Abstract
Cemento‐osseous dysplasia (COD) is defined as a condition in which normal bone is replaced by fibrous connective tissue and cementum‐like deposits. It is generally asymptomatic and occurs mostly in female patients. Radiologically, it appears as an opaque, lobulated mass. When facing such lesions, it is advised to avoid performing any surgical procedures due to the decreased vascularization and healing potential. The main reported complications being poor healing, sequestrum formation, risk of infection, and fracture of the jaw. Treating posterior mandibular edentulism in presence of a COD can be a challenging situation especially when the patient requires an implant‐supported fixed rehabilitation. The aim of this paper is to describe a three‐stage modified protocol for implant placement in a compromised site presenting a focal cemento‐osseous dysplasia.
Keywords: cemento‐osseous dysplasia, dental implant, fibro‐osseous lesion, infection
Elective surgery is contraindicated in presence of a cemento‐osseous dysplasia due to the avascular nature of the lesion thus the high risk of infection. This case report describes a modified three‐stage protocol for implant placement in a site with COD.
![]()
1. INTRODUCTION
Cemento‐osseous dysplasia is a benign fibro‐osseous lesion affecting mainly African/African American female patients aged between 40 and 50. 1
Cemento‐osseous dysplasia is classified into three categories according to its location:
-
‐
Periapical COD in the periapical region of the anterior teeth.
-
‐
Focal COD associated with a single tooth.
-
‐
Florid COD (FCOD). In FCOD, lesions appear in more than one quadrant predominantly in the mandible. 2
Radiologically, the lesion is radiolucent at first but becomes progressively opaque as it matures with the deposition of a cementum‐like non‐vascularized tissue. 3 For this reason, elective surgery such as periodontal surgery, extractions, or implant placement is contraindicated. 4
In this case report, we will present a successful implant rehabilitation of a posterior mandibular edentulism in a patient presenting focal COD using a modified protocol.
2. CASE PRESENTATION
A 48‐year‐old female patient was referred to the Outpatient and Implantology department of the University Dental Clinic of Monastir—Tunisia for an implant rehabilitation. She was non‐smoker, and the medical history did not reveal any significant systemic diseases.
Clinically, she presented two edentulous sites; the first one was located in the right maxilla (tooth 16 and 17), while the second was located in the right mandible (tooth 47). Only the management of the mandibular site will be described in this paper.
A dental panoramic radiograph (OPG) was prescribed and showed a radiopaque lobular lesion in the site of tooth 47. Later, the CBCT's coronal sections enabled a better visualization of the lesion. The findings of the radiological examination were attributable to focal COD. (Figures 1 and 2).
FIGURE 1.
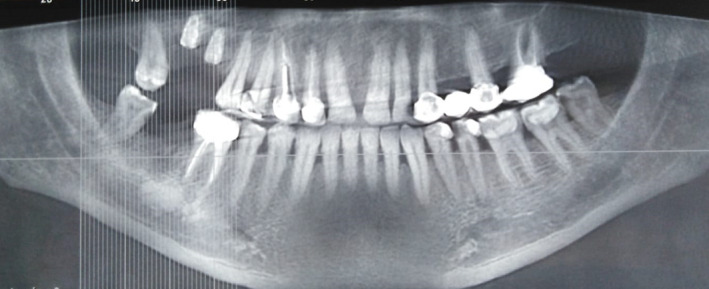
Pre‐operative panoramic reconstruction
FIGURE 2.
