Abstract
Aim:
To evaluate the overall health and functioning in patients with axial spondyloarthritis (axSpA) and related factors affecting these during the COVID-19 pandemic and lockdown measures.
Methods:
Data from 587 axSpA patients participating in the first phase (April–July 2020) of the REUMAVID study who completed the ASAS Health Index (ASAS-HI) were analysed. REUMAVID is a cross-sectional study that collects data through an online survey to assess the impact of the COVID-19 pandemic on patients with rheumatic and musculoskeletal diseases across seven European countries. Poor health was defined as ASAS-HI ⩾ 12. The World Health Organization Five well-being index, self-perceived health status and change in health status during COVID-19 pandemic were evaluated as secondary outcomes. Logistic regression models were used to identify the factors associated with poor health.
Results:
According to the ASAS-HI, 147 (25.0%) patients reported poor health. Pain and moving around were the main affected categories. In addition, 14.0% reported their self-perceived health status as ‘bad’ or ‘very bad’ and 46.8% as worse than before the pandemic. In the multivariate analysis, smoking (OR = 1.98), diabetes (OR = 4.89) and taking painkillers (OR = 2.82) or corticosteroids use (OR = 2.20) were significantly associated with poor health, while engaging in physical activity (OR = 0.54) and being actively employed (OR = 0.48) were inversely associated with this.
Conclusions:
During the first wave of the COVID-19 pandemic, one in four axSpA patients reported poor health and functioning, while the self-perceived health status of almost half of these patients worsened. Nonsmoking, physical activity and being employed were associated with better outcomes.
Keywords: ASAS-HI, axial spondyloarthritis, COVID-19, pandemic, patient-reported outcomes
Background
The ongoing COVID-19 pandemic is having a significant impact on patients with rheumatic and musculoskeletal diseases (RMDs). 1 People with axial spondyloarthritis (axSpA), in particular, may have felt this impact harder due to a lack of physical activity during the periods of home confinements. 2 Most studies evaluating the impact of the pandemic on patients with axSpA have focused on disease outcomes such as the risk of contracting an infection or the clinical evolution after doing so. Data on evaluating the impact of the pandemic and lockdown measures on the overall health of patients with axSpA, regardless of the risk of contracting the COVID-19 infection, however, are limited.
Different aspects likely impacted by the lockdown measures, such as changes in daily lifestyle habits, work restrictions or difficulties in accessing healthcare resources, may have contributed to a decline in the overall health and functioning of patients with axSpA. 3 In this sense, the few studies to date assessing patients’ experiences have highlighted the worsening of disease outcomes during this pandemic.4 –6 This aligns with the limited access to routine rheumatological care during this period. 7 Further insights from patients are therefore needed to fully understand the real impact of the pandemic and lockdown measures on the overall health of patients with axSpA.8,9
The main goal in axSpA management is to maximize health-related quality of life through the control of symptoms and inflammation. 10 Reports have described a substantial impact of the disease on the quality of life in axSpA patients, affecting different spheres of life such as social participation and employment. 11 To properly assess this impact, it is essential to make use of adequate instruments specifically developed and validated for this purpose. 12 One of the most recently developed tools to assess such disease outcomes in patients with spondyloarthritis (SpA) is the Assessment of SpondyloArthritis International Society Health Index (ASAS-HI), a patient-reported instrument developed to evaluate overall health and functioning. 13 The ASAS-HI assesses relevant aspects of health and contextual environmental factors. It addresses the concept of ‘functioning, disability and health’ – a construct which is conceptualized in the International Classification of Functioning, Disability and Health (ICF), published by the World Health Organization (WHO). 14 The ASAS-HI has demonstrated good measurement properties, proving to be a valid, reliable and discriminative instrument to assess overall health and functioning in patients with SpA. It has been cross-culturally validated in 15 additional languages.15,16
The main objective of this study is to evaluate the overall health and functioning in European patients with axSpA during the beginning of the COVID-19 pandemic and lockdown and to identify factors associated with its impact.
Methods
Study design
Data from the first phase of the REUMAVID study were included in this project. REUMAVID is a cross-sectional observational study that collects data via an online survey with the objective of evaluating the impact of the COVID-19 pandemic and lockdown measures on the physical and psychological health, well-being and lifestyle habits and access to healthcare in patients with RMDs. 17 This initiative is promoted through an international collaboration led by the Health & Territory Research group at the University of Seville (Spain), together with a multidisciplinary team, including rheumatologists and patient organizations. REUMAVID included data from seven European countries (Cyprus, France, Greece, Italy, Portugal, Spain and the United Kingdom) in two phases: (1) during the first wave of the pandemic between April and July 2020 and (2) between February and April 2021. Participants provided informed consent prior to their participation in the survey. Further information has been published in detail in the seminal manuscript. 18
Participants
The population of this specific study included all REUMAVID patients with axSpA recruited during the first phase of the study. Recruitment was carried out by patient organizations in each of the seven countries. The inclusion criteria in the REUMAVID study were as follows: (1) at least 18 years old, (2) a self-reported clinician-made diagnosis of RMD (based on the question ‘Which of the following conditions were you diagnosed with by a physician?’, with responses that comprised a list of 15 rheumatic conditions, including ankylosing spondylitis/axSpA and peripheral SpA), (3) the ability to understand and complete the questionnaires included in the original study, (4) fulfilment of at least 70% of the REUMAVID questionnaire and (5) those who were seen by a rheumatologist in the last 12 months (unless prevented so by COVID-19-related issues). Of 1800 patients fulfilling the inclusion criteria for REUMAVID study, 670 patients had axSpA. 18 To perform this ancillary analysis on patients with axSpA, we only included axSpA patients (including ankylosing spondylitis, nonradiographic axSpA and peripheral SpA) who had completed the ASAS-HI scale. Hence, all patients with any other diagnosis other than axSpA or who did not complete the ASAS-HI were excluded. A total of 587 patients with axSpA completed the ASAS-HI and, therefore, 83 were discarded from our study. There were no patients from Cyprus or Greece fulfilling these characteristics, so patients from the other 5 countries were included in the analysis.
Data collection
The online survey included 120 items addressing sociodemographic characteristics, healthcare and medication, health status, complementary therapy and psychological care, the role of patient organizations, COVID-19-related issues, working situation, contact with the outside world and fears and hopes in relation to the COVID-19. The survey was developed in collaboration with patient research partners and rheumatologists, who helped identify the most relevant items and tools from the patient’s perspective. The following validated measurement instruments to assess overall health and/or well-being were collected: ASAS-HI, the WHO (Five) Well-Being Index (WHO-5), self-perceived health and changes in health status during the COVID-19 pandemic. In addition, changes in lifestyle, daily activities, employment, healthcare resources utilization and comorbidities were also collected.
