Abstract
Periodontal disease (PD) is one of the most prevalent disorders globally and is strongly associated with many other diseases. Inflammatory bowel disease (IBD), an inflammatory condition of the colon and the small intestine, is reported to be associated with PD through undetermined mechanisms. We analyzed taxonomic assignment files from the Crohn’s Disease Viral and Microbial Metagenome Project (PRJEB3206). The abundance of Porphyromonadaceae in fecal samples was significantly different between patients with Crohn’s disease and control volunteers. Dextran sulfate sodium was used to induce colitis in mice to reveal the effect of this periodontopathic pathogen in vivo. After intrarectal implantation of Porphyromonas gingivalis (Pg)—the primary pathogen causing PD—the disease activity index score, colonic epithelial loss, and inflammatory cell infiltration were intensified. In addition, tumor necrosis factor-α and interleukin-6 showed the highest levels in Pg-infected colons. This revealed the importance of Pg in the exacerbation of IBD. Thus, simultaneous treatment of PD should be considered for people with IBD. Moreover, implantation of Pg in the rectum worsened the clinical symptoms of colitis in mice. Because Pg participates in the pathogenesis of IBD, reducing the chances of it entering the intestine might prevent the worsening of this disorder.
Keywords: periodontal disease, Porphyromonas gingivalis, inflammatory bowel disease, gut inflammation
1. Introduction
Periodontal disease (PD) involves the development of lesions on the periodontium (gingiva, alveolar bone, cementum, and periodontal ligament) [1]. This oral disease involves a wide range of inflammatory conditions caused by bacterial biofilm [2]. The severity of PD increases with age, and affected individuals typically have other comorbidities [2,3,4]. Thus, improving the prevention and control of PD involves the core governance activities of public health assessment, policy development, and insurance [5].
Epidemiologic studies have shown a positive association between PD and overall cancer risk [6]. For example, PD might worsen tumor-promoting effects and has been linked to many human cancers, such as oral, esophageal, lung, prostate, and liver cancers [7,8,9,10]. The increased cancer risk may be associated with PD by microbial stimulation of a destructive inflammatory response [3,11,12].
Inflammatory bowel disease (IBD), which includes Crohn’s disease (CD) and ulcerative colitis (UC), is correlated with an increased risk of colorectal cancer [13]. These chronic, relapsing–remitting systemic diseases cause similar clinical burdens and have similar treatment strategies [14]. Anti-inflammatory agents can protect against IBD [15]. On the other hand, PD and IBD are often found to have a comorbid relationship, and modulating excessive inflammation [6,16,17,18,19] might have potential in PD treatment [20]. Because there is dysbiosis of the microbiota in these two inflammatory diseases [17,19,21], microbiota might help explain the link between PD and IBD. Such imbalance in host–microbiota interactions might lead to undesired immune responses to the intestinal microbiota and result in chronic bowel inflammation [22,23,24]. The bacteria present in individuals with gingivitis can penetrate deeper into the tissues and surrounding periodontium. This triggers a host immune response against the invading bacteria [1].
Porphyromonas gingivalis (Pg) is known to be a pathogen that contributes to the initiation and progression of PD [25,26]. Besides PD, several systemic pathologies, such as cardiovascular diseases, rheumatoid arthritis, pancreatic cancer, nonalcoholic steatohepatitis, and neurodegenerative pathologies, have been linked to Pg infection [27,28,29,30]. In this regard, IBD and PD are both chronic inflammatory diseases [31]. However, the underlying pathological and molecular network between IBD and PD is not fully understood. Therefore, understanding the influence of Pg in IBD might help patients with PD to evade IBD or prevent its deterioration. Here, we hypothesized that Pg might play a role in the clinical signs of IBD, and a dextran sulfate sodium (DSS)-induced mouse model of colitis was applied to test the possible causal relationship between Pg infection and IBD.
2. Results
2.1. Porphyromonadaceae Showed Higher Abundance in the Feces of Patients with Crohn’s Disease
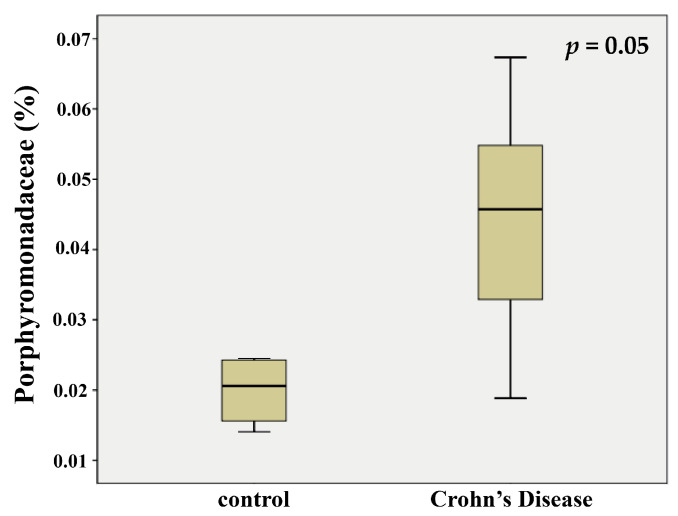
We downloaded taxonomic assignment files from the Crohn’s Disease Viral and Microbial Metagenome Project (PRJEB3206), which comprise 11 amplicon-sequenced files from fecal samples of patients with CD and eight amplicon-sequenced files from control fecal samples of volunteers. The extracted information included the bacterial taxonomic composition and abundance at the family level. At the end of the analysis, we compared samples from the two groups. The abundance of Porphyromonadaceae in fecal samples was significantly different between the patients with CD and control volunteers. In the feces of patients, the abundance of Porphyromonadaceae (Figure 1) was substantially higher than in the control samples. This observation suggested that Pg, a member of this family, might influence the clinical signs of CD.
