Abstract
The wear of acrylic denture teeth is a serious problem that can change the vertical dimensions of dentures. This study evaluates the effect of adding salinized nano ZrO2 particles on the microstructure, hardness, and wear resistance of acrylic denture teeth. Heat polymerizing polymethyl methacrylate resin was mixed with salinized ZrO2 at concentrations of 5 wt.% and 10 wt.%. Acrylic resin specimens without filler addition were used as a control group. SEM/EDS analyses were performed and the Vickers’ hardness was evaluated. Two-body wear testing was performed using a chewing simulator with a human enamel antagonist. After subjecting the samples to 37,500 cycles, both height loss and weight loss were used to evaluate the wear behavior. The microstructural investigation of the reinforced-denture teeth indicates sound nanocomposite preparation using the applied regime without porosity or macro defects. The addition of zirconium oxide nanofillers to PMMA at both 5% and 10% increased the microhardness, with values of up to 49.7 HV. The wear mechanism in the acrylic base material without nanoparticle addition was found to be fatigue wear; a high density of microcracks were found. The addition of 5 wt.% ZrO2 improved the wear resistance. Increasing the nanoparticles to 10 wt.% ZrO2 further improved the wear resistance, with no microcracks found.
Keywords: nanocomposite, acrylic denture teeth, nano ZrO2 particles, wear behavior, microstructure, microhardness, polymerization, polymethyl methacrylate resin
1. Introduction
Denture teeth are currently made of either methacrylate-based resins (acrylic resin) or porcelain, but acrylic teeth have nearly eliminated porcelain teeth from the market [1] due to a number of advantages, including their chemical bonding to the denture base [2,3], lower susceptibility to fracture [4,5] and decreased clicking [6,7]. Acrylic resin tooth wear is a serious complication during denture service and can change the vertical dimension of dentures. This process harms the denture and exerts an impact on facial aesthetics and the function of the masticatory muscles, resulting in less efficient mastication. This can result in temporomandibular disorders, digestive disturbances and decreased patient comfort [6,7,8,9]. Efforts were made to enhance the wear resistance of the acrylic resin denture teeth, such as the formation of cross-linked polymer teeth (interpenetrated polymer network) [8,9]. Another possible solution is to add nanofillers to enhance mechanical properties. Despite this, these materials are softer than composite resin or porcelain teeth [8,9,10]. Nano-fillers, such as metal oxides, carbon, and glass fibers have also been used to improve the mechanical behavior of the acrylic resin denture base materials [11,12,13,14,15,16]. Recently, zirconium oxide nanoparticles (ZrO2 NPs) have been recognized for their high biocompatibility. However, because they are white in color, they are thought to be less likely to change aesthetics than other metal oxide nanoparticles [17]. ZrO2 NPs are not only biocompatible but are also resistant to wear and corrosion. In addition to these characteristics, ZrO2 NPs offer high toughness and mechanical strength [18,19,20]. ZrO2 NPs are frequently used to mechanically reinforce polymers [12]. Saline coupling agents are applied to the surface of ZrO2 NPs to decrease the risk of aggregation and enhance compatibility with the polymer matrix [21]. The stresses caused by the dispersion of ZrO2 NPs are transferred from the weak Polymethylmethacrylate (PMMA) matrix to the strong nanoparticles [20]. Ayad et al. [18] reported a minor increase in the surface hardness and the impact strength of zirconium dioxide acrylic composite when compared to the unreinforced resin (control specimen). Another study reported a reduction in impact strength as well as surface hardness when 10 wt.% ZrO2 and 20 wt.% ZrO2 were added [22]. Alternatively, a study found that increasing the amount of modified (ZrO2) added to nano-ZrO2/PMMA composite increased the hardness by up to 10%, and increased the hardness of groups 5% and 10% (water storage groups) compared with the zero and 20% (p < 0.01). The highest hardness value was observed in group 5% (TC− 36.8, TC+ 35.2) [23,24]. Furthermore, after incorporating salinized zirconia NPs in acrylic resin, there was a significant increase in hardness and a minor improvement in surface roughness, as well as a decrease in porosity [25,26]. However, investigations into the addition of salinized nano-ZrO2 powder to acrylic resin teeth are lacking. The overall aim of this study is to develop nanocomposite denture teeth with high wear resistance. To this end, the effect of incorporating salinized nano-ZrO2 particles into acrylic resin on the acrylic denture tooth microstructure, hardness, and wear resistance was investigated.
2. Materials and Methods
2.1. ZrO2 Nanoparticles Surface Treatment
To enhance the ZrO2 nanoparticle’s wettability with the resin matrix through the formation of a reactive group on their surface, the salinization process was carried out in the laboratory of Inorganic Chemistry, Chemistry Department, Faculty of Science, Suez Canal University. The ZrO2 nanoparticle powder of 99.9% purity, with 9 ± 2 m2/g surface area and an average particle size of 40 ± 3 nm, (Nanogate, Cairo, Egypt) was saline-treated using the saline coupling agent 3-trimethoxysilyl propylmethacrylate (TMSPM) (Sigma-Aldrich, Berlin, Germany) [27]. This procedure was accomplished by mixing 30 g of ZrO2 nanoparticles with 0.3 g of TMSPM dissolved in 100 mL of acetone for 1 h with the help of a magnetic stirrer at 300 rpm (Hot plate with a magnetic stirrer, MSH-A 30A, Seoul, Korea) for 60 min. Subsequently, the solvent was removed using a rotary evaporator under vacuum for 30 min at 60 °C and 150 rpm, followed by heating for 2 h at 120 °C. Next, the treated powder was allowed to cool to 28 °C [28,29,30].
2.2. PMMA Powder of Artificial Teeth/ZrO2 Nanocomposite Preparation
The salinized nano-Zirconium oxide particles and PMMA powder of artificial teeth (Pigeon Dental Co Shanghai, Beijing, China) (Figure 1a) were pre-weighed using an electronic balance (Sartorius, Done Biopharmaceutical and Laboratories, Berlin, Germany) with an accuracy of 0.0001 gm so that the Nano-filler (Figure 1b) concentrations were 5% and 10% by weight. Pre-weighed Nano-filler ZrO2 powder with two concentrations (5% and 10%) was added individually to the heat polymerized PMMA powder of artificial teeth and thoroughly mixed using an electric mixer to produce a uniform blend and ensure that the homogeneous mix of PMMA/ZrO2, was mixed independently [18,20,29,31,32].
Figure 1.
Macro images for the raw material powder used in this work (a) acrylic resin powder of artificial teeth and (b) ZrO2 powder.
Twenty-four cylindrical samples 4 mm in diameter × 8 mm in height, were prepared from acrylic resin of teeth material. The control group (GI) was made from the conventional PMMA without zirconium oxide nano-particles. Two other groups GII, GIII, featured concentrations of 5 and 10 wt.% of zirconium oxide reinforced acrylic resin tooth-forming material. These samples were used to evaluate the wear behavior by using the chewing simulator and also to evaluate the hardness. Wax cylinders, of 8 mm × 100 mm shown in Figure 2, (Cavex, Haarlem, The Netherlands) were used for wax pattern fabrication that invested in a metal flask with dental stone (Zeta Mufle, Nevilicure, Italy).
