Key Points
Question
What is the availability of medications for opioid use disorder (MOUD) for pregnant people in US jails?
Findings
In this cross-sectional study of 836 survey respondents from jails across the US, respondents at 60% of jails reported continuing to provide MOUD to pregnant individuals who were receiving medication before incarceration, but only 32% of jails initiated MOUD during pregnancy. Most medication-providing jails discontinued MOUD during the postpartum period.
Meaning
This study found that US jails did not consistently provide pregnant people with access to medications that meet the standard of care for treatment of opioid use disorder, which suggests that there is an opportunity for intervention to improve care for pregnant people who are incarcerated.
Abstract
Importance
Thousands of pregnant people with opioid use disorder (OUD) enter US jails annually, yet their access to medications for OUD (MOUD) that meet the standard of care (methadone and/or buprenorphine) is unknown.
Objective
To assess the availability of MOUD for the treatment of pregnant individuals with OUD in US jails.
Design, Setting, and Participants
In this cross-sectional study, electronic and paper surveys were sent to all 2885 identifiable US jails verified in the National Jails Compendium between August 19 and November 7, 2019. Respondents were medical and custody leaders within the jails.
Main Outcomes and Measures
The primary outcome was the availability of MOUD (methadone and/or buprenorphine) for the treatment of pregnant people with OUD in US jails. Availability of MOUD was assessed based on (1) continuation of MOUD for pregnant incarcerated individuals (if the individual was receiving MOUD before incarceration), with or without initiation of MOUD; (2) both initiation and continuation of MOUD for pregnant individuals; (3) only continuation of MOUD for pregnant individuals; and (4) management of opioid withdrawal for pregnant individuals. Secondary outcomes included MOUD availability during the postpartum period and logistical factors associated with the provision of MOUD. Multivariate logistic regression analysis was used to assess factors associated with MOUD availability during pregnancy.
Results
Among 2885 total surveys sent, 1139 (39.5%) were returned; of those, 836 surveys (73.4%; 29.0% of all surveys sent) could be analyzed, with similar proportions from metropolitan (399 jails [47.7%]) and rural (381 jails [45.6%]) settings. Overall, 504 jails (60.3%) reported that MOUD was available for medication continuation, with or without medication initiation, during pregnancy. Of those, 267 jails (53.0%; 31.9% of surveys included in the analysis) both initiated and continued MOUD, and 237 jails (47.0%; 28.3% of surveys included in the analysis) only continued MOUD; 190 of 577 jails (32.9%; 22.7% of surveys included in the analysis) reported opioid withdrawal as the only management for pregnant people with OUD. Among the 504 medication-providing jails, only 120 (23.8%) continued to provide MOUD during the postpartum period. Methadone was more commonly available at jails that only continued MOUD (84 of 123 jails [68.3%]), whereas buprenorphine was more commonly available at jails that both initiated and continued MOUD (73 of 119 jails [61.3%]). In an adjusted model, jails with higher odds of MOUD availability were located in the Northeast (odds ratio [OR], 10.72; 95% CI, 2.43-47.36) or metropolitan areas (OR, 1.92; 95% CI, 1.31-2.83), had private health care contracts (OR, 1.49; 95% CI, 1.03-2.14) and a higher number of women (≥70) reported in the female census (OR, 1.69; 95% CI, 1.02-2.80), and provided pregnancy testing within 2 weeks of arrival at the jail (OR, 2.66; 95% CI, 1.69-4.17).
Conclusions and Relevance
In this cross-sectional study, a substantial proportion of US jails did not provide access to MOUD to pregnant people with OUD. Although most jails reported continuing to provide MOUD to individuals who were receiving medication before incarceration, few jails initiated MOUD, and most medication-providing jails discontinued MOUD during the postpartum period. These results suggest that many pregnant and postpartum people with OUD in US jails do not receive medication that is the standard of care and are required to endure opioid withdrawal, signaling an opportunity for intervention to improve care for pregnant people who are incarcerated.
This cross-sectional study uses verified data from the National Jail Compendium to assess the availability of medication for the treatment of opioid use disorder among pregnant individuals incarcerated in US jails.
Introduction
Incarcerated individuals and institutions of incarceration in the US have experienced and played a role in the broad-reaching and fatal consequences of the opioid epidemic. The burden of opioid use disorder (OUD) is high among people in jail, with one-quarter to one-third of the 2 million people with OUD cycling in and out of jails each year.1,2 Compared with the general population, incarcerated people with OUD are more than 100 times more likely to die of opioid overdoses when they return to their communities, in part because of reduced opioid tolerance associated with untreated OUD while in custody.3,4,5 Despite increasing recognition of the important role of carceral facilities in providing medications for OUD (MOUD) to incarcerated individuals, little research has addressed the needs of pregnant people with OUD in jails.
It has been estimated that among the nearly 55 000 admissions of pregnant people to jails each year, approximately 7700 individuals (14%) have OUD.6,7 Rates of OUD during pregnancy quadrupled in the US between 1999 and 2016, with fatal consequences; by 2016, 10% of deaths among pregnant and postpartum individuals were associated with opioid use.8,9,10,11 This problem impacts not only pregnant individuals but their children, families, and communities. Pregnant people with substance use disorders are often criminalized rather than given access to treatment.12 They encounter intersecting forms of discrimination and stigma from being incarcerated, pregnant, and using drugs. Structural racism undergirds the marginalization of pregnant people who use drugs, with policies that disproportionately penalize pregnant Black individuals and mandate separation from their children.12,13,14,15
The well-established standard of care for OUD during pregnancy is MOUD consisting of methadone or buprenorphine.16 Maternal and fetal benefits include increases in adherence to addiction treatment, prenatal care, and in-hospital delivery and decreases in the risk of overdose death, HIV, hepatitis, preterm birth, and infants with low birth weight.17,18,19,20 Medically supervised opioid withdrawal is not recommended during pregnancy and has been associated with return to opioid use, producing fetal and maternal risks.18 One study19 found that incarceration during pregnancy or the postpartum period was associated with 4 times greater odds of postpartum overdose, whereas receiving MOUD during pregnancy was protective. For pregnant people in jail, the potential benefit of providing MOUD is substantial, combining the established benefits of medication both during pregnancy and while in custody. Provision of MOUD to people in custody has been associated with reductions in fatal and nonfatal overdoses, decreases in involuntary opioid withdrawal, improvements in engagement with addiction treatment, reductions in reincarceration rates, and increases in employment rates.21,22,23,24,25,26,27,28
Amid national calls to expand access to MOUD in carceral settings, little is known about the availability of these medications in jails.29 One reason for this gap is the large number of jails in the US for which no publicly available database exists. Jails differ from prisons on many levels, including the fact that most people in jails, which are locally administered, have pretrial status and will return to their communities after a short stay. This fluidity between jails and the community highlights the importance of MOUD availability in jails as a point along the cascade of care.30 We conducted the first study, to our knowledge, to use verified data from the National Jails Compendium.31 The study involved a national cross-sectional survey of all identifiable jails in the US to assess practices regarding MOUD and opioid withdrawal among pregnant people at those facilities.
