Abstract
Whole-exome sequencing (WES) is an effective approach to identify the susceptibility of genetic variants of autism spectrum disorder (ASD). The Israel Ministry of Health supports WES as an adjunct tool for ASD diagnosis, despite its unclear diagnostic yield and cost effectiveness. To address this knowledge gap, we applied WES to a population-based sample of 182 Bedouin and Jewish children with ASD from southern Israel, and assessed its yield in a gene panel of 205 genes robustly associated with ASD. We then compared the incremental cost-effectiveness ratios (ICERs) for an ASD diagnosis by WES, chromosomal microarray analysis (CMA), and CMA + WES. Overall, 32 ASD candidate variants were detected in 28 children, corresponding to an overall WES diagnostic yield of 15.4%. Interestingly, the diagnostic yield was significantly higher for the Bedouin children than for the Jewish children, i.e., 27.6% vs. 11.1% (p = 0.036). The most cost-effective means for genetic testing was the CMA alone, followed closely by the CMA + WES strategy (ICER = USD 117 and USD 124.8 per child). Yet, WES alone could become more cost effective than the other two approaches if there was to be a 25% increase in its yield or a 50% decrease in its cost. These findings suggest that WES should be recommended to facilitate ASD diagnosis in Israel, especially for highly consanguineous populations, such as the Bedouin.
Keywords: autism spectrum disorder, genetics, whole-exome sequencing, diagnostic yield, cost-effectiveness analysis
1. Introduction
Autism spectrum disorder (ASD) is a collection of heterogeneous neurodevelopmental disorders that affects nearly 2% of children worldwide [1]. While the specific etiologies of ASD are still largely unknown, it is currently believed that ASD has a significant genetic susceptibility component, as is evident from multiple twin, familial and population studies [2,3,4,5,6,7]. Indeed, the genetic studies of ASD over the past two decades have revealed hundreds of rare genetic variants associated with ASD susceptibility [8], most commonly, the rare copy number variants (CNVs) [9,10,11,12,13] and single nucleotide variants (SNVs) [14,15,16]. To date, these variants together can explain up to 35% of ASD cases [17,18,19,20], and can be used for genetic screening of ASD [21]. In this realm, whole-exome sequencing (WES), which captures 1–2% of protein-coding sequences in the genome, is the genomic technique most relevant for clinical use [22,23].
In Israel, an ASD diagnosis is based on behavioral and cognitive assessments and is determined by a psychiatrist and a developmental pediatrician, or a child neurologist together with a clinical psychologist [24]. In addition, each child diagnosed with ASD is eligible for a government-funded chromosomal microarray (CMA) test [25]. Recently, the Israel Ministry of Health recommended supplementing this test with a WES analysis, especially for children with severe ASD and/or those from multiplex ASD families [25]. While genetic testing for ASD has obvious clinical benefits (e.g., facilitating early intervention and, hence, improved outcomes), its economic implications are currently not clear.
Raising a child with ASD involves a substantial financial burden on the family, further exacerbating the physical, psychological and social difficulties associated with ASD [26,27,28]; for example, in an Australian study published in 2014, the median cost to the family of a child with ASD was estimated to be USD 23,700 per year, 90% of which was due to a loss of employment hours [29]. In another study that was performed in the United States and the United Kingdom, the lifetime cost of supporting an individual with ASD exceeded USD 2.2 million [30]. In Israel, the child allowance (paid by the National Insurance Institute of Israel) for a child with ASD can reach USD 15,600 per year, constituting 188% of the regular child allowance [31]. This payment is made to help the child’s family partially cover the costs associated with raising a child with ASD. At the age of 18 years, the allowance paid to the person with ASD may be significantly increased to USD 2760 per month [32,33] to cover the daily expenditure of a disabled person, if it is proven that the disabled person has limited earning possibilities.
In health systems management, a cost-effectiveness analysis is an economic assessment tool that is used to quantify the gains in population health due to a specific intervention or policy implementation [34]. In this analysis, the gains are typically assessed by disability-adjusted life year (DALY) or quality-adjusted life year (QALY), indices that incorporate morbidity and mortality, and, therefore, cover both quality of life and life span. Costs include both direct and indirect costs, and comparisons can be made against alternative strategies or against no intervention at all. At present, there is not sufficient research regarding the cost effectiveness of genetic testing of ASD (e.g., [35]), primarily because data about the yield of next-generation sequencing approaches (e.g., WES) in detecting ASD susceptibility variants are sparse, and there is also a lack of data about the lifelong outcomes of a genetic-based ASD diagnosis. In this study, we applied WES analysis to a population-based sample of children with ASD from southern Israel to assess the yield of WES in detecting genetic variants associated with ASD, and to estimate the cost effectiveness of WES findings for families with children with ASD.
