Abstract
Objectives:
The coronavirus disease 2019 pandemic is a threat to public health that impacts the life of frontline pharmacists as they are more susceptible to getting infected by the coronavirus. This study aimed to assess the knowledge, risk perceptions, and preventive practices associated with coronavirus disease 2019 among pharmacy students of Bangladesh to evaluate their preparedness as future frontline workers against the ongoing pandemic.
Methods:
An online-based cross-sectional study was conducted among pharmacy undergraduate students of Bangladesh during the early months of the pandemic in April 2020. Respondents voluntarily submitted an online questionnaire regarding sociodemographics, knowledge, risk perceptions, and preventive practices related to coronavirus disease 2019.
Results:
A total of 418 participants submitted their responses, and we included 395 responses for final analysis. The mean age of the participants was 20.65 years. The study revealed that out of 395 pharmacy students, 68 (17.2%) had high levels of knowledge, 210 (53.2%) possessed high risk perceptions regarding coronavirus disease 2019, and 165 (41.7%) were adopting high levels of preventive practices. Average scores for knowledge, risk perceptions, and preventive practices were 5.7, 8.4, and 8.2 out of 10. Chi-square test and logistic regression analyses showed that having high knowledge levels was associated with high risk perceptions regarding coronavirus disease 2019. Similarly, higher risk perceptions were associated with having high knowledge and preventive measures, while higher preventive measures were associated with female gender, low monthly family income, and having high risk perceptions.
Conclusion:
We found moderate knowledge, risk perceptions, and preventive practices related to coronavirus disease 2019 among the undergraduate pharmacy students. We recommend awareness-building discussions or seminars focusing on pharmacy students. In addition, the upgradation of the existing curriculum may help future pharmacists.
Keywords: COVID-19, knowledge, risk perceptions, preventive practices, pharmacy students
Introduction
In late 2019, several cases of pneumonia were reported in Wuhan City, China, which later spread out as a global pandemic termed as “coronavirus disease 2019” (COVID-19). 1 The disease is caused by the “severe acute respiratory syndrome coronavirus-2” (SARS-CoV-2) virus, which has phylogenetic similarity to other viruses of the beta-coronavirus genus, such as “Middle East respiratory syndrome coronavirus (MERS-CoV)” and “severe acute respiratory syndrome coronavirus (SARS-CoV).” 2 These predecessor viruses of SARS-CoV-2 were also responsible for outbreaks of severe respiratory illness, though not in such a global scale. Because of its high transmission rate, SARS-CoV-2 continues to spread rapidly, with more than 200 million infected worldwide and 4.3 million deaths so far, according to World Health Organization (WHO). 3 To stop this rapid outbreak and reduce the transmission rate, several safety measures were taken by governments of different countries which included implementation of lockdown, closure of educational institutes, restaurants, different industrial factories, restriction on travel, etc.4–7 Despite all these safety measures and steps being taken, densely populated countries, such as Bangladesh, are still struggling to maintain social distance practices and strict lockdowns. 8 The fragile healthcare system of the country, with overburdened hospitals, only makes dealing with the pandemic much harder.9–14
Patients infected with COVID-19 need palliative care and those having severe disease need medical support accordingly. To ensure this, the healthcare system and outbreak management personnel, such as frontline physicians, nurses, pharmacists, etc., need to play their respective roles properly. Pharmacists are a very important part of any health care system and play a critical role to ensure that pandemic management is handled properly.15,16 According to the International Pharmaceutical Federation (FIP), in outbreak-affected and unaffected countries, community pharmacists are often the first person of contact for those seeking health-related information or reliable advice. 17 Therefore, it is very important to measure how prepared pharmacists are in managing their new role and duty during the COVID-19 pandemic. A study in China, from where the pandemic began, concluded that pharmacists played a key role in providing lifesaving drugs, spreading information about COVID-19, monitoring adverse drug reactions, and ensuring an adequate supply of medicine, face masks, sanitizers, etc. 18
The role of undergraduate pharmacy students cannot be ignored either, as students of medical and pharmacy schools are important assets of the healthcare system. The pandemic, as of now, is unlikely to end anytime soon. Thus, these future pharmacists will soon be frontline healthcare personnel against COVID-19 and their preparedness can be measured from their knowledge level and perception of the disease. A study reported. that students of medical schools felt they were not fully prepared for their role and implications during any pandemic and suggested to include pandemic or crisis management content into the curriculum. 19 This will aid pharmacy students to prepare against the COVID-19 crisis that they may face in the future and improve the transition from student to reliable healthcare personnel. Though future pandemics cannot be always foreseen, the preparedness of medical and pharmacy students can ensure better management of COVID-19 or other pandemics of the future. 20
This study was designed to assess the knowledge, risk perceptions, and preventive practices adopted by undergraduate pharmacists in Bangladesh. To manage and fight against the outbreak, knowledge about the disease, perceptions regarding the SARS-CoV-2 virus, and practices of prevention are important measures for determining the preparedness of future pharmacists. With only a fraction of the target population vaccinated so far in Bangladesh, behavior and attitude toward COVID-19 will impact heavily on the effectiveness of controlling the pandemic. With the help of the findings of this study, we can determine appropriate steps to increase the awareness among students and propose necessary curriculum changes accordingly to deal with this new “normal.”
Method
Study participants
An online-based cross-sectional survey was conducted on pharmacy undergraduate students of different public and private universities in Bangladesh to assess their knowledge, risk perception, and self-reported preventive practices against COVID-19. Study participants included undergraduate pharmacy students studying in any public or private university in Bangladesh, whereas graduate or post-graduate pharmacy students or undergraduate students belonging to other majors were excluded. The participants were asked to fill up an online questionnaire in the English language during April 2020. Participants’ written informed consent was obtained at the beginning of the study. In addition, they were well briefed about the nature, aim, and procedure of this research beforehand. As the government had already implemented a lockdown to prevent the spread of COVID-19 by this time, we designed an online self-reported questionnaire using Google Forms to conduct our survey without the need for any physical involvement of the students. The questionnaire was pretested for validity by conducting a pilot study on 30 participants (7.6% of study participants). After the pilot study, we distributed the survey form link to around 1000 students through email, WhatsApp, Facebook messenger, etc. Based on an estimated population of 20,000 and response distribution of 50%, we determined the sample size using the Raosoft sample size calculator (http://www.raosoft.com/samplesize.html) that gave us a required sample size of 377 with a 5% margin of error and confidence interval of 95%. 21
Data collection
The questionnaire was segmented into four sections: student demographics, knowledge associated with COVID-19, risk perception of the disease, and self-reported preventive practices adopted by the participants. Demographic information collected from the students included six variables (gender, age, current residential status, level of education, and monthly family income).
COVID-19-related knowledge assessment
The second segment of the questionnaire contained 10 questions that assessed the knowledge regarding COVID-19 of the study participants. The questions encompassed topics, such as whether participants had heard about COVID-19, the origin of the virus, incubation period, symptoms, disease fatality, the transmission of the virus, vulnerable group, and lingering time of the virus on surfaces. The questions were designed from a previously conducted Knowledge, attitude and practice (KAP) study during MERS-CoV disease outbreak, 22 and current verified information is available on WHO’s webpage. 18 Each question was scored 1 point for correct answers, 0.5 for partially correct answers in multiple response questions, and 0 for incorrect answers. The total score in the knowledge section ranged from 0 to 10. The overall score obtained from the knowledge assessing questions was tallied and classified into three groups—participants who scored above 6.5 were considered to possess high knowledge, those who scored between 5.5 and 6.5 were considered of medium knowledge, and anyone with scores less than 5.5 was considered to have low knowledge levels.
