Abstract
Background
Generalized pustular psoriasis (GPP) is a rare disease characterized by episodic worsening (flares). Knowledge of the burden of GPP and the experience of affected individuals is limited.
Aims
To conduct a survey of people living with GPP to understand how they experience GPP flares, which therapies they have received and are receiving, and how GPP impacts their activities of daily living.
Methods
The online survey consisted of 43 questions answered by individuals recruited from an opt-in market research database. The research team performed a targeted outreach to identify individuals with GPP. The survey included screening questions to determine if potential participants qualified for inclusion. Eligible individuals were US residents aged ≥ 18 years who self-reported that they had been diagnosed with GPP. Respondents provided consent to participate and received compensation (fair market value) for their time.
Results
Between August 4 and 14, 2020, 66 people living with GPP in the USA were surveyed. Most participants were female, aged 40–59 years, had been diagnosed ≥ 1 year previously, and had experienced ≥ 2 flares in the past year. A substantial proportion of respondents had symptoms for years, had consulted multiple healthcare professionals, and experienced misdiagnoses before receiving a diagnosis of GPP. Emotional stress was the most common cause of flares and many respondents reported a fear of flares. Respondents defined flares by the presence of itching, an increase in the size of the affected area, more crusts or pustules, and fatigue. A change in mood was the most burdensome symptom. Most respondents were receiving topical corticosteroids and only approximately one-third felt their condition was well controlled. GPP had an impact on activities of daily living even in the absence of flares and many respondents felt that their physician did not understand the level of emotional, psychological, or physical pain caused by GPP.
Conclusions
GPP imposes a substantial emotional burden on patients, with wide-ranging impacts on activities of daily living beyond the physical discomfort of skin lesions.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40257-021-00663-y.
| Digital Features for this article can be found at 10.6084/m9.figshare.16823503. |
Key Points
| Generalized pustular psoriasis (GPP) is under-recognized and individuals with the condition are often undiagnosed for years. |
| Respondents defined disease worsening as episodes of flares; they defined flares by the presence of itching, an increase in the size of the affected area, more crusts or pustules, and fatigue. A change in mood was reported as the most burdensome symptom. |
| Individuals living with GPP experience a substantial emotional and physical burden that impacts their ability to perform activities of daily living. |
Introduction
Generalized pustular psoriasis (GPP) is a rare, chronic, and potentially life-threatening neutrophilic skin disease characterized by the presence of sterile pustules. Although GPP is distinct from plaque psoriasis, they can occur concurrently and with or without systemic inflammation [1]. The clinical course of GPP is characterized by episodic worsening (flares), during which sterile pustules become more widespread [1]. The severity of flares varies between individuals [1].
Knowledge of the burden of GPP and the experience of affected individuals is limited. We conducted a survey of people living with GPP in 2020 to better understand how they experience GPP flares, how GPP impacts their activities of daily living, and which therapies they have received and are receiving.
Participants and Methods
How was the Survey Conducted?
The survey was developed by three of the authors (NK, SB, WV) in collaboration with HealthiVibe, a division of CorEvitas, LLC (Arlington, VA, USA); HealthiVibe also administered the survey. A virtual focus group comprising eight women and one man with GPP was conducted on June 23 and 24, 2020. The moderator asked open-ended questions to gain insights to inform questions included in an online survey; these insights are not described in this manuscript. Four participants had completed post-graduate studies, three had bachelor’s degrees, and two had completed training at a trade school; all participants received US$250.00 as compensation (fair market value) for their time.
The resulting online survey consisted of 43 questions (Supplementary Information). Individuals were recruited from an opt-in market research database of over 10 million consumers in the USA; this provided a sample of individuals who had previously opted-in to participate in market research that is representative of the general population. The research team performed a targeted outreach to identify individuals with GPP. The survey was designed to include screening questions to determine if potential participants qualified for inclusion; eligible individuals were US residents aged ≥ 18 years who had been diagnosed with GPP. Respondents had to sign a consent form prior to completing the survey and received US$25.00 as compensation (fair market value) for their time. A survey link was provided to respondents interested in taking the online survey.
The survey results, which are the subject of this report, were summarized descriptively by HealthiVibe in collaboration with three authors (NK, SB, WV) and interpreted by these same three authors, together with a person living with GPP (DR), a physician (KE), and a representative (FDJ) from a global patient organization (International Federation of Psoriasis Associations [IFPA]) that supports people living with psoriatic disease. The latter three authors (DR, KE, FDJ) provided the context for these data using their perspectives.
