Abstract
The required minimum number of psychiatric inpatient beds is highly debated and has substantial resource implications. The present study used the Delphi method to try to reach a global consensus on the minimum and optimal psychiatric bed numbers. An international board of scientific advisors nominated the Delphi panel members. In the first round, the expert panel provided responses exploring estimate ranges for a minimum to optimal numbers of psychiatric beds and three levels of shortage. In a second round, the panel reconsidered their responses using the input from the total group to achieve consensus. The Delphi panel comprised 65 experts (42% women, 54% based in low- and middle-income countries) from 40 countries in the six regions of the World Health Organization. Sixty psychiatric beds per 100 000 population were considered optimal and 30 the minimum, whilst 25–30 was regarded as mild, 15–25 as moderate, and less than 15 as severe shortage. This is the first expert consensus on minimum and optimal bed numbers involving experts from HICs and LMICs. Many high-income countries have psychiatric bed numbers that fall within the recommended range. In contrast, the number of beds in many LMIC is below the minimum recommended rate.
Subject terms: Psychiatric disorders, Addiction, Schizophrenia
Introduction
Psychiatric inpatient bed capacities vary between countries [1] and international consensus is lacking on how many psychiatric beds should be available for optimal functioning of mental health systems. The bed rates in low (median 1.9 beds per 100,000), lower-middle (median 6.3 beds per 100,000), and upper-middle-income (median 24.3 beds per 100,000) countries (LMICs) are, on average, much lower than in high-income (median 52.6 beds per 100,000) countries (HICs) and in the OECD (mean 62 beds per 100,000) [1, 2]. Variations in the provision of psychiatric beds, even among OECD member countries [3], can only partially be explained by geographical location and income levels [4]. Several contextual factors may have an impact on this variation. These include demographic characteristics of the population [5, 6], mental health budgets [7], morbidity levels, migration, and local poverty [8], the availability of social support services [9, 10], incarceration rates [11], availability of psychiatric outpatient and residential services, mental health stigmatization levels and the continuity of mental health care across sectors [12]. Especially home treatment, such as multidisciplinary crisis resolution teams, and assertive outreach treatment may reduce the need for hospitalization in highly resourced care systems.
The expert consensus approaches may serve as guidance when strict epidemiological estimations are impractical. It is a valuable resource as a basis for decision-making where experimental evidence is not available or when the subject is not easy to study otherwise [13]. This is especially the case in the complex area of resource utilization in mental health care [14]. The required number of psychiatric beds is still a matter of debate and attempts to find a consensus among experts have been limited to HICs [15, 16]. On the basis of expert opinion, Canadian and American organizations have recommended a target of 50 publicly funded psychiatric beds per 100,000 population [15, 17]. However, the recommendations do not specify how the experts arrived at their consensus estimates and do not consider the situation in LMICs [18].
Therefore, the aim of this study was to reach a global expert consensus on the minimum and optimal psychiatric bed numbers. We also aimed to explore factors that may be considered relevant for local planning.
Methods
This study (ISRCTN10786216) used structured and sequential questionnaires with controlled feedback as per the Delphi method. A Scientific Advisory Board with 13 members from different WHO regions was formed. Members were selected—based on relevant contributions to mental health research—to advise on the survey design and procedures as well as data processing and analyses. They also proposed experts who were invited to be part of the Delphi panel. At least two survey rounds were considered. Consensus as defined below was the criterion to stop the Delphi process [19, 20].
Recruitment and survey design
The members of the Board were asked to propose at least 12 professionals with experience in the field of psychiatric service development, especially researchers with published scientific articles related to the topic, and mental health service managers at a local (institutional) or regional/national level. Board members were asked to consider experts from different disciplines (i.e., psychiatrists, psychologists, mental health nurses, administrators, user- and family-organizations) and from all WHO regions.
Based on proposals by Board members, 158 potential experts were sent two invitations via email between August 5 and August 31, 2020 to be part of the Delphi panel. Of the 158 experts invited, 83 declined to participate or did not respond to the invitation. A panel of 75 members was formed and were contacted for the second round. We established a priori that only rounds with at least 30 participants would be included in the analyses.