Measurement of risk perceptions
In the third segment, risk perceptions regarding COVID-19 were evaluated using 10 questions adopted from the “Mythbusters” page of the WHO 23 which was established for COVID-19 infection prevention and control. Several facts and myths regarding the susceptibility of the virus in hot or cold weather, transmission methods, vulnerable population, antibiotics, medications, vaccines against COVID-19, double masking, receiving packages from coronavirus-affected areas, etc. were asked to the study participants so that their risk perception could be determined. For all correct answers, 1 point was given, whereas for each incorrect answer the score was 0. The total score in the risk perception section also ranged from 0 to 10. Participants scoring above 8.5 were considered to have high risk perceptions regarding COVID-19, while those scoring between 7.5 and 8.5 were considered of having medium risk perceptions, and those scoring less than 7.5 were considered to have low risk perception levels.
Knowledge about preventive practices
The participant’s preventive practices in minimizing the spread of COVID-19 were measured using nine questions in the fourth segment. The questions mainly assessed whether participants were adhering to necessary practices, such as washing hands, social distancing, avoiding touching eyes, covering up before coughing, self-quarantine, masking, staying at home, confidence in government, etc., and were designed based on the guidelines provided by the Institute of Epidemiology, Disease Control and Research (IEDCR) 24 of Bangladesh. However, 1 point was given for proactively spreading awareness on prevention practices, 0.5 points for practicing only self-prevention, and 0 points for no preventive practices at all. A score ranging from 0 to 2 was given based on how many times the participants had gone out of home after the implementation of nationwide lockdown. The final preventive practice score ranged from 0 to 10. Participants who scored above 8.5 were considered to adhering high prevention practices, those who scored between 7.5 and 8.5 were considered to follow medium prevention practices and anyone with scores less than 7.5 was considered to maintain low prevention practices.
Statistical analysis
All data were analyzed using Microsoft Excel 2019 and IBM SPSS version 25.0 (Chicago, IL, USA). Microsoft Excel was used to sort and code all survey answers which were then exported to the SPSS software. Students’ demographic characteristics, knowledge, risk perception, and preventive practices associated with COVID-19 were measured using descriptive statistics. Correlations between categorical variables were measured using Pearson’s chi-square test or Fisher’s exact test if the expected cell count was less than 5. Multiple logistic regression analysis models were carried out through the “Enter” method to determine the influence of gender, current residence, level of education, monthly family income, knowledge, risk perception, and preventive practice scores on the probability of possessing high levels of knowledge, risk perceptions, and preventive practices. A p-value less than 0.05 was considered of statistical significance in all tests. Cut-off points for each of the knowledge, perception, and preventive measures sections were set based on the mean of the scores of study participants.
Results
Characteristics of the respondents
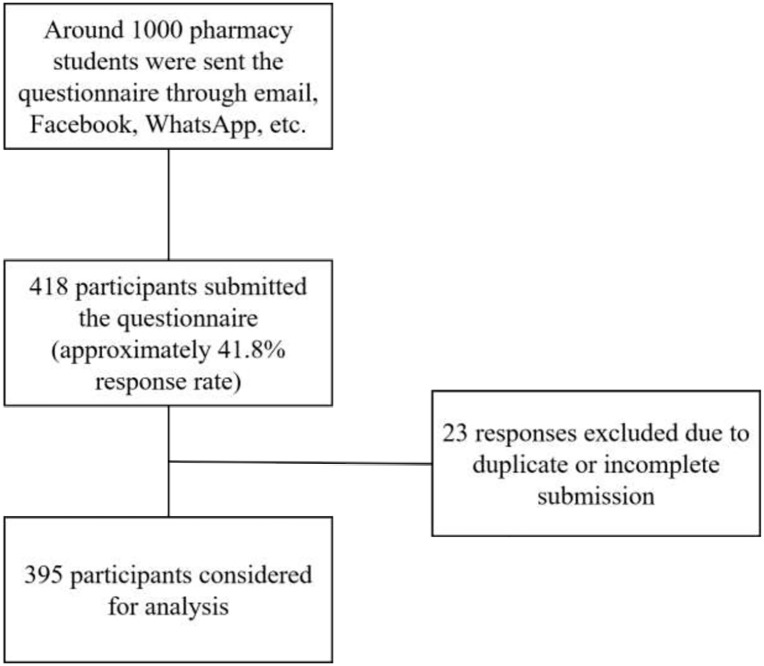
A total of 418 pharmacy undergraduate students responded to the survey. Among them, 23 entries were deleted because of duplicate or incomplete submissions. The final sample size was 395 among which 196 (49.6%) were male and 199 (50.4%) were female (Figure 1). The average age of subjects was 20.65 ± 1.33 years with a range between 18 and 25 years of age. The majority of the subjects were staying with family during the time of survey (90.4%), were students of first year (48.6%) of undergraduate studies, and 46.3% had family income of 25,000–50,000 Bangladesh Taka (BDT) which is roughly between US$300 and US$600. Demographic characteristics of the study subjects have been presented in Table 1.
Figure 1.
Flow diagram of study population and participants recruitment.
Table 1.
Demographic characteristics of study participants (N = 395).
| Characteristics | Total, n (%) |
|---|---|
| Gender | |
| Male | 196 (49.6) |
| Female | 199 (50.4) |
| Age (M ± SD) | |
| Current residence | 20.65 ± 1.33 |
| Living at home with family | 357 (90.4) |
| Living in hostel away from family | 38 (9.6) |
| Level of education (undergraduate) | |
| First year | 139 (35.2) |
| Second year | 192 (48.6) |
| Third Year | 36 (9.1) |
| Fourth Year | 28 (7.1) |
| Monthly family income (BDT) | |
| <10,000 | 23 (5.8) |
| 10,000–25,000 | 94 (23.8) |
| 25,000–50,000 | 183 (46.3) |
| 50,000–100,000 | 67 (17.0) |
| >100,000 | 28 (7.1) |
BDT: Bangladesh Taka. 10,000 BDT equals to approximately US$118.
COVID-19-related knowledge
COVID-19 associated knowledge was evaluated with 10 questions which are presented in Table 2. Most participants believe that COVID-19 originated from bats or humans, whereas only 20.3% selected that the origin has not been confirmed yet. Moreover, 60% of study participants wrongly think that COVID-19 cannot spread from a person who has no symptoms.
Table 2.
