Abstract
Sphingosine-1-phosphate (S1P), a pleiotropic lipid mediator, participates in various cellular processes during tumorigenesis, including cell proliferation, survival, drug resistance, metastasis, and angiogenesis. S1P is formed by two sphingosine kinases (SphKs), SphK1 and SphK2. The intracellularly produced S1P is delivered to the extracellular space by ATP-binding cassette (ABC) transporters and spinster homolog 2 (SPNS2), where it binds to five transmembrane G protein-coupled receptors to mediate its oncogenic functions (S1PR1-S1PR5). MicroRNAs (miRNAs) are small non-coding RNAs, 21–25 nucleotides in length, that play numerous crucial roles in cancer, such as tumor initiation, progression, apoptosis, metastasis, and angiogenesis via binding to the 3′‐untranslated region (3′‐UTR) of the target mRNA. There is growing evidence that various miRNAs modulate tumorigenesis by regulating the expression of SphKs, and S1P receptors. We have reviewed various roles of miRNAs, SphKs, S1P, and S1P receptors (S1PRs) in malignancies and how notable miRNAs like miR-101, miR-125b, miR-128, and miR-506, miR-1246, miR-21, miR-126, miR499a, miR20a-5p, miR-140-5p, miR-224, miR-137, miR-183-5p, miR-194, miR181b, miR136, and miR-675-3p, modulate S1P signaling. These tumorigenesis modulating miRNAs are involved in different cancers including breast, gastric, hepatocellular carcinoma, prostate, colorectal, cervical, ovarian, and lung cancer via cell proliferation, invasion, angiogenesis, apoptosis, metastasis, immune evasion, chemoresistance, and chemosensitivity. Therefore, understanding the interaction of SphKs, S1P, and S1P receptors with miRNAs in human malignancies will lead to better insights for miRNA-based cancer therapy.
Keywords: Sphingosine-1-phosphate (S1P), Metastasis, Angiogenesis, MicroRNAs, Cancer
Introduction
Sphingosine-1-phosphate (S1P) is a bioactive lipid that is produced from the conversion of ceramide to sphingosine and then phosphorylation of sphingosine through sphingosine kinases (SphKs) [1]. To induce cell responses, S1P can either interact with intracellular proteins or be exported from the cell to bind S1P receptors (S1PRs) on cells [2]. The binding of S1P to G protein-coupled receptors (S1PR1-S1PR5) activates S1PRs and stimulates the associated G proteins to trigger intracellular signals and regulate different processes, such as cell growth, survival, and migration [3]. S1P has a secondary role in the modulation of calcium homeostasis as well. It also enhances the proliferation of cells, survival and inhibits apoptosis [4]. There is also compelling evidence that supports the role of S1P in cancer, including promoting transformation, cell survival, epithelial-mesenchymal transition (EMT), replicative immortality, aerobic glycolysis, and tumor angiogenesis [5–7]. S1P function has also been allied with in cancer inflammatory pathways, cell invasion, and resistance to chemotherapy [8]. S1P-SphK1pathway is involved in head and neck cancer, renal cancer, glioblastoma and leukemias of various types [9]. Mouse models have shown that S1P pathway is also implicated in colon carcinogenesis [10]. Thus, targeting S1P, S1PR and associated proteins in its signaling pathway is a novel therapeutic approach in cancer therapy.
MicroRNAs (miRNAs), with 21–25 nucleotides in length, are a member of non-coding RNAs (ncRNAs) that regulate gene expression via binding to the 3′-untranslated region (3′-UTR) of the target gene, leading to degradation of target mRNA and repression of its translation [11]. Since Lee et al. discovered the first miRNA, lin‐4, from Caenorhabditis elegans worm [12], more than 2300 mature human miRNAs have been identified [13]. Due to regulate the expression of approximately 90% of human genes, miRNAs are vital factors in controlling cellular processes [14]. There is increasing evidence of crosstalk between miRNAs with SphKs, S1P, and S1PRs that regulates different cellular functions during cancer. This review focuses on the miRNA biogenesis, their involvement in cancer, S1P biosynthesis, and its importance in tumorigenesis and cancer development. Finally, the interaction between miRNAs with SphKs, S1P, and S1PRs is discussed.
miRNAs biogenesis and their role in cancer
miRNA biogenesis is a complex and multi-step process that starts in the nucleus and undergoes post-transcriptional modifications and then subsequently transported to the cytoplasm to regulate gene expression. In the nucleus, miRNAs are transcribed mostly by RNA polymerase II as mRNAs, while other miRNAs are transcribed by RNA polymerase III, leading to generate the primary miRNA (pri-miRNA) that is capped and polyadenylated at 5´ and 3´, respectively [15, 16]. The hairpin-structured pri-miRNA is recognized and cleaved by the microprocessor composed of an RNase III enzyme, DROSHA, and its cofactor, DGCR8, which produces precursor miRNA (pre-miRNA) with about 60–70 nucleotides in length [17, 18]. Exportin 5 (Exp5) binds to and transports pre-miRNA into the cytoplasm in a RanGTP-dependent manner [19, 20]. In the cytoplasm, another RNase III enzyme, DICER, cleaves pre-miRNA, releasing a miRNA duplex [21]. Then, the miRNA duplex generated through DICER is loaded onto the Argonaute (AGO) protein which selects a strand as mature miRNA (guide strand) and discards the passenger strand (miRNA*) [22]. Finally, the selected strand is loaded into the miRNA-induced silencing complex (miRISC) and directs the complex to target mRNAs in processing bodies (P-bodies) [23].
It has been demonstrated that miRNA expression is dysregulated during human cancers. Indeed, some miRNAs act as oncogenes (OGs), and others act as tumor suppressors (TSs). Interestingly, some miRNAs can act as both OGs and TSs, depending on the specific tissue they express and target genes [24, 25]. Hanahan and Weinberg proposed that cancer consists of six hallmarks, including sustaining proliferative signaling, resisting cell death, evading growth suppressor, activating invasion and metastasis, enabling replicative immortality, and inducing angiogenesis [26]. It is supposed that dysregulated miRNAs affect one or several hallmarks of cancer for tumor initiation and development. Table1 summarizes the role of different miRNAs in various cancers.
Table 1.
The role of miRNAs in various cancers
| miRNA | Target | Cancer | Mechanism of action | Refs. | |
|---|---|---|---|---|---|
| miR-1246 | CCNG2 | Breast | ↑Proliferation, invasion, drug resistance | [27] | |
| miR-21 | PTEN | CRC | ↑Tumor growth and invasion | [28] | |
| miR-126 | EZH2 | Gastric | ↑Chemosensitivity | [29] | |
| miR-499a | SOX6 | Cervical | ↑Chemoresistance | [30] | |
| miR-20a-5p | SMAD4 | CRC | ↑Invasion and metastasis | [31] | |
| miR-140-5p | VEGF-A | Breast | ↓Invasion and angiogenesis | [32] | |
| miR-224 | RASSF8 | Gastric | ↑Tumor growth, invasion, migration | [33] | |
| miR-210 | FGFRL1 | HCC | ↑Angiogenesis | [34] | |
| miR-137 | XIAP | Ovarian | ↑Apoptosis | [35] | |
| miR-183-5p | PDCD4 | Breast | ↑Proliferation, ↓Apoptosis | [36] | |
| miR-194 | SOCS2 | Prostate | ↑Metastasis | [37] | |
| miR-181b | Bcl-2 | Lung | ↓Chemoresistance | [38] | |
| miR-136 | Notch3 | Ovarian | ↓CSCs activity, ↑Chemosensitivity | [39] | |
| miR-675-3p | CXXC4 | Gastric | ↑Immune escape | [40] |
CCNG2 cyclin-G2, CRC colorectal cancer, PTEN phosphatase and tensin homolog, EZH2 enhancer of zeste homolog 2, SOX6 sex-determining region Y box 6, SMAD4 drosophila mothers against decapentaplegic protein4, VEGF-A vascular endothelial growth factor A, RASSF8 ras association domain family member 8, FGFRL1 fibroblast growth factor receptor-like 1, HCC hepatocellular carcinoma, XIAP X-linked inhibitor of apoptosis, PDCD4 programmed cell death protein 4, SOCS2 suppressor of cytokine signaling 2, CSCs cancer stem cells, CXXC4 CXXC finger protein 4
S1P biosynthesis and its receptors
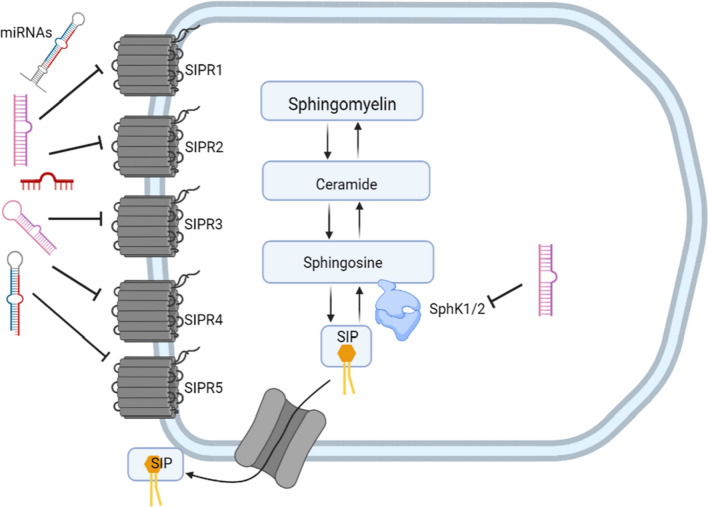
To generate S1P, two enzymatic reactions take place inside the cell: first, the ceramide is converted to sphingosine by ceramidase, and then the SphK enzymes convert sphingosine into its phosphorylated form (S1P) using ATP [2]. S1P can inhibit ceramide-mediated apoptosis (including intranucleosomal DNA fragmentation and other structural changes), which occurs in response to the accumulation of ceramide [41]. There are two isoforms of SphK: SphK1 and SphK2. SphK1 is localized close to the cell membrane in the cytosol, where it participates in its substrate's transport [42]. Cytokine-mediated activation of SphK1 leads to the phosphorylation of Sph. This generates intracellular S1P which is then exported from cells by Sphingolipid Transporter 2 (SPNS2) [43]. On the other hand, SphK2 is located in the mitochondria and nucleus. In the mitochondria, S1P can interact with prohibitin 2 to regulate the assembly of complex IV and respiration [44], whereas it regulates the transcription of genes via epigenetic modulations in the nucleus [45, 46]. Thus, S1P generated by SphK1 can export to the outside of the cell to trigger “inside-out” signaling, while S1P generated by SphK1 and SphK2 act intracellularly to regulate cellular functions. “Inside-out” signaling indicates that inside the cell-produced S1P is transported outside the cell to act as autocrine or paracrine via binding to its receptors [47]. Figure 1 shows the biosynthetic process of S1P.
Fig. 1.
Schematic representation of the biosynthesis process of Sphingosine-1-phosphate (S1P)
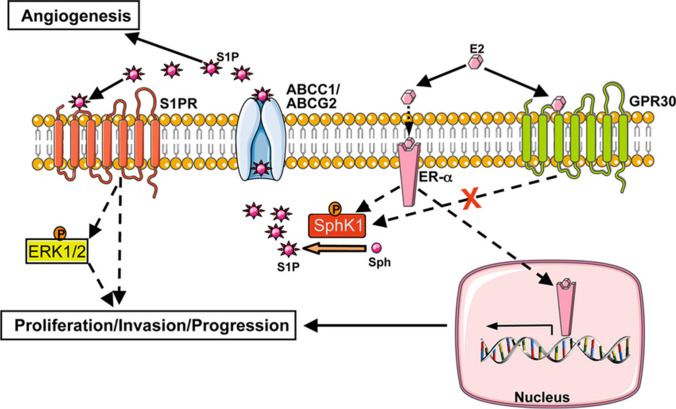
Given to a polar head group, S1P is unable to pass through the plasma membrane freely. It has been demonstrated that ATP-binding cassette (ABC) transporters are involved in S1P export from cancer and non-cancer cells. For example, ABCC1 (MRP1; multidrug-resistant protein 1) transports S1P from mast cells [48], ABCA1 from astrocytes [49], ABCA1 and ABCC1 from endothelial cells [50], and ABCC1 and ABCG2 from breast cancer cells as presented in Fig. 2 [51]. Moreover, spinster homolog 2 (SPNS2), belonging to the non-ATP-dependent organic ion transporters family, also mediates S1P transport [52, 53]. Bradley et al. revealed that SPNS2 plays a critical role in S1P transport in lung cancer cells, while its inhibition abolished cancer cell survival and migration [54]. It has been shown that S1P is determined at higher levels in lymph and blood than in tissue [55]. However, two enzymes reduce and control S1P levels: S1P phosphatase and S1P lyase [56]. S1P phosphatase 1 (SGPP1) removes the phosphate group of S1P and converts it to sphingosine which is subsequently converted to ceramide by ceramide synthase [57]. S1P lyase irreversibly cleaves C2–C3 bond in S1P to produce hexadecenal and phosphoethanolamine [58, 59].
