Abstract
The frequency of hand hygiene has increased due to the COVID-19 pandemic, but there is little evidence regarding the impact of water exposure and temperature on skin. The aim of this study is to evaluate the effect of water exposure and temperature on skin barrier function in healthy individuals. A prospective observational study was conducted. Temperature, pH, transepidermal water loss (TEWL), erythema and stratum corneum hydration (SCH) were measured objectively before and after hot- and cold-water exposure and TempTest® (Microcaya TempTest, Bilbao, Spain) contact. Fifty healthy volunteers were enrolled. Hot-water exposure increased TEWL (25.75 vs. 58.58 g·h−1·m−2), pH (6.33 vs. 6.65) and erythema (249.45 vs. 286.34 AU). Cold-water immersion increased TEWL (25.75 vs. 34.96 g·h−1·m−2) and pH (6.33 vs. 6.62). TEWL (7.99 vs. 9.98 g·h−1·m−2) and erythema (209.07 vs. 227.79 AU) increased after being in contact with the hot region (44 °C) of the TempTest. No significant differences were found after contact with the cold region (4 °C) of the TempTest. In conclusion, long and continuous water exposure damages skin barrier function, with hot water being even more harmful. It would be advisable to use cold or lukewarm water for handwashing and avoid hot water. Knowing the proper temperature for hand washing might be an important measure to prevent flares in patients with previous inflammatory skin diseases on their hands.
Keywords: dermatological diseases, homeostasis, skin barrier, temperature, water
1. Introduction
The skin is the largest organ in the human body and accomplishes regulatory and defensive functions that reside in the epidermis, mainly in the stratum corneum [1]. To evaluate the epidermal barrier, measurements of transepidermal water loss (TEWL) are usually performed [2]. A high TEWL is associated with a deficiency in the skin barrier [3]. Other parameters to assess epidermal function are the stratum corneum hydration (SCH), pH of the skin surface, temperature, erythema and melanin index [4]. These parameters can change depending on the anatomical location and can be affected by skin diseases such as psoriasis or atopic dermatitis [4]. Skin-related studies should not be based on a single parameter to cover all the functions of the epidermal barrier, as an integrated and multiparametric approach is needed to evaluate the properties of the skin barrier [5]. The epidermal barrier is necessary to maintain cutaneous homeostasis and protect the body against multiple external factors, such as environmental conditions, chemical stress and ultraviolet radiation [6].
Recently, the coronavirus 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has increased the frequency of hand hygiene in the overall population [7] as it is important to wash hands properly to avoid transmission of the virus [8]. However, frequent hand washing might also be challenging because hand hygiene products may damage skin [9]. Moreover, it has been noted that skin barrier dysfunction increases the expression of angiotensin-converting enzyme 2, the cell receptor for SARS-CoV-2, in the basal layer of the epidermis which may increase the risk of being infected with this virus [10,11,12].
Several risk factors are associated with skin damage, such as having a previous history of atopic dermatitis or hand eczema, female sex and longer working hours [13], but there is little research on the effect of water exposure and temperature [14,15]. Hot environments increase sweat production, which leads to higher hydration, TEWL, sebum production and greasiness, and lower pH [16]. It has been shown that water temperature does not have an impact on microbe removal [14,17] while the American Contact Dermatitis Society recommends washing hands with cold or lukewarm water to avoid skin irritation [18].
As there is no solid evidence regarding the effect of water exposure and temperature on skin, the objective of this study is to evaluate the impact of water exposure and temperature on cutaneous homeostasis and skin barrier function.
2. Materials and Methods
2.1. Design
A prospective observational study was conducted.
2.2. Study Population
Participants were recruited from February to May 2021 at the Dermatology Department of the Hospital Universitario Virgen de las Nieves in Granada.
Inclusion criteria: Healthy subjects, aged between 18 and 65 years who signed the informed consent form.
Exclusion criteria: Subjects who did not sign the informed consent, subjects with an inflammatory skin disease (psoriasis, hidradenitis, atopic dermatitis) or another type of disease that may alter the epidermal barrier function and skin homeostasis; subjects receiving any topical, physical or systemic treatment which may alter the epidermal barrier function and skin homeostasis.
2.3. Study Variables Measurement
Sociodemographic variables (age and sex), smoking, skin care or use of body moisturizers were recorded by taking a clinical history. Biophysical parameters related to skin barrier function were measured by non-invasive tools. SCH was measured in Arbitrary Units (AU) using the Corneometer® (CM 825, Bilbao, Spain); TEWL in g·h−1·m−2 with the Tewameter® (TM 300, Bilbao, Spain); pH with the Skin-pH-Meter® (PH 905, Bilbao, Spain); erythema index in AU using the Mexameter® MX 18, and skin temperature in °C with the Skin-Thermometer ST 500; Bilbao, Spain. All these parameters were measured with the multi-probe adapter (MPA, Courage + Khazaka electronic GmbH, Bilbao, Spain). All measurements were taken in the same room at a mean room temperature of 23 ± 1 °C and ambient air humidity of 35% (range, 30–40%). All participants underwent an adaptation period of 20 min before the measurements were taken.
2.4. Water and Temperature Exposure
Skin barrier function parameters were measured at baseline on the right volar forearm and on both palms.
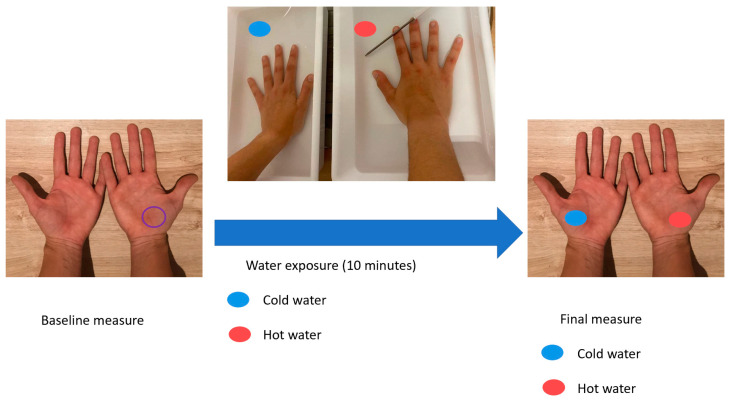
To evaluate the impact of water exposure on the epidermal barrier, participants immersed their right hand in hot water (41.29 (2.29 SD) °C) and their left hand in cold water (11.13 (2.71 SD) °C). They kept both hands submerged in 50 cm3 of water for 10 min. Skin barrier function parameters were measured again on both palms after this exposure (Figure 1).