COVID-19 associated knowledge among study participants.
| Variable categories | Options (determination) | Score | N (%) |
|---|---|---|---|
| K1: Have you heard about novel coronavirus disease (COVID-19)? | Yes (positive) | 1.0 | 387 (98.0) |
| No (negative) | 0 | 8 (2.0) | |
| K2: Have you attended any lectures or discussions regarding COVID-19? | Yes (positive) | 1.0 | 269 (68.1) |
| No (negative) | 0 | 126 (31.9) | |
| K3: COVID-19 is thought to originate from- | Humans (incorrect) | 0 | 118 (29.9) |
| Mosquitoes (incorrect) | 0 | 0 (0.0) | |
| Bats (incorrect) | 0 | 181 (45.8) | |
| Rats (incorrect) | 0 | 8 (2.0) | |
| Birds (incorrect) | 0 | 8 (2.0) | |
| Not confirmed yet (correct) | 1.0 | 80 (20.3) | |
| K4: The incubation period of COVID-19 is- | 1–7 days (incorrect) | 0 | 15 (3.8) |
| 1–14 days (correct) | 1.0 | 353 (89.4) | |
| 1 month (incorrect) | 0 | 4 (1.0) | |
| Not known (incorrect) | 0 | 23 (5.8) | |
| K5: Which are the most common symptoms of COVID-19?* | Fever (correct) | 6 symptoms correct = 1.0 | 359 (90.9) |
| Tiredness (correct) | 3–5 symptoms correct = 0.5 | 133 (33.7) | |
| Blurred vision (incorrect) | < 3 symptoms correct = 0 | 17 (4.3) | |
| Dry cough and sore throat (correct) | 308 (78.0) | ||
| Muscle ache and pain (correct) | 120 (30.4) | ||
| Diarrhea (correct) | 171 (43.3) | ||
| Hallucination (incorrect) | 21 (5.3) | ||
| Nasal congestion (correct) | 113 (28.6) | ||
| Red eyes and skin rash (incorrect) | 21 (5.3) | ||
| K6: COVID-19 is a fatal disease. Death is certain if you get infected. | True (incorrect) | 0 | 150 (38.0) |
| False (correct) | 1.0 | 245 (62.0) | |
| K7: Can the virus that causes COVID-19 transmit through air? | Yes (incorrect) | 0 | 241 (61.0) |
| No (correct) | 1.0 | 153 (38.7) | |
| K8: Can COVID-19 be caught from a person who has no symptoms? | Yes (correct) | 1.0 | 158 (40.0) |
| No (incorrect) | 0 | 237 (60.0) | |
| K9: Who is at risk of developing severe illness from COVID-19?* | Older persons (correct) | Selected both correct responses = 1.0 | 350 (88.6) |
| Young adults (incorrect) | 82 (20.8) | ||
| Persons with pre-existing medical conditions (correct) | 308 (78.0) | ||
| Children (incorrect) | 135 (34.2) | ||
| Pregnant women (incorrect) | 102 (25.8) | ||
| K10: How long does the virus survive on surfaces? | 1 h (incorrect) | 0 | 29 (7.3) |
| 1 day (incorrect) | 0 | 40 (10.1) | |
| Few hours to several days (correct) | 1.0 | 289 (73.2) | |
| Few months (incorrect) | 0 | 37 (9.4) |
Indicates multiple response questions.
The average knowledge score of study participants was 5.7 out of 10. Among the 395 participants, 68 (17.2%) possessed high (> 6.5), 185 (46.8%) possessed medium (5.5–6.5), and 142 (35.9%) possessed low (< 5.5) levels of knowledge associated with COVID-19 according to our scoring system (Table 3). Significant differences in knowledge levels were associated with participants’ level of risk perceptions (p = 0.013). Among the study participants, higher knowledge scores were seen most in students with high risk perceptions (20.5%), whereas low knowledge scores were most frequently seen in students with low risk perception scores (55.6%). The logistic regression model confirmed the finding from the chi-square test, as compared to participants with low perception scores, the odds of having high knowledge levels were 3.16 times greater in participants with high risk perception scores (p = 0.043; 95% CI, 1.04–9.62).
Table 3.
Distribution and comparison of COVID-19 associated knowledge among different groups.
| Variables | High (> 6.5) | Medium (5.5–6.5) | Low (< 5.5) | χ2 (df) | OR* | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | p-value | ||||
| Gender | ||||||||||
| Male | 40 | (20.5) | 85 | (43.6) | 70 | (35.9) | 2.32 (2) | 1.475 | 0.766–2.842 | 0.245 |
| Female | 28 | (14.0) | 100 | (50.0) | 72 | (36.0) | 0.313 | Ref. | ||
| Current residence | ||||||||||
| Staying with family | 61 | (16.9) | 170 | (47.2) | 129 | (35.8) | 0.235 (2) | 1.002 | 0.339–2.957 | 0.997 |
| Living away from family | 7 | (20.0) | 15 | (42.9) | 13 | (37.1) | 0.889 | Ref. | ||
| Level of education (undergraduate) | ||||||||||
| First year | 24 | (17.3) | 68 | (48.9) | 47 | (33.8) | 3.457 (6) 0.75 |
1.044 | 0.306–3.564 | 0.946 |
| Second year | 31 | (16.1) | 89 | (46.4) | 72 | (37.5) | 0.987 | 0.297–3.287 | 0.988 | |
| Third year | 8 | (22.2) | 19 | (52.8) | 9 | (25.0) | 1.498 | 0.343–6.551 | 0.591 | |
| Fourth year | 5 | (17.9) | 9 | (32.1) | 14 | (50.0) | Ref. | Ref. | Ref. | |
| Monthly family income (BDT) | ||||||||||
| <10,000 | 4 | (17.4) | 15 | (65.2) | 4 | (17.4) | 4.549 (8) 0.805 |
1.455 | 0.194–10.901 | 0.715 |
| 10,000–25,000 | 18 | (19.1) | 40 | (42.6) | 36 | (38.3) | 1.664 | 0.322–8.6 | 0.543 | |
| 25,000–50,000 | 32 | (17.5) | 86 | (47.0) | 65 | (35.5) | 1.785 | 0.374–8.524 | 0.468 | |
| 50,000–100,000 | 11 | (16.4) | 29 | (43.3) | 27 | (40.3) | 1.65 | 0.306–8.896 | 0.56 | |
| >100,000 | 3 | (10.7) | 15 | (53.6) | 10 | (35.7) | Ref. | Ref. | Ref. | |
| Risk perceptions | ||||||||||
| High (> 8.5) | 43 | (20.5) | 104 | (49.5) | 63 | (30.0) | 12.73 (4) 0.013 |
3.156 | 1.036–9.617 | 0.043 |
| Medium (7.5–8.5) | 20 | (17.7) | 54 | (47.8) | 39 | (34.5) | 2.867 | 0.876–9.386 | 0.082 | |
| Low (< 7.5) | 5 | (6.9) | 27 | (37.5) | 40 | (55.6) | Ref. | Ref. | Ref. | |
| Preventive practices | ||||||||||
| High (> 8.5) | 25 | (15.2) | 82 | (49.7) | 58 | (35.2) | 1.358 (4) 0.851 |
0.86 | 0.354–2.089 | 0.74 |
| Medium (7.5–8.5) | 30 | (20.0) | 68 | (45.3) | 52 | (34.7) | 1.155 | 0.482–2.765 | 0.747 | |
| Low (< 7.5) | 13 | (16.3) | 35 | (43.8) | 32 | (40.0) | Ref. | Ref. | Ref. | |
Odds ratio (OR) of possessing high levels of knowledge was determined by a multiple logistic regression model carried out through the “Enter” method.