Figure 1.
The abundance of Porphyromonadaceae in patients with or without Crohn’s disease. Bacterial 16S rRNA sequencing data was obtained from the Crohn’s Disease Viral and Microbial Metagenome Project (PRJEB3206). The abundance of Porphyromonadaceae in fecal samples showed significant differences between the patients with CD (n = 11) and control volunteers (n = 8). Data were presented as the means ± SD. p = 0.05, compared with the control (volunteers) group.
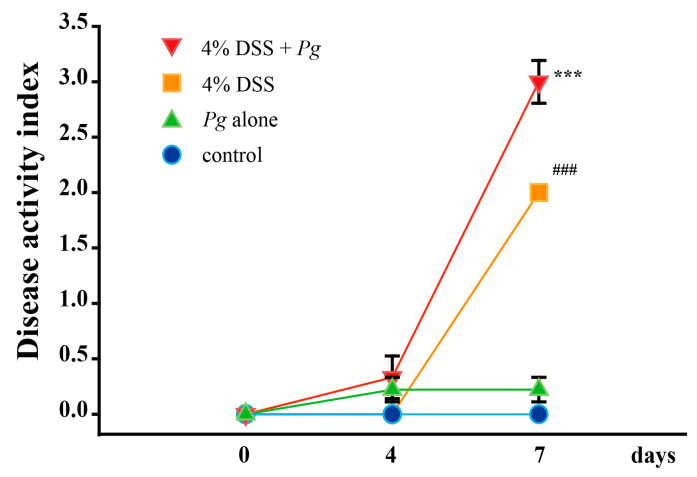
2.2. Effect of Pg on Clinical Signs of Colitis Induced by DSS
It is well-established that CD is a major type of IBD [32]. The DAI is a score that grades weight changes, stool consistency, and rectal bleeding to assess the clinical evolution of colitis. As shown in Figure 2, after four days of 4% DSS administration, there was no statistically significant difference between all groups. After seven days of 4% DSS treatment, the Pg-treatment groups showed a slight increase in the DAI score but no significant difference with the control (no treatment) group. The 4% DSS treatment group demonstrated the clinical sign of IBD for having two points on the DAI score. Compared with the 4% DSS treatment group, 3 points of DAI score was recorded in the 4% DSS plus Pg group, a significant difference.
Figure 2.
Analyzing the disease activity index (DAI) change after 4 and 7 days of treatment with 4% DSS. 4% DSS insulted animals showed no statistically significant difference in DAI between all groups at day 4. After seven days of 4% DSS treatment, the Pg-treatment alone group (group 2) showed in the DAI score a slight increase but no significant difference with the control (no treatment, group 1) group. The 4% DSS treatment group (group 3) had two points, and 4% DSS plus Pg group (group 4) had three points in the DAI score. Data were presented as the means ± SD (n = 3). ### p < 0.001, compared with the control group; *** p < 0.001, compared with the 4% DSS group.
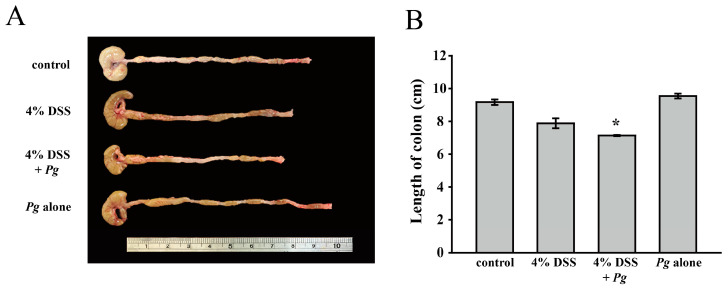
Colon length has been proven to be a biological marker in assessing colonic inflammation: the shorter the colon, the more severe the colitis [33]. Figure 3A illustrates the colons of each group; the length of colons was measured at the end of the experiment (seven days after treating DSS). In Figure 3B, there was no significant difference between the control and Pg-alone groups; the 4% DSS treatment group had shorter colons, and the shortest colon was found in the 4% DSS plus Pg group. DSS treatment clearly caused colitis, but Pg infection by itself showed no marked effect on clinical signs of colitis. However, in the 4% DSS plus Pg group, the highest DAI score, and the shortest colon revealed that Pg treatment exacerbated the inflammatory response of the colon and was associated with IBD. The data in Figure 4 demonstrated that the clinical signs, including colon length and DAI score, showed similar patterns.
Figure 3.
Examine the effect of Pg and DSS on the variety of colon lengths. (A) Photograph of dissected colon (with cecum) specimen was a representative example of three similar experiments. (B) The colon lengths of each group were presented respectively as the means ± SD of the means (n = 3). * p < 0.05, compared with the 4% DSS group.
Figure 4.