Figure 1.
Flow chart of the measurements taken before and after water exposure.
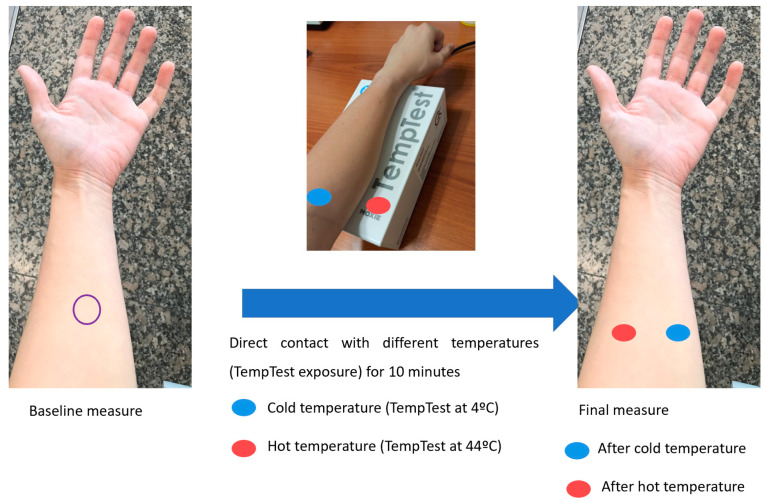
To evaluate changes after contact with different temperatures, patients placed their forearm for five minutes on the TempTest® (Microcaya TempTest, Bilbao, Spain) thermal element, which is used clinically to diagnose heat or cold contact urticaria [19,20]. The aluminium template of TempTest produces a temperature range continuously between 4 and 44 °C [21]. Skin barrier function parameters were measured at baseline and after the exposure on the regions of the volar forearm that were in contact with the aluminium template at 4 and at 44 °C (Figure 2).
Figure 2.
Flow chart of the measurements taken before and after direct contact with different temperatures (TempTest exposure).
The two exposures are not expected to interfere with each other. All participants immersed their hand in water first, whereas the volar forearm was not wet after water exposure, and there was an adaptation period of 20 min between the last measure on the palms and the baseline measure on the volar forearm.
2.5. Statistical Analysis
First, a descriptive analysis was carried out. Quantitative variables were expressed as means (standard deviation, SD) and qualitative variables as absolute (relative) frequency distributions. The normality of the variables was checked using the Shapiro–Wilk test. To compare continuous variables between independent samples, the Student’s t-test for independent samples or Welch’s test were used according to the homogeneity of the variances, previously evaluated by Levene’s test. The Student’s t-test for paired samples was used to compare variables in the same individuals. Statistical significance was considered when p < 0.05 with two tails. Statistical analyses were performed using SPSS version 24.0 (SPSS Inc., Chicago, IL, USA).
2.6. Ethics
All participants were informed of the study’s objectives when they signed the informed consent form to participate. This study was approved by the Ethics Committee of Hospital Universitario Virgen de las Nieves in Granada. All measurements were non-invasive, and the confidentiality of participant data was strictly preserved.
3. Results
3.1. Participants’ Characteristics
The study included 50 healthy individuals (20 men and 30 women) with a mean age of 33.3 (12.94 SD) years old. The demographic characteristics of the participants are displayed (Table 1).
Table 1.
Descriptive characteristics of the sample.
| Sociodemographic Features | Study Population (N = 50) |
|---|---|
| Age (years) | 33.3 (12.94) |
| Gender | |
| Male | 20 (40%) |
| Female | 30 (60%) |
| Phototype | |
| I | 1 (2%) |
| II | 14 (28%) |
| III | 29 (58%) |
| IV | 5 (10%) |
| VI | 1 (2%) |
| Smoking habit (yes) | 4 (8%) |
| Cigarettes per day | 7.25 (3.78) |
| Residence | |
| City | 45 (90%) |
| Country | 5 (10%) |
| Regular moisturizing | 34 (68%) |
| Regular sunlight exposure | 4 (8%) |
| Sun protection | |
| Always | 21 (42%) |
| Sometimes | 20 (40%) |
| Never | 9 (18%) |
| Occupational category | |
| Doctors | 23 (46%) |
| Nurses | 18 (36%) |
| Miscellaneous | 9 (18%) |
Data is expressed as relative (absolute) frequencies and means (standard deviations).
3.2. Changes in Skin Barrier Function after Water Exposure
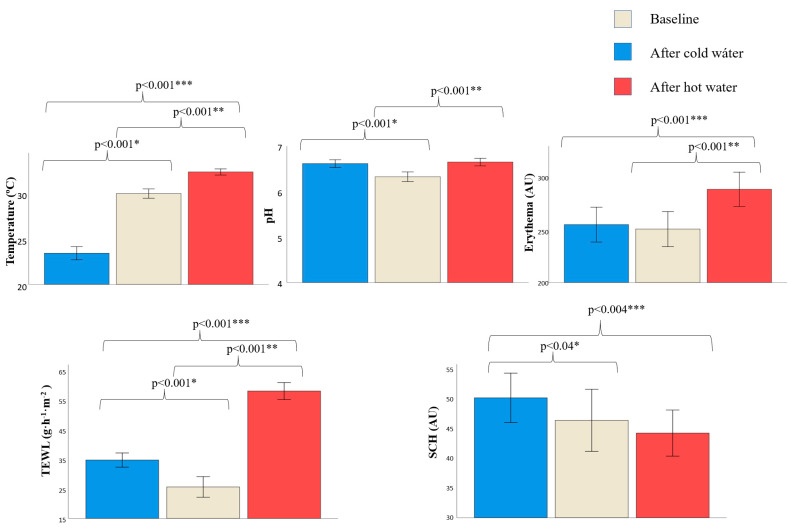
Differences in skin barrier parameters were found before and after water exposure (Figure 3, Table S1). Temperature, pH, TEWL and SCH changed after cold water exposure. Temperature decreased (30.18 vs. 23.49 °C, p < 0.001) while pH (6.33 vs. 6.62, p < 0.001), TEWL (25.75 vs. 34.96 g·h−1·m−2, p < 0.001) and SCH (46.69 vs. 50.55 AU, p = 0.04) increased. No differences were found in erythema.
Figure 3.
