Abstract
Filth flies, cockroaches, and dung beetles have been close neighbors with humans and animals throughout our joint histories. However, these insects can also serve as vectors for many zoonotic enteric parasites (ZEPs). Zoonoses by ZEPs remain a paramount public health threat due to our close contact with animals, combined with poor water, sanitation, and hygiene access, services, and behaviors in many global regions. Our objective in this systematic review was to determine which ZEPs have been documented in these vectors, to identify risk factors associated with their transmission, and to provide effectual One Health recommendations for curbing their spread. Using PRISMA guidelines, a total of 85 articles published from 1926 to 2021 were reviewed and included in this study. Qualitative analysis revealed that the most common parasites associated with these insects included, but were not limited to: Ascaris spp., Trichuris spp., Entamoeba spp., and Cryptosporidium spp. Additionally, prominent risk factors discovered in the review, such as poor household and community WASH services, unsafe food handling, and exposure to domestic animals and wildlife, significantly increase parasitic transmission and zoonoses. The risk of insect vector transmission in our shared environments makes it critically important to implement a One Health approach in reducing ZEP transmission.
Keywords: zoonoses, parasites, one health, water, sanitation, hygiene
1. Introduction
Flies (Diptera), cockroaches (Blattodea), and dung beetles (Coleoptera) share their environment with humans, animals, and other insects. While their presence can be beneficial—for example, through pollination, management of other pests, as a food source, and as an organic disposal system for decaying matter—they can also pose risks to human and animal health. Our close ecological connection to these insects presents the public health risk of disease transmission when one or more vectors are infected or contaminated with pathogenic organisms, such as zoonotic enteric parasites (ZEPs) [1,2,3,4,5]. ZEPs can be transmitted through direct contact with an insect vector harboring or carrying a parasite, or by accidental fecal–oral ingestion from contaminated food, water, hands, surfaces, and fomites [1].
Flies, particularly filth flies, are synanthropic and can be found anywhere humans are present, particularly in areas with poor water, sanitation, and hygiene services and practices [6,7]. Of the 46 species of flies that are associated with unclean environments or conditions of “filth”, 21 species are considered “disease-causing flies” or known to be vectors of foodborne pathogens [8] (p. 199). Many species of filth flies are coprophagic, feeding on the fecal waste of animals and humans. While these insects often favor indoor spaces, they frequently move back and forth between contaminated environmental settings and human living spaces. This repeated contact introduces the risk of exposure to enteric diseases of public health concern [1,8]. Filth flies are drawn to damp, organic matter (e.g., prepared food, garbage, sewage, or feces) to feed and lay eggs [7]. These behaviors create the risk of transmission of a variety of bacteria, viruses, and parasites that are shed in excreta [2,5,7,9]. As filth flies land on materials which can host a variety of pathogens and parasites, they are able to mechanically collect infectious particles or parasitic oocysts on their legs, bodies, or mouthparts as well as ingest the pathogen. Transmission to humans or animals occurs mechanically through contact with shared surfaces or other items, hands and faces, or food products [1,7,8].
While over 3500 species of cockroaches exist worldwide, only thirty species are known to be associated with human habitation [10]. Cockroaches have strong nocturnal habits and are often prevalent in areas of significant warmth, moisture, darkness, and where they can access exposed food particles [3]. Cockroaches commonly exist in the residential domain, but can also be found in restaurants, grocery stores, hospitals, and commercial facilities [11]. In addition to the triggering of asthma and other respiratory conditions due to residential infestations, cockroaches have been found to harbor parasitic microorganisms, externally on their cuticle or internally in their gastrointestinal tract [12]. They have been known to spread multiple pathogens, including bacteria, protozoa, fungi, and pathogenic intestinal worms [1,10]. Human consumption of vector-contaminated food is a risk factor for foodborne illness and the acquisition of parasitic infections. Additionally, human consumption of cockroaches, directly as entomophagy or accidentally, can also represent a risk of infection that is of public health importance [13]. Due to cockroaches’ feeding habits and preferences for human food and feces, they have the potential to become mechanical vectors for the spread of various zoonotic enteric parasites [3].
Dung beetles are coprophagous insects that depend on the fecal material of vertebrates in order to consume and reproduce. Dung beetles are found worldwide, including in places such as farms, peri-urban regions, and urban areas [14]. More than 7000 species of dung beetles handle, bury, or move wildlife feces every day [15]. Dung beetles may transmit disease mechanically on their exoskeletons or within their gastrointestinal systems [1,15]. Through contact with feces from a variety of sources such as livestock and companion animals as well as wild animals, dung beetles pose the threat of ZEP transmission of these parasites to humans. Dung beetles may also further spread disease in urban areas where unmanaged fecal waste is prevalent, such as communities with poor sanitation measures and areas where livestock and domestic animals live near humans [14].
The aim of this study was to determine which zoonotic enteric parasites (ZEPs) have been reported in filth flies, cockroaches, and dung beetles, and to identify the risk factors associated with their transmission. Understanding more about these vectors of public health importance will inform opportunities for One Health research, guidance, intervention, and collaboration.
2. Methods
2.1. Search Strategy
Between 28 January and 4 February 2021, we initially searched the following databases: Pubmed; Web of Science Core Collection; Google Scholar; Environment Complete; Science Direct; GALE databases of Agriculture Collection; Nursing and Allied Health Outcomes; Environmental Studies and Policy; the ProQuest databases of the ABI/INFORM Collection; Agricola, Earth, Atmospheric, and Aquatic Sciences Collection; Agricultural and Environmental Science Collection; Health and Medicine; MEDLINE (Proquest); and TOXLINE. Search strings were developed for each database using keywords related to filth flies, cockroaches, and dung beetles in conjunction with zoonotic enteric parasites [16]. When the option was available, database search results were further restricted to journal articles and the title and abstract keywords only. Accessible results were copied into the citation manager Refworks by database, and a master folder was created for all titles found in the initial search. An updated search was conducted on 27 December 2021 for any relevant titles published in the months following the initial search using the same search parameters as above. An informal protocol with the full listing of all search strings used and their corresponding database is provided in Supplementary Materials Table S1. A formal protocol was not prepared and the review was not registered.
2.2. Screening Process and Study Selection
Following PRISMA guidelines, titles were screened first for eligibility based on full and legible citations and journal article titles only [17]. Then, in groups of two reviewers at a time, the titles and abstracts were assessed. Inclusion criteria consisted of titles that were: (a) peer-reviewed journal articles; (b) from any publication year; with (c) primary research documenting the presence of a recognized or probable ZEP in an insect vector, either through natural or experimental infection; and the (d) ZEP has a primarily enteric transmission route. Exclusion criteria comprised: (a) any publication that was not a peer-reviewed journal article; (b) titles written in a language other than English without relevant information provided in an English abstract; (c) reviews or models that did not contain primary research; (d) research on vectors other than filth flies, cockroaches, or dung beetles; (e) research on enteric or gastrointestinal parasites that are not considered zoonotic or likely to be zoonotic; or (f) research that included negative results. When an abstract was not available for the first round of screening, the title was included in the next round for full text review. Titles that studied zoonotic enteric parasites not on our initial list of search terms were included after review by the team against the criteria outlined above.
Full text documents were retrieved by the authors and through the assistance of university librarians. Each full text title was reviewed by at least two authors based on the eligibility criteria above and subsequently marked for inclusion or exclusion. The senior author (AB) served as a tie-breaker when needed. If more than one title addressed the same study or data, the more complete publication was retained for inclusion. When the full text of the article was written in a language other than English, the titles were retained if the relevant inclusion criteria were met in an available English abstract. A second round of review was performed on the excluded full-text articles as a quality control measure in order to ensure a comprehensive list of final studies for inclusion.
2.3. Data Extraction
A qualitative analysis was conducted on the included studies by the reviewers to account for the wide variety of publication styles and research methods presented. From the included studies, data were extracted to determine the publication year, the location of the study site, the source or location of the samples, the vector(s) analyzed, the parasite(s) analyzed, specific prevalence rates, if provided, and the means through which the vector was infected (natural or experimental). Information on risk factors for human or animal transmission outlined in the article was also noted.
3. Results
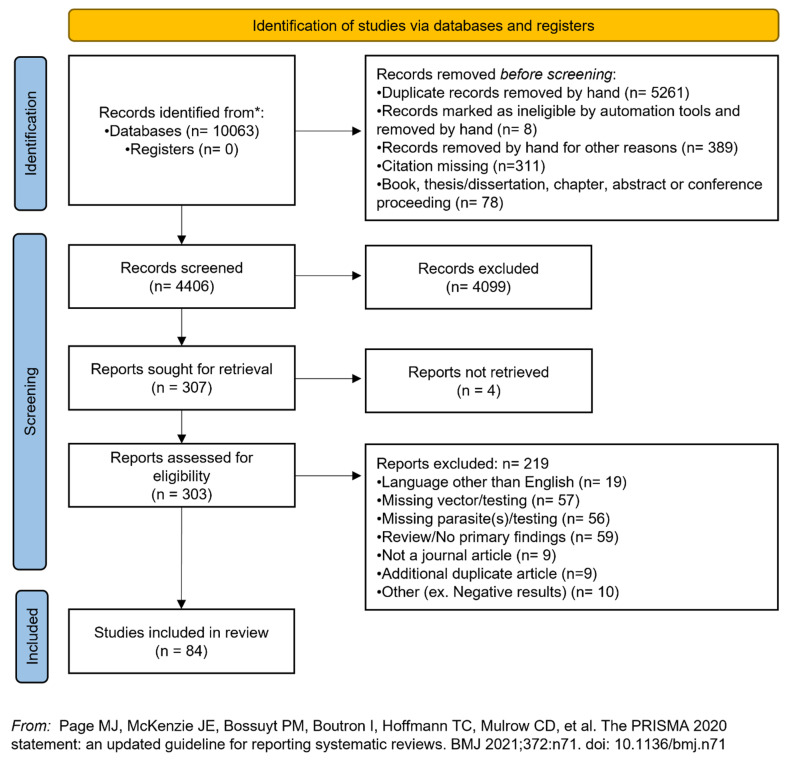
The full search resulted in 10,063 accessible titles. We removed 5261 duplicate records, 8 titles that were not legible with the use of automation tools, 311 records with missing citations, and 78 books, book chapters, abstracts, thesis/dissertations, and conference proceedings. At this point, 4406 records remained for the title and abstract screening, and 4099 were excluded using the eligibility criteria outlined above. We attempted to find the full-text versions of 307 titles, but 4 records were not accessible through institutional library channels. A total of 303 articles were read in their entirety, if written in English, or the abstract was reviewed if the full text was not available in English. All titles at this stage were screened against the inclusion/exclusion criteria, and 85 titles were incorporated into the final tally of the study results. Full-text articles were excluded for language (n = 19, missing vector or vector not tested (n = 57), missing zoonotic enteric parasite or not testing for parasite (n = 55), article was a review or did not have primary findings (n = 59), the publication was not a journal article (n = 9), the title was an additional duplicate not removed at the earlier stage (n = 9), or other reasons such as negative results (n = 10). A PRISMA flow diagram of the screening process is available in Figure 1.
Figure 1.
PRISMA screening flowchart of study selection.
Studies were conducted worldwide, across countries on every continent, except for Antarctica (n = 85; Table 1). The most common included the United States (n = 13), Nigeria (n = 7), Ethiopia (n = 5), and Poland (n = 5). More broadly, studies were conducted in the continental regions of North America (n = 13), South America (n = 13), Europe (n = 20), Africa (n = 17), Asia (n = 19), and Australia (n = 2). Publication dates ranged from 1926 through 2021. Several of the studies (n = 11) identified met the inclusion criteria based on an English abstract and were conservatively included in the results. However, the full text could not be analyzed due to language limitations of the authors.
Table 1.