Significant p-values are presented in bold.
Risk perceptions regarding COVID-19
Risk perceptions regarding coronavirus infection were evaluated with 10 questions which have been presented in Table 4. In each question, the majority of the participants were correct in their perception of COVID-19 associated risks. This was reflected in the average 8.4 risk perception score of the study participants. Out of the 395 study participants, 210 (53.2%) participants possessed high perception scores (> 8.5), 113 (28.6%) participants possessed medium perception scores (7.5–8.5), and 72 (18.2%) participants possessed low level (< 7.5) of risk perceptions about COVID-19. Study findings indicate that there were no significant differences among different groups of demographic characteristics regarding risk perceptions toward COVID-19 (Table 5). However, the level of right perception was significantly different among groups with different levels of knowledge (p = 0.013) and preventive practice scores (p = 0.005). Students with high and medium levels of knowledge had a higher frequency of possessing higher risk perceptions (63.2 and 56.2, respectively), while lower perception levels were seen more in participants with low knowledge scores (28.2%). Participants with high and medium levels of preventive practices showed a higher frequency (53.9% and 61.3%, respectively) of possessing high risk perceptions, while low perception level was more frequently seen in participants with low preventive scores (30%). According to the logistic regression model, compared to participants with low knowledge scores, the odds of showing high risk perceptions scores were 2.05 times greater in students with high knowledge scores (p = 0.046; 95% CI, 1.01–4.16) and 1.71 times greater in students with medium knowledge scores (p = 0.047; 95% CI, 1.01–2.92). Similarly, compared to participants with low scores of practices, the odds of showing high risk perception scores were 2.25 times greater in participants with high preventive practice (p = 0.019; 95% CI, 1.15–4.43) and 3.0 times greater in participants with medium preventive practice scores (p = 0.002; 95% CI, 1.52–5.92).
Table 4.
COVID-19 associated risk perceptions among study participants.
| Variable categories | Options (determination) | Score | N (%) |
|---|---|---|---|
| R1: Exposing yourself to sun or to temperatures higher than 25°C can prevent the COVID-19. | Yes (incorrect) | 0 | 138 (34.9) |
| No (correct) | 1.0 | 257 (65.1) | |
| R2: Cold weather and snow can kill the novel coronavirus. | Yes (incorrect) | 0 | 25 (6.3) |
| No (correct) | 1.0 | 370 (93.7) | |
| R3: The novel coronavirus can be transmitted through mosquito bites. | Yes (incorrect) | 0 | 47 (11.9) |
| No (correct) | 1.0 | 348 (88.1) | |
| R4. The novel coronavirus only affects older people and younger people are not affected by the disease. | Yes (incorrect) | 0 | 21 (5.3) |
| No (correct) | 1.0 | 374 (94.7) | |
| R5: Are antibiotics effective in preventing and treating the new coronavirus? | Yes (incorrect) | 0 | 94 (23.8) |
| No (correct) | 1.0 | 301 (76.2) | |
| R6: Are there any specific medicines to treat the novel coronavirus? | Yes (incorrect) | 0 | 23 (5.8) |
| No (correct) | 1.0 | 372 (94.2) | |
| R7: Are there currently any vaccines to prevent the novel coronavirus? | Yes (incorrect) | 0 | 23 (5.8) |
| No (correct) | 1.0 | 372 (94.2) | |
| R8: Can wearing multiple masks together increase my protection against COVID-19? | Yes (correct) | 1.0 | 230 (58.2) |
| No (incorrect) | 0 | 165 (41.8) | |
| R9: Is it safe to receive a package from any area where COVID-19 has been reported? | Yes (incorrect) | 0 | 83 (21.0) |
| No (correct) | 1.0 | 312 (79.0) | |
| R10: Do you think that as a pharmacist you can play an important role in stopping the spread of COVID-19? | Yes (correct) | 1.0 | 382 (96.7) |
| No (incorrect) | 0 | 13 (3.3) |
Table 5.
Distribution and comparison of COVID-19 associated risk perceptions among different groups.
| Variables | High (> 8.5) | Medium (7.5–8.5) | Low (< 7.5) | χ2 (df) | OR* | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | p-value | ||||
| Gender | ||||||||||
| Male | 111 | (56.6) | 54 | (27.6) | 31 | (15.8) | 1.861 (2) | 1.525 | 0.913–2.545 | 0.107 |
| Female | 99 | (49.7) | 59 | (29.6) | 41 | (20.6) | 0.394 | Ref. | Ref. | Ref. |
| Current residence | ||||||||||
| Staying with family | 190 | (53.2) | 101 | (28.3) | 66 | (18.5) | 0.188 (2) | 1.192 | 0.505–2.816 | 0.689 |
| Living away from family | 20 | (52.6) | 12 | (31.6) | 6 | (15.8) | 0.91 | Ref. | Ref. | Ref. |
| Level of education (undergraduate) | ||||||||||
| First Year | 73 | (52.5) | 43 | (30.9) | 23 | (16.5) | 5.477 (6) 0.484 |
0.819 | 0.303–2.211 | 0.819 |
| Second Year | 101 | (52.6) | 52 | (27.1) | 39 | (20.3) | 0.887 | 0.336–2.338 | 0.887 | |
| Third Year | 20 | (55.6) | 7 | (19.4) | 9 | (25.0) | 0.907 | 0.267–3.08 | 0.907 | |
| Fourth Year | 16 | (57.1) | 11 | (39.3) | 1 | (3.6) | Ref. | Ref. | Ref. | |
| Monthly family income (BDT) | ||||||||||
| <10,000 | 11 | (47.8) | 9 | (39.1) | 3 | (13.0) | 5.262 (8) 0.729 |
0.703 | 0.174–2.847 | 0.622 |
| 10,000–25,000 | 58 | (61.7) | 21 | (22.3) | 15 | (16.0) | 1.527 | 0.529–4.407 | 0.434 | |
| 25,000–50,000 | 95 | (51.9) | 55 | (30.1) | 33 | (18.0) | 1.048 | 0.392–2.797 | 0.926 | |
| 50,000–100,000 | 34 | (50.7) | 20 | (29.9) | 13 | (19.4) | 0.987 | 0.336–2.902 | 0.982 | |
| >100,000 | 13 | (46.4) | 7 | (25.0) | 8 | (28.6) | Ref. | Ref. | Ref. | |
| Knowledge | ||||||||||
| High (> 6.5) | 43 | (63.2) | 20 | (29.4) | 5 | (7.4) | 12.73 (4) 0.013 |
2.053 | 1.014–4.158 | 0.046 |
| Medium (5.5–6.5) | 104 | (56.2) | 54 | (29.2) | 27 | (14.6) | 1.714 | 1.006–2.92 | 0.047 | |
| Low (< 5.5) | 63 | (44.4) | 39 | (27.5) | 40 | (28.2) | Ref. | Ref. | Ref. | |
| Preventive practices | ||||||||||
| High (> 8.5) | 89 | (53.9) | 55 | (33.3) | 21 | (12.7) | 14.95 (4) 0.005 |
2.252 | 1.146–4.425 | 0.019 |
| Medium (7.5–8.5) | 92 | (61.3) | 31 | (20.7) | 27 | (18.0) | 2.995 | 1.515–5.92 | 0.002 | |
| Low (< 7.5) | 29 | (36.3) | 27 | (33.8) | 24 | (30.0) | Ref. | Ref. | Ref. | |
Odds ratio (OR) of possessing high levels of risk perceptions was determined by a multiple logistic regression model carried out through the “Enter” method.