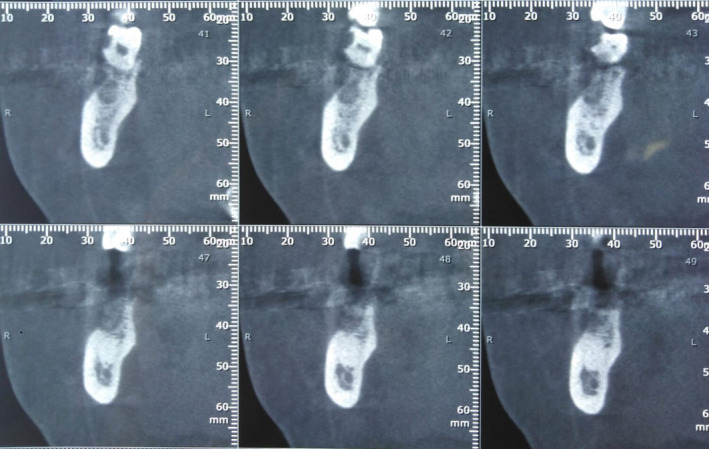
CBCT coronal sections of the site of tooth 47
The patient was informed of all the prosthetic solutions and the possible complications, and still requested an implant rehabilitation. An informed consent was signed prior to the procedure.
The implant surgery was performed in three steps to minimize the risk of infection:
1st stage: After local anesthesia, a crestal incision completed with two partial intra‐sulcular incisions on the adjacent teeth were performed. Then, a full‐thickness flap was elevated, and the drilling sequence was carried out. Afterward, tooth 48 was extracted because of dental decay, and the flap was repositioned and sutured. (Figures 3, 4, 5, 6, 7, 8).
FIGURE 3.
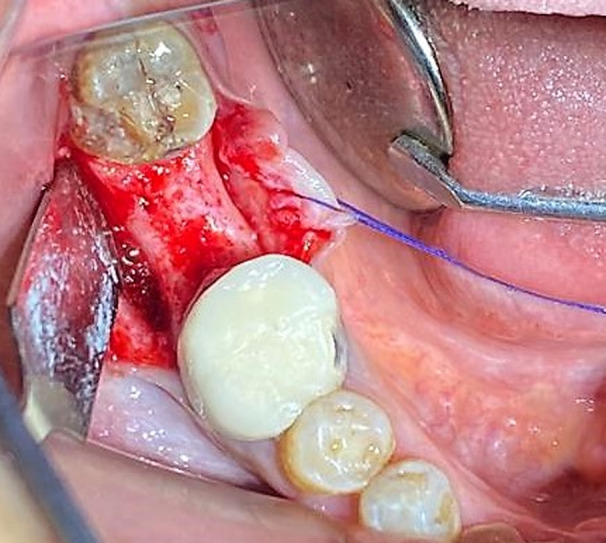
Full‐thickness flap elevation
FIGURE 4.
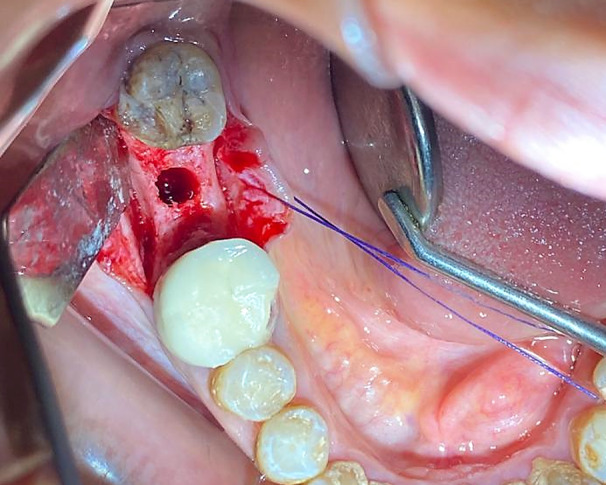
Drilling of the implant site
FIGURE 5.