No formal statistical analysis was planned or conducted. The data are described descriptively.
Results
The survey was completed between August 4 and 14, 2020 by 66 people living with GPP.
Who were the Survey Participants?
Most of the survey participants were women (80%), aged 40–59 years (62%), and had been diagnosed with GPP at least 1 year previously (96%; Table 1). Prior to the COVID-19 pandemic, approximately half of survey participants were working (48%) and approximately one-quarter identified as disabled (27%; Table 1).
Table 1.
Demographics and baseline characteristics of survey participants
| Characteristic | Proportion of participants, n (%) |
|---|---|
| Gender | |
| Female | 53 (80.3) |
| Male | 13 (19.7) |
| Age, years | |
| 18–39 | 15 (22.7) |
| 40–59 | 41 (62.1) |
| ≥ 60 | 10 (15.2) |
| Time since GPP diagnosis, years | |
| < 1 | 3 (4.5) |
| 1–10 | 36 (54.5) |
| > 10 | 27 (40.9) |
| Employment status prior to the COVID-19 pandemic | |
| Working | 32 (48.5) |
| Not working due to disability | 18 (27.3) |
| Not working due to other reasons | 16 (24.2) |
| Self-reported comorbid conditions | |
| GPP | 66 (100) |
| Plaque psoriasis | 46 (69.7) |
| Arthritis | 33 (50.0) |
| Depression | 28 (42.4) |
| Generalized anxiety disorder | 24 (36.4) |
| Obesity | 21 (31.8) |
| Hypertension | 20 (30.3) |
| Diabetes (type 1 or 2) | 17 (25.7) |
| Asthma | 11 (16.7) |
| Chronic obstructive pulmonary disease | 9 (13.6) |
| Heart disease | 2 (3.0) |
| Other | 6 (9.1) |
GPP generalized pustular psoriasis
How did the Survey Participants Describe Their Journey to a GPP Diagnosis?
Many survey participants reported that they had experienced a delay before being diagnosed with GPP. For example, 36% reported living with symptoms for months and 38% reported living with symptoms for years before receiving a GPP diagnosis. The common reasons cited by respondents for the delay were misdiagnosis (59%) and having to visit multiple healthcare professionals and/or specialists before a diagnosis was made (51%). Affordability of healthcare or lack of medical insurance (37%) and lack of access to specialists (18%) were also cited as reasons for the delay in receiving a GPP diagnosis. Survey participants reported receiving a GPP diagnosis from a dermatologist (68%), rheumatologist (18%), or primary care physician (14%).
How did the Survey Participants Describe Worsening GPP (Flares)?
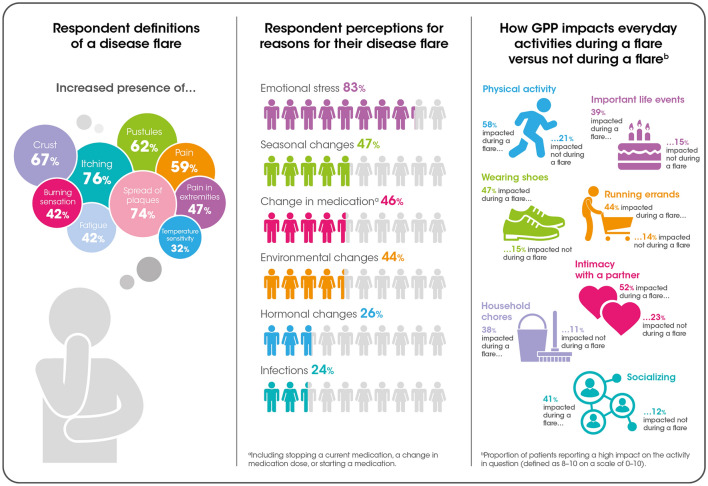
All respondents reported experiencing at least one episode of worsening GPP (flares) in the past 12 months, and most (86%) had experienced at least two flares in the past 12 months. The top three factors to which survey participants attributed flares were emotional distress (83%), seasonal changes (47%), and medication changes (46%). Infections (24%) and stopping (21%), starting (11%), or changing the dose of a medication (14%) were less commonly cited as a trigger for flares (Fig. 1).
Fig. 1.