Online surveys
The surveys were hosted on the online platform SurveyMonkey, and links to respond were delivered to Delphi panel members via email. The first-round survey was open between September 3, 2020 and October 2, 2020; the second-round survey was open between November 9, 2020 and January 4, 2021. We used an electronic informed consent form to be completed by the participants. The form was reviewed and approved by the Ethics Committee of the Diego Portales University, Santiago, Chile. Panel members were asked to provide optimal and minimum numbers per 100,000 population, as well as ranges for mild, moderate, and severe shortages if minimum numbers were higher than zero. The concept of “psychiatric bed” provided in the section heading was based on WHO’s definition [1]. This included mental hospital short-term and long-stay services, general hospital psychiatric units, community-based psychiatric inpatient units, and forensic inpatient units. The definition also included both public and private nonprofit and for-profit facilities, mental hospitals for children and adolescents only, and those for other specific populations (e.g., old age). However, the definition excluded facilities that treat only people with alcohol and substance use disorders or intellectual disability without accompanying mental disorder diagnoses, community residential facilities, and services exclusively providing recovery and rehabilitation treatments. Panel members were also invited to identify contextual factors in open textboxes, that may specify or modify recommendations on psychiatric bed numbers at the local or regional level based on their personal experience and evidence in the scientific literature. All factors given in the first round were submitted to thematic analysis [21]; the resulting statements were sent to the panel members in the second round who scored each statement on Likert-type five-point scales (Not relevant, Not very important, Very important, Essential, and Don’t know/depends).
Multiple-choice questions to characterize the Delphi panel were also included in the surveys. The income level of the countries where the panel members were working was based on the World Bank classification [22]. The geographical distribution was based on the six WHO regions [23]. Because of important cultural and socio-economic differences, the Region of the Americas (Pan American Health Organization [PAHO]) was divided into two subregions: PAHO North America (including the United States and Canada) and PAHO Latin America and the Caribbean (including all the remaining countries of PAHO). Professional background (psychiatrist, other mental health professional, or other professions), areas of expertise (clinical, research/academia, administration, and policy), gender, and age were all recorded.
Data analysis
Regarding the numbers that were requested, we did not expect normal distribution. Therefore, median values and IQR, as well as mean and standard deviation (SD), were calculated for each indicator. Median values and interquartile ranges (IQR) resulting from the first round were provided to panel members in order to reconsider their response in an effort to improve consensus. The consensus was considered to be reached if at least 85% of the responses from the last round fell between the first and third quartiles of the answers given in the first round [24]. Extreme outliers were retrospectively identified and excluded based on the 3*IQR rule [25]. Second round responses were also assessed by income group and WHO region.
In the second round, the percentage of each response (Not relevant, Not very important, Very important, Essential, and Don’t know/depends) to each contextual factor was calculated. The contextual factors were sorted within each thematic group based on the sum of Very Important and Essential responses, and the mean percentages for those responses in each thematic group were calculated. Consensus on contextual factors was a priori defined as at least 85% of the panel rating the item as Essential or Very Important. Raw data are available upon reasonable request from the corresponding author.
Results
In the first round we received 63 responses and in the second round 61 responses from respondents from 40 different countries representing all six WHO regions. Composition of the Delphi panel in the first and second round was similar although four panel members responded to the first round but not the second one, and two panel members only responded to the second round without having answered the first one. The characteristics of the panel are shown in Table 1. More details on the panel members are provided in the supplementary material (Table S1).
Table 1.
Characterization of the Delphi panel members in the first and second rounds.
| First round (N) | Second round (N) | |
|---|---|---|
| Total | 63 | 61 |
| Age range | ||
| 34 or younger | 3 | 2 |
| 35–44 | 18 | 17 |
| 45–54 | 16 | 17 |
| 55–64 | 16 | 13 |
| 65+ | 9 | 11 |
| WHO region | ||
| AFRO | 7 | 6 |
| EMRO | 8 | 8 |
| EURO | 13 | 13 |
| PAHO Latin | 10 | 9 |
| PAHO North | 9 | 9 |
| SEARO | 4 | 4 |
| WPRO | 12 | 12 |
| Income | ||
| High | 30 | 30 |
| Upper-middle | 18 | 16 |
| Lower-middle | 13 | 13 |
| Low | 2 | 2 |
| Gender | ||
| Male | 36 | 35 |
| Female | 27 | 26 |
| Profession | ||
| Psychiatrists | 42 | 40 |
| Other professionals | 21 | 21 |
| Area of expertize | ||
| Academia/research | 20 | 22 |
| Administration/policy/other | 16 | 14 |
| Clinician | 27 | 25 |
AFRO African region, EMRO Eastern Mediterranean region, EURO European region, PAHO Pan American health organization, SEARO South-East Asian region (SEARO), WPRO Western Pacific region.