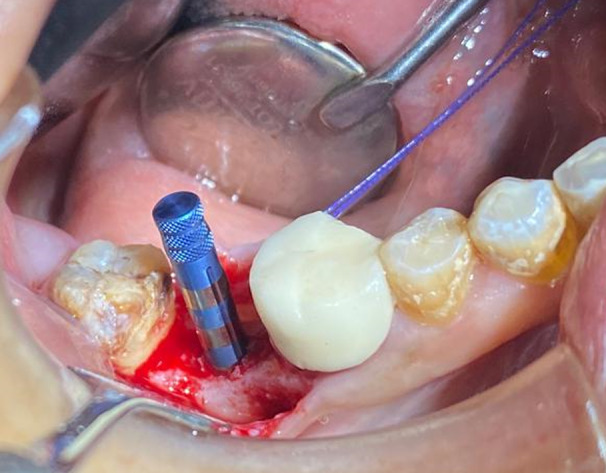
Use of a parallel guide to verify the axis
FIGURE 6.

Betadine wash
FIGURE 7.
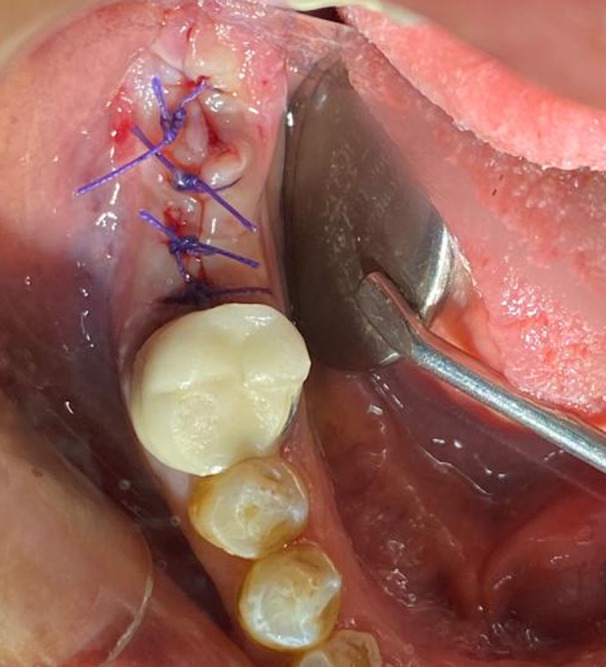
Extraction of tooth 48 and sutures
FIGURE 8.

Post‐operative retroalveolar radiography
Despite the prescription of an association of antibiotics (amoxicillin‐clavulanic acid) after the first surgery, the 7‐day check‐up revealed signs of infection such as pain and local swelling. The abscess was drained, and a betadine wash was performed to control the infection. (Figure 9).
FIGURE 9.

Infection of the site (7‐day follow‐up)
2nd stage: 3 weeks afterward: The flap was re‐opened, an implant (4.2 mm × 10 mm, Kontact®, Biotech dental) was placed into the prepared site and the cover screw was put in place. Finally, the flap was sutured. (Figures 10, 11, 12).
FIGURE 10.
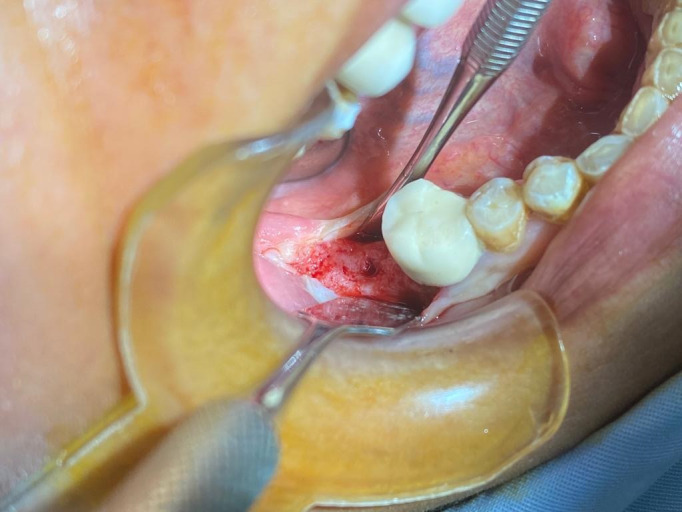
Elevation of a full‐thickness flap
FIGURE 11.
Implant placement
FIGURE 12.
