly increased the KT infection risk.
Combining of heparin and Gentamicin used as catheter lock solution reduced the risk of catheter-related infection (p = 0.011).
Two hundred and eighty-eight AVF were created on 199 patients, the mean number of AVF was 1.44 ± 0.72 AVF/patient [0-5 AVF]. Patients features receiving fistula are represented in Table 1.
Table 1. Features of patients receiving fistula .
|
characteristics |
value |
|
Mean age |
57.8 ± 15.2 |
|
Sex ratio |
1.56± 0.52 |
|
smoking |
83 (41.5%) |
|
Obesity (BMI >30 kg /m2) |
32 (16%) |
|
Hypertension |
168 (84%) |
|
Diabetes Diabetes as primary cause of ESRD |
57 (28.5%) 53 (26.5%) |
|
BMI : body mass index ; ESRD : end stage renal disease |
AVF were native on 95% of cases, radio-cephalic on 42% of cases, humero-cephalic in 30.2% of cases, and humero-basilica on 22.9% of cases.
Fourteen arteriovenous bypass operations (5%) were performed.For the first 199 AVF, their site was radiocephalic on 102 cases (51%), their preparation before the start of hemodialysis was observed on 49 cases (24.5%). For the remaining 150 cases, they were created after an average of 107 days.
Immediate postoperative complications (haemorrhage or infection) were observed on 11 cases (3.8%). Primary failures were recorded on 23 cases (7.9%). Thrombosis, aneurysm and stenosis were found on 36.2%, 29.9%, and 22.6%, respectively.The mean AVF survival time was 1500 days [0-11710 days]. Survival was 76% at 1000 days (≈2.7 years), 62% at 2000 days (≈5.4 years) and 47% at 4000 days (≈11 years) Figure 2.
Figure 2. Arteriovenous fistula survival.
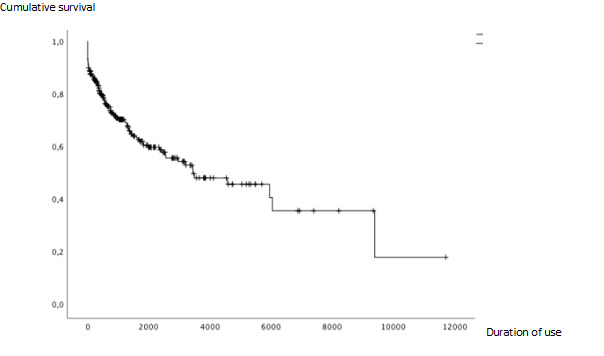
Associated factors with the loss of AVF were diabetes (p = 0.05), obesity (p = 0.05), previous AVF making (p = 0.011), prosthetic AVFs compared to native AVFs (p = 0.016), taking an anticoagulant after making AVF (p = 0.0001).
Associated factor with better survival of AVF was the use of an antiplatelet drug (p = 0.02) Table 2 .
Table 2. AVFs survival factors.
|
Factor |
P (log rank) |
|
No impact : Age Gender Smoking Hypertension Prior use of venous catheter AVF creation before HD AVF location ARA II, ACE inhibitors treatment Statine |
0.468 0.528 0.077 0.591 0.505 0.578 0.502 0.502 0.431 |
|
Negative impact : Obesity Diabetes Anterior creation of AVF anticoagulant |
0.05 0.05 0.011 <0.001 |
|
Positive impact : Antiplatelets drug intake |
0.02 |
|
AVF : arteriovenous fistula ; HD : hemodialysis ; ARA II : Angiotensin II receptor antagonists ; ACE inhibitors : Angiotensin-converting-enzyme inhibitors |
Discussion
The main features of our study are the late discovery of ESRD requiring start of extra-renal purification before making permanent vascular access and non-tunneled CVC predominance. Obesity and tunneled CVC were risk factors for catheter dysfunction. Prolonged duration use of CVC, and an hemoglobin level < 8 g/dl were risk factors for CVC infection. Lock combining heparin and Gentamicin was a protective factor.
Diabetes, obesity, prosthetic AVF, history of making AVF, anticoagulants had negative impact on AVF survival. Taking an antiplatelet drug was associated with better AVF survival.
Highlights of the study are its multicentric nature, number of cases, the study of the two types of catheters (tunnelled/non-tunnelled) and VFVs survival with a large degree of hindsight.
Weaknesses of the study are the interest to only prevalent patients and absence of multivariate analysis.