Methods
Participants
We administered a cross-sectional survey between August 19 and November 7, 2019, to medical and custody leaders at all 2885 US jails verified by the National Jails Compendium,31 the first known database containing information on the contact persons and mailing addresses of all known US jails. We specified that the survey should be completed by someone knowledgeable about the jail’s MOUD services. The Johns Hopkins School of Medicine Institutional Review Board approved the study, with respondents' completion of the survey serving as their informed consent to participate in the study. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.32
Survey Instrument and Outcomes
Our primary outcome was the availability of MOUD at jails (termed MOUD-available jails). We first identified whether MOUD (methadone and/or buprenorphine) was available to pregnant individuals for continuation of medication (if the individual was receiving MOUD before incarceration), with or without initiation of medication, among the 836 jails included in the analysis. We then subdivided MOUD-available jails into those that both initiated and continued MOUD and those that only continued but did not initiate MOUD. Jails reporting that they provided only naltrexone during pregnancy were not classified as MOUD-available jails because the use of naltrexone is generally not recommended during pregnancy.16 The survey was adapted from a previous study on prison access to MOUD during pregnancy7 and consisted of 49 items pertaining to methadone and/or buprenorphine for the treatment of pregnant people with OUD, opioid withdrawal practices during pregnancy, MOUD dosing arrangements, and access to MOUD in the postpartum period. Other characteristics included health care delivery arrangements, pregnancy testing practices, the position and/or title of the person completing the survey, and the number of women and pregnant people at the facilities based on a female census item included in the survey (with June 30, 2019, as the date of census).
Recruitment and Survey Distribution
The National Sheriff’s Association endorsed our study, and we promoted this support in recruitment materials. We first sent electronic surveys to those with an email address (2039 jails [70.7%]) using REDCap (Johns Hopkins University), a secure web-based platform (Figure).33 We then mailed surveys via US Postal Service to those without an email address and those who did not respond to the online survey after 2 reminders. Recruitment strategies have been published elsewhere.31 Jails were considered nonrespondents if their surveys were not received by March 31, 2020.
Figure. Recruitment, Response, and Surveys That Could Be Analyzed Among All Known US Jails.
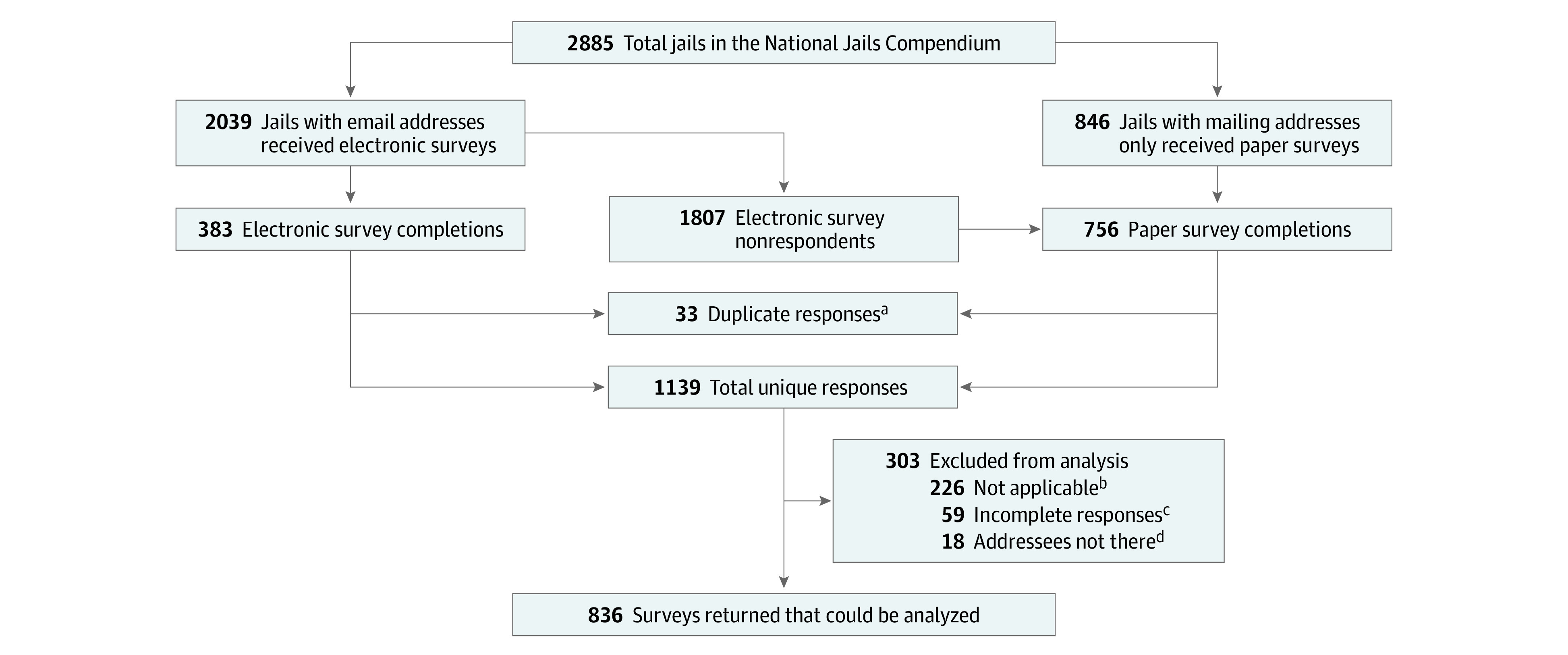
aTrue duplicate responses were defined as more than 1 response (complete or partially complete) from the same address.
bRespondents indicated the survey was not appropriate for their jail setting. Sample reasons included short-term holding facility, no jail at the location, no women (and/or pregnant individuals) housed at the jail, and all detainees were sent to another jail.
cSurveys that included no information about the primary outcome.
dIndividuals who responded to the survey by communicating that the person to whom the survey was addressed was not at that location.