Fig. 2.
The role of ABC transporters and S1P/dihydro-S1P export from the cell in the nongenomic effects of E2 is depicted in this diagram. S1P (and dihydro-S1P, not shown here) is released via ABC transporters ABCC1 and ABCG2 when E2 binds to ER- but not GPR30. This S1P then binds to and activates S1P receptors, causing ERK1/2 to be activated, resulting in downstream signaling events that are critical for breast cancer proliferation, development, and invasion. (Adopted from [45])
High-affinity binding of exported S1P to five transmembrane GPCRs mediates downstream signaling pathways, including pathways mediated by Jun N-terminal kinase (JNK) [60], adenylate cyclase [61], PI3K and Akt [62], and GTPases of the Rho family [63]. The diversity of responses mediated with S1PRs1-5 such as heart development, angiogenesis, cell migration, and immunity, depends on the downstream effectors and receptor expression pattern. For instance, binding to S1PR1 or S1PR3 can increase the migration of endothelial cells, whereas activation of S1PR2 showed an opposite effect [64, 65].
Roles of S1P and its receptors in cancer and cancer therapy
Since the important role of S1P was demonstrated in inhibiting apoptosis and enhancing proliferation [41, 66], many studies have focused on S1P and its receptor's role in cancer and cancer therapy.
SphKs and cancer
There is substantial evidence suggesting the crucial role of dysregulated SphKs (specifically SphK1) along with a transformed signaling mechanism, in cancer development. For example, Acharya et al. found that SphK1 promoted metastasis of triple-negative breast cancer (TNBC) by upregulating the expression of the FSCN1 (fascin) gene through NF-κB activation. They showed that the activation of the SphK1/NF-κB/FSCN1 pathway was associated with poor patient survival and distance metastasis, whereas inhibition of SphK1 or NF-κB remarkably inhibited tumor growth and lung metastasis in a TNBC mouse model [67]. SphK1 also leads to the enhanced growth factor receptor (EGFR) transactivation, via estrogen (E2) induction in human breast cancer cells. The mechanism is based on a novel signaling mechanism where E2 triggers activation of SphK1 and as a result, S1P is released. This results in the EGFR transactivation, revealing the role of SphK1 in the signal pairing between S1P, E2, and EGF triggered events [68, 69]. It has been reported that 31% of patients with colorectal cancer (CRC) exhibited higher SphK1 expression and it was correlated with higher histological grade, vascular invasion, lymphatic invasion, distance metastasis, and lower overall survival times [70]. Lee et al. revealed that lipopolysaccharide (LPS), the main component in the membrane of Gram-negative bacteria, could activate SphK1 by inducing the S225 phosphorylation of SphK1 and its translocation to the plasma membrane, resulting in S1P production and S1PR4 receptor activation which enhances invasion and metastasis of prostate cancer cells [71]. In another study, the comparison of SphK1 expression levels in tumor tissues and adjacent normal tissue samples revealed that patients with hepatocellular carcinoma (HCC) had significantly upregulated SphK1 levels, and higher SphK1 expression was correlated with shorter overall survival times. Furthermore, higher expression of SphK1 in HCC cell lines mediates resistance to oxaliplatin via modulating Akt/GSK3β pathway, while SphK1 knockdown increases chemosensitivity of HCC cell lines [72]. Over expression of SphK1 is also involved in resistance to daunorubicin and cisplatin in leukemia and colon cancer cells [73, 74].
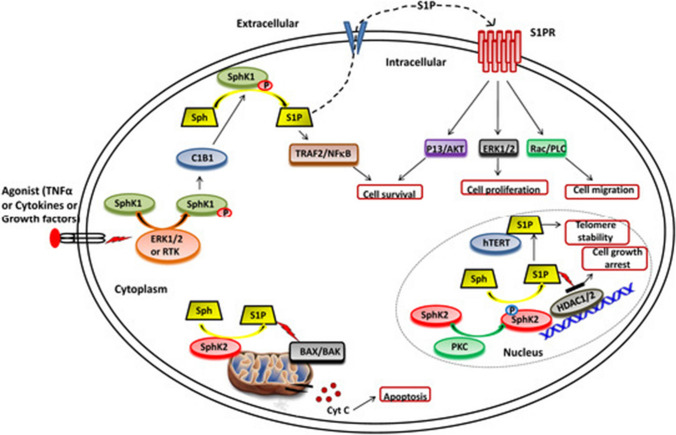
It has been shown that SphK1 could suppress apoptosis of cancer cells. For instance, Taha et al. found that SphK1 knockdown led to cell cycle arrest and induction of apoptosis as shown in Fig. 3, characterized by caspase activation, cytochrome c (Cyt c) release, and oligomerization of Bax in the mitochondrial membrane of breast cancer cells [75]. Song et al. found that the expression of SphK1 was significantly increased in non-small cell lung cancer (NSCLC) patients which was correlated with poor survival of patients. They also showed that over expression of SphK1 markedly inhibited docetaxel or doxorubicin-induced apoptosis via inducing anti-apoptotic proteins such as Bcl-xl, TRAF1, c-IAP1, and c-IAP2 as indicated in Fig. 3, whereas SphK1 inhibition or silencing enhanced NSCLC cells sensitivity to chemotherapy-induced apoptosis [76]. It has been demonstrated that SphK1 contributes to apoptosis resistance via regulating the Akt/FOXO3a/Bim pathway in glioma cells and gastric cancer cells, leading to the downregulation of Bim as a pro-apoptotic protein [77, 78].
Fig. 3.
SphKs and S1P have different functions in cells. SphK1 is translocated from the cytoplasm to the plasma membrane and interacts with calcium-myristoyl switch protein 1 after ERK1/2 phosphorylation/activation in the presence of different agonists (such as TNF, cytokines, and other growth hormones) (C1B1). This allows for the phosphorylation of sphingosine to produce S1P, which can then be released or interact with intracellular targets (such as TRAF2) to perform its functions. S1P interacts to the S1P receptor (S1PR) located in the plasma membrane after being secreted out of the cell, activating numerous downstream signalling pathways that affect cell survival, proliferation, and migration. SphK2 facilitates the phosphorylation of sphingosine in the nucleus to produce S1P, which inhibits histone deacetylases (HDAC1/2) and controls gene expression. In human and mouse fibroblasts, S1P binds to human telomerase reverse transcriptase (hTERT) in the nuclear periphery, inhibiting its interaction with makorin ring finger protein 1 (MKRN1) and promoting telomerase stability. SphK2 also causes S1P to be produced in the mitochondria. (https://encyclopedia.pub/10045)
Due to its role in tumor growth and progression, some SphK inhibitors have been developed to combat cancer. For example, MP-A08 reduces S1P levels via selectively targeting the ATP-binding site of SphK1 and SphK2, leading to inhibition of cancer cell proliferation and apoptosis induction [79]. A dual SphK1/SphK2 inhibitor, called SphKI-II, enhances the sensitivity of HCC cells to 5-Fluorouracil (5-FU) and reduces cell proliferation and migration as well as inducing apoptosis [80]. It has been reported as toxic for bladder carcinoma and breast cancer cells [81]. SK1-I, an inhibitor of SK1, induces apoptosis of leukemia cells [82]. LCL146 and LCL351 are SphK activity inhibitors and are harmful to cancer cells [83]. FTY720 vinyl phosphonate inhibits SK1 in breast and prostate cancer cells [84]. Dai et al. reported that ABC294640, an SphK2 inhibitor, could suppress Kaposi sarcoma-associated herpesvirus (KSHV)-induced tumor growth by inducing autophagic death instead of apoptosis [85]. A phase I clinical trial indicated that ABC294640 was well tolerated in patients with solid tumors [86]. Patwardhan et al. reported reduced S1P levels in lymphoma cultured cells by the action of SLP7111228, an SphK1-selective inhibitor, and SLP120701, an SphK2-selective inhibitor [87].
S1P, its receptors, and cancer
The five S1PRs show presence in several of the human organs/systems. Initially, Wang et al. [88] reported the presence of S1PR3 in nucleus only, while various studies reported that rest of them exist in both the nucleus and cytoplasm. However, Park et al. [89] has reported S1PR3 presence in apoptotic exosome-like vesicles, lumen and membrane as well. Presence of S1PRs on cellular membranes is limited and the expression pattern of all these varies from cell to cell and tissue to tissue, in benign and invasive cells [88]. S1PRs play various roles in cancer [90]. S1PR1 enhances the migratory ability of the proliferating cells in a kidney-derived tumor cell line wiT49 [91]. Apart from this, it also enhances the invasion and migration of cancerous cells in glioblastoma [92] and oncogenic fibrosarcoma cell line [93]. S1PR2 plays a dual role, with pro-oncogenic and inhibitory properties. It suppresses migration in glioblastoma [94], invasion in melanoma cells [95], and proliferation in Wilms tumor cells [96] while it enhances proliferation in liver cancer cells [97], invasion in glioblastoma cell lines [98], and migration in oral squamous cell carcinoma [99]. Ponnusamy et al. demonstrated that the activated S1PR2 facilitates lung colonization/metastasis through S1P/S1PR2/Brms1 (breast carcinoma metastasis suppressor 1) pathway [100]. On the other hand, it has been shown that S1P reduces hepatocyte growth factor (HGF)-induced migration of HCC via S1PR2, but not through other S1PRs [101]. Furthermore, Du et al. identified S1PR2 as a negative regulator of tumor angiogenesis and growth [102].
SIPR3 enhances migration and invasion in gastric [6], breast [103], and nasopharyngeal cancer cell lines [104]. S1P enhances invasion and migration of breast cancer cells both in vitro and in vivo by inducing the expression of matrix metalloproteinase-9 (MMP-9) in the S1P/S1PR3/Gαq axis [103]. MMP9 facilitates the migration and invasion of cancer cells via cleaving extracellular matrix (ECM) proteins [105]. Recently, Sukocheva et al. have reported SphK1 and S1P3 nuclear translocation due to the action of S1P and estrogen results in the cell proliferation in MCF-breast cancer cell lines and vice versa on inhibition [106]. The S1P/S1PR3 interaction also mediates metastasis of TNBC via promoting the Notch signaling pathway [107]. It has also been found that S1PR4 is associated with poor prognosis and reduces the survival time in estrogen receptor-negative breast cancer cells. S1PR5 is also implicated in both suppressing tumors as in squamous cell carcinoma and promoting autophagy in prostate cancer [108].
As mentioned above, there is evidence that S1PRs are involved in tumor angiogenesis. Angiogenesis, sprouting new vessels from the preexisting ones, provides oxygen and nutrients for distant tumor cells to guarantee their growth [109, 110]. Sphingomab®, a monoclonal antibody against S1P, has been developed to block S1P interaction with SIPRs. The anti-S1P monoclonal antibody could reduce tumor proliferation, growth, invasion, and angiogenesis [111]. Sphingomab antibody neutralization of the S1P has been reported to reduce the tumor growth in the murine model. This was also effective in treating the mice resistant to sunitinib treatment [112], probably because it binds with higher affinity than receptors of S1P. This prevents interaction with S1PRs. Old antibodies are no longer available and new ones are being developed [113]. It has been shown that FTY720, an antagonist of S1PRs, could inhibit tumor growth, metastasis, vascularization, and angiogenesis by internalizing S1PRs, inhibiting their recycling to the cell surface, and desensitizing their function [114]. Chae et al. developed RNA interference against the S1PR1 receptor and found that the S1PR1 is required for endothelial cell (EC) migration and tumor angiogenesis, whereas S1PR1 silencing suppresses angiogenesis and tumor growth in vivo [115]. Mechanistically, S1P activates S1PR1 amplifies VEGFR2‐dependent c‐Abl1 and Rac activation and EC migration to support tumor growth [116]. Dai et al. found that S1PR1 and S1PR3, but not S1PR2, mediate the angiogenic effect of S1P. The inhibition of S1PR1 and S1PR3, but not S1PR2, could attenuate tumor angiogenesis and inhibit the expression of angiogenic factors. They also showed that the expression level of SphK1, but not SphK2, was positively correlated with the microvascular density of ovarian cancer tissue [117]. In contrast to the mentioned studies, Gaengel et al. indicated that S1PR1 signaling restricts angiogenesis, whereas loss of S1PR1 increases EC sprouting and vessel branch formation [118].