Figure 2.
An image for the metal flask with the wax specimens invested and a magnified region of the wax specimen.
After setting the stone, the wax was melted by placing the flasks in a wax elimination machine for 10 min. After removing the softened wax and all wax traces, a separating medium (Acrostone(A), Anglo-Egyptian Company. Hegaz, Cairo, Egypt, Batch No.505/04) was applied on the warm stone mold surfaces. When the flasks cooled to room temperature, heat-polymerized resin (pure or reinforced with nano-ZrO2) was mixed and packed into the mold spaces at the dough stage. The flask parts were brought together under pressure using a hydraulic bench press for 5 min and then allowed to rest for 30 min. To polymerize the resin, the flasks were placed in a laboratory curing bath for 90 min at 74 °C, and then 30 min at 100 °C. After curing, the flasks were left for slow bench cooling till 28 °C before opening. Acrylic samples were retrieved from the stone, finished, and polished. Initially, the excess resin was trimmed using progressively finer grits of silicon carbide papers (grits 120–500) in wet conditions, followed by polishing using a rag wheel and pumice on a dental lathe and felt disc on a polishing machine, and the samples were cut to the required dimensions (4 × 8 mm). A digital micrometer (Mitutoyo, Digimatic Caliper 25SB, Mitutoyo Corporation, Tokyo, Japan) with a precision of 1/1000 was used to measure specimen dimensions [27]. An electronic balance (Sartorius, Biopharmaceutical and Laboratories, Berlin, Germany) with an accuracy of 0.001 gm was used to measure samples weight before and after the wear test.
2.3. Micro-Hardness Test Procedure
Micro-hardness of all the acrylic samples was investigated using Digital Display Vickers Micro-hardness Tester (Model HVS-50, Laizhou Huayin Testing Instrument Co., Ltd. Beijing, China) using a Vickers diamond indenter with a 20× objective lens. A load of 0.98 N was applied to the surface of the specimens for a 10 s dwell time. Three indentations, which were equally placed over a circle and not closer than 0.5 mm to the adjacent indentations, were made on the surface of each sample. The diagonal length of the indentations was measured by a built-in scaled microscope and Vickers micro-hardness values were obtained [30]. The micro-hardness mean value was then calculated for each sample. The micro-hardness was obtained using Equation (1).
| HV = 1.854 P/d2 | (1) |
where HV is Vickers hardness in Kgf/mm2, P is the load in Kgf, and d is the length of the diagonals in mm.
2.4. Wear Testing with Natural Teeth Surface Antagonist
Carie-free human premolar teeth without fractures or worn cusps that were recently extracted for orthodontic treatment plans were chosen for this study and stored in 0.1% thymol solution (approved by the accredited ethics committee of the Faculty of Dentistry Suez Canal University, no297/2020). The buccal cusps with buccal surface were cut using no. 943 Miniflex diamond disc (Brasseler, Lemgo, Germany). They were then inserted into a self-cured acrylic resin mold (Acrostone Co., Cairo, Egypt) inside copper specimen holder with diameter15 mm. The insertion of the natural tooth surfaces was guided by a dental surveyor to ensure proper alignment of the tooth surface to the long axis of the specimen holder [33,34]. Figure 3 shows the assembly of the natural teeth within the self-cured acrylic resin mold.
Figure 3.
Image of assembly of the natural teeth within the self-cured acrylic resin mold.
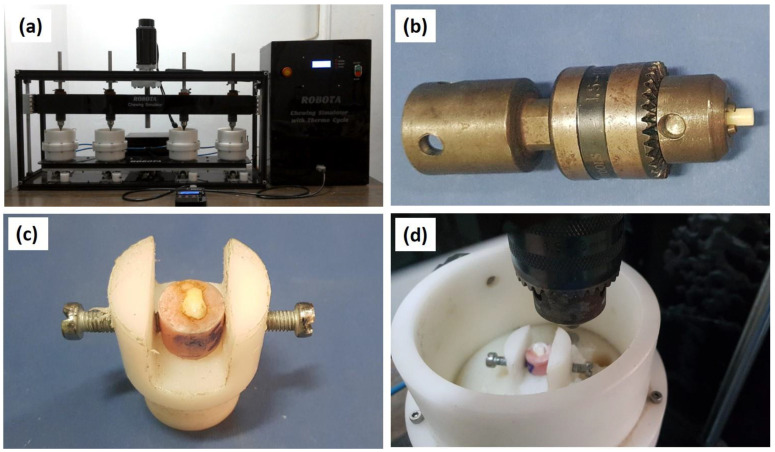
As a preparation for the wear test, the buccal surface of each tooth specimen was wet abraded and finished with grit abrasive paper (1000, 2500, and 4000), to a total depth of 0.5 mm. As a result, a flat area of about 2–3 mm was obtained for loading during the wear test [34,35]. Next, the two-body wear test was performed using the newly developed four stations multimodal Dual-axis ROBOTA chewing simulator integrated with thermo-cyclic protocol operated on servo-motor (Model ACH-09075DC-T, AD-TECH Technology Co., LTD., Berlin, Germany). The device allows the simulation of vertical and horizontal movements simultaneously in the thermodynamic condition in a range of 5 °C to 55 °C with a dwell time of 10 s. The ROBOTA chewing simulator features four chambers, each consisting of an upper part as a sample holder and a lower plastic antagonist holder Figure 4a. Samples were mounted into the metal receptacle present in the chewing simulator upper part Figure 4b. All the samples were tested under standard conditions in which the buccal surface of premolar teeth was used in the lower plastic holder of the device acting as antagonist Figure 4c. The acrylic samples were positioned on the upper samples holder in point contact with the teeth surfaces Figure 4d. A weight of 5 kg, which is comparable to 49 N of chewing force, was exerted. The samples were subjected to 37,500 cycles to simulate three months of clinical function. After 37,500 cycles, the samples were removed from the holder, cleaned with running water, and followed by cleaning in an ultrasonic cleaner for 2 min to remove any abraded particles from the surface before measurements.
Figure 4.
Images of the wear testing stages: (a) chewing simulator setup, (b) fixing the acrylic teeth sample in the holder, (c) plastic holder of the device acting as the antagonist, (d) positioning of the upper samples holder in point contact with the teeth surfaces.
Both height loss and weight loss were used to evaluate the wear behavior of the pure PMMA- and ZrO2-reinforced tooth samples. Height loss was measured using the digital micrometer (Mitutoyo, Digimatic Caliper 25SB, Mitutoyo Corporation, Tokyo, Japan) with a precision of 1/1000. The difference between the readings before and after the wear simulation gave the amount of vertical sample height loss. Furthermore, weight loss was measured by weighing samples in the electronic analytical balance (Sartorius, Biopharmaceutical and Laboratories, Berlin, Germany) with an accuracy of 0.001 gm to show the difference in weight before and after the wear test. As this electronic balance featured a fully automated calibration technology and a micro weighing scale, values of all the mounted discs and antagonist samples were accurately measured. Each mounted sample was cleaned and dried with tissue paper before weighing. All data were calculated, tabulated, and statistically analyzed using SPSS for Windows, version 22.0 (Statistical Package for Social Science, Armonk, NY, USA: IBM Corp) at significant levels 0.05 (p-Value ≤ 0.5). A normality test was done to check the normal distribution of the sample, and all groups and subgroups showed normal distributions.