Significant p-values are presented in bold.
Preventive practices adopted against COVID-19
Preventive practices adopted against COVID-19 by our study participants were evaluated by nine questions (Table 6). The majority of the participants reported that they were actively practicing preventive practices, such as wearing masks, maintaining social distance, etc., and also educating others to do so. However, 52.9% of study participants had not gone out of their homes at all since the government had implemented nationwide lockdown. However, the majority of the participants (64.1%) were not fully confident that Bangladesh will be able to keep their fatality count low and the situation might deteriorate shortly.
Table 6.
COVID-19 associated preventive practices among study participants.
| Variable categories | Options | Score | N (%) |
|---|---|---|---|
| P1: Do you regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water? | No | 0 | 7 (1.8) |
| Yes, I do it for myself | 0.5 | 39 (9.9) | |
| Yes, I do it for myself and also educate others to do so | 1.0 | 349 (88.4) | |
| P2: Do you maintain at least 1 m (3 ft) distance between yourself and anyone who is coughing or sneezing? | No | 0 | 14 (3.5) |
| Yes, I do it for myself | 0.5 | 54 (13.7) | |
| Yes, I do it for myself and also educate others to do so | 1.0 | 327 (82.8) | |
| P3: Do you avoid touching your eyes, nose, and mouth? | No | 0 | 48 (12.2) |
| Yes, I do it for myself | 0.5 | 76 (19.2) | |
| Yes, I do it for myself and also educate others to do so | 1.0 | 271 (68.6) | |
| P4: Do you cover your mouth and nose with your bent elbow or tissue when you cough or sneeze? | No | 0 | 14 (3.5) |
| Yes, I do it for myself | 0.5 | 67 (17.0) | |
| Yes, I do it for myself and also educate others to do so | 1.0 | 314 (79.5) | |
| P5: Will you self-isolate by staying at home if you begin to feel unwell, even with mild symptoms, such as headache, low grade fever, and runny nose? | No | 0 | 19 (4.8) |
| Yes, I will do it for myself | 0.5 | 105 (26.6) | |
| Yes, I will do it for myself and also educate others to do so | 1.0 | 271 (68.6) | |
| P6: Do you use a mask when going outside? | No | 0 | 8 (2.0) |
| Yes, I do it for myself | 0.5 | 56 (14.2) | |
| Yes, I do it for myself and also educate others to do so | 1.0 | 331 (83.8) | |
| P7: After implementation of lockdown in Bangladesh, how many times have you gone outside your home? | None at all | 2.0 | 209 (52.9) |
| 1–2 times | 1.5 | 95 (24.1) | |
| 2–4 times | 1.0 | 48 (12.2) | |
| 4–10 times | 0.5 | 19 (4.8) | |
| More than 10 times | 0 | 24 (6.1) | |
| P8: Have you convinced any of your family members to not go outside their home unless necessary? | Yes (positive) | 1.0 | 346 (87.6) |
| No (negative) | 0 | 49 (12.4) | |
| P9: Do you think that Bangladesh will be able to minimize the death rate or will the situation become worse like Italy, Spain and the United States? | Yes (positive) | 0 | 59 (14.9) |
| Maybe (neutral) | 0.5 | 253 (64.1) | |
| No (negative) | 1.0 | 83 (21.0) |
Among 395 study participants, 165 (41.7%) possessed high (> 8.5), 150 (38%) possessed medium (7.5–8.5), and 80 (20.3%) possessed low (< 7.5) level of preventive practice scores and the average score was 8.2 out of 10. We found that preventive practice against COVID-19 significantly varied based on gender (p = 0.015) (Table 7). Females showed significantly high preventive practice scores compared to males (47.7% vs 35.7%) and males showed a higher frequency of low preventive practice scores compared to females (26.5% vs 14.1%). The logistic regression model also confirms this, as males had about 0.48 odds of having high preventive practice scores compared to females (p = 0.005; 95% CI, 0.29–0.78). The model also suggests that compared to participants with monthly family income greater than 100,000 BDT, those with monthly family income below 10,000 BDT had 5.9 times greater odds (p = 0.019; 95% CI, 1.34–25.85), those with monthly family income between 10,000 and 25,000 BDT had 3.7 times greater odds (p = 0.03; 95% CI, 1.13–11.78), and those with family income between 25,000 and 50,000 BDT had 3.05 times greater odds (p = 0.048; 95% CI, 1.01–9.18) of showing high preventive practice scores. The scores were also significant in different risk perception groups (p = 0.005) with high and medium levels of risk perception groups showing a higher frequency (41.9% and 48.7%, respectively) of possessing high preventive practice scores, while low scores were more frequently seen in participants with low risk perceptions (33.3%). This was reflected in the logistic regression model as well, where participants with medium risk perception had 2.2 times greater odds of showing high preventive practice scores compared to those with low risk perceptions (p = 0.042; 95% CI, 1.03–4.72).
Table 7.
Distribution and comparison of COVID-19 associated preventive practices among different groups.
| Variables | High (> 8.5) | Medium (7.5–8.5) | Low (< 7.5) | χ2 (df) | OR* | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | p-value | ||||
| Gender | ||||||||||
| Male | 70 | (35.7) | 74 | (37.8) | 52 | (26.5) | 8.341 (2) | 0.478 | 0.286–0.797 | 0.005 |
| Female | 95 | (47.7) | 76 | (38.2) | 28 | (14.1) | 0.015 | Ref. | Ref. | Ref. |
| Current residence | ||||||||||
| Staying with family | 148 | (41.5) | 131 | (36.7) | 78 | (21.8) | 5.037 (2) | 0.858 | 0.364–2.021 | 0.725 |
| Living away from family | 18 | (47.4) | 19 | (50.0) | 1 | (2.6) | 0.081 | Ref. | Ref. | Ref. |
| Level of education (undergraduate) | ||||||||||
| First year | 67 | (48.2) | 51 | (36.7) | 21 | (15.1) | 6.102 (6) 0.412 |
1.793 | 0.661–4.861 | 0.251 |
| Second year | 77 | (40.1) | 71 | (37.0) | 44 | (22.9) | 1.209 | 0.456–3.205 | 0.703 | |
| Third year | 11 | (30.6) | 14 | (38.9) | 11 | (30.6) | 0.716 | 0.202–2.538 | 0.605 | |
| Fourth year | 11 | (39.3) | 13 | (46.4) | 4 | (14.3) | Ref. | Ref. | Ref. | |
| Monthly family income (BDT) | ||||||||||
| <10,000 | 13 | (56.5) | 5 | (21.7) | 5 | (21.7) | 4.82 (8) 0.777 |
5.893 | 1.343–25.845 | 0.019 |
| 10,000–25,000 | 40 | (42.6) | 36 | (38.3) | 18 | (19.1) | 3.654 | 1.134–11.777 | 0.030 | |
| 25,000–50,000 | 76 | (41.5) | 68 | (37.2) | 39 | (21.3) | 3.047 | 1.012–9.175 | 0.048 | |
| 50,000–100,000 | 30 | (44.8) | 25 | (37.3) | 12 | (17.9) | 3.272 | 0.993–10.786 | 0.051 | |
| >100,000 | 7 | (25.0) | 14 | (50.0) | 7 | (25.0) | Ref. | Ref. | Ref. | |
| Knowledge | ||||||||||
| High (> 6.5) | 26 | (38.2) | 29 | (42.6) | 13 | (19.1) | 1.358 (4) 0.851 |
0.798 | 0.387–1.644 | 0.54 |
| Medium (5.5–6.5) | 82 | (44.3) | 68 | (36.8) | 35 | (18.9) | 1.037 | 0.6–1.791 | 0.897 | |
| Low (< 5.5) | 58 | (40.8) | 52 | (36.6) | 32 | (22.5) | Ref. | Ref. | Ref. | |
| Risk perceptions | ||||||||||
| High (> 8.5) | 88 | (41.9) | 92 | (43.8) | 30 | (14.3) | 14.95 (4) 0.005 |
1.8 | 0.89–3.639 | 0.102 |
| Medium (7.5–8.5) | 55 | (48.7) | 31 | (27.4) | 27 | (23.9) | 2.204 | 1.03–4.716 | 0.042 | |
| Low (< 7.5) | 21 | (29.2) | 27 | (37.5) | 24 | (33.3) | Ref. | Ref. | Ref. | |
Odds ratio (OR) of possessing high levels of preventive practices was determined by a multiple logistic regression model carried out through the “Enter” method.