S1P and S1PRs also mediate the immune escape of cancer cells. For example, Liu et al. showed that S1PR1 could promote tumor-associated regulatory T cell (Treg) expansion in bladder cancer patients, leading to poor overall survival. Mechanistically, the S1PR1 receptor activates TGF-β signaling pathway results in TGF-β and IL-10 secretion from tumor cells. The secreted TGF-β and IL-10 could promote Treg migration into the tumor microenvironment [119]. Chakraborty et al. demonstrated that S1P could promote T cells' differentiation into Tregs in a receptor-independent pathway and intracellular peroxisome proliferator-activated receptor gamma (PPARγ)-dependent manner. They showed that SphK1-deficient T cells reduce differentiation to Tregs and inhibition of SphK1 improves the anti-tumor activity of T cells [120].
Interaction of miRNAs with SphKs, S1P, and its receptors in cancer
There is accumulating evidence that miRNAs mediate tumor development, progression, and treatment via targeting SphKs, S1P, and S1P receptors (Fig. 1). Interaction with various miRNAs has been summed up below.
miR-148a
MiR-148a is located on chromosome 7p15.2 (68 nucleotide in length) and its expression is downregulated in various cancers, including colorectal, liver, gastric, breast, lung, esophageal, and pancreatic cancers [121]. Recently, Paczkowska et al. reported that mir-148a is inactivated due to methylation in classical Hodgkin lymphoma, whereas its over expression reduces tumor cell proliferation [122]. Also, it has been shown that miR-148a inhibits tumor cell invasion, migration, and metastasis [123]. Zhang et al. showed that miR-148a expression is significantly downregulated in HCC tissue and cell lines, while its upregulation notably inhibits HCC cell invasion. They found that miR-148a negatively regulates S1PR1 in HCC cells [124].
miR-542-3p
MiR-542-3p, as a tumor suppressor miRNA, is located on chromosome Xq26.3 which is downregulated in various types of cancers, including astrocytoma, esophageal squamous cell carcinoma, and bladder cancer [125]. For instance, Yuan et al. indicated that downregulation of miR-542-3p is markedly associated with lymph node metastasis and advanced tumor stage in patients with CRC. Moreover, the induced upregulation of miR-542-3p could suppress tumor cell proliferation, migration, and invasion as well as induce apoptosis both in vitro and in vivo [126]. It has been shown that there is a negative correlation between the expression levels of miR-542-3p and S1PR1 in breast cancer tissue and cell line. Breast cancer cells significantly reduce the expression of miR-542-3p, while the expression of S1PR1 is upregulated, depicting a yin yang relationship. It was demonstrated that transfection of miR-542-3p into MCF-7 cells could inhibit tumor cell proliferation, colony formation, migration, and invasion. MiR-542-3p directly binds to 3′-UTR of S1PR1 mRNA and suppresses its tumorigenesis activity [127].
miR-506
MiR-506, a component of the X chromosome-linked cluster in the primate, is involved in various physiological and pathological conditions, including cancer [128, 129]. Most studies demonstrated miR-506 as a tumor suppressor miRNA in cancer such as CRC [130], lung [131], and ovarian [132] cancers. For example, it has been shown that miR-506 is markedly reduced in nasopharyngeal carcinoma tissues and cell lines. In contrast, its ectopic upregulation significantly suppresses cell proliferation, colony formation, and invasion by targeting Forkhead box Q1 (FOXQ1), which is involved in tumor cell proliferation and metastasis [133]. Lu et al. found that transient transfection of miR-506 in hepatoma cells restrained SphK1 expression at both mRNA and protein levels, whereas treatment with miR-506 inhibitor leads to opposite results, suggesting that miR-506 directly targets SphK1. They also indicated that inhibition of SphK1 via miR-506 suppresses tumor angiogenesis [134]. In another study, Li et al. indicated that downregulation of miR-506 is notably associated with pathological tumor status, clinical stage, distant metastasis, and decreased survival in patients with pancreatic cancer. Furthermore, miR-506 ectopic overexpression inhibits cell proliferation and induces cell cycle arrest, apoptosis, and chemosensitivity. They identified that tumor-suppressive effects of miR-506 are associated with targeting SphK1 and inhibition of the SphK1/Akt/NF-κB signaling pathway. They also studied the mechanism responsible for miR-506 downregulation in cancer tissues and identified that hypermethylation of one of five CpG sites in the miR-506 promoter region silences its expression in pancreatic cancer [135].
miR‐101
MiR-101 is generated from two precursors: miR-101–1 and miR-101–2, which are located on chromosomes 1p31 and 9p24, respectively. As a tumor suppressor miRNA, miR-101 is downregulated in various cancers, including HCC, osteosarcoma, oral squamous cell carcinoma, gastric, bladder, and cervical cancer [136]. For example, miR-101 can inhibit tumor cell proliferation, growth, migration, and metastasis and enhance apoptosis and the inhibitory effect of chemotherapy agents on cancerous cells [137–139]. Chen et al. showed that the exogenous expression of miR-101 by CRC cell lines inhibits cell growth by targeting and inhibiting SphK1 expression, leading to ceramide production as a pro-apoptotic product. In contrast, miR-101 downregulation increases SphK1 expression and reduces ceramide levels in CRC cells. They also reported that overexpression of miR-101 increases the chemosensitivity of CRC cells both in vitro and in vivo [140]. It has been shown that S1P could suppress tumor cell migration and downregulate MMP-2 expression in chondrosarcoma cells through upregulation of tissue inhibitor of metalloproteinase‐3 (TIMP‐3), which is the target miR-101. Thus, the S1P/TIMP-3/miR-101 pathway determines the metastasis of chondrosarcoma [141].
miR-9
There are three precursor transcripts for miR-9: miR-9-1, miR-9-2, and miR-9-3, which are located on chromosomes 1, 5, and 15, respectively [142]. MiR-9 displays opposite roles in various cancers. For instance, it has been demonstrated that the absorption of exosomal miR-9 via ECs could promote tumorigenesis and angiogenesis in glioma [143]. On the other hand, miR-9 acts as an inhibitor of cell proliferation and invasion and an inducer of apoptosis in ovarian cancer [144]. MiR-9 also enhances the sensitivity of lung cancer cells to cisplatin [145]. Recently, Yao et al. investigated the role of miR-9 in angiogenesis and found that miR-9 is upregulated in ECs from glioblastoma and medulloblastoma xenograft. They showed that miR-9 overexpression is negatively associated with the expression of S1PR1 and S1PR3. Although miR-9 meaningfully suppresses both S1PR1 and S1PR3 at mRNA and protein levels, only S1PR1 was directly targeted via miR-9. Furthermore, S1PR1 upregulation inhibited the miR-9-induced angiogenesis [146].
miR-124
Three genes have been identified for human miR-124, including miR-124a-1, miR-124a-2, and miR-124a-3, located on the chromosomes 8p23.1, 8q12.3, and 20q13.33, respectively [147]. There is evidence indicating miR-124 dysregulates in various cancers and acts as a tumor suppressor miRNA. For example, Xie et al. found that miR-124 expression is downregulated in CRC patients, whereas its upregulation in CRC cells could intensify the cytotoxicity effects of chemotherapy agents [148]. In gastric cancer, it downregulates SPHK1 expression via direct targeting of its 3′-UTR [149]. MiR-124 also suppresses the migration and invasion of HCC cells by inhibiting integrin αV [150]. Integrins are essential transducers of bidirectional cellular signaling and regulators of cell adhesion, migration, invasion, and tissue remodeling [151, 152]. It has been demonstrated that miR-124 exerts its anti-tumor effects via targeting SphK1 in osteosarcoma, melanoma, head, and neck squamous cell carcinoma, and ovarian cancer [153–156]. The inhibition of SphK1 by miR-124 leads to ceramide accumulation, an increase in the levels of pro-apoptotic PARP, BAX, and BAD proteins, and a decrease in the levels of anti-apoptotic Bcl-xL and Bcl-2 proteins [155]. In another study, Zhang et al. indicated that the exosomal transfer of miR-124 hinders normal fibroblasts' transition to cancer-associated ones and cell mobility via inhibiting SphK1 in ovarian cancer [156]. So, miR-124 upregulation is a promising candidate in controlling tumor growth and metastasis.
miR-125-b
There are two precursor transcripts for miR-125-b, including miR-125b-1 and miR-125b-2, located on the chromosomes 11q24 and 21q21. It has been shown that miR-125-b plays a dual role in tumorigenesis [157]. For example, miR-125-b is remarkably upregulated in retinoblastoma and leukemia, leading to tumor growth, drug resistance, and apoptosis suppression [158, 159]. On the other hand, the miR-125-b expression is significantly reduced in breast, ovarian, and thyroid cancer [160–162]. Zhao et al. investigated the expression levels and potential role of miR-125-b in the pathogenesis of bladder cancer. They indicated that patients with bladder cancer downregulate miR-125-b expression, whereas the external overexpression of miR-125-b could inhibit cellular growth, migration, and cell cycle arrest via directly targeting the 3′-UTR of SphK1 [163]. In another study, Zhang et al. found that patients with non-small cell lung cancer (NSCLC) and NSCLC cell lines significantly reduce the expression levels of miR-125b-1-3p. Furthermore, overexpression of miR-125b-1-3p suppresses cell proliferation, migration, and invasion and induces apoptosis of NSCLC cells by binding to the 3′-UTR of S1PR1 [164].
miR-128
Two genes encode miR-128: miR-128–1 located on chromosome 2q21.3 and miR-128–2 located on chromosome 3p22.3 [165]. It has been demonstrated that miR-128 aberrantly expresses in many kinds of malignancies. Hu et al. reported that miR-128 expression was notably reduced in NSCLC tissues and cells, and it is correlated with cancer cell differentiation, lymph node metastasis, and pathological stage. In contrast, ectopic upregulation of miR-128 inhibited cell proliferation, colony formation, migration, invasion, and angiogenesis and induced cell cycle arrest and apoptosis [166]. The expression levels of miR-128 are remarkably downregulated in papillary thyroid cancer and follicular thyroid carcinoma tissues and cell lines, whereas its ectopic upregulation hampers tumor cell proliferation and invasion and induces cell cycle arrest and apoptosis by targeting SphK1. On the other hand, SphK1 upregulation notably abrogated anti-tumor functions of miR-128, which promotes proliferation and metastasis and reduces apoptosis. Furthermore, miR-128 overexpression in a tumor mice model reduces tumor weight and tumor growth rate and suppresses SphK1 [167]. Thus, miR-128 may be considered as an anti-tumor agent owing to its tumor-suppressive role.
miR-613
MiR-613 is located on chromosome 12p13.1 and there is growing evidence revealing its crucial role, generally its tumor suppressor role, in tumorigenesis [168]. It has been demonstrated that the expression levels of miR-613 are significantly reduced in various cancers, including glioma, gastric, and breast cancer [169–171]. The lower levels of miR-613 were remarkably negatively associated with the overall free survival in patients with melanoma, whereas its ectopic upregulation inhibited tumor cell proliferation, colony formation, migration, and invasion via targeting the sex-determining region Y-box 9 (SOX9), which promotes cell proliferation and invasion as an oncogene [169]. Moreover, both SphK1 and SphK2 are the direct target of miR-613. MiR-613 is downregulated in bladder and papillary thyroid cancer cell lines and tissues. In contrast, its ectopic upregulation suppresses tumor cell growth, migration, invasion, and EMT by targeting the 3′-UTR of SphK1 and SphK2 in the bladder and papillary thyroid cancers, respectively [172, 173].
miR-515-5p
MiR-515-5p is located on chromosome 19, which acts as a tumor suppressor. For instance, Zhang et al. found that prostate cancer cell lines and tissues significantly reduce the expression of miR-515-5p, whereas its overexpression negatively regulates tumor cell proliferation and migratory characteristics by binding to thyroid hormone receptor interactor 13 (TRIP13), as a tumor promoter. Furthermore, the expression levels of miR-515-5p in the advanced T stage of patients with prostate cancer are remarkably lower than those in the early T stage [174]. It has been shown that miR-515-5p also mediates its tumor suppressor roles via targeting SphK1. Pinho et al. demonstrated that estrogen receptor α (ERα) suppresses the expression of miR-515-5p in breast cancer and its enforced expression reduces tumor cell proliferation and SphK1 activity and induces caspase-dependent apoptosis. They reported that miR-515-5p downregulation increases the proliferation of breast cancer cells and estrogen-dependent SphK1 activity [175].
