Abstract
Background
Musculoskeletal physiotherapy practice rapidly adopted telehealth during the COVID-19 pandemic, providing a unique opportunity to evaluate the experiences and attitudes of people who would not usually engage with these services.
Methods
A sequential mixed-methods study recruited people with musculoskeletal pain conditions accessing Australian private practice physiotherapist services. Part 1 involved an online survey of telehealth services accessed, treatments and resources provided, self-reported global change in condition, and attitudes toward telehealth. Part 2 involved semi-structured interviews with a subset of survey participants, exploring experiences and attitudes towards telehealth. Quantitative data was reported descriptively. Qualitative data was evaluated using inductive thematic analysis.
Results
172 participants responded to the survey, and 19 were interviewed. 95% accessed video-based telehealth, and 85% reported condition improvement. 84% agreed it was an efficient use of their time, 75% agreed it was financially viable, and 73% agreed their condition was accurately diagnosed. 62% percent believed telehealth should be less expensive than in-person services. Qualitative analysis revealed four themes (17 subthemes), including (i) telehealth had value, but generally perceived as inferior to in-person care; (ii) challenges related to assessment, diagnosis, ‘hands on’ treatment, observation, communication, and technology; (iii) advantages to access safe, expert, and convenient care; and (iv) importance of supportive technology, including video and supplementary resources.
Conclusion
Physiotherapist telehealth services provided to people with musculoskeletal pain during the pandemic was valued. However, telehealth was generally perceived as inferior to traditional in-person care, and may be best used as part of a hybrid model of care.
Keywords: Telehealth, Musculoskeletal, Physiotherapy, Coronavirus
Telehealth involves remotely delivered phone- or video-based patient-clinician interaction via synchronous or asynchronous means to facilitate healthcare (Dorsey and Topol, 2016). Advantages of telehealth include better access to care for people living in rural and remote areas, reduced travel time and costs, and flexible work arrangements for clinicians (Cottrell and Russell, 2020; Turolla et al., 2020). Providing guideline recommended care, such as patient education and exercise therapy for common musculoskeletal pain conditions through telehealth has been reported to produce similar improvements in pain and disability when tested against in-person care (Cottrell et al., 2017).
Telehealth uptake for physiotherapy services in people with musculoskeletal pain conditions was slow prior to the coronavirus (COVID-19) pandemic (Cottrell and Russell, 2020). However, government-imposed restrictions on in-person care during the pandemic resulted in rapid adoption of telehealth services internationally (Malliaras et al., 2021; Rethorn et al., 2021), providing a unique opportunity for real-world evaluation of the experience and attitudes toward this underused method of delivering physiotherapy. A key facilitator of this rapid uptake was improved reimbursement models for telehealth in countries such as Australia (Tanne et al., 2020). Physiotherapists in Australia surveyed during the pandemic generally see telehealth as part of their role (Bennell et al., 2021; Malliaras et al., 2021). Yet, our survey of 827 allied health clinicians, mostly Australian physiotherapists, indicated just one in five felt adequately trained to provide telehealth to people with musculoskeletal pain conditions (Malliaras et al., 2021). Additionally, only 42% believed telehealth was as effective as in-person care, and only 25% believed patients valued telehealth as much as in-person care (Malliaras et al., 2021). This suggests that physiotherapists adopted telehealth due to the necessity, and sustained use post-pandemic-related restrictions is unlikely without further education and training.
Qualitative findings from clinical trials prior to the pandemic provide insight into the acceptability, challenges, and enablers to the uptake of telehealth from the perspective of chronic musculoskeletal pain patients (Fernandes et al., 2021). Key enablers reported include convenience and patient empowerment, while key challenges were described as difficulties establishing a patient-therapist relationship, technological barriers, and limited digital literacy (Fernandes et al., 2021). Patient insights about physiotherapy telehealth services during the pandemic can guide future implementation strategies to support uptake and sustainability beyond the pandemic. A large Australian survey (n = 1369) indicated that 62% of adults rated their experience as “just as good” or “better” than in-person medical appointments, and on average telehealth services would be moderately to very useful beyond the pandemic (Isautier et al., 2020). A mixed-methods survey study related specifically to physiotherapy practice in Australia reported generally positive experiences of patients with video-based telehealth during the pandemic (Bennell et al., 2021). However, qualitative evaluation of patient experiences and attitudes were absent from this study. This study aimed to explore the experiences and attitudes of patients receiving physiotherapy telehealth services for musculoskeletal pain conditions during the COVID-19 pandemic.
1. Methods
1.1. Design
We used a sequential mixed-methods explanatory design. In Part 1 (quantitative) we surveyed people with musculoskeletal pain receiving telehealth care from physiotherapists throughout Australia during the country's nationwide lockdown in May 2020. Part 2 (qualitative) was designed to enrich our understanding of findings from Part 1, by exploring experiences and attitudes with a subset of survey participants. Quantitative and qualitative work can be mutually illuminating, with the combination providing rich knowledge (Andrew and Halcomb, 2006).
Reporting of this mixed-methods study has been guided by the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) (Eysenbach, 2004), Consolidated criteria for reporting qualitative research (COREQ) (Tong et al., 2007) Checklist and the Good Reporting of A Mixed Methods (GRAMM) Study Checklist (O'Cathain et al., 2008).
2. Part 1 – survey
2.1. Participant recruitment
We contacted Australian physiotherapy clinics within our national networks (>200 clinics across all states and territories) and asked them to alert patients via printable flyers, which provided details about the study and the electronic survey link containing the information sheet and consent form. Prospective participants were able to read an electronic information statement on the first page of the survey and complete an electronic consent form.
2.2. Data collection and analysis
Each participant completed an online survey (live between June and September 2020) including questions related to demographics, telehealth services accessed (amount, type, platform), treatments and resources provided via telehealth, self-reported global rating of change (Kamper et al., 2009), and attitudes toward telehealth (Additional file 1). The survey was informed by previous telehealth research and the theoretical domains framework (Huijg et al., 2014; Michie et al., 2011), and developed by five researchers, piloted with five patients (male and female, and varying ages). The final survey was administered using Qualtrics software (Qualtrics, Provo, Utah). All surveys were completed anonymously, with informed consent provided on the opening page.
