Abstract
Recently, the well-known geographically wide distribution of sporotrichosis in Brazil, combined with the difficulties of effective domestic feline treatment, has emphasized the pressing need for new therapeutic alternatives. This work considers a range of synthetic derivatives as potential antifungals against Sporothrix brasiliensis isolated from cats from the hyperendemic Brazilian region. Six S. brasiliensis isolates from the sporotrichotic lesions of itraconazole responsive or non-responsive domestic cats were studied. The minimum inhibitory concentrations (MICs) of three novel hydrazone derivatives and eleven novel quinone derivatives were determined using the broth microdilution method (M38-A2). In silico tests were also used to predict the pharmacological profile and toxicity parameters of these synthetic derivatives. MICs and MFCs ranged from 1 to >128 µg/mL. The ADMET computational analysis failed to detect toxicity while a good pharmacological predictive profile, with parameters similar to itraconazole, was obtained. Three hydrazone derivatives were particularly promising candidates as antifungal agents against itraconazole-resistant S. brasiliensis from the Brazilian hyperendemic region. Since sporotrichosis is a neglected zoonosis currently spreading in Latin America, particularly in Brazil, the present data can contribute to its future control by alternative antifungal drug design against S. brasiliensis, the most virulent and prevalent species of the hyperendemic context.
Keywords: sporotrichosis, Felis catus, quinones, hydrazones, zoonoses
1. Introduction
Sporotrichosis is a post-traumatic implantation subcutaneous mycosis of worldwide occurrence and increasing incidence, especially in tropical and subtropical regions such as Asia and Latin America. In Brazil, it is a hyperendemic neglected zoonosis and a major public health concern [1,2]. The pathogenic fungi causing this dermatozoonosis, from the genus Sporothrix, are thermo-dimorphic and saprophytic microorganisms [2]. Sporothrix brasiliensis is the most prevalent species in Brazil, directly related to the cat-transmitted zoonotic route [2,3]. The recent detection of feline and human patients with S. brasiliensis-caused sporotrichosis in Argentina [4,5,6] in addition to reports of zoonotic cases in other countries such as Paraguay and Panamá [7,8]. Suspected or possible cases were detected in Bolivia and Colombia, revealing its potential dissemination across South America [9]. One of the main challenges to be addressed is the occurrence of severe non-responsive forms of this mycosis in cats, in addition to recurrences and reinfections, characterizing zoonotic sporotrichosis as a matter of large relevance to public health [3,10].
Currently, the drug of choice for human and animal sporotrichosis treatment is itraconazole [11,12]. This azole is hepatotoxic, exclusively administered orally, with a high cost for the affected population, most of which live in socially vulnerable areas [13]. Thus, despite being improved, sporotrichosis therapy remains an unsolved problem since the reduction in S. brasiliensis sensitivity to this azole has been reported [12,14,15]. These authors described S. brasiliensis isolates obtained from patients residing in distinct Brazilian states such as Rio de Janeiro [16,17,18], São Paulo [16], Minas Gerais [18] and Rio Grande do Sul [12,14,19]. Our research group recently described the unprecedented existence of domestic felines coinfected by wild-type and non-wild-type S. brasiliensis in distinct areas of the hyperendemic region [17]. The ability to adapt and manifest the phenomenon of antifungal resistance to conventional antifungals is a reality for Sporothrix species originating from human and animal cases. Furthermore, S. brasiliensis presents a high ability to display resistance mechanisms, although these have not yet been fully elucidated [15].
The pharmaceutical industry is currently seeking new approaches for developing antimicrobial drugs to mitigate the worldwide burden of fungal diseases. In addition, the discovery and commercialization of new antifungal agents occurs in the long term and is costly. With regard to Sporothrix spp. infections, a few synthetic derivatives [20,21,22] have been investigated and described in the literature. Additionally, the potential correlation between feline therapeutic follow up with the in vitro itraconazole performance against S. brasiliensis has rarely been investigated. The present study aimed to determine the potential antifungal properties of a range of synthetic derivatives against wild-type and non-wild-type S. brasiliensis from diseased cats of the Brazilian hyperendemic area.
2. Results
2.1. Clinical Epidemiological Data
Table 1 summarizes the clinical epidemiological data of the six diseased felines from which the S. brasiliensis isolates were obtained. More than half were male (66.7%) and half of the total were unneutered. The average age of these animals was 3.58 years (SD ± 3.47 years), ranging from one to ten years. The majority were free roaming (83.3%), residing in urban areas with contact with soil and/or plants. Lesions were distributed in different anatomical sites, regardless of disease severity and the extent of itraconazole treatment.
Table 1.
Clinical epidemiological and laboratorial data of domestic cats infected by the six S. brasiliensis isolates investigated in the present study.
| Clinical/Epidemiological | Wild Type | Non-Wild Type | ||||
|---|---|---|---|---|---|---|
| WT1 | WT2 | WT3 | NWT1 | NWT2 | NWT3 | |
| Age (years) | 10 | 5 | 2.5 | 2 | 1 | 1 |
| Sex | M | F | M | M | M | F |
| Castration | Yes | No | No | Yes | No | Yes |
| Free roaming | No | Yes | Yes | Yes | Yes | Yes |
| Anatomical site | Abdomen, head, chest and pelvic limb | Head and neck | Head, thoracic and pelvic limb | Base of tail and paw | Head | Pelvic limb |
| Relapse | No | No | Yes | Yes | No | No |
| Duration of ITC treatment (months) | 60 | NI | 8 | >120 | NI | 2 |
WT: wild type; NWT: non-wild type to ITC [23]; M: male; F: female; ITC: itraconazole; NI: not informed.
Two domestic felines, the carriers of the WT3 and of the NWT1 isolates, presented more than one episode of sporotrichosis relapse. The NWT1 carrier underwent tail amputation 4 years ago and suffered from a new episode of sporotrichosis in the tail stump at the time of this study. Itraconazole treatment ranged from 2 to more than 120 months, with a dosage of 100 mg/cat/day.
2.2. Antifungal Susceptibility Assay
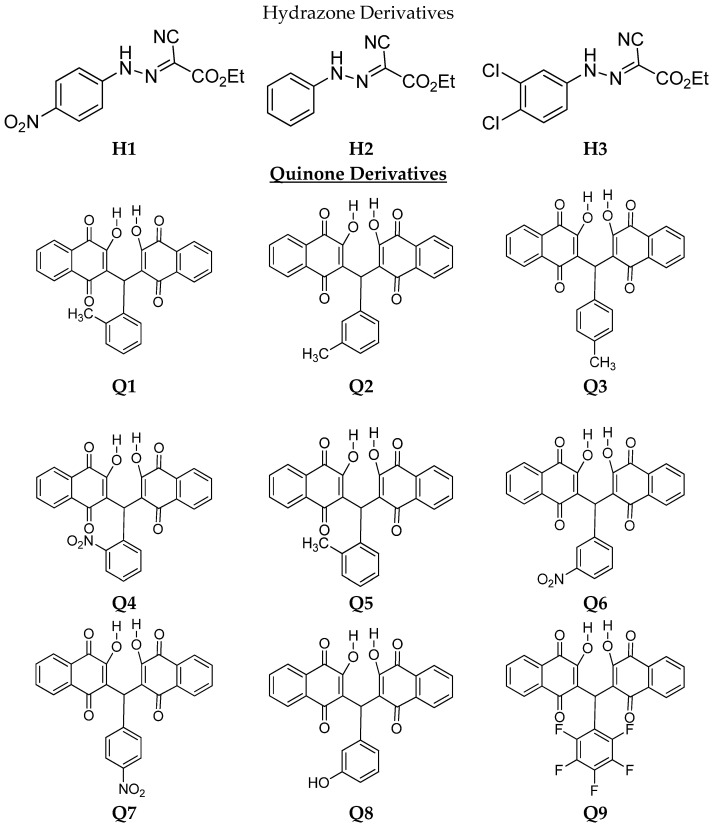
After the positive initial screening by an adaptation of the diffusion disc method (CLSI M2-A8) [24], eleven quinone derivatives (Q1–Q11) and three hydrazones (H1–H3) were selected for further investigation by the microdilution broth test against S. brasiliensis yeast-like forms (Figure 1). The results of the MIC and MFC values of the six clinical isolates and the standard strain against both hydrazone and quinone derivatives as well as itraconazole are shown in Table 2, Table 3 (geometric means to hydrazones) and Table 4.
