Abstract
Introduction
Situs inversus totalis represents an unusual anomaly characterized by a mirror-image transposition of the abdominal and thoracic viscera. It often occurs concomitantly with other disorders, hindering the diagnosis and management of abdominal pathology. The relationship between situs inversus totalis and cancer remains unclear.
Presentation of case
We describe a 79-year old Japanese female with situs inversus totalis who presented with obstructive jaundice. Imaging and endoscopic examinations showed a mass in the distal common bile duct, which was identified as an adenocarcinoma on biopsy. The patient was successfully treated by cephalic pancreaticoduodenectomy and the histological diagnosis was adenosquamous cell carcinoma. Ten months following surgery, the patient received chemotherapy and radiotherapy due to the presence of liver metastasis.
Discussion and conclusion
The occurrence of an adenosquamous carcinoma of the bile duct in a patient with situs inversus totalis is an extremely rare coincidence. In this setting, when the tumor is resectable, surgical management should be considered without contraindication and must be preceded by careful preoperative staging.
Keywords: Situs inversus totalis, Bile duct carcinoma, Surgical management, Adenosquamous carcinoma, Case report
Highlights
-
•
Situs inversus totalis (SIT) is a rare congenital condition characterized by a mirror-image transposition of both the abdominal and thoracic viscera.
-
•
The association of SIT with cancer of the common bile duct is a rare congenital malformation but presents no importance in relation to morbidity.
-
•
However, it may represent a difficulty when performing an operation.
-
•
This paper shows that the technique may be safely, speedily and effectively applied in the setting of SIT, although attention must be paid to the details of the left-to-right inversion, and to the anatomical assessment of the lesions, organs, and vessels.
1. Introduction
Situs inversus totalis (SIT) is a rare congenital condition characterized by a mirror-image transposition of both the abdominal and thoracic viscera, its incidence is of 1/8000 to 1/25,000 in the normal population [1]. This abnormality may cause difficulties in the diagnosis and therapeutic management of abdominal pathologies [2], [3]. An increased risk of cardiac, splenic, and hepatobiliary malformations is found in patients with SIT [4]. This condition is not considered to be a premalignant entity; however, rare malignant neoplasms have been reported. A case of successfully treated common bile duct adenosquamous carcinoma with SIT is described, in addition to a discussion of the literature. This paper has been reported in line with SCARE criteria [5].
2. Presentation of case
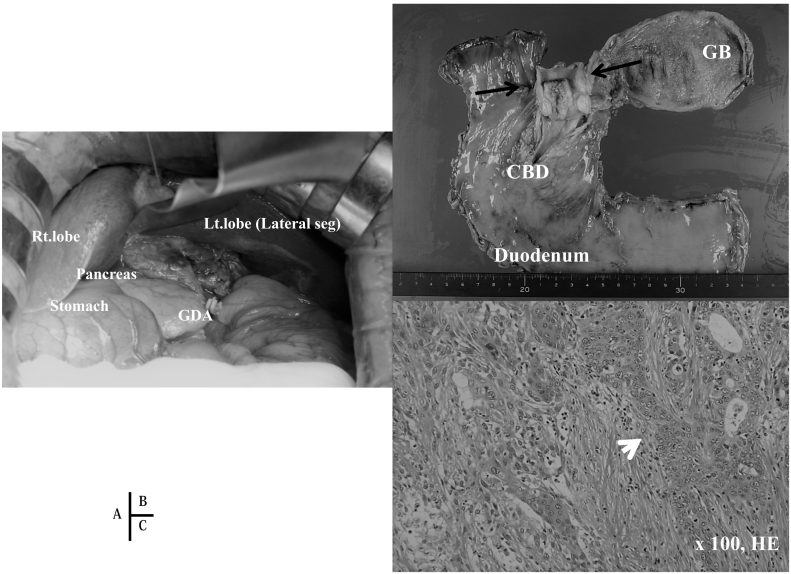
A 79-year-old previously healthy female with SIT presented with obstructive jaundice. Blood biochemical analysis evidenced liver dysfunction (total bilirubin 12.29 mg/dl, aspartate transaminase 289 IU/l, and alanine transaminase 337 IU/l), and biliary enzymes (alkaline phosphatase 1289 IU/l and ɤ-glutamyltransferase 927 IU/l) were increased. However, white blood cell count, C-reacitve protein, carcinoembryonic antigen and carbohydrate antigen 19–9 were within the normal ranges. Abdominal CT confirmed the complete transposition of viscera as follows: 1) dextrocardia; 2) left-sided liver, reversed superior vena cava and hepatic artery, and also revealed dilatation of the intra- and extra-hepatic bile ducts, secondary to stenosis of the distal common bile duct (CBD) (Fig. 1A and B). Magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangio- pancreatography (ERCP) confirmed tapered stricture of the CBD with upstream dilation of the bile ducts (Fig. 1C). Endoscopic ultrasound showed a 15 mm hypoechoic mass at the distal portion of the CBD, which biopsies identified as an adenocarcinoma. The preoperative staging evidenced no distant metastasis. We made her forecast figures which the position of the internal organs were the state of the reverse and the procedure before operation. After she displayed improvement of the cholangitis and jaundice using by stent for obstruction of the CBD (Fig. 1D), following an upper median laparotomy, she underwent operation. According to procedure during an operation, we taped each her vessels and were operated on while confirming each one organ, so she was successfully treated by pancreaticoduodenectomy with resection of lymph nodes, which were not found to be invaded by the tumor. Reconstruction was performed by Child's method. The procedure was evidently difficult and unusual due to the situs inversus (Fig. 2A), but there was no intraoperative complication (Table 1). Histopathological analysis of the specimen resection confirmed the diagnosis of carcinoma of the CBD, infiltrating the head of the pancreas (Fig. 2B), without metastatic lymph nodes in the retroportal lamina. The biliary, pancreatic, duodenal and retroperitoneal margins were also free of tumor. Histologically, the tumor consisted of an admixture of poorly differentiated adenocarcinoma and squamous cell carcinoma and was definitively diagnosed as adenosquamous carcinoma of the extrahepatic bile duct (Fig. 2C), classified as pT2N0M0 (stage II). The postoperative course was uneventful.
Fig. 1.
(A) Abdominal CT shows the stricture of the common bile duct with upstream dilation of the bile ducts. (B) Left-to-right reversal of the vascular arrangement with no vascular malformations. (C) ERCP confirms the stricture of the common bile duct (arrows), and the endoscopic view shows stent for stenosis of the distal common bile (D).
Fig. 2.
A shows intraoperative findings. Macroscopic view of the resected specimen shows the tumor of the common bile duct (B, arrows). (C) Histologically, this tumor presents the traditional findings of an adenocarcinoma and squamous cell carcinoma. The adenocarcinoma with a tubular pattern and the squamous cell carcinoma presented a transitional aspect (arrow) between both the squamous and adenocarcinoma components.
Table 1.
Surgical procedure and technique.
| 1. Preoperative: detective anatomical abnormalies associated SIT and prepare the plan for the pricedure. |
| 2. The right-handed surgeon stood on the right side of the patient |
| 3. To perform the mesenteric approach, the Kocher maneuver from left to right, the surgeon provided countertraction, and he first assitant mobilized the duodenum and the head of the pancreas. |
| 4. The major vessels were taped and identified as landmarks to avoid any errors, and the operation was performed in the same order as the standard procedure. |
| 5. To adequately suture the pancreatic duct to the jejunal mucosa for the pancreaticojejunostomy, the surgeon changed his position. |
| 6. Hepaticojejuostomy and gastroduodenostomy with Braun's anastomosis were performed asusual. |
The patient was healthy with no evidence of recurrence 10 months after surgical treatment, so complementary radiotherapy with concurrent chemotherapy, based on capecitabine, was administrated. However, unfortunately, she died 2 years after the operation due to the presence of liver metastasis.