Data Management
Electronic surveys were completed by respondents using REDCap, and paper surveys sent by respondents were manually entered into REDCap by study team members. Surveys were excluded from the analyses if they were duplicates (ie, more than 1 response [complete or partially complete] from the same address), were from a jail setting that was not applicable for this study (ie, jails that did not house pregnant people), or were incomplete (ie, included no information associated with the study’s primary outcome) (Figure).
We encountered discrepancies in some participants’ responses to survey items pertaining to our main outcome, MOUD availability; these discrepancies were mainly found in paper surveys. For instance, some respondents reported that they did not offer methadone during pregnancy but then provided details on how they administered methadone. Therefore, we developed an algorithm to adjudicate discrepancies. If a respondent provided credible responses regarding how methadone or buprenorphine was administered, the facility was considered an MOUD-available jail. Discrepancies that could not, after review by 3 raters (C.S., C.T.K., and C.L.), clarify MOUD availability were categorized as MOUD-uncertain jails and were not included in the primary analysis of MOUD-available jails. Surveys from respondents at MOUD-uncertain jails generally consisted of those reporting that MOUD was available during pregnancy without subsequent valid responses regarding how MOUD was provided. We then conducted 2 sensitivity analyses, one in which MOUD-uncertain jails were reclassified as MOUD-available jails and another that classified MOUD-uncertain jails as withdrawal only. We did not apply the adjudication process to opioid withdrawal responses and reported opioid withdrawal as those who selected withdrawal on the survey.
Statistical Analysis
We analyzed outcomes and important variables using descriptive statistics and applying Pearson χ2 or Wilcoxon rank sum tests. Observations with missing outcomes were excluded from denominators for proportion calculations. We used zip codes to categorize jail locations as metropolitan or rural.34 We used respondents’ reported positions and/or titles to categorize them as having vs not having decision-making capacity and as having custody vs medical roles. Univariate logistic regression models were used to identify jail characteristics and practices of MOUD-available jails. Significant factors were included in a multivariate model. Multivariate models were repeated for the provision of both methadone and buprenorphine. Before conducting multivariate modeling, we confirmed that survey type (paper vs online) was not significantly associated with main outcomes. All analyses were performed using SAS software, version 9.4.(SAS Institute Inc), and the significance threshold was 2-sided P < .05.
Results
Of 2885 surveys sent, we received 1139 unique responses (383 electronic and 756 paper), representing a response rate of 39.5% (Figure). A total of 836 surveys (29.0% of all surveys sent and 73.4% of survey responses) could be analyzed. Overall, 1048 of 1746 nonrespondents (60.0%) were from rural counties, with a greater proportion from the South and Midwest regions; 586 nonrespondents (33.6%) had a physical address only. The 836 respondents with surveys that could be analyzed were from jails representing a broad geographic range, with similar distribution of metropolitan (399 jails [47.7%]) and rural (381 jails [45.6%]) settings (Table 1). Most respondents who provided information about their position or title had a custody role (654 of 820 respondents [79.8%]) or a decision-making role (509 of 820 respondents [62.1%]). Few jails (259 of 836 [31.0%]) conducted routine pregnancy testing at intake or within 2 weeks of arrival. The most common health care delivery arrangement was through contracts with private correctional health care companies (384 of 836 jails [45.9%]). The 1-day median count of pregnant people across all included jails on June 30, 2019, was 1506 (range, 0-65 people per facility), or 3.0% of all women (N = 50 248) in study jails.
Table 1. Characteristics of Respondents and Jails.
| Characteristic | No. /total No. (%) |
|---|---|
| Total respondents, No. | 836 |
| Region | |
| West | 169/836 (20.2) |
| Midwest | 282/836 (33.7) |
| South | 314/836 (37.6) |
| Northeast | 71/836 (8.5) |
| Geographic classificationa | |
| Metropolitan | 399/836 (47.7) |
| Rural | 381/836 (45.6) |
| Role of survey respondent | |
| Custody | 654/820 (79.8) |
| Health care | 166/820 (20.2) |
| Decision-making | 509/820 (62.1) |
| Non–decision-making | 311/820 (37.9) |
| Women reported at female census on June 30, 2019, median (IQR)b | 29 (10-69.5) |
| Pregnant women reported on June 30, 2019, median (IQR) | 1 (0-2) |
| Pregnancy testing policies | |
| No testing performed under any circumstances | 46/836 (5.5) |
| All individuals tested at intake | 193/836 (23.1) |
| All individuals tested within 2 weeks of arrival but not at intake | 66/836 (7.9) |
| Individuals tested only at practitioner or individual request | 524/829 (63.2) |
| Routine prenatal care service delivery | |
| On-site care from a health care professional (physician, certified nurse-midwife, nurse practitioner, or physician assistant) | 345/816 (42.3) |
| Off-site care only | 422/816 (51.7) |
| Other care only | 49/816 (6.0) |
| Health care service deliveryc | |
| Contract with private correctional health care companyd | 384/836 (45.9) |
| Public agency | 108/836 (12.9) |
| University health care center contract | 24/836 (2.9) |
| Individual health care professional | 127/836 (15.2) |
| Direct through jail | 147/836 (17.6) |
| Community health care professional, clinic, hospital, or community nonprofit organization | 227/836 (27.2) |
| Othere | 75/836 (9.0) |
Geographic classification was based on zip code and National Center for Health Statistics urban and rural county categories criteria.34 Metropolitan includes large metropolitan urban, large metropolitan suburban, and medium to small metropolitan areas. A total of 56 respondents (6.7%) had a missing zip code.
Online responses had a greater median female census than paper responses (32.5 vs 25.0; P = .04).
Categories were not mutually exclusive; therefore, percentages total greater than 100%.
Privately contracted health care was reported less frequently among online responses than paper responses (151 vs. 233; P = .01).
Health care services delivery arrangements with other organizations or health care professionals were more common among paper responses than they were among online responses (64 vs 11; P < .001).
Overall, among 836 jails included in the analysis, 504 (60.3%) met our criteria for having a high certainty of continuing MOUD during pregnancy (Table 2). A total of 267 jails (31.9% of all jails included in the analysis and 53.0% of MOUD-available jails) both initiated and continued MOUD, and 237 jails (28.3% of all jails included in the analysis and 47.0% of MOUD-available jails) continued but did not initiate MOUD during pregnancy. Among all 836 jails, 190 (22.7%) reported managing OUD only through opioid withdrawal. An additional 142 jails (17.0%) reported that MOUD was available during pregnancy, but details were missing or contradictory (MOUD-uncertain jails).