Characteristics of included studies examining zoonotic enteric parasites of public health concern in flies, cockroaches, and/or dung beetles.
| Zoonotic Enteric Parasite(s) † | Vector(s) | Country of Study | Sample Source | Type of Iinfection | Citation | |
|---|---|---|---|---|---|---|
| Class and Family | Genus an/or Species and Natural Prevalence (%), When Provided | |||||
| Chromadorea, Ascarididae | Ascaris spp. | Cockroach | India | Village area | Experimental | Chandler 1926 [18] |
| Chromadorea Ancylostomatidae | Hookworm (Unspecified) | |||||
| Enoplea, Trichuridae | Trichuris spp. | |||||
| Lobosa, Entamoebidae | Entamoeba histolytica | Fly | England | Laboratory | Experimental | Roberts 1947 [19] |
| Cestoda, Taeniidae | Echinococcus spp. | Fly | United States | Laboratory | Experimental | Schiller 1954 [20] |
| Cestoda, Taeniidae | Echinococcus granulosus | Fly | South Africa | Laboratory | Experimental | Heinz and Brauns 1955 [21] |
| Conoidasida, Sarcocystidae | Toxoplasma gondii | Fly | Netherlands | Laboratory | Experimental | Laarman 1956 [22] |
| Chromadorea, Ascarididae | Ascaris lumbricoides | Dung beetle | United States | Farm/Field | Experimental | Miller et al. 1961 [23] |
| Zoomastigophora, Hexamitidae | Giardia lamblia | |||||
| Chromadorea Ancylostomatidae | Hookworm (Necator americanus) | |||||
| Enoplea, Trichuridae | Trichuris trichiura | |||||
| Conoidasida, Sarcocystidae | T. gondii | Fly | Brazil | Laboratory | Experimental | Paim and Queiroz 1963 * [24] |
| Chromadorea, Toxocaridae | Toxocara canis | Fly | England | Laboratory | Experimental | Pegg 1971 [25] |
| Conoidasida, Sarcocystidae | T. gondii | Fly | United States | Laboratory | Experimental | Wallace 1971 [26] |
| Chromadorea, Ascarididae | Ascaris spp. | Fly | Azerbaijan | Laboratory Village area |
Mixed | Nadzhafov 1972 * [27] |
| Chromadorea Ancylostomatidae | Hookworm (Unspecified) | |||||
| Cestoda, Hymenolepididae | Hymenolepis nana | |||||
| Enoplea, Trichuridae | Trichuris spp. | |||||
| Conoidasida, Sarcocystidae | T. gondii | Cockroach | United States | Laboratory | Experimental | Wallace 1972 [28] |
| Enoplea, Trichinellidae | Trichinella spiralis | Cockroach | United States | Laboratory | Experimental | Young and Babero 1974 [29] |
| Chromadorea, Ascarididae | Ascaris columnaris (Baylisascaris procyonis) | Cockroach | United States | Laboratory | Experimental | Young 1975 [30] |
| Ascaris suum | ||||||
| Cestoda, Dipylidiidae | Dipylidium caninum | |||||
| Cestoda, Hymenolepididae | Hymenolepis dimenuta | |||||
| H. nana | ||||||
| Cestoda, Mesocestoididae | Mesocestoides lineatus | |||||
| Chromadorea, Physalopteridae | Physaloptera turgida § | |||||
| Chromadorea, Setariidae | Setaria equina § | |||||
| Chromadorea, Oxyuridae | Syphacia obvelata | |||||
| Chromadorea, Toxocaridae | Toxascaris leonine § | |||||
| T. canis | ||||||
| Toxocara cati | ||||||
| Conoidasida, Sarcocystidae | T. gondii | Cockroach | Costa Rica | Unspecified | Experimental | Chinchilla and Ruiz 1976 [31] |
| Lobosa, Entamoebidae | Entamoeba spp. | Cockroach | Tunisia | Urban area | Natural | Gonzalez and Mishra 1976 * [32] |
| Archiacanthocephala, Moniliformidae | Moniliformis moniliformis | |||||
| Chromadorea, Ascarididae | A. lumbricoides (18.8–62.5%) | Fly | Bangladesh | Abattoir/Butchery/Slaughterhouse/ Food market Hospital Household Open defecation area Public transportation Waste disposal area |
Natural | Khan and Huq 1978 [33] |
| Zoomastigophora, Hexamitidae | Giardia spp. (6.2%) | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified; 15.6%) | |||||
| Enoplea, Trichuridae | Trichuris trichiura (46.9%) | |||||
| Conoidasida, Sarcocystidae | Sarcocystis muris | Cockroach | United States | Laboratory | Experimental | Smith and Frenkel 1978 [34] |
| T. gondii | ||||||
| Cestoda, Taeniidae | Taenia saginata | Dung beetle | Poland | Unspecified | Experimental | Lonc 1980 [35] |
| Conoidasida, Sarcocystidae | Sarcocystis spp. | Fly | England | Dog Kennel | Natural | Markus 1980 [36] |
| Zoomastigophora, Hexamitidae | Giardia intestinalis | Cockroach Fly |
Poland | Open defecation area Waste disposal area |
Mixed | Kasprzak and Majewska 1981 * [37] |
| Chromadorea, Ascarididae | A. lumbricoides | Fly | Nigeria | School/University | Experimental | Dipeolu 1982 [38] |
| Chromadorea Ancylostomatidae | Hookworm (Unspecified) | |||||
| Cestoda, Taeniidae | Taenia hydatigena § | Fly | New Zealand | Farm/Field Laboratory |
Mixed | Lawson and Gemmell 1985 [39] |
| Chromadorea, Ascarididae | A. lumbricoides | Fly | Malaysia | Farm/Field Household Waste disposal area |
Natural | Sulaiman et al. 1988 [40] |
| Chromadorea Ancylostomatidae | Hookworm (Necator americanus) | |||||
| Enoplea, Trichuridae | T. trichiura | |||||
| Chromadorea, Ascarididae | A. lumbricoides | Fly | Malaysia | Household | Natural | Sulaiman et al. 1989 [41] |
| Chromadorea Ancylostomatidae | Hookworm (Necator americanus and/or Ancylostoma duodenale §) | |||||
| Enoplea, Trichuridae | T. trichiura | |||||
| Chromadorea, Ascarididae | A. lumbricoides (0.20–0.81%) | Fly | Nigeria | Food market Household |
Natural | Umeche and Mandah 1989 [42] |
| Chromadorea, Strongyloididae | Strongyloides stercoralis (0.40–1.80%) | |||||
| Chromadorea, Toxocaridae | T. canis (2.40–2.11%) | |||||
| Conoidasida, Sarcocystidae | T. gondii | Dung beetle | Japan | Laboratory School/University |
Mixed | Saitoh and Itagaki 1990 [43] |
| Chromadorea, Ascarididae | Ascaris spp. (72.8–82.4%) | Fly | Philippines | Urban area | Natural | Monzon et al. 1991 [44] |
| Enoplea, Capillariidae | Capillaria hepatica (0.0–0.005%) | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified; (0.02–13.1%) | |||||
| Cestoda, Taeniidae | Taenia spp. (0.005–0.02%) | |||||
| Chromadorea, Toxocaridae | Toxocara spp. (0.005–0.04%) | |||||
| Enoplea, Trichuridae | T. trichiura (18.8–60.1%) | |||||
| Archiacanthocephala, Moniliformidae | M. moniliformis | Cockroach | Scotland | Laboratory | Experimental | Stoddart et al. 1991 [45] |
| Conoidasida, Sarcocystidae | T. gondii | Cockroach | Costa Rica | Laboratory | Experimental | Chinchilla et al. 1994 [46] |
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. | Cockroach | Peru | Garden Household |
Natural | Zerpa and Huicho 1994 [47] |
| Chromadorea, Ascarididae | Ascaris spp. | Fly | Slovakia | Wastewater treatment area | Natural | Juris et al. 1995 * [48] |
| Enoplea, Capillariidae | Capillaria spp. | |||||
| Cestoda, Hymenolepididae | Hymenolepis spp. | |||||
| Cestoda, Taeniidae | Taenia spp. | |||||
| Chromadorea, Toxocaridae | Toxocara spp. | |||||
| Enoplea, Trichuridae | Trichuris spp. | |||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium parvum | Fly | United States | Laboratory | Experimental | Graczyk et al. 1999 [49] |
| Conoidasida, Cryptosporidiidae | C. parvum | Dung beetle | Czech Republic | Farm/Field Forest |
Experimental | Mathison and Ditrich 1999 [50] |
| Zoomastigophora, Hexamitidae | G. lamblia (22%) | Fly | Spain | Farm/Field | Natural | Doiz et al. 2000 [51] |
| Conoidasida, Cryptosporidiidae | C. parvum | Fly | United States | Farm/Field | Mixed | Graczyk et al. 2000 [52] |
| Palaeacanthocephala, Unspecified | Acanthocephala spp. | Fly | Brazil | Waste disposal area Zoo |
Natural | de Oliveira et al. 2002 * [53] |
| Chromadorea, Ascarididae. | Ascaris spp. | |||||
| Enoplea, Capillariidae | Capillaria spp. | |||||
| Chromadorea, Ascarididae. | Toxascaris spp. § | |||||
| Chromadorea, Toxocaridae | Toxocara spp. | |||||
| Chromadorea, Trichostrongylidae | Trichostrongylidae spp. | |||||
| Enoplea, Trichuridae | Trichuris spp. | |||||
| Chromadorea, Oxyuridae | Unspecified oxyuridae spp. | |||||
| Conoidasida, Cryptosporidiidae | C. parvum | Fly | United States | Farm/Field Food market Waste disposal area |
Natural | Graczyk et al. 2003 [54] |
| Zoomastigophora, Hexamitidae | G. lamblia | |||||
| Lobosa, Entamoebidae | Entamoeba histolytica/dispar (10.3–25.4%) | Cockroach | Taiwan | Kitchen area Laboratory School/University |
Mixed | Pai et al. 2003 [55] |
| Chromadorea, Oxyuridae | Enterobius vermicularis (3%) | Cockroach | United States | Hospital School/University |
Natural | Chan et al. 2004 [56] |
| Enoplea, Trichinellidae | Trichinella spp. (1.0%) | |||||
| Conoidasida, Cryptosporidiidae | C. parvum | Fly | United States Poland | Farm/Field Laboratory Waste disposal area |
Mixed | Graczyk et al. 2004 [57] |
| Conoidasida, Cryptosporidiidae | C. parvum | Fly | Poland | Farm/Field Waste disposal area |
Natural | Szostakowska et al. 2004 [58] |
| Zoomastigophora, Hexamitidae | G. lamblia | |||||
| Chromadorea, Ascarididae | A. lumbricoides | Cockroach | Nigeria | Household | Natural | Tatfeng et al. 2005 [59] |
| Litostomatea, Balantiididae | Balantidium coli | |||||
| Conoidasida, Cryptosporidiidae | C. parvum | |||||
| Lobosa, Entamoebidae | E. histolytica | |||||
| Chromadorea, Oxyuridae | E. vermicularis | |||||
| Chromadorea, Strongyloididae | S. stercoralis | |||||
| Enoplea, Trichuridae | T. trichiura | |||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (55.56%) | Fly | United States | Farm/Field Garden School/University |
Natural | Conn et al. 2007 [60] |
| Zoomastigophora, Hexamitidae | Giardia spp. (7.94%) | |||||
| Chromadorea, Ascarididae | A. lumbricoides | Fly | Ethiopia | Abattoir/Butchery/Slaughterhouse/ Food market Open defecation area Waste disposal area |
Natural | Getachew et al. 2007 [61] |
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. | |||||
| Lobosa, Entamoebidae | E. histolytica/dispar | |||||