Figure 1.
Molecular structures of hydrazone and quinone derivatives.
Table 2.
In vitro susceptibility (µg/mL) of the six isolated Sporothrix brasiliensis (yeast forms) to the novel hydrazone derivatives.
| Azole/Hydrazones | ATCC/Clinical Isolates | |||||||
|---|---|---|---|---|---|---|---|---|
| S. bra | WT 1 | WT 2 | WT 3 | NWT 1 | NWT 2 | NWT 3 | ||
| ITC | MIC | 2 | 1 | 4 | 1 | 32 | 16 | 8 |
| MFC | 16 | 8 | 32 | 8 | >128 | 128 | 128 | |
| H1 | MIC | 8 | 2 | 4 | 2 | 1 | 8 | 8 |
| MFC | 4 | 2 | 8 | 2 | 2 | 16 | 8 | |
| H2 | MIC | 8 | 16 | 16 | 8 | 8 | 16 | 8 |
| MFC | 8 | 16 | 16 | 8 | 16 | 16 | 16 | |
| H3 | MIC | 4 | 2 | 4 | 16 | 1 | 16 | 1 |
| MFC | 4 | 4 | 8 | 16 | 1 | 16 | 1 | |
Sbra: Sporothrix brasiliensis (ATCC MYA-4823); MIC: minimum inhibitory concentration; MFC: minimum fungicidal concentration.
Table 3.
Geometric means generated from the in vitro susceptibility (µg/mL) of the six isolated Sporothrix brasiliensis (yeast forms) to novel hydrazone derivatives.
| Azole/Hydrazones | ATCC/Clinical Isolates | |||
|---|---|---|---|---|
| S. bra | WT GM |
NWT GM |
||
| ITC | MIC | 2 | 2 | 18.6 |
| MFC | 16 | 16 | 128 | |
| H1 | MIC | 8 | 2.7 | 5.7 |
| MFC | 4 | 4 | 8.7 | |
| H2 | MIC | 8 | 13.3 | 10.7 |
| MFC | 8 | 13.3 | 16 | |
| H3 | MIC | 4 | 7.3 | 6 |
| MFC | 4 | 9.3 | 6 | |
Sbra: Sporothrix brasiliensis (ATCC MYA-4823); MIC: minimum inhibitory concentration; MFC: minimum fungicidal concentration; GM: geometric mean.
Table 4.
In vitro susceptibility (µg/mL) of the six isolated Sporothrix brasiliensis (yeast form) to novel quinone derivatives.
| Azole/Quinones | ATCC/Clinical Isolates | |||||||
|---|---|---|---|---|---|---|---|---|
| S. bra | WT 1 | WT 2 | WT 3 | NWT 1 | NWT 2 | NWT 3 | ||
| Itraconazole | MIC | 2 | 1 | 4 | 1 | 32 | 16 | 8 |
| MFC | 16 | 8 | 32 | 8 | >128 | 128 | 128 | |
| Q1 | MIC | >128 | 32 | >128 | NA | 128 | NA | 64 |
| MFC | >128 | 32 | >128 | NA | 128 | NA | 64 | |
| Q2 | MIC | >128 | 64 | NA | NA | >128 | NA | 64 |
| MFC | >128 | 64 | NA | NA | >128 | NA | 128 | |
| Q3 | MIC | >128 | 64 | NA | NA | >128 | NA | 128 |
| MFC | >128 | 128 | NA | NA | >128 | NA | 128 | |
| Q4 | MIC | >128 | 128 | NA | NA | >128 | >128 | 128 |
| MFC | >128 | 128 | NA | NA | >128 | >128 | 128 | |
| Q5 | MIC | >128 | NA | NA | NA | NA | NA | 128 |
| MFC | >128 | NA | NA | NA | NA | NA | 128 | |
| Q6 | MIC | NA | 128 | NA | NA | NA | NA | 64 |
| MFC | NA | 128 | NA | NA | NA | NA | 64 | |
| Q7 | MIC | NA | 128 | NA | NA | NA | NA | 64 |
| MFC | NA | 128 | NA | NA | NA | NA | 64 | |
| Q8 | MIC | 32 | 128 | >128 | NA | 32 | >128 | 64 |
| MFC | 64 | 128 | >128 | NA | 32 | >128 | 64 | |
| Q9 | MIC | >128 | 128 | NA | NA | NA | NA | 128 |
| MFC | >128 | 128 | NA | NA | NA | NA | 128 | |
| Q10 | MIC | 128 | 128 | NA | NA | NA | NA | 128 |
| MFC | 128 | 128 | NA | NA | NA | NA | 128 | |
| Q11 | MIC | 128 | 64 | NA | NA | NA | NA | 128 |
| MFC | 128 | 64 | NA | NA | NA | NA | 128 | |
Sbra: Sporothrix brasiliensis (ATCC MYA-4823); MIC: minimum inhibitory concentration; MFC: minimum fungicidal concentration; NA: not analyzed due to the lack of evidence after TSA screening.
An itraconazole MIC variation between 1 and 32 µg/mL and an MFC variation between 8 and >128 µg/mL against S. brasiliensis were observed (Table 2). Isolates obtained from the lesions of long-term treated cats with recurrent episodes presented the highest MICs for itraconazole (NWT1 MIC = 32 µg/mL; NWT2 MIC = 16 µg/mL and NWT3 MIC = 8 µg/mL) as well as the highest MFCs (Table 2).
S. brasiliensis exposure to hydrazones provided MICs varying from 1 to 16 µg/mL (Table 2), while for quinones, the MICs ranged from 32 to >128 µg/mL (Table 4). MICs’ and MFCs’ geometric means (GMs) for the hydrazone derivatives ranged from 2.7 to 13.3 µg/mL (Table 3). The GMs of the MICs obtained for NWT isolates exposed to the three hydrazones were between a third and a half lower (5.7–10.7 µg/mL) than those obtained for itraconazole (Table 3). In contrast, for the quinone derivatives, higher MICs and MFCs were detected (32–>128 µg/mL; Table 4). The clinical isolate NWT1, obtained from a two-year-old domestic feline irresponsive to itraconazole, showing several episodes of relapse, presented in vitro results suggestive of sensitivity to the Q8 (MIC/MFC = 32 µg/mL; Table 4) as well as to H1, H2 and H3 (MIC = 1–8µg/mL; MFC = 1–16 µg/mL; Table 2).
The WT1 clinical isolate from the feline treated with itraconazole for 60 months showed MICs compatible with sensitivity after exposure to itraconazole (1 µg/mL), Q1 (32 µg/mL), H1 (2 µg/mL), H2 (16 µg/mL) and H3 (2 µg/mL). Meanwhile, the MFCs were, respectively, Q1 (32 µg/mL), H1 (2 µg/mL), H2 (16 µg/mL) and H3 (4 µg/mL). WT2 and WT3 exposed to hydrazones exhibited the same suggestive phenotype (Table 2). MICs and MFCs of the quinones were also high for the wild-type isolates (Table 4). According to the MFCs, all hydrazones and quinones presented a fungicidal profile.