Table 2. Availability of Medication for the Treatment of Opioid Use Disorder Among Pregnant Individuals in US Jails.
| MOUD availability | Jails, No./total No. (%) |
|---|---|
| During pregnancy | |
| MOUD availablea | 504/836 (60.3) |
| Continuation only | 237/504 (47.0) |
| Initiation and continuation | 267/504 (53.0) |
| Methadone available | 385/504 (76.4) |
| Continuation only | 247/385 (64.2) |
| Initiation and continuation | 137/385 (35.6) |
| Buprenorphine available | 381/504 (75.6) |
| Continuation only | 171/381 (44.9) |
| Initiation and continuation | 210/381 (55.1) |
| Methadone only available | 123/504 (24.4) |
| Continuation only | 84/123 (68.3) |
| Initiation and continuation | 39/123 (31.7) |
| Buprenorphine only available | 119/504 (23.6) |
| Continuation only | 46/119 (38.7) |
| Initiation and continuation | 73/119 (61.3) |
| Both methadone and buprenorphine available | 262/504 (52.0) |
| Continuation only | 107/262 (40.8) |
| Initiation and continuation | 152/262 (58.0) |
| Withdrawal only (no MOUD available)b | 190/577 (32.9) |
| Withdrawal and MOUD availablec | 387/577 (67.1) |
| During postpartum period | |
| MOUD available for continuationd | 120/504 (23.8) |
| No MOUD continuation | 274/504 (54.4) |
| Discontinuation with tapering | 165/274 (60.2) |
| Abrupt discontinuation | 61/274 (22.3) |
| Conditional discontinuatione | 47/274 (17.2) |
| Did not report | 110/504 (21.8) |
Abbreviation: MOUD, medication for opioid use disorder.
Data do not include jails for which the provision of MOUD was uncertain.
There was a higher likelihood of doing withdrawal only among paper responses than among online responses (126 vs. 64; P = .01).
There was a higher likelihood of doing withdrawal and MOUD among paper responses than among online responses (267 vs. 120; P = .03).
Among jails providing MOUD during pregnancy.
Some respondents stated that they did not routinely continue providing MOUD after pregnancy but would consider allowing it depending on the remaining time in an individual’s jail sentence or whether an individual was expressing breast milk.
Jails that only provided methadone were more likely to continue medication only (84 of 123 jails [68.3%]) than to initiate and continue medication (39 of 123 jails [31.7%]). In contrast, jails that only provided buprenorphine were more likely to initiate and continue medication (73 of 119 jails [61.3%]) than to continue medication only (46 of 119 jails [38.7%]) (Table 2). A total of 262 jails (52.0% of MOUD-available jails) provided access to both methadone and buprenorphine, and 76 jails (15.1% of MOUD-available jails) routinely switched from 1 medication to the other when providing MOUD to pregnant individuals. Although naltrexone is not recommended during pregnancy,16 141 jails (28.0% of MOUD-available jails) reported providing naltrexone to pregnant individuals.
In the first sensitivity analysis, when MOUD-uncertain jails were classified as MOUD-available jails, the overall proportion of facilities providing MOUD increased from 504 of 836 (60.3%) to 646 of 836 (77.3%; P < .001). In the second sensitivity analysis, when MOUD-uncertain jails were classified as jails managing OUD only through opioid withdrawal, the overall proportion of jails managing OUD only through withdrawal increased from 131 of 577 (22.7%) to 229 of 577 (39.7%; P < .001). Although only 14 of 141 respondents (9.9%) at MOUD-uncertain jails had a medical role, 124 of 494 respondents (25.1%) at MOUD-available jails had a medical role (P < .001). A similar proportion of respondents at MOUD-available and MOUD-uncertain jails had decision-making roles (315 of 494 respondents [63.8%] and 89 of 141 respondents [63.1%], respectively; P = .24). Respondents at several jails wrote in their own responses, reporting that they managed OUD during pregnancy by releasing people from jail (8 respondents) or transferring them to another jail or prison at which they could have access to medications (12 respondents).
Few of the 504 MOUD-available jails continued MOUD during the postpartum period (120 jails [23.8%]) (Table 2). Among 274 MOUD-available jails (54.4%) that discontinued MOUD after pregnancy, discontinuation practices ranged from abrupt cessation (61 jails [22.3%]) to tapering (165 jails [60.2%]) of medication. Some respondents reported that continuation of MOUD during the postpartum period was conditional (47 jails [17.2%]) based on whether the person had a short interval until expected jail release (or transfer to another facility) or whether the person was breastfeeding or expressing breast milk.
The most common dispensing arrangement among 386 jails providing methadone was picking up or sending medication to the jail for administration by jail staff (205 jails [53.1%]) followed by transporting the pregnant person off site to receive medication (199 jails [51.6%]) (Table 3). Of 386 jails providing buprenorphine, most (262 jails [67.9%]) dispensed medication on site, with fewer (96 jails [24.9%]) transporting the pregnant person off site to receive medication. Among 577 jails reporting information on opioid withdrawal during pregnancy, most withdrawals occurred on site (472 jails [81.8%]). Although most jails (437 [75.7%]) provided medications for symptom relief during withdrawal, 28 jails (4.9%) did not. A total of 114 jails (19.8%) used opioids other than methadone or buprenorphine for withdrawal management.
Table 3. Medication for Opioid Use Disorder, Logistical Details of Medication Provision, and Opioid Withdrawal Arrangements Among US Jails Providing Medication for the Treatment of Pregnant Individuals With Opioid Use Disorder.