| Zoomastigophora, Hexamitidae | G. lamblia | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified) | |||||
| Cestoda, Hymenolepididae | H. nana | |||||
| Chromadorea, Strongyloididae | S. stercoralis | |||||
| Cestoda, Taeniidae | Taenia spp. | |||||
| Enoplea, Trichuridae | T. trichiura | |||||
| Chromadorea, Ascarididae | A. lumbricoides | Cockroach | Ethiopia | Household | Natural | Kinfu and Erko 2008 [62] |
| Lobosa, Entamoebidae | E. histolytica/dispar | |||||
| Chromadorea, Oxyuridae | E. vermicularis | |||||
| Cestoda, Taeniidae | Taenia spp. | |||||
| Enoplea, Trichuridae | T. trichiura | |||||
| Chromadorea, Toxocaridae | T. canis | Cockroach | India | Kitchen area | Experimental | Sasmal et al. 2008 [63] |
| Chromadorea, Ascarididae | A. lumbricoides (36.9%) | Fly | Ethiopia | Abattoir/Butchery/Slaughterhouse/ Food market Waste disposal area |
Natural | Fetene and Worku 2009 [64] |
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (16.7%) | |||||
| Lobosa, Entamoebidae | E. histolytica/dispar (48.1%) | |||||
| Zoomastigophora, Hexamitidae | G. lamblia (10.4%) | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified; 13.0%) | |||||
| Cestoda, Hymenolepididae | H. nana (0.6%) | |||||
| Chromadorea, Strongyloididae | S. stercoralis (1.7%) | |||||
| Cestoda, Taeniidae | Taenia spp. (8.4%) | |||||
| Enoplea, Trichuridae | T. trichiura (38.8%) | |||||
| Chromadorea, Ascarididae | A. suum | Fly | Germany | Farm/Field Laboratory |
Mixed | Förster et al. 2009 [65] |
| Chromadorea, Metastrongylidae | Metastrongylus spp. § | |||||
| Chromadorea, Strongyloididae | Strongyloides ransomi § | |||||
| Enoplea, Trichuridae | Trichuris suis § | |||||
| Chromadorea, Gongylomatidae | Gongylonema spp. (17.7%) | |||||
| Chromadorea, Rhabditidae | Rhabditis spp. (2.2%) | |||||
| Chromadorea, Gongylomatidae | Gongylonema spp. (17.7%) | Dung beetle | Iran | Farm/Field | Natural | Mowlavi et al. 2009 [66] |
| Chromadorea, Rhabditidae | Rhabditis spp. (2.2%) | |||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (18.9%) | Fly | Poland | Farm/Field Waste disposal area |
Natural | Racewicz et al. 2009 * [67] |
| Chromadorea, Ascarididae | A. lumbricoides (0.3%) | Cockroach | Thailand | Food market | Natural | Chamavit et al. 2011 [68] |
| Litostomatea, Balantiididae | B. coli (5.8%) | |||||
| Bigyra, Blastocystidae | Blastocystis hominis (1.2%) | |||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (28.1%) | |||||
| Conoidasida, Eimeriidae | Cyclospora spp. (1.3%) § | |||||
| Lobosa, Entamoebidae | E. histolytica/dispar (4.6%) | |||||
| Chromadorea, Strongyloididae | S. stercoralis (0.8%) | |||||
| Cestoda, Taeniidae | Taenia spp. (0.1%) | |||||
| Enoplea, Trichuridae | T. trichiura (0.3%) | |||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. | Fly | Ethiopia | Abattoir/Butchery/Slaughterhouse/ Farm/Field Food market Open defecation area |
Mixed | Fetene et al. 2011 [69] |
| Unspecified | Unspecified helminths and protozoa | Fly | Brazil | Waste disposal area | Natural | Ribeiro et al. 2011 * [70] |
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. | Dung beetle | Australia | Unspecified | Experimental | Ryan et al. 2011 [71] |
| Chromadorea, Ascarididae |
Flies Ascaris spp. |
Fly Cockroach | Egypt | Household Open defecation area |
Natural | El-Sherbini and Gneidy 2012 [72] |
| Chromadorea, Oxyuridae | E. vermicularis | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified) | |||||
| Cestoda, Hymenolepididae | H. nana | |||||
| Enoplea, Trichuridae | T. trichiura | |||||
|
Cockroaches Unspecified parasitic agents |
||||||
| Chromadorea, Ascarididae | A. lumbricoides (34.08%) | Fly | Nigeria | Abattoir/Butchery/Slaughterhouse/ Food market Open defecation area Waste disposal area |
Natural | Adenusi and Adewoga 2013 [73] |
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (1.81%) | |||||
| Lobosa, Entamoebidae | E. histolytica/dispar (27.26%) | |||||
| Zoomastigophora, Hexamitidae | G. lamblia (3.34%) | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified; 20.45%) | |||||
| Cestoda, Hymenolepididae | H. nana (1.11%) | |||||
| Chromadorea, Strongyloididae | S. stercoralis (3.89%) | |||||
| Cestoda, Taeniidae | Taenia spp. (2.36%) | |||||
| Enoplea, Trichuridae | T. trichiura (25.87%) | |||||
| Chromadorea, Ascarididae | A. lumbricoides (52.2%) | Fly | Nigeria | Open defecation area Waste disposal area |
Natural | Adenusi and Adewoga 2013 [74] |
| Cestoda, Taeniidae | Taenia spp. (1.0%) | |||||
| Enoplea, Trichuridae | T. trichiura (47.2%) | |||||
| Chromadorea, Ascarididae | A. suum | Fly | Sweden | Laboratory | Experimental | Lalander et al. 2013 [75] |
| Chromadorea Ancylostomatidae | Hookworm (Ancylostoma duodenale) (4.9%) § | Cockroach | Ghana | Hospital | Natural | Tetteh-Quarcoo et al. 2013 [76] |
| Cestoda, Hymenolepididae | H. nana (1.6%) | |||||
| Cestoda, Taeniidae | Taenia spp. (1.6%) | |||||
| Chromadorea, Toxocaridae | Toxocara spp. | Fly | Thailand | Farm/Field Food market School/University Waste disposal area |
Natural | Bunchu et al. 2014 [77] |
| Chromadorea, Ascarididae | Ascaris spp. | Fly | Brazil | Farm/Field School/University |
Natural | Cruz Souza Lima et al. 2014 [78] |
| Lobosa, Entamoebidae | Entamoeba spp. | |||||
| Chromadorea, Oxyuridae | E. vermicularis | |||||
| Zoomastigophora, Hexamitidae | Giardia spp. | |||||
| Cestoda, Hymenolepididae | H. nana | |||||
| Cestoda, Taeniidae | Taenia spp. | |||||
| Enoplea, Trichuridae | Trichuris spp. | |||||
| Cestoda, Taeniidae | Taenia solium | Dung beetle | Peru | Farm/Field | Experimental | Gomez-Puerta et al. 2014 [79] |
| Chromadorea, Ascarididae | A. lumbricoides | Cockroach | Ethiopia | Household | Natural | Hamu et al. 2014 [80] |
| Litostomatea, Balantiididae | B. coli | |||||
| Lobosa, Entamoebidae | Entamoeba spp. | |||||
| Zoomastigophora, Hexamitidae | G. duodenalis | |||||
| Cestoda, Taeniidae | Taenia spp. | |||||
| Enoplea, Trichuridae | T. trichiura | |||||
| Unspecified Strongyloides-like nematodes | ||||||
| Chromadorea, Ascarididae | A. lumbricoides (2.9–13.2%) | Cockroach | Nigeria | Household | Natural | Isaac et al. 2014 [81] |
| Litostomatea, Balantiididae | B. coli (1.1–1.2%) | |||||
| Lobosa, Entamoebidae | E. histolytica (1.2–2.2%) | |||||
| Enoplea, Trichuridae | T. trichiura (4.4–4.7%) | |||||
| Unspecified coccidia spp. (3.3%) § | ||||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. | Fly | China | Farm/Field | Natural | Zhao et al. 2014 [82] |
| Zoomastigophora, Hexamitidae | Giardia spp. | |||||
| Chromadorea, Ascarididae | Ascaris spp. | Cockroach | Venezuela | Food market Hospital School/University |
Natural | Cazorla Perfetti et al. 2015 * [83] |
| Bigyra, Blastocystidae | Blastocystis spp. (82.9%) | |||||
| Conoidasida, Eimeriidae | Cyclospora spp. § | |||||
| Chromadorea, Oxyuridae | E. vermicularis | |||||
| Bigyra, Blastocystidae | Blastocystis spp. | Fly | Venezuela | Waste disposal area | Natural | Muñoz 2015 * [84] |
| Conoidasida, Eimeriidae | Cyclospora cayetanensis § | |||||
| Lobosa, Entamoebidae | E. histolytica | |||||
| Zoomastigophora, Hexamitidae | G. intestinalis | |||||
| Chromadorea, Toxocaridae | Toxocara spp. | |||||
| Chromadorea, Ascarididae | Ascaris spp. (33.76%) | Cockroach | Cameroon | Household | Natural | Atiokeng Tatang et al. 2017 [10] |
| Enoplea, Capillariidae | Capillaria spp. (6.16%) | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified; 4.86%) | |||||
| Chromadorea, Toxocaridae | Toxocara spp. (4.86%) | |||||
| Enoplea, Trichuridae | T. trichiura (11.97%) | |||||
| Bigyra, Blastocystidae | Blastocystis spp. (40.4%) | Cockroach | Malaysia | Food market Household Waste disposal area |
Natural | Farah et al. 2017 [85] |
| Chromadorea, Toxocaridae | T. canis | Cockroach | Mexico | Laboratory | Experimental | González-García et al. 2017 [86] |
| Unspecified | Amoeba spp. (25.4%) | Cockroach | Spain | Hospital Kitchen area School/University |
Natural | Martínez-Girón et al. 2017 [87] |
| Chromadorea, Ascarididae | A. lumbricoides (3%) | Cockroach | Turkey | Household | Natural | Oğuz et al. 2017 [88] |
| Bigyra, Blastocystidae | B. hominis (41%) | |||||
| Lobosa, Entamoebidae | E. histolytica/dispar (16.7%) | |||||
| Zoomastigophora, Hexamitidae | Giardia spp. (13.6%) | |||||
| Chromadorea, Toxocaridae | Toxocara spp. (3%) | |||||
| Chromadorea, Trichostrongylidae | Trichostrongylus spp. (1.5%) | |||||
| Enoplea, Trichuridae | T. trichiura (1.5%) | |||||
| Unspecified unsporulated coccidial oocyst (7.6%) § | ||||||
| Chromadorea, Ascarididae | A. lumbricoides (61.3%) | Cockroach | Nigeria | Household Kitchen area |
Natural | Adenusi et al. 2018 [89] |
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (13.85) | |||||
| Lobosa, Entamoebidae | E. histolytica/dispar (44.1%) | |||||
| Chromadorea, Oxyuridae | E. vermicularis (17.2%) | |||||
| Zoomastigophora, Hexamitidae | G. lamblia (18.7%) | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified; 11.6%) | |||||
| Cestoda, Hymenolepididae | H. nana (11.6%) | |||||
| Chromadorea, Strongyloididae | S. stercoralis (11.7%) | |||||
| Cestoda, Taeniidae | Taenia spp./Echinococcus spp. (10.5%) | |||||
| Enoplea, Trichuridae | T. trichiura (55.8%) | |||||
| Cestoda, Taeniidae | E. granulosus | Fly | Iran | Abattoir/Butchery/Slaughterhouse/ Farm/Field |
Mixed | Hemmati et al. 2018 [90] |
| Chromadorea, Toxocaridae | T. canis | Fly | Ukraine | Dog kennel | Natural | Paliy et al. 2018 [91] |
| Enoplea, Trichuridae | Trichuris vulpis | |||||
| Chromadorea, Ascarididae | A. suum | Fly | Ukraine | Farm/Field | Natural | Paliy et al. 2018 [92] |
| Chromadorea, Chabertiidae | Oesophagostomum dentatum § | |||||
