Abstract
Purpose
Women are experiencing greater unemployment and increased stress from childcare responsibilities than men during the COVID-19 pandemic. Women with these experiences may be at particular risk for mental illness and increased substance use during the COVID-19 pandemic. The purpose of the study was to assess women's substance use, mental health, and experiences of COVID-19 pandemic impacts.
Methods
A national online survey was administered to adult women from September to November 2020. The survey included questionnaires assessing mental health, loneliness, intolerance for uncertainty, social support, substance use, and intimate partner violence (IPV).
Results
A total of 499 women responded; most were White, college educated, and in their mid-30s. Of the 20.24% who acknowledged at least one IPV problem, 29.7% stated that their IPV problems have gotten worse since the pandemic began, and 16.83% said that they have increased their drug or alcohol use to cope with their relationship problems. Anxiety, perceived daily impact of COVID-19, and lower self-efficacy were significant predictors of COVID-19 anxiety. Those with risky alcohol use had significantly higher anxiety (p = .028) and depression (p = .032) than those with low-risk alcohol use.
Conclusions
Greater anxiety about COVID-19, greater reported changes in daily life due to the pandemic, and high-risk alcohol use are related to greater mental health–related distress among women. For some, IPV has gotten worse during the pandemic and drug or alcohol use is a coping mechanism.
Depression, anxiety, and stress have been highly prevalent since the onset of the COVID-19 pandemic (Salari et al., 2020) and women in particular have faced unprecedented challenges (Lefkowitz & Armin, 2020; Malik & Naeem, 2020; Osland, Røysamb, & Nortvedt, 2020). Preliminary studies have shown that women faced greater stress and anxiety caused by the spread of COVID-19 and the subsequent social distancing policies (Conner et al., 2020). COVID-related psychological distress has been linked to increased alcohol consumption, and a stronger effect was noted for women (Rodriguez, Litt, & Stewart, 2020). Women have faced underemployment almost three times as much as men during COVID-19 (Golden & Kim, 2020), as well as more severe stress due to health and childcare issues (Conner et al., 2020). Childcare challenges have also been associated with using substances to cope with stress during the pandemic (MacMillan et al., 2021). Moreover, COVID-19 restricted women's access to resources for intimate partner violence (IPV) while it also escalated their risk for IPV victimization (Van Gelder et al., 2020). Moreover, these impacts on women are not only observed during the COVID pandemic, but also evidenced in pre-COVID research. In general, depression and anxiety disorders are more prevalent in women than in men globally (Albert, 2015; Pigott, 2003); women take much more of childcare responsibilities than men do even in dual-earner households (Yavorsky, Dush, & Schoppe-Sullivan, 2015); women are found to be more likely to be victimized and injured than men by IPV (Hamberger & Larsen, 2015); women suffer from higher risk of drug misuse (Lex, 1994); and women are more likely to misuse substances because of the interpersonal reasons (Kauffman, Silver, & Poulin, 1997; Tuchman, 2010).
However, few empirical studies have been conducted on women's daily pandemic-related psychosocial changes. Recent commentaries on the impact of the pandemic on mental health and substance use did not discuss how women may be differentially affected (Cullen, Gulati, & Kelly, 2020; Pfefferbaum & North, 2020; Zaami, Marinelli, & Varì, 2020; Zhou, Liu, Xue, Yang, & Tang, 2020). Therefore, the current study aimed to provide initial evidence of how the spread of COVID-19 and the resulting policy changes affect women's day-to-day life in terms of COVID-specific anxiety, depression, stress, loneliness, substance use, financial and employment loss, and IPV.
Methods
Participants and Procedures
Participants were nationally recruited online through Qualtrics panels as part of a larger longitudinal study. Qualtrics partners with panel companies that invite potential participants. When someone joins a panel company, they complete a profile, which includes demographic questions that allow for the determination of potential eligibility for studies. A random sample of those who are potentially eligible (older than 18 and live in the United States) receive an e-mail inviting them to learn more about the study and complete a screening survey to determine eligibility. The screening questionnaire for the current study included a brief description of the study and asked for initial interest in participating before asking screening questions. These questions included whether they were older than 18, if they use Facebook, and if they have a smartphone. Although the data are not described in the current study, participants were asked to share their Facebook data and meet a minimum threshold of 500 words and at least five posts to participate in the larger study. Eligible participants were then forwarded to the survey starting with the consent form. The consent form included a description of the study and expectations for participation. Participants were considered “consented” after they read the consent form and answered that they were interested in participating in the study. Participants responded to a series of questionnaires that addressed demographics, experiences during the COVID-19 pandemic, drug use, mental health, and IPV. Only questions relating to the current study and respondents who indicated that they were women are included here. Responses were collected from September 30 to November 18, 2020. This study was considered exempt by the University of Pennsylvania's institutional review board.