Skin barrier function parameters on the hands at baseline and after hot and cold-water exposure. Data is expressed as mean (standard deviations). AU, arbitrary units; SCH, stratum corneum hydration; TEWL, transepidermal water loss. * p-value after using Student’s t-test for paired samples to compare skin barrier function between baseline and after cold water exposure. ** p-value after using Student’s t-test for paired samples to compare skin barrier function between baseline and after hot water exposure. *** p-value after using Student’s t-test for paired samples to compare skin barrier function after cold and hot water exposure. Only significative p-values are shown (p < 0.05).
Temperature, pH, erythema and TEWL changed after hot water exposure. Temperature (30.18 vs. 32.60 °C, p < 0.001), pH (6.33 vs. 6.65, p < 0.001), TEWL (25.75 vs. 58.58 g·h−1·m−2, p < 0.001) and erythema (249.45 vs. 286.34 AU, p < 0.001) increased. No differences were found in SCH.
There were differences in temperature, erythema, TEWL and SCH between cold and hot water exposure. Temperature (23.49 vs. 32.60 °C, p < 0.001), TEWL (34.96 vs. 58.58 g·h−1·m−2, p < 0.001) and erythema values (253.63 vs. 286.34 AU, p < 0.001) were higher in hot water vs. cold water respectively, while SCH values (50.55 vs. 44.50 AU, p < 0.004) were lower. No differences were found in pH.
3.3. Changes in Skin Barrier Function after Direct Contact with Different Temperatures
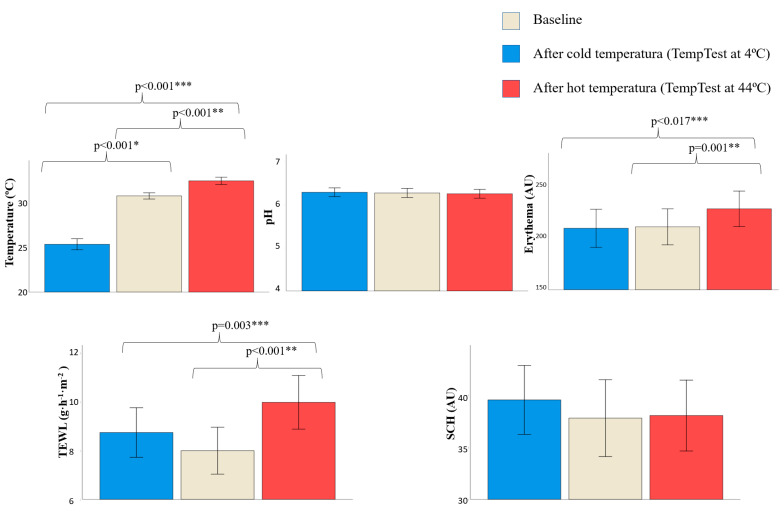
Skin barrier function parameters also changed after direct contact with different temperatures (TempTest exposure) (Figure 4, Table S2). Only temperature decreased after direct contact with cold temperature (exposure to TempTest at 4 °C) (30.76 vs. 25.35 °C, p < 0.001). No differences in pH, erythema, TEWL and SCH were found.
Figure 4.
Skin barrier function parameters on the volar forearm at baseline and after direct contact to different temperatures. Data is expressed as mean (standard deviations). AU, arbitrary units; SCH, stratum corneum hydration; TEWL, transepidermal water loss. * p-value after using Student’s t-test for paired samples to compare skin barrier function between baseline and contact with cold temperatura (TempTest at 4 °C). ** p-value after using Student’s t-test for paired samples to compare skin barrier function between baseline and after contact with hot temperature (TempTest at 44 °C). *** p-value after using Student’s t-test for paired samples to compare skin barrier function after contact with cold and hot temperature. Only significative p-values are shown (p < 0.05).
Temperature (30.76 vs. 32.45 °C, p < 0.001), TEWL (7.99 vs. 9.98 g·h−1·m−2, p < 0.001) and erythema (210.45 vs. 227.79 AU, p = 0.001) increased after direct contact with hot temperature (exposure to TempTest at 44 °C). No differences were found in pH or SCH.
There were differences between direct contact with cold and hot temperature. Temperature (25.35 vs. 32.45 °C, p < 0.001), TEWL (8.74 vs. 9.98 g·h−1·m−2, p = 0.003) and erythema values (209.07 vs. 227.79 AU, p = 0.017) were higher after contact with hot temperature vs. contact with cold temperature. No differences were found in pH or SCH.
3.4. Differences in Skin Barrier Changes between Sexes and Ages
Some differences were found in skin barrier changes between sexes (Table 2). The temperature decrease was higher in women than men (−7.29 vs−5.78, p = 0.02) after cold water. Erythema values on palm at baseline were higher in men (278.08 vs. 230.37 AU, p = 0.003) but changes were similar between sexes. SCH decreased in men while it increased in women after cold water (−1.96 vs. +7.74, p = 0.008). No differences were found in pH or TEWL.
Table 2.
Changes in skin barrier function after hot and cold and water exposure, stratified by sex.