Patient experience of GPP flares. N = 66. GPP generalized pustular psoriasis
Respondents defined flares by the presence of itching (76%), an increase in the size of the affected area (74%), more crusts (67%) or pustules (62%), and/or fatigue (42%; Fig. 1). When asked to reflect on the symptoms experienced during a flare, changes in mood (1), pain (2), and fever (3) were ranked the highest. The most prominent among these was changes in mood, the burden of which was described as high (8–10 on a scale of 0–10) by 57% of respondents and medium (5–7) by 43% of respondents. The burden imposed by pain was described as high by 74% of respondents and medium by 26% of respondents.
In total, 59% of participants reported that pain was associated with flares. A general increase in pain was reported by 45% of respondents, increased pain in the hands, arms, feet, or toes was reported by 47% of respondents, and a burning sensation was reported by 42% of respondents. Consistent with the finding that emotional distress was the most cited cause of flares, the majority of survey participants reported feelings of fear and anxiety about GPP (67%), with 71% reporting a fear of flares, 65% worrying that their current medication would stop working, 59% reporting that GPP was accompanied by feelings of hopelessness and depression, and 56% worrying that their condition would become more severe with age.
How did the Survey Participants Describe the Severity of Their GPP?
The survey participants were asked to reflect on the severity of their symptoms when GPP was under control and during flares. When their condition was under control, approximately half of the respondents (52%) reported that they had few or no symptoms and 42% reported that they were able to engage in activities that they enjoy. In addition, a substantial proportion of participants reported having symptoms that did not cause pain or discomfort (39%) or that were accompanied by minimal pain (38%) when their GPP was under control.
Most survey participants (70%) reported that their symptoms were of low severity when GPP was under control, defined as 0–4 on a scale of 0 (no impact) to 10 (highest possible impact). Of note, 24% of respondents reported their symptoms were of moderate severity (5–7) and 6% reported high severity (8–10) when GPP was under control. In contrast, during flares, most survey participants (76%) described the severity of their symptoms as high and 6% described the severity as low.
How did the Survey Participants Describe the Effect of GPP on Activities of Daily Living?
Many survey participants reported that GPP interfered with activities of daily living during flares as well as when they were not experiencing symptoms (Fig. 1). During flares, approximately half of respondents reported that GPP had a high impact (defined as 8–10 on a scale of 0–10) on their ability to exercise (58%), to be intimate with a spouse or partner (52%), to wear shoes (47%), to complete errands (44%), or to socialize with family, friends, or neighbors (41%). When not experiencing symptoms, up to one-quarter of respondents reported that GPP had a high impact on their ability to be intimate with a spouse or partner (23%), to exercise (21%), to attend important life events (15%), or to wear shoes (15%).
What Treatments had the Survey Participants Received for GPP?
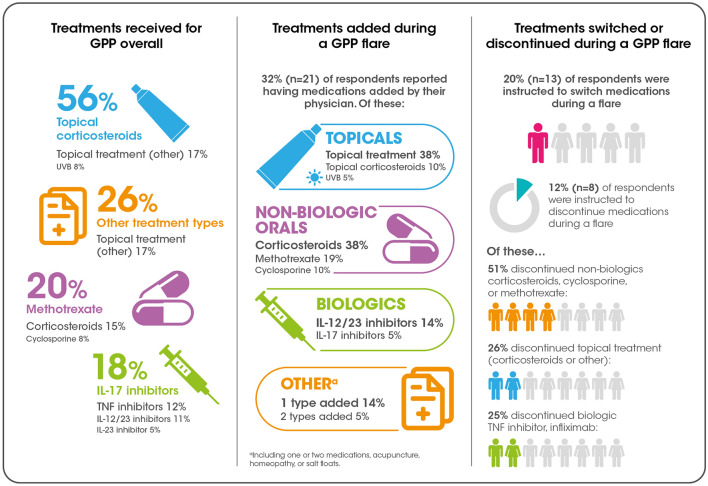
The survey participants were asked to describe their treatment history for GPP, the effectiveness of their current regimen, and how their regimen may have been modified during a flare. Most respondents (56%) reported that they were currently receiving topical corticosteroids (Fig. 2). In addition, 20% were currently receiving methotrexate, 18% were receiving an interleukin (IL)-17 inhibitor, 12% were receiving a tumor necrosis factor (TNF) inhibitor, 11% were receiving an IL-12/23 inhibitor, and 5% were receiving an IL-23 inhibitor.
Fig. 2.
