Abstract
Objective
The present study investigates the COVID-19 survivors' perspective on speech, swallowing, and hearing-related issues post-COVID-19. We further investigate the recovery duration for speech, swallowing, and hearing-related symptoms post-COVID.
Design
Survey study; E-survey.
Methodology
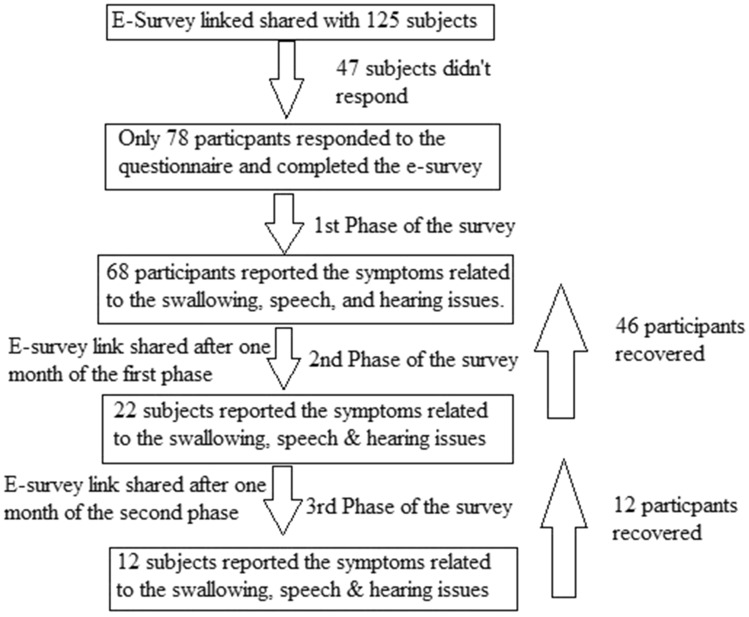
A total of 78 subjects (35.78 years ± 11.93) participated in the survey. All the participants were diagnosed with the RTPCR method. To understand the recovery duration for the speech, swallowing and hearing issues post-COVID-19, we conducted a three-phase study.
Results
In the first phase of the survey, 68 subjects reported symptoms related to speech, swallowing, and hearing issues 15 days of post-COVID recovery. A total of 76.4% of subjects reported only swallowing-related issues, 4.41% only speech-related issues, whereas 1.47% reported the problem in speech and hearing functions. The 2nd phase of the study was conducted after the first phase of the study. Only 22 subjects reported the presence of swallowing, speech and hearing-related issues from the 68 subjects. During the last phase, only 12 subjects reported speech, swallowing, and hearing issues. All subjects recovered from the olfaction and gustation impairment, whereas 50% of subjects reported the presence of xerostomia.
Conclusion
From the present study, we conclude that the SARC-CoV-2 virus directly affects the respiratory system and affects the aero-digestive system and laryngeal system physiology. Individuals with comorbid conditions admitted in ICU during COVID-19 treatment and prolonged hospital stay were at higher risk of developing speech, swallowing, and hearing-related issues post-COVID-19. The present study indicated that all COVID-19 survivors should be screened for speech, swallowing, and hearing-related issues for early rehabilitation if needed.
Keywords: COVID-19, Dysphagia, Xerostomia, Hearing loss, Tinnitus, Vocal fatigue
Introduction
On March 11, 2020, World Health Organization (WHO) declared COVID-19 disease a pandemic condition spared by the SARS-CoV-2 virus. As per the WHO [27] report worldwide, there are 126,359,540 confirmed cases of COVID-19 and more than 2,769,473 deaths. According to the Ministry of Health and Family Welfare [20] statistics, presently, India has 486,310 active patients, and a total of 11,323,762 patients recovered. This condition manifests with a diverse range of symptoms, including asymptomatic infection, severe viral pneumonia, respiratory failure, or death [12, 28]. Epidemiological studies [17, 21] reported the presence of dysphagia, dysphonia and hearing loss [1, 21] in some COVID-19 patients. Recent studies [4, 11, 24, 29] reported that post-COVID-19 patients might manifest the following symptoms, such as the risk of heart damage, lung infections, brain damage, dysphonia [2, 3], reduced hearing sensitivity, impaired swallowing [2], impaired olfaction and gustation [5, 22] and other physical and mental health [14, 15] issues.
Recently some follow-up studies were conducted post-COVID-19 and result indicated the presence of swallowing related issues [10, 13], voice changes [10, 13], moderate to severe anxiety [10, 13, 23], depression [10, 13, 19, 23], poor quality of life [13, 23], fatigue [10, 13, 19], cough [5, 6, 13, 19], shortness of breath [6, 8, 10, 19], taste and smell dysfunction [5, 8, 13], poor pulmonary strength [8, 13], Vertigo [5, 13] and disturbed sleep [8, 13]. To date, there are some published works related to the post-COVID-19 effect on speech, voice, swallowing, and hearing, but in our view, there is no study exploring the patient's perspective regarding the same. Therefore, the present study aims to explore the patient's perspective related to speech, swallowing, and hearing issues post-COVID-19 recovery. We further aim to explore how speech, swallowing, and hearing-related symptoms recover with the period.