2.3. The In Silico Toxicological Profile and Pharmacokinetics
Toxicity was predicted as described in Table 5. The oral rat acute toxicity (LD50) of all derivatives and itraconazole ranged from 1.952 to 2.984 mol/kg. In contrast, oral rat chronic toxicity (LOAEL) varied from 0.055 log mg/kg bw/day to 2.974 mg/kg bw/day. Minnow toxicity varied between −6.407 log LC50 and 0.919 log LC50. Q6, Q7, H1 and H3 did not show evidence of a hepatotoxic effect. No hydrazone was a potential inhibitor of HERG I and II channels, while quinones did not seem to inhibit HERG I. The in silico predictions of four toxicological endpoints revealed that Q4, Q11 and itraconazole were immunotoxic, and that Q4, Q5 and H1 were mutagenic. No compound presented any presumed carcinogenic or cytotoxic properties.
Table 5.
Toxicological in silico profile of synthetic derivatives.
| Compounds | Toxicity | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Oral Rat Acute Toxicity (LD50) | Oral Rat Chronic Toxicity (LOAEL) | Minnow Toxicity | HERG I | HERG II | Hepatotoxicity | Toxicological End Points | ||||
| Immunotoxicity | Carcinogenicity | Cytotoxicity | Mutagenicity | |||||||
| Numeric (mol/kg) | Numeric (log mg/kg_bw/day) | Numeric (log LC 50) | Categorical (Yes/No) | Categorical (Active/Inactive) | ||||||
| Itraconazole | 2.966 | 0.055 | −4.446 | No | Yes | Yes | Yes | No | No | No |
| Q1 | 1.952 | 2.322 | −2.223 | No | Yes | Yes | No | No | No | No |
| Q2 | 2.098 | 2.398 | −2.889 | No | Yes | Yes | No | No | No | No |
| Q3 | 2.245 | 2.381 | −2.098 | No | Yes | Yes | No | No | No | No |
| Q4 | 2.580 | 1.549 | −1.846 | No | Yes | Yes | Yes | No | No | Yes |
| Q5 | 2.577 | 1.581 | −1.211 | No | Yes | Yes | No | No | No | Yes |
| Q6 | 2.972 | 1.221 | 0.919 | No | Yes | No | No | No | No | No |
| Q7 | 2.965 | 2.426 | 0.274 | No | Yes | No | No | No | No | No |
| Q8 | 2.711 | 2.974 | −6.407 | No | Yes | Yes | No | No | No | No |
| Q9 | 2.844 | 1.724 | −0.550 | No | No | Yes | No | No | No | No |
| Q10 | 2.905 | 1.578 | −1.852 | No | Yes | Yes | No | No | No | No |
| Q11 | 2.247 | 2.597 | −2.126 | No | Yes | Yes | Yes | No | No | No |
| H1 | 2.596 | 1.380 | 0.167 | No | No | No | No | No | No | Yes |
| H2 | 2.549 | 1.340 | 0.644 | No | No | Yes | No | No | No | No |
| H3 | 2.984 | 1.238 | −0.396 | No | No | No | No | No | No | No |
Itra: itraconazole; HERG I: Type 1 human Ether-a-go-go-related gene; HERG II: Type 2 human Ether-a-go-go-related gene.
The pharmacokinetics profile of THE synthetic derivatives in silico shown in Table S1 summarizes the in silico intestinal absorption analysis of all compounds showing values above 80% (84.81–100%), and most of the derivatives (8/14) exhibited good Caco-2 permeability, similarly to itraconazole. In contrast, Q1, Q7, H2 and H3 were not determined to be P-glycoprotein substrates. No hydrazone derivative was suggested as an inhibitor of P-glycoprotein I/II while Q9 was not assigned as a P-glycoprotein II inhibitor.
The volume of distribution (VDss) showed lower values (−0.807 and −0.169 log L/kg) for almost all derivatives. Likewise, low values were shown for the majority of derivatives with regard to the unbound drug fraction (UF). However, H1, H2, H3 and Q8 compounds presented estimated values ranging from 0.274 to 0.386, above those of itraconazole (Table S1). In addition, H3 was the only derivative with a suggested capability of blood–brain barrier permeability (BBB).
These compounds were also analyzed for interaction with CYP 450 enzymes, as substrates (2D6 and 3A4) or as inhibitors (CYP1A2, CYP2C19, CYP2C9, CYP2D6, CYP3A4). The hydrazone derivatives were not substrates for CYP3A4, and none of them were substrates for CYP2D6. As inhibitors, only the H3 compound showed an inhibitory profile and only against CYP1A2. Q1, Q2, Q3, Q4 and Q10 compounds inhibited CYP2C19, CYP2C9, CYP2D6 and CYP3A4. The candidates showed total clearance activity ranging from −0.926 log mL/min/kg to 0.786 log mL/min/kg. Similarly, no renal OCT2 substrate activity was found for either classes.
3. Discussion
The present work investigated S. brasiliensis isolates obtained from the lesions of domestic cats with sporotrichosis, clinically classified as responsive or non-responsive to treatment with itraconazole. This treatment varied from 2 to 60 months, and as expected, S. brasiliensis showed MICs compatible with reduced sensitivity to itraconazole or the “non-wild-type” phenotype, whenever obtained from non-responsive cats, as previously proposed (ESPINEL-INGROFF et al. [23] Almeida-Paes et al. [25]. The cats’ mean age of approximately 3 year was in accordance with previous reports on sporotrichosis, as was the predominance of males. Indeed, with this species, sexual maturity increases fighting for females and concomitant exposure to other diseased animals [1,2,3].
Although itraconazole is the first therapeutic option for human and domestic feline sporotrichosis treatment [12,14,23], broth microdilution cut-off points have not been established. As a consequence, the definition of qualitative parameters of Sporothrix spp. response (sensitivity or resistance) to the different antifungal drugs remains a riddle to be solved. In the attempt to clarify this definition, epidemiological cutoff values (ECVs) were suggested [23,25] though not yet fully correlated to the patients’ clinical responses [12,14,23]. Recently, Nakasu et al. [12] published a single study in an attempt to draw a parallel between in vitro data and the feline therapeutic follow up.
Recent publications have suggested that ECVs with MICs in the range of 0.5–2 mg/L for itraconazole were considered indicative of S. brasiliensis in vitro sensitivity [12,14,23,25]. The present study data on S. brasiliensis clinical isolates support this indication since those originating from domestic felines with an effective therapeutic response to the azole presented an in vitro MIC of 2 µg/mL. In contrast, the S. brasiliensis obtained from animals showing poor therapeutic response to itraconazole provided MIC values between 8 and 32 µg/mL, and could therefore be considered as “non-wild type” [23,25] or even resistant [12,14,15]. Likewise, in a veterinary hospital in southern Brazil (Pelotas, RS), Nakasu et al. [12] showed that approximately half of the investigated cats were non-responsive to itraconazole, with the corresponding isolates “resistant” to this drug. However, the reported MICs for itraconazole detected in the present investigation were higher than those reported by these authors. This might reflect the fact that the South Region of Brazil is located 1800 km away from the hyperendemic area (Rio de Janeiro, Southeast Brazil) with a lower level of sporotrichosis endemicity [1,3].