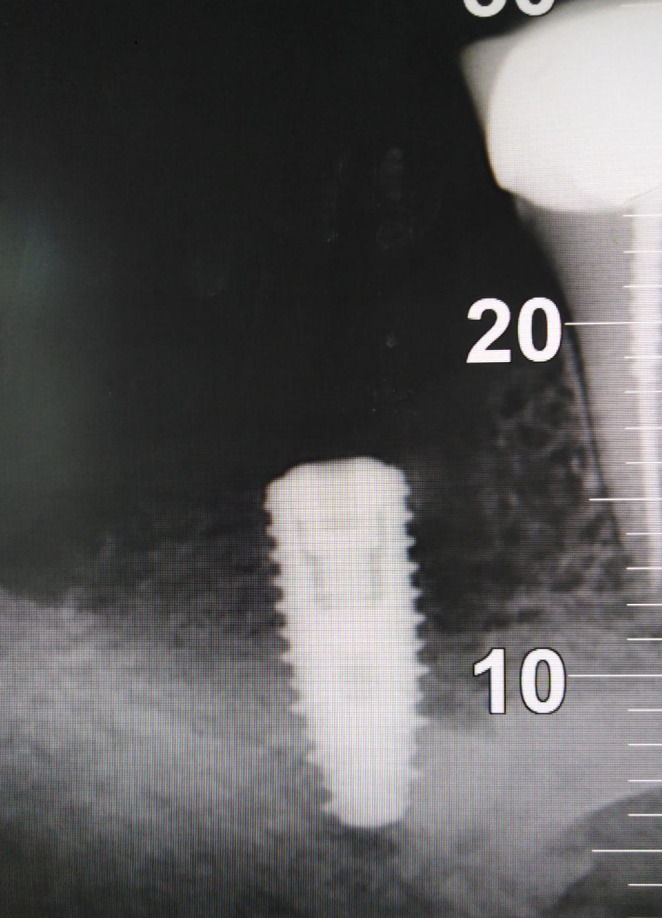
Post‐operative radiography
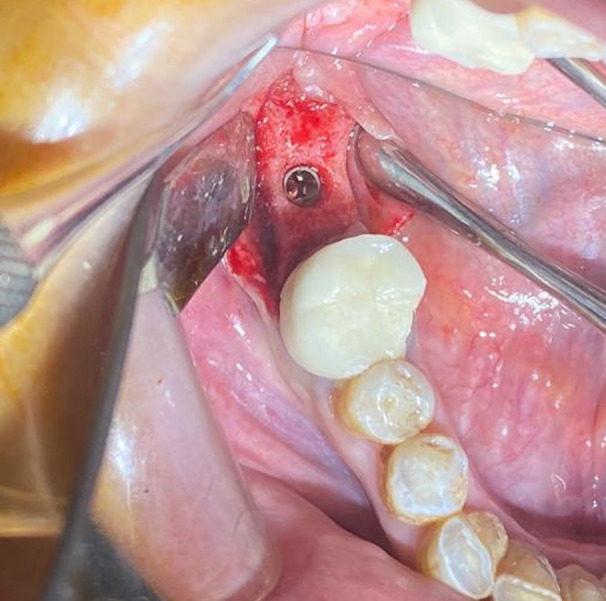
3rd stage: 3 months after the 2nd stage: The cover screw was replaced by the healing abutment. (Figure 13).
FIGURE 13.