| Arrangement | Jails, No. (%) | |||
|---|---|---|---|---|
| Type of MOUD | Opioid withdrawal | |||
| Methadone | Buprenorphine | Reported that opioid withdrawal was used for pregnant people | Did not provide information about opioid withdrawal practices for pregnant people | |
| MOUD provision | ||||
| Total jails, No. | 137 | 210 | NA | NA |
| Location of treatment initiationa,b | ||||
| Jail | 47 (34.3) | 145 (69.0) | NA | NA |
| Hospital | 31 (22.6) | 51 (24.3) | ||
| Other community site | 72 (52.6) | 45 (21.4) | ||
| Other | 74 (54.0) | 49 (23.3) | ||
| Logistical details of MOUD provision a , c | ||||
| Total jails, No. | 386 | 386 | NA | NA |
| On-site dispensing (certified OTP or buprenorphine treatment professional with waiver) | 15 (3.9) | 262 (67.9) | NA | NA |
| Transportation to community site for dosing | 199 (51.6) | 96 (24.9) | ||
| Medication brought to jail by OTP staff | 63 (16.3) | 53 (13.7) | ||
| Medication picked up or sent to jail for jail staff to administer | 205 (53.1) | 17 (4.4) | ||
| Other | 50 (13.0) | 51 (13.2) | ||
| Opioid withdrawal | ||||
| Total jails, No. | NA | NA | 577 | 259d |
| Location of withdrawala | ||||
| Jail | NA | NA | 472 (81.8) | NA |
| Hospital | 136 (23.6) | NA | ||
| Transfer to another jail or release from custody | 20 (3.5) | NA | ||
| Othere | 49 (8.5) | NA | ||
| Withdrawal practices during pregnancy | ||||
| Abrupt withdrawal only | NA | NA | 28 (4.9) | NA |
| Withdrawal with medication supporta | 437 (75.7) | NA | ||
| Withdrawal with nonopioid medications for symptoms | 303 (52.5) | NA | ||
| Withdrawal with opioids not used as MOUDf | 114 (19.8) | NA | ||
| Withdrawal with methadone or buprenorphine for symptoms only | 131 (22.7) | NA | ||
| Not reported | 112 (19.4) | NA | ||
Abbreviations: MOUD, medication for opioid use disorder; NA, not applicable; OTP, opioid treatment professional.
Categories are not mutually exclusive; therefore, percentages do not total 100%.
Initiation site is only reported for jails that initiated treatment with methadone and/or buprenorphine.
Logistical details apply to initiation and/or continuation of MOUD, whichever the jail had available. The jails were not asked about logistical details for continuation or initiation of MOUD separately.
Includes 142 jails for which the provision of MOUD was uncertain because they did not provide information about opioid withdrawal.
One statistically significant difference between paper and online responses was found, with more paper responses selecting the other category.
Includes acetaminophen with codeine and acetaminophen with hydrocodone (eg, Norco and Vicodin).
We used logistic regression analysis to identify jail characteristics associated with MOUD availability during pregnancy (Table 4). In the unadjusted multivariate model, facilities with higher odds of providing MOUD during pregnancy were located in the Northeast (odds ratio [OR], 5.66; 95% CI, 2.31-13.85; P < .001) or metropolitan settings (OR, 2.89; 95% CI, 2.15-3.89; P < .001), had a higher number of women (≥70) reported in the female census (OR, 3.42; 95% CI, 2.33-5.03; P < .001), provided routine pregnancy testing within 2 weeks of arrival (OR, 4.27; 95% CI, 3.00-6.09; P < .001), and used private health care contractors for care delivery (OR, 2.07; 95% CI, 1.56-2.76; P < .001). Jails with lower odds of providing MOUD during pregnancy were located in the South (OR, 0.66; 95% CI, 0.44-0.97; P < .001) and comprised survey respondents who were employed in a custody role (OR, 0.44; 95% CI, 0.30-0.65; P < .001).
Table 4. Factors Associated With Availability of Medication for the Treatment of Opioid Use Disorder During Pregnancy in US Jails.
| Factor | OR (95% CI) | P value |
|---|---|---|
| Unadjusted model of factors associated with provision of MOUD | ||
| Census region | ||
| Midwest vs West | 0.62 (0.42-0.92) | <.001 |
| Northeast vs West | 5.66 (2.31-13.85) | |
| South vs West | 0.66 (0.44-0.97) | |
| Geographic classification | ||
| Metropolitan vs rural | 2.89 (2.15-3.89) | <.001 |
| Health care service delivery | ||
| Private vs not private | 2.07 (1.56-2.76) | <.001 |
| Role of survey respondent | ||
| Custody vs health care | 0.44 (0.30-0.65) | <.001 |
| Decision-making vs non–decision-making | 1.20 (0.90-1.60) | .22 |
| Female census ≥70 vs <70 womena | 3.42 (2.33-5.03) | <.001 |
| Pregnancy test within 2 wk of arrival (yes vs no) | 4.27 (3.00-6.09) | <.001 |
| On-site vs off-site prenatal care | 1.51 (1.12-2.04) | .007 |
| Adjusted model of factors associated with provision of MOUDb | ||
| Census region | ||
| Midwest vs West | 0.62 (0.38-1.02) | <.001 |
| Northeast vs West | 10.72 (2.43-47.36) | |
| South vs West | 0.54 (0.33-0.89) | |
| Geographic classification | ||
| Metropolitan vs rural | 1.92 (1.31-2.83) | <.001 |
| Health care service delivery | ||
| Private vs not private | 1.49 (1.03-2.14) | .03 |
| Role of survey respondent | ||
| Custody vs health care | 0.54 (0.33-0.87) | .011 |
| Female census ≥70 vs <70 womena | 1.69 (1.02-2.80) | .04 |
| Pregnancy testing within 2 wk of arrival (yes vs no) | 2.66 (1.69-4.17) | <.001 |
| On-site vs off-site prenatal care | 1.03 (0.72-1.48) | .87 |
| Adjusted model of factors associated with provision of both methadone and buprenorphine | ||
| Census region | ||
| Midwest vs West | 0.86 (0.48-1.51) | .09 |
| Northeast vs West | 1.57 (0.76-3.22) | |
| South vs West | 0.68 (0.40-1.16) | |
| Geographic classification | ||
| Metropolitan vs rural | 2.01 (1.23-3.20) | .004 |
| Role of survey respondent | ||
| Custody vs medical | 0.90 (0.56-1.43) | .64 |
| Health care service delivery | ||
| Private vs not private | 1.31 (0.87-1.98) | .19 |
| Female census ≥70 vs <70 womena | 0.93 (0.56-1.54) | .79 |
| Pregnancy testing within 2 wk of arrival (yes vs no) | 0.76 (0.49-1.12) | .24 |
| On-site vs off-site prenatal care | 1.03 (0.68-1.57) | .89 |
Abbreviations: MOUD; medication for opioid use disorder; OR, odds ratio.
The cutoff for small vs large jails was set at 70 women based on the IQR of the female census counts reported by respondents.
The sensitivity analysis using the model in which MOUD-uncertain jails were categorized as MOUD-available jails revealed that only the South had lower odds of providing MOUD (OR, 0.45; 95% CI, 0.26-0.82) vs the West, and jails that performed routine pregnancy testing within 2 weeks of arrival had higher odds of providing MOUD (OR, 2.54; 95% CI, 1.58-4.26) vs those that did not.