3. Part 2 – semi-structured interviews
3.1. Participant recruitment
Participants who had agreed and consented to be contacted via email for Part 2 within the larger survey were emailed an invitation to participate. Purposive sampling was used to ensure that both males and females, and varying ages, were represented as adequately as possible from the pool of participants that had agreed to be interviewed. We invited potential participants for interview in sequential stages, depending on the response to prior emails. Participants were recruited until data saturation was achieved. Data saturation (i.e. no new themes emerging) was determined firstly by the researcher completing interviews and an iterative preliminary analysis.
3.2. Data collection
Semi-structured interviews enabled exploration of participant's experience with telehealth, including: perceived value, advantages, challenges and enablers. Interviews were conducted between July and November 2020 via Zoom, with no other people present. Each was then transcribed verbatim and de-identified before further analysis. Transcripts were not sent to participants for checking. The interviewer was a female physiotherapist (NM), with 13 years clinical experience, who received training from an experienced qualitative researcher (CJB), including pilot testing the topic guide with one participant. The interviewer did not have any existing relationship with participants. A topic guide (Additional file 2) was used to guide the interview process developed by authors. Field notes were not taken, and no repeat interviews were completed.
4. Data analysis
4.1. Survey data
Survey data were exported from Qualtrics to SPSS version 25 (IBM Corp., Armonk, NY, USA) data analysis software. The completion rate (proportion who completed 80% or more of the survey) was reported. Descriptive data summarised demographic and telehealth related questions (i.e. number of sessions, software and device used, and views about cost compared to in-person care [see Additional file 1 for list of all questions]). Global rating of change and attitudes towards telehealth were described by reporting distributions across the relevant Likert scales.
4.2. Interviews
Two physiotherapist researchers (CJB, AME), who both have PhDs and extensive experience in conducting interviews and evaluating qualitative data, led the qualitative data analysis. First, one researcher (AME) read each transcript to gain familiarity. Data categories were subsequently developed using an inductive thematic analysis to identify themes (Charmaz, 2006; Glaser and Strauss, 2017) from the interview data. NVivo software (QSR International Ptd Ltd, Melbourne) was used to support this analysis. A second reviewer (CJB) also read each transcript multiple times, and checked the thematic framework, including the accuracy of themes and subthemes. Two meetings were held between the two researchers to refine the thematic framework, including wording of each theme and subtheme. Any disagreements were discussed, and themes and subthemes were edited until consensus was reached. A third researcher (PM) with qualitative research experience also read through the thematic framework to validate the analysis performed. Themes and sub-themes were finalised through discussion between the three researchers (CJB, AME, PM). During this time researchers acknowledged their own experiences providing telehealth and held each other accountable for the influence they may have had during data analysis.
5. Results
Two-hundred and eight people read the electronic consent form, 89% (186/208) consented. Among people who consented, the completion rate was 93% (172/186). The mean age of the survey cohort (part 1) was 49 (SD = 28) years and 62% were women. Most were from metropolitan regions (169/172, 98%) as opposed to rural or remote regions (3/172, 2%). A minority of participants self-reported to have comorbidities, including: hypertension (10%, 17/172), clinical depression (7%, 12/172), elevated cholesterol (6%, 10/172), rheumatoid arthritis (4%, 6/172), fibromyalgia (3%, 5/172), and inflammatory bowel disease and psoriatic arthritis (1% for each condition, 2/172). 19 participants (60% women) with a mean age of 53 (SD = 17) years were interviewed prior to reaching data saturation (part 2).
5.1. Part 1 – quantitative
5.1.1. Type and mode of telehealth care
Participants had between 1 and 14 telehealth sessions (median = 2, IQR 1–3). Almost a third (30%, 52/172) undertook initial consultations (with or without follow-ups) via telehealth, whereas most undertook only telehealth follow-ups (70%, 120/172). Most received one-to-one telehealth services (88%, 151/172), and some received group-based care (9%, 16/172) or a combination of individual and group-based care (3%, 5/172). Among participants that had ceased telehealth care at the time of the survey, the most common reason for cessation was commencing in-person care (62%, 44/71), followed by the condition improving (23%, 16/71). Only one person (1% of the cohort in each instance) gave the reason that they were too busy, the condition was not improving, or that they could not afford any further out of pocket payment to continue. Participants who chose the ‘other’ category volunteered that they went on to have surgery, their exercise program was completed, they could not make the next appointment, or that they were part of a research study.
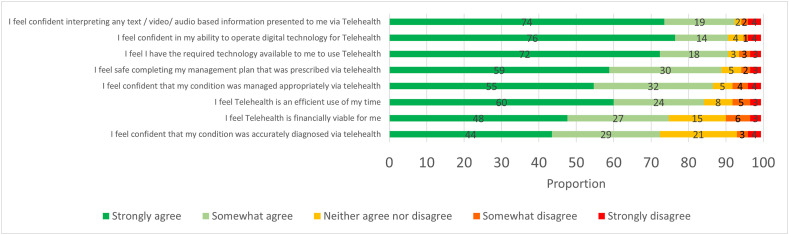
The mode of delivery of telehealth care was mostly via teleconference with or without telephone consultation (95%, 164/172) and via telephone exclusively for 5% (8/172) of participants. Among participants that used teleconference (n = 164), the most used software was Zoom, followed by Cliniko (Fig. 1 a), and the most common devices used were laptops, iPads and smartphones or, combinations of these (Fig. 1b).
Fig. 1.