Significant p-values are presented in bold.
Discussion
After the outbreak of the COVID-19 pandemic in China and gradually in other countries, Bangladesh was in serious threat due to its dense population and inadequate health infrastructures.25–30 This threat became real when Bangladesh reported its first COVID case on 8 March 2020, and in response, the government took various measures, such as self-quarantine, closure of educational institutions, and finally imposing lockdown throughout the country to slow down the transmission of the disease. 4 As an integral part of the healthcare system, pharmacists can play a vital role in tackling COVID-19. 31 So, effective public health education is necessary among future pharmacists to prepare them as valiant frontline health personnel for such situations.32,33
In terms of knowledge associated with COVID-19, most of the participants (89.4%) had a clear idea about the incubation period of the SARS-CoV-2 virus, which was also seen in a study conducted on Peruvian community members. 34 Majority of the participants could identify some common symptoms (fever, dry cough) of COVID-19 which is probably because the pharmacy undergraduate curriculum gives considerable focus on diseases and their characteristic symptoms. This was also seen in a similar study conducted among medical students of Baghdad city. 35 Most participants believe that COVID-19 originated from bats or humans, whereas only 20.3% correctly selected that the origin has not been confirmed yet. 36 Majority of our study participants reported older persons (88.6%) and persons with pre-existing medical conditions (78%) as more vulnerable groups, which is very close to result obtained from studies conducted on Saudi pharmacy students and Bangladeshi undergraduate students of public universities.37,38 Interestingly, 38.7% believed that SARS-CoV-2 does not transmit through the air, which we have considered correct knowledge only because airborne transmission of the virus was not confirmed until much later than the completion of this survey. 39 Alternatively, 61.3% of respondents believed that coronavirus transmits through the air. However, studies reported that COVID-19 transmits through respiratory droplets of an infected person during this study in April 2020. There are no confirmed reports of airborne transmission based on the current knowledge. 39 Therefore, the transmission of COVID-19 can occur by direct contact with an infected person and indirect contact with materials or surfaces used by the infected person. This seems to be very commonly mistaken information and was also seen in studies conducted in UAE 32 and Iran. 40 Most concerning of all is that 60% of study participants believe that COVID-19 cannot spread from a person who has no symptoms, even though the spread of SARS-CoV-2 from asymptomatic patients is already concretely proven.
Overall risk perception of the study participants regarding COVID-19 was quite good. The majority of participants (94.2%) responded that there are no specific medicines to treat COVID-19, which is comparatively higher than the percentage of medical students of Baghdad (74.8%) in a similar study. 35 Most participants (76.2%) also had the right attitude toward the use of antibiotics against coronavirus, quite similar to the students of a UAE university. 41 Although multiple masks increase the protection against COVID-19, 41.8% of participants showed a negative attitude toward wearing more than one mask.42,43 In terms of preventive practices, almost all participants had the belief that they can play an important role as a pharmacist in terminating the spread of COVID-19. Our study found that most of the participants are aware of the best preventive practices, such as washing hands with soap (88.4%), maintaining at least 1 m distance with others (82.8%), avoiding touching eyes, nose, and mouth (68.6%), wearing masks when going outside (83.8%), and trying to educate others for following these practices as well. These findings are very similar to a study on medical students in Afghanistan. 44 Overall, 95.2% of the participants preferred self-isolation at home in case of having suspected symptoms, which is consistent with the data found in a public health practice conducted among the Chinese population (93.1%). 45 During lockdown implemented by the government, 52.9% of the participants did not go out of home at all and 87.6% of the participants convinced at least one of their family members not to go outside unless necessary. Only 14.9% of the participants believed that Bangladesh would be able to take the COVID situation under control. However, in another study conducted among general Bangladeshi people, they were optimistic about their countries’ handling of the COVID-19 situation. 46
Our study revealed moderate levels of knowledge and comparatively higher risk perceptions and preventive practices related to COVID-19 among undergraduate pharmacy students. Though our study participants’ average knowledge score (5.7) was lower than the knowledge score of undergraduate students in China, 47 regarding risk perceptions (average 8.4) and preventive practice (average 8.2), the scores were satisfactory. This significant knowledge gap across the participants indicates poor proclamation of public health information by the government and choosing unreliable information sources by the public. Questions in the knowledge section were basic and university education level should not have played a big factor here. Information regarding the questions was available on the Internet and anyone keen to know about COVID-19 could acquire this basic knowledge.
We found no significant differences among different sociodemographic groups regarding risk perceptions toward COVID-19. Ferdous et al. 48 found age, education level, occupation, and monthly family income as good predictors of positive attitude toward COVID-19 in the Bangladeshi population. Our participants were all undergraduate pharmacy students and their understanding of the disease might be a probable cause of having no significant difference among the different sociodemographic groups, as all of them possessed good risk perception scores (average 8.4). However, good preventive practices were positively associated with having good risk perceptions.
We found gender as a significant contributing factor in terms of preventive practices. Our female participants were more aware of the preventive practices against COVID-19 than the male participants. The same fact was revealed in other previous studies as well.38,49,50 Generally, females are more concerned about seeking and practicing health information than males 38 and are more conscious about leading a healthy lifestyle. 51 Studies have also shown that males are more likely to be in danger of developing COVID-19-related severe conditions. 52 Moreover, the rate of death from COVID-19 is significantly higher in males than females throughout the world 53 and also in Bangladesh. 54 These could be the reasons why more preventive behaviors were seen in females compared to males. Lower monthly family income seemed to be a good predictor of having higher preventive practices compared to having a higher monthly income. These findings contradict a study on the Chinese population, where people with higher family income did well in both the knowledge and practice section. 52 As pharmacy undergraduate students, the study participants might be aware of the severity of the disease and expenses (hospitalization cost, medicine cost, and ICU cost) associated with hospitalization. This awareness could drive the students with lower family incomes to adopt significantly higher preventive behaviors. Good risk perception was also positively associated with having higher preventive practices.