When we adjusted the multivariate model to categorize MOUD-uncertain jails as MOUD-available jails, facilities with routine pregnancy testing within 2 weeks of arrival (OR, 2.66; 95% CI, 1.69-4.17; P < .001), facilities located in the Northeast (OR, 10.72; 95% CI, 2.43-47.36; P < .001) or metropolitan areas (OR, 1.92; 95% CI, 1.31-2.83; P < .001), and facilities that had private health care contracts (OR, 1.49; 95% CI, 1.03-2.14; P = .03) and a greater number of women recorded in the female census (OR, 1.69; 95% CI, 1.02-2.80; P = .04) continued to have higher odds of providing MOUD, and facilities located in the South (OR, 0.54; 95% CI, 033-0.89; P < .001) continued to have lower odds of providing MOUD. In the second adjusted multivariate model including jails with both methadone and buprenorphine available, only those located in a metropolitan setting had higher odds of providing MOUD (OR, 2.01; 95% CI, 1.23-3.20; P = .004) (Table 4).
Discussion
This cross-sectional study is, to our knowledge, the largest study to date of US jails using verified data from the National Jails Compendium.31 The study found that a substantial proportion of jails did not provide access to MOUD, which is the standard of care, to pregnant people with OUD. Overall, 39.7% of jails did not allow continuation of MOUD during pregnancy, and only 31.9% permitted initiation of MOUD during pregnancy. This finding suggests that thousands of pregnant people entering jails are likely required to endure opioid withdrawal each year.7 Withdrawal is not only a difficult experience, especially when in custody, but it is also accompanied by short- and long-term risks for both pregnant people and their fetuses, including increased risk of overdose combined with higher risk of overdose at jail release and greater risk of suicide.4,18,19,21,35,36 In addition, allowing a pregnant person to experience opioid withdrawal during pregnancy increases the need for staff to respond to medical issues resulting from withdrawal. However, 60.3% of jails provided continuation of MOUD during pregnancy, suggesting that implementation of MOUD is feasible across a range of jail sizes and locations.
Providing methadone to individuals in custody requires complex logistical arrangements because a jail has to either have a licensed opioid treatment program or devise arrangements with a community organization to transport individuals or medications, often on a daily basis. Treatment with buprenorphine, in contrast, requires only a practitioner with an X waiver to prescribe.37 In our study, methadone and buprenorphine were similarly available overall, but jails that only provided continuation of MOUD were more likely to do so using methadone only; jails that initiated and continued MOUD were more likely to provide buprenorphine than methadone. This difference may reflect the different logistical issues associated with medication administration. If a jail employs a buprenorphine prescriber who has a waiver, it can easily initiate and continue MOUD on site. If a jail only provides access to methadone, it is likely to do so only for people who were receiving MOUD before incarceration.
The standard of care for pregnant people with OUD is access to both methadone and buprenorphine and the ability to choose (with practitioner guidance) the medication that works best. However, only 152 jails (18.2% of all jails included in the analysis and 30.2% of MOUD-available jails) provided access to initiation and continuation of MOUD with both medications. It is concerning that 54.4% of MOUD-available jails discontinued MOUD during the postpartum period. This practice implies that the benefit of MOUD is solely for the fetus, overlooks the importance of the mother’s long-term well-being for herself and her infant, and does not reflect standard practices for chronic disease management of OUD. Furthermore, postpartum cessation of MOUD is known to increase the risk of fatal and nonfatal overdose.8,9,19
The provision of MOUD during pregnancy was less common in smaller rural jails and jails not located in the Northeast, which is consistent with patterns in the national availability of MOUD.38,39,40 Jails without routine pregnancy testing were also less likely to provide MOUD, reflecting an absence of standardized pregnancy care. Jails with routine pregnancy testing may also be more attentive to the distinct needs of this population. Jails that had privately contracted health care were more likely to provide MOUD, which may reflect the contractors’ awareness of national guidelines and their desire to reduce medicolegal risks. Compared with a national survey of 245 jails conducted 20 years ago,41 in which 15% of jails continued providing methadone during pregnancy, there has been modest improvement.
Previous survey studies of prisons29,42 found that most prisons providing MOUD do so exclusively during pregnancy, although details on initiation or continuation of MOUD were not reported; these studies29,42 may have cultivated a misperception that pregnant people in custody have greater access to MOUD than nonpregnant individuals.43 A more recent (2020) study7 of 22 state prison systems and 6 jails found that, although most systems continued providing MOUD to individuals who were receiving medication before incarceration, only 4 prison systems would initiate MOUD during pregnancy; likewise, of 6 jails in that study, only 2 initiated MOUD. The fact that few prisons initiate MOUD during pregnancy highlights the importance across the incarceration spectrum of jails providing MOUD. Because most prisons only continue but do not initiate MOUD,7 it is important that pregnant individuals receive these medications while in jail and before arrival at prison.
The high proportion of jails that did not provide MOUD during pregnancy in our study was similar to the proportion found in a survey study of 53 jails,44 in which at least 46% of jails reported opioid withdrawal, not access to MOUD, as their means of managing OUD among pregnant individuals. In addition, among 179 pregnant people with OUD in the North Carolina prison system, which includes pretrial detention, almost one-half of individuals endured opioid withdrawal.45
The lack of required health care standards and oversight in carceral facilities, despite a constitutional requirement to provide health care, has produced substantial variability in available health care services,46,47 which is consistent with our findings of variable access to MOUD during pregnancy. Furthermore, with more than 3000 jails in the US, most of which are under local jurisdiction, some jail leaders may not have the resources to obtain information or enact standards of care. Lawsuits have established that nonprovision of MOUD violates the Americans with Disabilities Act along with other legal precedents and that carceral facilities must make MOUD available48; nonetheless, practice lags behind legal and ethical standards.21
Jails are short-stay facilities in which people are temporarily detained after arrest; thus, they are largely responsible for the immediate management of treatment for people with OUD within the incarceration system. Jails have direct continuity with the community because people frequently come and go. Whether pregnant people receive MOUD or experience opioid withdrawal while in jail has direct implications for their well-being and survival in both the facility and the community.
Thus, providing MOUD to pregnant people in jails is an important strategy for optimizing maternal and infant health. Moreover, given racial and ethnic disparities in incarceration rates, providing MOUD during pregnancy to those in custody is also important for addressing racial and ethnic inequities in maternal health. Providing links to care via established partnerships with community organizations and health care professionals is equally important. Continuation of MOUD requires communication between the jail and the community organization or health care professional at jail entry, and continuing MOUD after leaving jail requires early and active planning to ensure continuity of medications. Increased resources, practice changes, standardization and oversight, and links to care are necessary for jails to provide access to MOUD during pregnancy. Such actions are needed to improve pregnancy outcomes, mitigate the intergenerational harms of the opioid epidemic, and address maternal health inequities.