According to theDialysis Outcomes and Practice Patterns Study (DOPPS) register 10, the duration of nephrological follow-up before the start of the extra-renal purification varied from one country to another: A nephrological consultation at least 4 months before dialysis start was seen in 80% of cases in Spain, 69% of cases in the United States and in 37% of cases in China. In our series, 58.5% of patients had seen a nephrologist at least 3 months before the start of hemodialysis.
According to the latest Kidney Disease Outcomes Quality Initiative (KDOQI) recommendations, AVF is considered the optimal vascular access in hemodialysis due to its better long-term patency and lower rate of complications compared to catheters. The latter, preferably tunneled, should only be used in the short term or in valid circumstances such as depletion of venous capital or limited life expectancy 11.
In the prospective multicenter DOPPS 5 study comparing practices in different countries (from 2012 to 2014), 28% of American patients, 50 to 60% of European patients and 84% of Japanese started hemodialysis with AVF. In the same register, 67% of Americans started hemodialysis with a catheter 10.
In France and according to the annual report of the REIN registry on 2016, 18% of incident hemodialysis patients were dialysed via CVC 12.
In Tunisia, concerning 533 patients who started hemodialysis on 2001 and whose follow-up lasted until 2005, no patient had a functional AVF before the first hemodialysis session 13.
In our study, an AVF was created before the start of hemodialysis in only 24.5% of cases.
This can be explained by the reduced number of vascular surgery services in our country or even their absence in some regions, implying laborious travel for chronic hemodialysis patients and late operating appointments, as well as by the late discovery of chronic renal failure. In our work, 26.8% of patients started hemodialysis in an emergency setting.
It is recommended that CVC have to be tunneled. The duration use of single catheter should not exceed 15 days 11. According to the DOPPS registry, the majority of catheters were tunneled (11% versus 3% non-tunneled) 14. In our study, single catheters were used much more than tunneled catheters (68.3% versus 32.7%). This could be explained by the high cost of tunneled catheters which are not covered by health insurance funds and the low to medium socio-economic level of our population.
The major indication for catheter placement is the absence of AVF at the initiation of hemodialysis 10, 15, 16. This percentage varies from 61.9% in the USA to 8% in Japan 10, 15. It is 68.9% in our study. In the United States, after the implementation of the “Fistula First” strategy, which was based on sensitizing practitioners to the advantages of native AVF, the number of KT has clearly decreased, from 27% on 2003 to 19, 5% on 2016 15, 17.
Immediate complications are related to the KT placement procedure and the doctor's experience. They vary from 5 to 19% 18. In our work, they were at 11.5%.
Regarding CVC infectious complications, in the literature, bacteremia is the most described form with an incidence varying from 0.2 to 9/1000 KT days 19, 20, on our study, the incidence of bacteremia was 1.67 / 1000 KT days.
Catheter dysfunction varies from 17 to 33% 21. It is 23.6% in our series.
Tunnel catheter was associated in our study with a significantly greater risk of dysfunction compared to the single catheter (p = 0.042), which could be explained by the much longer duration of use of permanent catheters. Obesity also significantly increased the risk of dysfunction (p = 0.035), this is probably due to the risk of catheter mispositioning in this population as well as dyslipidemia and atherosclerosis which increase the risk of coagulopathy.
In Japan, the distal AVF is the most used with a rate around 95% from 1996 to 2015. In Europe, Australia and New Zealand, the use of distal AVF has increased from 77% in 1996 to 66% in 2015. However, in the USA, the rate of preparation of distal AVFs halved between 1996 and 2015, going from 70% to 32% against an increase in the rate of preparation of proximal AVFs from 30 to 68% during this same period.
In our study, distal AVF was found in 42%. This could be explained by causes linked to patients (diabetes, elderly subjects, absence of nearby vascular surgery department) and by surgical habits. At the proximal level, the diameter of the vessels is larger, offering surgical ease with more success for AVFs at this level.
According to the DOPPS study, native AVF accounts for 65-92% of vascular accesses for hemodialysis in Russia, Japan, China, Turkey, Germany, Italy, United Kingdom, New Zealand, and Australia. Its prevalence is 57% in the Gulf countries and 49% in Canada 10. It is of 95% in our series.
In the United States, native AVF has significantly increased, it went from 24% in 1997 to 68% in 2013 10, 17.
Native AVF is preferred to bypass surgery because of a lower risk of infectious complications, better survival, and its lower cost.