Median and mean numbers of psychiatric beds recommended by the panel are provided in Table 2. In the first round, the respondents were asked to provide five numerical values: optimal and minimum numbers of psychiatric beds, and three cut-off points to define mild, moderate, and severe levels of shortage. However, the median numbers for minimum level and the cut-off point to define mild shortage were identical, so for the second round, we only asked for four rates: two numbers for an “adequate range” of beds between an optimal and a minimum number and two cut-off numbers (an upper one delineating mild and moderate shortage and a lower one separating moderate and severe shortage). Four extreme outliers defined as all responses over 232 beds per 100 000 population (3*IQR rule) were excluded from the analyses provided for the first round. The outliers were from four different WHO regions, including HIC and LMIC. No extreme outliers were observed in the second round (Table 2). None of the 61 respondents skipped the questions in this section.
Table 2.
Optimal, minimum, and shortage levels of psychiatric beds per 100,000 inhabitants recommended by the Delphi panel: median and mean rates and distribution based on income group and WHO region of the countries, in which the panel members are based.
| First round | Second round | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Optimal | Minimum | Mild shortagea | Moderate shortage | Severe shortage | Optimal | Minimum | Moderate shortage | Severe shortage | |
| Overall responses | N 63 | N 61 | |||||||
| Median (IQR) | 50 (58) | 30 (36) | 30 (35) | 20 (27) | 10 (21) | 60 (20) | 30 (15) | 25 (13) | 15 (10) |
| Minimum value | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q1 | 25 | 14 | 10 | 8 | 4 | 50 | 25 | 20 | 10 |
| Q3 | 83 | 50 | 45 | 35 | 25 | 70 | 40 | 33 | 20 |
| Maximum valueb | 2000 | 1000 | 1500 | 1000 | 400 | 100 | 65 | 60 | 50 |
| Mean (SD) | 59 (44) | 33 (25) | 34 (28) | 24 (20) | 16 (15) | 61 (17) | 34 (13) | 26 (12) | 15 (9) |
| No. (%) of second-round responses between Q1 and Q3 of first round | NA | NA | NA | NA | NA | 59 (97) | 58 (95) | 58 (95) | 59 (97) |
| Income level | |||||||||
| High-Income Countries | N 30 (1 extreme outlier) | N 30 | |||||||
| Median (IQR) | 50 (50) | 40 (30) | 40 (30) | 30 (25) | 20 (20) | 60 (23) | 40 (20) | 30 (17) | 15 (10) |
| Mean (SD) | 65 (39) | 38 (23) | 43 (30) | 30 (20) | 20 (13) | 64 (15) | 38 (13) | 29 (13) | 17 (11) |
| Lower- and Middle-Income Countries (combined) | N 33 (3 extreme outliers) | N 31 | |||||||
| Median (IQR) | 50 (65) | 20 (34) | 20 (30) | 10 (25) | 5 (19) | 60 (20) | 30 (20) | 20 (10) | 10 (10) |
| Mean (SD) | 52 (47) | 28 (26) | 25 (24) | 18 (19) | 12 (15) | 58 (19) | 30 (12) | 23 (10) | 14 (7) |
| Upper-Middle-Income Countries | N 18 (1 extreme outlier) | N 16 | |||||||
| Median (IQR) | 15 (45) | 10 (36) | 9 (25) | 6 (19) | 4 (11) | 50 (14) | 28 (10) | 20 (8) | 10 (6) |
| Mean (SD) | 41 (48) | 25 (24) | 22 (25) | 16 (19) | 11 (24) | 54 (14) | 28 (10) | 20 (8) | 12 (6) |
| Lower-Middle-Income Countries | N 13 (2 extreme outliers) | N 13 | |||||||
| Median (IQR) | 60 (75) | 20 (20) | 20 (24) | 10 (20) | 5 (15) | 60 (30) | 30 (15) | 30 (15) | 10 (10) |
| Mean (SD) | 66 (48) | 31 (29) | 26 (24) | 18 (19) | 10 (14) | 60 (24) | 30 (13) | 30 (15) | 10 (9) |
| Low-Income Countries | N 2 | N 2 | |||||||
| Median (IQR) | 70 (10) | 40 (10) | 43 (3) | 35 (5) | 35 (15) | 68 (8) | 40 (0) | 28 (8) | 20 (5) |
| Mean (SD) | 70 (14) | 40 (14) | 44 (4) | 35 (7) | 35 (21) | 68 (11) | 40 (0) | 28 (11) | 20 (7) |