Outcomes
The primary endpoint for this study was defined as poor overall health and functioning according to the ASAS-HI score. This index is composed of 17 items regarding functional limitation in daily activities with two possible answers for each: agree or disagree. The total score is calculated by adding 1 per each positive answer, resulting in a score ranging from 0 to 17, in which a lower score indicates a better health status. A score of 12 or more indicates a poor state of health. 19
Secondary endpoints included tools assessing general health status like the WHO-5 well-being index, and self-perceived health status (including changes in health status during the pandemic). The WHO-5 is comprised of five items that evaluate overall well-being through a 6-point Likert-type scale ranging from 0 to 5, resulting in a total score between 0 and 25. Higher values represent a better state of well-being. To obtain a percentage score ranging from 0 to 100, the raw score is multiplied by 4; a cut-off score below 50 indicates poor well-being. 20 Self-perceived health status was assessed using the question ‘How is your health in general?’, with a 5-degree scale that ranged from ‘very bad’ to ‘very good’. Similarly, changes in health status were evaluated by the question, ‘During the COVID-19 pandemic lockdown, how has your health status changed?’, with 5-degree scale that ranged from ‘much worse than before’ to ‘much better than before’. 20
Statistical analysis
First, descriptive analyses were used to analyse sociodemographic characteristics, clinical-reported characteristics and health outcomes (including ASAS-HI, WHO-5 index and self-perceived health status). Patients were stratified in two groups according to their total ASAS-HI scores, which were analysed as a single categorical variable classifying patients as having acceptable/good health (ASAS-HI < 12) or poor health (ASAS-HI ⩾ 12). For comparisons between the groups, a chi-square test was used for categorical variables and the Student’s t test for continuous variables. Results were presented as the mean and standard deviation (SD) for continuous variables, and as absolute numbers and percentages of relative frequencies for categorical variables. In addition, Pearson’s correlation coefficients between the ASAS-HI and secondary health outcomes were calculated.
Those factors associated with poor health (ASAS-HI ⩾ 12) were then identified. Univariable and multivariable binomial logistic regression models were used, adding the possible explanatory factors as independent variables and the ASAS-HI category as the outcome. Interactions with age, sex, physical activity, educational level, marital status, country and employment status were tested. If no relevant interactions were found, variables were entered as covariates. All variables with a p value lower than 0.05 in the univariable analysis were included in the multivariable analysis. Odds ratios (ORs) with 95% confidence intervals (CIs) were used as measures of association for logistic regression models. In addition, the same analysis was employed to identify which factors were associated with worsening health status during the pandemic or lockdown. For this, the self-perceived changes in health status were categorized into two groups: ‘moderately worse’ and ‘much worse’ than before versus ‘same’, ‘moderately better’ and ‘much better’ than before.
Only clean and coded data were processed. Where missing values were found for a particular variable, these values were removed from all analyses where said variable was used. There was no imputation of missing data.
All analyses were performed using SPSS, version 24.0 and the cut-off for considering differences statistically significant was a value for p < 0.05 based on a two-sided testing.
Results
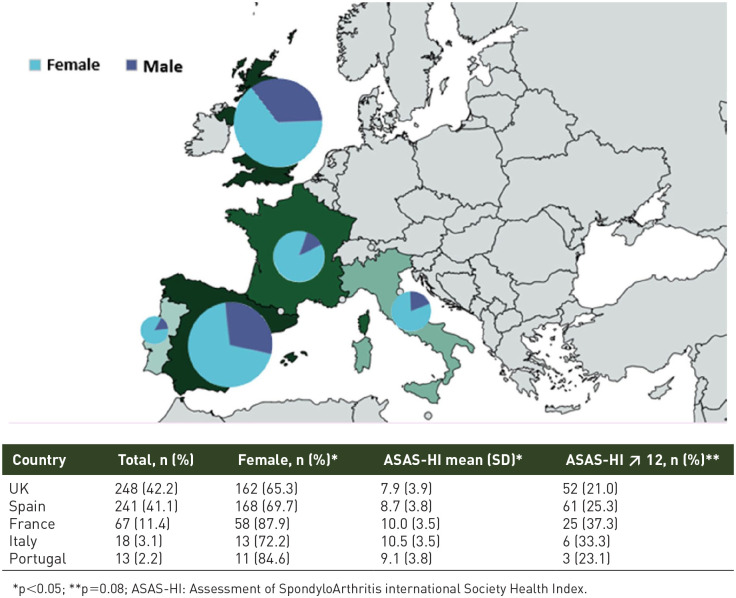
A total of 587 patients with axSpA who completed the ASAS-HI were included in the analysis (Supplementary Figure 1). Sociodemographic, clinical characteristics and the treatments of these patients are shown in Table 1. There were not relevant differences between included patients and those who did not fulfil the inclusion criteria (Supplementary Table 1). In summary, 413 (70.4%) patients were females and the total mean (SD) age at study visit was 49.9 (12.8) years. Overall, 46.7% (n = 274) of participants had university degree, 37.6% (n = 221) were employed and 72.6% (n = 426) were married or in a relationship. Most patients were from the United Kingdom (42.2%) or Spain (41.1%), while the remaining patients were from France (11.4%), Italy (3.1%) and Portugal (2.2%). Regarding sex distribution, there was a female predominance in all countries (Figure 1).
Table 1.
Sociodemographic, life habits and disease characteristics of the patients with axial spondyloarthritis included in the REUMAVID study stratified by the ASAS-HI score..