Methodology
Participants
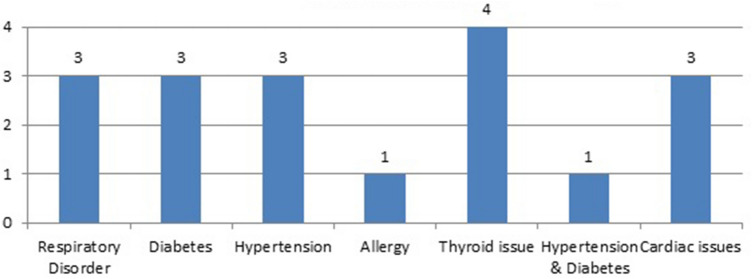
We e-mailed the questionnaire to 125 subjects diagnosed with COVID-19, and 78 responded to the questionnaire. All subjects were from the age range of 18–59 years (35.78 years ± 11.93). Among 78 subjects, 28 were females and 50 were males. All the subjects were diagnosed with COVID-19 using the RTPCR diagnosis method. Among 78 subjects, 19 were asymptomatic, whereas 59 were symptomatic. Among 78 subjects, 18 (23.08%) participants had comorbid conditions, as shown in Fig. 1. A total of 19 participants had a smoking habit (2.7 per/day ± 1.30), whereas 15 subjects were alcoholics.
Fig. 1.
Showing the comorbid condition in participants
Research design: Observational Study (survey design).
Formation of the Questionnaire
In the present study we didn’t use standardized and validated patient-reported outcome measures questionnaire or tool, such as Eating Assessment Tool (EAT-10), Dysphagia Handicap Index (DHI), Speech Handicap Index, and etc. as these tools are not available in the Hindi language. Therefore, the survey questionnaire developed in the Hindi language to explore the patient's perspective about speech, swallowing, and hearing status post-COVID-19 recovery. The questionnaire was divided into five sections. The first section included the demographic details, daily living, dietary, and tobacco consumption habits. The second section contained ten questions related to the COVID-19 diagnosis, symptoms, and other related information. The third section included the questions related to the swallowing, olfaction and gustation status post-COVID-19 recovery. The fourth section deal with the respiratory and speech outcomes post-COVID-19, whereas the fifth section included questions related to the hearing post-COVID-19. The two medical physicians working with COVID-19, one speech-swallowing pathologist, and one audiologist were asked to validate the questionnaire. The changes were made as per suggestions given by the professionals.
Procedure
Before collecting the data, participants were asked to fill the informed consent form. The study's objectives were explained to the participants, and an explanation was made to all the queries on the video call made by WhatsApp software. The study was conducted using online mode. The google questionnaire was formed, and the link was shared with the participants. The participants also asked to upload the softcopy of RTPCR report on the given google survey. The video call was made using WhatsApp, Google meet, or Zoom as per the comfort of participants, and they were instructed to fill the questionnaire during the video call session only. The study was conducted in three phases. In the first phase, the link was sent to the participants who got recovered from the COVID-19. The participants with a minimum of 15 days and a maximum of 20 day post-COVID-19 recovery period participated in the study. The second phase of the study was conducted after 1 month of the first phase. In the second phase, only those subjects participated who had any difficulty with speech, swallowing, and hearing. During this phase, subjects were asked to fill only the last three sections of the questionnaire. The last phase of the study was conducted post 1 month of the second phase. Subjects who showed impaired speech, swallowing, and hearing functions during the second phase of the study were included in the study's third phase.
Data analysis: We performed descriptive analysis using SPSS 20.00 version statistical software.
Results
First phase of the study
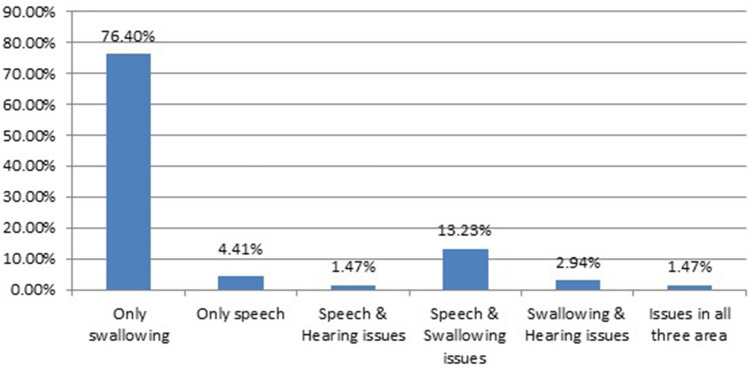
A total of 78 subjects filled the questionnaire, and 68 subjects reported symptoms related to speech, swallowing, and hearing issues 15 days of post-COVID recovery. A total of 9 (13.23%) subjects had issues related to speech and swallowing, whereas two (2.94%) subjects indicated a problem in swallowing and hearing. Only one (1.47%) participant reported issues in all three areas (i.e., swallowing, speech, and hearing). Fifty-two (76.4%) subjects reported only swallowing-related issues, three (4.41%) reported only speech, whereas one (1.47%) subject responded to the problem in speech and hearing functions, as shown in Fig. 2. The subject had issues in all three areas, reported the presence of comorbid conditions (i.e., diabetes, asthma, & hypertension) before the COVID-19, and had a more extended stay in the hospital due to low oxygen level. Only two subjects needed ICU facility due to low oxygen concentration in the blood.