3. Discussion
Situs inversus is the condition, in which there is a left-to-right mirror-image inversion of some or all of the internal organs relative to their normal positions. The condition is comparatively rare, being observed in 1 of 8000 to 25,000 people [1]. Situs inversus totalis is the, in which the positions of all the thoracic and abdominal organs are inverted, while situs inversus incompletus. Their ratio of incidence is said to be 6:1, situs inversus totalis is more frequent [1]. The following causes for the condition have been proposed: (1) the total organ transposition hypothesis, whereby the primordial positional arrangement of the major organs is disrupted at an early stage of embryonic development and this induces the inverted formation of other organs, (2) the non-uniform heating hypothesis, in which displacement occurs because part of the embryo is strongly heated, (3) the twin embryo hypothesis, given that organ inversion is often seen in conjoined twins, (4) the embryonic rotation hypothesis, which states that the condition is induced by the developing embryo turning in the opposite direction to normal, to the right, so that the yolk sac is to the right, (5) the genetic hypothesis, (6) the organizer hypothesis, but there is not yet an established theory [2], [3]. In the particular case, in which it occurs together with sinusitis and bronchiectasis, it is also termed Kartagener syndrome [6]; however, these complications were not present in our case.
Situs inversus, itself, has no pathological significance; clinically, the problem is that there are often complicating deformities, e.g. in the cardiovascular and the digestive systems. Furthermore, the inversion complicates diagnosis and surgical procedures. It is claimed that complicating vascular defects occur in 8–10% of cases, which is circa 10 times the incidence when compared to normal subjects [4]. Complicating digestive tract defects such as intestinal malrotation, congenital biliary atresia, preduodenal portal vein, duodenal atresia, polysplenia, annular pancreas, and diaphragmatic hernia have been reported [4]. However, the frequency of other complicating defects appears to be lower with situs inversus totalis than with situs inversus incompletus. As for surgical complications, besides the very defects, attention has been drawn to an increase in reported cases of appendicitis, biliary calculus, and, in recent years, malignant disorders [6]. When treating complicating malignant tumors, surgical procedures are often performed as the standard treatments for cancer, i.e. as in the case of normal anatomy [7], [8].
Among the reports malignant disorders in patients presenting situs inversus, cases of digestive tract cancers are particularly frequent, but the causal relationship is yet unclear [9]. Many of these reports are of gastric cancer, but there are few studies describing this condition associated with bile duct cancer. So far, there have only been 6 such cases reported, including our own case [10], [11], [12], [13], [14], [15], [16] (Table 2). In all the cases, pancreaticoduodenectomy was performed. The surgical procedure applied in these cases was conventional pancreaticobiliary resection and reconstruction with simultaneous hepatic resection. However, deformities of the vascular system and/or the biliary system, and especially many arterial abnormalities have been identified in patients with this condition [9], [10], [11], [12], [13], [14], [15], [16]. Many variations have been reported in the coeliac artery and superior mesenteric artery system. Preoperative confirmation of their pathways by abdominal angiography is very important [17]. Nevertheless, advances in imaging diagnosis in recent years have made angiography unnecessary; alternatively, a picture of the vasculature may be constructed by using MRI or multidimensional CT (MDCT) [18]. In our case, various imaging techniques were used, but no anomalies were noted.
Table 2.