Our cross-sectional study has some limitations. First, as a cross-sectional study, it is unable to establish causal relationships among the variables. Second, we cannot eliminate selection bias because of convenient sampling, which renders the internal validity of the study at risk. Third, our study subjects were enrolled from a few public and private universities in Bangladesh, but not from all universities that have pharmacy undergraduate students. As a result, they are unlikely to reflect the accurate presentation of the whole undergraduate pharmacy students of Bangladesh. Fourth, most of the participants (83.8%) are actually from first and second year pharmacy students and senior pharmacy students are less represented in this study. Finally, this study assigned a limited number of questions to evaluate knowledge, risk perceptions, and preventive practices of the participants toward COVID-19. Including more questions and aspects of knowledge, risk perceptions and preventive practices could make the study even stronger.
Conclusion
Our study involving undergraduate pharmacy students provided us with some valuable insights into the preparedness of future pharmacists. The overall knowledge, risk perceptions, and preventive practices among the participants were good but this could be even better. Government can arrange online seminars, discussions to disseminate proper public health education among them. University authorities can also include some courses in the undergraduate pharmacy curriculum to educate the students against any pandemic. Another important finding was the reluctance of exercising preventive practices against COVID-19 by males compared to females. In general, males are less interested in health information and lack the inspiration to be involved. To improve their awareness, there is no alternative to designing and implementing gender-specific awareness programs focusing on male students. A well-prepared generation of pharmacists could play a vital role in the upcoming years as the COVID-19 pandemic continues to shape our world to a new “normal.”
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211073014 for A cross-sectional study of COVID-19-related knowledge, risk perceptions, and preventive practices among pharmacy students in Bangladesh by Sadia Afruz Ether, Faisal Abdullah Emon, ASM Roknuzzaman, Md Rakibuzzaman, Fahad Imtiaz Rahman and Md Rabiul Islam in SAGE Open Medicine
Acknowledgments
The authors thank the Department of Pharmacy, Daffodil International University for providing facilities to conduct this research.
Footnotes
Author contributions: S.A.E. and F.I.R. conceived the idea, collected responses from study participants, analyzed the data, and wrote the initial draft of the article; F.A.E., A.S.M.R., and M.R.I. collected data and wrote the initial draft; M.R.I. conceived the idea, gave intellectual contents, reanalyzed the data, and revised the initial draft of the article. All the authors reviewed and approved the final submission.
Availability of data: The data supporting these study findings can be obtained from the corresponding author on reasonable request.
Consent for publication: We obtained written permission from all the study participants for the publication of anonymous data in journal articles.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval and consent to participate: Ethical approval was taken from the Ethical Review Committee of Daffodil International University, Dhaka, Bangladesh (Approval No. DIU/ERC/02/2020). Participant’s written informed consent was taken at the beginning of the study. Also, they were well briefed about the nature, aim, and procedure of this research beforehand. The study was conducted in accordance with the principle stated in the declaration of Helsinki. Anonymity of study participants was strictly maintained.
Ethical approval: Ethical approval for this study was obtained from Ethical Review Committee of Daffodil International University, Dhaka, Bangladesh (Approval No. DIU/ERC/02/2020).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was self-funded.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Md Rabiul Islam  https://orcid.org/0000-0003-2820-3144
https://orcid.org/0000-0003-2820-3144
Supplemental material: Supplemental material for this article is available online.
References
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382(8): 727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol 2019; 17(3): 181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. WHO coronavirus (COVID-19) dashboard, 2020, https://covid19.who.int/ (accessed 10 August 2021).
- 4. Islam MT, Talukder AK, Siddiqui MN, et al. Tackling the COVID-19 pandemic: the Bangladesh perspective. J Public Health Res 2020; 9(4): 389–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Daria S, Islam MR. The second wave of COVID-19 pandemic in Bangladesh: an urgent call to save lives. Asia Pac J Public Health 2021; 33(5): 665–666. [DOI] [PubMed] [Google Scholar]
- 6. Daria S, Islam MR. The use of cow dung and urine to cure COVID-19 in India: a public health concern. Int J Health Plann Manage 2021; 36(5): 1950–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Das R, Hasan MR, Daria S, et al. Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open 2021; 11(4): e045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Daria S, Asaduzzaman M, Shahriar M, et al. The massive attack of COVID-19 in India is a big concern for Bangladesh: the key focus should be given on the interconnection between the countries. Int J Health Plann Manage 2021; 36(5): 1947–1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moona AA, Daria S, Asaduzzaman M, et al. Bangladesh reported delta variant of coronavirus among its citizen: actionable items to tackle the potential massive third wave. Infect Prev Pract 2021; 3(3): 100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rahman MA, Shanjana Y, Tushar MI, et al. Hematological abnormalities and comorbidities are associated with COVID-19 severity among hospitalized patients: experience from Bangladesh. PLoS ONE 2021; 16(7): e0255379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Islam MR, Hossain MJ. Social stigma and suicide in Bangladesh: the COVID-19 has worsened the situation. Chronic Stress 2021; 5: 24705470211035602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rahman FI, Islam MR. Sexual violence against woman at quarantine center during coronavirus disease 2019 in Bangladesh: risk factors and recommendations. Womens Health 2021; 17: 17455065211043851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Islam MR, Daria S, Das R, et al. A nationwide dataset on the mental health of the Bangladeshi population due to the COVID-19 pandemic. Data Brief 2021; 38: 107347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rahman FI, Ether SA, Islam MR. The “Delta Plus” COVID-19 variant has evolved to become the next potential variant of concern: mutation history and measures of prevention. J Basic Clin Physiol Pharmacol. Epub ahead of print 27 September 2021. DOI: 10.1515/jbcpp-2021-0251. [DOI] [PubMed] [Google Scholar]
- 15. Repon MAU, Pakhe SA, Quaiyum S, et al. Effect of COVID-19 pandemic on mental health among Bangladeshi healthcare professionals: a cross-sectional study. Sci Prog 2021; 104(2): 368504211026409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Basheti IA, Nassar R, Barakat M, et al. Pharmacists’ readiness to deal with the coronavirus pandemic: assessing awareness and perception of roles. Res Soc Adm Pharm 2021; 17(3): 514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ung COL. Community pharmacist in public health emergencies: quick to action against the coronavirus 2019-nCoV outbreak. Res Soc Adm Pharm 2020; 16(4): 583–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Meng L, Huang J, Qiu F, et al. Roles of the Chinese clinical pharmacist during the COVID-19 pandemic. J Am Coll Clin Pharm 2020; 3(5): 866–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. O’Byrne L, Gavin B, McNicholas F. Medical students and COVID-19: the need for pandemic preparedness. J Med Ethics 2020; 46(9): 623–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miller DG, Pierson L, Doernberg S. The role of medical students during the COVID-19 pandemic. Ann Intern Med 2020; 173(2): 145–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Taghrir MH, Borazjani R, Shiraly R. COVID-19 and Iranian medical students; a survey on their related-knowledge, preventive behaviors and risk perception. Arch Iran Med 2020; 23(4): 249–254. [DOI] [PubMed] [Google Scholar]
- 22. ALdowyan N, Abdallah AS, El-Gharabawy R. Knowledge, attitude and practice (KAP) study about Middle East respiratory syndrome coronavirus (MERS-CoV) among population in Saudi Arabia. Int Arch Med 2017; 10: 1–12. [Google Scholar]
- 23. World Health Organization. Coronavirus disease (COVID-19) advice for the public: mythbusters, 2021, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters (accessed 10 August 2021).