Measures
Mental health, substance use, and other non-COVID-19 specific measures
A number of previously validated questionnaires were used, including the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001), Generalized Anxiety Disorder 7 (GAD-7; Spitzer, Kroenke, Williams, & Löwe, 2006), General Self-Efficacy Scale (Chen, Gully, & Eden, 2001), Three-Item Loneliness Scale (Hughes, Waite, Hawkley, & Cacioppo, 2004), Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983), Intolerance for Uncertainty Scale (IUS-12; Carleton, Norton, & Asmundson, 2007), Perceived Social Support Questionnaire (Kliem et al., 2015), National Institute on Drug Abuse–modified Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST; WHO ASSIST Working Group, 2002), and the Alcohol Use Disorders Identification Test (AUDIT-C; Bradley et al., 2003). IPV was also assessed by adapting screener questionnaires from Heron, Thompson, Jackson, and Kaslow (2003) and Feldhaus, Koziol-McLain, Amsbury, Lowenstein, and Abbott (1997). These items have been used successfully in previous online studies (Elphinstone, 2018; Groarke, Berry, Graham-Wisener, McKenna-Plumley, McGlinchey, & Armour, 2020; Krusche, Cyhlarova, & Williams, 2013; Parlapani et al., 2020; Phelps, Paniagua, Willcockson, & Potter, 2018; Russel & Barry, 2021; Wilde & Hsu, 2019).
Demographics and COVID-19–specific measures
Standard items were used to gather demographic information. To assess the severity of the impact of COVID-19 on daily life, the question “How much does COVID-19 (coronavirus) impact your day-to-day life” was used (Harkness Behar-Zusman, & Safren, 2020). This item was scaled from 1 (Not at all) to 5 (Extremely). Other questions were asked regarding the specific impact of COVID-19, such as experiences of financial loss.
A three-item scale was developed to measure anxiety specific to COVID-19. The scale included the following items: “During the past month, how often have you thought about your chances (or risks) of getting COVID-19?” “During the past month, how often have thoughts about your chances (or risks) of getting COVID-19 affected your mood?” and “During the past month, how often have thoughts about your chances (or risks) of getting COVID-19 affected your ability to perform daily activities?” All items were scaled from 1 (Not at all) to 4 (A lot). The average of these questions was used as the COVID-19 anxiety score for each individual (α = .76).
Location-based policy measures in response to COVID-19 were downloaded from the Oxford COVID-19 government response tracker (Hale et al., 2021). A lockdown index score was calculated by summing the closure policy indicators (e.g., school closures, restrictions of public gatherings).
Data Analysis
Analyses were limited to respondents who identified as women. Analyses were completed using R software version 3.6.1. Descriptive statistics such as means, SDs, and percentages were used to summarize the sample. Pearson correlations with a Bonferroni correction were used to analyze relationships among mental health, self-efficacy, intolerance for uncertainty, and daily impact of COVID-19. Variables that were significantly related to COVID-19 anxiety were included in a multiple regression analysis. Backward stepwise regression was used to identify the most parsimonious model by identifying the model with the lowest Akaike information criterion. Participants were categorized as being at low (n = 303), moderate (n = 165), or severe risk (n = 31) for problematic alcohol use based on AUDIT-C scores. One-way analyses of variance were used to compare AUDIT-C severity on depression, anxiety, perceived stress, and social support. Tukey tests were used for post hoc analyses.
Results
We gathered 1998 responses to the screener survey. Of these, 20 indicated they were not interested, 27 did not have Facebook, 329 did not meet minimum Facebook activity requirements, and 561 completed the screening questions but did not share Facebook data. Of the 1055 people who were forwarded to the study survey, 667 people completed it, with 499 (74.81%) being women, 145 (21.74%) being men, and 23 (3.45%) indicating being gender fluid or nonbinary.