| WHO region | |||||||||
| AFRO | N 7 (1 extreme outlier) | N 6 | |||||||
| Median (IQR) | 55 (70) | 25 (44) | 33 (36) | 23 (34) | 15 (34) | 73 (24) | 35 (25) | 38 (5) | 20 (11) |
| Mean (SD) | 62 (56) | 36 (38) | 33 (30) | 25 (24) | 20 (22) | 61 (33) | 32 (19) | 32 (16) | 18 (11) |
| EMRO | N 8 (1 extreme outlier) | N 8 | |||||||
| Median (IQR) | 60 (55) | 20 (38) | 25 (20) | 15 (18) | 10 (15) | 55 (13) | 23 (16) | 20 (15) | 10 (9) |
| Mean (SD) | 74 (64) | 35 (34) | 35 (31) | 25 (24) | 15 (17) | 51 (11) | 27 (10) | 19 (8) | 11 (5) |
| EURO | N 13 | N 13 | |||||||
| Median (IQR) | 50 (30) | 25 (27) | 30 (22) | 20 (20) | 10 (24) | 60 (20) | 40 (20) | 30 (15) | 15 (10) |
| Mean (SD) | 67 (47) | 38 (27) | 38 (37) | 28 (26) | 18 (17) | 60 (17) | 35 (15) | 30 (13) | 19 (12) |
| PAHO North America | N 9 (1 extreme outlier) | N 9 | |||||||
| Median (IQR) | 70 (45) | 50 (30) | 40 (16) | 30 (9) | 20 (5) | 60 (15) | 50 (15) | 30 (5) | 20 (10) |
| Mean (SD) | 66 (29) | 37 (16) | 48 (27) | 33 (14) | 21 (9) | 69 (17) | 43 (9) | 29 (7) | 18 (8) |
| PAHO Latin America and the Caribbean | N 10 | N 9 | |||||||
| Median (IQR) | 10 (33) | 8 (29) | 7 (4) | 5 (2) | 3 (2) | 50 (10) | 25 (10) | 20 (10) | 10 (5) |
| Mean (SD) | 23 (21) | 17 (16) | 12 (12) | 9 (10) | 6 (8) | 54 (14) | 27 (9) | 19 (8) | 11 (6) |
| SEARO | N 4 (1 extreme outlier) | N 4 | |||||||
| Median (IQR) | 30 (46) | 20 (8) | 8 (2) | 5 (1) | 1 (1) | 55 (18) | 35 (13) | 25 (13) | 13 (15) |
| Mean (SD) | 46 (48) | 15 (9) | 8 (3) | 5 (1) | 1 (1) | 63 (19) | 38 (10) | 23 (10) | 13 (9) |
| WPRO | N 12 | N 12 | |||||||
| Median (IQR) | 63 (50) | 48 (33) | 50 (30) | 30 (23) | 20 (20) | 60 (16) | 30 (16) | 20 (19) | 10 (15) |
| Mean (SD) | 65 (34) | 40 (19) | 39 (18) | 29 (15) | 19 (13) | 62 (15) | 34 (14) | 27 (15) | 14 (9) |
NA not applicable, AFRO African region, EMRO Eastern Mediterranean region, EURO European region, PAHO Pan American health organization, SEARO South-East Asian region, WPRO Western Pacific region.
aThe category Mild shortage was defined as the range between the minimum number and the cut off point for moderate shortage in the second round. Therefore, no value was retrieved for this category in the second round.
bFour extreme outliers were excluded from analyses of the first round.
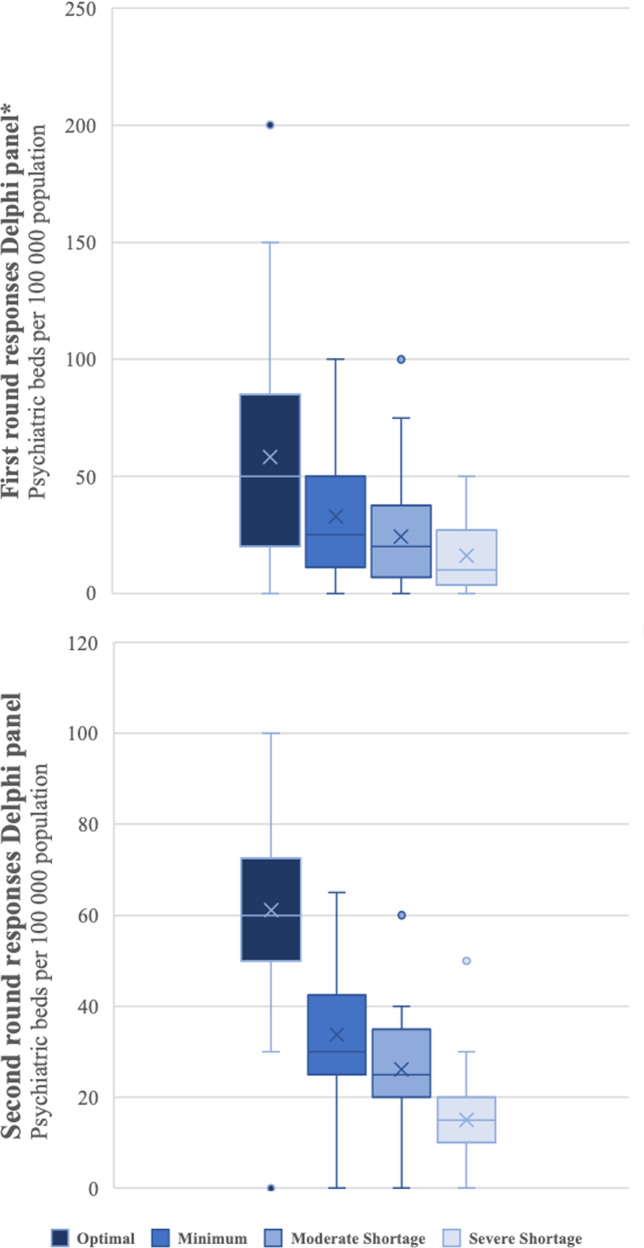
In the second round, more than 85% of responses for all four indicators fell between the first and third quartiles of the first round. Consequently, the high dispersion of responses found in the first round was reduced in the second round, which was evidenced in the proximity of means and medians of the second round and in the IQR and SD values (Fig. 1). The consensus was reached that 30 to 60 psychiatric beds per 100,000 population was an acceptable range, with 30 as a minimum and 60 an optimal rate. Rates between 25 and 30 were defined as mild shortage, while 15 to 25 defined moderate shortage. Rates lower than 15 beds per 100,000 were considered a severe shortage of psychiatric beds.
Fig. 1. Distribution of estimates for optimal, minimum, and shortage levels of psychiatric beds in the first and second round of a Delphi process.
*Four extreme outliers were removed in the first round.
Respondents from HICs provided a higher median rate of 40 per 100,000 population as a minimum, compared to 30 in LMICs. The differences observed for countries from different income groups or geographic regions also tended to diminish between rounds. The most notable case was the region of PAHO Latin America, where the medians for an acceptable range of beds increased from 7.5–10 to 25–50 per 100,000 inhabitants, which still was the lowest among the six WHO regions. Median values for Upper-Middle-Income countries also increased from 10–15 to 27.5–50 beds per 100,000 population between rounds.