miR-330-3p
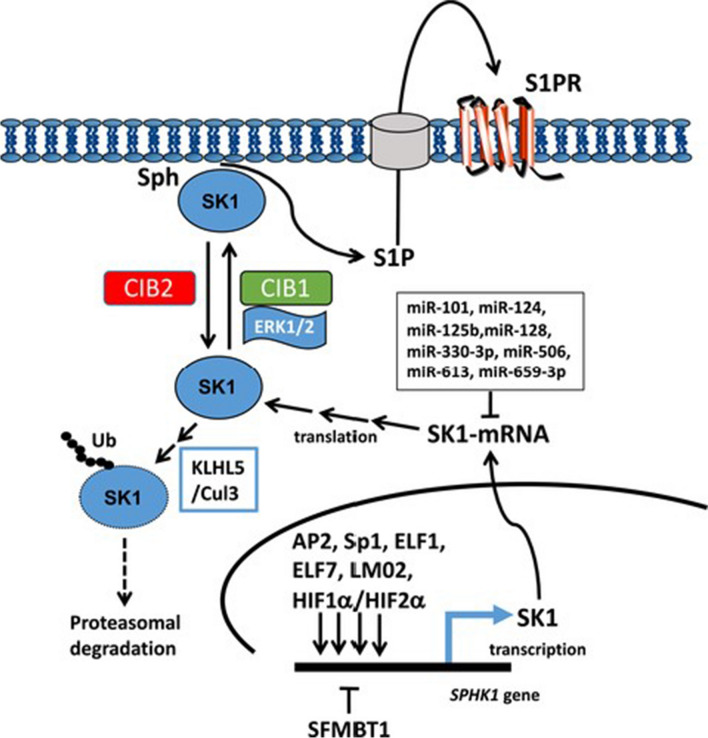
MiR-330-3p, located on chromosome 19q13.32 [176], is dysregulated in various cancers. It has been demonstrated that miR-330-3p is downregulated in laryngeal squamous cell carcinoma [177] and glioma [178] but overexpressed in lung cancer [179] and esophageal squamous cell carcinoma (ESCC) [180]. For example, miR-330-3p can regulate the proliferation and migration of glioma cells as a tumor suppressor miRNA [178]. On the other hand, upregulation of miR-330-3p notably promotes proliferation, migration, invasion, and survival of ESCC cells in vitro and stimulates tumor formation in the mice model [180]. Wang et al. found that miR-330-3p directly targets SphK1 and S1PR1 in gastric cancer cells. They reported that SphK1 knockdown could remarkably suppress tumor cell proliferation, block cell cycle, induce apoptosis, and inhibit their invasiveness. Furthermore, miR-330-3p upregulation inhibits SphK1 and S1PR1 expression levels like FTY720 (an SphK1 inhibitor) and VPC23019 (an S1PR1 antagonist) [181]. There are numerous examples of SK1 (SphK1) overexpression at the mRNA and protein levels, which is frequently associated with poor prognosis in cancer patients, including shorter survival and earlier disease recurrence [5]. Triple-negative breast cancer [67], Melanoma [182], non-small cell lung cancer [183], colorectal cancer [70] and papillary thyroid carcinoma [184] are some recent examples. This is in line with SK1's propensity to enhance cell survival, proliferation, and neoplastic transformation, and it backs up SK1(SphK1) inhibitors' therapeutic potential. The molecular processes that regulate SK1 (SphK1) is abridged in Fig. 4.
Fig. 4.
Sphingosine kinase 1 regulation in cancer. The transcriptional and post-translational processes that regulate SK1 in cancer are depicted in this diagram. AP2, Sp1, ELF1, ELF7, LM02, and HIF1a/HIF2a are involved in stimulated transcriptional regulation of SK1 gene expression, whereas SFMBT2 is involved in inhibition. SK1 is translocated to the plasma membrane after being post-translationally changed (phosphorylation) by ERK-2; translocation is favourably controlled by CIB1 and hindered by CIB2. Because SK1 is localized at the plasma membrane, it can access its substrate, resulting in the synthesis of S1P, which is subsequently released to act on S1P receptors. SK1 is regulated by KLH5-Cul3, which promotes ubiquitin-proteasomal degradation of the protein. (Adopted from [195])
miR-144-3p
MiR-144-3p, encoded by chromosome 17q11.2 [185], plays a controversial role in various cancers. It acts as an oncogene in papillary thyroid carcinoma [186] and renal carcinoma [187], whereas it also can act as a tumor suppressor in laryngeal squamous cell carcinoma [188] and gastric cancer [189]. For instance, miR-144-3p upregulation promotes tumor cell survival, growth, and metastasis in papillary thyroid carcinoma, while it can suppress proliferation, EMT, and invasiveness of gastric cancer cells [189]. Using bioinformatics predictions and digital gene expression (DGE) analysis, Liang et al. found that miR-144-3p mediates the pro-invasive role of SphK1 in papillary thyroid cancer cells via targeting the fibronectin 1 (FN1) protein. They also showed that miR- 144-3p expression levels are decreased by SphK1 overexpression [190].
miR-133b
MiR-133b, encoded by chromosome 6p12.2, is abnormally expressed in different types of cancers and plays a dual role in tumorigenesis [191]. For example, it has been shown that miR-133b is downregulated in tissues and cell lines of breast cancer, whereas its exogenous upregulation could inhibit tumorigenesis, colony formation, and metastasis characteristics of breast cancer [192]. On the other hand, miR-133b can act as an oncogene in cervical cancer, which promotes tumorigenesis and metastasis [193]. Cheng et al. investigated the expression, roles, and underlying mechanisms of miR-133b in nasopharyngeal carcinoma. They demonstrated that nasopharyngeal carcinoma tissues significantly reduced the expression levels of miR-133b compared with adjacent normal tissues. The exogenous miR-133b upregulation could significantly inhibit nasopharyngeal carcinoma cell proliferation via targeting S1PR1 and regulating STAT3 signaling. Since S1PR1 is crucial for STAT3 activation in cancer cells, they found that overexpression of miR-133b markedly reduced the expression levels of STAT3 in the phosphorylated form [194].
Other miRNAs
In addition to the mentioned miRNAs, other ones also regulate SphKs, S1P, and S1PRs in several types of cancer. For instance, miR-659-3p negatively regulates SphK1 in chronic myeloid leukemia and CRC, leading to inhibition of cell proliferation, induction of apoptosis, and regulation of resistance to chemotherapy [195, 196]. MiR-659-3p expression was notably reduced in cisplatin-resistant CRC clinical samples and cell lines, whereas the expression levels of SphK1 were increased in cisplatin-resistant CRC samples. Additionally, knockdown of SphK1 could resensitize parental CRC cell lines to cisplatin [196]. Another miRNA that regulates response to therapy by targeting the S1P pathway is miR-95. Huang et al. found that miR-95 mediates resistance to radiotherapy by targeting S1P phosphatase 1 (SGPP1), while FTY720 treatment of tumor cells sensitized them to radiotherapy [197]. Zhang et al. showed that miR-338-3p expression levels are downregulated in NSCLC tissues. In contrast, miR-338-3p overexpression notably induced apoptosis and inhibited the proliferation of NSCLC cells via directly inhibiting SphK2 [198]. In another study, Bao et al. indicated that CRC tissues and cell lines significantly decreased miR-27a levels, which was associated with clinical pathological stages and distant metastasis, whereas its overexpression could attenuate CRC cell proliferation and migration and promote apoptosis by targeting SGPP1 and Smad2 [199]. In gastric cancer tissues and cell lines, overexpression of miR-31 remarkably reduced SGPP2 and Smad4 levels, leading to inhibition of tumor cell proliferation and migration and promotion of apoptosis [200]. We also retrieved oncogenic miRNA interactions with S1P, S1PRs, and SphKs via miRTex database (URL: https://research.bioinformatics.udel.edu/miRTex/) shown in the Table 2.
Table 2.
miRNA interactions with S1P, S1PRs, and SphKs with a role in cancer pathogenesis
| Serial no | miRNA | Regulation | Cancer type/function | Interacting/target gene | References |
|---|---|---|---|---|---|
| 1 | miR-506 | Downregulates | Liver cancer angiogenesis | SPHK1/S1P | [134] |
| 2 | miR-17 | Downregulates | Migration of thyroid cancer cells | S1P | [201] |
| 3 | miR-95 | Upregulates | Tumor growth and radiation resistance in PC3 prostate and breast cancer cells | S1P and SGPP1 | [197] |
| 4 | MicroRNA-363 | Downregulates | Proliferation of hepatocellular carcinoma cells | S1PR1 | [202] |
| 5 | microRNA-148a | Downregulates | Hepatocellular carcinoma cell invasion | S1PR1 | [124] |
| 6 | miR302-367 | Downregulates | Tumor growth and angiogenesis | S1PR1 | [203] |
| 7 | miR-92a | Downregulates | Tumor growth and angiogenesis | S1PR1 | [204] |
| 8 | MiR-101 | Downregulates | Colorectal cancer cells expression | SphK1 | [140] |
| 9 | MiR-124 | Downregulates | Ovarian cancer cell invasion/migration | SphK1 | [205] |
| 10 | miR-125b | Downregulates | Bladder cancer cell proliferation and migration | SphK1 | [163] |
| 11 | miR-659-3p | Downregulates | Colorectal cancer cells | SphK1 | [196] |
| 12 | miR-107 | Upregulates | Tumor angiogenesis in liver cancer | SphK1 | [206] |
| 13 | miR-613 | Downregulates | Papillary thyroid carcinoma | SphK2 | [173] |
Conclusions
In the last decades, significant effort has been expended to clarify the function of S1P signaling and its modulators, including SphKs and S1P receptors, in the development and treatment of human malignancies. The interaction between SphKs, S1P, and S1P receptors with miRNAs and their roles in tumorigenesis has attracted increasing interest in finding out this regulatory network in different aspects of cancer. The researchers recognized that targeting SphKs, S1P, and S1P receptors with different miRNAs can inhibit tumor cell proliferation, survival, migration, and metastasis. Today, SphK2 inhibitor ABC294640 has undergone clinical trials to treat pancreatic cancer and multiple myeloma (NCT01488513 and NCT02757326). Furthermore, the loss of S1PR1 in T-cell dysfunction for anti-tumor activities is under investigation (NCT04657146). Uncovering the crosstalk between miRNAs and the S1P pathway will provide promising outcomes in clinical trials. On the other hand, emerging novel isothermal amplification techniques for quantifying miRNAs, including duplex-specific nuclease signal amplification and rolling circle amplification, may overcome current methods' limitations by minimizing equipment demands, reducing cost and time, and providing specific and sensitive miRNA detection. The ease and speed of these techniques will help to identify the targets of miRNAs in the S1P pathway and, ultimately, proper preventive and therapeutic interventions. Therefore, fully understanding the interaction between SphKs, S1P, and S1P receptors with miRNAs in human malignancies will provide a new approach in cancer therapy based on miRNAs.
Acknowledgements
Not applicable.
Abbreviations
- S1P
Sphingosine-1-phosphate
- SphKs
Sphingosine kinases
- S1PRs
S1P receptors
- EMT
Epithelial-mesenchymal transition
- miRNAs
MicroRNAs
- 3′-UTR
3′-Untranslated regions
- ABC
ATP-binding cassette
- SPNS2
Spinster homolog 2
- CRC
Colorectal cancer
- HCC
Hepatocellular carcinoma
- NSCLC
Non-small cell lung cancer
- EC
Endothelial cell
Authors’ contributions
GX and ZY conceived the idea. GX, ZY, YS, HD, and JM searched the literature, collected the required contents, and wrote the manuscript. The final version of this manuscript was approved by all the authors.
Funding
None.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Guangmeng Xu, Email: jlumeng@jlu.edu.cn.
Zecheng Yang, Email: zcyang@jlu.edu.cn.
Yamin Sun, Email: 153202883@qq.com.
Hongmei Dong, Email: DONGHM@jlu.edu.cn.
Jingru Ma, Email: jrma@jlu.edu.cn.