On average, the participants were in their mid-30s and White and had a college education (see Table 1 ). Of respondents, 391 women (78.36%) experienced personal financial loss after the onset of the pandemic, such as losing a job or wages, losing retirement funds or investments, or travel-related cancellations. In addition, 107 (21.44%) increased their alcohol or other drug use after the onset of the pandemic. There were no differences between White and non-White respondents on depression (p = .698), anxiety (p = .914), COVID-19 anxiety (p = .452), perceived stress (p = .158), social support (p = .944), loneliness (p = .930), or AUDIT-C scores (p = .066).
Table 1.
Demographics
| Variable | m (SD) or n (%) |
|---|---|
| Age | 36.4 (13.44) |
| Hispanic | 48 (9.62) |
| Race | |
| Asian | 43 (8.62) |
| Black or African American | 52 (10.42) |
| White | 365 (73.15) |
| Other | 17 (3.41) |
| Multi-racial | 18 (3.61) |
| Prefer not to say | 4 (.8) |
| Income, $ | |
| Less than 10,000 | 41 (8.22) |
| 10,000–19,999 | 41 (8.22) |
| 20,000–29,999 | 47 (9.42) |
| 30,000–39,999 | 47 (9.42) |
| 40,000–49,999 | 48 (9.62) |
| 50,000–59,999 | 59 (11.82) |
| 60,000–69,999 | 36 (7.21) |
| 70,000–79,999 | 42 (8.42) |
| 80,000–89,999 | 19 (3.81) |
| 90,000–99,999 | 14 (2.81) |
| 100,000–149,000 | 67 (13.43) |
| 150,000 or more | 38 (7.62) |
| Religion | |
| Protestant/Other Christian | 147 (29.46) |
| Catholic | 81 (16.23) |
| Mormon | 9 (1.8) |
| Jewish | 25 (5.01) |
| Muslim | 1 (.2) |
| Hindu | 6 (1.2) |
| Buddhist | 9 (1.8) |
| Other non-Christian religion | 20 (4.01) |
| None/Atheist/Agnostic | 168 (33.67) |
| Other | 33 (6.61) |
| Political affiliation | |
| Conservative | 38 (7.62) |
| Moderate | 170 (34.07) |
| Liberal | 266 (53.31) |
| Apolitical | 13 (2.61) |
| Other | 12 (2.4) |
| Children in household | 178 (35.67) |
| Education | |
| Less than high school | 2 (.4) |
| High school | 36 (7.21) |
| Technical/Vocational school | 13 (2.61) |
| Some college | 101 (20.24) |
| Associate's degree | 44 (8.82) |
| Bachelor's degree | 188 (37.68) |
| Postgraduate/Professional degree | 115 (23.05) |
A total of 101 (20.24%) women acknowledged at least one problem related to IPV, such as being forced into sex, physically abused, threatened, insulted, or yelled at by their partners. The most frequently acknowledged IPV problem was being insulted or yelled at by their partner (n = 88, 87%). Other acknowledged IPV problems were being threatened (n = 11, 10.89%), forced to have sex (n = 4, 3.96%), and physically abused (n = 10, 9.9%). Thirty (29.7%) of these women stated that their IPV problems have gotten worse since the pandemic started, and 17 (16.83%) said that they have increased their drug or alcohol use to cope with their relationship problems.
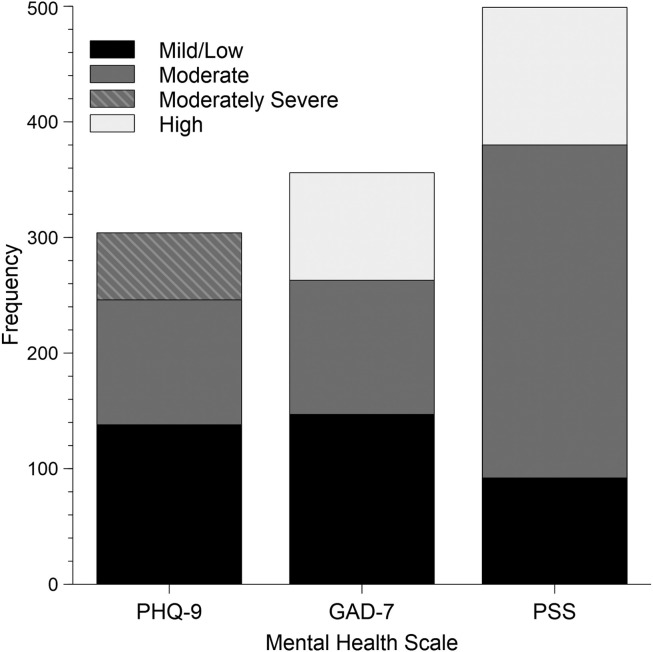