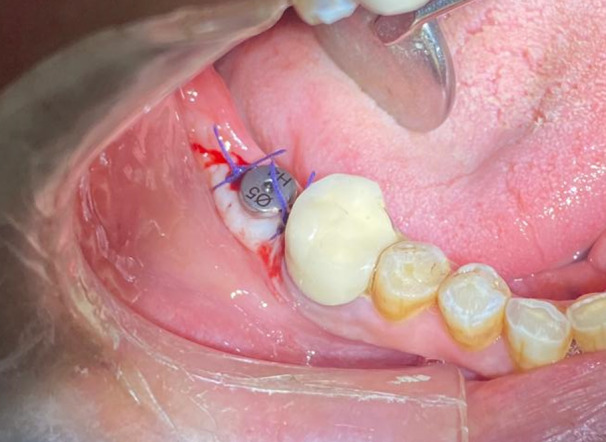
Placement of the healing abutment
3. DISCUSSION
3.1. Cemento‐osseous dysplasia
Cemento‐osseous dysplasia is a fibro‐osseous lesion characterized by a modification of the bone structure. Histologically, it appears as a cellular fibrous stroma with mineralizing tissues consisting of osteoid, bone, and cementum‐like material. The diagnosis requires a combined assessment of clinical and radiographic findings. 5 In its late stages, the lesion appears as a radiopaque lobulated calcified mass surrounded by a radiolucent margin. 4 The pathogenesis remains unknown.
The classification and terminology of these lesions are controversial and have drastically evolved over the years. 6 The latest World Health Organization (WHO) classification published in 2017 defined three categories of COD based on their anatomic location. In fact, COD lesions have periapical, focal, and florid variants.
Periapical COD (PCOD) mainly involves the periapical region of the anterior mandibular teeth, whereas focal COD (FocCOD) is usually located in the mandibular molar region, often in edentulous areas. Finally, the florid‐COD (FCOD) has more specific and distinct clinical and radiographic signs compared to the other two variants: It involves two or more jaw quadrants and is in most cases bilateral and symmetric. 7
Cemento‐osseous dysplasia mostly affects the middle‐aged African/African American women. In fact, a systematic review published in 2003 assessed 159 cases of FCOD; 59% occurred in blacks, 37% in Asians and 3% in Caucasians; 97% of all patients were female. 8
3.2. COD and implant therapy
In the presence of a COD, the general rule is to avoid any type of elective surgery such as extractions, periodontal surgery, or implant therapy. 4 Implant placement in these cases should only be performed after the patient has been informed of the risks and signed a consent form.
Literature treating the subject of implant rehabilitation with COD is quite poor. It has been suggested that implant placement in an affected site could induce osteomyelitis. In fact, overheating during the drilling sequence added to the lack of vascularization and the reduced capacity of bone regeneration would lead to infection and necrosis of the surrounding tissue. 9 Moreover, the lesion's response to antibiotics would be insufficient due to its avascular nature. 3
Shin et al. reported a case of chronic osteomyelitis induced by the placement of dental implants on COD. The implants failed to osseointegrate and were removed along with a sequestrum after an episode of swelling and pain. 10
Nevertheless, Park et al. described a case of successful osseotegration of an implant placed in a dysplastic site. The implant survived 15 years without any complication. However, at the 16‐year follow‐up, the implant was removed with a sclerotic mass due to peri‐implantatis. Histology showed that the hard mass attached to the implant was formed by a cementum‐like tissue (CLT) free of any soft tissue. The implant placed into the FCOD lesion achieved integration similar to that of conventional osseointegration. Rather than bone, the CLT was in direct contact with the titanium surface. The integrity of the union was maintained for up to 16 years. 11
To our knowledge, two case reports have described a successful implant rehabilitation on COD. Shadid et al. reported a successful implant rehabilitation of a lower posterior edentulous site in presence of a FCOD. Two implants were placed with strict infection control. This was achieved by prescribing prophylactic antibiotic (amoxicillin/clavulanic acid 500 mg/125 mg) 1 h before surgery and chlorhexidine mouthwash preoperatively and postoperatively, by ensuring sterile environment during the procedure, minimizing periosteal reflection, making the procedure as short as possible, and avoiding overheating of the bone using cool sterile saline and sharp drills. No complications have occurred after an 8‐year follow‐up. 12
Similarly, another case report described a successful implant rehabilitation of a posterior lower edentulism with an uneventful functional integration at the 18‐month follow‐up. 13
3.3. The proposed three‐stage protocol
The protocol used in our case report consists in dividing implant placement into three distinct surgeries:
-
‐
First stage: Drilling sequence with abundant cooling solution, betadine rinsing of the newly created socket, hermetic closure of the wound, and prescription of antibiotic therapy.