References
- 1.Stunff HL, Milstien S, Spiegel S. Generation and metabolism of bioactive sphingosine-1-phosphate. J Cell Biochem. 2004;92(5):882–899. doi: 10.1002/jcb.20097. [DOI] [PubMed] [Google Scholar]
- 2.Pyne NJ, et al. Role of sphingosine 1-phosphate receptors, sphingosine kinases and sphingosine in cancer and inflammation. Adv Biol Regul. 2016;60:151–159. doi: 10.1016/j.jbior.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Pyne S, Pyne NJ. Sphingosine 1-phosphate signalling in mammalian cells. Biochemical Journal. 2000;349(2):385–402. doi: 10.1042/bj3490385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spiegel S, Milstien S. Sphingosine 1-phosphate, a key cell signaling molecule. J Biol Chem. 2002;277(29):25851–25854. doi: 10.1074/jbc.R200007200. [DOI] [PubMed] [Google Scholar]
- 5.Pyne S, Adams DR, Pyne NJ. Sphingosine 1-phosphate and sphingosine kinases in health and disease: recent advances. Prog Lipid Res. 2016;62:93–106. doi: 10.1016/j.plipres.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Pyne NJ, Pyne S. Sphingosine 1-phosphate and cancer. Nat Rev Cancer. 2010;10(7):489–503. doi: 10.1038/nrc2875. [DOI] [PubMed] [Google Scholar]
- 7.Maczis M, Milstien S, Spiegel S. Sphingosine-1-phosphate and estrogen signaling in breast cancer. Adv Biol Regul. 2016;60:160–165. doi: 10.1016/j.jbior.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Hannun YA, Obeid LM. Sphingolipids and their metabolism in physiology and disease. Nat Rev Mol Cell Biol. 2018;19(3):175–191. doi: 10.1038/nrm.2017.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heffernan-Stroud LA, Obeid LM. Sphingosine kinase 1 in cancer. Adv Cancer Res. 2013;117:201–235. doi: 10.1016/B978-0-12-394274-6.00007-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chumanevich AA, et al. Suppression of colitis-driven colon cancer in mice by a novel small molecule inhibitor of sphingosine kinase. Carcinogenesis. 2010;31(10):1787–1793. doi: 10.1093/carcin/bgq158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goradel NH, et al. Regulation of tumor angiogenesis by microRNAs: state of the art. J Cell Physiol. 2019;234(2):1099–1110. doi: 10.1002/jcp.27051. [DOI] [PubMed] [Google Scholar]
- 12.Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75(5):843–854. doi: 10.1016/0092-8674(93)90529-Y. [DOI] [PubMed] [Google Scholar]
- 13.Alles J, et al. An estimate of the total number of true human miRNAs. Nucleic Acids Res. 2019;47(7):3353–3364. doi: 10.1093/nar/gkz097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miranda KC, et al. A pattern-based method for the identification of MicroRNA binding sites and their corresponding heteroduplexes. Cell. 2006;126(6):1203–1217. doi: 10.1016/j.cell.2006.07.031. [DOI] [PubMed] [Google Scholar]
- 15.Kim VN, Han J, Siomi MC. Biogenesis of small RNAs in animals. Nat Rev Mol Cell Biol. 2009;10(2):126–139. doi: 10.1038/nrm2632. [DOI] [PubMed] [Google Scholar]
- 16.Winter J, et al. Many roads to maturity: microRNA biogenesis pathways and their regulation. Nat Cell Biol. 2009;11(3):228–234. doi: 10.1038/ncb0309-228. [DOI] [PubMed] [Google Scholar]
- 17.Gregory RI, et al. The Microprocessor complex mediates the genesis of microRNAs. Nature. 2004;432(7014):235–240. doi: 10.1038/nature03120. [DOI] [PubMed] [Google Scholar]
- 18.Denli AM, et al. Processing of primary microRNAs by the Microprocessor complex. Nature. 2004;432(7014):231–235. doi: 10.1038/nature03049. [DOI] [PubMed] [Google Scholar]
- 19.Yi R, et al. Exportin-5 mediates the nuclear export of pre-microRNAs and short hairpin RNAs. Genes Dev. 2003;17(24):3011–3016. doi: 10.1101/gad.1158803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bohnsack MT, Czaplinski K, Görlich D. Exportin 5 is a RanGTP-dependent dsRNA-binding protein that mediates nuclear export of pre-miRNAs. RNA. 2004;10(2):185–191. doi: 10.1261/rna.5167604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hutvágner G, et al. A cellular function for the RNA-interference enzyme Dicer in the maturation of the let-7 small temporal RNA. Science. 2001;293(5531):834–838. doi: 10.1126/science.1062961. [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi H, Tomari Y. RISC assembly: coordination between small RNAs and Argonaute proteins. Biochimica et Biophysica Acta (BBA) Gene Regul Mech. 2016;1859(1):71–81. doi: 10.1016/j.bbagrm.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 23.Lin S, Gregory RI. MicroRNA biogenesis pathways in cancer. Nat Rev Cancer. 2015;15(6):321–333. doi: 10.1038/nrc3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gaur A, et al. Characterization of microRNA expression levels and their biological correlates in human cancer cell lines. Can Res. 2007;67(6):2456–2468. doi: 10.1158/0008-5472.CAN-06-2698. [DOI] [PubMed] [Google Scholar]
- 25.Iorio MV, Croce CM. MicroRNAs in cancer: small molecules with a huge impact. J Clin Oncol. 2009;27(34):5848. doi: 10.1200/JCO.2009.24.0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 27.Li XJ, et al. Exosomal MicroRNA MiR-1246 promotes cell proliferation, invasion and drug resistance by targeting CCNG2 in breast cancer. Cell Physiol Biochem. 2017;44(5):1741–1748. doi: 10.1159/000485780. [DOI] [PubMed] [Google Scholar]
- 28.Lv Q, et al. Engineered human adipose stem-cell-derived exosomes loaded with miR-21-5p to promote diabetic cutaneous wound healing. Mol Pharm. 2020;17(5):1723–1733. doi: 10.1021/acs.molpharmaceut.0c00177. [DOI] [PubMed] [Google Scholar]
- 29.Wang P, et al. MicroRNA-126 increases chemosensitivity in drug-resistant gastric cancer cells by targeting EZH2. Biochem Biophys Res Commun. 2016;479(1):91–96. doi: 10.1016/j.bbrc.2016.09.040. [DOI] [PubMed] [Google Scholar]
- 30.Chen Y et al. microRNA-499a promotes the progression and chemoresistance of cervical cancer cells by targeting SOX6. Apoptosis, 2020. p. 1–12. [DOI] [PubMed]
- 31.Cheng D, et al. MicroRNA-20a-5p promotes colorectal cancer invasion and metastasis by downregulating Smad4. Oncotarget. 2016;7(29):45199. doi: 10.18632/oncotarget.9900. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Lu Y, et al. Correction: MicroRNA-140-5p inhibits invasion and angiogenesis through targeting VEGF-A in breast cancer. Cancer Gene Ther. 2020;27(10):838–839. doi: 10.1038/s41417-020-00240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.He C, et al. Hypoxia-inducible microRNA-224 promotes the cell growth, migration and invasion by directly targeting RASSF8 in gastric cancer. Mol Cancer. 2017;16(1):1–14. doi: 10.1186/s12943-016-0568-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang Y, et al. MicroRNA-210 promotes cancer angiogenesis by targeting fibroblast growth factor receptor-like 1 in hepatocellular carcinoma. Oncol Rep. 2016;36(5):2553–2562. doi: 10.3892/or.2016.5129. [DOI] [PubMed] [Google Scholar]
- 35.Li X, et al. microRNA-137 promotes apoptosis in ovarian cancer cells via the regulation of XIAP. Br J Cancer. 2017;116(1):66–76. doi: 10.1038/bjc.2016.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheng Y, et al. MiRNA-183-5p promotes cell proliferation and inhibits apoptosis in human breast cancer by targeting the PDCD4. Reprod Biol. 2016;16(3):225–233. doi: 10.1016/j.repbio.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 37.Das R, et al. MicroRNA-194 promotes prostate cancer metastasis by inhibiting SOCS2. Can Res. 2017;77(4):1021–1034. doi: 10.1158/0008-5472.CAN-16-2529. [DOI] [PubMed] [Google Scholar]
- 38.Liu H-N, et al. miR-181b inhibits chemoresistance in cisplatin-resistant H446 small cell lung cancer cells by targeting Bcl-2. Arch Med Sci AMS. 2018;14(4):745. doi: 10.5114/aoms.2018.76066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jeong J-Y, et al. MicroRNA-136 inhibits cancer stem cell activity and enhances the anti-tumor effect of paclitaxel against chemoresistant ovarian cancer cells by targeting Notch3. Cancer Lett. 2017;386:168–178. doi: 10.1016/j.canlet.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 40.Li P, et al. GC-derived EVs enriched with microRNA-675-3p contribute to the MAPK/PD-L1-mediated tumor immune escape by targeting CXXC4. Mol Ther Nucl Acids. 2020;22:615–626. doi: 10.1016/j.omtn.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cuvillier O, et al. Suppression of ceramide-mediated programmed cell death by sphingosine-1-phosphate. Nature. 1996;381(6585):800–803. doi: 10.1038/381800a0. [DOI] [PubMed] [Google Scholar]
- 42.Takabe K, Spiegel S. Export of sphingosine-1-phosphate and cancer progression. J Lipid Res. 2014;55(9):1839–1846. doi: 10.1194/jlr.R046656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spiegel S, et al. New insights into functions of the sphingosine-1-phosphate transporter SPNS2. J Lipid Res. 2019;60(3):484–489. doi: 10.1194/jlr.S091959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strub GM, et al. Sphingosine-1-phosphate produced by sphingosine kinase 2 in mitochondria interacts with prohibitin 2 to regulate complex IV assembly and respiration. FASEB J. 2011;25(2):600–612. doi: 10.1096/fj.10-167502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hait NC, et al. Regulation of histone acetylation in the nucleus by sphingosine-1-phosphate. Science. 2009;325(5945):1254–1257. doi: 10.1126/science.1176709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alvarez SE, et al. Sphingosine-1-phosphate is a missing cofactor for the E3 ubiquitin ligase TRAF2. Nature. 2010;465(7301):1084–1088. doi: 10.1038/nature09128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Takabe K, et al. “Inside-out” signaling of sphingosine-1-phosphate: therapeutic targets. Pharmacol Rev. 2008;60(2):181–195. doi: 10.1124/pr.107.07113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mitra P, et al. Role of ABCC1 in export of sphingosine-1-phosphate from mast cells. Proc Natl Acad Sci. 2006;103(44):16394–16399. doi: 10.1073/pnas.0603734103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sato K, et al. Critical role of ABCA1 transporter in sphingosine 1-phosphate release from astrocytes. J Neurochem. 2007;103(6):2610–2619. doi: 10.1111/j.1471-4159.2007.04958.x. [DOI] [PubMed] [Google Scholar]
- 50.Lee Y-M, et al. A novel method to quantify sphingosine 1-phosphate by immobilized metal affinity chromatography (IMAC) Prostaglandins Other Lipid Mediat. 2007;84(3–4):154–162. doi: 10.1016/j.prostaglandins.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Takabe K, et al. Estradiol induces export of sphingosine 1-phosphate from breast cancer cells via ABCC1 and ABCG2. J Biol Chem. 2010;285(14):10477–10486. doi: 10.1074/jbc.M109.064162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nijnik A, et al. The role of sphingosine-1-phosphate transporter Spns2 in immune system function. J Immunol. 2012;189(1):102–111. doi: 10.4049/jimmunol.1200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fukuhara S, et al. The sphingosine-1-phosphate transporter Spns2 expressed on endothelial cells regulates lymphocyte trafficking in mice. J Clin Investig. 2012;122(4):1416–1426. doi: 10.1172/JCI60746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bradley E, et al. Critical role of Spns2, a sphingosine-1-phosphate transporter, in lung cancer cell survival and migration. PLoS ONE. 2014;9(10):e110119. doi: 10.1371/journal.pone.0110119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nagahashi M, et al. Sphingosine-1-phosphate in the lymphatic fluid determined by novel methods. Heliyon. 2016;2(12):e00219. doi: 10.1016/j.heliyon.2016.e00219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nagahashi M, et al. The role of sphingosine-1-phosphate in inflammation and cancer progression. Cancer Sci. 2018;109(12):3671–3678. doi: 10.1111/cas.13802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moro K, et al. Ceramide species are elevated in human breast cancer and are associated with less aggressiveness. Oncotarget. 2018;9(28):19874. doi: 10.18632/oncotarget.24903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kumar A, et al. S1P lyase regulation of thymic egress and oncogenic inflammatory signaling. Mediat Inflamm. 2017;2017:1–19. doi: 10.1155/2017/7685142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nakahara K, et al. The Sjögren-Larsson syndrome gene encodes a hexadecenal dehydrogenase of the sphingosine 1-phosphate degradation pathway. Mol Cell. 2012;46(4):461–471. doi: 10.1016/j.molcel.2012.04.033. [DOI] [PubMed] [Google Scholar]