Figure 1 shows the distribution of scores from the mental health questionnaires (PHQ-9, GAD-7, PSS) within clinical severity categories. Most participants indicated that they had mild or higher depression (61%) and anxiety (71%), and moderate or higher stress (82%). There was no relationship between state-mandated closures and depression (p = .366), anxiety (p = .856), COVID-19 anxiety (p = .365), or perceived stress (p = .736), and lockdown-based closures were not considered in further analyses. Table 2 displays the correlation matrix for mental health variables, self-efficacy, daily impact of COVID-19, and household income. COVID-19 anxiety was moderately positively related to daily impact of COVID-19. There was a significant positive relationship between the COVID-19 anxiety measure and mental health measures, including depression, anxiety, and perceived stress. Self-efficacy, loneliness, and intolerance of uncertainty were also related to COVID-19 anxiety. These relationships were further explored using a multiple regression analysis (see Table 3 ). Anxiety, daily impact of COVID-19, and lower self-efficacy were significant predictors of COVID-19–specific anxiety. The variance in COVID-19 anxiety accounted for by this model was 29.53%. These findings together suggest that anxiety in general, more daily impact from the pandemic, and lower self-efficacy were uniquely associated with greater anxiety about COVID-19.
Figure 1.
Frequency of scores from mental health questionnaires (PHQ-9, GAD-7, PSS) within clinical severity categories. PHQ-9 is the only scale that has a moderately severe category.
Table 2.
Pearson Correlations Between Mental Health, Daily Impact of COVID, Loneliness, Self-Efficacy, Social Support, and Intolerance for Uncertainty
| Anxiety (GAD-7) | COVID-19 Anxiety | Daily Impact of COVID | Depression (PHQ-9) | IUS-12 | Loneliness | Perceived Stress | Self-Efficacy | Social Support | m | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety (GAD-7) | — | 8.7 | 5.88 | ||||||||
| COVID Anxiety | .47∗∗∗ | — | 2.18 | 0.73 | |||||||
| Daily Impact of COVID | .27∗∗∗ | .36∗∗∗ | — | 3.67 | 1.04 | ||||||
| Depression (PHQ-9) | .77∗∗∗ | .36∗∗∗ | .17∗∗ | — | 8.67 | 6.40 | |||||
| IUS-12 | .56∗∗∗ | .35∗∗∗ | .21∗∗∗ | .47∗∗∗ | — | 33.39 | 10.17 | ||||
| Loneliness | .45∗∗∗ | .27∗∗∗ | .21∗∗∗ | .55∗∗∗ | .38∗∗∗ | — | 5.97 | 1.96 | |||
| Perceived Stress | .81∗∗∗ | .42∗∗∗ | .27∗∗∗ | .75∗∗∗ | .58∗∗∗ | .52∗∗∗ | — | 20.64 | 7.85 | ||
| Self-Efficacy | −.44∗∗∗ | −.32∗∗∗ | −.08 | −.53∗∗∗ | −.40∗∗∗ | −.39∗∗∗ | −.56∗∗∗ | — | 3.86 | 0.78 | |
| Social Support | −.37∗∗∗ | −.17∗∗ | −.09 | −.36∗∗∗ | −.28∗∗∗ | −.47∗∗∗ | −.43∗∗∗ | .44∗∗∗ | — | 23.2 | 5.25 |
Abbreviations: GAD-7, Generalized Anxiety Disorder 7; PHQ-9, Patients Health Questionnaire 9; IUS-12, Intolerance for Uncertainty.
∗p < .05, ∗∗p < .01, ∗∗∗p < .001.
Table 3.
Regression Results for COVID-19 Anxiety
| β | SE | t | p | 95% CI | F | p | Adj. R2 | |
|---|---|---|---|---|---|---|---|---|
| Overall Model | 53.06 | <.001 | 29.53% | |||||
| Anxiety | .292 | .049 | 6.01 | <.001 | [.282 to .302] | |||
| Daily Impact of COVID-19 | .258 | .039 | 6.56 | <.001 | [.182 to .334] | |||
| IUS-12 | .007 | .047 | 1.59 | .112 | [−.085 to .099] | |||
| Self-Efficacy | −.143 | .043 | −3.32 | <.001 | [−.227 to −.059] |
Abbreviations: Adj R2, adjusted R-squared values; β, standardized coefficients; CI, confidence intervals; SE, standard error; IUS-12, Intolerance for Uncertainty Scale.