2. Materials and Methods
2.1. Study Sample and Statistical Analysis
The study sample was drawn from children who were diagnosed with ASD at the National Autism Research Center of Israel (NARCI) [36,37], which is located in Be’er Sheva, the capital city of the southern region, between January 2015 and December 2019. The sample included all the children whose parents consented to provide DNA samples for themselves and the children. Based on our clinical records, none of the parents in the study have been diagnosed with ASD, intellectual disability, or any other type of neurodevelopmental disorder. The study sample thus comprised 182 children with ASD (135 Jewish and 47 Bedouin) from 169 families. Of these, one Bedouin family had three affected children, 11 families (10 Jewish and 1 Bedouin) had two affected children, and the remaining 157 families each had one affected child. Demographic and clinical variables were compared between children included in this study and other children in the NARCI database, as well as between children with and without identified genetic variants by WES using standard univariate statistics. Specifically, Mann–Whitney rank sum test was used to assess group differences in continuous and ordinal variables while chi-square or Fisher exact tests were used to assess differences in nominal variables. All statistical tests were performed in IBM SPSS statistical software version 23.
2.2. Whole-Exome Sequencing
Genomic DNA was purified from saliva samples collected from the affected children and their parents with Genotek OG-500 and OG-575 saliva collection kits. The DNA samples were sent for WES at the Broad Institute (USA) as part of the autism sequencing consortium (ASC) initiative, as described before [38]. WES results for each DNA sample were obtained in both bam file format (*.bam) and in variant call file format (*.vcf), with the latter format summarizing the variant calls and annotation of the entire sample.
2.3. Identification of Candidate ASD Genetic Variants
We developed a bioinformatics pipeline to analyze the WES data with the goal to identify ASD susceptibility variants in genes robustly associated with ASD according to the SFARI gene database [39] (all genes with score 1 as of January 2021 (n = 205) listed in Supplementary Table S1). We restricted our search to this high-confidence ASD gene panel to assess the current lowest bounds of WES yield and its cost-effectiveness for ASD diagnosis. The pipeline was applied to the multi-sample VCF file that was generated according to the GATK (Genome Analysis Toolkit) best practice guidelines [40]. First, we removed variants with a minor allele frequency of >5% and also variants with low sequence coverage (DP ≤ 20) or low genotype quality (GQ ≤ 50). Then, we used the Ensembl Variant Effect Predictor (VEP) [41] to assess the effect of the variant on the protein sequence. We only considered variants with the following protein sequence effects: stop gained/lost, start lost, splice acceptor/donor, frameshift, and nonsynonymous missense variants with a “deleterious effect” according to either SIFT [42] or PolyPhen-2 [43]. Next, we evaluated the segregation of each of the remaining variants in each family trio (proband and parents) to identify only those variants with proband-specific genotypes (i.e., de novo, recessive, and compound heterozygote, and for male probands X-linked). Of note, de novo variants that appeared in more than two individuals were removed from the analysis, as these are likely to be false positives. Finally, we visually validated (manual curation) the existence of the remaining variants using IGV software [44].
2.4. Cost-Effectiveness Analysis
We calculated the incremental cost-effectiveness ratios (ICERs) [45] of a genetic diagnosis for ASD for the following three different diagnostic strategies: (1) CMA alone; (2) WES alone; (3) CMA followed by WES for those with inconclusive CMA findings (CMA + WES). ICER is the ratio between the difference in cost and the difference in outcomes between two interventions (i.e., ICER = ∆Costs/∆Outcomes). The cost of the genetic diagnosis in each scenario included the cost of the genetic test (comprising laboratory expenses and bioinformatics costs) [46,47], the cost of genetic counseling [48], and the parents’ productivity cost (total time spent in clinical consultations) based on the average salary/hour in Israel on 1 January 2021 [49] and assuming that both parents were employed and had to spend two work hours for the genetic test. The details of these costs are presented in Supplementary Table S2. We used the genetic yield of each genetic strategy as the outcome measure for its ICER calculation. Specifically, we used the reported CMA diagnostic yield of 10% [50], the WES diagnosis yield found in this study, and the WES + CMA yield, assuming no overlap between WES and CMA findings. For each of the three genetic diagnosis strategies, ICER was calculated using “ASD diagnosis without genetic test” as the reference. Thus, the differences in ICER values between the genetic tests represent the actual difference in their cost effectiveness.
3. Results
The WES analysis was completed for 182 of the 872 children with ASD (20.9%) who were registered in the NARCI database at the time of the study (February 2021). Table 1 presents the basic demographic and clinical characteristics of this sample of 182 children in comparison with the other children in the NARCI database. Children with exome data vs. children without exome data were diagnosed earlier (3.01 ± 1.43 vs. 3.35 ± 1.37 years, respectively; p = 0.0004), had a higher Autism Diagnostic Observation Schedule (ADOS™) comparison score (7.47 ± 2.3 vs. 6.65 ± 2.3; p < 0.0001), and were characterized by more severe ASD symptoms, according to both DSM-5 severity criteria A (49.4% vs. 39.4%; p = 0.0014) and B (38.0% vs. 27.0%; p < 0.0001). These differences suggest that the parents of children with more severe ASD symptoms are more interested in understanding the genetic causes of ASD in their children.
Table 1.