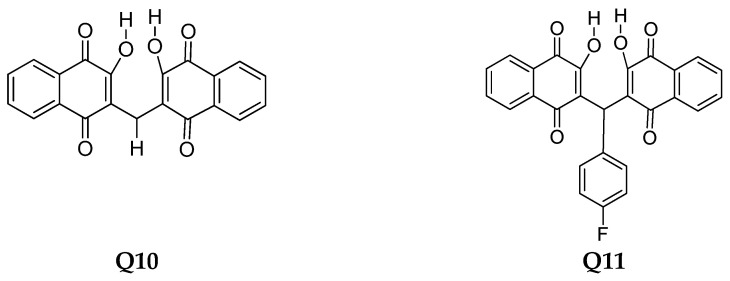
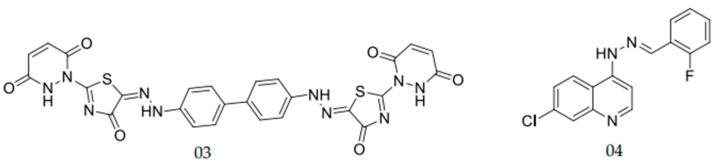
Different authors have suggested that S. brasiliensis shows reduced sensitivity to azoles [12,14,23,25], underlining the need to distinguish therapeutic alternatives. Recently, quinones became the subject of several studies due to their diverse known biological activities, such as their antibacterial [26,27] and antifungal potential [21,28,29]. These drugs also have antifungal properties against S. schenckii [29]. The present study analyzed eleven new quinone derivatives against WT and NWT clinical isolates and the standard strain of S. brasiliensis. Quinone derivatives Q1 and Q8 exhibited MIC and MFC values compatible with potential antifungal molecules [28,29]. Indeed, Tandon et al. [29,30], assessing quinone derivatives’ antibacterial and antifungal potential, showed MICs between 6.25 and ≥50 µg/mL for distinct S. schenckii isolates. Another example of an antifungal naphthoquinone is the substituted α-and-β-2,3-dihydrofuranaphthoquinones which were synthesized and evaluated against the main zoonotic Sporothrix species [21]. Two compounds were strongly active against these dimorphic fungi, namely naphthoquinone 1a, (Figure 2) which presented an MIC of 4 mg/mL, and naphthoquinone 1b (Figure 2), which presented an MIC of 2 mg/mL and 4 mg/mL against S. brasiliensis and S. schenckii, respectively. In the present study, the MICs obtained after the in vitro exposure of S. brasiliensis versus quinones were higher than those reported by Ferreira et al. [21], but still compatible with therapeutic potential.
Figure 2.
Naphthoquinones which previously presented antifungal activity against Sporothrix spp. as published by Janeczko et al. [31].
The antifungal activity of naphthoquinones can also be found against other fungi, such as Candida albicans. In the work of Janeczko et al. [31], a series of 1,4-naphthoquinones was prepared and tested against C. albicans. The compound (2) was the most active with an MIC of 8 mg/mL (Figure 2). The precedents for antifungal activities indicate that this class of compounds has good prospects, especially for hybrids with heterocyclic nuclei. Altogether, these data corroborate the potential of this class of molecules as a source of antifungal drug candidates.
Three hydrazones investigated in the present study also showed potential antifungal activity against different clinical isolates of S. brasiliensis. The in vitro exposure to H1 resulted in an MIC of 1 µg/mL against the S. brasiliensis NWT1, while the corresponding itraconazole value was 32-fold higher. Remarkably, this isolate infected a cat with a history of prolonged itraconazole-non-responsive sporotrichosis manifested by lesion recurrence at the base of its amputated tail. The standard strain of S. brasiliensis (Sbra) revealed the same in vitro response to these molecules.
The therapeutic potential for the hydrazones was previously investigated with several described biological activities [32]. Its antimycotic potential against dimorphic fungi, such as Coccidioides posadasii, as well as highly relevant yeasts including Candida spp. and Trichosporon asahii, in both community and hospital-acquired infections [32,33,34,35], were reported. Previously, Cordeiro et al. [34] described hydrazone MICs ranging from 2 to 250 µg/mL against Coccidioides posadasii, higher than those reported for S. brasiliensis in the present study, as compatible with the further investment of hydrazones as candidate drugs against this dimorphic fungus. Furthermore, distinct Candida species challenged this in vitro growth in the presence of different hydrazone derivatives resulting in MICs ranging from 0.25 to 128 µg/mL [35]. Previously, Casanova et al. [33] proposed that an MIC value between 8 and 32 µg/mL could be considered an encouraging result after the in vitro testing of new hydrazones against Candida parapsilosis and Trichosporon asahii. Our results indicate the strong potential of future investment in hydrazones for controlling fungal infections.
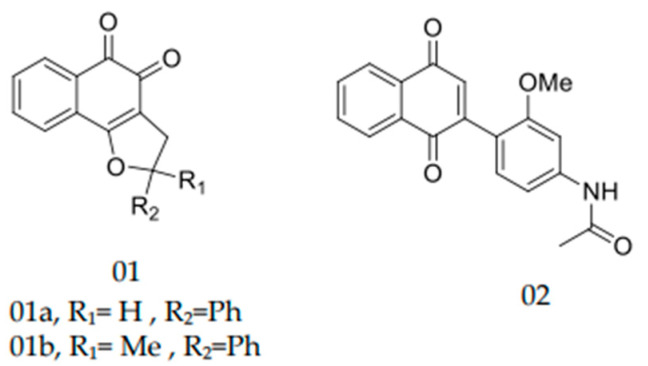
Hydrazones are present in different aryl groups which confer antifungal activity [36,37]. Abu-Melha et al. [37] performed tests with a one bis aryl hydrazine containing a thiazole ring (Hydrazone 03; Figure 3) against C. albicans. This compound resulted in MICs of 0.18 µg/mL and 3.18 µg/mL against azole-sensitive and azole-resistant C. albicans, respectively [37]. Carvalho et al. [36] evaluated a series of hydrazones containing the nucleus 7-chloroquinoline. The hydrazone shown in Figure 3 (hydrazone 04) stood out with a high percentage of inhibition against C. albicans (71% growth inhibition at a concentration of 12.5 mg/mL).
Figure 3.
Aryl hydrazones which previously presented antifungal activity against Candida albicans, as published by Carvalho et al. and Abu-Melha et al. [36,37].
Hydrazone and quinone derivatives were submitted to in silico ADME/Tox property analyses. Absorption is the process whereby the drug candidate moves from the point of administration (extravascular site) to the blood (systemic circulation). The values above 90%, present an optimal intestinal profile [38]. In the present work, all tested derivatives revealed good theoretical absorption in the intestine, similarly to itraconazole. Moreover, some quinone derivatives and itraconazole presented permeability to Caco-2 cells [39]. The Caco-2 in silico assay is a useful feature to analyze the passive absorption in the intestine, so the hydrophobic parameters shows the most relevance in this relationship [40]. Thus, parameters such as hydrophobic (LogP), molecular polar surface area (TPSA), molecular weight and donor/acceptor of hydrogen may influence Caco-2 results. Therefore, due to the hydrophilic profile of the quinolone derivatives such as Q4, Q5 and Q11 and of the hydrazone derivatives (H1–H3), these did not show permeability profiles to the in silico Caco-2 assay.
One last absorption parameter was analyzed by employing the P-glycoprotein transporters’ substrate or inhibitor [41]. The non-linear absorption kinetics of P-glycoprotein substrates has been reported due to the saturation transporter-mediated efflux activity, promoting the inhibition of intestinal P-glycoprotein resulting in significant effects of drug interaction (DDI) [42,43]. The results suggested that Q1, Q7, H2 and H3 derivative compounds were not P-glycoprotein substrates suggesting a good in silico oral bioavailability for all analyzed derivatives to be further explored.