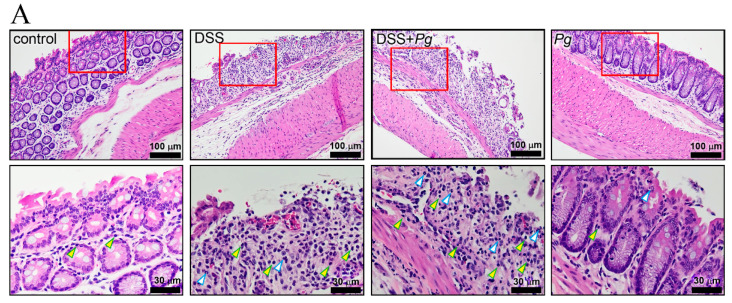
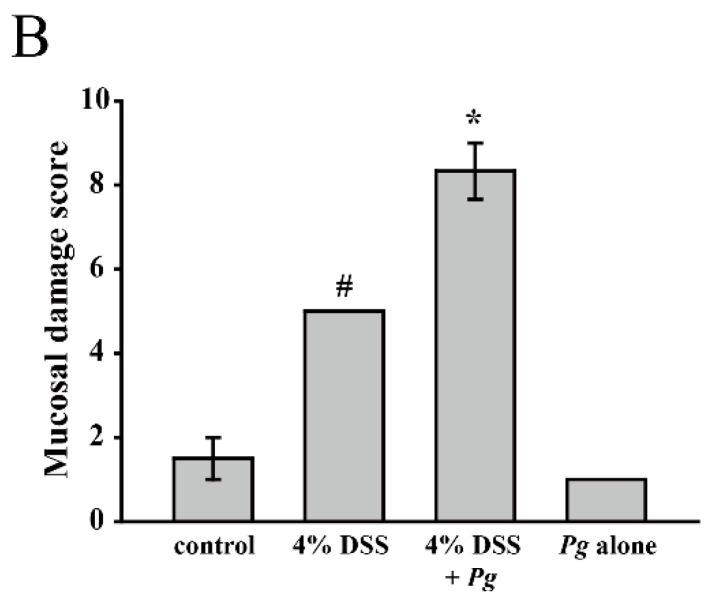
Histologic examination of colon tissue samples. (A) Representative photomicrographs of colon specimens were representative examples of three similar experiments. The yellow arrow indicated the mononuclear leukocytes, and the polymorphonuclear leukocytes were indicated by the white arrow. (B) The mucosal damage score of each group was calculated and presented respectively as the means ± SD of the means (n = 3), # p < 0.05, compared with the control group; * p < 0.05, compared with the 4% DSS group.
2.3. Pg Implantation Exacerbated DSS-Mediated Colitis by IHC Score
Epithelial changes, overall mucosal architecture, and the degree of inflammatory cell infiltration are the symptoms of intestinal inflammation in mouse models [34]. Here we evaluated the surface epithelial loss, crypt destruction, and inflammatory cell infiltration into the mucosa (Figure 4A) and summed the score of these parameters as the mucosal damage score (Figure 4B). H&E staining was used to demonstrate the histopathology pattern of the colon under different treatments.
The mice with active colitis induced by 4% DSS treatment showed mucosal erosion with crypt architectural distortion and mixed infiltrates of acute and chronic inflammatory cells. Pg implantation, together with 4% DSS treatment, resulted in severe active inflammation with pronounced epithelial loss, marked crypt architectural alterations, and dense cellular infiltrates. Significant inflammatory cell infiltrates and crypt architectural changes were absent in both the control and Pg-alone groups, but the IHC scores were not significantly different. The score of the 4% DSS treatment group was statistically significantly different from the control group. Moreover, the 4% DSS plus Pg group had the highest score, which was significantly different from the treatment group receiving 4% DSS alone. Thus, Pg implantation without 4% DSS treatment did not affect the integrity of colonic tissues. However, Pg treatment worsened mucosal damage when colitis was induced by 4% DSS treatment.
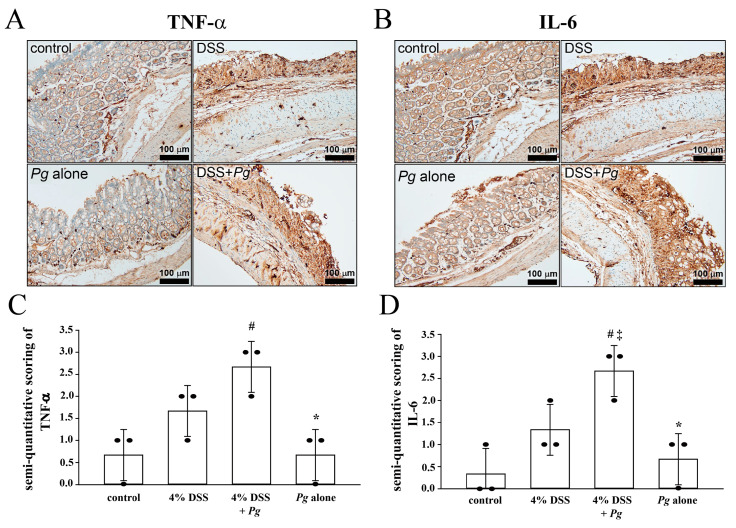
2.4. Overexpression of Tumor Necrosis Factor Alfa (TNF-α) and Interleukin (IL-6) in Pg-Infected Colons with Colitis
The levels of TNF-α and IL-6 are positively correlated with disease severity in patients with IBD [35,36]. TNF-α causes villous atrophy, decreases epithelial cell turnover, and increases cell apoptosis [37]. In addition, neutralizing IL-6 might effectively treat IBD [38]. For understanding the effect of Pg in colitis, we examined the expression level of each group of colons in this study. The results shown in Figure 5A demonstrated abundant inflammatory cells immunostained for TNF-α in the 4% DSS plus Pg group, with a higher expression level than in the 4% DSS treated group. Figure 5B shows the staining intensity of IL-6, with a marked increase in the 4% DSS plus Pg group, more than in the 4% DSS treated group. Compared with the 4% DSS plus Pg group, only a few IL-6-positive cells were found in the Pg-alone group.
Figure 5.