Characteristics of the 872 children with ASD in the NARCI database.
| Variable | Children with Exome (N = 182) | Children without Exome (N = 690) | p-Value | |
|---|---|---|---|---|
| Gender (Male) | 139 (76.4%) | 555 (80.4%) | 0.2844 a | |
| Ethnicity (Bedouin) | 47 (25.8%) | 165 (23.9%) | 0.5512 a | |
| Diagnosis age (years; mean, SD) | 3.01 (1.43) | 3.35 (1.37) | 0.0004 b | |
| IQ (mean, SD) | 72.71 (18.79) | 75.37 (17.89) | 0.1516 b | |
| ADOS module (N = 705) |
Toddler | 57 (39.3%) | 150 (26.8%) | 0.0165 c |
| 1 | 57 (39.3%) | 239 (42.7%) | ||
| 2 | 18 (12.4%) | 111 (19.8%) | ||
| 3 | 13 (9.0%) | 60 (10.7%) | ||
| ADOS comparison score (mean, SD) | 7.47 (2.3) | 6.65 (2.3) | <0.0001 b | |
| DSM-5 severity level (A) # (N = 782) |
1 | 12 (7.6%) | 112 (17.9%) | 0.0014 c |
| 2 | 68 (43.0%) | 266 (42.6%) | ||
| 3 | 78 (49.4%) | 246 (39.4%) | ||
| DSM-5 severity level (B) # (N = 782) |
1 | 15 (9.5%) | 145 (23.2%) | <0.0001 c |
| 2 | 83 (52.5%) | 310 (49.7%) | ||
| 3 | 60 (38.0%) | 169 (27.0%) | ||
Values are numbers of participants, with percentages in parentheses, unless specified otherwise. # DSM-5 severity levels: 1—“Requiring support”; 2—“Requiring substantial support”; 3—“Requiring very substantial support”. a χ2 test; b Mann-–Whitney U test; c χ2 linear-by-linear test.
3.1. Genetic Findings
Overall, 32 ASD candidate variants were detected in 28 children, corresponding to an overall diagnostic yield of 15.4% of the WES analysis. In four of these children, two ASD candidate variants were found, each variant in a different gene. Eight of the detected variants (25%) were protein-truncating variants (five frameshift and three nonsense variants), and the remaining (75%) were missense variants. In addition, 10 (26%) de novo variants were detected, 15 variants (47%) showed an autosomal recessive segregation (with four of them in the form of compound heterozygotes), and another seven variants (22%) were found in genes on the X-chromosome and showed X-linked segregation with ASD. Additional details about the 32 identified variants, including, for example, their exact genomic and protein sequence positions, are given in Supplementary Table S3.
Table 2 presents the sociodemographic and clinical characteristics of the children with positive and negative findings in the WES analysis. Interestingly, the Bedouin children comprised 46.4% of the children with WES-positive findings, more than twice their portion in the group of children with negative WES findings (22.1%). This means that the WES yield was significantly higher in the Bedouin children than in the Jewish children (27.7% vs. 11.1%, respectively; p = 0.036). No other differences were observed between the groups of children with and without WES-positive findings.
Table 2.
Characteristics of 182 children with ASD for whom WES results were available.
| Variable | Children with Positive WES Findings (N = 28) |
Children with Negative WES Findings (N = 154) |
p-Value | |
|---|---|---|---|---|
| Gender (Male) | 20 (71.4%) | 119 (77.3%) | 0.503 a | |
| Ethnicity (Bedouin) | 13 (46.4%) | 34 (22.1%) | 0.036 a | |
| Diagnosis age (years; mean, SD) | 2.62, 0.90 | 3.08, 1.50 | 0.114 b | |
| IQ (mean, SD) | 69.6, 18.42 | 73.2, 18.89 | 0.38 b | |
| ADOS module (N = 145) |
Toddler | 12 (50%) | 45 (37.2%) | 0.162 c |
| 1 | 9 (37.5%) | 48 (39.7%) | ||
| 2 | 2 (8.3%) | 16 (13.2%) | ||
| 3 | 1 (4.2%) | 12 (9.9%) | ||
| ADOS comparison score (mean, SD) | 8.04, 2.44 | 7.36, 2.252 | 0.073 b | |
| DSM-5 severity level (A) # (N = 158) |
1 | 3 (11.5%) | 9 (6.8%) | 0.33 c |
| 2 | 12 (46.2%) | 56 (42.4%) | ||
| 3 | 11 (42.3%) | 67 (50.8%) | ||
| DSM-5 severity level (B) # (N = 158) |
1 | 2 (7.7%) | 13 (9.8%) | 0.412 c |
| 2 | 17 (65.4%) | 66 (50%) | ||
| 3 | 7 (26.9%) | 53 (40.2%) | ||
Values are numbers of participants, with percentages in parentheses, unless otherwise specified. # DSM-5 severity levels: 1—“Requiring support”; 2—“Requiring substantial support”; 3—“Requiring very substantial support”. a χ2 test; b Mann–Whitney U test; c χ2 linear-by-linear test. Bold font represents significant differences.
3.2. Cost-Effectiveness Analysis
The results of the cost effective analysis for the different genetic tests are presented in Table 3. The most cost-effective genetic diagnosis strategy for ASD in Israel today, as evaluated by the ICER, is the CMA (ICER = USD 117 per child), followed by the combined CMA + WES strategy (ICER = USD 124.8 per child), and then by WES alone (ICER = USD 147.4 per child).
Table 3.