- 60.Kim YM, et al. Gα12/13 induction of CYR61 in association with arteriosclerotic intimal hyperplasia: effect of sphingosine-1-phosphate. Arterioscler Thromb Vasc Biol. 2011;31(4):861–869. doi: 10.1161/ATVBAHA.110.218552. [DOI] [PubMed] [Google Scholar]
- 61.Jiang LI, et al. Use of a cAMP BRET sensor to characterize a novel regulation of cAMP by the sphingosine 1-phosphate/G13 pathway. J Biol Chem. 2007;282(14):10576–10584. doi: 10.1074/jbc.M609695200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang H, Huang H, Ding SF. Sphingosine-1-phosphate promotes the proliferation and attenuates apoptosis of Endothelial progenitor cells via S1PR1/S1PR3/PI3K/Akt pathway. Cell Biol Int. 2018;42(11):1492–1502. doi: 10.1002/cbin.10991. [DOI] [PubMed] [Google Scholar]
- 63.Yu F-X, et al. Regulation of the Hippo-YAP pathway by G-protein-coupled receptor signaling. Cell. 2012;150(4):780–791. doi: 10.1016/j.cell.2012.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee M-J, et al. Akt-mediated phosphorylation of the G protein-coupled receptor EDG-1 is required for endothelial cell chemotaxis. Mol Cell. 2001;8(3):693–704. doi: 10.1016/S1097-2765(01)00324-0. [DOI] [PubMed] [Google Scholar]
- 65.Ryu Y, et al. Sphingosine-1-phosphate, a platelet-derived lysophospholipid mediator, negatively regulates cellular Rac activity and cell migration in vascular smooth muscle cells. Circ Res. 2002;90(3):325–332. doi: 10.1161/hh0302.104455. [DOI] [PubMed] [Google Scholar]
- 66.Olivera A, Spiegel S. Sphingosine-1-phosphate as second messenger in cell proliferation induced by PDGF and FCS mitogens. Nature. 1993;365(6446):557–560. doi: 10.1038/365557a0. [DOI] [PubMed] [Google Scholar]
- 67.Acharya S, et al. Sphingosine kinase 1 signaling promotes metastasis of triple-negative breast cancer. Can Res. 2019;79(16):4211–4226. doi: 10.1158/0008-5472.CAN-18-3803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sukocheva OA. Expansion of sphingosine kinase and sphingosine-1-phosphate receptor function in normal and cancer cells: from membrane restructuring to mediation of estrogen signaling and stem cell programming. Int J Mol Sci. 2018;19(2):420. doi: 10.3390/ijms19020420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sukocheva O, et al. Estrogen transactivates EGFR via the sphingosine 1-phosphate receptor Edg-3: the role of sphingosine kinase-1. J Cell Biol. 2006;173(2):301–310. doi: 10.1083/jcb.200506033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bae GE, et al. Increased sphingosine kinase 1 expression predicts distant metastasis and poor outcome in patients with colorectal cancer. Anticancer Res. 2019;39(2):663–670. doi: 10.21873/anticanres.13161. [DOI] [PubMed] [Google Scholar]
- 71.Lee C-F, et al. Activation of sphingosine kinase by lipopolysaccharide promotes prostate cancer cell invasion and metastasis via SphK1/S1PR4/matriptase. Oncogene. 2019;38(28):5580–5598. doi: 10.1038/s41388-019-0833-3. [DOI] [PubMed] [Google Scholar]
- 72.Wang F, Wu Z. Sphingosine kinase 1 overexpression is associated with poor prognosis and oxaliplatin resistance in hepatocellular carcinoma. Exp Ther Med. 2018;15(6):5371–5376. doi: 10.3892/etm.2018.6086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sobue S, et al. Implications of sphingosine kinase 1 expression level for the cellular sphingolipid rheostat: relevance as a marker for daunorubicin sensitivity of leukemia cells. Int J Hematol. 2008;87(3):266–275. doi: 10.1007/s12185-008-0052-0. [DOI] [PubMed] [Google Scholar]
- 74.Qin L, et al. Down-regulation of sphingosine kinase 1 (SphK1) enhances the chemosensitivity to cisplatin in human colon cancer RKO cells. Xi bao yu fen zi mian yi xue za zhi Chin J Cell Mol Immunol. 2017;33(5):623–629. [PubMed] [Google Scholar]
- 75.Taha TA, et al. Loss of sphingosine kinase-1 activates the intrinsic pathway of programmed cell death: modulation of sphingolipid levels and the induction of apoptosis. FASEB J. 2006;20(3):482–484. doi: 10.1096/fj.05-4412fje. [DOI] [PubMed] [Google Scholar]
- 76.Song L, et al. Sphingosine kinase-1 enhances resistance to apoptosis through activation of PI3K/Akt/NF-κB pathway in human non–small cell lung cancer. Clin Cancer Res. 2011;17(7):1839–1849. doi: 10.1158/1078-0432.CCR-10-0720. [DOI] [PubMed] [Google Scholar]
- 77.Guan H, et al. Sphingosine kinase 1 regulates the Akt/FOXO3a/Bim pathway and contributes to apoptosis resistance in glioma cells. PLoS ONE. 2011;6(5):e19946. doi: 10.1371/journal.pone.0019946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xiong H, et al. SphK1 confers resistance to apoptosis in gastric cancer cells by downregulating Bim via stimulating Akt/FoxO3a signaling. Oncol Rep. 2014;32(4):1369–1373. doi: 10.3892/or.2014.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pitman MR, et al. A selective ATP-competitive sphingosine kinase inhibitor demonstrates anti-cancer properties. Oncotarget. 2015;6(9):7065. doi: 10.18632/oncotarget.3178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Grbčić P, et al. Dual sphingosine kinase inhibitor SKI-II enhances sensitivity to 5-fluorouracil in hepatocellular carcinoma cells via suppression of osteopontin and FAK/IGF-1R signalling. Biochem Biophys Res Commun. 2017;487(4):782–788. doi: 10.1016/j.bbrc.2017.04.100. [DOI] [PubMed] [Google Scholar]
- 81.French SW, et al. Sp1 transactivation of the TCL1 oncogene. J Biol Chem. 2003;278(2):948–955. doi: 10.1074/jbc.M207166200. [DOI] [PubMed] [Google Scholar]
- 82.Paugh SW, et al. A selective sphingosine kinase 1 inhibitor integrates multiple molecular therapeutic targets in human leukemia. Blood, J Am Soc Hematol. 2008;112(4):1382–1391. doi: 10.1182/blood-2008-02-138958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sharma AK. Sphingo-guanidines and their use as inhibitors of sphingosine kinase (WO2010078247) Expert Opin Ther Pat. 2011;21(5):807–812. doi: 10.1517/13543776.2011.573787. [DOI] [PubMed] [Google Scholar]
- 84.Tonelli F, et al. FTY720 and (S)-FTY720 vinylphosphonate inhibit sphingosine kinase 1 and promote its proteasomal degradation in human pulmonary artery smooth muscle, breast cancer and androgen-independent prostate cancer cells. Cell Signal. 2010;22(10):1536–1542. doi: 10.1016/j.cellsig.2010.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dai L, et al. ABC294640, a novel sphingosine kinase 2 inhibitor, induces oncogenic virus-infected cell autophagic death and represses tumor growth. Mol Cancer Ther. 2017;16(12):2724–2734. doi: 10.1158/1535-7163.MCT-17-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Britten CD, et al. A phase I study of ABC294640, a first-in-class sphingosine kinase-2 inhibitor, in patients with advanced solid tumors. Clin Cancer Res. 2017;23(16):4642–4650. doi: 10.1158/1078-0432.CCR-16-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Patwardhan NN, et al. Structure− activity relationship studies and in vivo activity of guanidine-based sphingosine kinase inhibitors: discovery of sphK1-and sphK2-selective inhibitors. J Med Chem. 2015;58(4):1879–1899. doi: 10.1021/jm501760d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang C, et al. Systemic distribution, subcellular localization and differential expression of sphingosine-1-phosphate receptors in benign and malignant human tissues. Exp Mol Pathol. 2014;97(2):259–265. doi: 10.1016/j.yexmp.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Park SJ, et al. Molecular mechanisms of biogenesis of apoptotic exosome-like vesicles and their roles as damage-associated molecular patterns. Proc Natl Acad Sci U S A. 2018;115(50):E11721–E11730. doi: 10.1073/pnas.1811432115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Patmanathan SN, et al. Mechanisms of sphingosine 1-phosphate receptor signalling in cancer. Cell Signal. 2017;34:66–75. doi: 10.1016/j.cellsig.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 91.Li M-H, et al. S1P/S1P1 signaling stimulates cell migration and invasion in Wilms tumor. Cancer Lett. 2009;276(2):171–179. doi: 10.1016/j.canlet.2008.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Young N, Pearl DK, Van Brocklyn JR. Sphingosine-1-phosphate regulates glioblastoma cell invasiveness through the urokinase plasminogen activator system and CCN1/Cyr61. Mol Cancer Res. 2009;7(1):23–32. doi: 10.1158/1541-7786.MCR-08-0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fisher KE, et al. Tumor cell invasion of collagen matrices requires coordinate lipid agonist-induced G-protein and membrane-type matrix metalloproteinase-1-dependent signaling. Mol Cancer. 2006;5(1):1–23. doi: 10.1186/1476-4598-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lepley D, et al. The G protein–coupled receptor S1P2 regulates Rho/Rho kinase pathway to inhibit tumor cell migration. Can Res. 2005;65(9):3788–3795. doi: 10.1158/0008-5472.CAN-04-2311. [DOI] [PubMed] [Google Scholar]
- 95.Arikawa K, et al. Ligand-dependent inhibition of B16 melanoma cell migration and invasion via endogenous S1P2 G protein-coupled receptor: requirement of inhibition of cellular RAC activity. J Biol Chem. 2003;278(35):32841–32851. doi: 10.1074/jbc.M305024200. [DOI] [PubMed] [Google Scholar]
- 96.Li M-H, et al. Induction of antiproliferative connective tissue growth factor expression in Wilms' tumor cells by sphingosine-1-phosphate receptor 2. Mol Cancer Res. 2008;6(10):1649–1656. doi: 10.1158/1541-7786.MCR-07-2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.An S, Zheng Y, Bleu T. Sphingosine 1-phosphate-induced cell proliferation, survival, and related signaling events mediated by G protein-coupled receptors Edg3 and Edg5. J Biol Chem. 2000;275(1):288–296. doi: 10.1074/jbc.275.1.288. [DOI] [PubMed] [Google Scholar]
- 98.Young N, Van Brocklyn JR. Roles of sphingosine-1-phosphate (S1P) receptors in malignant behavior of glioma cells. Differential effects of S1P2 on cell migration and invasiveness. Exp Cell Res. 2007;313(8):1615–1627. doi: 10.1016/j.yexcr.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Patmanathan SN, et al. Aberrant expression of the S1P regulating enzymes, SPHK1 and SGPL1, contributes to a migratory phenotype in OSCC mediated through S1PR2. Sci Rep. 2016;6(1):1–13. doi: 10.1038/srep25650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ponnusamy S, et al. Communication between host organism and cancer cells is transduced by systemic sphingosine kinase 1/sphingosine 1-phosphate signalling to regulate tumour metastasis. EMBO Mol Med. 2012;4(8):761–775. doi: 10.1002/emmm.201200244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Matsushima-Nishiwaki R, et al. Sphingosine 1-phosphate (S1P) reduces hepatocyte growth factor-induced migration of hepatocellular carcinoma cells via S1P receptor 2. PLoS ONE. 2018;13(12):e0209050. doi: 10.1371/journal.pone.0209050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Du W, et al. S1P2, the G protein–coupled receptor for sphingosine-1-phosphate, negatively regulates tumor angiogenesis and tumor growth in vivo in mice. Can Res. 2010;70(2):772–781. doi: 10.1158/0008-5472.CAN-09-2722. [DOI] [PubMed] [Google Scholar]
- 103.Kim E-S, et al. Sphingosine 1-phosphate regulates matrix metalloproteinase-9 expression and breast cell invasion through S1P3–Gαq coupling. J Cell Sci. 2011;124(13):2220–2230. doi: 10.1242/jcs.076794. [DOI] [PubMed] [Google Scholar]
- 104.Lee HM, et al. Oncogenic S1P signalling in EBV-associated nasopharyngeal carcinoma activates AKT and promotes cell migration through S1P receptor 3. J Pathol. 2017;242(1):62–72. doi: 10.1002/path.4879. [DOI] [PubMed] [Google Scholar]