Expression pattern of TNF-α and IL-6 proteins. Immunohistochemistry (IHC) analysis stated the presence and location of TNF-α and IL-6 proteins in colon specimens. (A) TNF-α was stained remarkably in groups administrated with DSS, and DSS + Pg insulted colon showed the highest expression of TNF-α. (B) IHC labeled IL-6 protein in DSS + Pg insulted colon showed higher intensity level than the colon treated with DSS alone. Semi-quantitative scoring of (C) TNF-α and (D) IL-6 proteins. The score of each group was calculated and presented respectively as the means ± SD of the means (n = 3): # p < 0.05, compared with the control group in (C,D); * p < 0.05, compared with the 4% DSS plus Pg group in (C,D); ‡ p < 0.05, compared with the 4% DSS group in (D).
3. Discussion
PD is one of the most prevalent conditions worldwide, and it is reported to be related to IBD, although the mechanism of their relationship is still undetermined. Some studies have elucidated the relationship between PD and UC. Here, we found that Pg, the primary pathogen of PD, might serve to link PD and IBD. The presence of Pg increased the DAI score, colon epithelial loss, and inflammatory cell infiltration during DSS-induced colitis. In addition, the highest expression levels of TNF-α or IL-6 in mouse colons cotreated with DSS and Pg suggested that Pg intensified the expressions of TNF-α and IL-6.
Successful PD treatment is associated with a significantly reduced overall risk of cancer and reduced risks of certain types of cancers [39]. In previous studies, antibiotic treatments were found to delay the progression of rheumatoid arthritis and Alzheimer’s Disease in patients with PD [40,41]. Moreover, several systematic reviews and meta-analyses of clinical trials demonstrated that antibiotics such as ciprofloxacin and metronidazole [42] appear to effectively induce remission in patients with IBD [43,44]. Therefore, the use of antibiotics for inhibiting the pathogens causing PD, including minocycline, doxycycline, and metronidazole [45], might be considered for treating patients with IBD under an appropriate dosage to avoid gastrointestinal side effects.
In this study, Pg treatment by itself did not affect the integrity of the mouse colon or the expression of the proinflammatory cytokines TNF-α and IL-6. However, it showed an adverse effect in colons with mucosal damage caused by DSS. According to this result, without protecting the intestinal mucosal barrier, Pg showed more pathogenicity in the gut. Thus, the diagnosis of PD is vital for the prognosis and treatment of patients with IBD. However, the Pg-derived lipopolysaccharide (LPS) surprisingly showed partial benefit in DSS-induced murine colitis. In the previous studies, Pg LPS downregulated the expression of Lgr5, a representative marker for intestinal stem cells, and Alpi, a marker for absorptive enterocytes to modulate the differentiation of epithelial cells [46]. This finding showed another view of Pg in colitis, making researchers reconsider the role of Pg in colitis. In the future, more detailed mechanisms of Pg LPS should be investigated.
Some studies demonstrated that PD was most common in the elderly, tobacco smokers, and populations from high-income countries [47,48]. Therefore, the treatment of PD must be considered when IBD occurs in these populations.
Although animal models do not perfectly recapitulate human IBD, they have led to the discovery of important concepts in its pathogenesis [49]. Much recent progress in the understanding of immunity has been achieved using experimental animal models of intestinal inflammation [49]. Experimental colitis can be induced using chemical irritants such as DSS or transgenic mouse models. The picture of all the intestines in each group are presented in the supplementary Figure S1. Essentially, DSS does not cause intestinal inflammation directly; instead, it injures the intestinal epithelium, resulting in exposure of the lamina propria and submucosal compartment to luminal antigens and enteric bacteria, triggering inflammation [33,50,51] Thus, UC can be induced in mice by varying the concentration and duration of DSS administration in drinking water [33,52].
The limitation of this work was that there were not enough animals in this study. According to the principle of 3R (replacement, reduction, refinement), we inspected the fewest animals and obtained accurate data. To observe the diverse effects made by the target microbe, such as the major player in the current study, the Porphyromonas gingivalis, further enlarged sample size examination will be conducted in the future.
In conclusion, Pg plays a critical role in the progression of colitis. Pg implantation in the rectum induced overexpression of TNF-α and IL-6, followed by loss of surface epithelium, destruction of crypts, and infiltration of inflammatory cells, thereby exacerbating the clinical symptoms of colitis in this mouse model. Given the prevalence of PD, clinicians treating individuals susceptible to IBD should consider PD treatment simultaneously. Furthermore, since Pg participates in the pathogenesis of IBD, the importance of using antibiotics for treating PD, such as minocycline and metronidazole, needs to be further explored in the future.
4. Materials and Methods
4.1. Data Collection
We obtained the bacterial 16S rRNA sequencing data from the Crohn’s Disease Viral and Microbial Metagenome Project (PRJEB3206). The project information is available from the EMBL database (https://www.ebi.ac.uk/metagenomics/studies/MGYS00000307) (accessed on 30 August 2021). Vicente et al. documented the use of 16S rRNA gene sequences for bacterial identification, taxonomic analysis, and estimating diversity, and their approach was followed here [53].
4.2. Mouse Model of DSS-Induced Colitis
Male BALB/c mice (6–8 weeks old) were purchased from the National Laboratory Animal Center (Taipei, Taiwan) and maintained in the Animal Research Center, according to the Institutional Animal Care and Use Committees (approval no. IACUC 110-011) at Cathay General Hospital (Taipei, Taiwan). All animals were housed in plastic cages (two or three per cage) in controlled conditions of humidity (50 ± 10%), light (12/12 h light/dark cycle), and temperature (23 ± 2 °C). The mice were quarantined for seven days before being randomized by body weight into different groups for testing Pg: (1) subgroup with no treatment (control group, n = 3); (2) subgroup with Pg (1 × 108 colony forming units (CFU) in 100 μL) administration through anal injection (Pg alone group, n = 3); (3) subgroup with acute DSS-induced UC by drinking water containing 4% DSS (molecular weight, 36,000–50,000; MP Biomedicals, Solon, OH, USA) for seven days (4% DSS group, n = 3); (4) subgroup with Pg administration as subgroup 2 and 4% DSS administration as subgroup 3 (4% DSS + Pg group, n = 3). Mice were finally euthanized by high dose halogenated anesthetics (isoflurane: delivered via vaporizer for anesthetic induction (3%, 5 min) and euthanasia (5%, 15 min)). The colons were collected after confirmation of cessation of respiratory. All efforts were made to minimize the number of animals and their suffering.