Fig. 2.
Problems reported in different areas during first phase of the study
Swallowing, olfaction, and gustation related issues
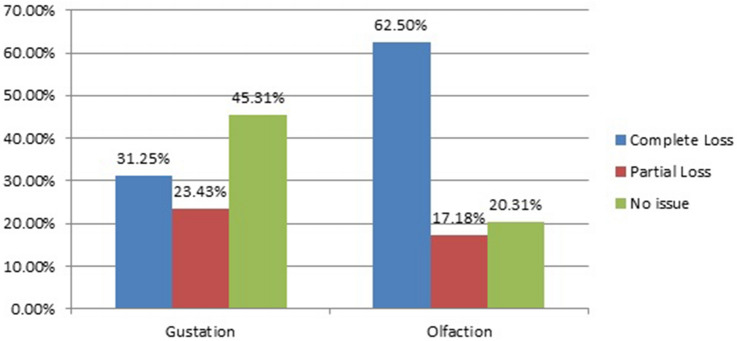
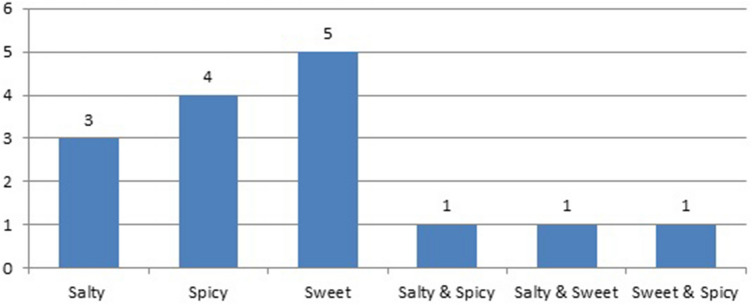
In the first phase, 64 subjects reported swallowing-related post-COVID symptoms. Among those, 23 (35.93%) were females, and 41 (64.06%) were males. A total of 16 participants (25%) from 64 had comorbid conditions before COVID-19 and were on medication for the same. Among 64 subjects, nine were asymptomatic, and 55 were symptomatic. A total of 20 (31.25%) reported the complete loss of taste, 15 (23.43%) reported partial, and the majority of the population (i.e., 29 subjects) had intact taste sensation after COVID-19, as shown in Fig. 3. The majority of participants (i.e., total 5) with partial taste sensation lost sweet sensation followed by spicy and salty taste sensation, as described in Fig. 4. A total of 40 (62.5%) participants said that they had complete loss of smell after COVID-19 recovery, whereas 13 (20.31%) subjects reported no loss of olfaction, as shown in Fig. 3.
Fig. 3.
Showing percentage of the population having an issue with gustation and olfaction sense
Fig. 4.
Loss of specific taste in partial loss
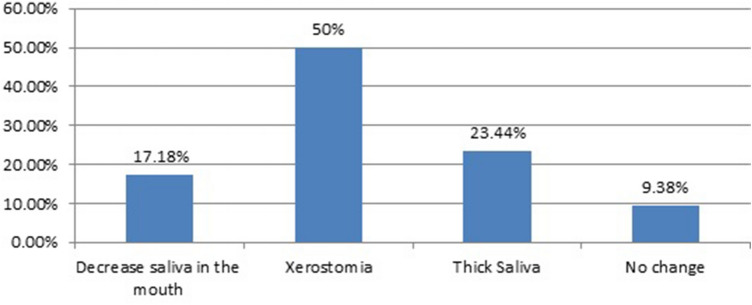
Only two individuals reported issues in tongue functions (i.e., tongue elevation & limited lateralization), which lead to difficulties in the utterance of some sounds (i.e., /r/, /ʧ/, /l/) and food manipulation in the oral stage of swallowing. A total of 49 subjects reported problems related to saliva post-COVID-19. The 11 subjects mentioned they had decreased amount of saliva in the mouth, 32 reported the presence of xerostomia, and 6 subjects reported thick saliva, as shown in Fig. 5. A total of 8 participants indicated that they had pain while swallowing. Many participants (i.e., 18 participants) reported that it took a longer duration to complete the one meal, whereas no subject reported choking before or after the meal. Eight participants (12.5%) said that they could feel a foul smell in the mouth after COVID-19, and two subjects reported the spillage of food from the mouth occasionally. A total of 13 (20.31%) individuals said that they lost weight after COVID-19 (Max: 8 kg; Min: 2 kg).