| Enoplea, Trichuridae | T. suis § | |||||
| Bigyra, Blastocystidae | Blastocystis spp. | Fly | Venezuela | Unspecified | Natural | Valles et al. 2018 * [93] |
| Lobosa, Entamoebidae | E. histolytica/dispar | |||||
| Cestoda, Taeniidae | T. hydatigena § | Dung beetle | Peru | Farm/Field Village area |
Natural | Vargas-Calla et al. 2018 [94] |
| T. solium | ||||||
| Palaeacanthocephala, Unspecified | Acanthocephala spp. (0.67%) | Cockroach | Various | Farm/Field Pet store |
Natural | Gałęcki and Sokół 2019 [95] |
| Litostomatea, Balantiididae | Balantidium spp. (4.67%) | |||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (11.87%) | |||||
| Lobosa, Entamoebidae | Entamoeba spp. (4.53%) | |||||
| Chromadorea, Physalopteridae | Physaloptera spp. (3.07%) | |||||
| Cestoda, Unspecified | Unspecified cysticercoids (0.53%) | |||||
| Maxillopoda, Unspecified | Unspecified pentastomida spp. (0.67%) | |||||
| Chromadorea, Spiruridae | Unspecified spiruroidea spp. (1.87%) | |||||
| Chromadorea, Ascarididae | A. suum | Fly | Germany | Laboratory | Experimental | Muller et al. 2019 [96] |
| Chromadorea, Ascarididae | A. lumbricoides (5.9%) | Cockroach | Thailand | Food market | Natural | Dokmaikaw and Suntaravitun 2020 [97] |
| Litostomatea, Balantiididae | B. coli (1.1%) | |||||
| Bigyra, Blastocystidae | B. hominis (6.6%) | |||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (15.4%) | |||||
| Conoidasida, Eimeriidae | Cyclospora spp. (7.0%) § | |||||
| Lobosa, Entamoebidae | E. histolytica/dispar (8.5%) | |||||
| Chromadorea Ancylostomatidae | Hookworm (Unspecified; 2.2%) | |||||
| Chromadorea, Strongyloididae | S. stercoralis (4.4%) | |||||
| Cestoda, Taeniidae | Taenia spp. (5.1%) | |||||
| Chromadorea, Toxocaridae | Toxocara spp. (8.5%) | |||||
| Enoplea, Trichuridae | T. trichiura (6.3%) | |||||
| Bigyra, Blastocystidae | Blastocystis spp. (82.8%) | Cockroach | China | Zoo | Natural | Ma et al. 2020 [98] |
| Litostomatea, Balantiididae | B. coli (2.1%) | Cockroach | Spain | Household | Natural | van Woerden et al. 2020 [99] |
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (9%) | |||||
| Lobosa, Entamoebidae | Entamoeba spp. (12.7%) | |||||
| Unspecified coccidia spp. (8.4%) § | ||||||
| Conoidasida, Cryptosporidiidae | Cryptosporidium spp. (0.9%) | Fly | Mongolia | Household Kitchen area |
Natural | Barnes et al. 2021 [100] |
| Zoomastigophora, Hexamitidae | Giardia spp. (14.8%) | |||||
| Bigyra, Blastocystidae | Blastocystis spp. (2.1%) | Cockroach | Iran | Hospital | Natural | Motevalli-Haghi et al. 2021 [101] |
† Only parasites with a primary enteric transmission route were included; § Unrecognized but potential zoonotic risk; * Table information from the article’s English abstract/summary only; The underline in Table 1 refers to a group of many different species of parasites.
Zoonotic Enteric Parasites and Vectors Included in Review
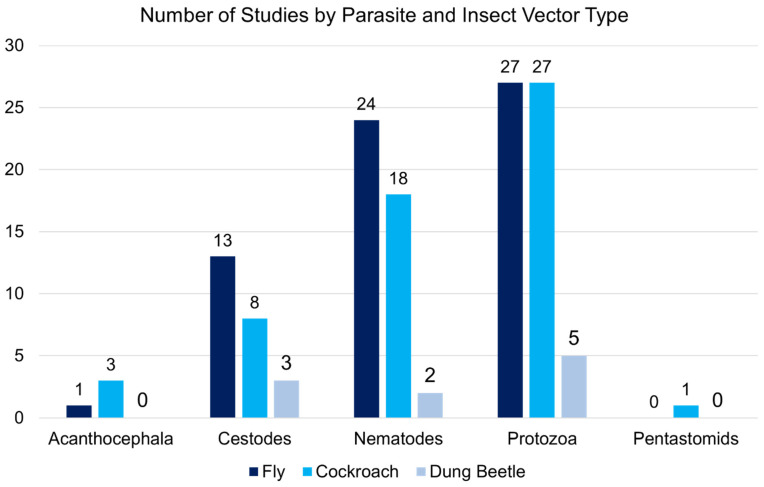
Most research was conducted on flies (n = 46), followed by cockroaches (n = 33) and dung beetles (n = 8). Two studies investigated two vectors at the same time (cockroaches and flies). The types of infection found in the insect vectors included natural (n = 49), experimental (n = 26), and mixed (n = 10). Parasites varied by different types and/or species classifications of the larval forms of protozoa (n = 8), the metacestodes stage (larva) of cestodes (n = 5), juvenile or larval nematodes (n = 14), acanthocephalans (n = 1), and pentastomids (n = 1). Protozoal species included Entamoeba histolytica (Schaudinn, 1903), Entamoeba dispar (Brumpt, 1925), Entamoeba moshkovskii (Tshalaia, 1941), Balantidium coli (Malmsten, 1857), Cryptosporidium parvum (Tyzer, 1912), Giardia lamblia (Kofoid and Christiansen, 1915) and Giardia intestinalis (Lambl, 1859), Toxoplasma gondii (Nicolle and Manceaux, 1908), Sarcocystis muris (Miescher, 1843), Cyclospora cayetanensis (Ortega, Gilman and Sterling, 1994), and Blastocystis hominis (Alexieff, 1911). Cestode species mentioned in the studies were Echinococcus granulosus (Batsch, 1786), Taenia saginata (Goeze, 1782), Taenia hydatigena (Pallas, 1766), Taenia solium (Linnaeus, 1758), Dipylidium caninum (Linnaeus, 1758), Hymenolepis nana (Bilharz, 1851), Hymenolepis diminuta (Rudolphi, 1819), and Mesocestoides lineatus (Goeze, 1782). Many species of nematodes were described in the included studies such as Ancylostoma duodenale (Dubini, 1843), Necator americanus (Stiles, 1902), Trichuris suis (Schrank, 1788), Trichuris vulpis (Froelich, 1789), Trichuris trichiura (Linnaeus, 1771), Ascaris lumbricoides (Linnaeus, 1758), Ascaris suum (Goeze, 1782), Baylisascaris procynois (Stefanski and Zarnowski, 1951), Toxascaris leonine (von Linstow, 1902), Toxocara canis (Werner, 1782), Toxocara cati (Schrank, 1788), Trichinella spiralis (Owen, 1835), Physaloptera turgida (Rudolphi, 1819), Capillaria hepatica (Bancroft, 1893), Strongyloides stercoralis (Bavay, 1876), Strongyloides ransomi (Schwartz and Alicata, 1930), Setaria equina (Abildgaard, 1789), Syphacia obvelata (Rudolphi, 1802), Enterobius vermicularis (Linnaeus, 1758), and Oesophagostomus dentatum (Rudolphi, 1803). An acanthocephalan species, Moniliformis (Bremser, 1811) was also named in the study results. The number of studies also varied by insect vector and parasite category, with most of the work investigating protozoa and nematodes in flies and cockroaches (Figure 2).
Figure 2.
Number of included studies conducted on each insect vector by parasite category.
Many fly species were examined for zoonotic enteric parasites, particularly flies of public health importance from the Muscidae, Sarcophagidae, and Calliphoridae families. The vector fly species most often identified in the included titles was Musca domestica (Linnaeus, 1758). Additional fly species commonly studied among the included titles were Chrysomya megacephala (Fabricius, 1794), Musca sorbens (Wiedemann, 1830), Stomoxys calcitrans (Bishop, 1913), Lucilia cuprina (Meigen, 1826), and Calliphora vicina (Robineau-Desvoidy, 1830).
Studies detailing the most common species of pathogens found on or in filth flies included: Ascaris spp. (n = 19), Trichuris spp. (n = 16), Giardia spp. (n = 13), Cryptosporidium spp. (n = 13), intestinal or non-specific hookworm (n = 10), Taenia spp. (n = 8), Hymenolepis spp. (n = 7), Entamoeba spp. (n = 7), Toxocara spp. (n = 9), and T. gondii (n = 3). The specimen locations of the fly samples were largely farms and/or pastures and fields (n = 16), waste disposal areas (n = 15), open markets and other food markets (n = 8), slaughterhouses or animal butcher areas (n = 6), households (n = 6), and schools and/or universities (n = 4). However, many included titles had received or reared fly samples in laboratory settings (n = 14).
While several species of cockroach were investigated among the titles for the presence of zoonotic enteric parasites, the two most common species examined in the included titles in this study were the German cockroach (Blattella germanica; Linnaeus, 1767) and the American cockroach (Periplaneta americana; Linnaeus, 1758). However, additional species were also studied such as Periplaneta brunnea (Burmeister, 1838), the Cuban burrowing cockroach (Byrsotria fumigata; Guérin-Méneville, 1857), the Madagascar hissing cockroach (Gromphadorhina portentosa; Schaum, 1853), the North American wood roach (Paracoblatta spp.), the oriental cockroach (Blatta orientalis; Linnaeus, 1758), the Turkestan cockroach (Shelfordella lateralis; Walker, 1868), the Australian cockroach (Periplaneta australasiae; Fabricius, 1775), the speckled cockroach (Nauphoeta cinerea; Oliver, 1789), among others.
Within the studies, parasitic pathogens were examined in or on cockroaches. These studies documented the Ascaris spp. (n = 12), Trichuris spp. (n = 10), Entamoeba spp. (n = 13), Cryptosporidium spp. (n = 7), Blastocystis spp. (n = 7), Taenia spp. (n = 6; one study may have also been Echinococcus spp.), Balantidium coli (n = 6), Toxocara spp. (n = 6), Strongyloides spp. (n = 5; in one study listed as Strongyloides-like nematodes), intestinal or non-specific hookworm (n = 4), Giardia spp. (n = 4), Hymenolepis spp. (n = 4), and T. gondii (n = 4). Cockroach specimens largely came from households (n = 11), specifically kitchen areas of living spaces (n = 4), hospitals (n = 5), open markets and other food markets (n = 4), schools/universities (n = 4). Many titles used cockroach specimens reared in laboratories (n = 8).
Several species of the dung beetle were studied by the included titles to determine if they could harbor, and potentially spread, zoonotic enteric parasites. The dung beetles were from the Scarabaeidae and Geotrupidae families, which primarily feed on fecal or decaying matter. Species came from the Onthophagus genus (e.g., O. fracticornis; Preyssler, 1790), the Bubas genus (e.g., B. bison; Linnaeus, 1767), the Aphodius genus including A. rufus (Moll, 1782) and A. fimetarius (Linnaeus, 1758), and the Anoplotrupes genus (e.g., A. stercorosus; Scriba, 1791), among others.
Within the titles that examined dung beetles, several parasite pathogens were found to have positive results. These zoonotic enteric parasites found on dung beetles included: Taenia spp. (n = 4), Cryptosporidium spp. (n = 2), Ascaris spp. (1), intestinal hookworm (n = 1), Trichuris spp. (n = 1), Gongylonema spp. (n = 1), and Rhabditis spp. (n = 1). Dung beetle samples were largely collected from farms, pastures, and fields (n = 5). The studies investigated natural infection (n = 2), used experimental design (n = 5), or a mixed-method approach (n = 1).