Reports of bile duct carcinoma in patients with situs inversus totalis.
| Author | Year | Age/sex | Location | Treatment | Blood loss (ml) | Operation time (min) |
|---|---|---|---|---|---|---|
| Bilimora [9] | 2001 | 44/F | AV | PD | NA | NA |
| Sano [10] | 2003 | 76/F | BD | HB | NA | NA |
| Tsunoda [11] | 2006 | 65/M | BD | PD | 1596 | 522 |
| Kyuno [13] | 2011 | 74/M | BD | PD | 600 | 564 |
| Kyuno [13] | 2011 | 67/M | BD | PD | 350 | 659 |
| Benhammane [14] | 2012 | 33/M | BD | PD | NA | NA |
| Yagi [15] | 2017 | 33/M | BD | PD | 1283 | 447 |
| Present case | 2021 | 77/F | BD | PD | 120 | 525 |
BD: bile duct, AV: ampulla of Vaer, PD: pancreaticoduodenectomy, SSPPD: subtotal stomach preserving pancreaticoduodenectomy, HB: extended rt.hepatic-lobectomy with resection of BD, NA: not available.
There are controversies regarding issues such as whether the surgeons should stand on the right or left side during surgery [18], [19]. We stood on the right side, as usual. Although the fact that the position of the organs is inverted was unusual, generally, there was no sense of inconvenience. We think standing in the normal position made it slightly easier for the surgeons to perform the procedure in the usual way.
The histopathological diagnosis was of adenosquamous cell carcinoma. Adenosquamous cell carcinomas are rare, accounting for only about 0.68–5.5% [19], [20], [21], [22], [23] of bile duct carcinomas; and there are no reports of bile duct carcinoma as a complication of situs inversus - our case is the first. In general, primary biliary adenosquamous cell carcinoma is known to be a cancer with higher histological malignancy when compared to other adenocarcinomas. There are various contributing factors, but pancreatic infiltration, lymph node metastasis, and poor curability are cited as adverse factors regarding pathomorphological prognosis [21], [22]. Another measure for evaluating malignancy is tumor growth potential. Squamous cancers grow twice as fast as adenocarcinomas; therefore, when an adenocarcinoma transforms into an adenosquamous carcinoma, malignancy becomes greater. Tumor growth potential and degree of malignancy are closely linked [22], [23]. Despite the realization of radical surgery, the prognosis is poor, with the one-year survival rate of 57%, the 3-year survival rate of 26%, the 5-year survival rate of 16%, and median 13 months. We also performed radical surgery in the present case, and although the degree of progression was stage II, in a mere 6 months metastatic recurrence was noted in the liver, which is thought to have been affected by the degree of histological malignancy.
Taking all into consideration, it is our opinion that when operating patients presenting situs inversus, while anatomical considerations may be expected to affect the procedure, there is no need to avoid surgical treatment because of the situs inversus. Our own case died 2 years after surgery, but the death was attributed to the histological malignancy, not to the surgical procedure.
4. Conclusion
The association of situs inversus totalis with cancer of the common bile duct is a rare congenital malformation but presents no importance in relation to morbidity. However, it may represent a difficulty when performing an operation. This paper shows that the technique may be safely, speedily and effectively applied in the setting of SIT, although attention must be paid to the details of the left-to-right inversion, and to the anatomical assessment of the lesions, organs, and vessels.
List of abbreviations
- SIT
situs inversus totalis
- T-Bil
total bilirubin
- AST
aspartate transaminase
- ALT
alanine transaminase
- ALP
alkaline phosphatase
- ɤ-GTP
ɤ-glutamyltransferase
- WBC
white blood cell count
- CRP
C-reactive protein
- CEA
carcinoembryonic antigen
- CT
computed tomography
- MRCP
magnetic resonance cholangiopancreatography
- ERCP
endoscopic retrograde cholangiopancreatography
- CBD
common bile duct
- PD
pancreaticoduodenectomy
Sources of funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written informed consent is available for review by the Editor-in-Chief of this journal.
Guarantor
Yoshito Wada, MD., PhD.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Y Wada, S Taniwaki and H Soh performed the operations. Y Wada, S and H Terabe managed the postoperative intensive care. All authors conceived the study and participated in its design and coordination. T Imamura supervised the study and drafted the manuscript. Y Morimitsu contributed to the pathological diagnosis. All authors declare that the paper is being submitted for consideration for publication in Journal of Medical Case Reports, that the content has not been published or submitted for publication elsewhere. All authors read and approved the final manuscript.