- 105.Huang H. Matrix metalloproteinase-9 (MMP-9) as a cancer biomarker and MMP-9 biosensors: recent advances. Sensors. 2018;18(10):3249. doi: 10.3390/s18103249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sukocheva OA, et al. Divergence of Intracellular trafficking of sphingosine kinase 1 and Sphingosine-1-phosphate receptor 3 in MCF-7 breast cancer cells and MCF-7-derived stem cell-enriched mammospheres. Int J Mol Sci. 2021;22(9):4314. doi: 10.3390/ijms22094314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang S, et al. Triple negative breast cancer depends on sphingosine kinase 1 (SphK1)/sphingosine-1-phosphate (S1P)/sphingosine 1-phosphate receptor 3 (S1PR3)/notch signaling for metastasis. Med Sci Monit Int Med J Exp Clin Res. 2018;24:1912. doi: 10.12659/MSM.905833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Nema R, et al. Emerging role of sphingosine-1-phosphate signaling in head and neck squamous cell carcinoma. Onco Targets Ther. 2016;9:3269. doi: 10.2147/OTT.S99989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hashemi Goradel N, et al. Nanoparticles as new tools for inhibition of cancer angiogenesis. J Cell Physiol. 2018;233(4):2902–2910. doi: 10.1002/jcp.26029. [DOI] [PubMed] [Google Scholar]
- 110.Goradel NH, Jahangiri S, Negahdari B. Effects of mesenchymal stem cell-derived exosomes on angiogenesis in regenerative medicine. Curr Regen Med Former Recent Pat on Regen Med. 2017;7(1):46–53. [Google Scholar]
- 111.Visentin B, et al. Validation of an anti-sphingosine-1-phosphate antibody as a potential therapeutic in reducing growth, invasion, and angiogenesis in multiple tumor lineages. Cancer Cell. 2006;9(3):225–238. doi: 10.1016/j.ccr.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 112.Zhang L, et al. Anti-S1P antibody as a novel therapeutic strategy for VEGFR TKI-resistant renal cancer. Clin Cancer Res. 2015;21(8):1925–1934. doi: 10.1158/1078-0432.CCR-14-2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Thuy AV, et al. Validation of a monoclonal antibody directed against the human sphingosine 1-phosphate receptor type 1. J Immunol Methods. 2021;490:112953. doi: 10.1016/j.jim.2020.112953. [DOI] [PubMed] [Google Scholar]
- 114.LaMontagne K, et al. Antagonism of sphingosine-1-phosphate receptors by FTY720 inhibits angiogenesis and tumor vascularization. Can Res. 2006;66(1):221–231. doi: 10.1158/0008-5472.CAN-05-2001. [DOI] [PubMed] [Google Scholar]
- 115.Chae S-S, et al. Requirement for sphingosine 1–phosphate receptor-1 in tumor angiogenesis demonstrated by in vivo RNA interference. J Clin Investig. 2004;114(8):1082–1089. doi: 10.1172/JCI200422716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ragunathrao VAB, et al. Sphingosine-1-phosphate receptor 1 activity promotes tumor growth by amplifying VEGF-VEGFR2 angiogenic signaling. Cell Rep. 2019;29(11):3472–3487.e4. doi: 10.1016/j.celrep.2019.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dai L, et al. Sphingosine kinase 1/sphingosine-1-phosphate (S1P)/S1P receptor axis is involved in ovarian cancer angiogenesis. Oncotarget. 2017;8(43):74947. doi: 10.18632/oncotarget.20471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gaengel K, et al. The sphingosine-1-phosphate receptor S1PR1 restricts sprouting angiogenesis by regulating the interplay between VE-cadherin and VEGFR2 in Angiogenesis. Dev Cell. 2013;23(6):1264. doi: 10.1016/j.devcel.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 119.Liu Y-N, et al. Sphingosine 1 phosphate receptor-1 (S1P1) promotes tumor-associated regulatory T cell expansion: leading to poor survival in bladder cancer. Cell Death Dis. 2019;10(2):1–11. doi: 10.1038/s41419-018-1298-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chakraborty P, et al. Pro-survival lipid sphingosine-1-phosphate metabolically programs T cells to limit anti-tumor activity. Cell Rep. 2019;28(7):1879–1893.e7. doi: 10.1016/j.celrep.2019.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Li Y, et al. The role of Mir-148a in cancer. J Cancer. 2016;7(10):1233. doi: 10.7150/jca.14616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Paczkowska J, et al. The tumor suppressive mir-148a Is epigenetically inactivated in classical Hodgkin lymphoma. Cells. 2020;9(10):2292. doi: 10.3390/cells9102292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shi H, et al. miR-148a suppresses cell invasion and migration in gastric cancer by targeting DNA methyltransferase 1. Oncol Lett. 2018;15(4):4944–4950. doi: 10.3892/ol.2018.7907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang SL, Liu L. microRNA-148a inhibits hepatocellular carcinoma cell invasion by targeting sphingosine-1-phosphate receptor 1. Exp Ther Med. 2015;9(2):579–584. doi: 10.3892/etm.2014.2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cai W, et al. MicroR-542-3p can mediate ILK and further inhibit cell proliferation, migration and invasion in osteosarcoma cells. Aging (Albany NY) 2019;11(1):18. doi: 10.18632/aging.101698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yuan L, et al. miR-542-3p inhibits colorectal cancer cell proliferation, migration and invasion by targeting OTUB1. Am J Cancer Res. 2017;7(1):159. [PMC free article] [PubMed] [Google Scholar]
- 127.Wu H, et al. miR-542-3p targets sphingosine-1-phosphate receptor 1 and regulates cell proliferation and invasion of breast cancer cells. Eur Rev Med Pharmacol Sci. 2017;21(1):108–114. [PubMed] [Google Scholar]
- 128.Yi F, et al. Overexpression of microRNA-506-3p aggravates the injury of vascular endothelial cells in patients with hypertension by downregulating Beclin1 expression. Exp Ther Med. 2018;15(3):2844–2850. doi: 10.3892/etm.2018.5733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Li J, et al. The emerging role of miR-506 in cancer. Oncotarget. 2016;7(38):62778. doi: 10.18632/oncotarget.11294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lin Y, et al. MiR-506 targets UHRF1 to inhibit colorectal cancer proliferation and invasion via the KISS1/PI3K/NF-κB signaling axis. Front Cell Dev Biol. 2019;7:266. doi: 10.3389/fcell.2019.00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yin M, et al. Selective killing of lung cancer cells by miRNA-506 molecule through inhibiting NF-κB p65 to evoke reactive oxygen species generation and p53 activation. Oncogene. 2015;34(6):691–703. doi: 10.1038/onc.2013.597. [DOI] [PubMed] [Google Scholar]
- 132.Yang D, et al. Integrated analyses identify a master microRNA regulatory network for the mesenchymal subtype in serous ovarian cancer. Cancer Cell. 2013;23(2):186–199. doi: 10.1016/j.ccr.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang Z, et al. MiR-506 suppresses tumor proliferation and invasion by targeting FOXQ1 in nasopharyngeal carcinoma. PLoS ONE. 2015;10(4):e0122851. doi: 10.1371/journal.pone.0122851. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 134.Lu Z, et al. MiR-506 suppresses liver cancer angiogenesis through targeting sphingosine kinase 1 (SPHK1) mRNA. Biochem Biophys Res Commun. 2015;468(1–2):8–13. doi: 10.1016/j.bbrc.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 135.Li J, et al. Downregulated miR-506 expression facilitates pancreatic cancer progression and chemoresistance via SPHK1/Akt/NF-κB signaling. Oncogene. 2016;35(42):5501–5514. doi: 10.1038/onc.2016.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wang C-Z, et al. MiR-101: a potential therapeutic target of cancers. Am J Transl Res. 2018;10(11):3310. [PMC free article] [PubMed] [Google Scholar]
- 137.Wang J, et al. MicroRNA-101 inhibits growth, proliferation and migration and induces apoptosis of breast cancer cells by targeting sex-determining region Y-Box 2. Cell Physiol Biochem. 2017;43(2):717–732. doi: 10.1159/000481445. [DOI] [PubMed] [Google Scholar]
- 138.Chen L-G, Xia Y-J, Cui Y. Upregulation of miR-101 enhances the cytotoxic effect of anticancer drugs through inhibition of colon cancer cell proliferation. Oncol Rep. 2017;38(1):100–108. doi: 10.3892/or.2017.5666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Le Han WC, et al. MiR-101 inhibits the proliferation and metastasis of lung cancer by targeting zinc finger E-box binding homeobox 1. Am J Transl Res. 2018;10(4):1172. [PMC free article] [PubMed] [Google Scholar]
- 140.Chen M-B, et al. MicroRNA-101 down-regulates sphingosine kinase 1 in colorectal cancer cells. Biochem Biophys Res Commun. 2015;463(4):954–960. doi: 10.1016/j.bbrc.2015.06.041. [DOI] [PubMed] [Google Scholar]
- 141.Tsai CH, et al. Sphingosine-1-phosphate suppresses chondrosarcoma metastasis by upregulation of tissue inhibitor of metalloproteinase 3 through suppressing miR-101 expression. Mol Oncol. 2017;11(10):1380–1398. doi: 10.1002/1878-0261.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chen X, et al. Oncogenic miR-9 is a target of erlotinib in NSCLCs. Sci Rep. 2015;5(1):1–11. doi: 10.1038/srep17031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chen X, et al. MiR-9 promotes tumorigenesis and angiogenesis and is activated by MYC and OCT4 in human glioma. J Exp Clin Cancer Res. 2019;38(1):1–16. doi: 10.1186/s13046-020-01803-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.He L, et al. miR-9 functions as a tumor inhibitor of cell proliferation in epithelial ovarian cancer through targeting the SDF-1/CXCR4 pathway. Exp Ther Med. 2017;13(4):1203–1208. doi: 10.3892/etm.2017.4118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Pan Q, et al. MicroRNA-9 enhanced cisplatin sensitivity in nonsmall cell lung cancer cells by regulating eukaryotic translation initiation factor 5A2. BioMed Res Int. 2018;2018:1–8. doi: 10.1155/2018/1769040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Yao X, Xie L, Zeng Y. MiR-9 promotes angiogenesis via targeting on sphingosine-1-phosphate receptor 1. Front Cell Dev Biol. 2020 doi: 10.3389/fcell.2020.00755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gacem RB, et al. Methylation of miR-124a-1, miR-124a-2, and miR-124a-3 genes correlates with aggressive and advanced breast cancer disease. Tumor Biol. 2014;35(5):4047–4056. doi: 10.1007/s13277-013-1530-4. [DOI] [PubMed] [Google Scholar]
- 148.Xie X-Q, et al. miR-124 intensified oxaliplatin-based chemotherapy by targeting CAPN2 in colorectal cancer. Mol Ther Oncolytics. 2020;17:320–331. doi: 10.1016/j.omto.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Xia J, et al. miR-124 inhibits cell proliferation in gastric cancer through down-regulation of SPHK1. J Pathol. 2012;227(4):470–480. doi: 10.1002/path.4030. [DOI] [PubMed] [Google Scholar]
- 150.Cai QQ, et al. MiR-124 inhibits the migration and invasion of human hepatocellular carcinoma cells by suppressing integrin αV expression. Sci Rep. 2017;7(1):1–10. doi: 10.1038/s41598-016-0028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Stupack DG. The biology of integrins. Oncology (Williston Park) 2007;21(9 Suppl 3):6–12. [PubMed] [Google Scholar]
- 152.Kechagia JZ, Ivaska J, Roca-Cusachs P. Integrins as biomechanical sensors of the microenvironment. Nat Rev Mol Cell Biol. 2019;20(8):457–473. doi: 10.1038/s41580-019-0134-2. [DOI] [PubMed] [Google Scholar]
- 153.Zhou Y, et al. MicroRNA-124 upregulation inhibits proliferation and invasion of osteosarcoma cells by targeting sphingosine kinase 1. Hum Cell. 2017;30(1):30–40. doi: 10.1007/s13577-016-0148-4. [DOI] [PubMed] [Google Scholar]
- 154.Gao M, et al. Reduction of COX-2 through modulating miR-124/SPHK1 axis contributes to the antimetastatic effect of alpinumisoflavone in melanoma. Am J Transl Res. 2017;9(3):986. [PMC free article] [PubMed] [Google Scholar]
- 155.Zhao Y, et al. MiR-124 acts as a tumor suppressor by inhibiting the expression of sphingosine kinase 1 and its downstream signaling in head and neck squamous cell carcinoma. Oncotarget. 2017;8(15):25005. doi: 10.18632/oncotarget.15334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhang Y, et al. Exosomal transfer of miR-124 inhibits normal fibroblasts to cancer-associated fibroblasts transition by targeting sphingosine kinase 1 in ovarian cancer. J Cell Biochem. 2019;120(8):13187–13201. doi: 10.1002/jcb.28593. [DOI] [PubMed] [Google Scholar]