4.3. Inflammation in Tissues of Mice with DSS-Induced Colitis
Mice with induced colitis were euthanized, and the abdominal cavity was opened. The colon was isolated and opened longitudinally. The inflammation status was characterized according to macroscopic damage, histopathology, and inflammation-related cytokines. Briefly, macroscopic damage to the entire colon sections was assessed from the degrees of body weight loss, stool consistency (diarrhea), and colonic bleeding using a previously established scoring system (disease activity index, DAI) [54]. Then, histopathology and immunohistochemical (IHC) staining were performed. Isolated colons were fixed, dehydrated, and embedded in paraffin wax using standard techniques, and 5-μm thick sections were transferred to slides. Histology was performed on the sections after hematoxylin and eosin (H&E) staining. The histological features of (i) surface epithelial loss, (ii) crypt destruction, and (iii) inflammatory cell infiltration into the mucosa were used to determine the severity of mucosal damage. According to the widely accepted scoring system, the damage was scored from 0 (normal) to 4 (extensive and severe) [55].
4.4. Immunohistochemical Staining and Semi-Quantitative Determination of Protein Expression
For IHC staining to detect various proteins, TNF-α and IL-6 were respectively immune-detected with anti-TNF-α antibody (1:100 in phosphate-buffered saline; Cat No. GTX15821; GeneTex, Irvine, CA, USA) and anti-IL-6 antibody (1:100 in phosphate-buffered saline; Cat No. ab208113; Abcam, Cambridge, UK) for 32 min at 37 °C under an automated Ventana Benchmark XT (Ventana Medical Systems, Tucson, AZ, USA). Labeling was detected with the Optiview DAB Detection Kit (Ventana Medical Systems, Inc., Tucson, AZ, USA) according to the manufacturer’s instruction. All sections were counterstained with hematoxylin in Ventana reagent (Ventana Medical Systems). After being dehydrated and mounted, the imaging results were scored by histopathologists.
The staining frequency of proteins was semiquantitatively scored based on the percentages of positive cells. The scoring criteria were as follows: (i) TNF-α, 0–10% of cells stained, score 0; 11–25% of cells stained, score 1; 26–50% of cells stained, score 2; 51–100% of cells stained, score 3 [56]; (ii) IL-6, 0% of cells stained, score 0; 1–25% of cells stained, score 1; 26–50% of cells stained, score 2; 51–100% of cells stained, score 3 [57].
4.5. Pg Preparation
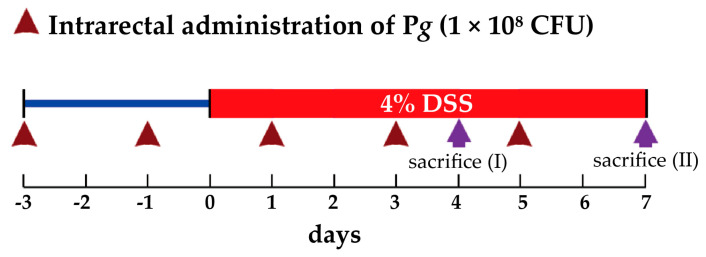
We commissioned the Bioresource Collection and Research Center (Hsinchu, Taiwan) to culture Pg following their protocols. Here we applied the most widely used chemical colitogen, DSS, to induce colitis in mice. To measure the effect of Pg on colitis, Pg (1 × 108 CFU) was administered intrarectally to mice with DSS-induced colitis, and the changes in disease activity index (DAI) scores were measured. As shown in the scheme (Figure 6), days one and three before DSS treatment, mice in Pg insulted groups (2 and 4) were administered Pg (1 × 108 CFU) by anal injection. Subsequently, mice in groups 3 and 4 were treated with 4% DSS for the next seven days. Pg insulted groups (2 and 4) were continued to receive Pg (1 × 108 CFU) by intrarectal injection at days one, three, and five after DSS treatment.
Figure 6.
Schematic of the treatment protocols. Animals in groups 3 and 4 were treated with 4% DSS (dissolved in drinking water) from day 0 to day 7. For transplanting the Pg, animals in groups 2 and 4 were administrated Pg (1 × 108 CFU in 100 μL) by the intrarectal injection method. Pg was preadministrated three days before day 0 (initiation of 4% DSS treatment) and followed every two days until the end of the examination. Animals were sacrificed (euthanasia) on day 4 for DAI score assessment and day 7 for colon length determination and histological analysis.
4.6. Statistics
The significance of any differences between the two groups was assessed using Student’s t-test. The Kruskal–Wallis one-way analysis of variance by ranks test determined whether four independent groups were significantly different. The commercial statistical package, SPSS (ver. 22.0, IBM SPSS statistics), was used in these analyses. Data are presented as means ± standard errors of the mean for the indicated number of independently performed experiments, and p < 0.05 was considered statistically significant.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pathogens11010084/s1, Figure S1: The picture of all the intestines in each group.