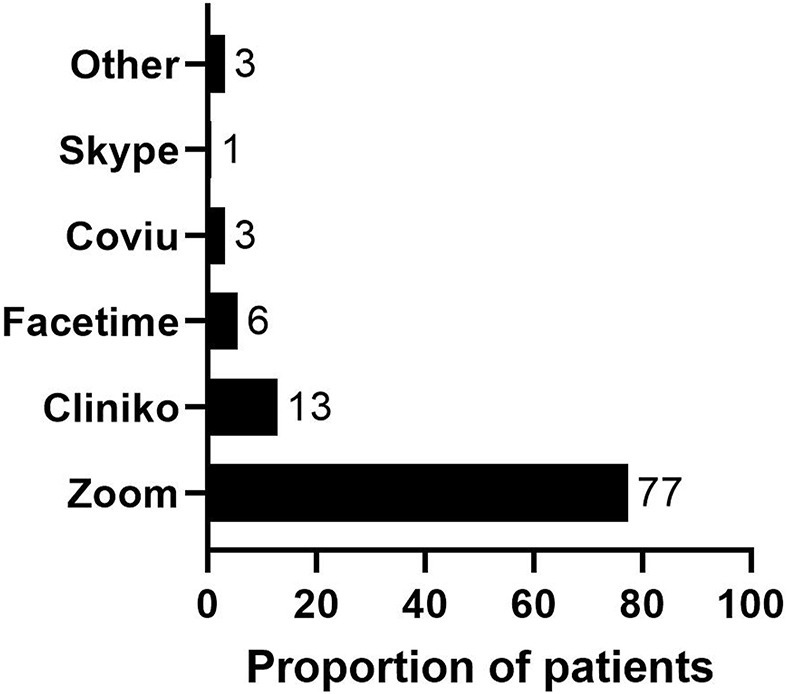
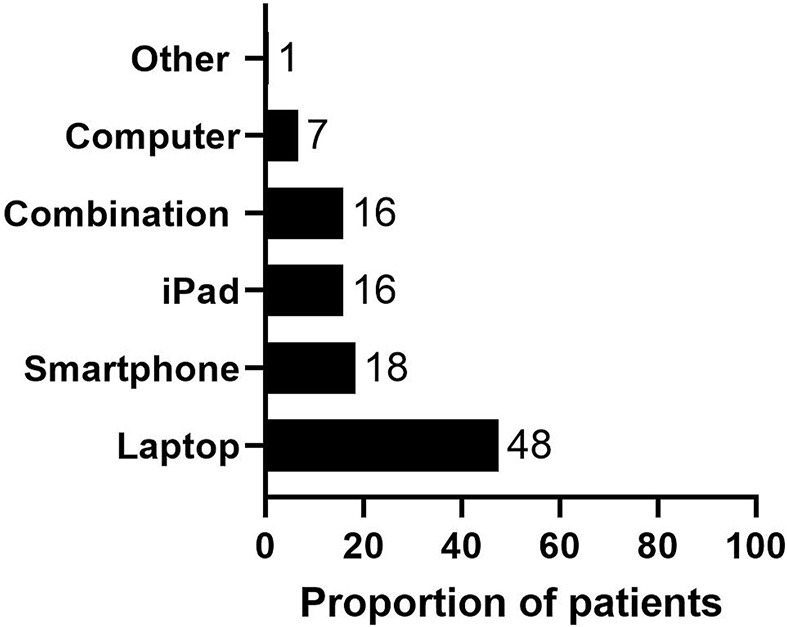
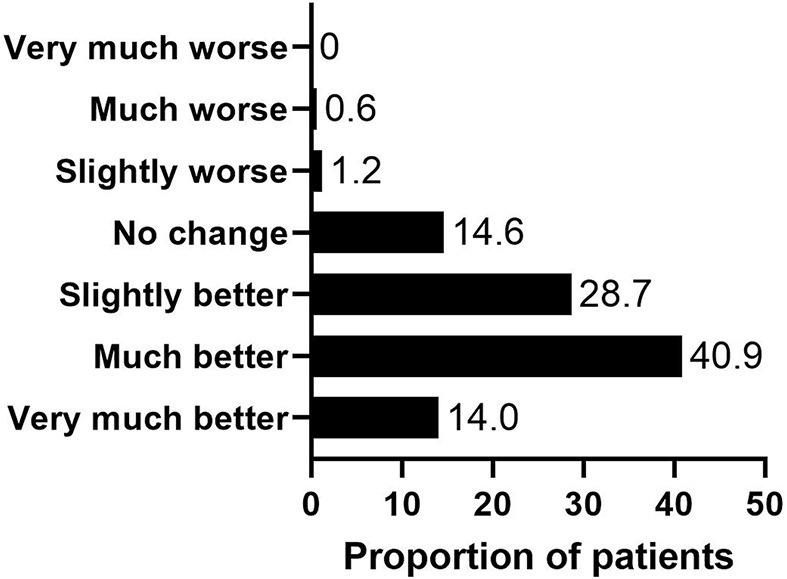
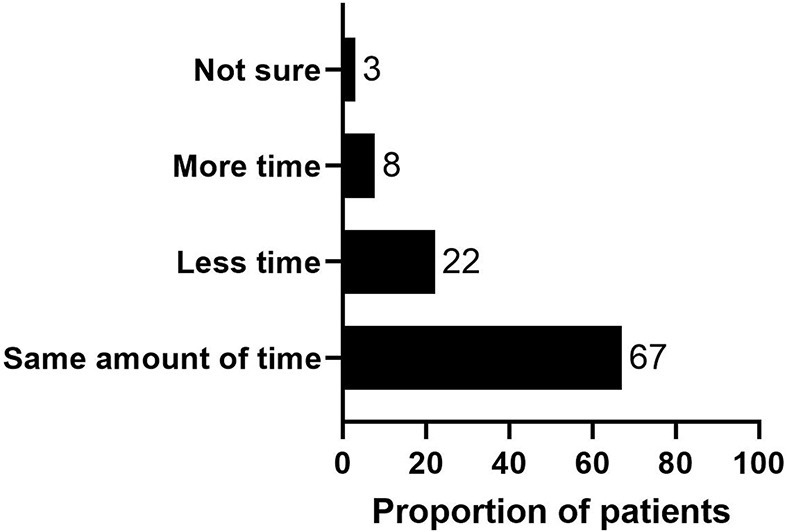
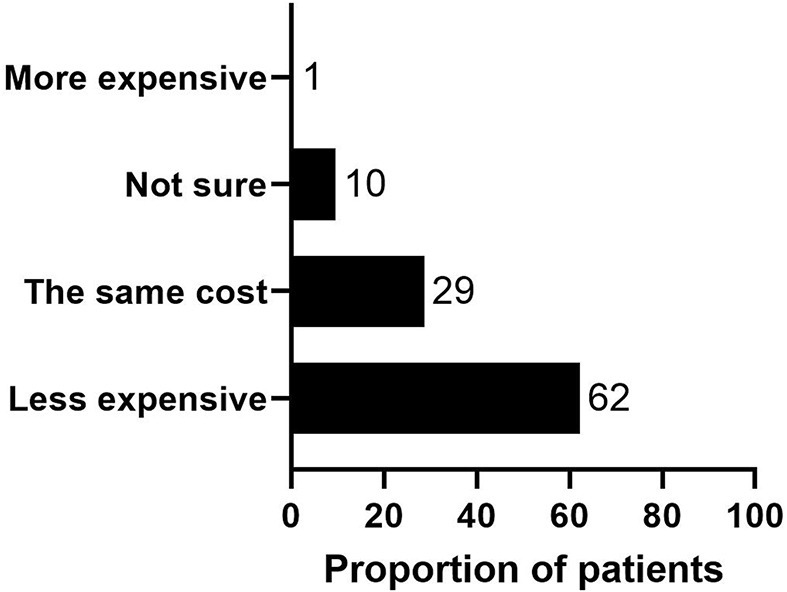
Proportion of respondents using particular software (1a) and type of devices (1b) to access telehealth; resources provided support telehealth consultations (1c); global rating of change outcomes (1d); and time spent during consultation (1e) and expectations of cost (1f) compared to in-person care.