Non-psychiatrist professionals tended to propose higher estimates for bed ranges than those provided by psychiatrists (40–70 beds per 100 000 vs 30–60 in the second round). There were no significant differences in the median rates with respect to the gender distribution of the respondents, nor for the area of expertise.
The panel provided 1408 responses for factors that should be considered for planning psychiatric bed numbers. After removing duplicate concepts, 471 contextual factors remained that were subjected to a thematic analysis. They were grouped into 60 codes representing comprehensive factors within six thematic groups that were fed back to the panel in the second round. Consensus was reached on 29 out of the 60 factors (85% responses of very important or essential), which are reported in the Online Supplement (Supplementary Table S2). The factors Comprehensive community care and continuity of care, Quality and standards of mental health care, and Mental health budget reached the highest consensus (97% responses of very important or essential).
Discussion
We provide the first expert consensus regarding minimum and optimal bed numbers with a global scope, involving experts from HICs and LMICs. The recommendation for an appropriate range of psychiatric bed rates was 30–60 beds per 100,000 population (30 as the minimum and 60 as the optimal number). We also established a consensus for two cut-offs between mild and moderate shortage and between a moderate and severe shortage of psychiatric beds. Mild shortage was defined as rates between 25 and 30 beds per 100,000 population, while moderate shortage corresponded to 15 to 25 per 100,000 inhabitants. Rates lower than 15 beds per 100,000 were considered a severe shortage of psychiatric beds.
Previous expert consensus studies had smaller panels, were more regional in scope, and only considered HICs [17, 26, 27]. An expert consensus conducted in 1973 in Switzerland retrieved the opinions of psychiatrists from six Western high-income countries [16]. The study included rates of psychiatric beds and other resources necessary for proper service functioning. Based on the seven responses from 18 participants, the study concluded that a mean of 100 inpatient psychiatric beds were appropriate per 100,000 population. The relatively high number could best be explained by the time of the investigations that was early to mid-deinstitutionalization in Western Europe. Recommendations established by our panel were more similar to those from the Treatment Advocacy Center (TAC) in the US (a non-peer-reviewed document based on the opinion of 15 experts who recommend a range of 40–60 publicly funded psychiatric beds per 100,000 population for the US) [15], which has been especially influential in many HICs [26, 28–30]. However, the minimum psychiatric bed rate of 30 established by our panel was lower than that reported by the TAC group [18]. This could indicate that expert opinions reflect real developments to lower recommendations over time. The global approach in our study may also have resulted in more suitable estimates for LMICs, and the range of psychiatric beds considered appropriate by our global panel (30–60 beds per 100,000 population) was higher than the actual provision of psychiatric beds for many countries, especially LMICs [4, 31, 32].