Numerous risk factors were mentioned for human and/or animal infection or exposure to zoonotic enteric parasites through insect vectors (Table 2). These included poor or inadequate water and sanitation services at home or in the community space (n = 27), having an open defecation site (n = 12) or unmanaged animal waste (n = 16) nearby, insufficient environmental hygiene or the absence of services such as garbage removal (n = 26), seasonal or climatic conditions preferred by the insect vector (n = 14), improper and unsafe food hygiene and storage (n = 23), insect behaviors and feeding practices (n = 29), direct animal contact (n = 22), and ingestion of infected vectors (n = 9).
Table 2.
Risk factors for exposure to and/or transmission of zoonotic enteric parasites from flies, cockroaches, or dung beetles, as addressed in the included studies.
| Risk Factor | Citations |
|---|---|
| Inadequate water and sanitation services or infrastructure at household or community level | [10,18,19,21,23,33,37,38,40,41,42,44,52,54,59,61,64,70,72,73,74,75,78,81,82,89,100] |
| Open defecation site near human or animal activities | [10,18,23,40,43,44,61,64,69,72,74,81] |
| Unmanaged animal waste near human or animal activities | [10,26,28,31,36,40,43,44,46,50,60,66,74,81,94,100] |
| Poor environmental hygiene, overcrowding, open slaughter, and/or a lack of garbage removal and processing services | [35,38,40,41,42,44,47,52,54,55,58,64,67,70,72,73,74,76,78,81,82,84,88,89,91,100] |
| Seasonality and environmental conditions for insect vector proliferation | [18,28,29,38,39,40,41,62,69,71,82,90,91,97] |
| Unsafe food preparation, storage, sale, and/or service | [19,20,21,26,29,33,38,40,46,54,55,57,62,63,68,69,72,73,81,85,90,101] |
| Insect vector feeding behaviors and preferences, movement patterns, and living habitat predilection | [19,29,30,31,34,35,39,43,46,49,52,54,55,57,59,60,61,64,71,72,73,76,79,85,86,88,90,97,101] |
| Animal contact, husbandry, and proximity to living spaces | [10,18,20,21,26,28,42,44,46,47,50,52,53,57,60,65,66,90,91,94,98,100] |
| Purposeful or accidental ingestion of contaminated insect vector by animals or humans | [25,30,34,56,66,72,75,95,96] |
4. Discussion
This review highlights the risk of ZEP transmission from insect vectors of interest, including flies, cockroaches, and dung beetles. Flies and cockroaches represent a significant hazard of being exposed to parasites in households and community spaces due to their synanthropic nature [1]. Close cohabitation with humans, especially in the household setting, poses an increased risk of transmission of ZEPs that can be compounded by other factors such as poor sanitation and hygiene. Alternatively, while dung beetles have demonstrated the capability to harbor parasites of public health concern, their preferences for pastures, forest floors, and other natural habitats, coupled with their species-specific dung removal patterns, could actually be of benefit in the removal of zoonotic parasites from the environment [102,103].
The included studies in this review were largely centered on filth flies, which feed and reproduce via human and animal fecal waste as well as through organic waste and garbage [6,7]. Similar to cockroaches, they are drawn to human food items where they may deposit parasitic organisms they have collected via external or internal contamination [1,7]. The mechanical transmission of ZEPs from these insect vectors in food preparation areas are a danger to health and safety in a variety of settings such as homes, restaurants, and hospitals. Food contamination from these insect vectors may be a neglected global threat to human and animal health.
4.1. Protozoa
Many species of zoonotic protozoa were found naturally occurring within the insect vectors examined in the included titles. Additionally, experimental and mixed-methods study designs demonstrated additional vector potential for protozoal transmission. Cockroaches were found to be naturally contaminated with Balantidium spp. [59,68,80,81,95,97,99]. They also harbored the Blastocystis spp. [68,83,84,85,88,93,97,98,101]. One title discussed the presence of Blastocystis spp. in cockroaches, but the primary data were presented in a previous study not available in our search results [104,105]. Both cockroach and fly vectors were found to harbor the Cryptosporidium spp. (cockroach: [47,59,68,89,95,97,99]; fly: [54,58,60,61,64,67,73,82,100]). However, dung beetles were only infected experimentally [50,71]. Entamoeba spp. were also found in cockroaches and flies (cockroach: [59,62,68,80,81,87,88,89,95,97,99]; fly: [61,64,73,78,84,93]). Contamination with Giardia spp. among flies and cockroaches were common in the included publications (fly: [33,51,54,58,60,61,64,73,78,82,84,100]; cockroach: [80,88,89]). Oocysts from Sarcocystis spp. protozoal parasites were found in cockroaches and flies (cockroach: [34]; fly: [36]). Toxoplasma gondii was found in cockroaches, flies, and dung beetles, but only through experimental infection (fly: [22,24,26]; dung beetle: [43]; cockroach: [28,31,34,46]).
4.2. Cestodes
The insect vectors were found to be naturally contaminated with parasitic worms from the Cestoda class. Flies and cockroaches were found to have naive infection with Hymenolepis spp. (fly: [48,61,64,72,73,78]; cockroach: [76,89]). Taenia spp. were reported in flies, cockroaches, and dung beetles (fly: [44,48,61,64,73,74,78]; cockroach: [62,68,76,80,95,97]; dung beetle: [94]). Experimental studies showed that flies were also able to harbor Echinococcus spp. [20,21,90]. This may have also been true for cockroaches [89]. Moreover, a cockroach was experimentally infected with the D. caninum and Mesocestoides spp. [30].
4.3. Nematodes
The included studies most frequently found parasitic roundworms naturally present in the insect vectors. Ascaris spp. were reported in cockroaches and flies (cockroach: [10,18,59,68,80,81,83,88,89,97]; fly: [33,40,41,42,44,48,53,61,62,64,72,73,74,78,92]). In addition, flies and cockroaches were found with Capillaria spp. infection (fly: [44,48,53]; cockroach: [10]). Pinworm, or E. vermicularis, and other Oxyuridae spp. were found naturally occurring in cockroaches and flies (cockroach: [56,59,62,83,89]; fly: [53,72,78]). Cockroaches were also experimentally infected with the rat pinworm S. obvelata [30]. Dung beetles were reported to carry Gongylonema spp. [66]. Intestinal hookworms were discovered inside or on the outside of flies and cockroaches (fly: [33,40,41,44,61,64,72,73]; cockroach: [10,76,89,97]). Cockroaches had naïve infections with Physaloptera spp. and Spiruroidea spp. [95]. Strongyloides spp. and Strongyloides-like nematodes spp. were reported in flies and cockroaches (fly: [42,61,64,73]; cockroach: [59,68,80,89,97]). Fly and cockroach vectors were also harboring Toxocara spp. (fly: [42,44,48,53,77,84,91]; cockroach; [10,88,97]). Natural cockroach infection with Trichinella spp. was reported in the included studies [56]. Additionally, natural Trichostrongylidae spp. infection was reported in flies and cockroaches (fly: [53]; cockroach: [88]). Trichuris spp. was also found in fly and cockroach vectors (fly: [33,40,41,44,48,53,61,64,72,73,74,78,91]; cockroach: [10,59,62,68,80,81,88,89,97]).
4.4. Acanthocephala and Pentastomida
Both cockroach and fly vectors were found to be naturally infected with the Acanthocephala spp. (fly: [53]; cockroach: [32,95]). Moreover, cockroaches demonstrated natural infection with Pentastomida spp. [95].
4.5. Parasites of Potential Zoonotic Concern
Within the included studies, several species of enteric parasites that were investigated have a possible, or even probable, zoonotic transmission risk. They include the Cyclospora spp., which were found to be naturally occurring in cockroaches and flies (cockroach: [68,81,83,88,97,99]; fly: [84]). O. dentatum and T. suis were found in fly samples [92]. Dung beetles were naturally contaminated with T. hydatigena [94]. Additional experimental infection of the insect vectors with Metastrongylus spp., P. turgida, S. equina, S. ransomi, and T. leonina also yielded positive results [30,65].
4.6. Non-Pathogenic and Non-Zoonotic Organisms
In addition to the pathogenic agents found in the vectors, several of the included studies found non-pathogenic protozoa and flagellate. These organisms often indicate that the vector has had fecal exposure. Entamoeba coli (Grassi, 1879) was found in cockroaches, flies, and dung beetles [23,33,61,62,64,68,73,78,84,88,93,97]. Entamoeba hartmanni (Prowazek, 1912) was listed in a cockroach study [93]. Iodamoeba bütschlii (Prowazek, 1912) was also found in flies and cockroaches [68,78,88,93,97]. Endolimax nana (Wenyon and O’Connor, 1817) was found in dung beetles, cockroaches, and flies [23,68,84,88,93,97]. Cockroaches demonstrated naïve infection with the flagellate Chilomastix mesnili (Wenyon, 1910) [68,88,97].
Using the term zoonoses defined as diseases transmitted between humans and vertebrate animals, several pathogens that were found in the insect vectors but do not cause human infection or disease were excluded from the results table [106]. Those included Cystoisopora and Isospora spp., Gregarina spp., Hydatigera (Taenia) taeniaeformis (Batsch, 1786), Hammerschmidtiella diesigni (Hammerschmidt, 1838), Lophomonas battaturm (Stein, 1860), Nyctotherus spp., Pharyngodon spp., and Thelastoma spp. [30,34,43,83,87,93,95,97,99,101]. The inclusion criteria also required that the mode of transmission for the parasite be gastrointestinal, so that it could be considered an enteric parasite. This also excluded Ascaridia galli (Schrank, 1758), Leptomonas spp., Pentatrichomonas spp., and extraintestinal hookworm such as Ancylostoma caninum (Ercolani, 1859) and Uncinaria spp. [30,42,83,91,93]. Further investigation into the potential role these organisms have in the global parasitic burden of humans and animals is warranted.
4.7. Sampling Locations and Risk Factors for Exposure
The insect vectors analyzed in the included studies originated from natural environments or were reared in laboratory settings. Overall, fly and cockroach insect vectors were collected from farms, pastures, open fields, and nearby livestock housing (i.e., barns) [39,40,51,52,54,57,58,60,65,67,69,78,82,90,92,95,100]. Fly samples were also drawn from village areas or areas of human habitation such as near kitchens, hospitals, food markets, and schools [27,33,38,40,41,42,43,44,54,60,61,64,69,72,73,77,78,100]. Nevertheless, many fly samples were collected near areas with a high risk of environmental contamination such as slaughterhouses/butchers and abattoirs, open defecation sites, and waste disposal or wastewater treatment areas [33,37,40,48,53,54,57,58,61,64,67,69,70,72,73,74,77,84,90]. Some fly specimens were also sampled from areas of public transportation, dog kennels, and from a zoo [33,36,53,91].
Cockroach specimens were also gathered from villages or household settings or human habitats [10,18,32,37,47,55,56,59,62,63,68,72,76,80,81,83,85,87,88,89,97,99,101]. Cockroach samples were also collected from a zoo and a pet store [95,98]. Dung beetles were sampled from wild settings of farms, pastures, forests, and fields [23,50,66,79]. However, one study did examine dung beetles in a village area [94]. Many studies used laboratory insect specimens for their analysis of parasite exposure and vector competence [19,20,21,22,24,25,26,27,28,29,30,34,39,43,45,46,49,57,65,75,86,96].