5.1.2. Telehealth treatments, resources, and outcome
Most participants received an exercise program (95%, 163/172) and activity modification advice (59%, 102/172) via telehealth, and some received education about their condition (38%, 66/172) and advice about other treatments (24%, 41/172). In open responses, participants stated that they also received ‘post-operation follow-up’, ‘diagnosis’ and ‘reports about their condition’. Participants were provided with a range of resources to support telehealth consultations, most commonly written information (sent via text or email) (Fig. 1c). Global rating of change outcomes are shown in Fig. 1d.
5.1.3. Self-efficacy and attitudes related to telehealth
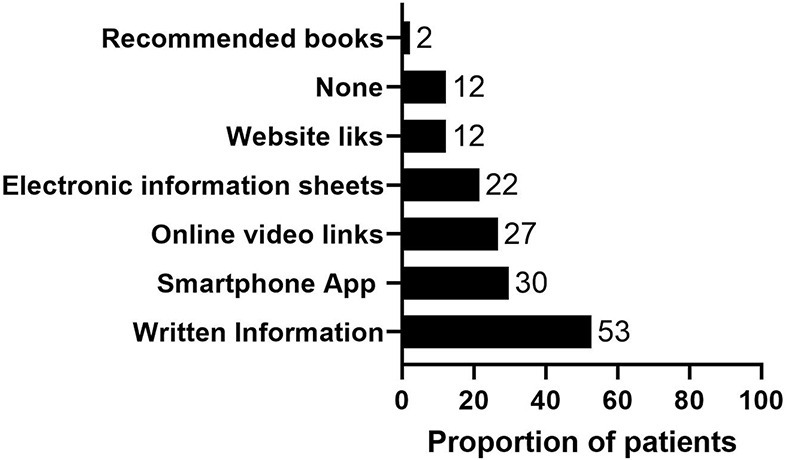
The median pain self-efficacy score was 54 (IQR 44 to 58). Most participants spent the same amount of time in telehealth consultations compared with in-person (Fig. 1e). Despite this, participants typically expected to pay less for telehealth services (Fig. 1f). Participant's attitudes towards telehealth are shown in Fig. 2 .
Fig. 2.
Attitudes towards telehealth related to various capability, opportunity and motivation factors.
5.2. Part 2 – qualitative
Interview Participants had between 1 and 14 telehealth sessions (median = 2, IQR 1–3). Duration of interviews ranged from 5 minutes, 30 seconds to 20 minutes, 21 seconds (median = 10 minutes; 3 seconds). Qualitative findings were split into four main themes, including (i) Table 1 : ‘ Telehealth had value, but generally perceived as inferior to in-person care’ (5 subthemes), (ii) Table 2 : ‘Challenges related to assessment, diagnosis, ‘hands on’ treatment, observation, communication, and technology’ (6 subthemes), (iii) Table 3 : ‘Advantages to access safe, expert, and convenient care’ (4 subthemes); and (iv) Table 4 : ‘Importance of supportive technology, including video and supplementary resources’ (2 subthemes).
Table 1.
Subthemes related to Theme 1: ‘Telehealth had value, but generally perceived as inferior to in-person care’.
| Subtheme | Illustrative quotes |
|---|---|
| Valuable if in-person care is not an option | The positive I feel is that it was better than not having any contact, but I would always prefer the physio, to go to the actual practitioner (P1); That physio wasn't seeing patients face-to-face. So, if telehealth hadn't been an option, I would've skipped it. [Telehealth] enabled it to happen as it opposed to not happen (P4); I think it's second-best, but I don't think it's a disaster (P3); I think these type of things [telehealth] they really, aren't as good as face-to-face. But in saying that I felt like they did, they served a purpose (P14). |
| Surprised at value, after initial hesitation | It's been pretty darn good. I've been pleasantly surprised … I was a little bit sceptical and thinking, “How is this gonna work?” but his delivery was fantastic and the outcomes had been great (P9); I was a bit sceptical at first cause I thought physios are more hands on and that's where you get your benefits but it was a really nice way to still get my treatment while being able to learn a few, I guess, ways where I could do it myself, so it's good (P12); I was a bit hesitant, but my physio was able to basically tell me and show me everything he needed to tell me and show me to give me the rehab exercises to improve, and the improvement was shown (P13). |
| Part of hybrid model in certain situations or conditions | I would hope it only became as an occasional arrangement rather than replacing the real thing …. So, it's not something I'd want to do all the time (P10); I think that anything that involves follow-up, maybe recovery rather than treatment – I don't know – initial acute treatment. I can imagine that being as successful as follow-up recovery, checking in about progress, changing exercises if need be or recovery pathways. I think they work quite well on Telehealth (P8); I realised I don't always need to see them face-to-face to get value from the consultation and it saves my travel and it saves their time as well. So I think there's a place for it across a range of options for people (P2); If you could use telehealth potentially to have an initial consult that may be set up for something that was physical later, then I think that was good in terms of basic diagnostic information … some of that triaging may be suitable for Telehealth (P11). |
| Cost should be the same or less | You are still getting an appointment with an experienced professional, so you're not really missing out in any way from that (P15); I would say that if you could create better Telehealth appointments in future that I wouldn't expect to pay any different for the service that's provided (P11); From the operator's point of view, it's as time-consuming and does the trick, then probably the price could be the same (P10); I was happy to pay for it, but I thought paying the full price when things like rents and the option of [certain] treatment wasn't available, so I thought a slightly reduced price was pretty reasonable (P13); I think there should be a difference in cost, absolutely. I think being face-to-face, it probably should be at a higher cost rather than through the computer. Why do I think that? Only because it's a little bit more impersonal. The full benefit of actually, like I just said, speaking to somebody, having that personal contact (P14). |
| Existing physiotherapist-patient relationship was considered valuable to facilitate telehealth | I have seen my same provider for 15 years, so when COVID happened, it was just a really easy step for us to do (P12); We'd met [the physio] before on numerous occasions, so I think that made a big difference. I don't think I'd want to do it to – as the first day effort (P10); He already knew about my problems and my history as I've been seeing him for a couple of years now. So, I don't know. It would've been a bit more hard if you were seeing someone for the first time or you had a new injury (P7). |
Table 2.