| Men (n = 20) | Women (n = 30) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Water Exposure | |||||||||
| Basal | Change after Cold Water | Change after Hot Water | Basal | Change after Cold Water | Change after Hot Water | p B | p C | p H | |
| Temperature (°C) | 30.39 (2.04) |
−5.78 (0.51) |
+2.31 (0.30) |
+30.03 (1.71) |
−7.29 (0.37) |
+2.50 (0.26) |
0.523 | 0.020 | 0.647 |
| pH | 6.30 (0.43) |
+0.37 (0.37) |
+0.41 (0.10) |
+6.35 (0.34) |
+0.23 (0.06) |
0.26 (0.06) |
0.645 | 0.165 | 0.215 |
| Erythema (AU) | 278.08 (46.99) |
+10.27 (10.75) |
+31.14 (10.42) |
+230.37 (56.12) |
+0.12 (11.31) |
+40.71 (9.82) |
0.003 | 0.539 | 0.519 |
|
TEWL
(g·h−1·m−2) |
24.35 (10.88) |
+12.21 (2.45) |
+33.30 (2.36) |
26.68 (13.41) |
+7.21 (2.30) |
+32.51 (2.32) |
0.521 | 0.154 | 0.814 |
| SCH (AU) | 49.54 (16.51) |
−1.96 (2.51) |
−3.21 (2.69) |
44.80 (20.13) |
+7.74 (2.31) |
−1.50 (3.22) |
0.386 | 0.008 | 0.685 |
| TempTest Exposure | |||||||||
| Basal | Change after 4 °C TempTest | Change after 44 °C TempTest | Basal | Change after 4 °C TempTest | Change after 44 °C TempTest | p Bt | p Ct | p Ht | |
| Temperature (°C) | 31.20 (1.24) |
−5.96 (0.56) |
+1.58 (0.28) |
30.47 (1.16) |
−5.06 (0.34) |
+1.76 (0.23) |
0.038 | 0.178 | 0.624 |
| pH | 6.25 (0.39) |
+0.04 (0.03) |
−0.03 (0.03) |
6.28 (0.37) |
−0.01 (0.03) |
−0.02 (0.03) |
0.787 | 0.275 | 0.830 |
| Erythema (AU) | 239.19 (63.79) |
+7.68 (12.94) |
+13.41 (7.16) |
191.30 (51.39) |
−7.41 (8.14) |
+19.95 (6.51) |
0.008 | 0.303 | 0.512 |
|
TEWL
(g·h−1·m−2) |
7.01 (3.29) |
+1.79 (0.87) |
+2.74 (0.07) |
8.65 (3.34) |
+0.05 (0.58) |
+1.48 (0.67) |
0.092 | 0.089 | 0.216 |
| SCH (AU) | 34.21 (10.67) |
−1.69 (1.65) |
+1.99 (1.47) |
40.14 (13.91) |
+1.58 (1.30) |
+1.53 (1.79) |
0.095 | 0.841 | 0.216 |
Data is expressed as mean (standard deviation). AU, arbitrary units; SCH, stratum corneum hydration; TEWL, transepidermal water loss. Data is expressed as means (standard deviations, SD). B p-value after using Student’s t-test for independent samples to compare skin barrier function at baseline between men and women. C p-value after using Student’s t-test for independent samples to compare skin barrier function changes after cold water exposure between men and women. H p-value after using Student’s t-test for independent samples to compare skin barrier function changes after hot water exposure between men and women. Bt p-value after using Student’s t-test for independent samples to compare skin barrier function at baseline between men and women. Ct p-value after using Student’s t-test for independent samples to compare skin barrier function changes after 4 °C TempTest exposure between men and women. Ht p-value after using Student’s t-test for independent samples to compare skin barrier function changes after 44 °C TempTest exposure between men and women.
Men showed higher temperature (31.20 vs. 30.47 °C, p = 0.038) and erythema (239.19 vs. 191.30 AU, p = 0.008) on the volar forearm at baseline but changes after TempTest were similar in both sexes. No differences in pH, TEWL or SCH were found.
Participants were classified according to their age: <30 years (56%, 28/50) or ≥30 years (44%, 22/50), as the turning points of skin barrier function appear in an individual’s thirties [22] (Table 3). Temperature (+ 2.60 vs. +2.20 °C, p = 0.012) and pH (+0.39 vs. +0.24, p = 0.04) increases were higher after hot water in participants < 30 years of age than in participants ≥30. Erythema (266.49 vs. 227.88 AU, p = 0.026) and SCH (53.62 vs. 37.87 AU, p = 0.002) on hands at baseline were higher in participants <30 than in participants ≥30, but changes after water exposure were similar between ages groups.
Table 3.
Changes in skin barrier function after hot and cold water exposure, stratified by age.
| Age < 30 (n = 28) | Age ≥ 30 (n = 22) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Water Exposure | |||||||||
| Basal | Cold Water | Hot Water | Basal | Cold Water | Hot Water | p B | p C | p H | |
| Temperature ( °C) | 30.02 (1.80) |
−5.99 (0.41) |
+2.60 (0.26) |
30.37 (1.90) |
−7.57 (0.44) |
+2.20 (0.30) |
0.507 | 0.322 | 0.012 |
| pH | 6.29 (0.43) |
+0.38 (0.07) |
+0.39 (0.07) |
6.37 (0.30) |
+0.18 (0.06) |
+0.24 (0.08) |
0.406 | 0.153 | 0.040 |
| Erythema (AU) | 266.49 (40.45) |
+2.66 (8.33) |
+35.18 (8.74) |
227.88 (68.29) |
+6.11 (14.99) |
+39.05 (12.16) |
0.026 | 0.792 | 0.833 |
| TEWL (g·h−1·m−2) | 25.36 (12.14) |
+10.79 (2.06) |
+33.75 (2.06) |
26.25 (12.99) |
+7.20 (2.02) |
+31.65 (2.63) |
0.804 | 0.528 | 0.302 |
| SCH (AU) | 53.62 (18.46) |
+1.75 (2.52) |
−5.91 (3.09) |
37.87 (15.33) |
+6.55 (2.61) |
+2.56 (2.85) |
0.002 | 0.055 | 0.196 |
| TempTest exposure | |||||||||
| Basal | 4 °C TempTest | 44 °C TempTest | Basal | 4 °C TempTest | 44 °C TempTest | p Bt | p Ct | p Ht | |
| Temperature (°C) | 30.89 (1.12) |
−5.68 (0.48) |
+1.75 (0.25) |
30.59 (1.38) |
−5.21 (0.39) |
+1.64 (0.25) |
0.399 | 0.778 | 0.446 |
| pH | 6.25 (0.39) |
−0.03 (0.03) |
−0.02 (0.03) |
6.28 (0.36) |
−0.05 (0.03) |
−0.02 (0.04) |
0.803 | 0.936 | 0.065 |
| Erythema (AU) | 228.80 (59.38) |
−5.10 (9.42) |
+19.43 (7.66) |
187.10 (55.56) |
+1.54 (10.45) |
+15.69 (6.26) |
0.015 | 0.705 | 0.648 |
| TEWL (g·h−1·m−2) | 7.21 (2.39) |
−0.08 (0.87) |
+2.50 (0.82) |
8.99 (4.19) |
+1.40 (0.57) |
+1.57 (0.62) |
0.087 | 0.359 | 0.163 |
| SCH (AU) | 34.76 (10.53) |
+1.20 (1.68) |
+0.97 (2.04) |
41.59 (14.85) |
+2.18 (1.13) |
−0.32 (1.63) |
0.063 | 0.618 | 0.621 |
Data is expressed as mean (standard deviations). AU, arbitrary units; SCH, stratum corneum hydration; TEWL, transepidermal water loss. Data is expressed as means (standard deviations, SD). B p-value after using Student’s t-test for independent samples to compare skin barrier function at baseline between <30 and ≥30 years old. C p-value after using Student’s t-test for independent samples to compare skin barrier function after cold water exposure between <30 and ≥30 years old. H p-value after using Student’s t-test for independent samples to compare skin barrier function after hot water exposure between <30 and ≥30 years old. Bt p-value after using Student’s t-test for independent samples to compare skin barrier function at baseline between <30 and ≥30 years old. Ct p-value after using Student’s t-test for independent samples to compare skin barrier function after 4 °C TempTest exposure between <30 and ≥30 years old. Ht p-value after using Student’s t-test for independent samples to compare skin barrier function after 44 °C TempTest exposure between <30 and ≥30 years old.