Cost-effective analysis of different genetic diagnosis strategies.
| Strategy | Total Cost (USD) | Outcome–Diagnostic Yield by Each Strategy (%) | Incremental Cost-Effectiveness Ratio (ICER) |
|---|---|---|---|
| CMA | 1170 | 10 | 117.0 |
| WES | 2270 | 15.4 | 147.4 |
| CMA + WES | 3170 | 25.4 | 124.8 |
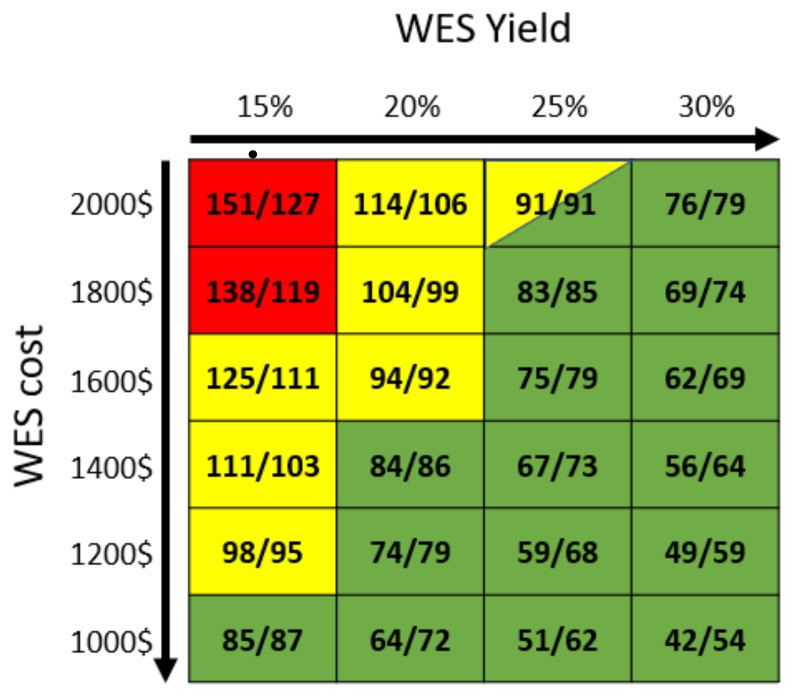
We then calculated the prospective ICER for both WES and CMA + WES for different increasing yields and decreasing costs of the WES analysis (Figure 1). As expected, the ICER for both WES alone and the WES + CMA approach decreased with either an increase in the WES yield or a decrease in the WES cost. Consequently, even a slight increase in the WES yield (from 15% to 20%) or a decrease of 20% in the cost of WES (from USD 2000 to USD 1600) would make the combined CMA + WES approach the most cost-effective approach for all, and an additional increase in the yield or decrease in the cost (or both) would make WES alone the most cost-effective approach. Notably, at a WES yield of 25% and a cost of USD 2000, WES alone and CMA + WES would have an identical ICER value of USD 91 per child.
Figure 1.
Incremental cost-effectiveness ratio (ICER) of WES alone and of CMA + WES strategies for different WES yields and costs. The ICERs of the WES strategy (numbers on the left) and of the CMA + WES (numbers on the right) strategy are depicted for different WES yields (X-axis) and costs (Y-axis). Cell colors indicate the most cost-effective strategy for each WES yield–cost combination (red, CMA alone; yellow, CMA + WES; green, WES alone).
4. Discussion
4.1. Whole-Exome Sequencing Yield
The ASD WES diagnostic yield of 15.4% that was obtained in this study is consistent with the 8–25% WES yield obtained for children with ASD in other similar studies around the world [34,48]. Obviously, relaxation of the strict criteria used for the identification of candidate ASD variants in this study would have increased the WES yield, but it could have also led to a higher rate of false-positive findings. Unfortunately, today, there are no clear diagnostic criteria for the WES analysis of ASD. The guidelines of the American College of Medical Genetics and Genomics (ACMG) for the interpretation of sequence variants [51] that are usually used for this purpose are largely applicable to inherited Mendelian disorders, and are, therefore, less appropriate for multifactorial conditions, such as ASD [52,53]. Obviously, ongoing and future genetic studies of ASD will lead to the identification of additional genes associated with ASD, and to an improved understanding of the genetic etiology of ASD, which, in turn, will increase the diagnostic yield of WES for ASD.
4.2. Ethnic Differences in Whole-Exome Sequencing Yield
The finding of significant differences in the WES yields between the Bedouin and Jewish families suggests that there may be different genetic causes of ASD in these two populations. This finding is not surprising, given the remarkable genetic differences between these two populations [54]. Specifically, the Bedouin, who live mainly in southern Israel and represent about 3.5% of the country’s population [55], constitute a highly inbred community (due to the high rates of consanguineous marriages [56]), resulting in relatively high incidences of specific genetic disorders [56], and possibly also in the aggregation of ASD susceptibility genetic variants in certain families. The higher rate of children with severe ASD in the Bedouin population, as reported previously [57], could partially derive from this lifestyle, although it could also be attributed to an underdiagnosis of milder types of ASD in this population [58].
4.3. Cost Effectiveness of Whole-Exome Sequencing for Children with ASD in the Israeli Health System
Our data show that, currently, the most cost-effective strategy for ASD genetic diagnosis in Israel is CMA alone. Nevertheless, our results suggest that adding WES analysis for children with negative findings in the CMA analysis will almost triple the diagnostic yield of the genetic test for ASD, with only a minor increase in the ICER of USD 7.8 per child. Importantly, the ICER difference between CMA alone and CMA + WES will close if there is a reduction in WES costs of a minimum of 25% (to USD 1600) or a 30% increase in the WES yield (to 20%). Importantly, we note that this is, in fact, the current situation in the Bedouin population, for which the WES diagnostic yield is 27.6%. An additional reduction in WES costs or an increase in yield will make WES alone the most cost-effective genetic test for ASD. In such a scenario, we should perhaps consider making WES the first-choice genetic test for children diagnosed with ASD and add a CMA analysis only for children with negative WES findings.