Treatment patterns for GPP overall and during a flare. N = 66. GPP generalized pustular psoriasis, IL interleukin, TNF tumor necrosis factor, UVB ultraviolet B
Only approximately one-third of survey participants (32%) felt their condition was well controlled by their current treatment (defined as 8–10 on a scale of 0–10). Less than half of survey participants (45%) felt that their condition was moderately-well controlled (5–7) and 23% felt their condition was poorly controlled (0–4) by their current treatment.
When reflecting on treatment during flares, most survey participants (80%) reported that their physician instructed them not to switch medications and approximately one-third (32%) reported receiving additional medications, the most common of which were oral corticosteroids and other topical treatments (38% for each; Fig. 2).
How did the Survey Participants Perceive Their Relationship with Their Physician?
When asked to reflect on their relationship with their healthcare provider, most participants reported being comfortable asking questions about GPP (86%) and felt that they understood their diagnosis (89%). Similarly, most respondents felt that their physician provided them with up-to-date information about GPP (77%) and knew how best to treat their disease (68%). In contrast, approximately half of the respondents felt that their physician did not understand the level of emotional or psychological pain (47%) and/or the level of physical pain (50%) that GPP was causing them, and 17% felt that their physician did not know how best to treat their disease (15% of participants reported feeling neutral in this regard).
Discussion
The results of this online survey of people living with GPP provide important insights into the journey to a diagnosis of GPP, how these individuals experience GPP, including the impact of the condition on activities of daily living, and their engagement with healthcare providers. The survey participants are representative of people living with GPP in that the majority were women and older than 40 years of age [2, 3]. It is noteworthy that approximately one-quarter of participants self-identified as disabled, further corroborating the high impact that GPP has on the quality of life (QoL) of individuals living with the condition. The video accompanying this article (available online) presents the thoughts of a patient and a representative from IFPA on the impact of living with GPP, and how the results of this survey can help advocacy groups support individuals living with GPP, as well as their healthcare providers.
Video 1 Patient and advocate perspectives (MP4 65427 kb)
An important insight is how people living with GPP describe their condition when their symptoms are under control. For many individuals, control of GPP does not mean the absence of symptoms. Rather, the presence of symptoms is a constant in their life. A substantial proportion of survey respondents reported experiencing moderate or severe pain when they considered their condition to be under control. Although not explored in this survey, an individual’s perception of disease control may change with the time since diagnosis or the duration of a flare. Over time, individuals with GPP have learned to live with a new concept of well-being; those who are newly diagnosed or less experienced may define control of their condition differently than those who have lived with GPP for a long time.
GPP takes an emotional toll on people living with the condition. According to the survey results, the most common cause of a flare was emotional stress and the most burdensome symptom associated with worsening GPP was changes in mood. In addition, people living with GPP reported that GPP impacts their ability to attend important life events, socialize with friends or family, or be intimate with a spouse or partner. A person living with GPP may also experience stigma when their condition becomes more obvious to others [4]. For example, people may be reluctant to shake hands with a person who has prominent GPP lesions. Greater effort is needed to reduce stigma, for example, by raising awareness in society that GPP is not a contagious condition. Having a supportive family or friends is paramount to the QoL of a person experiencing a flare, as family members and friends are often the people who can see past the physical manifestations of the condition. Family and friends can also become overwhelmed by caring for someone with a chronic condition. Patient advocacy organizations and support groups have an important role in providing support for all individuals affected by GPP.
Infections were also identified as a trigger for flares by study participants but were much less prominent than emotional stress. Infections are generally considered to be important precipitants of GPP flares [5, 6], and viral infections of the upper respiratory tract have recently been implicated in triggering flares [7]. This difference between patient perceptions and the medical literature may provide insights into what individuals living with GPP consider important to their QoL.
GPP affects all aspects of a person’s daily life. Pain and discomfort are prominent during flares and may interfere with an individual’s ability to participate in physical or social activities. These findings suggest that people living with GPP may benefit from comprehensive multidisciplinary care that includes emotional support as part of their treatment plan, especially during flares.
The survey provides insights into the relationship between people living with GPP and their clinicians. Those living with GPP often persevere for months or years before receiving a diagnosis because it is a rare disease that is not frequently encountered or readily diagnosed by primary healthcare providers. Delays in diagnosis may negatively affect perceptions of the medical profession and are just one of many factors that may decrease trust in healthcare providers. Several participants did not feel supported by their physician and a minority felt that their physician did not know how best to treat their GPP. It is not clear from the survey results whether these individuals had experienced delays in diagnosis or whether they were cared for by a primary care physician, a dermatologist, or other specialist. There may be a mismatch between how physicians and their patients define disease severity and/or treatment outcomes. For example, a decrease in the size of the affected area may be seen as a successful treatment outcome by a physician. However, this may not be perceived as a treatment success by a person who continues to experience physical discomfort or psychological distress.