The volume of distribution (VDss), fraction unbound (human) and blood–brain barrier membrane (BBB) permeability were also analyzed, as a distribution parameter for all the studied compounds. The VDss indicates the theoretical volume that a total dose would need to be uniformly distributed in the plasma to obtain the same concentration observed in blood plasma. All compounds showed lower values of VDss, suggesting that all these prototypes need low concentrations to remain in blood plasma. A fraction of the unbound drug of all hydrazones is higher than that of itraconazole. These results indicate that these groups of molecules have a good predictive distribution because the unbound form of the drug is responsible for exercising pharmacological activity [44]. The blood–brain barrier (BBB) was analyzed and according to the SwissADME calculation, only the H3 derivative could pass through the blood–brain barrier.
Enzymatic metabolism indicates the chemical biotransformation of a drug in the body, which plays a vital role in converting drug compounds [43]. CYP enzymes represent the most studied phase I drug-metabolizing enzymes and are also implicated in drug–drug interactions (DDIs) mediated by drug inhibition [45]. Although none of the derivatives were substrates for the tested Cytochrome P450 isozyme 2D6, all quinones are substrates of 3A4, such as itraconazole. Additionally, among these derivatives, only H3 acts as an inhibitor for CYP1A2. Interestingly, CYP1A2 is one main xenobiotic-metabolizing enzyme in humans, and a recent study associated this enzyme with the bioactivation of procarcinogens, including 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK), a tobacco-specific and potent pulmonary carcinogen [43,45].
Clearance is a constant that describes the relationship between drug concentration in the body and is important in determining the elimination of the drug [46]. Apart from hydrazone derivatives, all other new compounds exhibited lower values, including itraconazole. These metabolic and excretion results indicated that, theoretically, the quinone derivatives present a hepatic metabolization, while the hydrazone derivatives present a renal metabolization.
Toxicity has been a significant concern to the safety of drug candidates. Hepatotoxicity is still one of the major problems of drug toxicity [47]. Consequently, only Q6, Q7, H1 and H3 derivatives showed no predicted hepatotoxicity. Concerning the in silico toxicity test with minnows, an equivalent lethal concentration value (LC50), representing the concentration of a molecule necessary to cause the death of 50% of experimentally tested Fathead minnows, LC50 < 0.5 mM (i.e., log LC50 < −0.3) is regarded as causing acute toxicity. Q6, Q7, H1 and H2 derivatives do not seem to present acute toxicity in the minnow test. All quinones—apart from Q8—and hydrazones proved to be less toxic than itraconazole. No hydrazone was potentially an inhibitor of HERG I and II channels [48], while quinones did not seem to inhibit HERG I, avoiding fatal heart-beat problems and short QT syndrome.
The oral rat acute toxicity expresses the compound toxic potential in terms of lethal dosage values (LD50 in mol/kg). These chronic toxicity studies aim to detect the lowest doses of a compound that will cause the lowest observed adverse effect levels (LOAELs), and the treatment period and exposure time of the compound must also be considered [49]. Log LOAEL predicted values for the tested compounds suggest that a larger dose of each compound must be used to induce adverse effects, indicating safety for these compounds compared to itraconazole.
ProTox-II proposes to classify drugs into several different steps, including a toxicological (immunotoxicity model), genotoxicological (cytotoxicity, mutagenicity and carcinogenicity model) endpoints, and the toxicity of a specific protein target [50,51]. The in silico results revealed that all compounds do not present cytotoxicity and carcinogenicity. In general, theoretical toxicity studies show that the derivatives were less toxic than the antifungal of choice.
4. Materials and Methods
4.1. Fungal Isolates
Six clinical S. brasiliensis isolates were obtained from the lesions of cats with laboratory-confirmed sporotrichosis. The clinical evaluations were performed by veterinarians, and the six cats’ lesions, suspected to be from sporotrichosis, were later confirmed by mycological culture isolation and the genotyping of S. brasiliensis; all cats resided in the hyperendemic region of Rio de Janeiro, Brazil, as previously described [3]. These were selected from the Center for Microorganisms’ Investigation fungal collection, based on the itraconazole in vitro results [52,53,54] following the criteria proposed by Espinel-Ingroff et al. [23], as wild type (MIC ≤ 2µg/mL) or non-wild type (MIC ≥ 4µg/mL). These were further designated as “WT1”, “WT2”, “WT3” and “NWT1”, “NWT2”, “NWT3”, respectively. The reference strain S. brasiliensis ATCC MYA-4823 (Sbra) was included in all experiments.
4.2. Growth Conditions
The clinical isolates were maintained by cryopreservation in its yeast phase at −20 °C in the fungus collection of the Center for Microorganism’s Investigation (CIM) until its reactivation for the conduction of the experiments. For reactivation, cryotubes were defrosted with subsequent replication on Sabouraud agar 2% dextrose (Becton, Dickinson, and Company—BD, Franklin Lakes, NJ, USA) and incubated at room temperature for five days for microbial growth in the form of conidia.
4.3. Synthetic Derivatives
Seventy-eight novel chemical derivatives of seven different classes (pyrazoles, pyrazolones, quinolones, naphthoquinones, hydrazones, n-phthalimides and quinones) were screened by disk diffusion antimicrobial sensitivity test (adapted Kirby–Bauer methodology) [55].
4.4. Antifungal Susceptibility Assays
Susceptibility testing was performed according to the standardized broth microdilution technique described by the CLSI in documents M38-A2 and M27-A3 [52,53] for yeast-like cells and conidia. The antifungal used as the experimental control was itraconazole.
Minimum fungicidal concentrations (MFCs) were obtained from subcultures on Petri dishes, including Sabouraud agar 2% dextrose (SDA; Becton, Dickinson and Company—BD, Franklin Lakes, NJ, USA), filamentous phase and brain heart infusion (BHI; Becton, Dickinson and Company—BD, Franklin Lakes, NJ, USA), yeast phase, with 30 µL of the MIC cell suspension. In plates, they were incubated at 25 °C for five days (conidia) and at 37 °C for seven days (yeast). After reading the number of colonies, the MFC was established as the lowest derivative concentration capable of eliminating 99.9% of the fungal growth [16].
Prototypes providing MICs under ≤32 µg/mL against S. brasiliensis were considered to be promising candidates for future antifungal drug development. Three independent experiments were performed for all assays.
4.5. In Silico Toxicity and Pharmacological Profiles
In silico pharmacokinetic properties and toxicity estimations (ADMET) were evaluated using pkCSM—pharmacokinetic web server (http://biosig.unimelb.edu.au/pkcsm/ (accessed on 21 June 2021) [49], OSIRIS Property Explorer [56] and SwissADME webserver [57]. These results were compared with the itraconazole profile. The evaluated theoretical pharmacokinetic properties were absorption, distribution, metabolism and excretion. Absorption suggests a theoretical human intestinal absorption due to the Caco-2 permeability, P-glycoprotein substrate and P-glycoprotein I/II inhibition. For distribution, the theoretical steady-state volume of distribution was analyzed, the blood–brain barrier penetration (BBBP) and the fraction unbound to serum proteins in humans. The metabolism analyses were based on the relationships with cytochrome P450 (CYP) enzymes: the inhibition of CYP1A2, CYP3A4, CYP2C19, CYP2C9 and CYP2D6, and as the substrate of CYP3A4 and CYP2D6. Lastly, excretion parameters were assessed by the total theoretical clearance and renal OCT2 substrate. Toxicological analyses comprise toxicity target, hepatotoxicity, hERGI/II inhibitors and the toxicity end points such as carcinogenic, mutagenic, immunotoxic and cytotoxic parameters.