Severity of alcohol use was compared with depression, anxiety, perceived stress, and social support scores. There was a significant difference in depression and anxiety scores across AUDIT-C severity, F(2, 496) = 3.47, p = .032 and F(2,496) = 3.60, p = .028, respectively. Those with high-risk alcohol use had significantly higher depression (m = 11.45, SD = 6.64) and anxiety (m = 11.16, SD = 6.53) scores than those with low-risk use (m = 8.31, SD = 6.69, p = .025, and m = 8.31, SD = 6.11, p = .027, respectively). There was insufficient evidence to conclude whether a difference in perceived stress across alcohol use severity categories was present, F(2,496) = 2.4, p = .092. There was a significant difference in social support across alcohol use severity categories, F(2,496) = 4.76, p = .009, with those in the moderate alcohol risk group (m = 24.01, SD = 4.81) reporting significantly higher social support than the high-risk group (m = 21.13, SD = 5.92, p = .014).
Discussion
The current study provides initial information about women's mental health, substance use, and financial and social experiences during the COVID-19 pandemic. Our results suggest that women are experiencing poor mental health outcomes significantly related to the perceived daily impact of the COVID-19 pandemic and COVID-19–specific anxiety. These findings further support a gender-specific approach to combating the COVID-19 pandemic. Others have suggested that gender should be a consideration when making decisions regarding the health care response and allocation of charitable resources (Connor et al., 2020).
The large number of women experiencing mental health problems indicates a clear need for mental health services. As a response to the pandemic, many providers have offered more digital options for accessing medical services (frequently termed “telehealth”). Digital provision could expand access safely while helping overcome common barriers, such as distance and lack of reliable transportation. Our findings are useful in identifying factors related to mental health problems. Some factors, such as self-efficacy, could be included in mental health screening or part of a mental health treatment plan, regardless of whether the screening is digital or in-office. Finally, based on findings from this study and others (Arkins, Begley, & Higgins, 2016; Chang et al., 2011), we recommend that IPV should be included as part of mental health screening.
Using substances to cope with worsening mental health problems has negative physical and psychological impacts (Mauro, Canham, Martins, & Spira, 2015). Although men are at higher risk for substance use disorders, this gap is narrowing (McHugh, Votaw, Sugarman, & Greenfield, 2018), and women may be more likely to use alcohol to cope with stress (MacMillan et al., 2021; Nolen-Hoeksema & Harrell, 2002; Rice & Van Arsdale, 2010). High-risk alcohol use was associated with higher scores on anxiety and depression measures in our sample, suggesting that worsening mental health outcomes related to the pandemic may also relate to increased drinking. Our findings can be viewed in light of reports of increased alcohol sales (Zipursky et al., 2021) and opioid overdoses (Haley & Saitz, 2020; Slavova, Rock, Bush, Quesinberry, & Walsh, 2020) during the pandemic.
Approximately one in five women report having experienced severe physical violence or sexual violence from a partner in their lifetime (Smith et al., 2018). Similarly, approximately one-fifth of the women sampled experienced at least one aspect of IPV, with many reporting that these problems have gotten worse since the onset of the pandemic. A smaller proportion reported drinking or using substances to cope with violence in their relationships. The present findings lend additional evidence that during the COVID-19 pandemic, women are at increased risk for IPV, likely stemming from a variety of factors such as increased time spent alone with their partners, increased economic and psychological stress, and social isolation (Van Gelder et al., 2020). When addressing the consequences of the pandemic, IPV and its psychosocial consequences should be a major area of concern.
The present study is limited by the characteristics of the sample. There is no male comparison group, most of the sample is White and higher income, and only cisgender women are included. Based on this sample, we cannot be sure that the difficulties presented are women-specific, and future work should include men for comparison. Transgender, nonbinary, and gender nonconforming people are also affected by gender-based inequities, which likely extends to the effects of the COVID-19 pandemic. Transgender and gender nonconforming individuals experience higher rates of IPV (Valentine et al., 2017) and mental health concerns, such as anxiety and depression as compared with cisgender individuals (Downing & Przedworski, 2018). Although we did not detect any racial differences on mental health or alcohol use variables, a further limitation is that our mostly White sample led us to group all non-White people into one category. Further research is needed into the impact of the pandemic on psychosocial outcomes among women of color. Nonetheless, those who face marginalization based on their race, ethnicity, and/or gender should be included as part of a larger conversation regarding social and health care responses to the COVID-19 pandemic.