Author Contributions
Conceptualization, Y.-C.L., C.-L.L., C.-J.H., and T.-L.Y.; Data curation, C.-J.H.; Funding acquisition, T.-L.Y.; Methodology, C.-Y.L. and C.-J.H.; Project administration, C.-J.H.; Supervision, C.-L.L.; Validation, C.-J.H. and T.-L.Y.; Visualization, R.-H.Z.; Writing—original draft, Y.-C.L. and T.-L.Y.; Writing—review & editing, C.-J.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Cathay General Hospital, grant number CGH-MR-A10709.
Institutional Review Board Statement
The study procedures were approved by the Institutional Animal Care and Use Committees at Cathay General Hospital (approval no. IACUC 110-011).
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gasner N.S., Schure R.S. StatPearls [Internet] StatPearls Publishing; Treasure Island, FL, USA: 2021. [(accessed on 15 October 2021)]. Periodontal Disease. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554590/ [Google Scholar]
- 2.Pihlstrom B.L., Michalowicz B.S., Johnson N.W. Periodontal diseases. Lancet. 2005;366:1809–1820. doi: 10.1016/S0140-6736(05)67728-8. [DOI] [PubMed] [Google Scholar]
- 3.Michaud D.S., Fu Z., Shi J., Chung M. Periodontal Disease, Tooth Loss, and Cancer Risk. Epidemiol. Rev. 2017;39:49–58. doi: 10.1093/epirev/mxx006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Persson G.R. Periodontal complications with age. Periodontology 2000. 2018;78:185–194. doi: 10.1111/prd.12227. [DOI] [PubMed] [Google Scholar]
- 5.Janakiram C., Dye B.A. A public health approach for prevention of periodontal disease. Periodontology 2000. 2020;84:202–214. doi: 10.1111/prd.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nwizu N., Wactawski-Wende J., Genco R.J. Periodontal disease and cancer: Epidemiologic studies and possible mechanisms. Periodontology 2000. 2020;83:213–233. doi: 10.1111/prd.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Irani S., Barati I., Badiei M. Periodontitis and oral cancer - current concepts of the etiopathogenesis. Oncol. Rev. 2020;14:465. doi: 10.4081/oncol.2020.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzpatrick S.G., Katz J. The association between periodontal disease and cancer: A review of the literature. J. Dent. 2010;38:83–95. doi: 10.1016/j.jdent.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Chung P.-C., Chan T.-C. Association between periodontitis and all-cause and cancer mortality: Retrospective elderly community cohort study. BMC Oral Health. 2020;20:1–11. doi: 10.1186/s12903-020-01156-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Maweri S.A., Ibraheem W.I., Al-Ak’Hali M.S., Shamala A., Halboub E., Alhajj M.N. Association of periodontitis and tooth loss with liver cancer: A systematic review. Crit. Rev. Oncol. Hematol. 2021;159:103221. doi: 10.1016/j.critrevonc.2021.103221. [DOI] [PubMed] [Google Scholar]
- 11.Curtis M.A., Diaz P.I., Van Dyke T.E. The role of the microbiota in periodontal disease. Periodontology 2000. 2020;83:14–25. doi: 10.1111/prd.12296. [DOI] [PubMed] [Google Scholar]
- 12.Hoare A., Soto C., Rojas-Celis V., Bravo D. Chronic Inflammation as a Link between Periodontitis and Carcinogenesis. Mediat. Inflamm. 2019;2019:1–14. doi: 10.1155/2019/1029857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stidham R.W., Higgins P.D. Colorectal Cancer in Inflammatory Bowel Disease. Clin. Colon Rectal Surg. 2018;31:168–178. doi: 10.1055/s-0037-1602237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Le Berre C., Ananthakrishnan A.N., Danese S., Singh S., Peyrin-Biroulet L. Ulcerative Colitis and Crohn’s Disease Have Similar Burden and Goals for Treatment. Clin. Gastroenterol. Hepatol. 2020;18:14–23. doi: 10.1016/j.cgh.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Duan L., Cheng S., Li L., Liu Y., Wang D., Liu G. Natural Anti-Inflammatory Compounds as Drug Candidates for Inflammatory Bowel Disease. Front. Pharmacol. 2021;12:684486. doi: 10.3389/fphar.2021.684486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.She Y.-Y., Kong X.-B., Ge Y.-P., Liu Z.-Y., Chen J.-Y., Jiang J.-W., Jiang H., Fang S.-L. Periodontitis and inflammatory bowel disease: A meta-analysis. BMC Oral Health. 2020;20:1–11. doi: 10.1186/s12903-020-1053-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang L., Gao X., Zhou J., Chen S., Zhang J., Zhang Y., Chen B., Yang J. Increased risks of dental caries and periodontal disease in Chinese patients with inflammatory bowel disease. Int. Dent. J. 2020;70:227–236. doi: 10.1111/idj.12542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lorenzo-Pouso A.I., Castelo-Baz P., Rodriguez-Zorrilla S., Pérez-Sayáns M., Vega P. Association between periodontal disease and inflammatory bowel disease: A systematic review and meta-analysis. Acta Odontol. Scand. 2021;79:344–353. doi: 10.1080/00016357.2020.1859132. [DOI] [PubMed] [Google Scholar]