| Total N = 587 (100%) |
Good/acceptable Health
(ASAS-HI < 12) n = 440 (75%) |
Poor health
(ASAS-HI ⩾ 12) n = 147 (25%) |
p value | |
|---|---|---|---|---|
| Age at study visit (years) | 49.9 (12.8) | 50.3 (13.3) | 48.7 (11.1) | 0.16 |
| Gender (female) | 413 (70.4) | 304 (69.1) | 109 (74.1) | 0.25 |
| Body mass index | 26.7 (5.5) | 26.4 (5.3) | 27.6 (5.9) | 0.05 |
| Life habits | ||||
| Smoker | 127 (21.6) | 83 (18.9) | 44 (29.9) | 0.008 |
| Alcohol drinking (⩾ 3 drinks in a week) | 97 (16.5) | 78 (17.7) | 19 (12.9) | 0.20 |
| Exercise regularly prepandemic (No) | 170 (29.0) | 119 (27.0) | 51 (34.7) | 0.09 |
| Educational level | ||||
| No studies | 9 (1.5) | 8 (1.8) | 1 (0.7) | 0.47 |
| Primary/secondary | 112 (27.4) | 83 (18.9) | 29 (19.7) | |
| Vocational qualification | 192 (32.7) | 138 (31.4) | 54 (36.7) | |
| University | 274 (46.7) | 211 (48.0) | 63 (42.9) | |
| Employment status | ||||
| Employed | 221 (37.6) | 179 (40.7) | 42 (28.6) | 0.02 |
| Temporary/permanent sick leave | 99 (17.6) | 69 (15.7) | 30 (20.4) | |
| Retirement/early retirement | 130 (22.1) | 101 (23.0) | 29 (19.7) | |
| Unemployed/temporary regulatory | 47 (8.0) | 30 (6.8) | 17 (11.6) | |
| Housework | 26 (4.4) | 19 (4.3) | 7 (4.8) | |
| Student | 8 (1.4) | 7 (1.6) | 1 (0.7) | |
| Other | 56 (9.5) | 35 (8.0) | 21 (14.3) | |
| Marital status | ||||
| Single | 89 (15.2) | 71 (16.1) | 18 (12.2) | 0.39 |
| In a relationship/married | 426 (72.6) | 317 (72.0) | 109 (74.1) | |
| Separated/divorced/widow | 72 (12.2) | 42 (11.8) | 20 (13.6) | |
| Member of patient organization | 246 (41.9) | 187 (42.5) | 59 (40.1) | 0.63 |
| Extra-musculoskeletal manifestations | ||||
| Psoriasis | 80 (13.6) | 49 (11.1) | 31 (21.1) | 0.002 |
| Inflammatory bowel disease | 71 (12.1) | 49 (11.1) | 22 (15.0) | 0.22 |
| Uveitis | 110 (18.7) | 85 (19.3) | 25 (17.0) | 0.53 |
| Medication before lockdown | ||||
| Biologics | 299 (50.9) | 225 (51.1) | 74 (50.3) | 0.92 |
| NSAIDs | 272 (46.3) | 206 (46.8) | 66 (44.9) | 0.703 |
| Painkillers | 155 (26.4) | 93 (21.1) | 62 (42.2) | <0.001 |
| csDMARDs | 140 (23.9) | 81 (18.4) | 34 (23.1) | 0.40 |
| Oral corticosteroids | 70 (11.9) | 44 (10.0) | 26 (17.7) | 0.02 |
| Comorbidities | ||||
| High blood pressure | 88 (15.0) | 58 (13.2) | 30 (20.4) | 0.045 |
| Hypercholesterolemia | 44 (7.5) | 20 (4.5) | 24 (16.3) | <0.001 |
| Diabetes | 25 (4.3) | 9 (2.0) | 16 (10.9) | <0.001 |
| Kidney-related disease | 23 (3.9) | 13 (3.0) | 10 (6.8) | 0.048 |
| Respiratory disease | 41 (7.0) | 24 (5.5) | 17 (11.6) | 0.02 |
| Cardiovascular disease | 17 (2.9) | 12 (2.7) | 5 (3.4) | 0.78 |
| Liver disease | 11 (1.9) | 9 (2.0) | 2 (1.4) | 0.74 |
| Depression | 93 (15.8) | 60 (13.6) | 33 (22.4) | 0.01 |
| Anxiety | 89 (15.2) | 60 (13.6) | 29 (19.7) | 0.08 |
ASAS-HI, Assessment of SpondyloArthritis International Society Health Index; csDMARDs, conventional disease-modifying anti-rheumatic drugs; NSAIDs, nonsteroidal anti-inflammatory drugs.
Results are shown as absolute numbers (percentages) or expressed as the mean ± standard deviation (N = 587, unless specified).
Figure 1.
Geographic distribution of REUMAVID sample including patients with axial spondyloarthritis stratified by sex (N = 587).
With regard to extra-musculoskeletal manifestations, 80 (15.2%) patients had psoriasis, 71 (12.1%) had inflammatory bowel disease and 110 (18.7%) had uveitis. Before the COVID-19 pandemic, 299 (50.9%) patients were receiving biological drugs. The main reported comorbidities were depression (15.8%), anxiety (15.2%), high blood pressure (15.0%), hypercholesterolemia (7.5%) and diabetes (4.3%).
Overall health and functioning
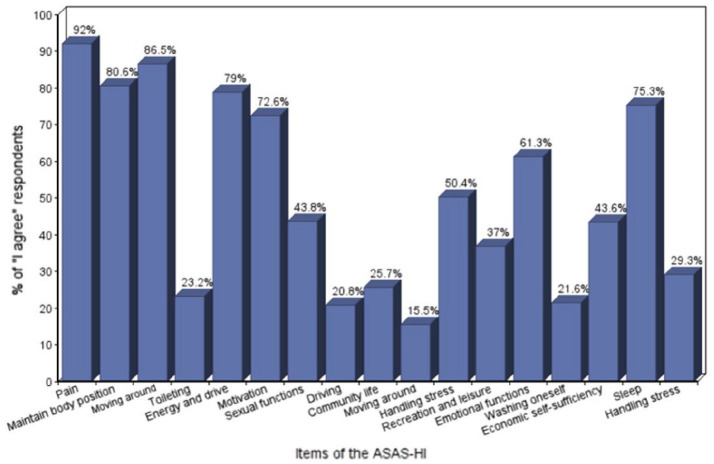
According to the ASAS-HI, 147 patients (25.0% of the total) presented poor health and functioning. The results in the different countries ranged from 21% in United Kingdom to 37.3% in France. Mean ASAS-HI score (SD) for all of the patients was 8.6 (3.9), ranging across 8.7 (3.8) in Spain to 10.5 (3.5) in Italy. The most affected domains of health and functioning were pain (92% of respondents), moving around (86.5%), maintenance of body position (80.6%), energy/drive (79.0%) and sleep (75.3%) (Figure 2). Distribution of the results of the total ASAS-HI scores per patient can be seen in Supplementary Figure 2.
Figure 2.
Results in the different items of the ASAS Health Index.
ASAS-HI, Assessment of SpondyloArthritis International Society Health Index.