On the volar forearm, erythema was higher in participants <30 than in participants ≥ 30 (228.80 vs. 187.10, p = 0.015) but changes were similar between age groups after TempTest. No differences in other parameters were found.
4. Discussion
The skin barrier is impaired by water exposure, especially hot water. This is reflected in increased TEWL and pH values. Regarding temperature (TempTest exposure), only direct contact with hot temperatures showed skin barrier damage by increasing both TEWL and erythema. For the first time, we report skin barrier function changes after cold and hot water exposure and direct contact to cold and hot temperature.
Water exposure could damage the skin barrier through several mechanisms. Long exposure to water leads to disruption of the stratum corneum intercellular lipid lamellae, induces swelling in the corneocytes and the formation of large pools of water in the intercellular space [23,24]. Moreover, it has been described that water exposure causes changes in stratum corneum morphology and increases hydration in a dose-dependent way, facilitating the penetration of extrinsic irritants or allergens and providing a suitable environment for bacterial overgrowth [24,25]. A significant correlation has also been found between TEWL and temperature, as temperature promotes the mass transfer of water from the stratum corneum to the environment [26]. This could explain why TEWL values were higher after hot water exposure than after cold water exposure.
Water temperature might be a significant factor which increases skin damage when frequent handwashing is necessary, even more so nowadays because hand hygiene awareness has increased due to the COVID-19 pandemic [7]. Lipid fluidization, or disorganized lipid structure, is affected by higher water temperatures, resulting in greater skin permeability [17,27]. It is not recommended to use alcohol-based hand gels [28] or gloves with wet hands because it increases irritating substances trapped on the hands [18] that have been proven to disrupt the skin barrier [29]. Moreover, the American Contact Dermatitis Society recommends washing hands with cold or lukewarm water [18]. Our study supports all these recommendations with objective parameters for the first time, as we found that long and continuous water exposure could damage the skin barrier and that hot water is more aggressive than cold water, as shown by higher increases in TEWL values. It would be advisable to use cold or lukewarm water for handwashing and avoid hot water. Further research with different water temperature ranges should be conducted to select the most adequate temperature for handwashing.
Although this study did not include a pediatric population, the actual guidelines for skin care in infants recommends that the water temperature to wash children should be 37−37.5 °C [30]. This recommendation is based on expertise opinion, but we did not find any study comparing skin barrier function impairment with different water temperature in children. There might be differences in skin barrier function and water impact between children and adults as it has been described that pediatric skin undergoes a process of adaptation and maturation postnatally [31]. It could thus be interesting to develop similar studies in a pediatric population to evaluate the proper water temperature to wash children.
It has previously been shown that that TEWL and pH increased after immersing the volar forearm in tap water (15–20 °C) for 30 min a day for five consecutive days [24]. Nevertheless, the experimental conditions were different from ours and it is difficult to compare these studies. Other research has also showed that TEWL increased after water-patch occlusion [32], but this study is biased as occlusion alone can disrupt the skin barrier [33,34] (Table 4). For the first time, we report skin barrier function changes after water immersion and compare the effect of cold and hot water.
Table 4.
Studies evaluating water and temperature exposure.
| Study | Number of Participants | Exposure | Results |
|---|---|---|---|
| Water Exposure | |||
| Firooz et al. 2015 [24] | 20 | Water immersion at 15–20 °C for 30 min a day for five days | TEWL increased pH increased |
| Agner et al. 1993 [32] | 14 | Water patch-occlusion during 24 h:
|
TEWL increased immediately and 30 min after removal of all test chambers. TEWL also increased 180 min after SLS and water patch removal. |
| Our study | 50 | Cold water exposure (11.13 (2.71 SD) °C) for 10 min | Temperature decreased by 6.69 °C pH increased by 0.29 TEWL increased by 9.21 (g·h−1·m−2) SCH increased 3.86 AU |
| Hot water exposure (41.29 (2.29 SD) °C) for 10 min | Temperature increased by 2.42 °C pH increased by by 0.32 Erythema increased by 36.88 AU TEWL increased by 32.83 (g·h−1·m−2) |
||
| Temperature exposure | |||
| Kim et al. 2019 [16] | 20 | Exposure to outdoor environment for 90 min (34.76 ± 2.79 °C, 53.13 ± 8.78% RH) |
SCH on the forearm and sebum secretion on the face increased. SCH and TEWL on the cheek and greasiness on the forearm and the forehead decreased. pH decreased in the face and the forearm. |
| Exposure to indoor environment for 90 min (22.97 ± 0.74 °C, 53.14 ± 2.37% RH) |
SCH in the forehead and the forearm. Sebum secretion and greasiness on the face increased. TEWL and pH in the face and the forearm decreased. |
||
| Cravello et al. 2008 [26] | 6 | Exposure to three levels of ambient temperature (20 °C, 25 °C and 30 °C) and four levels of RH (25%, 45%, 65% and 85%) |
TEWL is positively correlated to ambient temperature. Skin temperature is correlated positively to ambient temperature but not to RH. SCH is strongly affected by ambient temperature and RH. |
| Qiu et al. 2011 [35] | 354 | 6 month periods, summer (35–40 °C, RH ≥ 70%) and winter (0–5 °C, RH ≥ 70%) | SCH and melanin increased in summer compared to winter. |
| Our study | 50 | Cold temperatrue exposure (4 °C) | Temperature decreased by 5.41 °C |
| Hot temperature exposure (44 °C) | Temperatrure increased by 1.69 °C Erythema increased by 17.34 AU TEWL increased by 1.98 (g·h−1·m−2) |
||
AU, arbitrary units; RH, relative humidity; SCH, stratum corneum hydration; SLS, sodium lauryl sulphate; TEWL, transepidermal water loss.
