The challenges posed by the increasing incidence of haematological malignancies in older patients were highlighted recently in reviews and in a Workshop sponsored by the American Society of Hematology. (Lowenberg, 2018) There is a need for evidence to guide treatment decisions for older adults, particularly in the use of novel targeted or immunotherapeutic agents. This is largely a consequence of the under-representation of this demographic in cancer clinical trials.
Management of primary central nervous system (CNS) lymphoma (PCNSL) in patients aged ≥ 70 years represents a significant problem. (Welch et al., 2012, Mendez et al., 2017, Roth & Hoang-Xuan, 2014) While older PCNSL patients generally can tolerate and benefit from high-dose methotrexate-based induction, whole brain irradiation consolidation is not favoured because of excessive neurotoxicity. While intensive consolidation probably improves outcomes in patients aged < 70 years, high dose‐chemotherapy is not an option for most older PCNSL patients. Given that the median age of PCNSL at diagnosis is ~ 60 years, determination of the optimal consolidative approach for older patients is an important question. This problem is particularly significant given that the incidence of PCNSL continues to rise in this older age group (Villano et al., 2011).
PCNSL increasingly appears to be a curable brain tumour. However, in most clinical trials to date, outcomes for patients older than 60 years remain poor, with 1-year progression-free survival (PFS) rates of ~ 40% and median overall survival (OS) in the range of 14–30 months (Omuro et al., 2015, Zhu et al., 2009, Fritsch et al., 2017). Recent data from the Central Brain Tumor Registry and the Surveillance, Epidemiology and End Results Program demonstrated that, while median OS of all PCNSL patients doubled, from 12.5 months in the 1970’s to 26 months in the 2010’s, progress was restricted to younger patients. Median OS for PCNSL patients aged ≥ 70 years has not improved over 40 years: 6 months (1970’s) vs. 7 months (2010’s). (Mendez et al., 2017) These dismal results underscore the need for novel therapeutic approaches for the particularly vulnerable older PCNSL patient population.
We recently conducted a phase I investigation of lenalidomide in a cohort of patients with relapsed CNS lymphomas, median age 66 years, demonstrating both cerebrospinal fluid penetration of lenalidomide at doses as low as 10 mg, plus the activity of lenalidomide as monotherapy in refractory disease. In a parallel analysis, we described 10 consecutive relapsed PCNSL patients (median age 61.5 years) who received low-dose lenalidomide maintenance (5–10 mg/day) after salvage therapy and until disease progression. In most cases, remission duration with lenalidomide maintenance was significantly longer than previous response durations. (Rubenstein et al., 2018)
Beginning in late 2011, we began using low-dose lenalidomide as maintenance in consecutive older PCNSL patients (age ≥ 70 years, human immunodeficiency virus negative) after a partial or complete response to methotrexate/rituximab-based induction, in lieu of surveillance, irradiation or high-dose chemotherapeutic consolidation. This retrospective analysis of the first 13 consecutive patients was performed in accordance with a protocol approved by the University of California, San Francisco Institutional Review Board and patient’s signed informed consent.
Median age at diagnosis of this cohort was 77 years (range 70–86). Median Karnofsky performance status and International Extranodal Lymphoma Study Group PCNSL prognostic risk score was 60 (range 50–80) and 4 (range 3–5), respectively (Table I).
Table I.
Characteristics of Elderly PCNSL Patients who Received Low-Dose Lenalidomide Maintenance After Methotrexate-Based Induction Therapy.