Patients were stratified according to their total scores in the ASAS-HI as having either an acceptable/good versus poor state of health and functioning, as shown in Table 1. Differences between the two groups for certain characteristics were observed. Patients with poor health status versus those with an acceptable/good state of health were more frequently smokers (29.9% versus 18.9%, p < 0.01), had a higher body mass index (27.6 versus 26.4, p = 0.05), were less frequently employed (28.6% versus 40.7%, p = 0.02), more frequently reported a comorbidity such as psoriasis (21.1% versus 11.1%, p < 0.01), hypercholesterolemia (16.3% versus 4.5%, p < 0.001), diabetes (10.9% versus 2.0%, p < 0.001), kidney-related disease (6.8% versus 3.0%, p = 0.048), respiratory disease (11.6% versus 5.5%, p = 0.02), depression (22.4% versus 13.6%, p = 0.01), took more painkillers (42.2% versus 21.1%, p < 0.001) and/or oral corticosteroids (17.7% versus 10.0%, p = 0.02).
In addition, 82 (14.0%) patients reported bad or very bad self-perceived health status. According to the WHO-5, more than half of patients (56.5%; n = 330) reported poor well-being; total mean WHO-5 score was 46.3 (23.1) for all respondents. Compared with other RMDs, axSpA patients reported worse health status according to the WHO-5 questionnaire, and higher rates of poor well-being, also according to this index (Supplementary Table 2). In patients with axSpA, a statistically significant correlation was found between all secondary outcomes and the ASAS-HI, with the self-perceived health status being the most highly correlated, although still only moderate (Table 2). Remarkably, almost half of patients (46.8%; n = 274) reported that their self-perceived health status worsened during lockdown. In fact, only 7.0% (n = 41) declared feeling better than before.
Table 2.
Health status according to secondary outcomes.
| Secondary outcomes | Total (N = 587) |
Good/acceptable
health (ASAS-HI < 12) n = 440 (75%) |
Poor
health (ASAS-HI ⩾ 12) n = 147 (25%) |
p value | Correlation with ASAS-HI Spearman’s r |
|---|---|---|---|---|---|
| WHO-5 (0–100) | –0.212 † | ||||
| WHO-5 (0–100), n = 584 a | 46.3 (23.1) | 48.3 (22.1) | 40.2 (25.0) | <0.001 | |
| WHO-5 Poor well-being ⩽ 50 b | 330 (56.5) | 233 (53.2) | 97 (66.4) | 0.005 | |
| Self-perceived general health (1–5) | |||||
| Self-perceived general health b | 0.326 † | ||||
| Very good | 33 (5.6) | 31 (7.1) | 2 (1.4) | <0.001 | |
| Good | 214 (36.6) | 187 (42.6) | 27 (18.5) | ||
| Fair | 256 (43.8) | 173 (39.4) | 83 (56.8) | ||
| Bad | 69 (11.8) | 39 (8.9) | 30 (20.5) | ||
| Very bad | 13 (2.2) | 9 (2.1) | 4 (2.7) | ||
| Change in health status during lockdown b | |||||
| Much better than before | 6 (1.0) | 6 (1.4) | 0 | 0.001 | |
| Moderately better | 35 (6.0) | 27 (6.2) | 8 (5.5) | ||
| Same as before | 270 (46.0) | 220 (50.1) | 50 (34.2) | ||
| Moderately worse | 220 (37.6) | 155 (35.3) | 65 (44.5) | ||
| Much worse than before | 54 (9.2) | 31 (7.1) | 23 (15.8) | ||
ASAS-HI, Assessment of SpondyloArthritis International Society Health Index; WHO-5, World Health Organization-Five Well-Being Index; HADS, Hospital Anxiety and Depression Scale.
Results are shown as absolute numbers (percentages) or expressed as the mean ± standard deviation (N = 587, unless specified).
Mean (SD).
n (%).
p < 0.001.
Lifestyle and daily activities
Reported changes in lifestyle, daily activities, employment and healthcare resource utilization are shown in Table 3. On the subject of health habits, one of three smokers (33.0%, n = 58) reported increased smoking and one of five respondents (20.0%, n = 78) reported increased alcohol consumption. Almost half of patients (49.6%, n = 291) reported walking outside more than 1 day a week, whereas nearly half of the respondents who used to practise physical activity (41.7%, n = 175) did not continue to do so.
Table 3.
Impact in lifestyle, daily activities, employment and healthcare resources utilization during COVID-19 lockdown.
| Total (n = 587) | Good/acceptable health (ASAS-HI < 12) (n = 440) |
Poor
health (ASAS-HI ⩾ 12) (n = 147) |
p value | |
|---|---|---|---|---|
| Lifestyle factors | ||||
| Physical activity prepandemic (yes) a | 417 (71.0) | 321 (73.0) | 96 (65.3) | 0.09 |
| Physical activity in pandemics (yes), n = 417 | 243 (58.3) | 201 (62.6) | 42 (43.8) | 0.001 |
| Walk outside more than 1 day | 291 (49.6) | 236 (53.6) | 55 (37.4) | 0.001 |
| Smoking habit, n = 176 | ||||
| More than before | 58 (33.0) | 35 (29.9) | 23 (39.0) | 0.34 |
| Same as before | 54 (30.7) | 41 (35.0) | 13 (22.0) | |
| Less than before | 23 (13.1) | 15 (12.8) | 8 (13.6) | |
| Stop smoking | 41 (23.3) | 26 (22.2) | 15 (25.4) | |
| Drinking, n = 390 | ||||
| More than before | 78 (20.0) | 54 (18.0) | 24 (26.7) | 0.06 |
| Same as before | 142 (36.4) | 118 (39.3) | 24 (26.7) | |
| Less than before | 52 (13.3) | 36 (12.0) | 16 (17.8) | |
| Stop drinking | 118 (30.3) | 92 (30.7) | 26 (28.9) | |
| Employment | ||||
| Keyworker (yes) a | 113 (19.3) | 90 (20.5) | 23 (15.6) | 0.23 |
| Changes in work, n = 285 | ||||
| Similar as before | 37 (13.0) | 29 (13.4) | 8 (11.6) | 0.22 |
| Presential work but changes (time/place) | 39 (13.7) | 30 (13.9) | 9 (13.0) | |
| Teleworking working from home | 129 (45.3) | 104 (48.1) | 25 (36.2) | |
| Temporary sick leave | 33 (11.6) | 22 (10.2) | 11 (15.9) | |
| Work cessation | 47 (16.5) | 31 (14.4) | 16 (23.2) | |
| Healthcare resources utilization | ||||
| Rheumatologist visits before the COVID-19 pandemic lockdown a | ||||
| Every 2 months or more | 41 (7.0) | 28 (6.4) | 13 (8.8) | 0.13 |
| Every 3–4 months | 135 (23.0) | 97 (22.0) | 38 (25.9) | |
| Every 6 months | 236 (40.2) | 173 (39.3) | 63 (42.9) | |
| Yearly or less frequently | 175 (29.8) | 142 (32.3) | 33 (22.4) | |
| Resources during the pandemic lockdown | ||||
| Scheduled visit with rheumatologist | 257 (43.8) | 195 (44.3) | 62 (42.2) | 0.35 |
| Completed appointment with rheumatologist, n = 256 | 91 (35.5) | 66 (34.0) | 25 (40.5) | 0.37 |
| Access to primary care (yes), n = 153 | 95 (62.1) | 73 (64.0) | 22 (56.4) | 0.45 |
| Change of treatment in pandemics (yes), n = 565 | 73 (12.9) | 48 (11.3) | 25 (17.7) | 0.06 |
| Quality of information received (1–5), n = 383 | 2.81 (1.5) | 2.86 (1.5) | 2.63 (1.6) | 0.19 |
ASAS-HI, Assessment of SpondyloArthritis International Society Health Index.