- 157.Banzhaf-Strathmann J, Edbauer D. Good guy or bad guy: the opposing roles of microRNA 125b in cancer. Cell Commun Signal. 2014;12(1):1–13. doi: 10.1186/1478-811X-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Bai S, et al. MicroRNA-125b promotes tumor growth and suppresses apoptosis by targeting DRAM2 in retinoblastoma. Eye. 2016;30(12):1630–1638. doi: 10.1038/eye.2016.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zhang H, et al. Upregulation of microRNA-125b contributes to leukemogenesis and increases drug resistance in pediatric acute promyelocytic leukemia. Mol Cancer. 2011;10(1):1–13. doi: 10.1186/1476-4598-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hu G, et al. miR-125b regulates the drug-resistance of breast cancer cells to doxorubicin by targeting HAX-1. Oncol Lett. 2018;15(2):1621–1629. doi: 10.3892/ol.2017.7476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ying X, et al. MicroRNA-125b suppresses ovarian cancer progression via suppression of the epithelial-mesenchymal transition pathway by targeting the SET protein. Cell Physiol Biochem. 2016;39(2):501–510. doi: 10.1159/000445642. [DOI] [PubMed] [Google Scholar]
- 162.Bu Q, et al. MiR-125b inhibits anaplastic thyroid cancer cell migration and invasion by targeting PIK3CD. Biomed Pharmacother. 2017;88:443–448. doi: 10.1016/j.biopha.2016.11.090. [DOI] [PubMed] [Google Scholar]
- 163.Zhao X, et al. MiRNA-125b inhibits proliferation and migration by targeting SphK1 in bladder cancer. Am J Transl Res. 2015;7(11):2346. [PMC free article] [PubMed] [Google Scholar]
- 164.Zhang X, et al. MiR-125b-1-3p exerts antitumor functions in lung carcinoma cells by targeting S1PR1. Chin Med J. 2018;131(16):1909. doi: 10.4103/0366-6999.238135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Li M, et al. miR-128 and its target genes in tumorigenesis and metastasis. Exp Cell Res. 2013;319(20):3059–3064. doi: 10.1016/j.yexcr.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 166.Hu J, et al. microRNA-128 plays a critical role in human non-small cell lung cancer tumourigenesis, angiogenesis and lymphangiogenesis by directly targeting vascular endothelial growth factor-C. Eur J Cancer. 2014;50(13):2336–2350. doi: 10.1016/j.ejca.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 167.Cao X-Z, Bin H, Zang Z-N. MiR-128 suppresses the growth of thyroid carcinoma by negatively regulating SPHK1. Biomed Pharmacother. 2019;109:1960–1966. doi: 10.1016/j.biopha.2018.08.052. [DOI] [PubMed] [Google Scholar]
- 168.Mei J, et al. MicroRNA-613: a novel tumor suppressor in human cancers. Biomed Pharmacother. 2020;123:109799. doi: 10.1016/j.biopha.2019.109799. [DOI] [PubMed] [Google Scholar]
- 169.Sang Q, Liu X, Sun D. Role of miR-613 as a tumor suppressor in glioma cells by targeting SOX9. Onco Targets Ther. 2018;11:2429. doi: 10.2147/OTT.S156608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Zhu J, et al. Myocardial reparative functions of exosomes from mesenchymal stem cells are enhanced by hypoxia treatment of the cells via transferring microRNA-210 in an nSMase2-dependent way. Artif Cells Nanomed Biotechnol. 2018;46(8):1659–1670. doi: 10.1080/21691401.2017.1388249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Liu C, Jiang Y, Han B. miR-613 suppresses chemoresistance and stemness in triple-negative breast cancer by targeting FAM83A. Cancer Manage Res. 2020;12:12623. doi: 10.2147/CMAR.S276316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Yu H, et al. miR-613 inhibits bladder cancer proliferation and migration through targeting SphK1. Am J Transl Res. 2017;9(3):1213. [PMC free article] [PubMed] [Google Scholar]
- 173.Qiu W, et al. MicroRNA-613 inhibits cell growth, migration and invasion of papillary thyroid carcinoma by regulating SphK2. Oncotarget. 2016;7(26):39907. doi: 10.18632/oncotarget.9530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhang X, et al. MiR-515-5p acts as a tumor suppressor via targeting TRIP13 in prostate cancer. Int J Biol Macromol. 2019;129:227–232. doi: 10.1016/j.ijbiomac.2019.01.127. [DOI] [PubMed] [Google Scholar]
- 175.Pinho FG, et al. Downregulation of microRNA-515-5p by the estrogen receptor modulates sphingosine kinase 1 and breast cancer cell proliferation. Can Res. 2013;73(19):5936–5948. doi: 10.1158/0008-5472.CAN-13-0158. [DOI] [PubMed] [Google Scholar]
- 176.Lee K-H, et al. MicroRNA-330 acts as tumor suppressor and induces apoptosis of prostate cancer cells through E2F1-mediated suppression of Akt phosphorylation. Oncogene. 2009;28(38):3360–3370. doi: 10.1038/onc.2009.192. [DOI] [PubMed] [Google Scholar]
- 177.Cheng Y, Zhu H, Gao W. MicroRNA-330–3p represses the proliferation and invasion of laryngeal squamous cell carcinoma through downregulation of Tra2β-mediated Akt signaling. Mol Cell Probes. 2020;52:101574. doi: 10.1016/j.mcp.2020.101574. [DOI] [PubMed] [Google Scholar]
- 178.Wang H, et al. MiR-330-3p functions as a tumor suppressor that regulates glioma cell proliferation and migration by targeting CELF1. Arch Med Sci AMS. 2020;16(5):1166. doi: 10.5114/aoms.2020.95027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Shen L, et al. miR-330-3p promotes lung cancer cells invasion, migration, and metastasis by directly targeting hSOD2b. Biotechnol Appl Biochem. 2019;66(1):21–32. doi: 10.1002/bab.1691. [DOI] [PubMed] [Google Scholar]
- 180.Meng H, et al. MicroRNA-330-3p functions as an oncogene in human esophageal cancer by targeting programmed cell death 4. Am J Cancer Res. 2015;5(3):1062. [PMC free article] [PubMed] [Google Scholar]
- 181.Wang Z, et al. Up-regulation and tumor-promoting role of SPHK1 were attenuated by miR-330-3p in gastric cancer. IUBMB Life. 2018;70(11):1164–1176. doi: 10.1002/iub.1934. [DOI] [PubMed] [Google Scholar]
- 182.Imbert C, et al. Resistance of melanoma to immune checkpoint inhibitors is overcome by targeting the sphingosine kinase-1. Nat Commun. 2020;11(1):1–14. doi: 10.1038/s41467-019-14218-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Gachechiladze M, et al. Sphingosine kinase-1 predicts overall survival outcomes in non-small cell lung cancer patients treated with carboplatin and navelbine. Oncol Lett. 2019;18(2):1259–1266. doi: 10.3892/ol.2019.10447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Li J, et al. Upregulation of sphingosine kinase 1 is associated with recurrence and poor prognosis in papillary thyroid carcinoma. Oncol Lett. 2019;18(5):5374–5382. doi: 10.3892/ol.2019.10910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Gao Z, et al. Possible tumor suppressive role of the miR-144/451 cluster in esophageal carcinoma as determined by principal component regression analysis. Mol Med Rep. 2016;14(4):3805–3813. doi: 10.3892/mmr.2016.5691. [DOI] [PubMed] [Google Scholar]
- 186.Liu C, et al. MiR-144-3p promotes the tumor growth and metastasis of papillary thyroid carcinoma by targeting paired box gene 8. Cancer Cell Int. 2018;18(1):1–13. doi: 10.1186/s12935-016-0378-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Xiao W, et al. Mir-144-3p promotes cell proliferation, metastasis, sunitinib resistance in clear cell renal cell carcinoma by downregulating ARID1A. Cell Physiol Biochem. 2017;43(6):2420–2433. doi: 10.1159/000484395. [DOI] [PubMed] [Google Scholar]
- 188.Zhang S-Y, et al. miR-144-3p, a tumor suppressive microRNA targeting ETS-1 in laryngeal squamous cell carcinoma. Oncotarget. 2016;7(10):11637. doi: 10.18632/oncotarget.7025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Li B, et al. MicroRNA-144-3p suppresses gastric cancer progression by inhibiting epithelial-to-mesenchymal transition through targeting PBX3. Biochem Biophys Res Commun. 2017;484(2):241–247. doi: 10.1016/j.bbrc.2017.01.084. [DOI] [PubMed] [Google Scholar]
- 190.Liang W, et al. Comprehensive gene and microRNA expression profiling reveals a role for miRNAs in the oncogenic roles of SphK1 in papillary thyroid cancer. J Cancer Res Clin Oncol. 2017;143(4):601–611. doi: 10.1007/s00432-016-2315-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Li D, et al. miR-133b, a particular member of myomiRs, coming into playing its unique pathological role in human cancer. Oncotarget. 2017;8(30):50193. doi: 10.18632/oncotarget.16745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Wang Q-Y, et al. MiR-133b targets Sox9 to control pathogenesis and metastasis of breast cancer. Cell Death Dis. 2018;9(7):1–14. doi: 10.1038/s41419-018-0715-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Qin W, et al. MicroRNA-133b is a key promoter of cervical carcinoma development through the activation of the ERK and AKT1 pathways. Oncogene. 2012;31(36):4067–4075. doi: 10.1038/onc.2011.561. [DOI] [PubMed] [Google Scholar]
- 194.Cheng N, Wang GH. miR-133b, a microRNA targeting S1PR1, suppresses nasopharyngeal carcinoma cell proliferation. Exp Ther Med. 2016;11(4):1469–1474. doi: 10.3892/etm.2016.3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Liu Z, et al. MiR-659-3p regulates the progression of chronic myeloid leukemia by targeting SPHK1. Int J Clin Exp Pathol. 2018;11(5):2470. [PMC free article] [PubMed] [Google Scholar]
- 196.Li S, et al. miR-659-3p is involved in the regulation of the chemotherapy response of colorectal cancer via modulating the expression of SPHK1. Am J Cancer Res. 2016;6(9):1976. [PMC free article] [PubMed] [Google Scholar]
- 197.Huang X, et al. miRNA-95 mediates radioresistance in tumors by targeting the sphingolipid phosphatase SGPP1. Can Res. 2013;73(23):6972–6986. doi: 10.1158/0008-5472.CAN-13-1657. [DOI] [PubMed] [Google Scholar]
- 198.Zhang G, et al. MicroRNA-338-3p suppresses cell proliferation and induces apoptosis of non-small-cell lung cancer by targeting sphingosine kinase 2. Cancer Cell Int. 2017;17(1):1–10. doi: 10.1186/1475-2867-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Bao Y, et al. Tumor suppressor microRNA-27a in colorectal carcinogenesis and progression by targeting SGPP1 and Smad2. PLoS ONE. 2014;9(8):e105991. doi: 10.1371/journal.pone.0105991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Ruoming W, et al. Tumor suppressor microRNA-31 inhibits gastric carcinogenesis by targeting Smad4 and SGPP2. Cancer Gene Ther. 2015;22(12):564–572. doi: 10.1038/cgt.2015.41. [DOI] [PubMed] [Google Scholar]
- 201.Zhao S, Li J. Sphingosine-1-phosphate induces the migration of thyroid follicular carcinoma cells through the microRNA-17/PTK6/ERK1/2 pathway. PLoS ONE. 2015;10(3):e0119148. doi: 10.1371/journal.pone.0119148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zhou P, et al. MicroRNA-363-mediated downregulation of S1PR1 suppresses the proliferation of hepatocellular carcinoma cells. Cell Signal. 2014;26(6):1347–1354. doi: 10.1016/j.cellsig.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 203.Pi J, et al. A MicroRNA302-367-Erk1/2-Klf2-S1pr1 pathway prevents tumor growth via restricting angiogenesis and improving vascular stability. Circ Res. 2017;120(1):85–98. doi: 10.1161/CIRCRESAHA.116.309757. [DOI] [PubMed] [Google Scholar]
- 204.Bonauer A, et al. MicroRNA-92a controls angiogenesis and functional recovery of ischemic tissues in mice. Science. 2009;324(5935):1710–1713. doi: 10.1126/science.1174381. [DOI] [PubMed] [Google Scholar]
- 205.Zhang H, et al. MiR-124 inhibits the migration and invasion of ovarian cancer cells by targeting SphK1. J Ovar Res. 2013;6(1):1–9. doi: 10.1186/1757-2215-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Lu Z, et al. Long non-coding RNA HULC promotes tumor angiogenesis in liver cancer by up-regulating sphingosine kinase 1 (SPHK1) Oncotarget. 2016;7(1):241. doi: 10.18632/oncotarget.6280. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.