-
(A)
Descriptive data: Descriptive statistics were calculated in the form of Mean ± Standard deviation (SD), median, range (Max-Min).
-
(B)
ANOVA—test: One-way ANOVA (Analysis of variance) was used to compare between the three groups under study. Tukey Post hoc test was performed for the evaluation of statistical significance among the groups. p-value ≤ 0.05 is considered to be statistically significant.
2.5. Microstuctur Investigation
The microstructure of the acrylic nanocomposites was investigated using optical microscopy (OM) and scanning electron microscopy (SEM) equipped with EDS analysis. For the microstructural analysis, the samples were prepared using grinding with conventional silicon carbide emery papers of different grit sizes and then mechanically polished using alumina suspension of 0.05 µm [36,37]. Furthermore, the samples were investigated with SEM after the wear testing to study the worn surface and determine the wear mechanisms.
3. Results
3.1. Acrylic/ZrO2 Nanocomposites Microstructure
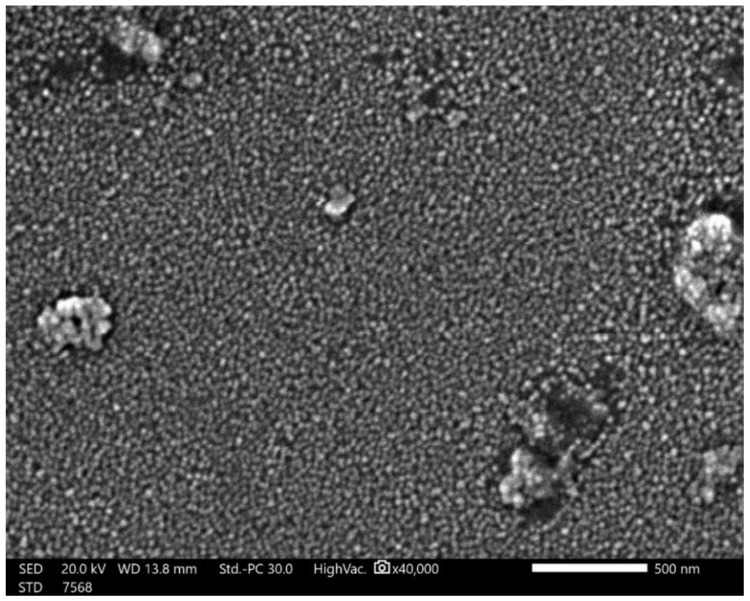
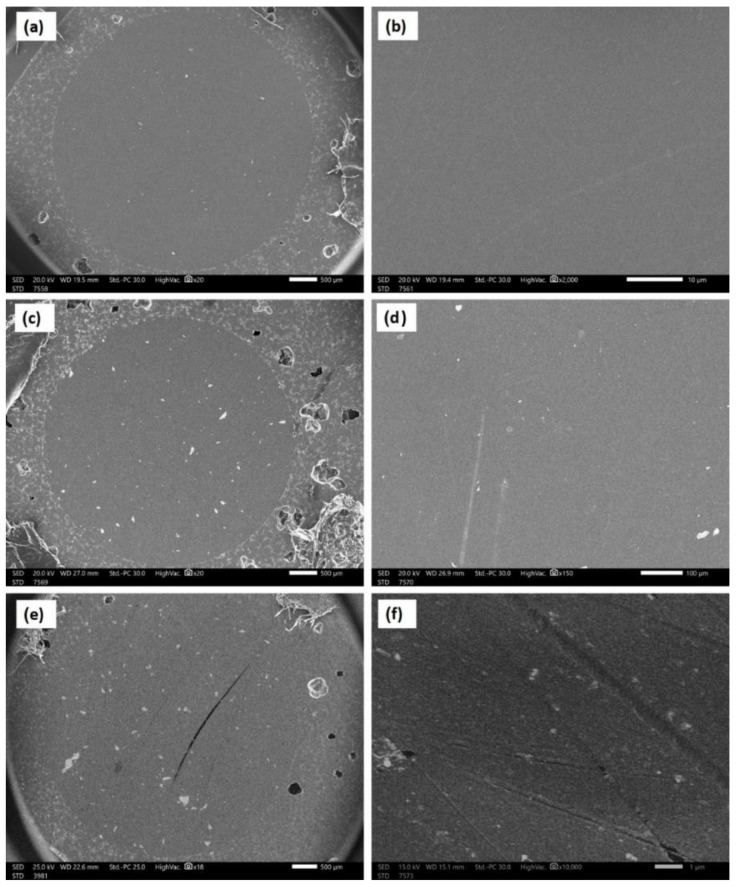
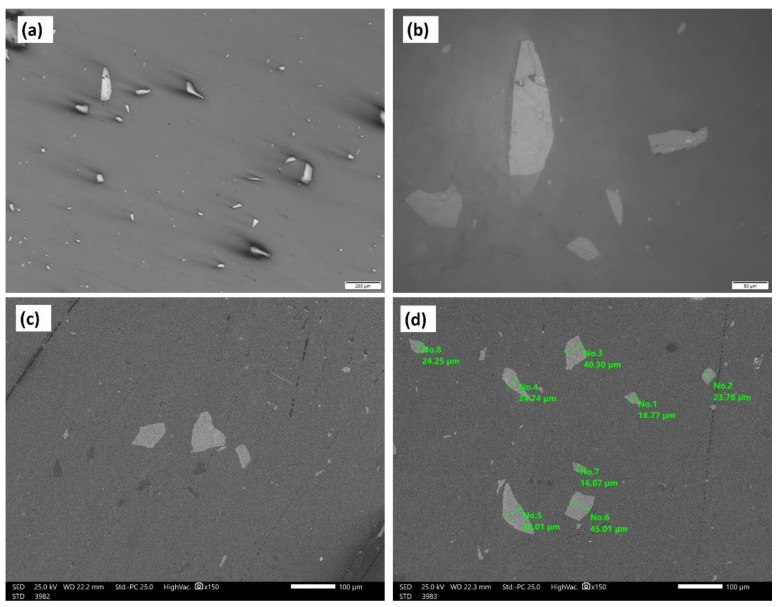
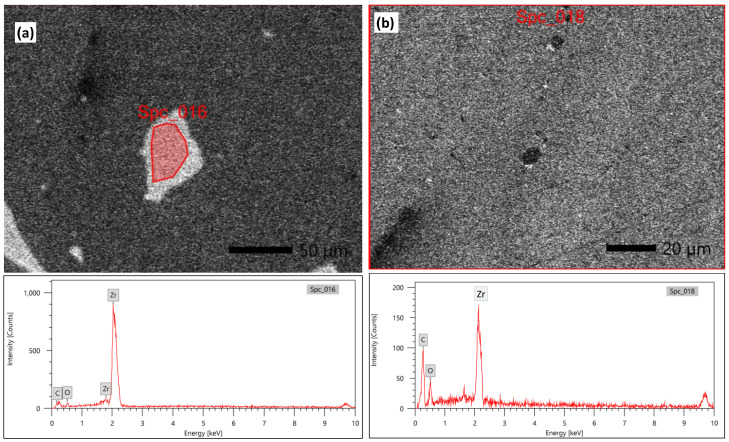
Figure 5 shows an SEM micrograph of the raw material powder of the ZrO2 nanoparticles that were used as reinforcing materials for the acrylic matrix. It can be observed that the powder is of nano-scale, with an almost homogenous particle size that is below 50 nm, except for some agglomerated particles of submicron or micron size. Figure 6 shows the SEM macro and micrographs of the base acrylic material (Figure 6a,b), 5 wt.% ZrO2 nanocomposites (Figure 6c,d) and 10 wt.% ZrO2 nanocomposites (Figure 6e,f). At the macro level, the samples showed no porosity defects, which indicates the effectiveness of the production procedure at producing sound acrylic nanocomposites at different percentages. On the other hand, the presence of macro-size particles, which increased in line with the increase in the ZrO2 weight percentage, can be observed. The sources of these macro-sized particles were the ZrO2 particles, as some macro-sized particles were noted within the SEM micrograph of the raw powder. In addition, at the micro-level, no defects were observed either, and nanoparticles can only be observed in the sample of 10 wt.% ZrO2 (Figure 6f). Figure 7 shows the optical microstructure at different magnifications (Figure 7a,b) and the SEM microstructure at different positions (Figure 7c,d) for the acrylic with 10 wt.