5. Conclusions
This original work was based on the premise of finding new potent and promising compounds with antifungal activity, based on the fact that antifungal armamentarium is very limited and many fungal species are resistant to clinically available drugs. Thus, our original aim was to evaluate the possible antifungal action of novel compounds, including those from the hydrazone and quinone classes, which are well-recognized molecules with several biological properties such as antimicrobial potential. Three hydrazone derivatives (H1, H2 and H3) showed good in vitro and in silico performances against the yeast pathogenic phase of the dimorphic fungi S. brasiliensis, compared with those of other promising antifungal drug candidates. These findings are particularly relevant if the results against itraconazole-resistant isolates, originally from non-responsive cats, are to be considered. Furthermore, although understanding the mechanisms of action and the antifungal drug targets are important, future studies of the mechanisms involved in S. brasiliensis drug resistance are necessary. Our results set the grounds for the discovery of novel promising compounds which can be used as a platform for the synthesis of more potent derivatives. Finally, since sporotrichosis is a neglected zoonosis currently spreading in Brazil and Latin America, the present data can contribute to its future control by alternative antifungal drug design against S. brasiliensis—the most virulent and prevalent species of the hyperendemic scenario.
Acknowledgments
The authors would like to thank the veterinarian collaborators and cat owners for allowing their animals to be part of this study. We are grateful to Norman Ratcliffe for editing and suggestions for improvements of the manuscript.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ph15010055/s1, Table S1: In silico pharmacokinetics profile of the hydrazone and quinone synthetic derivatives.
Author Contributions
Conceptualization, A.R.d.S.B., P.A.d.M.-S., R.L.D.M., A.L.S.d.S. and H.C.C.; data curation, A.R.d.S.B. and L.C.d.S.V.d.S.; formal analysis, A.R.d.S.B., L.C.d.S.V.d.S., D.S.d.O., R.B.G. and A.L.S.d.S.; funding acquisition, A.R.d.S.B. and R.L.D.M.; investigation, L.C.d.S.V.d.S., L.M.A. and N.F.R.; methodology, A.R.d.S.B., P.A.d.M.-S. and H.C.C.; project administration, A.R.d.S.B.; resources, A.R.d.S.B., D.S.d.O., R.L.D.M., R.B.G., A.L.S.d.S., V.F.F., D.T.G.G. and F.d.C.d.S.; supervision, A.R.d.S.B. and H.C.C.; validation, L.C.d.S.V.d.S., L.M.A. and N.F.R.; visualization, L.C.d.S.V.d.S. and P.A.d.M.-S.; writing—original draft, L.C.d.S.V.d.S. and N.F.R.; writing—review and editing, A.R.d.S.B., L.C.d.S.V.d.S., L.M.A., P.A.d.M.-S., R.L.D.M., R.B.G., V.F.F., D.T.G.G., F.d.C.d.S. and H.C.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by grants from the Brazilian Agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (PIBIC-CNPq-UFF, Brazil); Fundação de Amparo à Pesquisa no Estado do Rio de Janeiro, Brazil (FAPERJ-E-26/103.198/2011; E-26/010.001882/2014), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Brazil (CAPES)—Financial Code 001 and PROEX-MEC. R.L.D.M., A.L.S.S. and V.F.F. are research fellows of CNPq (PQ-CNPq).
Institutional Review Board Statement
This study was approved by and conducted according to the norms of the Ethics Committee on Animal Use by the Fluminense Federal University, Rio de Janeiro/BR (CEUA-UFF, protocol number 208/2012; 13 December 2012 and protocol number 7561040518; 14 June 2018).
Informed Consent Statement
Informed consent was obtained from all the tutors of the domestic feline involved in the study.
Data Availability Statement
All data are contained in the main text of the article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gremião I.D.F., Miranda L.H.M., Reis E.G., Rodrigues A.M., Pereira S.A. Zoonotic Epidemic of Sporotrichosis: Cat to Human Transmission. PLoS Pathog. 2017;13:e1006077. doi: 10.1371/journal.ppat.1006077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gremião I.D.F., Rocha E.M.D.S.D., Montenegro H., Carneiro A.J.B., Xavier M.O., de Farias M.R., Monti F., Mansho W., Pereira R.H.D.M.A., Pereira S.A., et al. Guideline for the management of feline sporotrichosis caused by Sporothrix brasiliensis and literature revision. Braz. J. Microbiol. 2021;52:107–124. doi: 10.1007/s42770-020-00365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macêdo-Sales P.A., Souto S.R.L.S., Destefani C.A., Lucena R.P., Machado R.L.D., Pinto M.R., Rodrigues A.M., Lopes-Bezerra L.M., Rocha E.M.S., Baptista A.R.S. Domestic feline contribution in the transmission of Sporothrix in Rio de Janeiro State, Brazil: A comparison between infected and non-infected populations. BMC Vet. Res. 2018;14:19. doi: 10.1186/s12917-018-1340-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Etchecopaz A., Scarpa M., Mas J., Cuestas M.L. Sporothrix brasiliensis: A growing hazard in the Northern area of Buenos Aires Province? Rev. Argent. Microbiol. 2020;52:350–351. doi: 10.1016/j.ram.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Etchecopaz A.N., Lanza N., Toscanini M.A., Devoto T.B., Pola S.J., Daneri G.L., Iovannitti C.A., Cuestas M.L. Sporotrichosis caused by Sporothrix brasiliensis in Argentina: Case report, molecular identification and in vitro susceptibility pattern to antifungal drugs. J. Mycol. Med. 2020;30:100908. doi: 10.1016/j.mycmed.2019.100908. [DOI] [PubMed] [Google Scholar]
- 6.Etchecopaz A., Toscanini M., Gisbert A., Mas J., Scarpa M., Iovannitti C., Bendezú K., Nusblat A., Iachini R., Cuestas M. Sporothrix brasiliensis: A Review of an Emerging South American Fungal Pathogen, Its Related Disease, Presentation and Spread in Argentina. J. Fungi. 2021;7:170. doi: 10.3390/jof7030170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rios M.E., Suarez J., Moreno J., Vallee J., Moreno J.P. Zoonotic Sporotrichosis Related to Cat Contact: First Case Report from Panama in Central America. Cureus. 2018;10:e2906. doi: 10.7759/cureus.2906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.García Duarte J.M., Wattiez Acosta V.R., Fornerón Viera P.M.L., Aldama Caballero A., Gorostiaga Matiauda G.A., Rivelli de Oddone V.B., Pereira Brunell J.G. Esporotricosis trasmitida por gato doméstico. Reporte de un caso familiar. Rev. Nac. 2017;9:67–76. doi: 10.18004/RDN2017.0009.02.086-095. [DOI] [Google Scholar]