Subthemes related to Theme 2: ‘Challenges related to assessment, diagnosis, ‘hands on’ treatment, observation, communication, and technology’.
| Subtheme | Illustrative quotes |
|---|---|
| Accurate assessment and diagnosis | I think if it'd been face-to-face, he would've been able to do a better clinical assessment. I have a couple of little sort of tender spots, which I think he would be able to determine as I've described and pointed them out to him. It's really not quite the same as him being able to examine me and assess it himself (P3); Maybe the assessment might be a bit harder to do online just because they can't physically look at the area, and do tests, and exercises (P7); So if I've just go for a run and felt my calf go, I'd need to go to him to assess it for me. So more for a diagnostic level, I'd rather him be present and be able to feel the swelling, feel the injury, feel exactly where it is instead of me trying to point and explain it on video (P12); I believe it would've been more useful if somebody could've had their hands on and felt around, or at least been able to work out a little bit more detail around the injury (P8). |
| Lack of hands-on treatment | I understand what alignment needs and how to do these exercises correctly. But for other people, if they've never done something like that and they're on telehealth, they might need someone to give them cues to fix their positioning and it's a lot harder to do that over the internet than it is for someone to get physical cue (P13); If you needed to do something which was hands-on, then you couldn't do that (P10); I have a physio that I see for my back and there's no point – I wouldn't even – he does manual manipulation and there's just no point in doing that remotely (P4). |
| Difficulty with observation | The scope to kind of observe is limited in telehealth unless you've got a really well-positioned camera or you can kind of move this around so that [the physio] is able to see what he needs to see (P11); I was doing the exercises on – with my laptop, moving my laptop around on the floor, on the chair that I was doing the exercises, and – I don't know. I just felt like he wasn't getting as complete a picture of what I was doing as he would've if we were in the same room (P4); I obviously much prefer face-to-face as its just easier to show him like spots that might be hurting and my technique for some exercises cause it can be hard trying to angle the camera and find a place to show him the whole body and things like that (P7); The hardest bit was trying to find an angle to set up my iPad so that [physio] could see me when I was doing the exercises and all that sort of thing (P5). |
| Understanding and communicating | You don't get the same information from a patient by talking to them on the phone or seeing a picture of them that you get by actually being there (P10); I find better being face-to-face. It just triggers more questions, triggers – I can actually feel more comfortable in showing him my exercises and where I'm having issues, where my knees hurt … I found it easier face-to-face than online in telehealth (P6); You can't see the facial expressions as well, so you can't really gauge whether or not he's totally understood what you're meaning … You feel like the person understands you more, just being physically there (P7). |
| Perceived as less personal typically but not always | I suppose the disadvantage is, that face-to-face, which is always nice to have human contact. But now, all I feel like is I'm talking to a screen. You don't get to feel the energy in the room, you don't get to feel that person's energy (P14); I'd like to speak to people, see people face-to-face …. I think it's just more personal if you're there, over telehealth (P5); I like technology, so I don't have a problem with technology. … You still get all the personal stuff. So, there's no issue around feeling close to the practitioner (P8). |
| Technology concerns | This Zoom business is quite complicated (P10); I think that the platform – that [the clinic] was not a very good platform … there were some issues with the browser that you needed to have in order to operate the software on a laptop … I would have preferred to have the consult on my laptop for some bigger screen real estate, I ended up having to use it on my phone because that's all I could make the software work on (P11); I don't know what the problem was, but initially when we started … something went wrong with it and [physio]and I ended up FaceTime-ing (P5); I was down in my shed, I wasn't in the house, so I was running off 4G, and I don't have very good connection here where I am (P5); I didn't have earphones so I didn't quite understand this whole process. I think it was the second time that I'd used it. His receptionist was fabulous in coaching me through it and she set it up (P6); The internet connection is also – wasn't the best for me here, so it was cutting in and out a lot. So, sometimes it was hard and I had to get him to repeat things (P7); [Technology] needs to be supported right through that entire chain of activities and so, not just around sort of booking the activity, but also paying as well (P11). |
Table 3.
Subthemes related to Theme 3: ‘Advantages to access safe, expert, and convenient care’.
| Subtheme | Illustrative quotes |
|---|---|
| Facilitates access to the right expertise | It's the convenience of telehealth, of being able to do a consultation with a health professional – a chosen health professional without leaving your front door (P3); I guess there would be times when I would consider [telehealth], if I was overseas or something and I wanted to see an Australian practitioner, as opposed to someone (P4); It's used a lot in rural practice and I don't see an issue with it being brought into metropolitan clients as well (P8). |
| Convenience of not having to travel | The travel time to get to and from the practice … then there was definitely advantage in doing that I could come from a previous meeting and literally be in the practice in a matter of seconds (P11); I think the positive would be that I could do it at home, so I didn't have to incorporate travel time and money for petrol, and trying to get there after work and all that type of stuff (P13); There is that added convenience that it was in my house and I didn't have to put my shoes on and drive there, but I would rather put my shoes on and drive there (P4); The time factor straight up because it's a 40-minute trip for me to where [my physio] works from in [place] and with my condition, it's my knee, my hip, plantar fascia, and a bit of back, so I don't really like being in the car for any great deal of time (P9); I don't have to go out of the house (P16). |
| No risk of contracting COVID | Because of the current situation, the COVID, I like the fact that we could be safe both from the physio's perspective and I can do it in the safely of my own home (P15); Just the fact that I didn't have to go in at the time that I didn't really feel comfortable. They were still open for most of the time but I've got a few immune issues, so I wasn't willing to risk going in (P12); I liked the fact that we could be safe, both from a physio's perspective and from mine (P17). |
| Exercises in home environment | I liked him giving me things that I can do at home instead of at the gym … so it's a bit more adaptable to the situation (P12); [The physio] was able to see the exercises that I was doing, and how I'd set up my home gym, and able to give me some feedback on them (P5); We had to make adaptions and [he] is magical in his ability to make using things at home and the way he went about showing me, physically showing me, and talking me through how to maintain what I've achieved until I get back to the gym so that there's no backward or negative steps as part of the process (P9). |
Table 4.