| Pt | Age (years)/ Sex |
Disease site | KPS at Dx |
IELSG score |
Medical comorbidities |
Induction therapy |
Median MTX dose (range) g/m2 |
Interval between diagnosis and lenalidomide (months) |
Lenalidomide dose |
Duration of maintenance lenalidomide (months) |
PFS (months) |
OS (months) |
Disease status |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 72/M | Cerebellum, IOL | 60 | 4 | CAD, HLD, DM2 | MT-R | 6 (6-8) | 19.6 | 5 mg/day | 65.2 | 84.8 | 89.8+ | CR2 |
| 2 | 78/M | Multifocal, IOL | 60 | 4 | HepB, HTN, DM2, Macular Degeneration | M-R | 3 | 3.4 | 5 mg/day | 40.4 | 43.8 | 84.2+ | CR2 |
| 3 | 75/M | Periventricular | 60 | 4 | HTN | MT-R | 5 (5-5.5) | 5.2 | 5 mg/day | 0.9 | 59.2 | 59.2 | CR1* |
| 4 | 86/F | Temporal lobe | 60 | 4 | HTN, HLD, Oral Cancer | MT-R | 2.5 (2.5-3.5) | 9.2 | 5/10 mg QOD | 38.8 | 48.0 | 57.9+ | PD |
| 5 | 86/M | Frontal lobe, IOL | 60 | 3 | GERD, HLD | 3 Fx WBRT → MT-R | 2 (1-2) | 6.0 | 5 mg/day | 21.0 | 29.4 | 40.0+ | CR2 |
| 6 | 75/M | Periventricular | 80 | 3 | PMR, CAD, HTN, GERD | MT-R | 8 (4-8) | 9.7 | 5 mg/day | 3.8 | 38.0+ | 38.0+ | CR1 |
| 7 | 77/F | Multifocal, deep | 60 | 4 | None | MT-R | 2 (1-4) | 8.3 | 5 mg/day | 23.3+ | 31.6+ | 31.6+ | CR1 |
| 8 | 70/F | Periventricular | 70 | 3 | Hypothyroidism | MT-R | 4.8 (4.4-6) | 7.7 | 5 mg/day | 19.4+ | 27.1+ | 27.1+ | CR1 |
| 9 | 77/M | Periventricular, deep | 70 | 4 | CAD | M-R | 2.5 (2-2.5) | 5.7 | 10 mg/day | 14.5+ | 20.2+ | 20.2+ | CR1 |
| 10 | 83/F | Multifocal, deep | 60 | 4 | HTN, DM2, Hypothyroidism, Stage 3 CKD | MT-R | 0.75 (0.5-1) | 4.6 | 5 mg/day | 17.5+ | 22.1+ | 22.1+ | CR1 |
| 11 | 75/F | Multifocal, deep | 50 | 5 | Stage 3 CKD | MT-R | 1 (0.5-1) | 9.0 | 5 mg/day | 8.4 | 27.2 | 27.7+ | PD |
| 12 | 85/F | Suprasellar, deep | 60 | 5 | HTN, Hypothyroidism, DM2, Stage 3 CKD | MT-R | 2.5 | 5.6 | 5 mg/day | 6.6+ | 12.2+ | 12.2+ | CR1 |
| 13 | 78/F | Multifocal, deep | 50 | 4 | HTN, Hypothyroidism, DM2 | MT-R | 1.5 (1.5-4) | 4.0 | 5 mg/day | 4.1+ | 8.1+ | 8.1+ | CR1 |
: deceased.
CAD: coronary artery disease; CKD: chronic kidney disease; CR1: first complete remission; CR2: second complete remission; DMII: type II diabetes mellitus; Dx: diagnosis; F: female; GERD: gastroesophageal reflux disease; HepB: hepatitis B; HLD: hyperlipidaemia; HTN: hypertension; IELSG: International Extranodal Lymphoma Study Group; IOL: intraocular lymphoma; KPS: Karnofsky performance status; M: male; MT-R: methotrexate, temozolomide, rituximab; MTX: methotrexate; OS: overall survival; PCNSL: primary central nervous system lymphoma; PD: progressive disease; PFS: progression-free survival; PMR: polymyalgia rheumatica; QOD: every other day; WBRT: whole brain irradiation.
All subjects received induction therapy with methotrexate plus rituximab, and 11 received methotrexate, temozolomide and rituximab (MT-R). Due to advanced age and decreased renal function, most subjects received reduced doses of methotrexate (median 2.5 g/m2, range 0.5 – 8). Induction therapy was well-tolerated with only two grade 3 toxicities: acute kidney injury and urinary tract infection.