These parameters reflect baseline situation. Results are shown as absolute numbers (percentages) or expressed as the mean ± standard deviation (N = 587, unless specified).
Concerning employment, only 37 (13.0%) had no change in their job routine. With regard to healthcare resources utilization, of the 257 patients who had an appointment scheduled with their rheumatologist, only 91 (35.5%) were able to keep the visit. In total, 245 patients (41.7%) reported not having received any specific information on how COVID-19 could affect their axSpA. Patients rated the quality of information they received from 0 (worst quality) to 5 (best quality), with a mean of 2.8 (1.5).
Explanatory factors for overall health status or worsening health status
In the multivariate analysis, aspects directly related with poor overall health and functioning included being a smoker (OR = 1.98; p = 0.03), having diabetes (OR = 4.89; p = 0.02), and taking painkillers (OR = 2.82; p < 0.001) or oral corticosteroid use (OR = 2.20; p = 0.04). Engaging in physical activity during the pandemic (OR = 0.54; p = 0.02) and remaining actively at work (OR = 0.48; p = 0.01), however, were inversely associated with a poor health and functioning (Table 4).
Table 4.
Factors associated with poor functioning and overall health (ASAS-HI ⩾ 12) (N = 587).
| Qualitative factors | Univariable logistic analysis | Multivariable logistic analysis | ||
| OR | 95% CI | OR | 95% CI | |
| Sociodemographics | ||||
| Gender: Male | 0.78 | 0.51–1.19 | ||
| Smoking status: Smoker | 1.84 | 1.20–2.81 | 1.98 | 1.07–3.68 |
| Education: University | 0.81 | 0.56–1.19 | ||
| Marital status: Married | 1.11 | 0.73–1.70 | ||
| Employment status: Working | 0.58 | 0.39–0.88 | 0.48 | 0.27–0.85 |
| Patient organization: Member | 0.59 | 0.612–1.32 | ||
| Comorbidities | ||||
| Hypertension | 1.69 | 1.04–2.75 | 0.93 | 0.41–2.10 |
| Diabetes | 5.85 | 2.52–13.54 | 4.89 | 1.35–17.65 |
| Hypercholesterolemia | 4.10 | 2.19–7.67 | 2.32 | 0.92–5.85 |
| Kidney-related disease | 2.40 | 1.03–5.60 | 1.25 | 0.39–4.03 |
| Respiratory disease | 2.27 | 1.18–4.35 | 1.51 | 0.59–3.81 |
| Depression | 1.83 | 1.14–2.94 | 1.50 | 0.73–3.08 |
| Anxiety | 1.56 | 0.95–2.54 | ||
| Extra-musculoskeletal manifestations | ||||
| Psoriasis | 2.07 | 1.26–3.40 | 1.83 | 0.92–3.62 |
| Drugs | ||||
| Painkillers | 2.72 | 1.82–4.06 | 2.82 | 1.58–5.05 |
| Oral corticosteroids | 1.93 | 1.14–3.27 | 2.20 | 1.02–4.76 |
| Country | ||||
| Country: UK | 0.68 | 0.46–1.01 | ||
| Country: France | 1.94 | 1.14–3.32 | 1.37 | 0.63–2.98 |
| Country: Italy | 1.52 | 0.50–4.12 | ||
| Country: Portugal | 0.90 | 0.24–3.30 | ||
| Country ref.: Spain | ||||
| Habits and healthcare | ||||
| Physical activity prepandemics | 0.70 | 0.47–1.04 | ||
| Physical activity in pandemics | 0.46 | 0.29–0.74 | 0.54 | 0.31–0.92 |
| Visit to rheumatologist. Yes | 0.80 | 0.52–1.25 | ||
| Key worker. Yes | 0.72 | 0.44–1.19 | ||
| Walk outside at least 2 days | 0.52 | 0.35–0.75 | 0.64 | 0.37–1.10 |
| Medication change | 0.59 | 0.35–1.01 | ||
| Quantitative factors | B | B | ||
| Age | –0.01 | 0.98–1.01 | ||
| BMI (n = 430) | 0.04 | 1.00–1.08 | ||
| Quality of received information (0–5) | –0.10 | 0.70–1.05 | ||
ASAS-HI, Assessment of SpondyloArthritis International Society Health Index; BMI, body mass index; 95% CI, 95% confidence interval; OR, odds ratio. Boldfaced values indicate statistical significance.
As for changes in their health status during lockdown, patients who reported a worsening of health were younger (48.6 versus 51.1 years, p = 0.02), more frequently females (78.1% versus 63.3%, p < 0.001) and smokers (26.3% versus 17.7%, p = 0.01), higher prevalence of psoriasis (17.9% versus 10.0%, p = 0.005) and respiratory disease (9.5% versus 4.8%, p = 0.03), and took more painkillers (32.5% versus 21.1%, p = 0.002) and nonsteroidal anti-inflammatory drugs (NSAIDs) (51.8% versus 41.5%, p = 0.01) compared with those who reported at least similar level of health or better than before the pandemic. Patients who maintained the same health status or better engaged more frequently in physical activity (69.3% versus 45.0%, p < 0.001), however, more frequently walked at least once a day (53.7% versus 44.5%, p = 0.03) and were more frequently drinkers (19.6% versus 12.4%, p = 0.02) than those who experienced a worsening health status. In the multivariate analysis, male gender (OR = 1.84; p = 0.01) and doing physical activity during pandemic (OR = 2.62; p < 0.001) were significantly associated with at least a similar level of health or better compared with that before the pandemic, while taking painkillers was inversely associated (OR = 0.59; p = 0.03) with this outcome.