- 19.Lin C.-Y., Tseng K.-S., Liu J.-M., Chuang H.-C., Lien C.-H., Chen Y.-C., Lai C.-Y., Yu C.-P., Hsu R.-J. Increased Risk of Ulcerative Colitis in Patients with Periodontal Disease: A Nationwide Population-Based Cohort Study. Int. J. Environ. Res. Public Health. 2018;15:2602. doi: 10.3390/ijerph15112602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aral K., Milward M.R., Kapila Y., Berdeli A., Cooper P.R. Inflammasomes and their regulation in periodontal disease: A review. J. Periodontal Res. 2020;55:473–487. doi: 10.1111/jre.12733. [DOI] [PubMed] [Google Scholar]
- 21.Hajishengallis G., Chavakis T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 2021;21:426–440. doi: 10.1038/s41577-020-00488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kamada N., Seo S.-U., Chen G.Y., Núñez G. Role of the gut microbiota in immunity and inflammatory disease. Nat. Rev. Immunol. 2013;13:321–335. doi: 10.1038/nri3430. [DOI] [PubMed] [Google Scholar]
- 23.Cader M.Z., Kaser A. Recent advances in inflammatory bowel disease: Mucosal immune cells in intestinal inflammation. Gut. 2013;62:1653–1664. doi: 10.1136/gutjnl-2012-303955. [DOI] [PubMed] [Google Scholar]
- 24.Cario E. Commensal-Innate Immune Miscommunication in IBD Pathogenesis. Dig. Dis. 2012;30:334–340. doi: 10.1159/000338120. [DOI] [PubMed] [Google Scholar]
- 25.Jain S., Darveau R.P. Contribution of Porphyromonas gingivalis lipopolysaccharide to periodontitis. Periodontology 2000. 2010;54:53–70. doi: 10.1111/j.1600-0757.2009.00333.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andrian E., Grenier D., Rouabhia M. Porphyromonas gingivalis-Epithelial Cell Interactions in Periodontitis. J. Dent. Res. 2006;85:392–403. doi: 10.1177/154405910608500502. [DOI] [PubMed] [Google Scholar]
- 27.Araújo V.M.A., Melo I.M., Lima V. Relationship between Periodontitis and Rheumatoid Arthritis: Review of the Literature. Mediat. Inflamm. 2015;2015:259074. doi: 10.1155/2015/259074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fiorillo L., Cervino G., Laino L., D’Amico C., Mauceri R., Tozum T.F., Gaeta M., Cicciù M. Porphyromonas gingivalis, Periodontal and Systemic Implications: A Systematic Review. Dent. J. 2019;7:114. doi: 10.3390/dj7040114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Furusho H., Miyauchi M., Hyogo H., Inubushi T., Ao M., Ouhara K., Hisatune J., Kurihara H., Sugai M., Hayes C.N., et al. Dental infection of Porphyromonas gingivalis exacerbates high fat diet-induced steatohepatitis in mice. J. Gastroenterol. 2013;48:1259–1270. doi: 10.1007/s00535-012-0738-1. [DOI] [PubMed] [Google Scholar]
- 30.Singhrao S.K., Olsen I. Assessing the role of Porphyromonas gingivalis in periodontitis to determine a causative relationship with Alzheimer’s disease. J. Oral Microbiol. 2019;11:1563405. doi: 10.1080/20002297.2018.1563405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rubin D.C., Shaker A., Levin M.S. Chronic intestinal inflammation: Inflammatory bowel disease and colitis-associated colon cancer. Front. Immunol. 2012;3:107. doi: 10.3389/fimmu.2012.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang Y.-Z., Li Y.-Y. Inflammatory bowel disease: Pathogenesis. World J. Gastroenterol. 2014;20:91–99. doi: 10.3748/wjg.v20.i1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chassaing B., Aitken J.D., Malleshappa M., Vijay-Kumar M. Dextran Sulfate Sodium (DSS)-Induced Colitis in Mice. Curr. Protoc. Immunol. 2014;104:15.25.1–15.25.14. doi: 10.1002/0471142735.im1525s104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Erben U., Loddenkemper C., Doerfel K., Spieckermann S., Haller D., Heimesaat M.M., Zeitz M., Siegmund B., Kühl A.A. A guide to histomorphological evaluation of intestinal inflammation in mouse models. Int. J. Clin. Exp. Pathol. 2014;7:4557–4576. [PMC free article] [PubMed] [Google Scholar]
- 35.Mudter J., Neurath M.F. Il-6 signaling in inflammatory bowel disease: Pathophysiological role and clinical relevance. Inflamm. Bowel Dis. 2007;13:1016–1023. doi: 10.1002/ibd.20148. [DOI] [PubMed] [Google Scholar]
- 36.Jones-Hall Y.L., Nakatsu C.H. The Intersection of TNF, IBD and the Microbiome. Gut Microbes. 2016;7:58–62. doi: 10.1080/19490976.2015.1121364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Parker A., Vaux L., Patterson A.M., Modasia A., Muraro D., Fletcher A.G., Byrne H.M., Maini P.K., Watson A.J.M., Pin C. Elevated apoptosis impairs epithelial cell turnover and shortens villi in TNF-driven intestinal inflammation. Cell Death Dis. 2019;10:108. doi: 10.1038/s41419-018-1275-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Danese S., Vermeire S., Hellstern P., Panaccione R., Rogler G., Fraser G., Kohn A., Desreumaux P., Leong R.W., Comer G.M., et al. Randomised trial and open-label extension study of an anti-interleukin-6 antibody in Crohn’s disease (ANDANTE I and II) Gut. 2019;68:40–48. doi: 10.1136/gutjnl-2017-314562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hwang I.-M., Sun L.-M., Lin C.-L., Lee C.-F., Kao C.-H. Periodontal disease with treatment reduces subsequent cancer risks. QJM Int. J. Med. 2014;107:805–812. doi: 10.1093/qjmed/hcu078. [DOI] [PubMed] [Google Scholar]