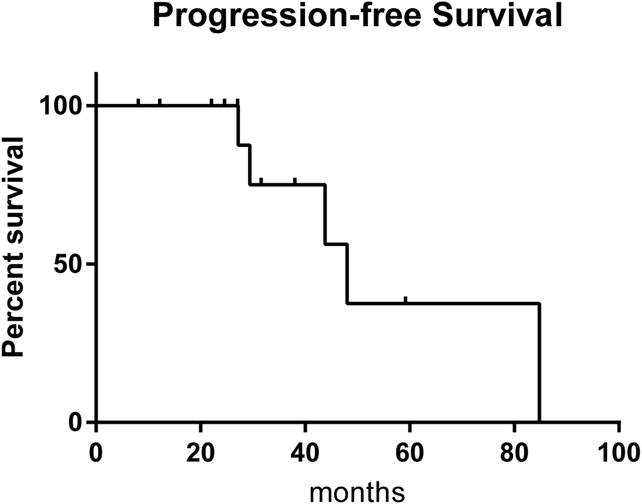
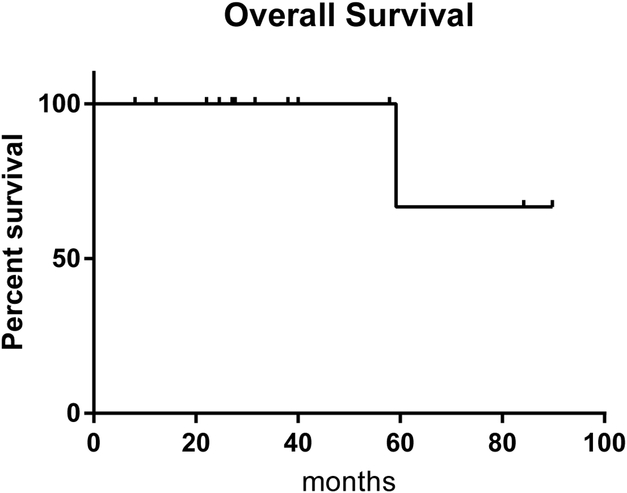
The median interval between diagnosis of PCNSL and initiation of adjuvant or maintenance lenalidomide (5‐10 mg/day on a 21-day cycle) plus aspirin was 6.0 months (range 3.4 – 19.6). Two patients received lenalidomide plus maintenance intravenous rituximab, every 6 months. With overall median follow‐up of 31.6 months, low-dose lenalidomide was well-tolerated by this older PCNSL population (Table SI): median time on lenalidomide maintenance was 18.9 months (range 0.9 ‐ 65.2). All patients were closely monitored with median of three surveillance magnetic resonance imaging scans/patient. Median PFS has not been reached, and thus far there has been only one death: Patient 3, who discontinued maintenance lenalidomide after developing a subdural haematoma, attributed to aspirin at one month, died from complications of a myocardial infarction four years later (Figure 1).
Figure 1. Progression-Free and Overall Survival of Elderly PCNSL Patients who Received Low-Dose Lenalidomide Maintenance After Methotrexate-Based Induction Therapy.
A. With median overall follow-up of 31.64 months, median progression-free survival has not been reached. Of the 5 patients who progressed thus far, 3 responded to salvage therapy and are maintained in second complete remission after repeat institution of maintenance lenalidomide at 5-10 mg/day (Patients 1, 2 and 5).
B. Overall survival. Thus far, 1 primary central nervous system lymphoma patient in this series has died. Median Karnofsky performance status at last follow-up is 100 (range, 50-100). Disease progression in Patient 1 resolved with vitrectomy and the patient resumed maintenance lenalidomide at 5 mg/day. Patient 2, who achieved only a partial response after acute renal failure with MT-R (methotrexate, temozolomide, rituximab) induction, exhibited stable intraocular lymphoma with lenalidomide maintenance for 40 months, before disease progression in the right occipital lobe. He received re-induction immunochemotherapy with MT-R and subsequently resumed lenalidomide at the higher dose of 10 mg/day, with remission now exceeding 24 months. Patient 4, who had progression after 39 months of lenalidomide, received salvage focal irradiation followed by pomalidomide. Patient 5 had isolated intraocular relapse after 65 months of lenalidomide and received salvage ocular irradiation at progression and resumed maintenance lenalidomide. Patient 11 relapsed with isolated extra-central nervous system disease (left leg) 9 months after discontinuation of maintenance lenalidomide.
To our knowledge, this is the first report of maintenance therapy of any type that focuses on older PCNSL patients, age ≥70 years, who are not candidates for whole brain irradiation or high‐dose chemotherapeutic consolidation. With median follow-up of 31.6 months, these encouraging preliminary results of prolonged PFS and OS with low-dose lenalidomide as maintenance compare favourably to previous prospective trials and population-based studies in this population in which, at best, the majority of patients exhibit tumour progression within the first year and die within two years. This data also illustrates the feasibility of maintenance in PCNSL with lenalidomide, a targeted agent with immunotherapeutic properties. Nine patients completed at least eight months of lenalidomide maintenance, toxicities were manageable, and there has been only 1 death, not related to disease or treatment. Finally, while it has long been assumed that methotrexate doses ≥ 3 g/m2 are associated with optimal outcome in PCNSL, these results suggest that reduced-dose methotrexate-based induction followed by low-dose lenalidomide maintenance is well tolerated in patients aged ≥70 years and associated with excellent PFS and OS.