Discussion
In this study, we explore the health status of 587 axSpA patients in five European countries during the first wave of the COVID-19 pandemic and lockdown, from their own perspective. To our knowledge, our analysis is the first to focus on the impact of the COVID-19 pandemics and lockdown in axSpA patients in a multinational setting. Several important observations have been made.
First, our results indicated that one of four patients with axSpA reported poor overall health and functioning according to the ASAS-HI, with the most affected domains being pain, moving around, maintenance of body position, energy/drive and sleep. Of note, in the assessment of self-perceived health status, one in seven patients reported themselves to be ‘bad’ or ‘very bad’. In addition, more than half of patients experienced poor well-being. In fact, around half of patients reported that their health worsened during lockdown, whereas less than one of 10 declared feeling better than before. These data are relevant as they reflect quite high and consistent rates of poor health in the axSpA population consistently, using different instruments. These high rates of poor health, both self-perceived and as shown by the ASAS-HI, demonstrate that although the SARS-CoV2 had a significant clinical effect on those who contracted the virus, the overall pandemic and lockdown measures have had far-reaching health consequences for axSpA patients as a whole. In fact, SARS-CoV2 infection represents a syndemic that may interact with and exacerbate pre-existing rheumatic conditions, as recently published. 21
In the assessment of lifestyle and daily activities, one of three patients reported increased smoking and one of five reported increased drinking. 22 An association between smoking and higher disease activity and structural damage has been well established in axSpA. 23 Hence, smoking cessation represents a steppingstone in the quest for better health outcomes. Some data that were unexpected were that patients who reported alcohol consumption maintained the same health status or better than those who did not. As the threshold that was established was three drinks or more in a week, the group that reported drinking, however, might include patients who occasionally complemented meals with a small amount of wine or beer, rather than excessive alcohol use.
Interestingly, engaging in physical activity and being employed were associated with better outcomes. This is especially relevant considering the mounting evidence that unveils how the routine disruptions imposed by the COVID-19 pandemic have led to a significant reduction in physical activity in different groups of patients, as well as an increase in sedentary behaviours.24,25 In our analysis, among the patients who reported engaging in physical activity before the pandemic, almost half halted doing so. In patients with axSpA, physical inactivity is not only a modifiable risk factors for cardiovascular disease and mortality, but has also been linked to higher disease activity and worse function. 26 This is sustained by our finding that maintaining physical activity was associated with a similar or better health status when assessing changes in health during the pandemic. These results support the main recommendations on nonpharmacological management by the last update of the ASAS-EULAR management recommendations for axSpA, which state that ‘patients should be educated about axSpA and encouraged to exercise on a regular basis and stop smoking’. 10
Comparing our results on ASAS-HI explanatory factors with previous studies, it is important to note that the ASAS-HI was developed fairly recently, and therefore, studies utilizing this outcome measure are scarce. In a recent study using data from the Catholic Axial Spondyloarthritis Cohort (CASCO), high NSAID intake and structural radiographic damage were positively associated with ASAS-HI, whereas higher economic status and alcohol consumption were negatively associated with ASAS-HI. 27 Although our study yielded some different predictors, it cannot be directly compared as it was conducted in a pandemic setting. Concerning the WHO-5 questionnaire addressing axSpA, in a sample of 1736 patients, 59% were found to have depressive symptoms/impaired well-being (WHO-5 ⩽ 50), yielding a mean WHO-5 score of 44.7. 28 These rates are quite similar to these reported in our study, in which 56.5% of patients reported poor well-being (WHO-5 ⩽ 50), with a mean score of 46.3. It is worth noting that the populations being compared, however, are not the same; thus, it is not possible to draw definitive conclusions from this comparison. Nonmedical factors may have influenced health outcomes. In this regard, the REUMAVID included questions on social determinants of health such as education, marital status or employment. Among these, employment status yielded the greatest impact on overall health and functioning, probably due to the fact that it has been the most affected. Only 13% of patients in the analysis reported to be working in a similar manner as before, which was even less than the 16.5% patients who reported stopping their work due to being fired, furloughed, or business closure. A reduction of stimuluses may lead to decreases in reinforcement or even to boredom and such factors are associated with depression. 29 It is worth noting that being employed was linked to better outcomes. It is possible that maintaining a daily work routine made these patients experience a greater sense of normality, which contributed to a better overall feeling of healthiness. Likewise, addressing any social determinant of health appropriately is deemed necessary for improving overall health.
Finally, it is worth noting that two of three appointments with the rheumatologists that were scheduled during the study period were ultimately cancelled, and approximately one of three respondents reported being unable to contact their primary care physician. Based on this data, we can assume that the health needs created by the COVID-19 pandemic went well beyond the capacity of our healthcare system during this period, negatively impacting axSpA patients. Despite several urgent calls to action to rheumatology departments, 30 it is likely that needs of patients could not had been fulfilled during that time. Fortunately, it does not appear that having an inflammatory rheumatic disease leads to a higher risk of severe COVID-19 respiratory complications or death in these patients compared with the general population. 31 Some biological drugs, such as rituximab and Janus kinase inhibitors (JAKi), have been associated with worse COVID-19 severity in patients with rheumatoid arthritis, but these outcomes have not been shown with biologic disease-modifying anti-rheumatic drugs (bDMARDs), which are mostly used in axSpA. 32
Some strengths and limitations should be acknowledged in our study. Using the ASAS-HI in this research can be regarded as an important strength, as the concept of overall health and functioning, as conceptualized by the ICF, encompasses relevant aspects of both functioning and well-being in patients with axSpA. It is also to be noted that this study assessed a large sample of unselected axSpA patients from five European countries. As limitations, the cross-sectional design of the survey resulted in a single time point assessment that may have biased the results for some variables. Moreover, to perform this analysis, we only included axSpA patients for whom we had a valid assessment of the ASAS-HI scale, which may have had some impact on the population selection. Because the ASAS-HI scale was exclusively validated in SpA, and the REUMAVID survey did not address healthy controls, we could not compare these results with a group of healthy patients, which possibly hindered our interpretation of the results. In addition, the results show slight variabilities due to the use of different indices. Although all of the validated measurement instruments employed in this study have demonstrated good psychometric properties, there are subtle differences between them. While ASAS-HI is a scale that was specifically developed and validated in axSpA, the WHO-5 was developed in a general population setting. While ASAS-HI purports to assess the construct of ‘functioning, disability and health’, WHO-5 aims to evaluate subjective psychological well-being by measuring five domains that are related to mental well-being, such as positive mood, vitality, and general interest. Although the WHO-5 has been shown to be a sensitive and specific tool for the screening of depression across many different fields, it has not been specifically validated in patients with axSpA. In addition, the sex distribution of axSpA does not match what was expected; there is an over-representation of women as compared with men. 33 This might be explained by reports suggesting that women might be more prone to participate in online surveys, which may be a cause of these over-representation. 34 As worse outcomes have been reported in women with axSpA than in men 35 in relation to disease activity, pain or fatigue, a greater impact of the disease than expected might be reflected in our study. In any case, our study provides a relevant sample of patients to assess the patient’s perspective that may help to understand the limitations imposed by the pandemic and the impact in overall health in patients with axSpA.