% ZrO sample. The micrographs show a macro-sized particle, with some particle measurements indicated. The EDS analysis of the micro-sized particle is presented in Figure 8a and the EDS of the nano-composite is shown in Figure 8b. The EDS analysis confirmed that the large size particles were mainly ZrO2 particles and also confirmed the presence of ZrO2 nanoparticles in the acrylic matrix, as indicated in Figure 8b. In addition, the peak carbon can be seen in both EDS charts. This may have been due to the polymeric material and may have resulted from interference from the instrument [38,39].
Figure 5.
SEM micrograph for the raw material powder of the ZrO2 nanoparticles used as a reinforcing material for the acrylic matrix.
Figure 6.
SEM macro and micrographs of the base acrylic material(a,b), (c,d) 5 wt.% ZrO2 nano-composites (c,d) and 10 wt.% ZrO2 nano-composites (e,f).
Figure 7.
Optical microstructure at different magnifications (a,b) and SEM microstructure at different positions (c,d) for the acrylic with 10 wt.% ZrO sample.
Figure 8.
The EDS analysis of the micro-sized particle is presented in (a) and the EDS of the nano-composite (b).
3.2. Micro-Hardness Analysis
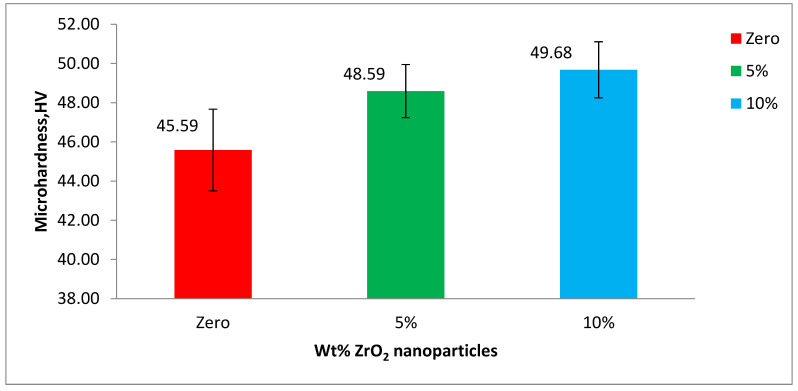
The mean microhardness values and their statistical data were obtained by analysis of variance (one-way ANOVA) at p-value < 0.05, for the base acrylic material and the ZrO2-reinforced groups. Furthermore, the data are illustrated in Figure 9 as a bar chart of microhardness against the wt.% of the ZrO2 nanoparticles. The microhardness of the base acrylic material is 45.59 HV that increased to 48.59 HV after adding 5 wt.% ZrO2 nanoparticles. A further increase in microhardness, up to 49.68 HV, was produced by increasing the concentration of the ZrO2 nanoparticles to 10 wt.%.
Figure 9.
Mean hardness (VHN) of the tested groups of PMMA.
3.3. Wear Behavior
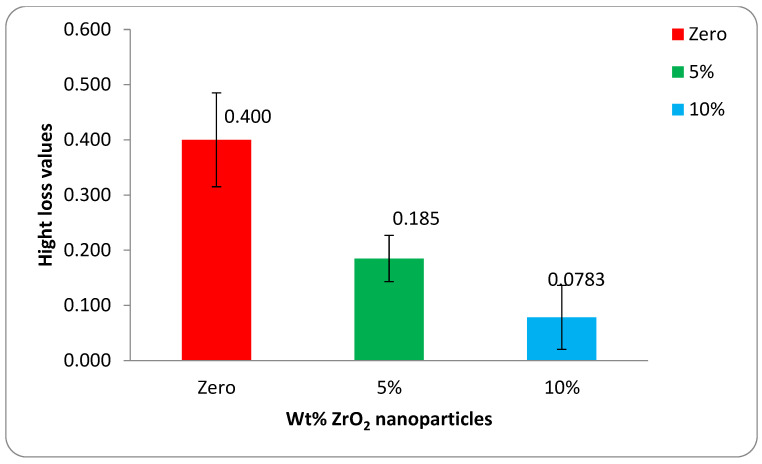
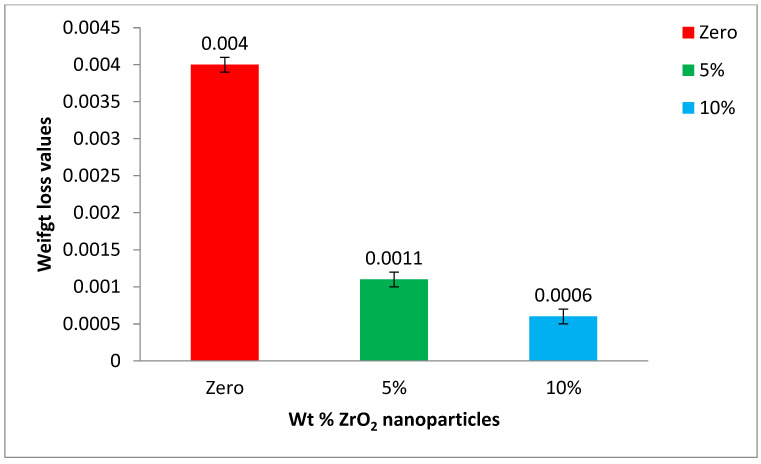
The mean height loss values and their statistical data were obtained by analysis of variance (one-way ANOVA) at p-value < 0.05 for the base acrylic material and the ZrO2-reinforced groups. The data are illustrated in Figure 10 as a bar chart of the mean height loss against the wt.% of the ZrO2 nanoparticles. Furthermore, the mean weight loss values and their statistical data were obtained by analysis of variance (one-way ANOVA) at p-value < 0.05 for the base acrylic material and the ZrO2-reinforced groups. The data are illustrated in Figure 11 as a bar chart of the mean weight loss against the wt.% of ZrO2 nanoparticles. The results of the wear tests of the height loss and weight loss both indicate a significant improvement in the wear resistance due to the addition of the ZrO2 nanoparticles and that the wear resistance increased by increasing the ZrO2 nanoparticle concentration.