Subthemes related to Theme 4: ‘Importance of supportive technology, including video and supplementary resources’.
| Subtheme | Illustrative quotes |
|---|---|
| Video calls important | I found it useful that he was able to – using Zoom or FaceTime, he was able to visualise my restricted movements and how things have changed (P3); You can check exercise, you can see what's happening, and he can tell you to turn around, and move to the left and what have you. So that worked (P10); He got me to show him exercises I had to do by holding up the screen and showing him. And he did a pretty good job just trying to gauge where I'm at and progression with my exercises (P7). |
| Supplemental resources | I think it was well-supplemented. So from the advice that my practitioner gave me, he was able to back that up with both factsheets and also videos to show you – that show – so with the exercises that I was required to do, the videos really helped in terms of doing that because it was – a lot of the time, they'll write down, “I want you to do these particular exercises,” and then [you had] a hard time remembering what the instructions (P11); [My physio] typed up a program for me and also some videos that I needed to watch to help me understand what he wanted me to do … he would send me a video and he would send me an email at the end of the consultation (P3); I got a link to a physio sort of app or website and that actually showed the technique of my exercises to do which really helps so I knew how to perform them (P7); When he has the interview with me, he [watches me] doing the exercises, and new one, he gets me to do them and takes his photo, and then he sends me that photo or that video. So I got no reason not to do it properly (P3). |
6. Discussion
This mixed-methods study provides unique insights into the experience and attitudes toward physiotherapist-delivered telehealth services for musculoskeletal pain conditions. Consistent with other patient experience research in physiotherapy (Bennell et al., 2021) and general practice (Imlach et al., 2020) during the pandemic, satisfaction with care was typically high, and telehealth was considered valuable when in-person care was not an option. Yet, our survey and interview findings indicate people with musculoskeletal pain conditions may not place the same value on telehealth as in-person care, which is consistent with the beliefs of some Australian physiotherapists (Malliaras et al., 2021). Reflecting this, the most common reason for ceasing telehealth care among survey participants was commencing in-person care. Collectively, these findings may explain why Australian physiotherapists have typically charged lower fees for telehealth compared in-person care during the pandemic (Bennell et al., 2021).
In contrast to the general perception in the study cohort that telehealth was less valuable compared to in-person care, numerous interview participants expressed surprise with the value and benefits of telehealth. This suggests beliefs about telehealth value are changeable through exposure to appropriately delivered services. Three in four survey participants agreed telehealth was financially viable, and most (84%) agreed telehealth was an efficient use of their time. Importantly, the majority (85%) of survey participants reported improvement following their telehealth consultations, with more than one in two reporting being much better or very much better. These positive clinical outcomes are consistent with current evidence suggesting similar improvements in pain and function between telehealth and in-person care for people with musculoskeletal pain conditions (Cottrell et al., 2017). Developing strategies to improve the perceived value of telehealth among physiotherapists and patients, especially those with limited experience delivering or accessing it, is needed to improve uptake beyond the pandemic. Considerations should include education and training of physiotherapists to address limitations in workforce capacity (Malliaras et al., 2021), and better education and marketing to the public to promote the value of telehealth, particularly in rural and remote areas where there is limited access to in-person care (Cottrell and Russell, 2020; Turolla et al., 2020).
A key qualitative finding from this study was the belief that telehealth may not be appropriate for all conditions, with several participants expressing concerns about the accuracy of assessment and diagnosis through telehealth. Triangulating this finding, only 44% of survey participants strongly agreed their condition was accurately diagnosed via telehealth. Limitations with assessment and diagnosis of telehealth is a view shared by physiotherapists managing musculoskeletal pain conditions (Malliaras et al., 2021), and patients receiving telehealth during the pandemic in New Zealand General Practices (Imlach et al., 2020). It also consistent with previous research indicating that some assessment requiring physical contact (e.g. some ‘special' tests, neurodynamic assessment) may not be valid via telehealth (Cottrell and Russell, 2020). Defining the appropriate scope of telehealth services for musculoskeletal pain conditions, including the identification of potential subgroups most likely to benefit, should be explored in future research.
Several interview participants in this study suggested that telehealth may be best used as part of a hybrid model of care, where telehealth consultations supplement in-person care, rather than replacing it. Most participants in our survey, and a previous similar survey (Bennell et al., 2021), adopted telehealth in Australia following previous consultation with the same physiotherapists in-person. Consistent with this, an established relationship with their physiotherapist was valued by interview participants as a key enabler to facilitate effective telehealth. The absence of physical contact with telehealth was viewed as a challenge to communication, and led to the care feeling less ‘personal’ in some instances. The perception of impersonal care with telehealth has been a key theme reported in previously published qualitative research embedded within clinical trials (Fernandes et al., 2021). To improve uptake and benefits of telehealth services, future research should explore the value of telehealth as part of a hybrid model, and how to enhance therapeutic alliance and communication during the delivery of telehealth services (Kinney et al., 2020).