There was a global consensus on the role of efficient discharge planning and the capacities of outpatient and residential services for the capacity planning of inpatient mental health facilities [33, 34]. The quality and standards of mental health care were a major concern, especially in LMICs, probably reflecting the concern for minimum standards of care that apart from the physical infrastructure of the bed also lack sufficient human resources, availability of medication and equipment to run existing facilities [35, 36]. The mental health budget was another major consensus factor for psychiatric bed planning. Low budgets can account for both shortage and inefficient distribution of mental health resources [37, 38]. Similar contextual factors had been identified in a recent systematic review on expert arguments for trends of psychiatric beds [39]. However, the present study provides a hierarchy of importance for the expert arguments.
Our study has several strengths. This is the first study with a global scope to reach expert consensus on appropriate psychiatric bed rates. The study achieved diversity of geographical representation with representation from 40 countries across all WHO regions, and more than half of the expert panel based in LMICs. The panel was representative of diverse professional backgrounds, included both psychiatrists and non-psychiatrist mental health and public health professionals, encompassing clinicians, researchers, and policymakers. Additionally, the expert panel was larger than in previous consensus attempts. Finally, there was a high retention level between sequential rounds, and high rates of valid responses.
There are also several limitations. The diversity of Scientific Advisory Board members and their role in the nomination of the members of the Delphi panel was intended to mitigate the selection bias. However, given the nature of the study and the need to recruit suitable experts, selection bias cannot be ruled out. Less than half of the nominated experts (65 out of 158, 41%) participated. The South-East Asia Region (SEARO) with four experts and low-income countries with two experts may have been underrepresented on the panel. Delphi processes usually take two to three rounds in health care research [19, 20]. Since consensus was obtained for the numerical outcomes, we decided to limit the process to two rounds in this study. Further rounds could have explored the importance of specialized inpatient units for populations with specific needs, such as children and adolescents, forensic populations, older people, and people with substance use problems or intellectual disabilities.
Our study provides a global framework for recommendations on psychiatric bed numbers as a point of reference for service planning that for the first time includes LMICs. Levels of shortage in specific countries can also be assessed based on this study, especially in LMIC and policies may be developed to address this shortage. The conversion of public psychiatric beds to serve COVID-19 patients in the context of the ongoing pandemic may have further limited the capacity to offer quality acute inpatient care in many places. Mental health agencies may advocate for health policies and governmental funding of public psychiatric beds in situations of shortage. Where governments are unlikely to provide adequate numbers, international organizations and donors can now consider the provision of psychiatric beds for their agendas based on this study. The consensus provided here is unlikely to end the debates about the required minimum and optimal bed numbers, but it may inform and guide them.
Supplementary information
Supplementary material, Characteristics of the Delphi panel and contextual factors for psychiatric bed numbers
Acknowledgements
This study had funding by the Agencia Nacional de Investigación y Desarrollo, Chile, FONDECYT Regular 1190613. The funder financed research assistance to coordinate the research network and data collection. The funding agency had no influence in the design of this study or in the analysis and interpretation of the data, nor in the writing or the decision to submit this article for publication. The authors would also like to acknowledge the members of the expert panel for having shared their expertize and dedicated time to this study: Alma Dzubur Kulenovic, Amanda Cotton, Ana María Peñuela, Ángel Almánzar, Ashvini Nath, Avinash Desousa, Balogun Osunbiyi, Barbara Kane, Ben Beaglehole, Briggite Khoury, Dan Siskind, David Copolov, David Ndetei, Dennis Daliri, Dermont Hurley, Desree Karen Providence, Domenico Giacco, Dominic Sisti, Dusica Lecic-Tosevsky, Elena Molchanova, Elizabeth Sinclair Hancq, Eugenia Xatse, Farid Talih, Fuad Ismayilov, Giuseppe Guaiana, Harischandra Gambheera, Isabel Perera, Jeffrei Looi, Jimmy Lee, John Bohorquez, Juan Camilo Martínez, Juliet Mwale Musabala, Lena Flyckt, Luciano Grosso, Luis Taboada, Majda Cheour, Maris Taube, Maritza Troya, Martha Shumway, Maureen Maduagwu, Medhat Elsabbahy, Mohammad Akmar Paiman, Muzafami Mizuno, Nasser Loza, Nina Kerimi, Olga Karpenko, Peter Tyrer, Rani Hoff, Roger Ng, Roumen Milev, SM Yasir Arafat, Sammy Ohene, Sherry Chan, Shih Ku Lin, Sim Kang, Simon Judkins, Santosh Kumar Chaturvedi, Swapna Verma, Tarek Okasha, Tsirisoa Hary Seheno, Vesna Svab, Victoria Bird, Vinay Lakra, Walid Sarhan, and Yury Razvodovsky.