Late infection usually occurs from the puncture sites. It is rare but worrying especially for bypass 22. Their rates vary from 0.35 to 9.6 according to studies it was of 2.4 % in our study.
AVF survival was variable: 68% at one year in the USA, 83% at 1 year in Europe and 76% at 1000 days (2.7 years) in our study.
This survival depends on several factors: advanced age 23, 24, female gender (smaller vessels diameter) 25; smoking 23, 26 , obesity 27, diabetes 26, 28, hypertension 29 , AVF creation after the start of dialysis 30, prior catheterization31, 32 , second AVF 25, 26, 27, 28, 29, 32, prosthetic AVF25 decreased the survival of AVF.
Factors associated with better survival of AVF were antiplatelet agents 29, 31, 32, 33, 34, also found in our study (p = 0.02) and renin angiotensin aldosterone system inhibitors 26, 34.
A large number of patients undergoing HD die every year and the type of vascular access has an important role in mortality of these patients 35. The total amount of time on a particular type of access is also important in mortality 3.
Conclusion
In our study, he late discovery of ESRD lead to extra-renal purification before making AVF. The predominant use of non-tunneled CVC is explained by their lower cost. Obesity and tunneled CVC were risk factors for catheter dysfunction. Prolonged duration use of CVC, and an hemoglobin level < 8 g/dl were risk factors for CVC infection. Diabetes, obesity, prosthetic AVF, history of making AVF, anticoagulants had negative impact on AVF survival.
In view of these findings and the literature, we offer these recommendations:
- Screening for chronic renal disease in populations at risk and their early management by the nephrologist
- Preservation of patient's venous capital.
- AVF preparation and maturation before the onset of ESRD.
Conflict of interest
This study was not subject to any conflict of interest.
References
- Banerjee Tanushree, Kim S. Joseph, Astor Brad, Shafi Tariq, Coresh Josef, Powe Neil R. American Journal of Kidney Diseases. 6. Vol. 64. Elsevier BV; 2014. Vascular Access Type, Inflammatory Markers, and Mortality in Incident Hemodialysis Patients: The Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study; pp. 954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Do Hyoung, Park Ji In, Lee Jung Pyo, Kim Yong-Lim, Kang Shin-Wook, Yang Chul Woo, Kim Nam-Ho, Kim Yon Su, Lim Chun Soo. Renal Failure. 1. Vol. 42. Informa UK Limited; 2020. The effects of vascular access types on the survival and quality of life and depression in the incident hemodialysis patients; pp. 30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firouraghi N, Jahromi S E, Sami A, Sharifian R. Duration of Vascular Access Usage and Patient Survival in the First Year of Hemodialysis. Iran J Kidney. 2019;13:398–403. [PubMed] [Google Scholar]
- Agarwal Anil K., Haddad Nabil J., Vachharajani Tushar J., Asif Arif. Kidney International. 5. Vol. 95. Elsevier BV; 2019. Innovations in vascular access for hemodialysis; pp. 1053–1063. [DOI] [PubMed] [Google Scholar]
- Murea Mariana, Geary Randolph L., Davis Ross P., Moossavi Shahriar. Seminars in Dialysis. 6. Vol. 32. Wiley; 2019. Vascular access for hemodialysis: A perpetual challenge; pp. 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raza H, Hashmi MN, Dianne V, Hamza M, Hejaili F, A-Sayyari A. Saudi Journal of Kidney Diseases and Transplantation. 1. Vol. 30. Medknow; 2019. Vascular access outcome with a dedicated vascular team based approach; pp. 39–39. [DOI] [PubMed] [Google Scholar]
- Brescia Michael J., Cimino James E., Appel Kenneth, Hurwich Baruch J. New England Journal of Medicine. 20. Vol. 275. Massachusetts Medical Society; 1966. Chronic Hemodialysis Using Venipuncture and a Surgically Created Arteriovenous Fistula; pp. 1089–1092. [DOI] [PubMed] [Google Scholar]