The authors of the studies identified water, sanitation, and hygiene-related risk factors that were associated with parasite presence in insect vectors, or were likely to increase the potential for parasite exposure and transmission. Inadequate or unsafe drinking water and sanitation services, infrastructure, and behaviors across individual, household, and community levels may contribute to the spread of ZEPs due to contact with, or food contamination from, flies and cockroaches [10,18,19,21,23,33,37,38,40,41,42,44,52,54,59,61,64,70,72,73,74,75,78,81,82,89,100]. Within the larger environment where a household is located, such as within a neighborhood, village, or municipality, potential drivers of ZEP transmission from insect vectors can result from open animal slaughterhouses, garbage and domestic waste piling up without regular removal, overcrowding, and insufficient or unsafe housing structures [35,38,40,41,42,44,47,52,54,55,58,64,67,70,72,73,74,76,78,81,82,84,88,89,91,100]. In particular, unmanaged, improperly stored, or untreated human waste within our living spaces, such as open defecation sites, may spread zoonotic enteric parasites through insect vectors [10,18,23,40,43,44,61,64,69,72,74,81]. Additionally, animal waste near human habitats is also a likely driver of ZEP transmission from insect vectors as they are contaminated by their contact with the human or animal waste for feeding and breeding [10,26,28,31,36,40,43,44,46,50,60,66,74,81,94,100]. Animal-related activities and husbandry in general could serve as a source of contamination for insects and people nearby as well as the animals themselves [10,18,20,21,26,28,42,44,46,47,50,52,53,57,60,65,66,90,91,94,98,100].
Several of studies mentioned that seasonality and environmental conditions such as rainfall, heat, and humidity could also contribute to the proliferation of the insect vectors and therefore increase the risk of exposure to ZEPs by humans and animals [18,28,29,38,39,40,41,62,69,71,82,90,91,97]. Moreover, the specific vector feeding, breeding, and habitat preferences coupled with their food predilections could also increase the risk of ZEP transmission [19,29,30,31,34,35,39,43,46,49,52,54,55,57,59,60,61,64,71,72,73,76,79,85,86,88,90,97,101]. The movements and behaviors of the insects should be considered, especially regarding food contamination. Unsafe food storage, preparation, and sale or service can transmit ZEPs to people and animals after contamination from a vector such as flies or cockroaches [19,20,21,26,29,33,37,38,40,46,54,55,57,62,63,68,69,72,73,81,85,90,101]. Furthermore, using insects as a food source for humans or animals, whether purposely or accidentally, can also present the risk of ZEP exposure [25,30,34,56,66,72,75,95,96].
4.8. Recommendations
One Health studies that simultaneously investigate parasite presence in humans, animals, food, and environmental reservoirs and vectors can demonstrate which groups and exposure pathways may be the biggest threat. For example, a recent publication conducted by a member of this research team found the zoonotic enteric parasites Cryptosporidium spp. and Giardia spp. among human, animals, flies, and drinking water in households in Mongolia [100]. The highest prevalence rate was round in the fly vectors (14.8%). This information, coupled with a household risk factor survey, demonstrated an association between ZEP presence and unimproved drinking water, not having a handwashing site at the home, domestic animal ownership, and rural location [100]. Researchers Dehghani and Kassiri even presented a question regarding the possible role of flies and cockroaches in the ongoing COVID-19 (SARS-CoV-2) pandemic due to their potential for environmental contamination [107]. More holistic research into water, sanitation, and hygiene (WASH) services and behaviors as well as food safety in personal and community spaces in connection with the prevalence of zoonotic enteric parasites in people, animals, and insect vectors who share these environments can shed light on how and where exposures are occurring. Armed with more robust One Health contexts for ZEP transmission routes, public and veterinary health professionals can collaborate with community members on targeted prevention and control efforts.
4.9. Limitations
This review identified studies of ZEPs in cockroaches, filth flies, and dung beetles from all over the world, yet due to the authors’ language barriers and lack of qualified translators, only English titles had the full text assessed. English abstracts from several titles illustrated parasite prevalence in vectors of interest and when possible, were included in the final analysis. However, the authors believe that valuable and important work in this subject area is likely to be available in additional languages and found through searching supplemental databases and sources. Furthermore, it is likely that titles of importance were left out of the results due to our search and screening parameters. For example, in one title, the authors spoke of a ZEP in cockroaches but referenced the initial presence data from another source that did not appear in our database results [104,105].
The breadth of parasites analyzed in the included studies demonstrate a wide range of species and hosts. In an effort to outline each pathogen, epidemiological details associated with every parasite were omitted. Information on exposure pathways and disease presentation associated with these zoonotic diseases would be helpful for public health professionals, veterinarians, and medical entomologists tasked with using this review for action against ZEP transmission. Similarly, validated information on the current systematic taxa of the pathogens included in the studies could be of further assistance in understanding more about these zoonotic enteric parasites.
5. Conclusions
One Health research collaboration is needed to build a better global assessment of ZEPs in insect vectors and the risks posed to human, animal, and environmental health. Implementing a joint approach to tackle these complex exposure pathways using experts and stakeholders in the disciplines of public health, epidemiology, veterinary sciences, biology, medical entomology, environmental health, and more can lead to targeted public and veterinary health education messages for the prevention and control of zoonotic enteric parasites.
Acknowledgments
The researchers would like to thank Austin C. Sprunger and Alisa Craddock, Library Research Associates at the UNF Thomas G. Carpenter Library, for their assistance and support in tracking down articles for this review.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pathogens11010090/s1, Table S1: Search Strings and Results by Database.
Author Contributions
Conceptualization, A.P., M.J., K.R. and A.N.B.; methodology, A.N.B.; investigation, A.P., M.J., K.R. and A.N.B.; resources, A.N.B.; data curation, A.P., M.J., K.R. and A.N.B.; writing—original draft preparation, A.P., M.J., K.R. and A.N.B.; writing—review and editing, A.P. and A.N.B.; supervision, A.N.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All of the data used in this study are openly available.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Graczyk T.K., Knight R., Tamang L. Mechanical transmission of human protozoan parasites by insects. Clin. Microbiol. Rev. 2005;18:128–132. doi: 10.1128/CMR.18.1.128-132.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hadi A.M. Study of Flyborne Parasites (Brachycera): A Review. Plant Arch. 2020;20:2419–2429. [Google Scholar]
- 3.Hayati R.Z., Susanna D. The Human Pathogens Carried by the Cockroaches in the Food-Related Environment Potentially Causing a Foodborne Diseases: A Systematic Review. Malays. J. Public Health Med. 2020;20:159–170. doi: 10.37268/mjphm/vol.20/no.2/art.271. [DOI] [Google Scholar]
- 4.Nichols E., Gomez A. Dung beetles and fecal helminth transmission: Patterns, mechanisms and questions. Parasitology. 2014;141:614–623. doi: 10.1017/S0031182013002011. [DOI] [PubMed] [Google Scholar]
- 5.Khamesipour F., Lankarani K.B., Honarvar B., Kwenti T.E. A systematic review of human pathogens carried by the housefly (Musca domestica L.) BMC Public Health. 2018;18:1049. doi: 10.1186/s12889-018-5934-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . The Housefly: Training and Information Guide. World Health Organization; Geneva, Switzerland: 1991. No. WHO/VBC/90.987. [Google Scholar]
- 7.Rozendaal J.A. Vector Control: Methods for Use by Individuals and Communities. World Health Organization; Geneva, Switzerland: 1997. [Google Scholar]
- 8.Olsen A.R. Regulatory action criteria for filth and other extraneous materials: III. Review of flies and foodborne enteric disease. Regul. Toxicol. Pharmacol. 1998;28:199–211. doi: 10.1006/rtph.1998.1271. [DOI] [PubMed] [Google Scholar]
- 9.Graczyk T.K., Knight R., Gilman R.H., Cranfield M.R. The role of non-biting flies in the epidemiology of human infectious diseases. Microbes Infect. 2001;3:231–235. doi: 10.1016/S1286-4579(01)01371-5. [DOI] [PubMed] [Google Scholar]
- 10.Atiokeng Tatang R., Tsila H., Wabo Poné J. Medically important parasites carried by cockroaches in Melong Subdivision, Littoral, Cameroon. J. Parasitol. Res. 2017;2017:7967325. doi: 10.1155/2017/7967325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zahraei-Ramazani A.R., Saghafipour A., Vatandoost H. Control of American cockroach (Periplaneta americana) in municipal sewage disposal system, Central Iran. J. Arthropod-Borne Dis. 2018;12:172. doi: 10.18502/jad.v12i2.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donkor E.S. Cockroaches and food-borne pathogens. Environ. Health Insights. 2020;14:1178630220913365. doi: 10.1177/1178630220913365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doi H., Gałęcki R., Mulia R.N. The merits of entomophagy in the post COVID-19 world. Trends Food Sci. Technol. 2021;110:849–854. doi: 10.1016/j.tifs.2021.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramírez-Restrepo L., Halffter G. Copro-necrophagous beetles (Coleoptera: Scarabaeinae) in urban areas: A global review. Urban Ecosyst. 2016;19:1179–1195. doi: 10.1007/s11252-016-0536-2. [DOI] [Google Scholar]
- 15.Nichols E., Alarcón V., Forgie S., Gomez-Puerta L.A., Jones M.S. Coprophagous insects and the ecology of infectious diseases of wildlife. ILAR J. 2017;58:336–342. doi: 10.1093/ilar/ilx022. [DOI] [PubMed] [Google Scholar]
- 16.Barnes A.N., Davaasuren A., Baasandagva U., Gray G.C. A systematic review of zoonotic enteric parasitic diseases among nomadic and pastoral people. PLoS ONE. 2017;12:e0188809. doi: 10.1371/journal.pone.0188809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chandler A.C. Some factors affecting the propagation of hookworm infections in the Asansol mining settlement, with special reference to the part played by cockroaches in mines. Indian Med. Gaz. 1926;61:209. [PMC free article] [PubMed] [Google Scholar]