- 40.Carter C.J. Genetic, Transcriptome, Proteomic, and Epidemiological Evidence for Blood-Brain Barrier Disruption and Polymicrobial Brain Invasion as Determinant Factors in Alzheimer’s Disease. J. Alzheimer’s Dis. Rep. 2017;1:125–157. doi: 10.3233/ADR-170017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lübcke P.M., Ebbers M.N.B., Volzke J., Bull J., Kneitz S., Engelmann R., Lang H., Kreikemeyer B., Müller-Hilke B. Periodontal treatment prevents arthritis in mice and methotrexate ameliorates periodontal bone loss. Sci. Rep. 2019;9:8128. doi: 10.1038/s41598-019-44512-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nitzan O., Elias M., Peretz A., Saliba W. Role of antibiotics for treatment of inflammatory bowel disease. World J. Gastroenterol. 2016;22:1078–1087. doi: 10.3748/wjg.v22.i3.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gupta V., Rodrigues R., Nguyen D., Sauk J., Khalili H., Yajnik V., Ananthakrishnan A.N. Adjuvant use of antibiotics with corticosteroids in inflammatory bowel disease exacerbations requiring hospitalisation: A retrospective cohort study and meta-analysis. Aliment. Pharmacol. Ther. 2016;43:52–60. doi: 10.1111/apt.13454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McIlroy J., Ianiro G., Mukhopadhya I., Hansen R., Hold G.L. Review article: The gut microbiome in inflammatory bowel disease-avenues for microbial management. Aliment. Pharmacol. Ther. 2018;47:26–42. doi: 10.1111/apt.14384. [DOI] [PubMed] [Google Scholar]
- 45.Kapoor A., Malhotra R., Grover V., Grover D. Systemic antibiotic therapy in periodontics. Dent. Res. J. 2012;9:505–515. doi: 10.4103/1735-3327.104866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seo Y., Oh S.-J., Ahn J.-S., Shin Y.Y., Yang J.W., Kim H.-S. Implication of Porphyromonas gingivalis in colitis and homeostasis of intestinal epithelium. Lab. Anim. Res. 2019;35:26. doi: 10.1186/s42826-019-0029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jiao J., Jing W., Si Y., Feng X., Tai B., Hu D., Lin H., Wang B., Wang C., Zheng S., et al. The prevalence and severity of periodontal disease in Mainland China: Data from the Fourth National Oral Health Survey (2015–2016) J. Clin. Periodontol. 2021;48:168–179. doi: 10.1111/jcpe.13396. [DOI] [PubMed] [Google Scholar]
- 48.Nazir M., Al-Ansari A., Al-Khalifa K., Alhareky M., Gaffar B., Almas K. Global Prevalence of Periodontal Disease and Lack of Its Surveillance. Sci. World J. 2020;2020:2146460. doi: 10.1155/2020/2146160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wirtz S., Neurath M.F. Mouse models of inflammatory bowel disease. Adv. Drug Deliv. Rev. 2007;59:1073–1083. doi: 10.1016/j.addr.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 50.Low D., Nguyen D.D., Mizoguchi E. Animal models of ulcerative colitis and their application in drug research. Drug Des. Dev. Ther. 2013;7:1341–1357. doi: 10.2147/dddt.s40107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nakata T., Hirano S., Yokota Y., Takahashi H., Kimura B., Kuda T., Eto T., Kato M. Protective effects of heat-killed Lactococcus lactis subsp. lactis BF3, isolated from the intestine of chum salmon, in a murine model of DSS-induced inflammatory bowel disease. Biosci. Microbiota Food Health. 2016;35:137–140. doi: 10.12938/bmfh.2016-007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shin M.-R., Kim K.J., Kim S.H., Kim S.J., Seo B.-I., An H.-J., Roh S.-S. Comparative Evaluation between Sulfasalazine Alone and in Combination with Herbal Medicine on DSS-Induced Ulcerative Colitis Mice. BioMed Res. Int. 2017;2017:6742652. doi: 10.1155/2017/6742652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Perez-Brocal V., Garcia-Lopez R., Vazquez-Castellanos J.F., Nos P., Beltrán B., Latorre A., Moya A. Study of the Viral and Microbial Communities Associated With Crohn’s Disease: A Metagenomic Approach. Clin. Transl. Gastroenterol. 2013;4:e36. doi: 10.1038/ctg.2013.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Van Der Sluis M., Bouma J., Vincent A., Velcich A., Carraway K.L., Büller H.A., Einerhand A.W., van Goudoever J.B., VAN Seuningen I., Renes I.B. Combined defects in epithelial and immunoregulatory factors exacerbate the pathogenesis of inflammation: Mucin 2-interleukin 10-deficient mice. Lab. Investig. 2008;88:634–642. doi: 10.1038/labinvest.2008.28. [DOI] [PubMed] [Google Scholar]
- 55.Nishiyama Y., Kataoka T., Yamato K., Taguchi T., Yamaoka K. Suppression of Dextran Sulfate Sodium-Induced Colitis in Mice by Radon Inhalation. Mediat. Inflamm. 2012;2012:239617. doi: 10.1155/2012/239617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jammal M.P., Da Silva A.A., Filho A.M., Côbo E.D.C., Adad S.j., Murta E.F.C., Nomelini R.S. Immunohistochemical staining of tumor necrosis factor-α and interleukin-10 in benign and malignant ovarian neoplasms. Oncol. Lett. 2015;9:979–983. doi: 10.3892/ol.2014.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thongchot S., Vidoni C., Ferraresi A., Loilome W., Khuntikeo N., Sangkhamanon S., Titapun A., Isidoro C., Namwat N. Cancer-Associated Fibroblast-Derived IL-6 Determines Unfavorable Prognosis in Cholangiocarcinoma by Affecting Autophagy-Associated Chemoresponse. Cancers. 2021;13:2134. doi: 10.3390/cancers13092134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.