- Böhlke Maristela, Uliano Gustavo, Barcellos Franklin C. The Journal of Vascular Access. 5. Vol. 16. SAGE Publications; 2015. Hemodialysis Catheter-related Infection: Prophylaxis, Diagnosis and Treatment; pp. 347–355. [DOI] [PubMed] [Google Scholar]
- Lee Timmy, Mokrzycki Michele, Moist Louise, Maya Ivan, Vazquez Miguel, Lok Charmaine E. Seminars in Dialysis. 5. Vol. 24. Wiley; 2011. Standardized Definitions for Hemodialysis Vascular Access; pp. 515–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisoni Ronald L., Zepel Lindsay, Port Friedrich K., Robinson Bruce M. American Journal of Kidney Diseases. 6. Vol. 65. Elsevier BV; 2015. Trends in US Vascular Access Use, Patient Preferences, and Related Practices: An Update From the US DOPPS Practice Monitor With International Comparisons; pp. 905–915. [DOI] [PubMed] [Google Scholar]
- KDOQI clinical practice guideline for vascular access; National Kidney Foundation-Dialysis Outcomes Quality Initiative; New York. 2018. [Google Scholar]
- Glaudet F, Jaïs J P, Moranne O, Lassalle M. Caractéristiques cliniques et indicateurs de prise en charge des patients en dialyse: rapport annuel du registre REIN. Agence of biomedecine. 2016:191–235. [Google Scholar]
- Hamida Ben, F, 'hibik M, Karoui S, Abderrahim C, Kaaroud E, Beji H, S. Indications, complications and cost of internal jugular catheters in hemodialysed patients: study of 533 cases. Tunis Med. 2005;83:519–542. [PubMed] [Google Scholar]
- Pisoni Ronald L., Arrington Charlotte J., Albert Justin M., Ethier Jean, Kimata Naoki, Krishnan Mahesh, Rayner Hugh C., Saito Akira, Sands Jeffrey J., Saran Rajiv, Gillespie Brenda, Wolfe Robert A., Port Friedrich K. American Journal of Kidney Diseases. 3. Vol. 53. Elsevier BV; 2009. Facility Hemodialysis Vascular Access Use and Mortality in Countries Participating in DOPPS: An Instrumental Variable Analysis; pp. 475–491. [DOI] [PubMed] [Google Scholar]
- Aran R, Li Y, Robinson B, Abbott K C, Agodoa Lyc, Ayanian J. United States renal data system: vascular access. Am J Kidney Dis. 2019;73:369–86. [Google Scholar]
- Randriamanantsoa L N, Rajaonera T A, Ramanamidora D A, Ravalisoa M L, Andriamarotia H W, Rabenatoandro R. Les complications des cathéters veineux centraux d'hémodialyse dans les centres d'hémodialyse d'Antananarivo. Rev Anest Rea Med Urg. 2011;3:1–5. [Google Scholar]
- Lee T. Cardiovascular Engineering and Technology. 3. Vol. 8. Springer Science and Business Media LLC; 2017. Fistula First Initiative: Historical Impact on Vascular Access Practice Patterns and Influence on Future Vascular Access Care; pp. 244–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusminsky Roberto E. Journal of the American College of Surgeons. 4. Vol. 204. Elsevier BV; 2007. Complications of Central Venous Catheterization; pp. 681–696. [DOI] [PubMed] [Google Scholar]
- Leou S, Garnier F, Testevuide P, Lumbroso C, Rigault S, Cordonnier C. Infectious complications rate from hemodialysis catheters: experience from the French Polynesia. Nephrol Ther. 2013;9:137–179. doi: 10.1016/j.nephro.2013.01.003. [DOI] [PubMed] [Google Scholar]
- David N, Ian R, Elias A, Mohamad Ala, Vincent B, Sandra C. 2018
- Chan M R. Hemodialysis central venous catheter dysfunction. Semin Dial. 2008;21:516–537. doi: 10.1111/j.1525-139X.2008.00495.x. [DOI] [PubMed] [Google Scholar]
- Bourquelot P. EMC - Cardiologie-Angéiologie. 4. Vol. 2. Elsevier BV; 2005. Abords vasculaires pour hémodialyse; pp. 566–571. [DOI] [Google Scholar]
- Smith George E., Gohil Risha, Chetter Ian C. Journal of Vascular Surgery. 3. Vol. 55. Elsevier BV; 2012. Factors affecting the patency of arteriovenous fistulas for dialysis access; pp. 849–855. [DOI] [PubMed] [Google Scholar]