Fig. 5.
Change in the saliva production post-COVID-19
Speech and respiration
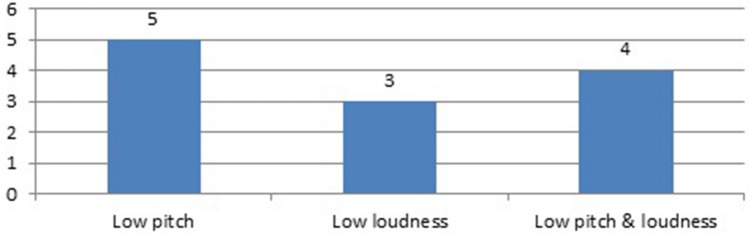
In this section, 13 (male: 7, female: 6) subjects reported speech & respiratory issues following the COVID-19 recovery. Among 13 subjects, 8 participants (61.54%) had comorbid conditions, and all subjects were symptomatic. A total of 12 subjects reported the change in the voice quality and loudness level, as shown in Fig. 6. One subject reported difficulty while speaking due to shortness of breath, whereas two subjects indicated a lump in the throat feeling. One subject reported tension around the neck muscle while speaking, and most of the population (53.85%) said they have vocal fatigue post-COVID-19. One subject was not able to utter /r/ and other palatal sounds adequately.
Fig. 6.
Change in voice quality and loudness post-COVID -19 in first phase of the survey
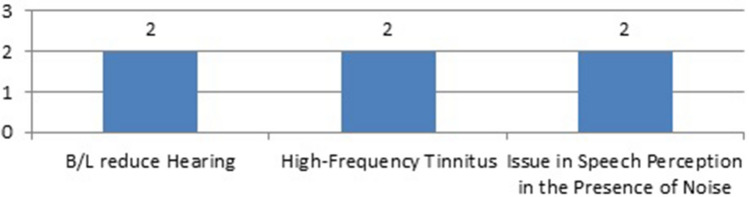
Hearing related issues
A total of four subjects indicated hearing-related issues post-COVID-19 in the first phase of the study. Among four subjects, 3 (75%) were males, and 1 (25%) were female. All participants had comorbid conditions prior to COVID-19 infection. As shown in Fig. 7, two subjects (50%) reported the reduced hearing sensitivity bilaterally, two subjects reported the presence of high-frequency tinnitus, and two subjects reported the speech perception issues in the presence of background noise. In the current survey, no subject reported the presence of vertigo post-COVID-19.
Fig. 7.
Presence of hearing related issues post-COVID-19
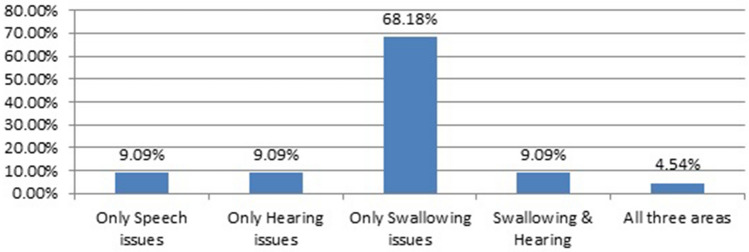
Second phase of the study
After 1 month of the first phase, we send the survey link to the participants who reported speech, swallowing, and hearing-related issues in the first phase of the study. Only 22 subjects reported swallowing, speech, and hearing-related issues from the 68 subjects during the second phase. A total of 9 females and 13 males responded to the survey. Most of the population (59.09%) had comorbid issues before the COVID-19. During the second phase, 2 (9.09%) subjects reported the presence of swallowing & hearing-related issues, 2 (9.09%) showed only speech-related symptoms, 2 (9.09%) only hearing-related concerns, and 15 (68.18%) subjects reported only swallowing-related issues. Only 1 (4.54%) subject showed issues in all three areas, as shown in Fig. 8.
Fig. 8.