An important aspect that should be considered in the evaluation of the cost effectiveness of WES for children with ASD is the reduction in lifelong financial burden resulting from positive findings in such a genetic test. In this realm, it is reasonable to assume that genetic tests will facilitate earlier and more robust ASD diagnosis, which will, in turn, lead to better intervention outcomes that will improve the child’s chances to join the workforce. As an adult, that child, diagnosed early with ASD, would be able to support him/herself partially or completely [59], thereby saving future costs, both for the family and for the health system. Nevertheless, an assessment of the financial benefit associated with such a genetic diagnosis is extremely complicated and is beyond the scope of this study.
4.4. Additional Implications of Whole-Exome Sequencing for Children with ASD
The results of postnatal WES analysis may have additional, non-financial implications for the families of children with ASD. The identification of an ASD susceptibility genetic variant in an affected child may help the parents in their future family planning. This, in fact, has been noted as the main factor for families to conduct such postnatal genetic tests [60]. The WES results may also help to better understand the molecular mechanism underlying ASD in affected children and consequently help guide precision medicine for these children [61]. Nevertheless, using WES as a diagnostic tool for ASD may also have some limitations that should be considered. The major limitation of this approach is its current low diagnostic yield. This means that many families will receive null results that might be false negative. Furthermore, despite the use of stringent criteria for the identification of ASD susceptibility variants in WES analysis, a positive WES finding could still be a false positive. Thus, performing an additional validation of WES-positive findings is highly recommended. Altogether, all these financial and non-financial implications should be considered and better communicated to families of children with ASD.
5. Conclusions
Our findings suggest that WES is a relevant and important method for identifying the possible genetic cause in >15% of children with ASD, and its diagnostic yield is expected to increase in the close future as more genes associated with ASD are identified. The indispensable clinical and financial benefits of such genetic findings, together with the predicted reduction in the ICER of this test in the next few years, would support a recommendation for wider utilization of this approach for clinical purposes in Israel and elsewhere.
Acknowledgments
We thank the families who participated in this research, without whose contributions genetic studies would be impossible. We thank Inez Mureinik for critical reviewing and editing of the manuscript.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/genes13010036/s1: Table S1: SFARI gene panel; Table S2: cost items; Table S3: list of identified ASD candidate variants.
Author Contributions
Conceptualization, R.T.-B.I., N.D. and I.M.; methodology, N.S., H.A.-K.; software, A.S.; validation, R.T.-B.I., A.S. and I.M.; formal analysis, R.T.-B.I. and A.S.; resources, G.M., H.F., A.M., I.D. and H.G.; data curation, R.T.-B.I. and A.S.; writing—original draft preparation, R.T.-B.I.; writing—review and editing, S.S.; supervision, N.D. and I.M.; project administration, I.M.; funding acquisition, I.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by The Israel Science Foundation, grant number 527/15.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Soroka University Medical Center (SOR-076-15; 17 April 2016).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
WES data were generated as part of the ASC and are available in dbGaP with study accession: phs000298.v4.p3.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sharma S.R., Gonda X., Tarazi F.I. Autism Spectrum Disorder: Classification, diagnosis and therapy. Pharmacol. Ther. 2018;190:91–104. doi: 10.1016/j.pharmthera.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Muhle R., Trentacoste S.V., Rapin I. The Genetics of Autism. Pediatrics. 2004;113:472–486. doi: 10.1542/peds.113.5.e472. [DOI] [PubMed] [Google Scholar]
- 3.Hansen S.N., Schendel D.E., Francis R.W., Windham G.C., Bresnahan M., Levine S.Z., Reichenberg A., Gissler M., Kodesh A., Bai D., et al. Recurrence Risk of Autism in Siblings and Cousins: A Multinational, Population-Based Study. J. Am. Acad. Child Adolesc. Psychiatry. 2019;58:866–875. doi: 10.1016/j.jaac.2018.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conti S.L., Eisenberg M.L. Paternal aging and increased risk of congenital disease, psychiatric disorders, and cancer. Asian J. Androl. 2016;18:420–424. doi: 10.4103/1008-682X.175097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller D.T., Adam M.P., Aradhya S., Biesecker L.G., Brothman A.R., Carter N.P., Church D.M., Crolla J.A., Eichler E.E., Epstein C.J., et al. Consensus Statement: Chromosomal Microarray Is a First-Tier Clinical Diagnostic Test for Individuals with Developmental Disabilities or Congenital Anomalies. Am. J. Hum. Genet. 2010;86:749–764. doi: 10.1016/j.ajhg.