Conclusion
In summary, these data highlight the negative impact of the first wave of the COVID-19 pandemic and lockdown on the health and well-being of patients with axSpA in Europe, with poor health and functioning according to the ASAS-HI, and worsened self-perceived health status reported by a quarter and half of participants, respectively. Several modifiable aspects were identified, such as nonsmoking, physical activity and being employed, which were associated with better health and functioning outcomes.
Supplemental Material
Supplemental material, sj-docx-1-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-2-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-3-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-4-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease
Acknowledgments
We would like to thank all patients who completed the survey as well as all of the patient organizations that participated in the REUMAVID study, including the Cyprus League Against Rheumatism from Cyprus, the Association Française de Lutte Anti-Rhumatismale from France, the Hellenic League Against Rheumatism from Greece, the Associazione Nazionale Persone con Malattie Reumatologiche e Rare from Italy, the Portuguese League Against Rheumatic Diseases from Portugal, the Spanish Federation of Spondyloarthritis Associations, the Spanish Patients’ Forum, UNiMiD, Spanish Rheumatology League, Andalusian Rheumatology League, Catalonia Rheumatology League and Galician Rheumatology League from Spain, and the National Axial Spondyloarthritis Society, National Rheumatoid Arthritis and Arthritis Action from the UK. We would like to thank also the Spanish Foundation of Rheumatology for providing medical writing/editorial assistance (FERBT2021) during the preparation of the manuscript.
Footnotes
Author Contribution: Diego Benavent: Conceptualization; Formal analysis; Investigation; Visualization; Writing – original draft; Writing – review & editing.
Marco Garrido Cumbrera: Conceptualization; Data curation; Investigation; Supervision; Validation; Writing – review & editing.
Chamaida Plasencia-Rodríguez: Conceptualization; Formal analysis; Supervision; Writing – review & editing
Helena Marzo-Ortega: Methodology; Validation; Writing – review & editing.
Laura Christen: Methodology; Writing – review & editing.
José Correa-Fernández: Formal analysis; Methodology; Supervision.
Pedro Plazuelo-Ramos: Conceptualization; Investigation.
Dale Webb: Conceptualization; Investigation; Writing – review & editing.
Victoria Navarro-Compan: Conceptualization; Investigation; Methodology; Project administration; Supervision; Validation; Visualization; Writing – review & editing.
Conflict of interest statement: The authors declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: DB reports honoraria/research support from AbbVie, Novartis and Roche. CP received grants/speaker/research supports from Pfizer, Sanofi, Novartis, Roche and Lilly. HM have grants and/or honoraria from Abbvie, Celgene, Janssen, Elli-Lilly, MSD, Novartis, Pfizer and UCB. LC is an employee of Novartis Pharma AG. DW has received grant funding from AbbVie, Biogen, Janssen, Lilly, Novartis and UCB. VN-C reports honoraria/research support from AbbVie, BMS, Janssen, Lilly, MSD, Novartis, Pfizer, Roche and UCB.
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article. REUMAVID study was supported by Novartis Pharma AG.
Data availability statement: The data underlying this article were provided by the REUMAVID Committee under licence/by permission. Data will be shared on request to the corresponding author with permission of the REUMAVID Committee.
Ethics: REUMAVID was first approved by the ethical committee of University Hospital La Paz under the code PI-4121 and was subsequently approved in all other participating countries as legally required.
ORCID iD: Diego Benavent  https://orcid.org/0000-0001-9119-5330
https://orcid.org/0000-0001-9119-5330
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Diego Benavent, Rheumatology Service, IdiPAZ, La Paz University Hospital, Paseo de la Castellana, 261, Madrid 28046, Spain.
Marco Garrido-Cumbrera, Health & Territory Research, Universidad de Sevilla, Seville, Spain.
Chamaida Plasencia-Rodríguez, Rheumatology Service, IdiPAZ, La Paz University Hospital, Madrid, Spain.
Helena Marzo-Ortega, NIHR Leeds Biomedical Research Centre, LTHT and LIRMM, University of Leeds, Leeds, UK.
Laura Christen, Novartis Pharma AG, Basel, Switzerland.
José Correa-Fernández, Health & Territory Research, Universidad de Sevilla, Seville, Spain.
Pedro Plazuelo-Ramos, Spanish Federation of Spondyloarthritis Associations (CEADE), Madrid, Spain.
Dale Webb, NASS, London, UK.
Victoria Navarro-Compán, Rheumatology Service, IdiPAZ, La Paz University Hospital, Madrid, Spain.