Declaration of competing interest
The authors have no conflict of interest.
Acknowledgments
Acknowledgement
We would like to thank Editage (www.editage.jp) for English language editing.
Contributor Information
Yoshito Wada, Email: yo-wada@kyoaikai.com.
Satoshi Taniwaki, Email: taniwaki@kyoaikai.com.
Hironobu So, Email: hi-sou@kyoaikai.com.
Tetsuo Imamura, Email: te-imamura@kyoaikai.com.
References
- 1.Lee S.E., Kim H.Y., Jung S.E., Lee S.C., Park K.W., Kim W.K. Situs anomalies and gastrointestinal abnormalities. J. Pediatr. Surg. 2006;41:1237–1242. doi: 10.1016/j.jpedsurg.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 2.Uemura S., Maeda H., Munekage M., Yoshioka R., Okabayashi T., Hanazaki K. Hepatic resection for metastatic colon cancer in patients with situs inversus totalis complicated by multiple anomalies of the hepatobiliary system: the first case report. J. Gastrointest. Surg. 2009;13:1724–1727. doi: 10.1007/s11605-009-0909-4. [DOI] [PubMed] [Google Scholar]
- 3.Blegen H.M. Surgery in situs inversus. Ann. Surg. 1949;129:244–259. doi: 10.1097/00000658-194902000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fonkalsrud E.W., Tompkins R., Clatworthy H.W., Jr. Abdominal manifestations of situs inversus in infants and children. Arch. Surg. 1966;92:791–795. doi: 10.1001/archsurg.1966.01320230139025. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline:updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Kobus C., Targarona E.M., Bendahan G.E., Alonso V., Balague C., Vela S., Garriga J., Trias M. Laparoscopic surgery in situs inversus: a literature review and a report of laparoscopic sigmoidectomy for diverticulitis in situs inversus. Langenbeck's Arch. Surg. 2004;389:396–399. doi: 10.1007/s00423-004-0500-0. [DOI] [PubMed] [Google Scholar]
- 7.Maekawa T. Dextrocardia, report of five autopsy cases, with special reference to hereditary. Aichi Igakkai Zasshi. 1927;34:481–493. [Google Scholar]
- 8.Kim Y.W., Ryu H., Kim D.S., Kim I.Y. Double primary malignancies associated with colon cancer in patients with situs inversus totalis: two case reports. World J. Surg. Oncol. 2011;23(suppl 9):109. doi: 10.1186/1477-7819-9-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haruki T., Maeta Y., Nakamura S. Advanced cancer with situs inversus totalis associated with KIF3 complex deficiency: report of two cases. Surg. Today. 2010;40(suppl 2):162–166. doi: 10.1007/s00595-009-4005-x. [DOI] [PubMed] [Google Scholar]
- 10.Bilimoria M.M., Parsons W.G., Small W., Jr., Talamonti M.S. Pancreaticoduodenectomy in a patient with ampullary carcinoma and situs inversus. Surgery. 2001;130:521–524. doi: 10.1067/msy.2001.113377. [DOI] [PubMed] [Google Scholar]
- 11.Sano T., Kamiya J., Nagino M., Kanai M., Uesaka K., Nimura Y. Hepatectomy for proximal bile duct carcinoma in a patient with situs inversus: a case report. Hepatogastroenterology. 2003;50(suppl 53):1266–1268. [PubMed] [Google Scholar]
- 12.Tsunoda S., Miyashita T., Murata M. Pancreaticoduodenectomy for common bile duct cancer in a patient with situs inversus totalis: a case report. Int. Surg. 2006;91:24–27. [PubMed] [Google Scholar]