-
‐
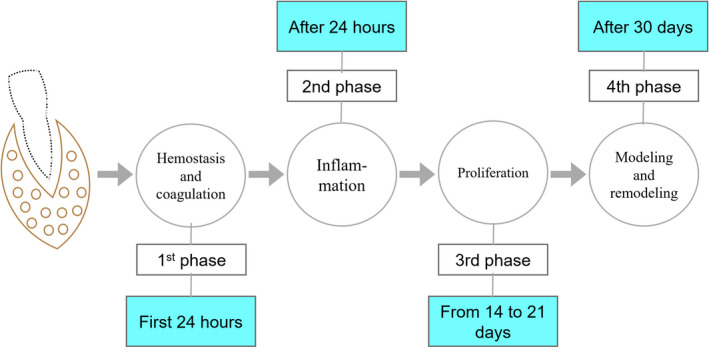
Second stage: Reopening of the site after 3 weeks (proliferation phase of the socket‐healing process) and implant placement.
-
‐
Third stage: Replacing the cover screw with the healing abutment after a healing period of 3 months.
The first surgery is undoubtedly the most risky; in fact, drilling through the dysplastic tissue generates heat which increases the risk of infection and necrosis of the surrounding tissue. Systematic antibiotherapy is highly advised in this stage to prevent such risks. In case it proved insufficient, infection must be treated with surgical curettage of the site, betadine rinsing, and the prescription of an antiseptic mouthwash.
Delaying implant insertion 3–4 weeks comes with two major advantages: first, preventing implant surface contamination in case of infection due to the drilling sequence, and second, the time lapse between the drilling sequence and implant placement matches the proliferation phase of the socket‐healing process characterized by the formation of a woven immature bone surrounded by a provisional fibrous matrix (Figure 14). 14 It has been hypothesized that this newly created healthy tissue surrounding the implant would act more like normal bone and would be more compatible with implant osseointegration than the cementum‐like tissue originally found in COD.
FIGURE 14.
Socket‐healing process
In addition, delaying the placement of the healing abutment is highly advised. In fact, exposing the implant to the oral cavity's flora simultaneously with its insertion increases the risk of infection. A 3‐month delay enables the surrounding hard tissue to reach a more mature state corresponding to the remodeling phase of the socket‐healing process. 14
4. CONCLUSION
Placing an implant in a site with COD comes with a high risk of infection. Patients must be informed of all the therapeutic options, and a consent form must be signed beforehand.
If implant rehabilitation is requested, our main concern is to minimize the risk of infection especially during and after the drilling sequence. The three‐stage protocol described in this paper proved to be successful in terms of preventing contamination of the implant surface even when infection occurs. Further clinical and histological studies must be carried out to further assess the benefits of this protocol.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interests regarding the publication of this paper.
AUTHOR CONTRIBUTIONS
Mootaz Mlouka ensured patient follow‐up and manuscript revision. Mohamed Tlili involved in surgery performance and manuscript revision. Faten Khanfir, Faten Ben Amor, and Mohamed Salah Khalfi contributed to manuscript revision. Ali Hamrouni involved in manuscript drafting.
ETHICAL APPROVAL
This manuscript is the authors' own original work, which has not been previously published or considered for publication elsewhere. The paper properly credits the meaningful contributions of co‐authors and co‐researchers. All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGEMENT
We sincerely thank Dr. Mohamed Tlili for the surgery performance and for his great help in the paper revision process.
Mlouka M, Tlili M, Khanfir F, Hamrouni A, Khalfi MS, Ben Amor F. Implant placement in a focal cemento‐osseous dysplasia: A modified protocol with a successful outcome. Clin Case Rep. 2022;10:e05307. doi: 10.1002/ccr3.5307
Funding information
This paper did not receive any special funding.