Conclusion
This study shows significant impact of COVID-19 on mental health of women. Although we report some of these effects, further research is needed into the unique impacts the pandemic has had on women. Gender should be included as a variable of interest in future studies that investigate the mental health and substance use impacts of COVID-19. Our data expand on the limited number of studies indicating the disproportionate psychosocial impact of the COVID-19 pandemic on women, and point to a critical need for pandemic-related mental health services that serve women.
Implications for Practice and/or Policy
Measures taken by governmental and public health organizations to mitigate the social consequences of the COVID-19 pandemic should consider that women may have been uniquely affected. Women who use substances and those who have experienced a greater day-to-day impact of the pandemic are especially at risk for poor mental health outcomes. Providing continued care for women who are in or out of substance use treatment may improve their mental health and resilience to relapse as they navigate the added stress of the COVID-19 pandemic. Providing digital mental health screenings to patients and connecting them to treatment resources could be beneficial. Decoupling health insurance and employment could ensure continued access to health care, including mental health care, for those who have lost their jobs during the pandemic. In addition, given that our findings support previous commentaries suggesting increased risk for IPV victimization during the pandemic, we suggest increased use of screening tools for IPV in spaces that primarily serve women, such as obstetrics/gynecology clinics, in order to identify women in need of support.
Acknowledgments
The corresponding author, Dr. Brenda Curtis, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Biographies
Amanda Devoto, PhD, is a Postdoctoral Fellow at the National Institute on Drug Abuse Intramural Research Program. Her research focus is on behavioral economic and incentive interventions in the promotion of health behaviors.
McKenzie Himelein-Wachowiak, BA, was a Post Baccalaureate Trainee at the National Institute on Drug Abuse Intramural Research Program and is currently pursuing a PhD in Clinical Psychology at Temple University. Her research focus is on nonsuicidal self-injury.
Tingting Liu, PhD, is a Postdoctoral Fellow at the National Institute on Drug Abuse Intramural Research Program. Her research uses interdisciplinary methodologies to understand the social facilitators behind decision-making and mental health issues.
Brenda Curtis, PhD, MsPH, is a Clinical Investigator at the National Institute on Drug Abuse Intramural Research Program. Her research leverages big data methodologies to better understand substance use, stigma, and health disparities.
Footnotes
This study was funded by the Intramural Research Program of the National Institutes of Health, National Institute on Drug Abuse.
The authors report no financial relationships with commercial interests.
References
- Albert P.R. Why is depression more prevalent in women? Journal of Psychiatry & Neuroscience. 2015;40(4):219–221. doi: 10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arkins B., Begley C., Higgins A. Measures for screening for intimate partner violence: a systematic review. Journal of Psychiatric and Mental Health Nursing. 2016;23(3–4):217–235. doi: 10.1111/jpm.12289. [DOI] [PubMed] [Google Scholar]
- Bradley K.A., Bush K.R., Epler A.J., Dobie D.J., Davis T.M., Sporleder J.L.…Kivlahan D.R. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Archives of Internal Medicine. 2003;163(7):821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Norton M.P.J., Asmundson G.J. Fearing the unknown: a short version of the Intolerance of Uncertainty Scale. Journal of Anxiety Disorders. 2007;21(1):105–117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Chang J.C., Cluss P.A., Burke J.G., Hawker L., Dado D., Goldstrohm S., Scholle S.H. Partner violence screening in mental health. General Hospital Psychiatry. 2011;33(1):58–65. doi: 10.1016/j.genhosppsych.2010.11.009. [DOI] [PubMed] [Google Scholar]