Our qualitative findings revealed that the absence of physical contact during telehealth consultations was a key limitation of this service, due to the resulting inability to receive ‘hands on’ treatment. Similar challenges with telehealth have been reported by physiotherapists responding to surveys during the pandemic (Bennell et al., 2021; Malliaras et al., 2021). Absence of ‘hands on’ care will undoubtedly lower perceived value of telehealth care among people who expect these treatments or perceive them as an essential component of physiotherapy practice. However, some physiotherapists believe the barrier to ‘hands on’ treatment created by telehealth may improve the value of care provided. Specifically, the adoption of more active management strategies (education, exercise therapy) forced by telehealth aligns care with evidence and guidelines for musculoskeletal pain (Bannuru et al., 2019; Booth et al., 2017; Lin et al., 2020; Malliaras et al., 2021; Oliveira et al., 2018; Willy et al., 2019). Reflecting high use of active management strategies with telehealth, most survey participants in this study (95%) received an exercise program when accessing telehealth physiotherapy care.
More than 95% of participants in this study reported receiving video-based telehealth services, typically via Zoom. This compares to just 5% of General Practice patients in New Zealand during the pandemic (Imlach et al., 2020). Strong adoption of video-based telehealth services by Australian physiotherapists is important, with the use video and supplementary digital resources considered by interview participants to be key enablers of telehealth, particularly for exercise therapy. Additionally, more than nine in ten people in this study used a portable device (laptop, tablet, phone) to access telehealth, which provides capability to alter camera angles for optimal assessment and observation of exercise (Cottrell and Russell, 2020).
Although popular in our cohort, challenges related to video-based telehealth were evident. Consistent with other published research (Cottrell and Russell, 2020; Fernandes et al., 2021; Turolla et al., 2020), our qualitative findings indicate that difficulties with internet connection, software and devices were key challenges to telehealth adoption. Additionally, approximately one in ten survey participants did not agree they were confident in their ability to operate the digital technology required, or that they had access to the digital technology required. Considering physiotherapists also report the need to troubleshoot technical issues as key challenges to telehealth implementation (Malliaras et al., 2021), developing support and solutions for these technical challenges is urgently needed. Developing and promoting the use of supplemental resources such as ‘how to’ guidance for engaging with telehealth for patients and physiotherapists (Davies et al., 2021) is encouraged. Additionally, findings from this study and previous research (Barton et al., 2021; Malliaras et al., 2021) indicates that education and training initiatives for physiotherapists to support them in integrating technology, exercise videos, supportive apps and referral to trusted health information websites may enhance the telehealth patient-experience.
Consistent with other qualitative research from clinical trials prior to the pandemic (Cottrell and Russell, 2020; Turolla et al., 2020), and patient surveys during the pandemic (Bennell et al., 2021), our qualitative findings highlighted other important advantages of telehealth, including facilitating access to the right expertise, the convenience of not having to travel to access care and being able to exercise at home. Considering a general perception that telehealth is of lower value compared to in-person care, physiotherapists and health systems more broadly are encouraged to promote the advantages of telehealth to people with musculoskeletal pain conditions. This promotion should particularly focus on people who may have difficulty accessing traditional in-person care due to geography or other barriers such as occupational and family responsibilities.
7. Limitations
The strengths of this study include a mixed-methods approach involving a large survey and semi-structured interviews. However, our findings should be considered in the context of some limitations. All participants were recruited from Australian private physiotherapy practices, meaning findings may not be reflective of publicly funded healthcare settings, other health services or an international context. Due the nature of our recruitment approach, which relied on physiotherapy clinics to facilitate recruitment, we are unable to determine the number of patients approached, or the proportion who consented to participate. Most participants resided in metropolitan areas, meaning our findings should not be generalised beyond this population. Our data therefore is likely to capture views of people who are traditionally less likely to require telehealth services. We recruited participants who had all accessed at least one telehealth consultation, indicating they had the financial means, hardware, internet access and computer literacy to facilitate telehealth. As such potential barriers related to other factors may be underestimated by out cohort. Only a minority of participants responding to our survey self-reported to have comorbidities, indicating our cohort may be healthier than the typical profile of people presenting for care with musculoskeletal pain conditions (Swain et al., 2020; Tousignant-Laflamme et al., 2017).
Our study took place in the context of initial COVID-19 lock downs in 2020, in a population who were forced to use telehealth to access physiotherapy care, and this may bias our findings. The number (median, range) of telehealth appointments provided to participants prior to our survey (2, 1 to 14) and interviews (2, 1 to 14) indicated limited exposure for most participants. Considering our qualitative finding of surprise in value of telehealth following exposure, the perceived value of telehealth may differ if this study is repeated in the future. Additionally, it is also possible our interview sample may have been biased by inclusion of participants with more positive telehealth experiences. Regardless, the pandemic environment provided a unique opportunity to explore ‘real world’ experiences and attitudes of telehealth which would not have been possible otherwise. Similar research is encouraged outside of times when pandemic lockdown restrictions are in place.