- Lazarides Miltos K., Georgiadis George S., Antoniou George A., Staramos Dimitrios N. Journal of Vascular Surgery. 2. Vol. 45. Elsevier BV; 2007. A meta-analysis of dialysis access outcome in elderly patients; pp. 420–426.e2. [DOI] [PubMed] [Google Scholar]
- Gibson Kathleen D., Gillen Daniel L., Caps Michael T., Kohler Ted R., Sherrard Donald J., Stehman-Breen Catherine O. Journal of Vascular Surgery. 4. Vol. 34. Elsevier BV; 2001. Vascular access survival and incidence of revisions: A comparison of prosthetic grafts, simple autogenous fistulas, and venous transposition fistulas from the United States Renal Data System Dialysis Morbidity and Mortality Study; pp. 694–700. [DOI] [PubMed] [Google Scholar]
- Gheith O A, Kamal M M. Dialysis risk factors of vascular access failure in patients on hemodialysis. Iran J Kidney Dis. 2008;2:201–208. [PubMed] [Google Scholar]
- Kats N., Hawxby A.M., Barker J. Journal of Vascular Surgery. 3. Vol. 46. Elsevier BV; 2007. Impact of obesity in arteriovenous fistula outcomes in dialysis patients; pp. 608–608. [DOI] [PubMed] [Google Scholar]
- Monroy-Cuadros Mauricio, Yilmaz Serdar, Salazar-Bañuelos Anastasio, Doig Christopher. Clinical Journal of the American Society of Nephrology. 10. Vol. 5. American Society of Nephrology (ASN); 2010. Risk Factors Associated with Patency Loss of Hemodialysis Vascular Access within 6 Months; pp. 1787–1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wayne Erik J., Brier Michael E., Dwyer Amy C. Seminars in Dialysis. 1. Vol. 26. Wiley; 2013. Association of Maturation Period Blood Pressure with Dialysis Access Patency; pp. 90–96. [DOI] [PubMed] [Google Scholar]
- Kalantarinia Kambiz, Campbell Adam, Mourad Shadi, Kauffnan Judy, Deaver Kim. American Journal of Kidney Diseases. 4. Vol. 55. Elsevier BV; 2010. 141: Timing of Hemodialysis Vascular Access Placement Determines Access Outcomes; pp. B67–B67. [DOI] [Google Scholar]
- Lammouchi MohamedAli, Zouaghi MohamedKarim, Hassen Mohaned, Rais Lamia, Krid Madiha, Smaoui Wided, Jebali Hela, Kheder Rania, Hamida FethiBen, Moussa FatmaBen, Fatma LiliaBen, Beji Soumaya. Saudi Journal of Kidney Diseases and Transplantation. 3. Vol. 29. Medknow; 2018. Determinants of patency of arteriovenous fistula in hemodialysis patients; pp. 615–615. [DOI] [PubMed] [Google Scholar]
- Asano Manabu, Thumma Jyothi, Oguchi Kenichi, Pisoni Ronald L., Akizawa Tadao, Akiba Takashi, Fukuhara Shunichi, Kurokawa Kiyoshi, Ethier Jean, Saran Rajiv, Saito Akira. Nephron Clinical Practice. 1-2. Vol. 124. S. Karger AG; 2013. Vascular Access Care and Treatment Practices Associated with Outcomes of Arteriovenous Fistula: International Comparisons from the Dialysis Outcomes and Practice Patterns Study; pp. 23–30. [DOI] [PubMed] [Google Scholar]
- Dember Laura M., Beck Gerald J., Allon Michael, Delmez James A., Dixon Bradley S., Greenberg Arthur, Himmelfarb Jonathan, Vazquez Miguel A., Gassman Jennifer J., Greene Tom, Radeva Milena K., Braden Gregory L., Ikizler T. Alp, Rocco Michael V., Davidson Ingemar J., Kaufman James S., Meyers Catherine M., Kusek John W., Feldman Harold I., Dialysis Access Consortium Study Group for the. JAMA. 18. Vol. 299. American Medical Association (AMA); 2008. Effect of Clopidogrel on Early Failure of Arteriovenous Fistulas for Hemodialysis; pp. 2164–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saran Rajiv, Dykstra Dawn M., Wolfe Robert A., Gillespie Brenda, Held Philip J., Young Eric W. American Journal of Kidney Diseases. 6. Vol. 40. Elsevier BV; 2002. Association between vascular access failure and the use of specific drugs: The dialysis outcomes and practice patterns study (DOPPS) pp. 1255–1263. [DOI] [PubMed] [Google Scholar]
- http://www.usrds.org/adr.aspx United States Renal Data System: Annual Data Report. 2018