- Chen G., Gully S.M., Eden D. Validation of a new general self-efficacy scale. Organizational Research Methods. 2001;4(1):62–83. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Connor J., Madhavan S., Mokashi M., Amanuel H., Johnson N.R., Pace L.E., Bartz D. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Social Science & Medicine. 2020;266:113364. doi: 10.1016/j.socscimed.2020.113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen W., Gulati G., Kelly B.D. Mental health in the Covid-19 pandemic. QJM: An International Journal of Medicine. 2020;113(5):311–312. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downing J.M., Przedworski J.M. Health of transgender adults in the US, 2014–2016. American Journal of Preventive Medicine. 2018;55(3):336–344. doi: 10.1016/j.amepre.2018.04.045. [DOI] [PubMed] [Google Scholar]
- Elphinstone B. Identification of a suitable short-form of the UCLA-Loneliness Scale. Australian Psychologist. 2018;53(2):107–115. [Google Scholar]
- Feldhaus K.M., Koziol-McLain J., Amsbury H.L., Lowenstein S.R., Abbott J.T. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA. 1997;277(17):1357–1361. [PubMed] [Google Scholar]
- Golden L., Kim J. Underemployment just isn't working for US part-time workers. The Center for Law and Social Policy. 2020. https://www.clasp.org/publications/report/brief/underemployment-just-isnt-working-us-part-time-workers Available:
- Groarke J.M., Berry E., Graham-Wisener L., McKenna-Plumley P.E., McGlinchey E., Armour C. Loneliness in the UK during the COVID-19 pandemic: cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS One. 2020;15(9):e0239698. doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T.…Tatlow H. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nature Human Behaviour. 2021;5(4):529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- Haley D.F., Saitz R. The opioid epidemic during the COVID-19 pandemic. JAMA. 2020;324(16):1615–1617. doi: 10.1001/jama.2020.18543. [DOI] [PubMed] [Google Scholar]
- Hamberger L.K., Larsen S.E. Men’s and women’s experience of intimate partner violence: a review of ten years of comparative studies in clinical samples; Part I. Journal of Family Violence. 2015;30(6):699–717. [Google Scholar]
- Harkness A., Behar-Zusman V., Safren S.A. Understanding the impact of COVID-19 on Latino sexual minority men in a US HIV hot spot. AIDS and Behavior. 2020;24(7):2017–2023. doi: 10.1007/s10461-020-02862-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron S.L., Thompson M.P., Jackson E., Kaslow N.J. Do responses to an intimate partner violence screen predict scores on a comprehensive measure of intimate partner violence in low-income black women? Annals of Emergency Medicine. 2003;42(4):483–491. doi: 10.1067/s0196-0644(03)00718-2. [DOI] [PubMed] [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauffman S.E., Silver P., Poulin J. Gender differences in attitudes toward alcohol, tobacco, and other drugs. Social Work. 1997;42(3):231–241. doi: 10.1093/sw/42.3.231. [DOI] [PubMed] [Google Scholar]
- Kliem S., Mößle T., Rehbein F., Hellmann D.F., Zenger M., Brähler E. A brief form of the Perceived Social Support Questionnaire (F-SozU) was developed, validated, and standardized. Journal of Clinical Epidemiology. 2015;68(5):551–562. doi: 10.1016/j.jclinepi.2014.11.003. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krusche A., Cyhlarova E., Williams J.M.G. Mindfulness online: an evaluation of the feasibility of a web-based mindfulness course for stress, anxiety and depression. BMJ Open. 2013;3(11):e003498. doi: 10.1136/bmjopen-2013-003498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefkowitz D., Armin J.S. Why employment during and after COVID-19 is a critical women’s health issue. Women's Health Issues. 2020;31(3):190–194. doi: 10.1016/j.whi.2020.12.004. [DOI] [PubMed] [Google Scholar]
- Lex B.W. Alcohol and other drug abuse among women. Alcohol Health and Research World. 1994;18(3):212–219. [PMC free article] [PubMed] [Google Scholar]
- MacMillan T., Corrigan M.J., Coffey K., Tronnier C.D., Wang D., Krase K. Exploring factors associated with alcohol and/or substance use during the COVID-19 pandemic. International Journal of Mental Health and Addiction. 2021:1–10. doi: 10.1007/s11469-020-00482-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik S., Naeem K. Sustainable Development Policy Institute; 2020. Impact of COVID-19 pandemic on women: health, livelihoods & domestic violence.http://www.jstor.org/stable/resrep24350 Available: [Google Scholar]
- Mauro P.M., Canham S.L., Martins S.S., Spira A.P. Substance-use coping and self-rated health among US middle-aged and older adults. Addictive Behaviors. 2015;42:96–100. doi: 10.1016/j.addbeh.2014.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh R.K., Votaw V.R., Sugarman D.E., Greenfield S.F. Sex and gender differences in substance use disorders. Clinical Psychology Review. 2018;66:12–23. doi: 10.1016/j.cpr.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., Harrell Z.A. Rumination, depression, and alcohol use: tests of gender differences. Journal of Cognitive Psychotherapy. 2002;16(4):391–403. [Google Scholar]