Affected areas post-COVID-19 in the second phase of the study
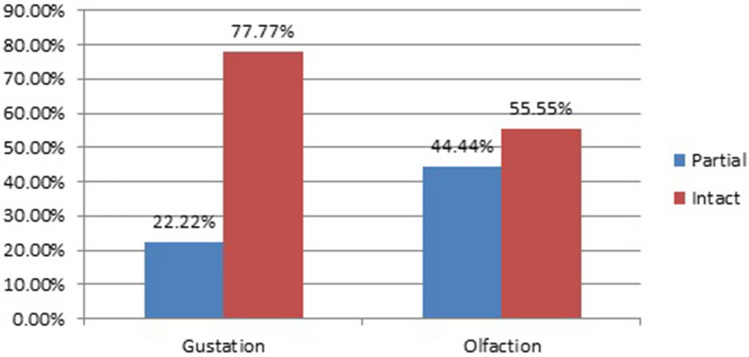
Swallowing, olfaction and gustation related issues
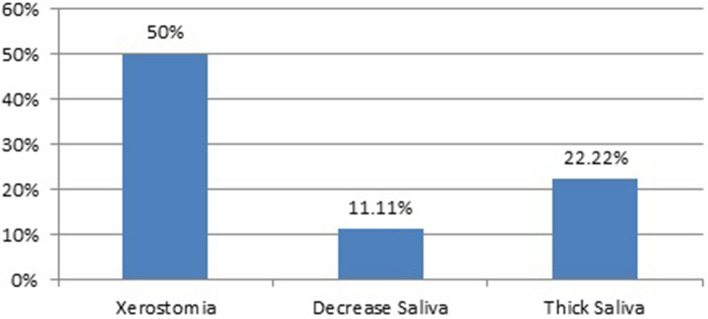
During the second phase, the symptoms related to swallowing disorders reduced, and only 18 subjects reported abnormal swallowing, olfaction and gustation-related symptoms. No one reported the complete loss of olfaction and gustation sensation during this phase, whereas 4 (22.22%) and 8 (44.44%) subjects reported the partial loss of the taste and smell, respectively, Fig. 9. Two subjects (11.11%) reported the limited elevation of the tongue, 2 (11.11%) reported the presence of foul smell in the mouth, and 3 (16.66%) reported the presence of pain while swallowing. The participants reported improvements in completing the meal, whereas three participants (16.66%) took more than 30 min to complete the meal. A total of 9 participants (50%) reported the presence of xerostomia, 2 (11.11%) decreased in the saliva, and four subjects (22.22%) reported the presence of thick saliva, as shown in Fig. 10.
Fig. 9.
Showing percentage of the population having an issue with gustation and olfaction sense during 2nd phase of the study
Fig. 10.
Change in saliva post-COVID-19 in the 2nd phase of the survey
Speech and respiration related
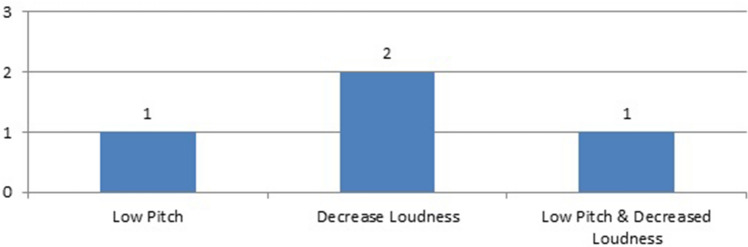
During the second phase of the survey, only five subjects reported speech and respiratory issues. None of them reported the presence of short breath and tension in the neck. However, change in the voice quality and loudness was reported by 4 subjects (80%), as shown in Fig. 11. The majority of the population (i.e., 4) reported the presence of vocal fatigue.
Fig. 11.
Change in the voice quality and loudness in the 2nd phase of the survey
Hearing-related concerns
One subject recovered from the reduced hearing sensitivity; however, 3 participants reported hearing-related issues. Only one subject reported bilaterally reduced hearing sensitivity, 2 (66.66%) had high-frequency tinnitus, and 2 (66.66%) had speech perception issues in the presence of background noise. The subject with bilaterally reduced hearing sensitivity had undergone for complete audiological test battery. The testing revealed mild to moderate high-frequency sensorineural hearing loss.
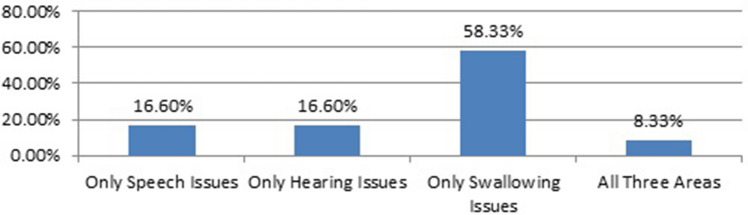
Third phase of the survey
In the third phase of the survey, only 12 participants reported f swallowing, speech, and hearing-related symptoms post-COVID-19 recovery. All the subjects had comorbid conditions prior to the COVID-19 infection and were on the medications for the same. As shown in Fig. 12, two subjects had only speech and respiration-related issues, seven subjects had only swallowing issues, and only one subject had an issue in all three areas.
Fig. 12.