8. Conclusion
People with musculoskeletal pain conditions who were provided telehealth during the COVID-19 pandemic in Australian private physiotherapy practice typically felt this care was valuable, although less so than traditional in-person care. Telehealth was seen as valuable when in-person care was not an option, and participants were surprised at its value once exposed. Key challenges to telehealth perceived by patients included the lack of physical contact preventing accurate assessment, diagnosis and ‘hands on’ treatment, and requirements for technology to facilitate a quality service. Advantages of telehealth included access to expert and convenient care, and patient outcomes were typically good among this cohort. Findings from this study can be used to inform initiatives to improve uptake and sustainability of telehealth delivered by physiotherapists to people with musculoskeletal pain conditions beyond the pandemic. Consideration of telehealth as part of a hybrid model, along with education and training initiatives for physiotherapists and patients to improve the quality and value of telehealth services is encouraged.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.msksp.2021.102500.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Andrew S., Halcomb E.J. Mixed methods research is an effective method of enquiry for community health research. Contemp. Nurse. 2006;23(2):145–153. doi: 10.5555/conu.2006.23.2.145. [DOI] [PubMed] [Google Scholar]
- Bannuru R.R., Osani M.C., Vaysbrot E.E., Arden N.K., Bennell K., Bierma-Zeinstra S.M.A., McAlindon T.E. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589. doi: 10.1016/j.joca.2019.06.011. [DOI] [PubMed] [Google Scholar]
- Barton C.J., Ezzat A.M., Bell E.C., Rathleff M.S., Kemp J.L., Crossley K.M. Knowledge, confidence and learning needs of physiotherapists treating persistent knee pain in Australia and Canada: a mixed-methods study. Physiother. Theory Pract. 2021:1–13. doi: 10.1080/09593985.2021.1906805. [DOI] [PubMed] [Google Scholar]
- Bennell K.L., Lawford B.J., Metcalf B., Mackenzie D., Russell T., van den Berg M., Hinman R.S. Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: a mixed-methods study. J. Physiother. 2021;67(3):201–209. doi: 10.1016/j.jphys.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth J., Moseley G.L., Schiltenwolf M., Cashin A., Davies M., Hübscher M. Exercise for chronic musculoskeletal pain: a biopsychosocial approach. Muscoskel. Care. 2017;15(4):413–421. doi: 10.1002/msc.1191. [DOI] [PubMed] [Google Scholar]
- Charmaz K. SAGE Publications; London, UK: 2006. Constructing Grounded Theory: a Practical Guide through Qualitative Analysis. [Google Scholar]
- Cottrell M.A., Galea O.A., O'Leary S.P., Hill A.J., Russell T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin. Rehabil. 2017;31(5):625–638. doi: 10.1177/0269215516645148. [DOI] [PubMed] [Google Scholar]
- Cottrell M.A., Russell T.G. Telehealth for musculoskeletal physiotherapy. Musculoskelet Sci Pract. 2020;48 doi: 10.1016/j.msksp.2020.102193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies L., Hinman R.S., Russell T., Lawford B., Bennell K., Group I.V.S. An international core capability framework for physiotherapists to deliver quality care via videoconferencing: a Delphi study. J. Physiother. 2021 doi: 10.1016/j.jphys.2021.09.001. [DOI] [PubMed] [Google Scholar]
- Dorsey E.R., Topol E.J. State of telehealth. N. Engl. J. Med. 2016;375(14):1400. doi: 10.1056/NEJMc1610233. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J. Med. Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes L.G., Devan H., Fioratti I., Kamper S.J., Williams C.M., Saragiotto B.T. At my own pace, space, and place: a systematic review of qualitative studies of enablers and barriers to telehealth interventions for people with chronic pain. Pain. 2021 doi: 10.1097/j.pain.0000000000002364. [DOI] [PubMed] [Google Scholar]
- Glaser B.G., Strauss A.L. Routledge; New York, USA: 2017. Discovery of Grounded Theory: Strategies for Qualitative Research. [Google Scholar]
- Huijg J.M., Gebhardt W.A., Dusseldorp E., Verheijden M.W., van der Zouwe N., Middelkoop B.J., Crone M.R. Measuring determinants of implementation behavior: psychometric properties of a questionnaire based on the theoretical domains framework. Implement. Sci. 2014;9:33. doi: 10.1186/1748-5908-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imlach F., McKinlay E., Middleton L., Kennedy J., Pledger M., Russell L., McBride-Henry K. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam. Pract. 2020;21(1):269. doi: 10.1186/s12875-020-01336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isautier J.M., Copp T., Ayre J., Cvejic E., Meyerowitz-Katz G., Batcup C., McCaffery K.J. People's experiences and satisfaction with telehealth during the COVID-19 pandemic in Australia: cross-sectional survey study. J. Med. Internet Res. 2020;22(12) doi: 10.2196/24531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamper S.J., Maher C.G., Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J. Man. Manip. Ther. 2009;17(3):163–170. doi: 10.1179/jmt.2009.17.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney M., Seider J., Beaty A.F., Coughlin K., Dyal M., Clewley D. The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: a systematic review of the literature. Physiother. Theory Pract. 2020;36(8):886–898. doi: 10.1080/09593985.2018.1516015. [DOI] [PubMed] [Google Scholar]
- Lin I., Wiles L., Waller R., Goucke R., Nagree Y., Gibberd M., O'Sullivan P.P.B. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br. J. Sports Med. 2020;54(2):79–86. doi: 10.1136/bjsports-2018-099878. [DOI] [PubMed] [Google Scholar]
- Malliaras P., Merolli M., Williams C.M., Caneiro J.P., Haines T., Barton C. 'It's not hands-on therapy, so it's very limited': telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021;52 doi: 10.1016/j.msksp.2021.102340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Cathain A., Murphy E., Nicholl J. The quality of mixed methods studies in health services research. J. Health Serv. Res. Pol. 2008;13(2):92–98. doi: 10.1258/jhsrp.2007.007074. [DOI] [PubMed] [Google Scholar]
- Oliveira C.B., Maher C.G., Pinto R.Z., Traeger A.C., Lin C.C., Chenot J.F., Koes B.W. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur. Spine J. 2018;27(11):2791–2803. doi: 10.1007/s00586-018-5673-2. [DOI] [PubMed] [Google Scholar]
- Rethorn Z.D., Lee A.C., Rethorn T.J. Connecting at the webside: rapid telehealth implementation for musculoskeletal clinicians. J. Orthop. Sports Phys. Ther. 2021;51(1):8–11. doi: 10.2519/jospt.2021.9902. [DOI] [PubMed] [Google Scholar]
- Swain S., Sarmanova A., Coupland C., Doherty M., Zhang W. Comorbidities in osteoarthritis: a systematic review and meta-analysis of observational studies. Arthritis Care Res. 2020;72(7):991–1000. doi: 10.1002/acr.24008. [DOI] [PubMed] [Google Scholar]
- Tanne J.H., Hayasaki E., Zastrow M., Pulla P., Smith P., Rada A.G. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ. 2020;368:m1090. doi: 10.1136/bmj.m1090. [DOI] [PubMed] [Google Scholar]
- Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- Tousignant-Laflamme Y., Martel M.O., Joshi A.B., Cook C.E. Rehabilitation management of low back pain - it's time to pull it all together. J. Pain Res. 2017;10:2373–2385. doi: 10.2147/JPR.S146485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turolla A., Rossettini G., Viceconti A., Palese A., Geri T. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys. Ther. 2020;100(8):1260–1264. doi: 10.1093/ptj/pzaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willy R.W., Hoglund L.T., Barton C.J., Bolgla L.A., Scalzitti D.A., Logerstedt D.S., McDonough C.M. Patellofemoral pain. J. Orthop. Sports Phys. Ther. 2019;49(9):CPG1–CPG95. doi: 10.2519/jospt.2019.0302. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.