Author contributions
APM, ERS, MI, and SP conceived of the study; APM and ERS wrote the protocol and designed the survey; MI, SP, ROR, SA, TB, SM, AK, AG, JE-K, S-CP, and LC critically revised the survey and nominated Delphi panel members; APM and ERS conducted the data collection, data analyses, and drafted the manuscript; all authors critically revised the manuscript and approved the final version.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41380-021-01435-0.
References
- 1.World Health Organization. Mental Health Atlas 2017. https://www.who.int/publications/i/item/9789241514019 (2018). Accessed 1 Jan 2022.
- 2.Mundt AP, Serri ER, Siebenförcher M, Alikaj V, Ismayilov F, Razvodovsky YE, et al. Changes in national rates of psychiatric beds and incarceration in Central Eastern Europe and Central Asia from 1990–2019: a retrospective database analysis. Lancet Reg Health Eur. 2021;7:100137. [DOI] [PMC free article] [PubMed]
- 3.Organisation for Economic Cooperation and Development. Hospital beds. https://www.oecd-ilibrary.org/content/data/0191328e-en (2018). Accessed 1 Jan 2022.
- 4.Siebenförcher M, Fritz FD, Irarrázaval M, Salcedo AB, Dedik C, Orellana AF, et al. Psychiatric beds and prison populations in 17 Latin American countries between 1991 and 2017: rates, trends and an inverse relationship between the two indicators. Psychol Med. 2020:1–10. 10.1017/S003329172000269X. Online ahead of print. [DOI] [PubMed]
- 5.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 6.Lora A, Sharan P. Information for global mental health. Glob Ment Health. 2015;2:e17–e17. doi: 10.1017/gmh.2015.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saxena S, Sharan P, Saraceno B. Budget and financing of mental health services: baseline information on 89 countries from WHO’s project atlas. J Ment Health Policy Econ. 2003;6:135–43. [PubMed] [Google Scholar]
- 8.Rapp MA, Kluge U, Penka S, Vardar A, Aichberger MC, Mundt AP, et al. When local poverty is more important than your income: mental health in minorities in inner cities. World Psychiatry. 2015;14:249–50. doi: 10.1002/wps.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gigantesco A, de Girolamo G, Santone G, Miglio R, Picardi A. Long-stay in short-stay inpatient facilities: risk factors and barriers to discharge. BMC Public Health. 2009;9:306. doi: 10.1186/1471-2458-9-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee S, Rothbard AB, Noll EL. Length of inpatient stay of persons with serious mental illness: effects of hospital and regional characteristics. Psychiatr Serv. 2012;63:889–95. doi: 10.1176/appi.ps.201100412. [DOI] [PubMed] [Google Scholar]
- 11.Mundt AP, Chow WS, Arduino M, Barrionuevo H, Fritsch R, Girala N, et al. Psychiatric hospital beds and prison populations in South America since 1990: does the Penrose hypothesis apply? JAMA Psychiatry. 2015;72:112–8. doi: 10.1001/jamapsychiatry.2014.2433. [DOI] [PubMed] [Google Scholar]
- 12.Pinals DA, Fuller DA. The vital role of a full continuum of psychiatric care beyond beds. Psychiatr Serv. 2020;71:713–21. doi: 10.1176/appi.ps.201900516. [DOI] [PubMed] [Google Scholar]
- 13.Minas H, Jorm AF. Where there is no evidence: use of expert consensus methods to fill the evidence gap in low-income countries and cultural minorities. Int J Ment Health Syst. 2010;4:33. doi: 10.1186/1752-4458-4-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jorm AF. Using the Delphi expert consensus method in mental health research. Aust N. Z J Psychiatry. 2015;49:887–97. doi: 10.1177/0004867415600891. [DOI] [PubMed] [Google Scholar]
- 15.Torrey EF, Entsminger K, Geller J, Stanley J, Jaffe DJ. The shortage of public hospital beds for mentally Ill persons - A report of the treatment advocacy center. 2008.