DATA AVAILABILITY STATEMENT
Data sharing not applicable – no new data generated.
REFERENCES
- 1. Pereira de Carvalho CH, Das Neves E, Dos Santos Pereira J, Costa de Medeiros AM, Dantas da Silveira ÉJ. Florid cemento‐osseous dysplasia and osteomyelitis: a case report of a simultaneous presentation. Rev OdontoCienc. 2012;27(2):166‐169. [Google Scholar]
- 2. Cavalcanti PH, Nascimento EH, Pontual ML, et al. Cemento‐osseous dysplasias: imaging features based on cone beam computed tomography scans. Braz Dent J. 2018;29:99‐104. [DOI] [PubMed] [Google Scholar]
- 3. Bencharit S, Schardt‐Sacco D, Zuniga JR, Minsley GE. Surgical and prosthodontic rehabilitation for a patient with aggressive florid cemento‐osseous dysplasia: a clinical report. J Prosthet Dent. 2003;90(3):220‐224. [DOI] [PubMed] [Google Scholar]
- 4. Gerlach RC, Dixon DR, Goksel T, Castle JT, Henry WA. Case presentation of florid cemento‐osseous dysplasia with concomitant cemento‐ossifying fibroma discovered during implant explantation. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(3):e44‐e52. [DOI] [PubMed] [Google Scholar]
- 5. El‐Mofty SK. Fibro‐osseous lesions of the craniofacial skeleton: an update. Head Neck Pathol. 2014;8:432‐444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Noffke CE, Raubenheimer EJ, MacDonald D. Fibro‐osseous disease: harmonizing terminology with biology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:388‐392. [DOI] [PubMed] [Google Scholar]
- 7. El‐Mofty SK, Nelson B, Toyosawa S, Wright J. Fibro‐osseous and osteochondromatous lesions. El‐Naggar CJKC, Grandis JR, Takata T, Slootweg PJ, ed. WHO classification of head and neck tumours. 4th edn. Lyon:IARC, 2017, 251‐255. [Google Scholar]
- 8. MacDonald‐Jankowski DS. Florid cemento‐osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2003;32:141‐149. [DOI] [PubMed] [Google Scholar]
- 9. Shnaiderman‐Shapiro A, Dayan D, Buchner A, Schwartz I, Yahalom R, Vered M. Histopathological spectrum of bone lesions associated with dental implant failure: osteomyelitis and beyond. Head Neck Pathol. 2015;9(1):140‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shin HS, Kim BC, Lim HJ, Jo SY, Lee J. Chronic osteomyelitis induced by the placement of dental implants on cemento‐osseous dysplasia. Br J Oral Maxillofac Surg. 2019;57(3):268‐270. [DOI] [PubMed] [Google Scholar]
- 11. Park WB, Han JY, Jang JS, et al. Longterm implant survivability of an implant having direct contact with cementumlike tissue in a preexisting mandibular intraosseous lesion with a 16‐year longitudinal follow‐up. Int J Periodontics Restorative Dent. 2019;39(6):895‐902. [DOI] [PubMed] [Google Scholar]
- 12. Shadid R, Kujan O. Success of dental implant osseointegration in a florid cemento‐osseous dysplasia: a case report with 8‐year follow‐up. Clin Pract. 2020;10(3):1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Esfahanizadeh N, Yousefi H. Successful implant placement in a case of florid cemento‐osseous dysplasia: a case report and literature review. J Oral Implantol. 2018;44(4):275‐279. [DOI] [PubMed] [Google Scholar]
- 14. de Sousa GP, Daugela P, Poskevicius L, Mariano L, Fernandes MH. Molecular and cellular aspects of socket healing in the absence and presence of graft materials and autologous platelet concentrates: a focused review. J Oral Maxillofac Res. 2019;10(3):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable – no new data generated.