- 24. Institute of Epidemiology, Disease Control and Research. General information on COVID-19, 2020, https://iedcr.gov.bd/covid-19/covid-19-general-information (accessed 10 August 2021).
- 25. Islam MR, Qusar MMAS, Islam MS. Mental health of children amid COVID-19 pandemic in Bangladesh: an exploratory observation. Asia Pac J Public Health 2021; 33(4): 469–470. [DOI] [PubMed] [Google Scholar]
- 26. Islam MR, Quaiyum S, Pakhe SA, et al. Dataset concerning the mental health of healthcare professionals during COVID-19 pandemic in Bangladesh. Data Brief 2021; 39: 107506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Islam MR, Hossain MJ. Increments of gender-based violence amid COVID-19 in Bangladesh: a threat to global public health and women’s health. Int J Health Plann Manage. Epub ahead of print 12 July 2021. DOI: 10.1002/hpm.3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hossain MJ, Soma MA, Islam MR, et al. Urgent call for actionable measures to fight the current co-epidemic of dengue burden during the SARS-CoV-2 delta variant era in South-Asia. Ethics Med Public Health 2021; 19: 100726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hossain MJ, Rahman S, Emran TB, et al. Recommendation and roadmap of mass vaccination against COVID-19 pandemic in Bangladesh as a lower-middle-income country (LMIC). Arch Razi Inst 2021; 76: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Islam MR. The COVID-19 pandemic and suicidal behavior in Bangladesh: social stigma and discrimination are key areas to focus on. Alpha Psychiatry 2021; 22: 275–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Visacri MB, Figueiredo IV, Lima TDM. Role of pharmacist during the COVID-19 pandemic: a scoping review. Res Soc Adm Pharm 2021; 17(1): 1799–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Moona AA, Islam MR. Mucormycosis or black fungus is a new fright in India during COVID-19 pandemic: associated risk factors and actionable items. Public Health Pract 2021; 2: 100153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rahman FI, Islam MR, Bhuiyan MA. Mucormycosis or black fungus infection is a new scare in South Asian countries during the COVID-19 pandemic: associated risk factors and preventive measures. J Med Virol. Epub ahead of print 22 July 2021. DOI: 10.1002/jmv.27207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zegarra-Valdivia J, Vilca BNC, Guerrero RJA. Knowledge, perception and attitudes in regard to COVID-19 pandemic in Peruvian population, 2020, 10.31234/osf.io/kr9ya [DOI] [PMC free article] [PubMed]
- 35. Sahib Khalil N, Al-Yuzbaki B, Tawfeeq RS. COVID-19 knowledge, attitude and practice among medical undergraduate students in Baghdad City. Eurasia J Biosci 2020; 14(2): 4179–4186. [Google Scholar]
- 36. World Health Organization. WHO-convened global study of origins of SARS-CoV-2: China part, 2021, https://www.who.int/publications/i/item/who-convened-global-study-of-origins-of-sars-cov-2-china-part (accessed 10 August 2021).
- 37. Alrasheedy AA, Abdulsalim S, Farooqui M, et al. Knowledge, attitude and practice about coronavirus disease (COVID-19) pandemic and its psychological impact on students and their studies: a cross-sectional study among pharmacy students in Saudi Arabia. Risk Manag Healthc Policy 2021; 14: 729–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rahman MM, Jhinuk JM, Nabila NH, et al. Knowledge, attitude, and practices towards COVID-19 during the rapid rise period: a cross-sectional survey among public university students of Bangladesh. SciMed J 2021; 3(2): 116–128. [Google Scholar]
- 39. World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations, 2021, https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed 5 December 2021).
- 40. Hasan H, Raigangar V, Osaili T, et al. A cross-sectional study on university students’ knowledge, attitudes, and practices toward COVID-19 in the United Arab Emirates. Am J Trop Med Hyg 2021; 104(1): 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Das AK, Gopalan SS. Epidemiology of COVID-19 and predictors of recovery in the Republic of Korea. Pulm Med 2020; 2020: 7291698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kakemam E, Ghoddoosi-Nejad D, Chegini Z, et al. Knowledge, attitudes, and practices among the general population during COVID-19 outbreak in Iran: a national cross-sectional online survey. Front Public Health 2020; 8: 585302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Centers for Disease Control and Prevention. Improve how your mask protects you, 2021, https://www.cdc.gov/coronavirus/2019-ncov/your-health/effective-masks.html (accessed 15 August 2021).
- 44. Nemat A, Raufi N, Sediqi MF, et al. Knowledge, attitudes, and practices of medical students regarding COVID-19 in Afghanistan: a cross-sectional study. Risk Manag Healthc Policy 2021; 14: 1491–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Xu Y, Lin G, Spada C, et al. Public knowledge, attitudes, and practices behaviors towards coronavirus disease 2019 (COVID-19) during a national epidemic-China. Front Public Health 2021; 9: 638430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rahman MM, Khan SJ, Sakib MS, et al. COVID-19 responses among general people of Bangladesh: status and individual view toward COVID-19 during lockdown period. Cogent Psychol 2021; 8(1): 1860186. [Google Scholar]
- 47. Peng Y, Pei C, Zheng Y, et al. A cross-sectional survey of knowledge, attitude and practice associated with COVID-19 among undergraduate students in China. BMC Public Health 2020; 20(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ferdous MZ, Islam MS, Sikder MT, et al. Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: an online based cross-sectional study. PLoS ONE 2020; 15(10): e0239254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Walter LA, McGregor AJ. Sex- and gender-specific observations and implications for COVID-19. West J Emerg Med 2020; 21(3): 507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ek S. Gender differences in health information behaviour: a Finnish population-based survey. Health Promot Int 2015; 30(3): 736–745. [DOI] [PubMed] [Google Scholar]
- 51. Wardle J, Haase AM, Steptoe A, et al. Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med 2004; 27(2): 107–116. [DOI] [PubMed] [Google Scholar]
- 52. Zheng H, Tan J, Zhang X, et al. Impact of sex and age on respiratory support and length of hospital stay among 1792 patients with COVID-19 in Wuhan, China. Br J Anaesth 2020; 125(4): e378–e380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun 2020; 11(1): 6317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Al-Bari MAA, Hossain S, Zahan MK. Exploration of sex-specific and age-dependent COVID-19 fatality rate in Bangladesh population. World J Radiol 2021; 13(1): 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211073014 for A cross-sectional study of COVID-19-related knowledge, risk perceptions, and preventive practices among pharmacy students in Bangladesh by Sadia Afruz Ether, Faisal Abdullah Emon, ASM Roknuzzaman, Md Rakibuzzaman, Fahad Imtiaz Rahman and Md Rabiul Islam in SAGE Open Medicine