- Osland K.M., Røysamb M.G., Nortvedt J. The impact of Covid-19 on the Women, Peace and Security Agenda. NUPI Covid-19 Brief. 2020. https://www.jstor.org/stable/pdf/resrep25732.pdf?acceptTC=true&coverpage=false Available:
- Parlapani E., Holeva V., Nikopoulou V.A., Sereslis K., Athanasiadou M., Godosidis A.…Diakogiannis I. Intolerance of uncertainty and loneliness in older adults during the COVID-19 pandemic. Frontiers in Psychiatry. 2020;11:842. doi: 10.3389/fpsyt.2020.00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. New England Journal of Medicine. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Phelps C.L., Paniagua S.M., Willcockson I.U., Potter J.S. The relationship between self-compassion and the risk for substance use disorder. Drug and Alcohol Dependence. 2018;183:78–81. doi: 10.1016/j.drugalcdep.2017.10.026. [DOI] [PubMed] [Google Scholar]
- Pigott T.A. Anxiety disorders in women. Psychiatric Clinics of North America. 2003;26(3):621–672. doi: 10.1016/s0193-953x(03)00040-6. [DOI] [PubMed] [Google Scholar]
- Rice K.G., Van Arsdale A.C. Perfectionism, perceived stress, drinking to cope, and alcohol-related problems among college students. Journal of Counseling Psychology. 2010;57(4):439. [Google Scholar]
- Rodriguez L.M., Litt D.M., Stewart S.H. Drinking to cope with the pandemic: the unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors. 2020;110:106532. doi: 10.1016/j.addbeh.2020.106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell A.M., Barry A.E. Psychometric properties of the AUDIT-C within an Amazon Mechanical Turk Sample. American Journal of Health Behavior. 2021;45(4):695–700. doi: 10.5993/AJHB.45.4.8. [DOI] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M.…Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Globalization and Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug and Alcohol Dependence. 2020;214:108176. doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S.G., Zhang X., Basile K.C., Merrick M.T., Wang J., Kresnow M.J., Chen J. Centers for Disease Control and Prevention; Atlanta, GA: 2018. The national intimate partner and sexual violence survey: 2015 data brief–updated release.https://stacks.cdc.gov/view/cdc/60893 Available: [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tuchman E. Women and addiction: The importance of gender issues in substance abuse research. Journal of Addictive Diseases. 2010;29(2):127–138. doi: 10.1080/10550881003684582. [DOI] [PubMed] [Google Scholar]
- Valentine S.E., Peitzmeier S.M., King D.S., O'Cleirigh C., Marquez S.M., Presley C., Potter J. Disparities in exposure to intimate partner violence among transgender/gender nonconforming and sexual minority primary care patients. LGBT Health. 2017;4(4):260–267. doi: 10.1089/lgbt.2016.0113. [DOI] [PubMed] [Google Scholar]
- Van Gelder N., Peterman A., Potts A., O'Donnell M., Thompson K., Shah N., Oertelt-Prigione S. COVID-19: reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine. 2020;21:100348. doi: 10.1016/j.eclinm.2020.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Wilde N., Hsu A. The influence of general self-efficacy on the interpretation of vicarious experience information within online learning. International Journal of Educational Technology in Higher Education. 2019;16(1):1–20. [Google Scholar]
- Yavorsky J.E., Dush C.M., Schoppe-Sullivan S.J. The production of inequality: the gender division of labor across the transition to parenthood. Journal of Marriage and the Family. 2015;77(3):662–679. doi: 10.1111/jomf.12189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaami S., Marinelli E., Varì M.R. New trends of substance abuse during COVID-19 pandemic: an international perspective. Frontiers in Psychiatry. 2020;11:700. doi: 10.3389/fpsyt.2020.00700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Liu L., Xue P., Yang X., Tang X. Mental health response to the COVID-19 outbreak in China. American Journal of Psychiatry. 2020;177(7):574–575. doi: 10.1176/appi.ajp.2020.20030304. [DOI] [PubMed] [Google Scholar]
- Zipursky J.S., Stall N.M., Silverstein W.K., Huang Q., Chau J., Hillmer M.P., Redelmeier D.A. Alcohol sales and alcohol-related emergencies during the COVID-19 pandemic. Annals of Internal Medicine. 2021;174(7):1029–1032. doi: 10.7326/M20-7466. [DOI] [PMC free article] [PubMed] [Google Scholar]