- 9.Rossow J.A., Queiroz-Telles F., Caceres D.H., Beer K.D., Jackson B.R., Pereira J.G., Ferreira Gremião I.D., Pereira S.A. A One Health Approach to Combatting Sporothrix brasiliensis: Narrative Review of an Emerging Zoonotic Fungal Pathogen in South America. J. Fungi. 2020;6:247. doi: 10.3390/jof6040247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gremião I.D.F., Oliveira M.M.E., De Miranda L.H.M., Freitas D.F.S., Pereira S.A. Geographic Expansion of Sporotrichosis, Brazil. Emerg. Infect. Dis. 2020;26:621–624. doi: 10.3201/eid2603.190803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brilhante R.S.N., Rodrigues A.M., Sidrim J.J.C., Rocha M.F.G., Pereira S.A., Gremião I.D.F., Schubach T.M.P., de Camargo Z.P. In vitrosusceptibility of antifungal drugs againstSporothrix brasiliensisrecovered from cats with sporotrichosis in Brazil: Table 1. Med. Mycol. 2016;54:275–279. doi: 10.1093/mmy/myv039. [DOI] [PubMed] [Google Scholar]
- 12.Nakasu C.C.T., Waller S.B., Ripoll M.K., Ferreira M.R.A., Conceição F.R., Gomes A.D.R., Osório L.D.G., de Faria R.O., Cleff M.B. Feline sporotrichosis: A case series of itraconazole-resistant Sporothrix brasiliensis infection. Braz. J. Microbiol. 2021;52:163–171. doi: 10.1007/s42770-020-00290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pereira S.A., Schubach T.M.P., Gremião I.D.F., Da Silva D.T., Figueiredo F.B., De Assis N.V., Passos S.R.L. Aspectos terapêuticos da esporotricose felina. Acta Sci. Vet. 2018;37:311–321. doi: 10.22456/1679-9216.16781. [DOI] [Google Scholar]
- 14.Waller S.B., Ripoll M.K., Madrid I.M., Acunha T., Cleff M.B., Chaves F.C., de Mello J.R.B., de Faria R.O., Meireles M.C.A. Susceptibility and resistance of Sporothrix brasiliensis to branded and compounded itraconazole formulations. Braz. J. Microbiol. 2021;52:155–162. doi: 10.1007/s42770-020-00280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waller S.B., Lana D.F.D., Quatrin P.M., Ferreira M.R.A., Fuentefria A.M., Mezzari A. Antifungal resistance on Sporothrix species: An overview. Braz. J. Microbiol. 2021;52:73–80. doi: 10.1007/s42770-020-00307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borba-Santos L.P., Rodrigues A.M., Gagini T.B., Fernandes G.F., Castro R., de Carmargo Z.P., Nucci M., Lopes-Bezerra L.M., Ishida K., Rozental S. Susceptibility of Sporothrix brasiliensis isolates to amphotericin B, azoles, and terbinafine. Med. Mycol. 2015;53:178–188. doi: 10.1093/mmy/myu056. [DOI] [PubMed] [Google Scholar]
- 17.Macêdo-Sales P.A., Souza L.O.P., Della-Terra P.P., Lozoya-Pérez N.E., Machado R.L.D., Rocha E.M.D.S.D., Lopes-Bezerra L.M., Guimarães A.J., Rodrigues A.M., Mora-Montes H.M., et al. Coinfection of domestic felines by distinct Sporothrix brasiliensis in the Brazilian sporotrichosis hyperendemic area. Fungal Genet. Biol. 2020;140:103397. doi: 10.1016/j.fgb.2020.103397. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigues A.M., de Hoog G.S., de Cássia Pires D., Brihante R.S.N., da Costa Sidrim J.J., Gadelha M.F., Colombo A.L., de Camargo Z.P. Genetic diversity and antifungal susceptibility profiles in causative agents of sporotrichosis. BMC Infect. Dis. 2014;14:219. doi: 10.1186/1471-2334-14-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanchotene K.O., Brandolt T.M., Klafke G.B., Poester V.R., Xavier M.O. In vitro susceptibility of Sporothrix brasiliensis: Comparison of yeast and mycelial phases. Med. Mycol. 2017;55:869–876. doi: 10.1093/mmy/myw143. [DOI] [PubMed] [Google Scholar]
- 20.Forezi L., Borba-Santos L.P., Cardoso M.F.C., Ferreira V.F., Rozental S., Silva F.D.C.D. Synthesis and Antifungal Activity of Coumarins Derivatives against Sporothrix spp. Curr. Top. Med. Chem. 2018;18:164–171. doi: 10.2174/1568026618666180221115508. [DOI] [PubMed] [Google Scholar]
- 21.Garcia Ferreira P., Pereira Borba-Santos L., Noronha L.L., Deckman Nicoletti C., de Sá Haddad Queiroz M., de Carvalho da Silva F., Rozental S., Omena Futuro D., Francisco Ferreira V. Synthesis, Stability Studies, and Antifungal Evaluation of Substituted α- and β-2,3-Dihydrofuranaphthoquinones against Sporothrix brasiliensis and Sporothrix schenckii. Molecules. 2019;24:930. doi: 10.3390/molecules24050930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathias L., Almeida J., Passoni L., Gossani C., Taveira G., Gomes V., Motta O. Antifungal activity of silver salts of Keggin-type heteropolyacids against Sporothrix spp. J. Microbiol. Biotechnol. 2020;30:540–551. doi: 10.4014/jmb.1907.07064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Espinel-Ingroff A., Abreu D.P.B., Almeida-Paes R., Brilhante R.S.N., Chakrabarti A., Chowdhary A., Hagen F., Córdoba S., Gonzalez G.M., Govender N.P., et al. Multicenter, International Study of MIC/MEC Distributions for Definition of Epidemiological Cutoff Values for Sporothrix Species Identified by Molecular Methods. Antimicrob. Agents Chemother. 2017;61:e01057-17. doi: 10.1128/AAC.01057-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.NCCLS . Performance Standards for Antimicrobial Disk Susceptibility Tests. Approved Standard—Eighth ed. NCCLS; Wayne, PA, USA: 2003. NCCLS document M2-A8. [Google Scholar]
- 25.Almeida-Paes R., Brito-Santos F., Figueiredo-Carvalho M.H.G., Machado A.C.S., Oliveira M.M.E., Pereira S.A., Gutierrez-Galhardo M.C., Zancopé-Oliveira R.M. Minimal inhibitory concentration distributions and epidemiological cutoff values of five antifungal agents against Sporothrix brasiliensis. Mem. Inst. Oswaldo Cruz. 2017;112:376–381. doi: 10.1590/0074-02760160527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Riffel A., Medina L., Stefani V., Santos R., Bizani D., Brandelli A. In vitro antimicrobial activity of a new series of 1,4-naphthoquinones. Braz. J. Med Biol. Res. 2002;35:811–818. doi: 10.1590/S0100-879X2002000700008. [DOI] [PubMed] [Google Scholar]
- 27.Tandon V.K., Chhor R.B., Singh R.V., Rai S., Yadav D.B. Design, synthesis and evaluation of novel 1,4-naphthoquinone derivatives as antifungal and anticancer agents. Bioorganic Med. Chem. Lett. 2004;14:1079–1083. doi: 10.1016/j.bmcl.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 28.Louvis A.D.R., Silva N.A.A., Semaan F.S., Silva F.D.C.D., Saramago G., de Souza L.C.S.V., Ferreira B.L.A., Castro H.C., Salles J.P., Souza A.L.A., et al. Synthesis, characterization and biological activities of 3-aryl-1,4-naphthoquinones—Green palladium-catalysed Suzuki cross coupling. New J. Chem. 2016;40:7643–7656. doi: 10.1039/C6NJ00872K. [DOI] [Google Scholar]
- 29.Tandon V.K., Maurya H.K., Mishra N.N., Shukla P.K. Micelles catalyzed chemoselective synthesis ‘in water’ and biological evaluation of oxygen containing hetero-1,4-naphthoquinones as potential antifungal agents. Bioorganic Med. Chem. Lett. 2011;21:6398–6403. doi: 10.1016/j.bmcl.2011.08.095. [DOI] [PubMed] [Google Scholar]
- 30.Tandon V.K., Yadav D.B., Maurya H.K., Chaturvedi A.K., Shukla P.K. Design, synthesis, and biological evaluation of 1,2,3-trisubstituted-1,4-dihydrobenzo[g]quinoxaline-5,10-diones and related compounds as antifungal and antibacterial agents. Bioorg. Med. Chem. 2006;14:6120–6126. doi: 10.1016/j.bmc.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 31.Janeczko M., Kubiński K., Martyna A., Muzyczka A., Boguszewska-Czubara A., Czernik S., Tokarska-Rodak M., Chwedczuk M., Demchuk O.M., Golczyk H., et al. 1,4-Naphthoquinone derivatives potently suppress Candida Albicans growth, inhibit formation of hyphae and show no toxicity toward zebrafish embryos. J. Med. Microbiol. 2018;67:598–609. doi: 10.1099/jmm.0.000700. [DOI] [PubMed] [Google Scholar]