The pathogenesis of PCNSL is associated with immunodeficiency, a condition linked to aging and immunosenescence, in which defects in T-cell chemotaxis and cytokine production are demonstrated. Notably, low-dose lenalidomide was shown to enhance proliferation and suppress apoptosis of stimulated T cells from older subjects, via interleukin 2-dependent mechanisms, and to restore diminished T-cell chemotactic responses to CCL21 and sphingosine 1-phosphate. (Huang et al., 2011) The reversal of T-cell abnormalities associated with immunosenescence by low concentrations of lenalidomide suggests a mechanistic basis for its utility as maintenance therapy in PCNSL. We suggest that studies be conducted to prospectively test these hypotheses regarding the benefit of low-dose lenalidomide maintenance in older patients with PCNSL.
Supplementary Material
Acknowledgments
This research was supported by the Leukemia & Lymphoma Society, by NIH R01CA139–83-01A1 and by the Sandler Program for Breakthrough Biomedical Research (JLR)
Footnotes
Disclosures of Conflicts of Interest
Dr. Rubenstein receives research funding from Genentech and Celgene.
Published in part at the 2017 Annual Meeting of the International Congress of Malignant Lymphoma, Lugano.
References
- Fritsch K, Kasenda B, Schorb E, Hau P, Bloehdom J, Mohle R, Low S, Binder M, Atta J, Keller U, Wolf HH, Krause SW, Hess G, Naumann R, Sasse S, Hirt C, Lamprecht M, Martens U, Mogner A, Panse J, Frickhofen N, Roth A, Hader C, Deckert M, Fricker H, Ihorst G, Finke J, Illerhaus G. High-dose methotrexate-based immuno-chemotherapy for elderly primary CNS lymphoma patients (PRIMAIN study). Leukemia 2017; 31: 846–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang MC, Greig NH, Luo W Tweedie D, Schwartz JB, Longo DL, Ferrucci L, Ershler WB, Goetzl EJ. Preferential enhancement of older human T cell cytokine generation, chemotaxis, proliferation and survival by lenalidomide. Clin Immunol 2011; 138: 201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowenberg B Introduction to a review series on hematologic disease at older age. Blood 2018; 131: 473. [DOI] [PubMed] [Google Scholar]
- Mendez JS, Ostrom QT, Gittleman H, Kruchko C, DeAngelis LM, Barnholtz-Sloan JS, Grommes C. The Elderly Left Behind - Changes in Survival Trends of Primary Central Nervous System Lymphoma Over The Past Four Decades. Neuro Oncol 2018. 20(5):687–694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omuro A, Chinot O, Taillandier L, Ghesquieres H, Soussain C, Delwail V, Lamy T, Gressin R, Choquet S, Soubeyran P, Huchet A, Benouaich-Amiel A, Lebouvier-Sadot S, Gyan E, Touitou V, Barrié M, del Rio MS, Gonzalez-Aguilar A, Houillier C, Delgadillo D, Lacomblez L, Tanguy ML, Hoang-Xuan K. Methotrexate and temozolomide versus methotrexate, procarbazine, vincristine, and cytarabine for primary CNS lymphoma in an elderly population: an intergroup ANOCEF-GOELAMS randomised phase 2 trial. Lancet Haematol 2015; 2: e251–259. [DOI] [PubMed] [Google Scholar]
- Roth P, Hoang-Xuan K. Challenges in the treatment of elderly patients with primary central nervous system lymphoma. Curr Opin Neurol 2014; 27: 697–701. [DOI] [PubMed] [Google Scholar]
- Rubenstein JL, Geng H, Fraser EJ, Formaker P, Chen L, Sharma J, Killea P, Choi K, Ventura J, Kurhanewicz J, Lowell C, Hwang J, Treseler P, Sneed PK, Li J, Wang X, Chen N, Gangoiti J, Munster PN, Damato B. Phase 1 investigation of lenalidomide/rituximab plus outcomes of lenalidomide maintenance in relapsed CNS lymphoma. Blood Adv 2018; 2: 1595–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villano JL, Koshy M, Shaikh H, Dolecek TA, McCarthy BJ. Age, gender, and racial differences in incidence and survival in primary CNS lymphoma. Br J Cancer 2011; 105: 1414–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch MR, Omuro A, Deangelis LM. Outcomes of the oldest patients with primary CNS lymphoma treated at Memorial Sloan-Kettering Cancer Center. Neuro Oncol 2012; 14: 1304–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu JJ, Gerstner ER, Engler DA, Mrugala MM, Nugent W, Nierenberg K, Hochberg FH, Betensky RA, Batchelor TT. High-dose methotrexate for elderly patients with primary CNS lymphoma. Neuro Oncol 2009; 11: 211–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.