Figure 10.
Mean height loss of the tested groups after wear testing.
Figure 11.
Mean weight loss of the tested groups after wear testing.
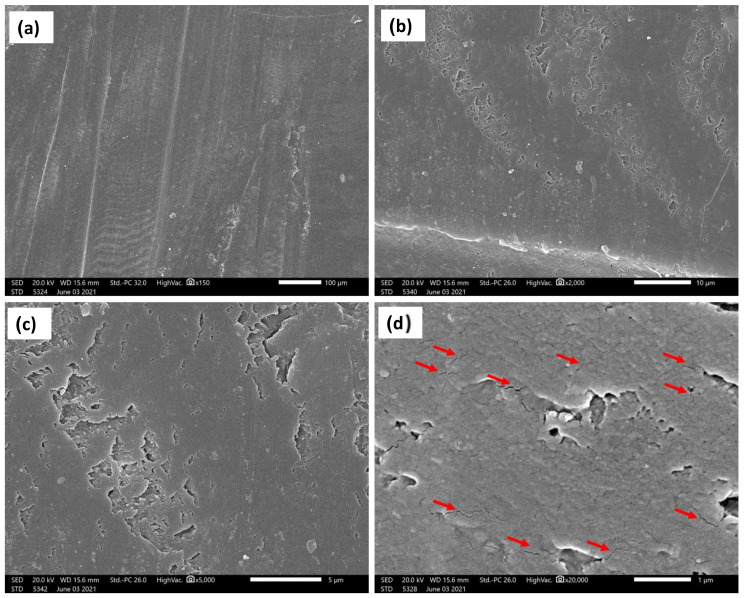
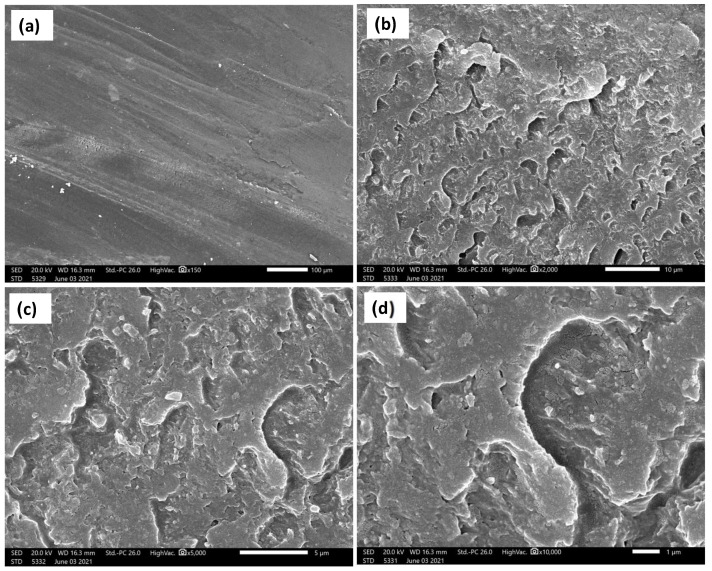
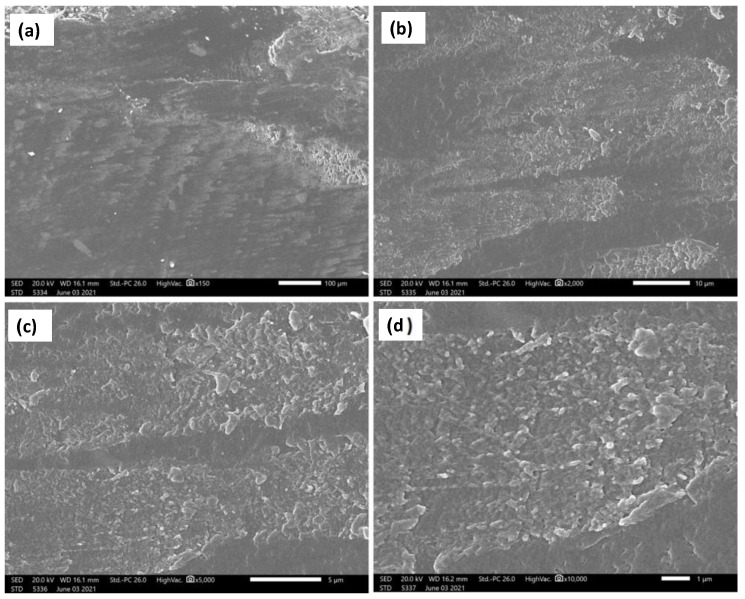
The current investigation showed a significant enhancement of the wear resistance by adding ZrO2 nanoparticles. Figure 12, Figure 13 and Figure 14 show the SEM micrographs at different magnifications, (a) 150×, (b) 2000×, (c) 5000×, and (d) 20,000× (Figure 12) and 10,000× (Figure 13 and Figure 14), for the wear surface of the different groups after conducting the wear test. The wear surface of the acrylic base material without ZrO2 nanoparticles (Figure 12) showed severe wear features with deep wear tracks that can be observed on the low magnifications micrograph (a) 150×. Furthermore, a high density of microcracks (indicated by red arrows (d) 20,000×) can be observed on the highest magnification micrograph. The incorporation of the ZrO2 nanoparticles changed the wear features of the wear surface, as can be observed in Figure 13 for the 5 wt.% ZrO2 and in Figure 14 for the 10 wt.% ZrO2. Less severe wear features were observed as the smoothness of the surface increased, in line with the increasing ZrO2 content. In addition, no microcracks were observed, especially at 10 wt.% ZrO2.
Figure 12.
SEM micrographs at different magnifications and positions of the base acrylic material after wear test. Red arrows indicate the microcracks. (a) 150×, (b)2000×, (c) 5000× and (d) 20,000×.
Figure 13.
SEM micrographs at different magnifications and positions of the 5 wt.% ZrO2 acrylic nanocomposite material after wear test. (a) 150×, (b)2000×, (c) 5000× and (d) 10,000×.
Figure 14.
SEM micrographs at different magnifications and positions of the 10wt.% ZrO2 acrylic nanocomposite material after wear test. (a) 150×, (b)2000×, (c) 5000× and (d)10,000×.