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu X.-Y., Phung M.T., Shaw C.A., Pham K., Neil S.E., Patel A., Sahoo T., Bacino C.A., Stankiewicz P., Kang S.-H.L., et al. Genomic Imbalances in Neonates With Birth Defects: High Detection Rates by Using Chromosomal Microarray Analysis. Pediatrics. 2008;122:1310–1318. doi: 10.1542/peds.2008-0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bai D., Yip B.H.K., Windham G.C., Sourander A., Francis R., Yoffe R., Glasson E., Mahjani B., Suominen A., Leonard H., et al. Association of Genetic and Environmental Factors With Autism in a 5-Country Cohort. JAMA Psychiatry. 2019;76:1035–1043. doi: 10.1001/jamapsychiatry.2019.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Devlin B., Scherer S.W. Genetic architecture in autism spectrum disorder. Curr. Opin. Genet. Dev. 2012;22:229–237. doi: 10.1016/j.gde.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Girirajan S., Dennis M.Y., Baker C., Malig M., Coe B.P., Campbell C.D., Mark K., Vu T.H., Alkan C., Cheng Z., et al. Refinement and Discovery of New Hotspots of Copy-Number Variation Associated with Autism Spectrum Disorder. Am. J. Hum. Genet. 2013;92:221–237. doi: 10.1016/j.ajhg.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sebat J., Lakshmi B., Malhotra D., Troge J., Lese-Martin C., Walsh T., Yamrom B., Yoon S., Krasnitz A., Kendall J., et al. Strong Association of De Novo Copy Number Mutations with Autism. Science. 2007;316:445–449. doi: 10.1126/science.1138659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vicari S., Napoli E., Cordeddu V., Menghini D., Alesi V., Loddo S., Novelli A., Tartaglia M. Copy number variants in autism spectrum disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2019;92:421–427. doi: 10.1016/j.pnpbp.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 12.Woodbury-Smith M., Zarrei M., Wei J., Thiruvahindrapuram B., O’Connor I., Paterson A.D., Yuen R.K.C., Dastan J., Stavropoulos D.J., Howe J.L., et al. Segregating patterns of copy number variations in extended autism spectrum disorder (ASD) pedigrees. Am. J. Med Genet. B Neuropsychiatr. Genet. 2020;183:268–276. doi: 10.1002/ajmg.b.32785. [DOI] [PubMed] [Google Scholar]
- 13.Kanduri C., Kantojärvi K., Salo P.M., Vanhala R., Buck G., Blancher C., Lähdesmäki H., Järvelä I. The landscape of copy number variations in Finnish families with autism spectrum disorders. Autism Res. 2015;9:9–16. doi: 10.1002/aur.1502. [DOI] [PubMed] [Google Scholar]
- 14.Shendure J., Fisher S., Bernier R., Nickerson D., Rieder M., Baker C., Ng S., Mackenzie A., Karakoc E., Girirajan S., et al. Exome sequencing in sporadic autism spectrum disorders identifies severe de novo mutations. Nat. Genet. 2011;43:585. doi: 10.1038/ng.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grove J., Ripke S., Als T.D., Mattheisen M., Walters R.K., Won H., Pallesen J., Agerbo E., Andreassen O.A., Anney R., et al. Identification of common genetic risk variants for autism spectrum disorder. Nat. Genet. 2019;51:431–444. doi: 10.1038/s41588-019-0344-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuen R.K.C., Merico D., Bookman M., Howe J.L., Thiruvahindrapuram B., Patel R.V., Whitney J., Deflaux N., Bingham J., Wang Z., et al. Whole genome sequencing resource identifies 18 new candidate genes for autism spectrum disorder. Nat. Neurosci. 2017;20:602–611. doi: 10.1038/nn.4524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geschwind D.H. Genetics of autism spectrum disorders. Trends Cogn. Sci. 2011;15:409–416. doi: 10.1016/j.tics.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rylaarsdam L.E., Guemez-Gamboa A. Genetic Causes and Modifiers of Autism Spectrum Disorder. Front. Cell. Neurosci. 2019;13:385. doi: 10.3389/fncel.2019.00385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiśniowiecka-Kowalnik B., Nowakowska B.A. Genetics and epigenetics of autism spectrum disorder—current evidence in the field. J. Appl. Genet. 2019;60:37–47. doi: 10.1007/s13353-018-00480-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woodbury-Smith M., Scherer S.W. Progress in the genetics of autism spectrum disorder. Dev. Med. Child Neurol. 2018;60:445–451. doi: 10.1111/dmcn.13717. [DOI] [PubMed] [Google Scholar]
- 21.Jeste S.S., Geschwind D.H. Disentangling the heterogeneity of autism spectrum disorder through genetic findings. Nat. Rev. Neurol. 2014;10:74–81. doi: 10.1038/nrneurol.2013.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wallace S.E., Bean L.J.H. Educational Materials—Genetic Testing: Current Approaches. University of Washington; Seattle, WA, USA: 2018. [Google Scholar]
- 23.Arteche-López A., Gómez Rodríguez M.J., Sánchez Calvin M.T., Quesada-Espinosa J.F., Lezana Rosales J.M., Palma Milla C., Gómez-Manjón I., Hidalgo Mayoral I., Pérez de la Fuente R., Díaz de Bustamante A., et al. Towards a Change in the Diagnostic Algorithm of Autism Spectrum Disorders: Evidence Supporting Whole Exome Sequencing as a First-Tier Test. Genes. 2021;12:560. doi: 10.3390/genes12040560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Israel Ministry of Health Circular letter: Autism Spectrum Disorder Diagnosis. [(accessed on 14 September 2021)];2013 Available online: https://www.health.govt.nz/publication/health-and-independence-report-2013.