- 13.Macafee D.A., Armstrong D., Hall R.I., Dhingsa R., Zaitoun A.M., Lobo D.N. Pancreaticoduodenectomy with a “twist”: the challenges of pancreatic resection in the presence of situs inversus totalis and situs ambiguus. Eur. J. Surg. Oncol. 2007;33:524–527. doi: 10.1016/j.ejso.2006.09.029. [DOI] [PubMed] [Google Scholar]
- 14.Kyuno D., Kimura Y., Imamura M., Uchiyama M., Ishii M., Meguro M., Kawamoto M., Mizuguchi T., Hirata K. Pancreaticoduodenectomy for biliary tract carcinoma in a patient with situs inversus totalis: difficulties and technical notes based on two cases. World J. Surg. Oncol. 2011;11:312. doi: 10.1186/1477-7819-11-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benhammane H., Kharmoum S., Terraz S., Berney T., Nguyen-Tang T., Genevay M., El Mesbahi O., Roth A. Common bile duct adenocarcinoma in a patient with situs inversus totalis: report of a rare case. BMC Res. Notes. 2012;5:681. doi: 10.1186/1756-0500-5-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yagi N., Arakawa K., Ando T., Tominaga N., Shimizu N., et al. A case report of duodenal papillary carcinoma with situs inversus totalis and anomalies with pancreaticoduodenectomy. J. Clin. Surg. 2017;72:1509–1514. (in Japanese) [Google Scholar]
- 17.Wada Y., Hayashida K., Edakuni S. Situs inversus totalis with a colonic cancer -a case report. J. Jpn. Surg. Assoc. 1998;59:2344–2347. (in Japanese) [Google Scholar]
- 18.Fletcher J.G., Wiersema M.J., Farrell M.A., Fidler J.L., Burgart L.J., Koyama T., Johnson C.D., Stephens D.H., Ward E.M., Harmsen W.S. Pancreatic malignancy: value of arterial, pancreatic, and hepatic phase imaging with multi-detector row CT. Radiology. 2003;229:81–90. doi: 10.1148/radiol.2291020582. [DOI] [PubMed] [Google Scholar]
- 19.Albores-Saavedra J., Henson D.E., Klimstra D.S. Atlas of Tumor Pathology. 3rd Series. Fascicle 20. Armed Forces Institute of Pathology; Washington DC: 1997. Tumors of the gallbladder, extrahepatic bile ducts, and ampulla of Vater; pp. 195–215. [Google Scholar]
- 20.Okabayashi T., Kobayashi M., Nishimori I., et al. Adenosquamous carcinoma of the extrahepatic biliary tract: clinicopathological analysis of japanese cases of this uncommon disease. J. Gastroenterol. 2005;40:192–199. doi: 10.1007/s00535-004-1520-9. [DOI] [PubMed] [Google Scholar]
- 21.Hong Seung-Mo, Kim Mi-Jung, Jang Kee-Taek, Yoon Ghil-Suk, Cho HyungJun, Frierson Henry F., Jr., Yu Eunsil., Jr. Adenosquamous carcinoma of extrahepatic bile duct: clinicopathologic study of 12 cases. Int. J. Clin. Exp. Pathol. 2008:147–156. [PMC free article] [PubMed] [Google Scholar]
- 22.Lim Sin Hyung, Yang Hyeon Woong, Kim Anna, Cha Sang Woo, Jung Sung Hee, Go Hoon, Lee Woong Chul. Adenosquamous carcinoma of extrahepatic bile duct: a case report. Korean J. Intern. Med. 2007;22:206–210. doi: 10.3904/kjim.2007.22.3.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naito Yoshiki, Higaki Koichi, Tanaka Masaya, Taniwaki Satoshi, Kojiro Masamichi. A case of adenosquamous carcinoma of the extrahepatic bile duct. Jpn. J. Gastroenterol. Surg. 2007;40:629–633. (in Japanese) [Google Scholar]