Presence of difference symptoms post-COVID-19 in the 3rd phase of the survey
Swallowing, olfaction and gustation related issues
A total of 8 subjects reported the presence of swallowing issues. All subjects recovered from the olfaction and gustation issues, and only one subject reported the presence of a bad smell in the mouth. Tongue functions were improved; however, still, one subject had limited tongue elevation. Two subjects mentioned that they still take more than 30 min to finish the meal. A total of 4 (50%) subjects reported the presence of xerostomia, and one reported the presence of thick saliva.
Speech and respiration related issues
During this phase, only 3 subjects reported the presence of speech-related issues. All three subjects reported the presence of vocal fatigue, whereas only one subject reported lowered pitch voice quality.
Hearing related issues
Three subjects reported the presence of hearing-related concerns. Among 3 subjects, 2 participants (66.66%) reported the problem in speech perception in the presence of background noise, and 2 (66.66%) reported the presence of high-frequency tinnitus. One subject had bilateral reduce hearing sensitivity. Repeated audiological test battery approach revealed no change in the previous interpretation.
Discussion
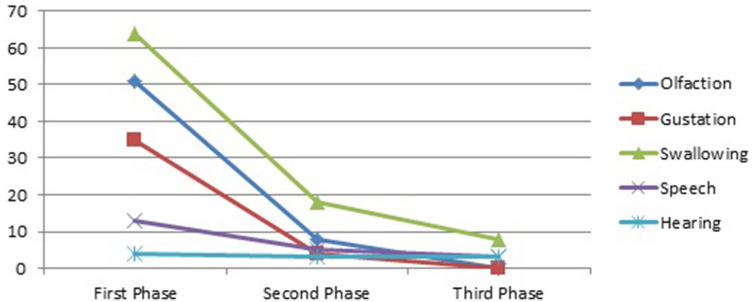
In the present study, we tried to explore the patient's perspective on swallowing, speech, and hearing issues post-COVID-19 recovery. We also looked into how speech, swallowing, and hearing-related symptoms recover with time, as demonstrated in Fig. 13.
Fig. 13.
Flowchart describing the three phase of the survey
The present survey revealed that most of the population reported speech, swallowing, and hearing-related issues post-COVID-19 recovery. Gradually 82.35% population recovered from these symptoms by the end of 3rd phase of the study. Leite et al. [18] conducted a similar line of study in the geriatric population diagnosed with COVID-19. They reported that most post-COVID-19 population referred to the speech-language pathologist for the rehabilitation related to swallowing and speech issues. Huang et al. [12] conducted the cohort 6-month follow-up study post-COVID-19 and their results were consistent with the present study. We can observe that individuals with speech, swallowing, and hearing-related issues following COVID-19 recovery in the 3rd phase had the presence of comorbid conditions. We could assume that individuals with comorbidities are at higher risk of a long-term effect of COVID-19 post-recovery. The same was discussed by Huang et al. [12], Carfi et al. [5], Raman et al. [23], and Mandal et al. [19]. The present study also reported that individual reported symptoms in all area (i.e., speech, swallowing, and hearing) were admitted in ICU and had a longer hospital stay. This statement is supported by Halpin et al. [10]. They reported that individuals with a more extended hospital stay and admitted to ICU during COVID-19 treatment took longer to recover and showed a diverse range of symptoms post-COVID-19 treatment.
In the present study, most of the population reported swallowing, olfaction, and gustation-related issues post-COVID-19 recovery, as shown in Fig. 14. These symptoms recovered with time (i.e., by the second phase, only some subjects reported the partial loss of gustation & olfaction). By the last phase of the study, all patients recovered from the olfaction and gustation issues. The study conducted by Carfi et al. [5] and Ninchritz-Becerra et al. [22] also reported the presence of impaired olfaction and gustation sensation post-COVID-19 for a short duration. Whereas Carfi et al. [5] also reported that some patients may have impaired olfaction and gustation for a longer duration and may need rehabilitation for the same. During the 3rd phase of the study, some patients reported xerostomia and thick saliva, which may interfere with the swallowing physiology and same was also reported by Wiertz et al. [26].
Fig. 14.
Change in the swallowing, olfaction, gustation, speech and hearing-related issues with the time
The result further indicated the presence of speech and respiratory-related issues post-COVID-19, and a majority of subjects recovered by the third phase of the survey. During the third phase of the survey, only 3 subjects reported voice-related issues, as shown in Fig. 14. During the first phase of the survey, 13 subjects reported speech and respiratory-related issues. From the literature, we know that the SARS-CoV-2 virus directly attacks the respiratory system [28], and due to that, the aero-digestive and laryngeal systems may get affected. This could result in impaired swallowing and laryngeal functions. Recent studies [2, 3, 10, 12, 17, 19] related to speech and swallowing impairment post-COVID-19 also found the similar results.