Regarding the direct effect of temperature on the skin, it has previously been observed that ambient air temperature affects skin properties such as pH, TEWL, sebum content, hydration, elasticity, wrinkles, skin pores and skin sensitivity [16,26,35]. This has been extensively studied in relation to the seasons of the year [16,26,35]. Sebum output, melanin content of pigmented spots, skin colour and skin hydration are increased in summer compared to in winter [35]. Higher ambient air temperature also positively correlates to high TEWL values [16,26] and promotes sweating, which increases hydration and sebum secretion and decreases pH [16] (Table 4). We found that temperature, TEWL and erythema increase after exposure to heat. We did not find any differences in pH or SCH, which may be explained by a short contact time or by differences in the type of temperature exposure. Our research assessed the impact on skin barrier function after direct contact with different temperatures while the others evaluated changes after ambient air. We did not find any study that compared epidermal barrier changes after direct contact with different temperatures. It would be interesting to develop further research to compare skin barrier impairment between ambient air exposure and direct contact with different temperatures.
As far as we know, no previous study included information regarding changes after water and temperature exposure between sexes and ages. We observed that women were more prone to have changes in temperature and SCH after cold water exposure, being likely explained by the slightly thicker stratum corneum in males [36]. However, the relationship between gender and skin barrier function seems to be outweighed by individualized factors [36]. In relation to different impact of water and temperature depending on age, we only found that temperature and pH increases were higher in the younger group after water exposure. One explanation could be that young individuals have a greater blood flow, especially in sites exposed to the environment like the hands, what would rapidly adapt the skin to the environmental conditions [37].
Chronic skin diseases which typically appear on the hands are contact dermatitis (both irritative and allergic), atopic dermatitis and palmoplantar psoriasis [38,39,40]. Long water exposure in these patients is related to disease worsening [41], as immersing irritated hands in water increases blood flow and aggravates inflammation [42]. Moreover, it has been observed that high water temperature also impacts on the irritant capacity of detergents and could increase the risk for developing irritant dermatitis [43]. Therefore, washing hands at a suitable temperature might be a simple but essential step for preventing disease flares in patients with hand skin diseases.
Our study shows that TEWL values in healthy individuals differ widely between the volar forearm and the palms, as has been reported previously [2,44]. This fact has been attributed to differences in the number of corneocyte cell layers and in the size and turnover rates of corneocytes [45], as well as the low amount of barrier lipids in the stratum corneum in the palm [46]. Moreover, the higher TEWL values on the palms could be due to their thicker stratum corneum, higher exposure to friction and damage, and greater density of eccrine sweat glands [47].
This study was subject to some limitations such as a limited sample size, the lack of a longer follow-up and the exposure time. It has been noted that a healthcare worker could wash their hands on average from 5 to as many as 42 times [7,48]. Moreover, WHO guidelines recommend that the whole procedure of hand washing should take 40–60 s [48]. Considering the lowest rates of hand washing, a person could wash his hands 10 times for 40 s each, exposing his hands to water around 8 min per day on average. It should be also considered that times of hand washing could impact on skin barrier function. This fact is not expected to change our conclusions because in our study we compared participants before and after each exposure, using paired samples, but it should be considered when designing this type of research. Future research could measure more parameters of skin barrier function and lengthen exposure time to both water and temperature as longer exposure would lead to even greater changes in skin barrier function parameters.
5. Conclusions
Water and temperature have a significant effect on the skin barrier. Skin is impaired by water exposure, even more so with hot water, as reflected by increased TEWL values. Hot temperature also damages the skin, as shown by increased erythema and TEWL values. Knowing the proper temperature for hand washing might be an important measure to prevent flares in patients with previous skin inflammatory diseases on their hands.
Acknowledgments
We would like to thank all the individuals who generously shared their time to participate in this research and Charlotte Bower for the English correction of this manuscript.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11020298/s1, Table S1. Changes in skin barrier function after cold and hot water exposure. Table S2. Changes in skin barrier function after TempTest.
Author Contributions
Conceptualization, S.A.-S.; methodology, S.A.-S. and T.M.-V.; software, A.B.-E.; validation, P.D.-C.; formal analysis, M.H.-F., S.A.-S. and T.M.-V.; investigation, M.H.-F., S.A.-S. and T.M.-V.; resources, M.H.-F. and S.A.-S.; data curation, M.H.-F., P.D.-C. and M.R.-V.; writing—original draft preparation, M.H.-F. and T.M.-V.; writing—review and editing, S.A.-S.; visualization, S.A.-S.; project administration, S.A.-S.; funding acquisition, S.A.-S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Hospital Universitario Virgen de las Nieves, Granada, Spain (protocol code HC01, 0442-N-20, and date of approval 8 May 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Clark R.A., Ghosh K., Tonnesen M.G. Tissue Engineering for Cutaneous Wounds. J. Investig. Dermatol. 2007;127:1018–1029. doi: 10.1038/sj.jid.5700715. [DOI] [PubMed] [Google Scholar]