References
- 1. Roux CH, Brocq O, Gerald F, et al. Impact of home confinement during the COVID-19 pandemic on medication use and disease activity in spondyloarthritis patients. Arthritis Rheumatol 2020; 72: 1771–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liew JW, Castillo M, Zaccagnino E, et al. Patient-reported disease activity in an axial spondyloarthritis cohort during the COVID-19 pandemic. ACR Open Rheumatol 2020; 2: 533–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seyahi E, Poyraz BC, Sut N, et al. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol Int 2020; 40: 1229–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Roux CH, Brocq O, Gerald F, et al. Clinical impact of COVID-19 on a French population of spondyloarthritis patients. Clin Rheumatol 2020; 39: 3185–3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Marzo-Ortega H, Whalley S, Hamilton J, et al. COVID-19 in axial spondyloarthritis care provision: helping to straighten the long and winding road. Lancet Rheumatol 2021; 3: e11–e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sirotich E, Dillingham S, Grainger R, et al. Capturing patient-reported outcomes during the COVID-19 pandemic: development of the COVID-19 global rheumatology alliance patient experience survey. Arthritis Care Res (Hoboken) 2020; 72: 871–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dejaco C, Alunno A, Bijlsma JW, et al. Influence of COVID-19 pandemic on decisions for the management of people with inflammatory rheumatic and musculoskeletal diseases: a survey among EULAR countries. Ann Rheum Dis 2021; 80: e171. [DOI] [PubMed] [Google Scholar]
- 8. Favalli EG, Monti S, Ingegnoli F, et al. Incidence of COVID-19 in patients with rheumatic diseases treated with targeted immunosuppressive drugs: what can we learn from observational data? Arthritis Rheumatol 2020; 72: 1600–1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ciurea A, Papagiannoulis E, Bürki K, et al. Impact of the COVID-19 pandemic on the disease course of patients with inflammatory rheumatic diseases: results from the Swiss Clinical Quality Management cohort. Ann Rheum Dis 2021; 80: 238–241. [DOI] [PubMed] [Google Scholar]
- 10. van der Heijde D, Ramiro S, Landewé R, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 2017; 76: 978–991. [DOI] [PubMed] [Google Scholar]
- 11. van Echteld I, Cieza A, Boonen A, et al. Identification of the most common problems by patients with ankylosing spondylitis using the international classification of functioning, disability and health. J Rheumatol 2006; 33: 2475–2483. [PubMed] [Google Scholar]
- 12. Chakravarty SD, Abell J, Leone-Perkins M, et al. A novel qualitative study assessing patient-reported outcome measures among people living with psoriatic arthritis or ankylosing spondylitis. Rheumatol Ther 2021; 8: 620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kiltz U, van der Heijde D, Boonen A, et al. Development of a health index in patients with ankylosing spondylitis (ASAS HI): final result of a global initiative based on the ICF guided by ASAS. Ann Rheum Dis 2015; 74: 830–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Functioning and Disability Reference Group. The ICF: an overview. Geneva: World Heal Organization, 2010. [Google Scholar]
- 15. Alonso-Castro S, Pardo E, Charca L, et al. Performance of the ASAS health index for the evaluation of spondyloarthritis in daily practice. J Rheumatol 2020; 47: 1483–1489. [DOI] [PubMed] [Google Scholar]
- 16. Chen H-H, Chen Y-M, Lai K-L, et al. Gender difference in ASAS HI among patients with ankylosing spondylitis. PLoS ONE 2020; 15: e0235678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Health & Territory Research. about REUMAVID – Reumavid, https://reumavid.com/home-reumavid/about-reumavid/ (accessed 28 April 2021).
- 18. Garrido-Cumbrera M, Marzo-Ortega H, Christen L, et al. Assessment of impact of the COVID-19 pandemic from the perspective of patients with rheumatic and musculoskeletal diseases in Europe: results from the REUMAVID study (phase 1). RMD Open 2021; 7: e001546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kiltz U, van der Heijde D, Boonen A, et al. Measurement properties of the ASAS Health Index: results of a global study in patients with axial and peripheral spondyloarthritis. Ann Rheum Dis 2018; 77: 1311–1317. [DOI] [PubMed] [Google Scholar]
- 20. Topp CW, Østergaard SD, Søndergaard S, et al. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015; 84: 167–176. [DOI] [PubMed] [Google Scholar]
- 21. Nikiphorou E, Alpizar-Rodriguez D, Gastelum-Strozzi A, et al. Syndemics & syndemogenesis in COVID-19 and rheumatic and musculoskeletal diseases: old challenges, new era. Rheumatology 2021; 60: 2040–2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Plurphanswat N, Kaestner R, Rodu B. The effect of smoking on mental health. Am J Health Behav 2017; 41: 471–483. [DOI] [PubMed] [Google Scholar]
- 23. Zhao SS, Goodson NJ, Robertson S, et al. Smoking in spondyloarthritis: unravelling the complexities. Rheumatology (Oxford) 2020; 59: 1472–1481. [DOI] [PubMed] [Google Scholar]
- 24. Meyer J, McDowell C, Lansing J, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health 2020; 17: 6469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog Cardiovasc Dis 2020; 63: 531–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sveaas SH, Bilberg A, Berg IJ, et al. High intensity exercise for 3 months reduces disease activity in axial spondyloarthritis (axSpA): a multicentre randomised trial of 100 patients. Br J Sports Med 2020; 54: 292–297. [DOI] [PubMed] [Google Scholar]
- 27. Min HK, Lee J, Ju JH, et al. Predictors of Assessment of Spondyloarthritis International Society (ASAS) health index in axial spondyloarthritis and comparison of ASAS health index between ankylosing spondylitis and nonradiographic axial spondyloarthritis: data from the Catholic Axial Spondyloarthritis COhort (CASCO). J Clin Med 2019; 8: 467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Redeker I, Callhoff J, Hoffmann F, et al. Determinants of diagnostic delay in axial spondyloarthritis: an analysis based on linked claims and patient-reported survey data. Rheumatol (United Kingdom) 2019; 58: 1634–1638. [DOI] [PubMed] [Google Scholar]
- 29. Kanter JW, Busch AM, Weeks CE, et al. The nature of clinical depression: symptoms, syndromes, and behavior analysis. Behav Anal 2008; 31: 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lewandowski LB, Hsieh E. Global rheumatology in the time of COVID-19. Lancet Rheumatol 2020; 2: e254–e255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Serling-Boyd N, D’Silva KM, Hsu TY, et al. Coronavirus disease 2019 outcomes among patients with rheumatic diseases 6 months into the pandemic. Ann Rheum Dis 2021; 80: 660–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sparks JA, Wallace ZS, Seet AM, et al. Associations of baseline use of biologic or targeted synthetic DMARDs with COVID-19 severity in rheumatoid arthritis: results from the COVID-19 Global Rheumatology Alliance physician registry. Ann Rheum Dis 2021; 80: 1137–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang R, Ward MM. Epidemiology of axial spondyloarthritis: an update. Curr Opin Rheumatol 2018; 30: 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Smith WG. Does gender influence online survey participation? A record-linkage analysis of university faculty online survey response behavior, 2008, https://eric.ed.gov/?id=ED501717
- 35. Mease PJ, McLean RR, Dube B, et al. Comparison of men and women with axial spondyloarthritis in the US-based Corrona Psoriatic Arthritis/Spondyloarthritis Registry. J Rheumatol 2021; 48: 1528–1536. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-2-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-3-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-4-tab-10.1177_1759720X211066685 for Poor health and functioning in patients with axial spondyloarthritis during the COVID-19 pandemic and lockdown: REUMAVID study (phase 1) by Diego Benavent, Marco Garrido-Cumbrera, Chamaida Plasencia-Rodríguez, Helena Marzo-Ortega, Laura Christen, José Correa-Fernández, Pedro Plazuelo-Ramos, Dale Webb and Victoria Navarro-Compán in Therapeutic Advances in Musculoskeletal Disease