- 16.Muller C. The future of the psychiatric institution: Utopia or reality? [The future of the psychiatric institution: Utopia or reality?] Soc Psychiatry. 1973;8:185–91. doi: 10.1007/BF00577850. [DOI] [Google Scholar]
- 17.Gordon A. Psychiatric bed levels. Position paper. Can Psychiatr Assoc Bull. 1997;29:1–4. [Google Scholar]
- 18.O’Reilly R, Allison S, Bastiampiallai T. Observed outcomes: an approach to calculate the optimum number of psychiatric beds. Adm Policy Ment Health. 2019;46:507–17. doi: 10.1007/s10488-018-00917-8. [DOI] [PubMed] [Google Scholar]
- 19.Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE. 2011;6:e20476. doi: 10.1371/journal.pone.0020476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niederberger M, Spranger J. Delphi technique in health sciences: a map. Front Public Health. 2020;8:457–457.. doi: 10.3389/fpubh.2020.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 22.The World Bank. World Bank Country and Lending Groups. 2021.
- 23.World Health Organization. Working with the regions. https://www.who.int/chp/about/regions/en/ (2021), Accessed 2021.
- 24.Rowe G, Wright G. The Delphi technique as a forecasting tool: issues and analysis. Int J Forecast. 1999;15:353–75. doi: 10.1016/S0169-2070(99)00018-7. [DOI] [Google Scholar]
- 25.André Q. Outlier exclusion procedures must be blind to the researcher’s hypothesis. J Exp Phychol Gen. 2021. PubMed PMID: 34060886. [DOI] [PubMed]
- 26.Allison S, Bastiampillai T, Licinio J, Fuller DA, Bidargaddi N, Sharfstein SS. When should governments increase the supply of psychiatric beds? Mol Psychiatry. 2018;23:796–800. doi: 10.1038/mp.2017.139. [DOI] [PubMed] [Google Scholar]
- 27.Tyrer P. Has the closure of psychiatric beds gone too far? Yes. BMJ. 2011;343:d7457. doi: 10.1136/bmj.d7457. [DOI] [PubMed] [Google Scholar]
- 28.Bloom JD, Krishnan B, Lockey C. The majority of inpatient psychiatric beds should not be appropriated by the forensic system. J Am Acad Psychiatry Law Online. 2008;36:438. [PubMed] [Google Scholar]
- 29.Knable M. William Whitney godding and the concepts of asylum and therapeutic community. Psychiatr Ann. 2015;45:45–48. doi: 10.3928/00485713-20150106-09. [DOI] [Google Scholar]
- 30.Wall BW. State Hospitals as “the most integrated setting according to their needs”. J Am Acad Psychiatry Law. 2013;41:484–7. [PubMed] [Google Scholar]
- 31.Okasha A, Karam E. Mental health services and research in the Arab world. Acta Psychiatr Scand. 1998;98:406–13. doi: 10.1111/j.1600-0447.1998.tb10106.x. [DOI] [PubMed] [Google Scholar]
- 32.Okasha A, Karam E, Okasha T. Mental health services in the Arab world. World Psychiatry. 2012;11:52–54. doi: 10.1016/j.wpsyc.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haselden M, Corbeil T, Tang F, Olfson M, Dixon LB, Essock SM, et al. Family involvement in psychiatric hospitalizations: associations with discharge planning and prompt follow-up care. Psychiatr Serv. 2019;70:860–6. doi: 10.1176/appi.ps.201900028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith TE, Abraham M, Bolotnikova NV, Donahue SA, Essock SM, Olfson M, et al. Psychiatric inpatient discharge planning practices and attendance at aftercare appointments. Psychiatr Serv. 2017;68:92–95. doi: 10.1176/appi.ps.201500552. [DOI] [PubMed] [Google Scholar]
- 35.Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low- and middle-income countries. Health Serv Insights. 2017;10:1178632917694350. doi: 10.1177/1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murali V, Oyebode F. Poverty, social inequality and mental health. Adv Psychiatr Treat. 2004;10:216–24. doi: 10.1192/apt.10.3.216. [DOI] [Google Scholar]
- 37.Knapp M, Funk M, Curran C, Prince M, Grigg M, McDaid D. Economic barriers to better mental health practice and policy. Health Policy Plan. 2006;21:157–70. doi: 10.1093/heapol/czl003. [DOI] [PubMed] [Google Scholar]
- 38.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–89. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 39.Mundt AP, Delhey Langerfeldt S, Rozas Serri E, Siebenförcher M, Priebe S. Expert arguments for trends of psychiatric bed numbers: a systematic review of qualitative data. Front Psychiatry. 2021;12:745247. doi: 10.3389/fpsyt.2021.745247. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material, Characteristics of the Delphi panel and contextual factors for psychiatric bed numbers