4. Discussion
Developing new materials with improved properties, especially high wear resistance, is an important focus of research. Thus, this work focuses on the improvement of wear resistance of acrylic denture teeth through the use of nanoparticle filler material. Different weight percentages of ZrO2 nanofillers (5% and 10%) were used with the acrylic matrix. The addition of zirconia filler significantly increased the Vicker’s hardness of the tested materials. This may have been due to the characteristics of the ZrO2 particles, as well as high interfacial shear strength between the nanofiller and resin matrix, which in turn increased the resistance of the material for penetration [40]. Similar results have been reported in previous studies [9,12]. The increase in microhardness by about 6–8% relative to the base material is similar to that reported in previous studies. Hameed and Abd-Elrahaman [25] investigated the effect of ZrO2 nanoparticles on the properties of acrylic denture base and reported an increase of about 5% in microhardness when increasing ZrO2 nanoparticles up to 7%.
Wear resistance is an important requirement of prosthetic materials, such as denture teeth, which do not provide a durable functional and esthetic restoration unless they exhibit high wear resistance [41]. Intraoral wear is a complex process related to both the composition of denture teeth and the patient’s oral condition. The ability to replicate and control these factors intraorally is challenging. Therefore, in vitro two-body wear testing is a valid model to measure antagonist wear without involving an intermediate medium that may influence the results [42]. The height and weight loss of the samples were evaluated. In dentistry, height loss is a more clinically relevant parameter, because the vertical distance between the maxilla and mandible is stabilized by the occlusal contact points. However, weight loss provides more accurate measurements, as indicated by lower variation. The wear resistance was significantly improved after the addition of zirconia nanofillers to the polymer matrix at both 5% and 10% concentrations. This result agrees with previous studies, in which concentrations of saline-treated alumina 0.1% [41] and silver nanoparticles 0.2–8% [43] considerably improved the resin wear resistance of PMMA. In terms of the effect of surface roughness on wear resistance, Benli et al. [44] investigated the relationship between the wear rate and surface roughness of occlusal splint materials made of contemporary and high-performance polymers and found that it is directly proportional. Furthermore, Nayyer et al. [45] reported that surface roughness is affected by clinical adjustments such as polishing, because polishing leads to smooth surfaces that undergo less wear and provides the advantage of extended longevity of the restoration [46,47]. It should be mentioned here that in this study, the samples were examined for wear behavior without polishing; thus it was expected that the polishing would significantly improve the wear resistance of the developed nanocomposites.
This improvement can be attributed to the fact that the ZrO2 particles exhibited greater hardness than the surrounding resin matrix and, therefore, were not as easily abraded by the antagonist [40]. The SEM of the acrylic base material without ZrO2 particles (Figure 12) showed high-density microcracks, which may have been the main mechanism behind the deterioration of the surface and the high reduction in both the height and weight observed in the measurements above. This might indicate that the type of wear was fatigue wear due to the formation of cracks under the subsurface. It has been reported that fatigue wear occurs when microcracks form below the surface of a material and eventually coalesce to free a small fragment of the material. Materials with a lower elastic modulus, such as unfilled resins, are susceptible to fatigue wear [42]. Furthermore, increasing the concentration of ZrO2 from 5% to 10% produced more improvement in the wear resistance, which can be attributed to the change in the wear mechanism from fatigue wear to abrasive wear type. This was confirmed by the elimination of microcracks at high ZrO2 particle concentrations, as can be observed in Figure 14. The results suggest that wear resistance may be influenced not only by the presence or absence of fillers, but also by the type, amount and size of the filler particles, as well as by how the filler particles are integrated into the matrix. However, the results of this study can provide guidance because the applied in vitro test arrangement cannot fully replicate the intraoral conditions. Although the use of natural enamel as an antagonist is considered the gold standard, disadvantages do exist, including variability in the form, fluoride content, and amount of aprismatic enamel; therefore, standardizing each stylus is not easy [48]. Further in vivo studies are needed to investigate the effect of adding nano ZrO2 with different concentrations on wear resistance and other mechanical properties intraorally in acrylic resin denture teeth.
5. Conclusions
This study investigated the effect of using ZrO2 nanoparticles as a filler material in acrylic denture teeth, aiming to enhance the wear resistance. Based on the obtained results, the following conclusions can be drawn:
-
(1)
The microstructural investigation of reinforced denture teeth indicates sound material preparation using the applied regime without porosity or macro defects. No segregation was observed for the nanoparticles; only submicron-sized ZrO2 particles were found.
-
(2)
The addition of zirconium oxide nanofillers to PMMA at both 5% and 10% increased the microhardness, with values up to 49.7 HV found after the addition of 10 wt.% ZrO2.
-
(3)
The wear mechanism in the acrylic base material without nanoparticle addition was found to be fatigue wear; a high density of microcracks was found.
-
(4)
The addition of 5 wt.% ZrO2 significantly reduced weight loss and height loss relative to the base material, which indicates improved wear resistance.
-
(5)
Increasing the nanoparticles to 10 wt.% ZrO2 further improved the wear resistance, with no microcracks found.
Acknowledgments
Sabry A. El-Korashy at Suez Canal University is greatly acknowledged for his support in carrying out the salinization process in the laboratory of Inorganic Chemistry, Chemistry Department, Faculty of Science. Furthermore, Mohamed M. Elsayed Seleman at Suez University is greatly acknowledged for his support in conducting the microstructural investigations.