Although there are several therapeutic approaches for GPP, the fact that survey participants reported receiving a wide range of treatments for GPP underscores the fact that this condition still has no standardized treatment regimen. Participants identified changes to their medication regimen as a precipitant of flares. This is not surprising given that withdrawal of corticosteroids is a prominent cause of flares cited in the literature [6, 8]. In addition, a small number of participants reported being instructed to stop medications during flares; however, it is not possible to state whether instructions to discontinue medications were prompted by the perception that a medication was ineffective or the precipitant of the flare. TNF inhibitors have previously been implicated as the cause of GPP flares [9–11], which may have prompted physicians to discontinue this class of medication and may partly explain the discontinuation of TNF inhibitors reported in this survey.
Limited data are available on the impact of GPP on health-related QoL. A small (N = 105), single-center survey conducted in Japan between 2003 and 2007 documented impaired “general health,” “social functioning,” and “role-emotional” using the Short Form 36 (SF-36) [12]. Approximately 10 years later (2016–2019), the QoL of Japanese patients (N = 83) with GPP was evaluated in a multicenter study again using the SF-36. The authors noted significant improvements in scores on all SF-36 subscales when compared with the earlier survey and interpreted the change over time as potential evidence of improved outcomes achieved with recent advances in treatment. It is not possible to compare our findings with those of this Japanese study; however, our results suggest that QoL is still impaired in people living with GPP and this continues to be an area of unmet medical need.
The limitations of this study include selection bias. Participants self-identified as having received a GPP diagnosis and information about the extent of disease is lacking. The inability to verify the GPP diagnosis and the possibility that individuals with similar conditions, such as palmoplantar pustulosis, participated in the study are other potential limitations. Since this was an online survey, it was not possible to collect data on the extent of disease (body surface area). These data may have provided insights into disease severity and the broad spectrum of GPP presentation. Participants were required to have access to the internet, which may have biased the sample towards more affluent individuals or those with a better education. In addition, the survey did not provide participants with guidance on how to define disease severity; for example, some questions were broad and ambiguous and therefore open to the interpretation of each individual.
Many survey questions pertained to the concept of control of GPP; however, no uniform definition of control was used. This is not necessarily a limitation but must be kept in mind when interpreting the results. In addition, some aspects of GPP were described as plaques, which may have been confusing for some respondents because plaques are a characteristic of plaque psoriasis rather than GPP. Thus, for people with concomitant GPP and plaque psoriasis, these questions may have evoked different responses than for those with GPP alone. It is not possible to know how this choice of terminology affected the survey results.
Participants were asked about their treatment history for GPP; however, it was not clear whether responses described treatments received prior to or after the diagnosis of GPP. Also, the questions and responses do not provide insights into the sequence in which treatments were administered.
In conclusion, the results of this US-based online survey provide valuable insights into the experiences of people living with GPP. These individuals often wait years before receiving an accurate diagnosis, and experience suboptimal control of symptoms and diminished QoL, even when their condition is under control. The results highlight the need for more rapid diagnosis, additional treatment options to address unmet needs, and a patient-centric approach in which healthcare providers engage in discussions with their patients to mutually agree treatment goals.
Acknowledgements
All authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors (ICMJE) and made the decision to submit the manuscript for publication. The authors did not receive payment related to the development of the manuscript. Agreements between Boehringer Ingelheim and the authors included the confidentiality of the study data. Blair Jarvis, MSc, of OPEN Health Communications (London, UK) provided medical writing, editorial and/or formatting support, which was contracted and funded by Boehringer Ingelheim. Boehringer Ingelheim was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Declarations
Disclosure statement
This article has been published as part of a journal supplement wholly funded by Boehringer Ingelheim.
Funding
Medical writing support was funded by Boehringer Ingelheim.
Conflict of Interest
Kilian Eyerich has received consulting fees from AbbVie, Almirall, Bristol Myers Squibb, LEO Pharma, Janssen, Lilly, Novartis, UCB, Pfizer, and Boehringer Ingelheim; grants and/or contracts from AbbVie, LEO Pharma, UCB, and Lilly; and speaking fees from AbbVie, LEO Pharma, Janssen, and Lilly. Kilian Eyerich also declares stock or stock options with Dermagnostix and Dermagnostix R&D. Nirali Kotowsky was employed by Boehringer Ingelheim at the time the study was conducted. Wendell Valdecantos and Steven Brunette are full-time employees of Boehringer Ingelheim.