- 2.Akdeniz M., Gabriel S., Lichterfeld-Kottner A., Blume-Peytavi U., Kottner J. Transepidermal water loss in healthy adults: A systematic review and meta-analysis update. Br. J. Dermatol. 2018;179:1049–1055. doi: 10.1111/bjd.17025. [DOI] [PubMed] [Google Scholar]
- 3.Alexander H., Brown S., Danby S., Flohr C. Research Techniques Made Simple: Transepidermal Water Loss Measurement as a Research Tool. J. Investig. Dermatol. 2018;138:2295–2300.e1. doi: 10.1016/j.jid.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Montero-Vilchez T., Segura-Fernández-Nogueras M.-V., Pérez-Rodríguez I., Soler-Gongora M., Martinez-Lopez A., Fernández-González A., Molina-Leyva A., Arias-Santiago S. Skin Barrier Function in Psoriasis and Atopic Dermatitis: Transepidermal Water Loss and Temperature as Useful Tools to Assess Disease Severity. J. Clin. Med. 2021;10:359. doi: 10.3390/jcm10020359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosso J.D., Zeichner J., Alexis A., Cohen D., Berson D. Understanding the Epidermal Barrier in Healthy and Compromised Skin: Clinically Relevant Information for the Dermatology Practitioner: Proceedings of an Expert Panel Roundtable Meeting. J. Clin. Aesthet. Dermatol. 2016;9:S2–S8. [PMC free article] [PubMed] [Google Scholar]
- 6.Elias P.M., Choi E.H. Interactions among stratum corneum defensive functions. Exp. Dermatol. 2005;14:719–726. doi: 10.1111/j.1600-0625.2005.00363.x. [DOI] [PubMed] [Google Scholar]
- 7.Kendziora B., Guertler A., Ständer L., Frey S., French L.E., Wollenberg A., Reinholz M. Evaluation of hand hygiene and onset of hand eczema after the outbreak of SARS-CoV-2 in Munich. Eur. J. Dermatol. 2020;30:668–673. doi: 10.1684/ejd.2020.3923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirose R., Ikegaya H., Naito Y., Watanabe N., Yoshida T., Bandou R., Daidoji T., Itoh Y., Nakaya T. Survival of SARS-CoV-2 and influenza virus on the human skin: Importance of hand hygiene in COVID-19. Clin. Infect. Dis. 2021;73:e4329–e4335. doi: 10.1093/cid/ciaa1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Araghi F., Tabary M., Gheisari M., Abdollahimajd F., Dadkhahfar S. Hand Hygiene among Health Care Workers during COVID-19 Pandemic: Challenges and Recommendations. Dermatitis. 2020;31:233–237. doi: 10.1097/DER.0000000000000639. [DOI] [PubMed] [Google Scholar]
- 10.Hamming I., Timens W., Bulthuis M.L.C., Lely A.T., Navis G.J., van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xue X., Mi Z., Wang Z., Pang Z., Liu H., Zhang F. High expression of ACE2 on the keratinocytes reveals skin as a potential target for SARS-CoV-2. J. Investig. Dermatol. 2021;141:206–209.e1. doi: 10.1016/j.jid.2020.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Benna S. Gene Expression of Angiotensin-Converting Enzyme 2 Receptor in Skin and the Implications for COVID-19. Adv. Skin Wound Care. 2021;34:31–35. doi: 10.1097/01.ASW.0000722748.73437.7d. [DOI] [PubMed] [Google Scholar]
- 13.Montero-Vilchez T., Cuenca-Barrales C., Martinez-Lopez A., Molina-Leyva A., Arias-Santiago S. Skin adverse events related to personal protective equipment: A systematic review and meta-analysis. J. Eur. Acad. Dermatol. Venereol. 2021;35:1994–2006. doi: 10.1111/jdv.17436. [DOI] [PubMed] [Google Scholar]
- 14.Michaels B., Gangar V., Schultz A., Arenas M., Curiale M., Ayers T., Paulson D. Water temperature as a factor in handwashing efficacy. Food Serv. Technol. 2002;2:139–149. doi: 10.1046/j.1471-5740.2002.00043.x. [DOI] [Google Scholar]
- 15.Carrico A., Spoden M., Wallston K.A., Vandenbergh M.P. The environmental cost of misinformation: Why the recommendation to use elevated temperatures for handwashing is problematic. Int. J. Consum. Stud. 2013;37:433–441. doi: 10.1111/ijcs.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim S., Park J.W., Yeon Y., Han J.Y., Kim E. Influence of exposure to summer environments on skin properties. J. Eur. Acad. Dermatol. Venereol. 2019;33:2192–2196. doi: 10.1111/jdv.15745. [DOI] [PubMed] [Google Scholar]
- 17.Jensen D.A., Macinga D.R., Shumaker D.J., Bellino R., Arbogast J.W., Schaffner D.W. Quantifying the Effects of Water Temperature, Soap Volume, Lather Time, and Antimicrobial Soap as Variables in the Removal of Escherichia coli ATCC 11229 from Hands. J. Food Prot. 2017;80:1022–1031. doi: 10.4315/0362-028X.JFP-16-370. [DOI] [PubMed] [Google Scholar]
- 18.Rundle C.W., Presley C.L., Militello M., Barber C., Powell D.L., Jacob S.E., Atwater A.R., Watsky K.L., Yu J., Dunnick C.A. Hand hygiene during COVID-19: Recommendations from the American Contact Dermatitis Society. J. Am. Acad. Dermatol. 2020;83:1730–1737. doi: 10.1016/j.jaad.2020.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schoepke N., Doumoulakis G., Maurer M. Diagnosis of urticaria. Indian J. Dermatol. 2013;58:211–218. doi: 10.4103/0019-5154.110831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kulthanan K., Tuchinda P., Chularojanamontri L., Kiratiwongwan R. Cold Urticaria: Clinical Features and Natural Course in a Tropical Country. Allergy Asthma Immunol. Res. 2019;11:538–547. doi: 10.4168/aair.2019.11.4.538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodrigues-Valle S., Azizi G., Duarte-Dortas S., Jr. TempTest(R): Un instrumento de precision en las urticarias fisicas. Rev. Alerg. Mex. 2021;68:2–6. doi: 10.29262/ram.v68i1.827. [DOI] [PubMed] [Google Scholar]
- 22.Pan Y., Ma X., Zhao J., Yan S., Liu Q., Zhao H. The Interaction of Age and Anatomical Region Influenced Skin Biophysical Characteristics of Chinese Women. Clin. Cosmet. Investig. Dermatol. 2020;13:911–926. doi: 10.2147/CCID.S286402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Warner R.R., Stone K.J., Boissy Y.L. Hydration Disrupts Human Stratum Corneum Ultrastructure. J. Investig. Dermatol. 2003;120:275–284. doi: 10.1046/j.1523-1747.2003.12046.x. [DOI] [PubMed] [Google Scholar]
- 24.Firooz A., Aghazadeh N., Estarabadi A.R., Hejazi P. The effects of water exposure on biophysical properties of normal skin. Skin Res. Technol. 2014;21:131–136. doi: 10.1111/srt.12167. [DOI] [PubMed] [Google Scholar]
- 25.Ogawa-Fuse C., Morisaki N., Shima K., Hotta M., Sugata K., Ichihashi T., Oguri M., Yoshida O., Fujimura T. Impact of water exposure on skin barrier permeability and ultrastructure. Contact Dermat. 2018;80:228–233. doi: 10.1111/cod.13174. [DOI] [PubMed] [Google Scholar]