Many studies [1, 12, 21] reported the presence of sensorineural hearing loss, vertigo, tinnitus, and other hearing-related issues post-COVID-19. However, in the present study, only 4 subjects reported hearing-related issues. Till the 3rd phase of the study, only one subject reported improved hearing, whereas the other 3 had persistent hearing-related issues. Common symptoms were high-frequency tinnitus, speech perception issues in the presence of noise, and reduce hearing sensitivity. From this, we could hypothesize that the SARC-CoV-2 virus may directly affect the cochlear function or indirectly by eliciting inflammatory responses [7]. Last year Frazier [9] indicated the presence of SARC-CoV-2 virus in the mastoid and middle ear and isolated the virus while performing surgery from the mastoid tissue and within the middle ear. In the present study, we observed that 2 subjects had speech perception issues in noise, which may indicate that SARC-CoV-2 affects the central auditory system functioning. Few studies [16, 25] reported the impaired vestibulocochlear system due to the SARC-CoV-2 virus, and the symptoms related to the same reported were disequilibrium, tinnitus, and sudden hearing loss.
In the present study, we didn’t use standardized and validated patient-reported outcome measures questionnaire due to the unavailability of tools in the Hindi language this could be consider as one of the limitation of the present study. The swallowing, speech, and hearing function were not evaluated by professional health professionals so; results heavily rely on patients’ self-reporting without subjective measurements. This could be considered as second limitation of the present study.
Conclusion
From the present study, we can conclude that COVID-19 survivors suffered from many issues that may affect daily activities. Hence, affect the quality of life. However, most subjects recovered from those impairments, but some survivors may need rehabilitation post-COVID-19. The SARC-CoV-2 virus directly affects the respiratory system and hence affects the physiology of aero-digestive system and laryngeal system. Individuals with comorbid conditions admitted in ICU during COVID-19 treatment and prolonged hospital stay were at higher risk to develop speech, swallowing, and hearing-related issues post-COVID-19. We know that questionnaires is not a “gold standard” to be used alone as tool to evaluate the impact of COVID-19 on speech, swallowing, and hearing. Therefore, other types of objective assessments, such as Video fluoroscopic Swallow Study (VFSS) and aerodynamic measurement of speech/voice, are necessary to use together to make any definite clinical conclusions. However, the result of the present study will help understand the post-COVID-19 effects from the patient's perspective. The present study indicated that all COVID-19 survivors should be screened for speech, swallowing, and hearing-related issues for early rehabilitation if needed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alves de Sousa F, Pinto-Costa R, Xara S, Nobrega-Pinto A, Almeida e Sousa C. SARS-CoV-2 and hearing: an audiometric analysis of COVID-19 hospitalized patients. J Otol. 2021 doi: 10.1016/j.joto.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Archer KS, Iezzi CM, Gilpin L. Swallowing and voice outcomes in patients hospitalized with COVID-19: an observational cohort study. Arch Phys Med Rehabil. 2021 doi: 10.1016/j.apmr.2021.01.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balakrishnan K, Brenner JM, Hillel AT. Laryngeal and tracheal pressure injuries in patients with COVID-19. JAMA-Otolaryngol Head-Neck Surg. 2021;147(5):484–485. doi: 10.1001/jamaoto.2021.0001. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky MB, Gilbert RJ. The long-term effects of COVID-19 on dysphagia evaluation and treatment. Arch Phys Med Rehabil. 2020;101(9):1662–1664. doi: 10.1016/j.apmr.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. J Am Med Assoc. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chopra V, Flanders SA, O'Malley M, Malani AN, Prescott HC. Sixty-day outcomes among patients hospitalized with COVID-19. Ann Intern Med. 2021;174(4):576–578. doi: 10.7326/M20-5661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen BE, Durstenfeld A, Roehm PC. Viral causes of hearing loss: a review for hearing health professionals. Trends Hear. 2014;18:1–17. doi: 10.1177/2331216514541361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curci C, Pisano F, Bonacci E, Camozzi DM, Ceravolo C, Bergonzi R, De Franceschi S, Moro P, Guarnieri R, Ferrillo M, Negrini F, De Sire A. Early rehabilitation in post-acute COVID-19 patients: data from an Italian COVID-19 rehabilitation unit and proposal of a treatment protocol. A cross-sectional study. Eur J Phys Rehabilit Med. 2020;56(5):633–641. doi: 10.23736/S1973-9087.20.06339-X. [DOI] [PubMed] [Google Scholar]