Limitations
This study has several limitations. These include the representativeness of the sample. Although the 39.5% response rate may appear low, it is substantially higher than the 14% response rate reported from a phone survey of 384 jails.44 Potential reasons for nonresponses from jail personnel could include apprehension or disinterest in participating in research studies and thinking such research would not be useful to them.31 Notably, nonresponses reveal the challenges of conducting jail-based research that could prevent progress in this area. Most nonrespondents were from rural counties and the South and Midwest regions of the US; based on respondents’ answers, provision of MOUD was lower among jails in the South and Midwest, suggesting that response bias likely overestimates the proportion of jails offering MOUD during pregnancy.
We did not assess the ways in which jails consider individual preferences for medication, and we did not ask about screening practices for OUD. The fact that we could not be certain about MOUD availability for 17.0% of responses highlights the difficulties of ascertaining consistent information about health care services among jails. Findings from the sensitivity analysis suggested that MOUD-uncertain jails were different from jails in which MOUD ascertainment was certain, which supported our strict adjudication process for discrepancies. Future research could investigate which individuals actually received counseling and which individuals wanted and received MOUD during pregnancy. Researchers could also interview administrators, especially those at jails with few resources, about the challenges of providing care for this population and interview pregnant people with OUD who are incarcerated.
Conclusions
This cross-sectional study found that a substantial proportion of US jails did not provide access to MOUD to pregnant and postpartum individuals. Although respondents at most jails reported that they continued to provide MOUD to pregnant individuals who were receiving medication before incarceration, few jails initiated MOUD, and most medication-providing jails discontinued MOUD during the postpartum period. These results suggest that many pregnant and postpartum individuals with OUD in US jails do not receive MOUD that meets the standard of care and are often required to endure opioid withdrawal, signaling an opportunity for intervention to improve care for pregnant individuals who are incarcerated.
References
- 1.Bronson J, Stroop J, Zimmer S, Berzofsky M. Drug use, dependence, and abuse among state prisoners and jail inmates, 2007-2009. Bureau of Justice Statistics, US Department of Justice; 2017. Updated August 10, 2020. Accessed October 5, 2021. https://bjs.ojp.gov/content/pub/pdf/dudaspji0709.pdf
- 2.Substance Abuse and Mental Health Services Administration . Results from the 2012 National Survey on Drug Use and Health: summary of national findings. Substance Abuse and Mental Health Services Administration, US Dept of Health and Human Services; September 2013. Accessed October 5, 2021. http://store.samhsa.gov/product/Results-from-the-2012-National-Survey-on-Drug-Use-and-Health-NSDUH-/SMA13-4795
- 3.Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592-600. doi: 10.7326/0003-4819-159-9-201311050-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merrall ELC, Kariminia A, Binswanger IA, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545-1554. doi: 10.1111/j.1360-0443.2010.02990.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mancher M, Leshner AI, eds. National Academies of Sciences, Engineering, and Medicine. Medications for Opioid Use Disorder Save Lives. National Academies Press; 2019. [PubMed] [Google Scholar]
- 6.Sufrin C, Jones RK, Mosher WD, Beal L. Pregnancy prevalence and outcomes in U.S. jails. Obstet Gynecol. 2020;135(5):1177-1183. doi: 10.1097/AOG.0000000000003834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sufrin C, Sutherland L, Beal L, Terplan M, Latkin C, Clarke JG. Opioid use disorder incidence and treatment among incarcerated pregnant women in the United States: results from a national surveillance study. Addiction. 2020;115(11):2057-2065. doi: 10.1111/add.15030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metz TD, Rovner P, Hoffman MC, Allshouse AA, Beckwith KM, Binswanger IA. Maternal deaths from suicide and overdose in Colorado, 2004-2012. Obstet Gynecol. 2016;128(6):1233-1240. doi: 10.1097/AOG.0000000000001695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiff DM, Nielsen T, Terplan M, et al. Fatal and nonfatal overdose among pregnant and postpartum women in Massachusetts. Obstet Gynecol. 2018;132(2):466-474. doi: 10.1097/AOG.0000000000002734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization—United States, 1999-2014. MMWR Morb Mortal Wkly Rep. 2018;67(31):845-849. doi: 10.15585/mmwr.mm6731a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gemmill A, Kiang MV, Alexander MJ. Trends in pregnancy-associated mortality involving opioids in the United States, 2007-2016. Am J Obstet Gynecol. 2019;220(1):115-116. doi: 10.1016/j.ajog.2018.09.028 [DOI] [PubMed] [Google Scholar]
- 12.Terplan M. Women and the opioid crisis: historical context and public health solutions. Fertil Steril. 2017;108(2):195-199. doi: 10.1016/j.fertnstert.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 13.Goodwin M. Policing the Womb: Invisible Women and the Criminalization of Motherhood. Cambridge University Press; 2020. [Google Scholar]
- 14.Bridges KM. Race, pregnancy, and the opioid epidemic: White privilege and the criminalization of opioid use during pregnancy. Harv Law Rev. 2020;133(33):770-851. [Google Scholar]
- 15.Terplan M. Can perinatal quality collaboratives address racial (in)justice? Am J Public Health. 2020;110(12):1728-1729. doi: 10.2105/AJPH.2020.305982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Obstetricians and Gynecologists . Opioid use and opioid use disorder in pregnancy. American College of Obstetricians and Gynecologists; August 2017. Committee opinion 711. Accessed October 5, 2021. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2017/08/opioid-use-and-opioid-use-disorder-in-pregnancy
- 17.Klaman SL, Isaacs K, Leopold A, et al. Treating women who are pregnant and parenting for opioid use disorder and the concurrent care of their infants and children: literature review to support national guidance. J Addict Med. 2017;11(3):178-190. doi: 10.1097/ADM.0000000000000308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Terplan M, Laird HJ, Hand DJ, et al. Opioid detoxification during pregnancy: a systematic review. Obstet Gynecol. 2018;131(5):803-814. doi: 10.1097/AOG.0000000000002562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nielsen T, Bernson D, Terplan M, et al. Maternal and infant characteristics associated with maternal opioid overdose in the year following delivery. Addiction. 2020;115(2):291-301. doi: 10.1111/add.14825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krans EE, Kim JY, Chen Q, et al. Outcomes associated with the use of medications for opioid use disorder during pregnancy. Addiction. 2021;116(12):3504-3514. doi: 10.1111/add.15582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milloy MJ, Wood E. Withdrawal from methadone in US prisons: cruel and unusual? Lancet. 2015;386(9991):316-318. doi: 10.1016/S0140-6736(15)60073-3 [DOI] [PubMed] [Google Scholar]