- 26.Cravello B., Ferri A. Relationships between skin properties and environmental parameters. Skin Res. Technol. 2008;14:180–186. doi: 10.1111/j.1600-0846.2007.00275.x. [DOI] [PubMed] [Google Scholar]
- 27.Park J.-H., Lee J.-W., Kim Y.-C., Prausnitz M.R. The effect of heat on skin permeability. Int. J. Pharm. 2008;359:94–103. doi: 10.1016/j.ijpharm.2008.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Plum F., Yüksel Y.T., Agner T., Nørreslet L.B. Skin barrier function after repeated short-term application of alcohol-based hand rub following intervention with water immersion or occlusion. Contact Dermat. 2020;83:215–219. doi: 10.1111/cod.13587. [DOI] [PubMed] [Google Scholar]
- 29.Montero-Vilchez T., Martinez-Lopez A., Cuenca-Barrales C., Rodriguez-Tejero A., Molina-Leyva A., Arias-Santiago S. Impact of Gloves and Mask Use on Epidermal Barrier Function in Health Care Workers. Dermatitis. 2021;32:57–62. doi: 10.1097/DER.0000000000000682. [DOI] [PubMed] [Google Scholar]
- 30.Blume-Peytavi U., Lavender T., Jenerowicz D., Ryumina I., Stalder J., Torrelo A., Cork M. Recommendations from a European Roundtable Meeting on Best Practice Healthy Infant Skin Care. Pediatr. Dermatol. 2016;33:311–321. doi: 10.1111/pde.12819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoeger P.H., Enzmann C.C. Skin Physiology of the Neonate and Young Infant: A Prospective Study of Functional Skin Parameters during Early Infancy. Pediatr. Dermatol. 2002;19:256–262. doi: 10.1046/j.1525-1470.2002.00082.x. [DOI] [PubMed] [Google Scholar]
- 32.Agner T., Serup J. Time course of occlusive effects on skin evaluated by measurement of transepidermal water loss (TEWL) Including patch tests with sodium lauryl sulphate and water. Contact Dermat. 1993;28:6–9. doi: 10.1111/j.1600-0536.1993.tb03316.x. [DOI] [PubMed] [Google Scholar]
- 33.Jungersted J.M., Høgh J.K., Hellgren L.I., Jemec G.B.E., Agner T. Skin barrier response to occlusion of healthy and irritated skin: Differences in trans-epidermal water loss, erythema and stratum corneum lipids. Contact Dermat. 2010;63:313–319. doi: 10.1111/j.1600-0536.2010.01773.x. [DOI] [PubMed] [Google Scholar]
- 34.Kligman A.M. A personal critique of diagnostic patch testing. Clin. Dermatol. 1996;14:35–40. doi: 10.1016/0738-081X(95)00106-P. [DOI] [PubMed] [Google Scholar]
- 35.Qiu H., Long X., Ye J.C., Hou J., Senee J., Laurent A., Bazin R., Flament F., Adam A., Coutet J., et al. Influence of season on some skin properties: Winter vs. summer, as experienced by 354 Shanghaiese women of various ages. Int. J. Cosmet. Sci. 2011;33:377–383. doi: 10.1111/j.1468-2494.2011.00639.x. [DOI] [PubMed] [Google Scholar]
- 36.Dąbrowska A., Spano F., Derler S., Adlhart C., Spencer N., Rossi R. The relationship between skin function, barrier properties, and body-dependent factors. Skin Res. Technol. 2018;24:165–174. doi: 10.1111/srt.12424. [DOI] [PubMed] [Google Scholar]
- 37.Waller J.M., Maibach H.I. Age and skin structure and function, a quantitative approach (I): Blood flow, pH, thickness, and ultrasound echogenicity. Skin Res. Technol. 2005;11:221–235. doi: 10.1111/j.0909-725X.2005.00151.x. [DOI] [PubMed] [Google Scholar]
- 38.Warshaw E.M., Goodier M., Dekoven J.G., Maibach H.I., Taylor J.S., Sasseville D., Belsito D.V., Fowler J.F., Fransway A.F., DeLeo V.A., et al. Contact Dermatitis Associated With Skin Cleansers: Retrospective Analysis of North American Contact Dermatitis Group Data 2000–2014. Dermatitis. 2018;29:32–42. doi: 10.1097/DER.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 39.Wollenberg A., Christen-Zäch S., Taieb A., Paul C., Thyssen J., De Bruin-Weller M., Vestergaard C., Seneschal J., Werfel T., Cork M., et al. ETFAD/EADV Eczema task force 2020 position paper on diagnosis and treatment of atopic dermatitis in adults and children. J. Eur. Acad. Dermatol. Venereol. 2020;34:2717–2744. doi: 10.1111/jdv.16892. [DOI] [PubMed] [Google Scholar]
- 40.Raposo I., Torres T. Palmoplantar Psoriasis and Palmoplantar Pustulosis: Current Treatment and Future Prospects. Am. J. Clin. Dermatol. 2016;17:349–358. doi: 10.1007/s40257-016-0191-7. [DOI] [PubMed] [Google Scholar]
- 41.Carøe T.K., Ebbehøj N.E., Bonde J.P.E., Flachs E.M., Agner T. Hand eczema and wet work: Dose-response relationship and effect of leaving the profession. Contact Dermat. 2018;78:341–347. doi: 10.1111/cod.12934. [DOI] [PubMed] [Google Scholar]
- 42.Ramsing D.W., Agner T. Effect of water on experimentally irritated human skin. Br. J. Dermatol. 1997;136:364–367. doi: 10.1111/j.1365-2133.1997.tb14945.x. [DOI] [PubMed] [Google Scholar]
- 43.Ohlenschlaeger J., Friberg J., Ramsing D., Agner T. Temperature dependency of skin susceptibility to water and detergents. Acta Derm. Venereol. 1996;76:274–276. doi: 10.2340/0001555576274276. [DOI] [PubMed] [Google Scholar]
- 44.Espinosa-Rueda M.I., Montero-Vilchez T., Martinez-Lopez A., Molina-Leyva A., Sierra-Sánchez A., Arias-Santiago S., Buendia-Eisman A. Cutaneous homeostasis and epidermal barrier function in a young healthy Caucasian population. Eur. J. Dermatol. 2021;31:176–182. doi: 10.1684/ejd.2021.4021. [DOI] [PubMed] [Google Scholar]
- 45.Ya-Xian Z., Suetake T., Tagami H. Number of cell layers of the stratum corneum in normal skin—Relationship to the anatomical location on the body, age, sex and physical parameters. Arch. Dermatol Res. 1999;291:555–559. doi: 10.1007/s004030050453. [DOI] [PubMed] [Google Scholar]
- 46.Tagami H. Location-related differences in structure and function of the stratum corneum with special emphasis on those of the facial skin. Int. J. Cosmet. Sci. 2008;30:413–434. doi: 10.1111/j.1468-2494.2008.00459.x. [DOI] [PubMed] [Google Scholar]
- 47.Wa C.V., Maibach H.I. Mapping the human face: Biophysical properties. Skin Res. Technol. 2010;16:38–54. doi: 10.1111/j.1600-0846.2009.00400.x. [DOI] [PubMed] [Google Scholar]
- 48.World Health Organization WHO Guidelines on Hand Hygiene in Health Care Provide Health-Care Workers (HCWs) 2009. [(accessed on 15 May 2021)]. Available online: https://www.who.int/publications/i/item/9789241597906.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.