Ethics Approval
This survey received a formal Exemption from a central Institutional Review Board (IRB) on June 8, 2020, and was provided by the IRB of AdvarraTM (formerly IntegReview).
Consent to Participate
The participants of this research study voluntarily agreed to participate.
Consent for Publication
The participants of this research study gave their consent for the publication.
Availability of Data and Material
Not applicable
Code Availability
Not applicable
Author Contributions
The sponsor of the supplement and all authors identified and discussed the concept for each chapter and the supplement as a whole; further development of this original research article was at the direction of the authors, who provided guidance to OPEN Health Communications on the content of the article, critically revised the work, and approved the content for publication.
References
- 1.Navarini AA, Burden AD, Capon F, Mrowietz U, Puig L, Koks S, et al. European consensus statement on phenotypes of pustular psoriasis. J Eur Acad Dermatol Venereol. 2017;31:1792–1799. doi: 10.1111/jdv.14386. [DOI] [PubMed] [Google Scholar]
- 2.Choon SE, Lai NM, Mohammad NA, Nanu NM, Tey KE, Chew SF. Clinical profile, morbidity, and outcome of adult-onset generalized pustular psoriasis: analysis of 102 cases seen in a tertiary hospital in Johor, Malaysia. Int J Dermatol. 2014;53:676–684. doi: 10.1111/ijd.12070. [DOI] [PubMed] [Google Scholar]
- 3.Chung J, Callis Duffin K, Takeshita J, Shin DB, Krueger GG, Robertson AD, et al. Palmoplantar psoriasis is associated with greater impairment of health-related quality of life compared with moderate to severe plaque psoriasis. J Am Acad Dermatol. 2014;71:623–632. doi: 10.1016/j.jaad.2014.04.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hrehorow E, Salomon J, Matusiak L, Reich A, Szepietowski JC. Patients with psoriasis feel stigmatized. Acta Derm Venereol. 2012;92:67–72. doi: 10.2340/00015555-1193. [DOI] [PubMed] [Google Scholar]
- 5.Marrakchi S, Guigue P, Renshaw BR, Puel A, Pei XY, Fraitag S, et al. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. N Engl J Med. 2011;365:620–628. doi: 10.1056/NEJMoa1013068. [DOI] [PubMed] [Google Scholar]
- 6.Bachelez H. Pustular psoriasis: the dawn of a new era. Acta Derm Venereol. 2020;100:adv00034. doi: 10.2340/00015555-3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sbidian E, Madrange M, Viguier M, Salmona M, Duchatelet S, Hovnanian A, et al. Respiratory virus infection triggers acute psoriasis flares across different clinical subtypes and genetic backgrounds. Br J Dermatol. 2019;181:1304–1306. doi: 10.1111/bjd.18203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crowley JJ, Pariser DM, Yamauchi PS. A brief guide to pustular psoriasis for primary care providers. Postgrad Med. 2021;133:330–344. doi: 10.1080/00325481.2020.1831315. [DOI] [PubMed] [Google Scholar]
- 9.Goiriz R, Daudén E, Pérez-Gala S, Guhl G, García-Díez A. Flare and change of psoriasis morphology during the course of treatment with tumour necrosis factor blockers. Clin Exp Dermatol. 2007;32:176–179. doi: 10.1111/j.1365-2230.2006.02315.x. [DOI] [PubMed] [Google Scholar]
- 10.Brunasso AM, Laimer M, Massone C. Paradoxical reactions to targeted biological treatments: a way to treat and trigger? Acta Derm Venereol. 2010;90:183–185. doi: 10.2340/00015555-0777. [DOI] [PubMed] [Google Scholar]
- 11.Benjegerdes KE, Hyde K, Kivelevitch D, Mansouri B. Pustular psoriasis: pathophysiology and current treatment perspectives. Psoriasis (Auckl) 2016;6:131–144. doi: 10.2147/PTT.S98954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayama K, Fujita H, Iwatsuki K, Terui T. Improved quality of life of patients with generalized pustular psoriasis in Japan: a cross-sectional survey. J Dermatol. 2021;48:203–206. doi: 10.1111/1346-8138.15657. [DOI] [PMC free article] [PubMed] [Google Scholar]