- 22.Rich JD, McKenzie M, Larney S, et al. Methadone continuation versus forced withdrawal on incarceration in a combined US prison and jail: a randomised, open-label trial. Lancet. 2015;386(9991):350-359. doi: 10.1016/S0140-6736(14)62338-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Green TC, Clarke J, Brinkley-Rubinstein L, et al. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry. 2018;75(4):405-407. doi: 10.1001/jamapsychiatry.2017.4614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fiscella K, Wakeman SE, Beletsky L. Implementing opioid agonist treatment in correctional facilities. JAMA Intern Med. 2018;178(9):1153-1154. doi: 10.1001/jamainternmed.2018.3504 [DOI] [PubMed] [Google Scholar]
- 25.Moore KE, Oberleitner L, Smith KMZ, Maurer K, McKee SA. Feasibility and effectiveness of continuing methadone maintenance treatment during incarceration compared with forced withdrawal. J Addict Med. 2018;12(2):156-162. doi: 10.1097/ADM.0000000000000381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brinkley-Rubinstein L, McKenzie M, Macmadu A, et al. A randomized, open label trial of methadone continuation versus forced withdrawal in a combined US prison and jail: findings at 12 months post-release. Drug Alcohol Depend. 2018;184:57-63. doi: 10.1016/j.drugalcdep.2017.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Malta M, Varatharajan T, Russell C, Pang M, Bonato S, Fischer B. Opioid-related treatment, interventions, and outcomes among incarcerated persons: a systematic review. PLoS Med. 2019;16(12):e1003002. doi: 10.1371/journal.pmed.1003002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krawczyk N, Eisenberg M, Schneider KE, et al. Predictors of overdose death among high-risk emergency department patients with substance-related encounters: a data linkage cohort study. Ann Emerg Med. 2020;75(1):1-12. doi: 10.1016/j.annemergmed.2019.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey. Drug Alcohol Depend. 2009;105(1-2):83-88. doi: 10.1016/j.drugalcdep.2009.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scott CK, Dennis ML, Grella CE, Watson DP. Improving retention across the OUD service cascade upon reentry from jail using Recovery Management Checkups-Adaptive (RMC-A) experiment. J Subst Abuse Treat. 2021;128:108245. doi: 10.1016/j.jsat.2020.108245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foudray CMA, Kramer C, Rudes DS, Sufrin C, Burr E, Parayil T. The compendium of U.S. jails: creating and conducting research with the first comprehensive contact database of U.S. jails. Health Justice. 2021;9(1):12. doi: 10.1186/s40352-021-00137-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 33.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Center for Health Statistics . NCHS urban-rural classification scheme for counties. Centers for Disease Control and Prevention; 2017. Accessed May 13, 2021. https://www.cdc.gov/nchs/data_access/urban_rural.htm
- 35.Covington EC, Argoff CE, Ballantyne JC, et al. Ensuring patient protections when tapering opioids: consensus panel recommendations. Mayo Clin Proc. 2020;95(10):2155-2171. doi: 10.1016/j.mayocp.2020.04.025 [DOI] [PubMed] [Google Scholar]
- 36.Agnoli A, Xing G, Tancredi DJ, Magnan E, Jerant A, Fenton JJ. Association of dose tapering with overdose or mental health crisis among patients prescribed long-term opioids. JAMA. 2021;326(5):411-419. doi: 10.1001/jama.2021.11013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Department of Health and Human Services. Practice guidelines for the administration of buprenorphine for treating opioid use disorder. Fed Regist. Published online April 28, 2021. Accessed August 16, 2021. https://www.federalregister.gov/documents/2021/04/28/2021-08961/practice-guidelines-for-the-administration-of-buprenorphine-for-treating-opioid-use-disorder
- 38.Cummings JR, Wen H, Ko M, Druss BG. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71(2):190-196. doi: 10.1001/jamapsychiatry.2013.3575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patrick SW, Buntin MB, Martin PR, et al. Barriers to accessing treatment for pregnant women with opioid use disorder in Appalachian states. Subst Abus. 2019;40(3):356-362. doi: 10.1080/08897077.2018.1488336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Andrilla CHA, Patterson DG. Tracking the geographic distribution and growth of clinicians with a DEA waiver to prescribe buprenorphine to treat opioid use disorder. J Rural Health. Published online March 18, 2021. [DOI] [PubMed]
- 41.Fiscella K, Moore A, Engerman J, Meldrum S. Jail management of arrestees/inmates enrolled in community methadone maintenance programs. J Urban Health. 2004;81(4):645-654. doi: 10.1093/jurban/jth147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scott CK, Dennis ML, Grella CE, Mischel AF, Carnevale J. The impact of the opioid crisis on U.S. state prison systems. Health Justice. 2021;9(1):17. doi: 10.1186/s40352-021-00143-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grella CE, Ostile E, Scott CK, Dennis M, Carnavale J. A scoping review of barriers and facilitators to implementation of medications for treatment of opioid use disorder within the criminal justice system. Int J Drug Policy. 2020;81:102768. doi: 10.1016/j.drugpo.2020.102768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kelsey CM, Medel N, Mullins C, Dallaire D, Forestell C. An examination of care practices of pregnant women incarcerated in jail facilities in the United States. Matern Child Health J. 2017;21(6):1260-1266. doi: 10.1007/s10995-016-2224-5 [DOI] [PubMed] [Google Scholar]
- 45.Knittel AK, Zarnick S, Thorp JM Jr, Amos E, Jones HE. Medications for opioid use disorder in pregnancy in a state women’s prison facility. Drug Alcohol Depend. 2020;214:108159. doi: 10.1016/j.drugalcdep.2020.108159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rold WJ. Thirty years after Estelle v. Gamble: a legal retrospective. J Correct Health Care. 2008;14(1):11-20. doi: 10.1177/1078345807309616 [DOI] [Google Scholar]
- 47.Olson MG, Khatri UG, Winkelman TNA. Aligning correctional health standards with Medicaid-covered benefits. JAMA Health Forum. 2020;1(7):e200885-e200885. doi: 10.1001/jamahealthforum.2020.0885 [DOI] [PubMed] [Google Scholar]
- 48.Toyoshima T, McNiel DE, Schonfeld A, Binder R. The evolving medicolegal precedent for medications for opioid use disorder in U.S. jails and prisons. J Am Acad Psychiatry Law. 2021;49(4):545-552. [DOI] [PubMed] [Google Scholar]