- 19.Roberts E.W. The part played by the faeces and vomit-drop in the transmission of Entamoeba histolytica by Musca domestica. Ann. Trop. Med. Parasitol. 1947;41:129–142. doi: 10.1080/00034983.1947.11685318. [DOI] [PubMed] [Google Scholar]
- 20.Schiller E.L. Studies on the helminth fauna of Alaska. XIX. An experimental study on blowflow (Phormia regina) transmission of hydatid disease. Exp. Parasitol. 1954;3:161–166. doi: 10.1016/0014-4894(54)90005-3. [DOI] [PubMed] [Google Scholar]
- 21.Heinz H., Brauns W. The Ability of Plies to transmit Ova of Echinococcus granulosus to Human Foods. S. Afr. J. Med. Sci. 1955;20:131–132. [PubMed] [Google Scholar]
- 22.Laarman J. Transmission of experimental toxoplasmosis by Stomoxys calcitrans. Doc. Med. Geogr. Trop. 1956;8:293–298. [PubMed] [Google Scholar]
- 23.Miller A., Chi-Rodriguez E., Nichols R.L. The fate of helminth eggs and protozoan cysts in human feces infested by dung beetles (Coleoptera: Scarabaeidae) Am. J. Trop. Med. Hyg. 1961;10:748–754. doi: 10.4269/ajtmh.1961.10.748. [DOI] [PubMed] [Google Scholar]
- 24.Paim G., Queiroz J. The Ability of Musca domestica to carry Toxoplasma gondii. Arch. Fac. Hig. Saude Publ. Univ. S. Paulo. 1963;28:213–216. [PubMed] [Google Scholar]
- 25.Pegg E.J. Infection of dogs by Toxocara canis carried by flies. Parasitology. 1971;62:409–414. doi: 10.1017/S0031182000077568. [DOI] [PubMed] [Google Scholar]
- 26.Wallace G.D. Experimental transmission of Toxoplasma gondii by filth-flies. Am. J. Trop. Med. Hyg. 1971;20:411–413. doi: 10.4269/ajtmh.1971.20.411. [DOI] [PubMed] [Google Scholar]
- 27.Nadzhafov I.G. Role of flies in the epidemiology of human helminthiases in the Azerbaijan SSR. Med. Parazitol. 1972;41:168–172. [PubMed] [Google Scholar]
- 28.Wallace G.D. Experimental transmission of Toxoplasma gondii by cockroaches. J. Infect. Dis. 1972;126:545–547. doi: 10.1093/infdis/126.5.545. [DOI] [PubMed] [Google Scholar]
- 29.Young P. Investigations on experimental transmission of Trichinella spiralis between rodents and cockroaches. Proc. La. Acad. Sci. 1974;37:54–59. [Google Scholar]
- 30.Young P.L. Studies on the transmission of helminth ova by cockroaches. Proc. Okla. Acad. Sci. 1975;55:169–174. [Google Scholar]
- 31.Chinchilla M., Ruiz A. Cockroaches as possible transport hosts of Toxoplasma gondii in Costa Rica. J. Parasitol. 1976;62:140–142. doi: 10.2307/3279075. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez J., Mishra G. Spontaneous parasitism of cockroach (insecta dictyoptera) in Tunis. Their part as an intermediate host of Mastophorus muris (Gmelin 1970) and Moniliformis moniliformis (Bremser 1811) Arch. L’institut Pasteur Tunis. 1976;53:211–238. [Google Scholar]
- 33.Khan A., Huq F. Disease agents carried by flies in Dacca city. Bangladesh Med. Res. Counc. Bull. 1978;4:86–93. [PubMed] [Google Scholar]
- 34.Smith D.D., Frenkel J. Cockroaches as vectors of Sarcocystis muris and of other coccidia in the laboratory. J. Parasitol. 1978;64:315–319. doi: 10.2307/3279682. [DOI] [PubMed] [Google Scholar]
- 35.Lonc E. The possible role of the soil fauna in the epizootiology of cysticercosis in cattle. II. Dung beetles—A biotic factor in the transmission of Taenia saginata eggs. Angew. Parasitol. 1980;21:139–144. [PubMed] [Google Scholar]
- 36.Markus M.B. Flies as natural transport hosts of Sarcocystis and other coccidia. J. Parasitol. 1980;66:361–362. doi: 10.2307/3280842. [DOI] [PubMed] [Google Scholar]
- 37.Kasprzak W., Majewska A. Transmission of Giardia cysts. I. The role of flies and cockroaches. Wiad. Parazytol. 1981;27:555–563. [PubMed] [Google Scholar]
- 38.Dipeolu O. Laboratory investigations into the role of Musca vicina and Musca domestica in the transmission of parasitic helminth eggs and larvae. Int. J. Zoonoses. 1982;9:57–61. [PubMed] [Google Scholar]
- 39.Lawson J., Gemmell M. The potential role of blowflies in the transmission of taeniid tapeworm eggs. Parasitology. 1985;91:129–143. doi: 10.1017/S0031182000056572. [DOI] [PubMed] [Google Scholar]
- 40.Sulaiman S., Sohadi A.R., Yunus H., Iberahim R. The role of some cyclorrhaphan flies as carriers of human helminths in Malaysia. Med. Vet. Entomol. 1988;2:1–6. doi: 10.1111/j.1365-2915.1988.tb00043.x. [DOI] [PubMed] [Google Scholar]
- 41.Sulaiman S., Sohadi A.R., Jeffery J. Human helminth parasite burdens on cyclorrhaphan flies (Diptera) trapped at an aboriginal settlement in Malaysia. Bull. Entomol. Res. 1989;79:625–629. doi: 10.1017/S0007485300018770. [DOI] [Google Scholar]
- 42.Umeche N., Mandah L. Musca domestica as a carrier of intestinal helminths in Calabar, Nigeria. East Afr. Med. J. 1989;66:349–352. [PubMed] [Google Scholar]
- 43.Saitoh Y., Itagaki H. Dung Beetles, Onthophagus spp., as Potential Transport Hosts of Feline Coccidia. Jpn. J. Vet. Sci. 1990;52:293–297. doi: 10.1292/jvms1939.52.293. [DOI] [PubMed] [Google Scholar]
- 44.Monzon R., Sanchez A., Tadiaman B., Najos O., Valencia E., De Rueda R., Ventura J. A comparison of the role of Musca domestica (Linnaeus) and Chrysomya megacephala (Fabricius) as mechanical vectors of helminthic parasites in a typical slum area of Metropolitan Manila. Southeast Asian J. Trop. Med. Public Health. 1991;22:222–228. [PubMed] [Google Scholar]
- 45.Stoddart R., Crompton D., Walters D. Influence of host strain and helminth isolate on the first phase of the relationship between rats and Moniliformis moniliformis (Acanthocephala) J. Parasitol. 1991;77:372–377. doi: 10.2307/3283122. [DOI] [PubMed] [Google Scholar]
- 46.Chinchilla M., Guerrero O., Castro A., Sabah J. Cockroaches as transport hosts of the protozoan Toxoplasma gondii. Rev. Biol. Trop. 1994;42:329–331. [PubMed] [Google Scholar]
- 47.Zerpa R., Huicho L. Childhood Cryptosporidial Diarrhea Associated with Identification of Cryptosporidium sp. in the Cockroach periplaneta Americana. Pediatr. Infect. Dis. J. 1994;13:546–548. doi: 10.1097/00006454-199406000-00019. [DOI] [PubMed] [Google Scholar]
- 48.Juris P., Világiová I., Plachý P. The importance of flies (Diptera-Brachycera) in the dissemination of helminth eggs from sewage treatment plants. Vet. Med. 1995;40:289–292. [PubMed] [Google Scholar]
- 49.Graczyk T.K., Cranfield M.R., Fayer R., Bixler H. House flies (Musca domestica) as transport hosts of Cryptosporidium parvum. Am. J. Trop. Med. Hyg. 1999;61:500–504. doi: 10.4269/ajtmh.1999.61.500. [DOI] [PubMed] [Google Scholar]
- 50.Mathison B.A., Ditrich O. The fate of Cryptosporidium parvum oocysts ingested by dung beetles and their possible role in the dissemination of cryptosporidiosis. J. Parasitol. 1999;85:678–681. doi: 10.2307/3285742. [DOI] [PubMed] [Google Scholar]
- 51.Doiz O., Clavel A., Morales S., Varea M., Castillo F.J., Rubio C., Gómez-Lus R. House fly (Musca domestica) as a transport vector of Giardia lamblia. Folia Parasitol. 2000;47:330–333. doi: 10.14411/fp.2000.057. [DOI] [PubMed] [Google Scholar]
- 52.Graczyk T.K., Fayer R., Knight R., Mhangami-Ruwende B., Trout J.M., Da Silva A.J., Pieniazek N.J. Mechanical transport and transmission of Cryptosporidium parvum oocysts by wild filth flies. Am. J. Trop. Med. Hyg. 2000;63:178–183. doi: 10.4269/ajtmh.2000.63.178. [DOI] [PubMed] [Google Scholar]
- 53.Oliveira V.C.D., Mello R.P.D., d’Almeida J.M. Muscoid dipterans as helminth eggs mechanical vectors at the zoological garden, Brazil. Rev. Saude Publica. 2002;36:614–620. doi: 10.1590/S0034-89102002000600011. [DOI] [PubMed] [Google Scholar]
- 54.Graczyk T.K., Grimes B.H., Knight R., Da Silva A.J., Pieniazek N.J., Veal D.A. Detection of Cryptosporidium parvum and Giardia lamblia carried by synanthropic flies by combined fluorescent in situ hybridization and a monoclonal antibody. Am. J. Trop. Med. Hyg. 2003;68:228–232. doi: 10.4269/ajtmh.2003.68.228. [DOI] [PubMed] [Google Scholar]
- 55.Pai H.-H., Ko Y., Chen E. Cockroaches (Periplaneta americana and Blattella germanica) as potential mechanical disseminators of Entamoeba histolytica. Acta Trop. 2003;87:355–359. doi: 10.1016/S0001-706X(03)00140-2. [DOI] [PubMed] [Google Scholar]
- 56.Chan O., Lee E.K., Hardman J.M., Navin J.J. The cockroach as a host for Trichinella and Enterobius vermicularis: Implications for public health. Hawaii Med. J. 2004;63:74–77. [PubMed] [Google Scholar]
- 57.Graczyk T.K., Grimes B.H., Knight R., Szostakowska B., Kruminis-Lozowska W., Racewicz M., Tamang L., Dasilva A.J., Myjak P. Mechanical transmission of Cryptosporidium parvum oocysts by flies. Wiadomości Parazytol. 2004;50:243–247. [PubMed] [Google Scholar]
- 58.Szostakowska B., Kruminis-Lozowska W., Racewicz M., Knight R., Tamang L., Myjak P., Graczyk T.K. Cryptosporidium parvum and Giardia lamblia recovered from flies on a cattle farm and in a landfill. Appl. Environ. Microbiol. 2004;70:3742–3744. doi: 10.1128/AEM.70.6.3742-3744.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tatfeng Y., Usuanlele M., Orukpe A., Digban A., Okodua M., Oviasogie F., Turay A. Mechanical transmission of pathogenic organisms: The role of cockroaches. J. Vector Borne Dis. 2005;42:129. [PubMed] [Google Scholar]
- 60.Conn D.B., Weaver J., Tamang L., Graczyk T.K. Synanthropic flies as vectors of Cryptosporidium and Giardia among livestock and wildlife in a multispecies agricultural complex. Vector-Borne Zoonotic Dis. 2007;7:643–652. doi: 10.1089/vbz.2006.0652. [DOI] [PubMed] [Google Scholar]
- 61.Getachew S., Gebre-Michael T., Erko B., Balkew M., Medhin G. Non-biting cyclorrhaphan flies (Diptera) as carriers of intestinal human parasites in slum areas of Addis Ababa, Ethiopia. Acta Trop. 2007;103:186–194. doi: 10.1016/j.actatropica.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 62.Kinfu A., Erko B. Cockroaches as carriers of human intestinal parasites in two localities in Ethiopia. Trans. R. Soc. Trop. Med. Hyg. 2008;102:1143–1147. doi: 10.1016/j.trstmh.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 63.Sasmal N., Pahari T., Laha R. Experimental infection of the cockroach Periplaneta americana with Toxocara canis and the establishment of patent infections in pups. J. Helminthol. 2008;82:97–100. doi: 10.1017/S0022149X07875936. [DOI] [PubMed] [Google Scholar]
- 64.Fetene T., Worku N. Public health importance of non-biting cyclorrhaphan flies. Trans. R. Soc. Trop. Med. Hyg. 2009;103:187–191. doi: 10.1016/j.trstmh.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 65.Förster M., Klimpel S., Sievert K. The house fly (Musca domestica) as a potential vector of metazoan parasites caught in a pig-pen in Germany. Vet. Parasitol. 2009;160:163–167. doi: 10.1016/j.vetpar.2008.10.087. [DOI] [PubMed] [Google Scholar]