- 25.Israel Ministry of Health Circular Letter: Genetic Tests Including Next Generation Sequencing. [(accessed on 14 September 2021)];2018 Available online: https://www.health.gov.il/English/Topics/Genetics/checks/Pages/exome.aspx.
- 26.Cappe E., Poirier N., Sankey C., Belzil A., Dionne C. Quality of life of French Canadian parents raising a child with autism spectrum disorder and effects of psychosocial factors. Qual. Life Res. 2017;27:955–967. doi: 10.1007/s11136-017-1757-4. [DOI] [PubMed] [Google Scholar]
- 27.van Tongerloo M.A.M.M.P., van Wijngaarden J.M., van der Gaag R.J., Lagro-Janssen A.L.M. Raising a child with an Autism Spectrum Disorder: ‘If this were a partner relationship, I would have quit ages ago. Fam. Pract. 2015;32:88–93. doi: 10.1093/fampra/cmu076. [DOI] [PubMed] [Google Scholar]
- 28.Dieleman L.M., Moyson T., De Pauw S.S., Prinzie P., Soenens B. Parents’ Need-related Experiences and Behaviors When Raising a Child With Autism Spectrum Disorder. J. Pediatr. Nurs. 2018;42:e26–e37. doi: 10.1016/j.pedn.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 29.Horlin C., Falkmer M., Parsons R., Albrecht M., Falkmer T. The Cost of Autism Spectrum Disorders. PLoS ONE. 2014;9:e106552. doi: 10.1371/journal.pone.0106552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buescher A.V.S., Cidav Z., Knapp M., Mandell D.S. Costs of Autism Spectrum Disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168:721–728. doi: 10.1001/jamapediatrics.2014.210. [DOI] [PubMed] [Google Scholar]
- 31.National Insurance Institute of Israel ASD—Autistic Spectrum Disorder—Eligibility (Based on Disabilities and Medical Conditions) [Hebrew] [(accessed on 6 July 2019)];2019 Available online: https://www.btl.gov.il/benefits/Disabled_Child/likuilist/Pages/autism.aspx.
- 32.ALUT—The Israeli Society for Children and Adults with Autism, General Disability Allowance. 2021. [(accessed on 6 November 2021)]. Available online: https://alut.org.il/?page_id=322.
- 33.ALUT—The Israeli Society for Children and Adults with Autism, Special Services Allowance. 2021. [(accessed on 6 November 2021)]. Available online: https://alut.org.il/?page_id=324.
- 34.WHO . Cost-Effectiveness Analysis for Health Interventions. World Health Organization; Geneva, Switzerland: 2010. [(accessed on 14 September 2021)]. p. 1. Available online: https://www.who.int/heli/economics/costeffanalysis/en/ [Google Scholar]
- 35.Yuen T., Carter M.T., Szatmari P., and Ungar W.J. Cost-effectiveness of Genome and Exome Sequencing in Children Di-agnosed with Autism Spectrum Disorder. Appl. Health Econ. Health Policy. 2018;16:481–493. doi: 10.1007/s40258-018-0390-x. [DOI] [PubMed] [Google Scholar]
- 36.Meiri G., Dinstein I., Michaelowski A., Flusser H., Ilan M., Faroy M., Bar-Sinai A., Manelis L., Stolowicz D., Yosef L.L., et al. Brief Report: The Negev Hospital-University-Based (HUB) Autism Database. J. Autism Dev. Disord. 2017;47:2918–2926. doi: 10.1007/s10803-017-3207-0. [DOI] [PubMed] [Google Scholar]
- 37.Dinstein I., Arazi A., Golan H.M., Koller J., Elliott E., Gozes I., Shulman C., Shifman S., Raz R., Davidovitch N., et al. The National Autism Database of Israel: A Resource for Studying Autism Risk Factors, Biomarkers, Outcome Measures, and Treatment Efficacy. J. Mol. Neurosci. 2020;70:1303–1312. doi: 10.1007/s12031-020-01671-z. [DOI] [PubMed] [Google Scholar]
- 38.Buxbaum J.D., Daly M.J., Devlin B., Lehner T., Roeder K., State M.W., Autism Sequencing Consortium NeuroView The Autism Sequencing Consortium: Large-Scale, High-Throughput Sequencing in Autism Spectrum Disorders. Neuron. 2012;76:1052–1056. doi: 10.1016/j.neuron.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abrahams B.S., Arking D.E., Campbell D.B., Mefford H.C., Morrow E.M., Weiss L.A., Menashe I., Wadkins T., Banerjee-Basu S., Packer A. SFARI Gene 2.0: A community-driven knowledgebase for the autism spectrum disorders (ASDs) Mol. Autism. 2013;4:36. doi: 10.1186/2040-2392-4-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McKenna A., Hanna M., Banks E., Sivachenko A., Cibulskis K., Kernytsky A., Garimella K., Altshuler D., Gabriel S., Daly M., et al. The Genome Analysis Toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20:1297–1303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McLaren W., Gil L., Hunt S.E., Riat H.S., Ritchie G.R.S., Thormann A., Flicek P., Cunningham F. The Ensembl Variant Effect Predictor. Genome Biol. 2016;17:1–14. doi: 10.1186/s13059-016-0974-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ng P.C., Henikoff S. SIFT: Predicting amino acid changes that affect protein function. Nucleic Acids Res. 2003;31:3812–3814. doi: 10.1093/nar/gkg509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adzhubei I., Jordan D., Sunyaev S.R. Predicting Functional Effect of Human Missense Mutations Using PolyPhen-2. Curr. Protoc. Hum. Genet. 2013;76:7.20.1–7.20.41. doi: 10.1002/0471142905.hg0720s76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robinson J.T., Thorvaldsdóttir H., Winckler W., Guttman M., Lander E.S., Getz G., Mesirov J.P. Integrative genomics viewer. Nat. Biotechnol. 2011;29:24–26. doi: 10.1038/nbt.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bambha K., Kim W.R. Cost-effectiveness analysis and incremental cost-effectiveness ratios: Uses and pitfalls. Eur. J. Gastroenterol. Hepatol. 2004;16:519–526. doi: 10.1097/00042737-200406000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Barzilai University Medical Center Common Services and Codes Price List. [(accessed on 23 March 2020)];2019 Available online: http://www.bmc.gov.il/?CategoryID=859&ArticleID=3665.