Author Contributions
Conceptualization, K.M.E.-T., D.A.B. and M.E.E.-S.; methodology, K.M.E.-T., D.A.B. and M.E.E.-S.; software, K.M.E.-T. and D.A.B.; validation, K.M.E.-T., D.A.B. and M.E.E.-S.; formal analysis, K.M.E.-T., D.A.B. and M.E.E.-S.; investigation K.M.E.-T., M.M.Z.A., D.A.B. and M.E.E.-S.; resources, K.M.E.-T., D.A.B. and M.E.E.-S.; data curation, K.M.E.-T., D.A.B. and M.E.E.-S.; writing—original draft preparation, K.M.E.-T., M.M.Z.A., D.A.B. and M.E.E.-S.; writing—review and editing, K.M.E.-T., M.M.Z.A. and D.A.B.; visualization K.M.E.-T., M.M.Z.A., D.A.B. and M.E.E.-S.; supervision, K.M.E.-T., M.M.Z.A., I.A. and D.A.B.; project administration, K.M.E.-T., M.M.Z.A. and D.A.B.; funding acquisition, M.M.Z.A. and I.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
This will be made available upon request through the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stober T., Lutz T., Gilde H., Rammelsberg P. Wear of resin denture teeth by two-body contact. Dent. Mater. 2006;22:243–249. doi: 10.1016/j.dental.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Kawano F., Ohguri T., Ichikawa T., Mizuno I., Hasegawa A. Shock absorbability and hardness of commercially available denture teeth. Int. J. Prosthodont. 2002;15:243–247. [PubMed] [Google Scholar]
- 3.Beall J.R. Wear of acrylic resin teeth (progress report) J. Am. Dent. Assoc. 1943;30:252–256. doi: 10.14219/jada.archive.1943.0043. [DOI] [Google Scholar]
- 4.Adams L.P., Jooste C.H., Thomas C.J., Harris A.M.P. Biostereometric quantification of clinical denture tooth wear. J. Oral Rehabil. 1996;23:667–674. doi: 10.1046/j.1365-2842.1996.d01-178.x. [DOI] [PubMed] [Google Scholar]
- 5.Satoh Y., Nagai E., Maejima K., Azaki M. Wear of denture teeth by use of metal plates part 2: Abrasive wear of posterior teeth. J. Nihon Univ. 1992;34:16–27. doi: 10.2334/josnusd1959.34.16. [DOI] [PubMed] [Google Scholar]
- 6.Akin H., Tugut F., Guney U., Akar T. Shear bond strength of denture teeth to two chemically different denture base resins after various surface treatments. J. Prosthodont. 2014;23:152–156. doi: 10.1111/jopr.12081. [DOI] [PubMed] [Google Scholar]
- 7.Mello P.C., Coppedê A.R., Macedo A.P., Da M., De Mattos G.C., Cristina R., Rodrigues S., Ribeiro R.F. Abrasion wear resistance of different artificial teeth opposed to metal and composite antagonists. J. Appl. Oral Sci. 2009;17:451–457. doi: 10.1590/S1678-77572009000500019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamonwanon P., Yodmongkol S., Chantarachindawong R., Thaweeboon S., Thaweeboon B., Srikhirin T. Wear resistance of a modified polymethyl methacrylate artificial tooth compared to five commercially available artificial tooth materials. J. Prosthet. Dent. 2015;114:286–292. doi: 10.1016/j.prosdent.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Stober T., Henninger M., Schmitter M., Pritsch M., Rammelsberg P. Three-body wear of resin denture teeth with and without nanofillers. J. Prosthet. Dent. 2010;103:108–117. doi: 10.1016/S0022-3913(10)60014-5. [DOI] [PubMed] [Google Scholar]
- 10.Suwannaroop P., Chaijareenont P., Koottathape N., Takahashi H., Arksornnukit M. In vitro wear resistance, hardness and elastic modulus of artificial denture teeth. Dent. Mater. J. 2011;30:461–468. doi: 10.4012/dmj.2010-200. [DOI] [PubMed] [Google Scholar]
- 11.Gürbüz Ö.A., Ünalan F., Kursoglu P. In vitro wear of denture teeth acrylic resin milled glass fiber composite. Oral Health Dent. Manag. Black Sea Ctries. 2005;4:46–51. [Google Scholar]
- 12.Gad M.M., Rahoma A., Al-Thobity A.M., ArRejaie A.S. Influence of incorporation of ZrO2 nanoparticles on the repair strength of polymethyl methacrylate denture bases. Int. J. Nanomed. 2016;11:5633–5643. doi: 10.2147/IJN.S120054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghaffari T., Barzegar A., Rad F.H., Moslehifard E., Author C. Effect of nanoclay on thermal conductivity and flexural strength of polymethyl methacrylate acrylic resin. J. Dent. Shiraz. Univ. Med. Sci. 2016;17:121–127. [PMC free article] [PubMed] [Google Scholar]
- 14.Labella R., Braden M., Deb S. Novel hydroxyapatite-based dental composites. Biomaterials. 1994;15:1197–1200. doi: 10.1016/0142-9612(94)90269-0. [DOI] [PubMed] [Google Scholar]
- 15.Ghahremani L., Shirkavand S., Akbari F., Sabzikari N. Tensile strength and impact strength of color modified acrylic resin reinforced with titanium dioxide nanoparticles. J. Clin. Exp. Dent. 2017;9:e661–e665. doi: 10.4317/jced.53620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mc Nally L., O’Sullivan D.J., Jagger D.C. An in vitro investigation of the effect of the addition of untreated and surface treated silica on the transverse and impact strength of poly(methyl methacrylate) acrylic resin. Biomed. Mater. Eng. 2006;16:93–100. [PubMed] [Google Scholar]
- 17.Gad M.M., Al-Thobity A.M., Rahoma A., Abualsaud R., Al-Harbi F.A., Akhtar S. Reinforcement of PMMA denture base material with a mixture of ZrO2 nanoparticles and glass fibers. Int. J. Dent. 2019;2019:2489393. doi: 10.1155/2019/2489393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ayad N.M., Dawi M.F., Fatah A.A. Effect of reinforcement of high-impact acrylic resin with micro-Zirconia on some physical and mechanical properties. Rev. Clínica Pesqui. Odontológica. 2008;4:145–151. [Google Scholar]
- 19.Gad M., Arrejaie A.S., Abdel-Halim M.S., Rahoma A. The reinforcement effect of nano-zirconia on the transverse strength of repaired acrylic denture base. Int. J. Dent. 2016;2016:7094056. doi: 10.1155/2016/7094056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gad M.M., Abualsaud R., Rahoma A., Al-Thobity A.M., Al-Abidi K.S., Akhtar S. Effect of zirconium oxide nanoparticles addition on the optical and tensile properties of polymethyl methacrylate denture base material. Int. J. Nanomed. 2018;13:283–292. doi: 10.2147/IJN.S152571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang E., Cheng G., Pang X., Ma X., Xing F. Synthesis of nano-ZnO/poly(methyl methacrylate) composite microsphere through emulsion polymerization and its UV-shielding property. Colloid Polym. Sci. 2006;284:422–428. doi: 10.1007/s00396-005-1389-z. [DOI] [Google Scholar]
- 22.Asopa V., Suresh S., Khandelwal M., Sharma V., Asopa S.S., Kaira L.S. A comparative evaluation of properties of zirconia reinforced high impact acrylic resin with that of high impact acrylic resin. Saudi J. Dent. Res. 2015;6:146–151. doi: 10.1016/j.sjdr.2015.02.003. [DOI] [Google Scholar]
- 23.Safi I.N., Hassanen K.A., Ali N.A. Assessment of zirconium oxide nano-fillers incorporation and silanation on impact, tensile strength and color alteration of heat polymerized acrylic resin. J. Baghdad Coll. Dent. 2012;24:36–42. [Google Scholar]