- 9.Frazier KM, Hooper JE, Mostafa HH, Stewart CM. SARS-CoV-2 virus isolated from the mastoid and middle ear: implications for COVID-19 precautions during ear surgery. JAMA-Otolaryngol Head-Neck Surg. 2020;146:964–966. doi: 10.1001/jamaoto.2020.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, Walshwa C, Kemp S, Corrado J, Singh R, Collins T, O’Connor RJ, Sivan M. Post-discharge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. 2020;93(2):1013–1022. doi: 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
- 11.Helding L, Carroll TL, Nix J, Johns MM, LeBorgne WD, Meyer D. COVID-19 after effects: concerns for singers. J Voice. 2020;20:30281–30282. doi: 10.1016/j.jvoice.2020.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J, Huang Z, Tu S, Zhao Y, Chen L, Xu D, Li Y, Li C, Peng L, Cau B. A 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Javed B, Sarwer A, Soto EB, Mashwani ZU. The coronavirus (COVID-19) pandemic's impact on mental health. Int J Health Plan Manag. 2020;35(5):993–996. doi: 10.1002/hpm.3008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kathirvel N. Post COVID-19 pandemic mental health challenges. Asian J Psychiatr. 2020;53:102430. doi: 10.1016/j.ajp.2020.102430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koumpa FS, Forde CT, Manjaly JG. Sudden irreversible hearing loss post COVID-19. BMJ Case Rep. 2020;13:13–15. doi: 10.1136/bcr-2020-238419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lechien JR, Chiesa-Estomba CM, Place S, Van Laethem Y, Cabaraux P, Mat Q, Huet K, Plzak J, Horoi M, Hans S, Rosaria Barillari M, Commaroto G, Fakhry N, Martiny D, Ayad T, Jouffe L, Hopkins C, Saussez S. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020;288(3):335–344. doi: 10.1111/joim.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leite VF, Rampim DB, Conceicao Jorge V, Correia-de-Lima MC, Cezarino LG, Nunes-da-Rocha C, Esper RB. Persistent symptoms and disability after COVID-19 hospitalization: data from a comprehensive tele-rehabilitation program. Arch Phys Med Rehabilit. 2021 doi: 10.1016/j.apmr.2021.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, Heightman M, Hillman TE, Jacob J, Jarvis CH, Lipman MCI, Naidu SB, Nair A, Porter JC, Tomlinson GS, Hurst JR. 'Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. BMC Thorax. 2021;76:396–398. doi: 10.1136/thoraxjnl-2020-215818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ministry of Health and Family Welfare (2021). Information on COVID. http://www.mohfw.gov.in/.
- 21.Mustafa MWM. Audiological profile of asymptomatic COVID-19 PCR-positive cases. Am J Otolaryngol. 2020;41(3):102483. doi: 10.1016/j.amjoto.2020.102483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ninchritz-Becerra E, Soriano-Reixach MM, Mayo-Yánez M, Calvo-Henríquez C, Martínez-Ruiz de Apodaca P, Saga-Gutiérrez C, Parente-Arias P, Maria Villareal I, Viera-Artiles J, Poletti-Serafini D, Alobid I, Ayad T, Saussez S, Lechien JR, Chiesa-Estomba CM. Subjective evaluation of smell and taste dysfunction in patients with mild COVID-19 in Spain. Medicinia Clinica (Barc) 2021;156:61–64. doi: 10.1016/j.medcle.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raman B, Cassar MP, Tunnicliffe EM, Filippini N, Griffanti L, Alfaro-Almagro F, Okell T, Sheerin F, Xie C, Mahmod M, Mozes FE, Lewandowski AJ, Ohuma EO, Holdsworth D, Lamlum H, Woodman MJ, Krasopoulos C, Mills R, Kennedy McConnell FA, Neubauer S. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. E Clin Med. 2021;31:100683. doi: 10.1016/j.eclinm.2020.100683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trecca E, Gelardi M, Cassano M. COVID-19 and hearing difficulties. Am J Otolaryngol. 2020;41(4):102496. doi: 10.1016/j.amjoto.2020.102496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Viola P, Ralli M, Pisani D, Malanga D, Sculco D, Messina L, Laria C, Aragona T, Leopardi G, Ursini F, Scarpa A, Topazio D, Cama A, Vespertini V, Quintieri F, Cosco L, Maria Cunsolo E, Chiarella G. Tinnitus and equilibrium disorders in COVID-19 patients: preliminary results. Eur Arch Oto-Rhino-Laryngol. 2020 doi: 10.1007/s00405-020-06440-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wiertz CMH, Vints WAJ, Maas GJCM, Rasquin SMC, Horn YY, Dremmen MPM, Hemmen B, Verbunt JA. COVID-19: patient characteristics in the first phase of post-intensive care rehabilitation. Arch Phys Med Rehabil. 2021 doi: 10.1016/j.arrct.2021.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization (2021) COVID-19 dashboard. Retrieved from https://covid19.who.int/
- 28.World Health Organization (2021) Corona-virus disease (COVID-19) outbreak. Available from: https://www.who.int/
- 29.World Health Organization Europe (2021) New policy brief calls on decision-makers to support patients as 1 in 10 report symptoms of “long COVID”. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-COVID-19/news/news/2021/2/new-policy-brief-calls-on-decision-makers-to-support-patients-as-1-in-10-report-symptoms-of-long-covid#:~:text=Known%20manifestations%20of%20post%2D,%2C%20lungs%20and%20brain