- 47.Hadassah University Medical Center Hadassah Medical Center Exome Sequencing Lab. [(accessed on 14 September 2021)]. Available online: https://www.hadassah.org.il/en/exome_sequencing_lab/
- 48.The National Insurance Property Development Company Limited, Ministry of Health Pharmaceutical Price List. [(accessed on 14 September 2021)];2021 Available online: https://nipdec.com/pharmaceutical/
- 49.National Insurance Institute of Israel Average Wages According to Sections 1 and 2 of the National Insurance Law. [(accessed on 23 March 2020)]; Available online: https://www.btl.gov.il/Mediniyut/GeneralData/Pages/%D7%A9%D7%9B%D7%A8%20%D7%9E%D7%9E%D7%95%D7%A6%D7%A2.aspx.
- 50.Clark M.M., Stark Z., Farnaes L., Tan T.Y., White S.M., Dimmock D., Kingsmore S.F. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. NPJ Genom. Med. 2018;3:16. doi: 10.1038/s41525-018-0053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Richards S., Aziz N., Bale S., Bick D., Das S., Gastier-Foster J., Grody W.W., Hegde M., Lyon E., Spector E., et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bahcall O.G. Genetic testing: ACMG guides on the interpretation of sequence variants. Nat. Rev. Genet. 2015;16:256–257. doi: 10.1038/nrg3940. [DOI] [PubMed] [Google Scholar]
- 53.DiCicco-Bloom E., Lord C., Zwaigenbaum L., Courchesne E., Dager S.R., Schmitz C., Schultz R.T., Crawley J., Young L.J. The Developmental Neurobiology of Autism Spectrum Disorder. J. Neurosci. 2006;26:6897–6906. doi: 10.1523/JNEUROSCI.1712-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zlotogora J. Genetics and genomic medicine in Israel. Mol. Genet. Genom. Med. 2014;2:85–94. doi: 10.1002/mgg3.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.The Knesset Bedouins in the State of Israel. [(accessed on 14 October 2020)]; Available online: https://www.knesset.gov.il/lexicon/eng/bedouim_eng.htm.
- 56.Na’Amnih W., Romano-Zelekha O., Kabaha A., Rubin L.P., Bilenko N., Jaber L., Honovich M., Shohat T. Prevalence of consanguineous marriages and associated factors among Israeli Bedouins. J. Community Genet. 2014;5:395–398. doi: 10.1007/s12687-014-0188-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Levaot Y., Meiri G., Dinstein I., Menashe I., Shoham-Vardi I. Autism Prevalence and Severity in Bedouin-Arab and Jewish Communities in Southern Israel. Community Ment. Heal. J. 2018;55:156–160. doi: 10.1007/s10597-018-0236-x. [DOI] [PubMed] [Google Scholar]
- 58.Kerub O., Haas E.J., Meiri G., Bilenko N., Flusser H., Michaelovski A., Dinstein I., Davidovitch N., Menashe I. Ethnic Disparities in the Diagnosis of Autism in Southern Israel. Autism Res. 2020;14:193–201. doi: 10.1002/aur.2421. [DOI] [PubMed] [Google Scholar]
- 59.Zaresani A., Emery H., Dutton D. Why Adults with Autism Spectrum Disorder Have Lower Labor Supply than the Other Disability Groups? 2018. [(accessed on 14 September 2021)]. Available online: https://azaresani.com/wp-content/uploads/Autism-and-labor.pdf.
- 60.Hendel Y., Meiri G., Flusser H., Michaelovski A., Dinstein I., Menashe I. Factors Affecting Family Compliance with Genetic Testing of Children Diagnosed with Autism Spectrum Disorder. J. Autism Dev. Disord. 2021;51:1201–1209. doi: 10.1007/s10803-020-04589-y. [DOI] [PubMed] [Google Scholar]
- 61.Kostic A., Buxbaum J.D. The promise of precision medicine in autism. Neuron. 2021;109:2212–2215. doi: 10.1016/j.neuron.2021.06.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
WES data were generated as part of the ASC and are available in dbGaP with study accession: phs000298.v4.p3.