- 24.Ergun G., Sahin Z., Ataol A. The effects of adding various ratios of zirconium oxide nanoparticles to poly (methyl methacrylate) on physical and mechanical properties. J. Oral Sci. 2018;60:304–315. doi: 10.2334/josnusd.17-0206. [DOI] [PubMed] [Google Scholar]
- 25.Ali Sabri B., Satgunam M., Abreeza N.M., Abed A.N. A review on enhancements of PMMA denture base material with different nano-fillers. Cogent Eng. 2021;8:1875968. doi: 10.1080/23311916.2021.1875968. [DOI] [Google Scholar]
- 26.Mohammed D., Mudhaffar M. Effect of modified zirconium oxide nano-fillers addition on some properties of heat cure acrylic denture base material. J. Baghdad Coll. Dent. 2012;24:1–7. [Google Scholar]
- 27.Zidan S., Silikas N., Alhotan A., Haider J., Yates J. Investigating the mechanical properties of ZrO2-impregnated PMMA nanocomposite for denture-based applications. Materials. 2019;12:1344. doi: 10.3390/ma12081344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eltamimi K.M., Bayoumi D. Microtesile bond strength of zirconia Nano-fillers reinforced acrylic resin to denture teeth after thermocylcling. Egypt. Dent. J. 2021;67:767–774. doi: 10.21608/edj.2021.52464.1394. [DOI] [Google Scholar]
- 29.Gad M.M., Fouda S.M., ArRejaie A.S., Al-Thobity A.M. Comparative effect of different polymerization techniques on the flexural and surface properties of acrylic denture bases. J. Prosthodont. 2019;28:458–465. doi: 10.1111/jopr.12605. [DOI] [PubMed] [Google Scholar]
- 30.Yuzugullu B., Acar O., Cetinsahin C., Celik C. Effect of different denture cleansers on surface roughness and microhardness of artificial denture teeth. J. Adv. Prosthodont. 2016;8:333–338. doi: 10.4047/jap.2016.8.5.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang X.Y., Zhang X.J., Huang Z.L., Zhu B.S., Rong-Rong R.R.C. Hybrid effects of zirconia nanoparticles with aluminum borate whiskers on mechanical properties of denture base resin PMMA. Dent. Mater. J. 2014;33:141–146. doi: 10.4012/dmj.2013-054. [DOI] [PubMed] [Google Scholar]
- 32.Pero A.C., Scavassin P.M., Leite A.R., Marin D.O., Paleari A.G., Compagnoni M.A. Effect of immersion cleansers on the bond strength between a denture base resin and acrylic resin teeth. Int. J. Adhes. Adhes. 2013;44:180–183. doi: 10.1016/j.ijadhadh.2013.02.011. [DOI] [Google Scholar]
- 33.Fisher R.M., Moore B.K., Swartz M.L., Dykema R.W. The effects of enamel wear on the metal-porcelain interface. J. Prosthet. Dent. 1983;50:627–631. doi: 10.1016/0022-3913(83)90198-1. [DOI] [PubMed] [Google Scholar]
- 34.Ghazal M., Yang B., Ludwig K., Kern M. Two-body wear of resin and ceramic denture teeth in comparison to human enamel. Dent. Mater. 2008;24:502–507. doi: 10.1016/j.dental.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 35.Ghazal M., Hedderich J., Kern M. Wear of feldspathic ceramic, nano-filled composite resin and acrylic resinartificial teeth when opposed todifferent antagonists. Eur. J. Oral Sci. 2008;116:585–592. doi: 10.1111/j.1600-0722.2008.00573.x. [DOI] [PubMed] [Google Scholar]
- 36.Ahmed M.M.Z., Elnaml A., Shazly M., El-Sayed Seleman M.M. The effect of top surface lubrication on the friction stir welding of polycarbonate sheets. Int. Polym. Process. 2021;36:94–102. doi: 10.1515/ipp-2020-3991. [DOI] [Google Scholar]
- 37.Shazly M., Ahmed M.M.Z., El-Raey M. Friction stir welding of polycarbonate sheets. In: Carpenter J.S., Bai C., Hwan -Y.J., Ikhmayies S., Li B., Monteiro S.N., Peng Z., Zhang M., editors. Characterization of Minerals, Metals, and Materials. Wiley; Hoboken, NJ, USA: 2014. TMS Annual Meeting. [Google Scholar]
- 38.Wang S., Gao H., Li J., Wang Y., Chen C., Yu X., Tang S., Zhao X., Sun G., Li D. Comparative study of the photoluminescence performance and photocatalytic activity of CeO2/MgAl2O4 composite materials with an n-n heterojunction prepared by one-step synthesis and two-step synthesis methods. J. Phys. Chem. Solids. 2021;150:109891. doi: 10.1016/j.jpcs.2020.109891. [DOI] [Google Scholar]
- 39.Parish C.M., Brewer L.N. Multivariate statistics applications in phase analysis of STEM-EDS spectrum images. Ultramicroscopy. 2010;110:134–143. doi: 10.1016/j.ultramic.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 40.Ahmed M.A., Ebrahim M.I. Effect of zirconium oxide nano-fillers addition on the flexural strength, fracture toughness, and hardness of heat-polymerized acrylic resin. World J. Nano Sci. Eng. 2014;4:50–57. doi: 10.4236/wjnse.2014.42008. [DOI] [Google Scholar]
- 41.Chaijareenont P., Takahashi H., Nishiyama N., Arksornnukit M. Effect of different amounts of 3-methacryloxypropyltrimethoxysilane on the flexural properties and wear resistance of alumina reinforced PMMA. Dent. Mater. J. 2012;31:623–628. doi: 10.4012/dmj.2012-056. [DOI] [PubMed] [Google Scholar]
- 42.Esquivel J., Lawson N.C., Kee E., Bruggers K., Blatz M.B. Wear of resin teeth opposing zirconia. J. Prosthet. Dent. 2020;124:488–493. doi: 10.1016/j.prosdent.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 43.Chladek G., Pakieła K., Pakieła W., Zmudzki J., Adamiak M., Krawczyk C. Effect of antibacterial silver-releasing filler on the physicochemical properties of poly(methyl methacrylate) denture base material. Materials. 2019;12:4146. doi: 10.3390/ma12244146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Benli M., Eker B., Yusuf G., Bilge K., Rohlig G., Evlioğlu G., Huck O. Surface roughness and wear behavior of occlusal splint materials made of contemporary and high-performance polymers. Odontology. 2020;108:240–250. doi: 10.1007/s10266-019-00463-1. [DOI] [PubMed] [Google Scholar]
- 45.Nayyer M., Zahid S., Hassan S.H., Mian S.A., Mehmood S., Khan H.A., Kaleem M., Zafar M.S., Khan A.S. Comparative abrasive wear resistance and surface analysis of dental resin-based materials. Eur. J. Dent. 2018;12:57–66. doi: 10.4103/ejd.ejd_380_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Matzinger M., Hahnel S., Preis V., Rosentritt M. Polishing effects and wear performance of chairside CAD/CAM materials. Clin. Oral Investig. 2019;23:725–727. doi: 10.1007/s00784-018-2473-3. [DOI] [PubMed] [Google Scholar]
- 47.Preis V., Behr M., Handel G., Schneider-Feyrer S., Hahnel S., Martin R. Wear performance of dental ceramics after grind- ing and polishing treatments. J. Mech. Behav. Biomed. Mater. 2012;10:13–22. doi: 10.1016/j.jmbbm.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 48.Heintze S., Zellweger G., Cavalleri A., Ferracane J. Influence of the antagonist material on the wear of different composites using two different wear simulation methods. Dent. Mater. 2006;22:166–175. doi: 10.1016/j.dental.2005.04.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This will be made available upon request through the corresponding author.