- 66.Mowlavi G., Mikaeili E., Mobedi I., Kia E., Masoomi L., Vatandoost H. A survey of dung beetles infected with larval nematodes with particular note on Copris lunaris beetles as a vector for Gongylonema sp. in Iran. Korean J. Parasitol. 2009;47:13. doi: 10.3347/kjp.2009.47.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Racewicz M., Kruminis-Łozowska W., Gabre R.M., Stańczak J. The occurrence of Cryptosporidium spp. in synanthropic flies in urban and rural environments. Wiad. Parazytol. 2009;55:231–236. [PubMed] [Google Scholar]
- 68.Chamavit P., Sahaisook P., Niamnuy N. The majority of cockroaches from the Samutprakarn province of Thailand are carriers of parasitic organisms. EXCLI J. 2011;10:218. [PMC free article] [PubMed] [Google Scholar]
- 69.Fetene T., Worku N., Huruy K., Kebede N. Cryptosporidium recovered from Musca domestica, Musca sorbens and mango juice accessed by synanthropic flies in Bahirdar, Ethiopia. Zoonoses Public Health. 2011;58:69–75. doi: 10.1111/j.1863-2378.2009.01298.x. [DOI] [PubMed] [Google Scholar]
- 70.Ribeiro M.J.R., Dias S.M.F., Teshima E., Barboni A.R. Unhealthy environment and social aspects associated with intestinal pathogens isolated of dipteral. Eng. Sanit. Ambient. 2011;16:83–90. doi: 10.1590/S1413-41522011000100012. [DOI] [Google Scholar]
- 71.Ryan U., Yang R., Gordon C., Doube B. Effect of dung burial by the dung beetle Bubas bison on numbers and viability of Cryptosporidium oocysts in cattle dung. Exp. Parasitol. 2011;129:1–4. doi: 10.1016/j.exppara.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 72.El-Sherbini G.T., Gneidy M.R. Cockroaches and flies in mechanical transmission of medical important parasites in Khaldyia Village, El-Fayoum, Governorate, Egypt. J. Egypt. Soc. Parasitol. 2012;240:165–174. doi: 10.12816/0006304. [DOI] [PubMed] [Google Scholar]
- 73.Adenusi A.A., Adewoga T.O.S. Human intestinal parasites in non-biting synanthropic flies in Ogun State, Nigeria. Travel Med. Infect. Dis. 2013;11:181–189. doi: 10.1016/j.tmaid.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 74.Adenusi A.A., Adewoga T.O. Studies on the potential and public health importance of non-biting synanthropic flies in the mechanical transmission of human enterohelminths. Trans. R. Soc. Trop. Med. Hyg. 2013;107:812–818. doi: 10.1093/trstmh/trt095. [DOI] [PubMed] [Google Scholar]
- 75.Lalander C., Diener S., Magri M.E., Zurbrügg C., Lindström A., Vinnerås B. Faecal sludge management with the larvae of the black soldier fly (Hermetia illucens)—From a hygiene aspect. Sci. Total Environ. 2013;458:312–318. doi: 10.1016/j.scitotenv.2013.04.033. [DOI] [PubMed] [Google Scholar]
- 76.Tetteh-Quarcoo P.B., Donkor E.S., Attah S.K., Duedu K.O., Afutu E., Boamah I., Olu-Taiwo M., Anim-Baidoo I., Ayeh-Kumi P.F. Microbial carriage of cockroaches at a tertiary care hospital in Ghana. Environ. Health Insights. 2013;7:EHI-S12820. doi: 10.4137/EHI.S12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bunchu N., Silaram M., Sukontason K., Sukontason K.L., Chaiwong T. Isolation of Toxocara eggs from flies in Northeast Thailand. J. Med. Assoc. Thail. 2014;97:S25–S28. [PubMed] [Google Scholar]
- 78.Lima M.S.C.S., Soares M.R.A., Pederassi J., Aguiar B.C.G., Pereira C.A.S. The housefly Musca domestica L. (Diptera: Muscidae) as a potential paratenic host in the city of Bom Jesus-Piauí, Brazil. Comun. Sci. 2014;5:349–355. [Google Scholar]
- 79.Gomez-Puerta L.A., Lopez-Urbina M.T., Garcia H.H., Gonzalez A.E. Longevity and viability of Taenia solium eggs in the digestive system of the beetle Ammophorus rubripes. Rev. Bras. Parasitol. Veter. 2014;23:94–97. doi: 10.1590/S1984-29612014014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hamu H., Debalke S., Zemene E., Birlie B., Mekonnen Z., Yewhalaw D. Isolation of intestinal parasites of public health importance from cockroaches (Blattella germanica) in Jimma Town, Southwestern Ethiopia. J. Parasitol. Res. 2014;2014:186240. doi: 10.1155/2014/186240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Isaac C., Orue P.O., Iyamu M.I., Ehiaghe J.I., Isaac O. Comparative analysis of pathogenic organisms in cockroaches from different community settings in Edo State, Nigeria. Korean J. Parasitol. 2014;52:177. doi: 10.3347/kjp.2014.52.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhao Z., Dong H., Wang R., Zhao W., Chen G., Li S., Qi M., Zhang S., Jian F., Zhao J. Genotyping and subtyping Cryptosporidium parvum and Giardia duodenalis carried by flies on dairy farms in Henan, China. Parasites Vectors. 2014;7:190. doi: 10.1186/1756-3305-7-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cazorla Perfetti D., Morales P., Navas P. Isolation of intestinal parasites from American cockroach (Periplaneta americana) in Coro, Falcon state, Venezuela. Boletín Malariol. Salud Ambient. 2015;55:184–193. [Google Scholar]
- 84.Muñoz D.J. Bacterial and Parasite Agents in Adult Housefly Musca domestica Collected in El Peñón, Sucre State, Venezuela. Rev. Cient. Fac. Cienc. Vet. 2015;25:159–166. [Google Scholar]
- 85.Farah Haziqah M., Asyiqin N., Mohd Khalid M., Suresh K., Rajamanikam A., Chandrawathani P., Mohd Zain S. Short Communication Current status of Blastocystis in cockroaches. Trop. Biomed. 2017;34:741–745. [PubMed] [Google Scholar]
- 86.González-García T., Muñoz-Guzmán M., Sánchez-Arroyo H., Prado-Ochoa M., Cuéllar-Ordaz J., Alba-Hurtado F. Experimental transmission of Toxocara canis from Blattella germanica and Periplaneta americana cockroaches to a paratenic host. Vet. Parasitol. 2017;246:5–10. doi: 10.1016/j.vetpar.2017.08.025. [DOI] [PubMed] [Google Scholar]
- 87.Martínez-Girón R., Martínez-Torre C., van Woerden H.C. The prevalence of protozoa in the gut of German cockroaches (Blattella germanica) with special reference to Lophomonas blattarum. Parasitol. Res. 2017;116:3205–3210. doi: 10.1007/s00436-017-5640-6. [DOI] [PubMed] [Google Scholar]
- 88.Oguz B., Ozdal N., Orunc Kilinc O., Deger M.S. First investigation on vectorial potential of Blattella germanica in Turkey. Ank. Univ. Vet. Fak. Derg. 2017;64:141–144. [Google Scholar]
- 89.Adenusi A.A., Akinyemi M.I., Akinsanya D. Domiciliary cockroaches as carriers of human intestinal parasites in Lagos Metropolis, Southwest Nigeria: Implications for public health. J. Arthropod-Borne Dis. 2018;12:141. doi: 10.18502/jad.v12i2.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hemmati S., Afshar A.A., Mohammadi M.A., Afgar A., Nasibi S., Harandi M.F. Experimental and field investigation of non-biting flies as potential mechanical vectors of Echinococcus granulosus eggs. Exp. Parasitol. 2018;189:43–48. doi: 10.1016/j.exppara.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 91.Paliy A., Sumakova N., Mashkey A., Petrov R., Ishchenko K. Contamination of animal-keeping premises with eggs of parasitic worms. Biosyst. Divers. 2018;26:327–333. doi: 10.15421/011848. [DOI] [Google Scholar]
- 92.Paliy A., Sumakova N., Ishchenko K. Biological control of house fly. Ukr. J. Ecol. 2018;8:230–234. [Google Scholar]
- 93.Valles L.T., Alejos M., Antonini M., Escobar C., Perez M., Perez F., Ramirez D., Tovar A., Najul M. Enteroparasitary contamination of flies captured in the Palavecino municipality, Lara state, Venezuela, 2017. Rev. Med. Urug. 2018;34:217–221. [Google Scholar]
- 94.Vargas-Calla A., Gomez-Puerta L.A., Pajuelo M.J., Garcia H.H., Gonzalez A.E., Cysticercosis Working Group in Peru Molecular detection of taeniid eggs in beetles collected in an area endemic for Taenia solium. Am. J. Trop. Med. Hyg. 2018;99:1198. doi: 10.4269/ajtmh.18-0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gałęcki R., Sokół R. A parasitological evaluation of edible insects and their role in the transmission of parasitic diseases to humans and animals. PLoS ONE. 2019;14:e0219303. doi: 10.1371/journal.pone.0219303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Muller A., Wiedmer S., Kurth M. Risk evaluation of passive transmission of animal parasites by feeding of black soldier fly (Hermetia illucens) larvae and prepupae. J. Food Prot. 2019;82:948–954. doi: 10.4315/0362-028X.JFP-18-484. [DOI] [PubMed] [Google Scholar]
- 97.Dokmaikaw A., Suntaravitun P. Prevalence of parasitic contamination of cockroaches collected from fresh markets in Chachoengsao province, Thailand. Kobe J. Med. Sci. 2019;65:E118. [PMC free article] [PubMed] [Google Scholar]
- 98.Ma L., Zhang Y., Qiao H., Li S., Wang H., Zhang N., Zhang X. Cockroach as a Vector of Blastocystis sp. is Risk for Golden Monkeys in Zoo. Korean J. Parasitol. 2020;58:583. doi: 10.3347/kjp.2020.58.5.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.van Woerden H.C., Martínez-Girón R., Martínez-Torre C. Protozoan cysts in faecal pellets of German cockroaches (Blattella germanica), with particular emphasis on Lophomonas blattarum. Acta Parasitol. 2020;65:831–836. doi: 10.2478/s11686-020-00213-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Barnes A.N., Davaasuren A., Baasandavga U., Lantos P.M., Gonchigoo B., Gray G.C. Zoonotic enteric parasites in Mongolian people, animals, and the environment: Using One Health to address shared pathogens. PLoS Negl. Trop. Dis. 2021;15:e0009543. doi: 10.1371/journal.pntd.0009543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Motevalli-Haghi S.F., Shemshadian A., Nakhaei M., Faridnia R., Dehghan O., Shafaroudi M.M., Kelarijani M.N., Nikookar S.H., Kalani H., Fakhar M. First report of Lophomonoas spp. in German Cockroaches (Blatella germanica) Trapped in Hospitals, Northern Iran. J. Parasit. Dis. 2021;45:937–943. doi: 10.1007/s12639-021-01381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sands B., Wall R. Dung beetles reduce livestock gastrointestinal parasite availability on pasture. J. Appl. Ecol. 2017;54:1180–1189. doi: 10.1111/1365-2664.12821. [DOI] [Google Scholar]
- 103.Fincher G.T. Dung beetles as biological control agents for gastrointestinal parasites of livestock. J. Parasitol. 1973;59:396–399. doi: 10.2307/3278842. [DOI] [PubMed] [Google Scholar]
- 104.Yoshikawa H., Wu Z., Howe J., Hashimoto T., Geok-Choo N., Tan K.S. Ultrastructural and phylogenetic studies on Blastocystis isolates from cockroaches. J. Eukaryot. Microbiol. 2007;54:33–37. doi: 10.1111/j.1550-7408.2006.00141.x. [DOI] [PubMed] [Google Scholar]
- 105.Zaman V., Ng G., Suresh K., Yap E., Singh M. Isolation of Blastocystis from the cockroach (Dictyoptera: Blattidae) Parasitol. Res. 1993;79:73–74. doi: 10.1007/BF00931221. [DOI] [Google Scholar]
- 106.Bauerfeind R., Von Graevenitz A., Kimmig P., Schiefer H.G., Schwarz T., Slenczka W., Zahner H. Zoonoses: Infectious Diseases Transmissible from Animals to Humans. John Wiley & Sons; Hoboken, NJ, USA: 2015. [Google Scholar]
- 107.Dehghani R., Kassiri H. A brief review on the possible role of houseflies and cockroaches in the mechanical transmission of coronavirus disease 2019 (COVID-19) Arch. Clin. Infect. Dis. 2020;15:e102863. doi: 10.5812/archcid.102863. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All of the data used in this study are openly available.