- 32.Chandra S., Vandana. Kumar, S Synthesis, spectroscopic, anticancer, antibacterial and antifungal studies of Ni(II) and Cu(II) complexes with hydrazine carboxamide, 2-[3-methyl-2-thienyl methylene] Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2015;135:356–363. doi: 10.1016/j.saa.2014.06.143. [DOI] [PubMed] [Google Scholar]
- 33.Casanova B.B., Muniz M.N., De Oliveira T., De Oliveira L.F., Machado M.M., Fuentefria A.M., Gosmann G., Gnoatto S.C.B. Synthesis and Biological Evaluation of Hydrazone Derivatives as Antifungal Agents. Molecules. 2015;20:9229–9241. doi: 10.3390/molecules20059229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cordeiro R.D.A., de Melo C.V.S., Marques F.J.D.F., Serpa R., Evangelista A.J.D.J., Caetano E.P., Mafezoli J., Oliveira M.D.C.F.D., da Silva M.R., Bandeira T.D.J.P.G., et al. Synthesis and in vitro antifungal activity of isoniazid-derived hydrazones against Coccidioides posadasii. Microb. Pathog. 2016;98:1–5. doi: 10.1016/j.micpath.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 35.Secci D., Bizzarri B., Bolasco A., Carradori S., D’Ascenzio M., Rivanera D., Mari E., Polletta L., Zicari A. Synthesis, anti-Candida activity, and cytotoxicity of new (4-(4-iodophenyl)thiazol-2-yl)hydrazine derivatives. Eur. J. Med. Chem. 2012;53:246–253. doi: 10.1016/j.ejmech.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 36.Carvalho P.H.D.A., Duval A.R., Leite F.R.M., Nedel F., Cunico W., Lund R.G. (7-Chloroquinolin-4-yl)arylhydrazones: C andida albicans enzymatic repression and cytotoxicity evaluation, Part 2. J. Enzym. Inhib. Med. Chem. 2015;31:126–131. doi: 10.3109/14756366.2015.1010527. [DOI] [PubMed] [Google Scholar]
- 37.Abu-Melha S., Gomha S., Abouzied A., Edrees M., Dena A.A., Muhammad Z. Microwave-Assisted One Pot Three-Component Synthesis of Novel Bioactive Thiazolyl-Pyridazinediones as Potential Antimicrobial Agents against Antibiotic-Resistant Bacteria. Molecules. 2021;26:4260. doi: 10.3390/molecules26144260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hadni H., Elhallaoui M. 3D-QSAR, docking and ADMET properties of aurone analogues as antimalarial agents. Heliyon. 2020;6:e03580. doi: 10.1016/j.heliyon.2020.e03580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ortiz C.L., Completo G.C., Nacario R.C., Nellas R.B. Potential Inhibitors of Galactofuranosyltransferase 2 (GlfT2): Molecular Docking, 3D-QSAR, and In Silico ADMETox Studies. Sci. Rep. 2019;9:17096. doi: 10.1038/s41598-019-52764-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Larregieu C.A., Benet L.Z. Drug Discovery and Regulatory Considerations for Improving In Silico and In Vitro Predictions that Use Caco-2 as a Surrogate for Human Intestinal Permeability Measurements. AAPS J. 2013;15:483–497. doi: 10.1208/s12248-013-9456-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deb P.K., Al-Attraqchi O., Prasad M.R., Tekade R.K. Dosage Form Design Considerations. Volume I. Elsevier; Amsterdam, The Netherlands: 2018. Protein and Tissue Binding: Implication on Pharmacokinetic Parameters. [Google Scholar]
- 42.Mikov M., Đanić M., Pavlović N., Stanimirov B., Golocorbin-Kon S., Stankov K., Al-Salami H. The Role of Drug Metabolites in the Inhibition of Cytochrome P450 Enzymes. Eur. J. Drug Metab. Pharmacokinet. 2017;42:881–890. doi: 10.1007/s13318-017-0417-y. [DOI] [PubMed] [Google Scholar]
- 43.Correia M.A., Monteflano P.R.O. Inhibition of cytochrome P450 enzymes. In: Ortiz de Montellano P.R., editor. Cytochrome P450. Springer; Cham, Switzerland: 2015. [Google Scholar]
- 44.de Oliveira Moraes A.D.T., de Miranda M.D.S., Jacob Í.T.T., da Cruz Amorim C.A., de Moura R.O., da Silva S.Â.S., Soares M.B.P., de Almeida S.M.V., de Lima Souza T.R.C., de Oliveira J.F., et al. Synthesis, in vitro and in vivo biological evaluation, COX-1/2 inhibition and molecular docking study of indole-N-acylhydrazone derivatives. Bioorg. Med. Chem. 2018;26:5388–5396. doi: 10.1016/j.bmc.2018.07.024. [DOI] [PubMed] [Google Scholar]
- 45.Nakajima M., Yoshida R., Shimada N., Yamazaki H., Yokoi T. Inhibition and inactivation of human cytochrome P450 isoforms by phenethyl isothiocyanate. Drug Metab. Dispos. 2001;29:1110–1113. [PubMed] [Google Scholar]
- 46.Hu B., Joseph J., Geng X., Wu Y., Suleiman M.R., Liu X., Shi J., Wang X., He Z., Wang J., et al. Refined pharmacophore features for virtual screening of human thromboxane A2 receptor antagonists. Comput. Biol. Chem. 2020;86:107249. doi: 10.1016/j.compbiolchem.2020.107249. [DOI] [PubMed] [Google Scholar]
- 47.Björnsson E.S. Hepatotoxicity by Drugs: The Most Common Implicated Agents. Int. J. Mol. Sci. 2016;17:224. doi: 10.3390/ijms17020224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vedani A., Smieško M. In Silico Toxicology in Drug Discovery—Concepts Based on Three-dimensional Models. Altern. Lab. Anim. 2009;37:477–496. doi: 10.1177/026119290903700506. [DOI] [PubMed] [Google Scholar]
- 49.Pires D.E.V., Blundell T.L., Ascher D.B. pkCSM: Predicting Small-Molecule Pharmacokinetic and Toxicity Properties Using Graph-Based Signatures. J. Med. Chem. 2015;58:4066–4072. doi: 10.1021/acs.jmedchem.5b00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drwal M.N., Banerjee P., Dunkel M., Wettig M.R., Preissner R. ProTox: A web server for the in silico prediction of rodent oral toxicity. Nucleic Acids Res. 2014;42:W53–W58. doi: 10.1093/nar/gku401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Banerjee P., Siramshetty V.B., Drwal M.N., Preissner R. Computational methods for prediction of in vitro effects of new chemical structures. J. Cheminform. 2016;8:51. doi: 10.1186/s13321-016-0162-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.CLSI . Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts. 3rd ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2008. [Google Scholar]
- 53.CLSI . Reference Method for Broth Dilution Antifungal Susceptibility Testing of Filamentous Fungi. 2nd ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2008. [Google Scholar]
- 54.Oliveira D.S. Master’s Thesis. Universidade Federal Fluminense, Faculdade de Medicina Veterinária; Rio de Janerio, Brazil: 2016. de Avaliação Clínico-Epidemiológica e Perfil de Sensibilidade a Antifúngicos de Sporothrix brasiliensis Isolados a Partir de Felinos Domésticos do Estado do Rio de Janeiro. [Google Scholar]
- 55.Novais J.S., Rosandiski A.C., De Carvalho C.M., Silva L.S.D.S., Souza L.C.D.S.V.D., Santana M.V., Martins N.R.C., Castro H.C., Ferreira V.F., Gonzaga D.T.G., et al. Efficient Synthesis and Antibacterial Profile of Bis(2-hydroxynaphthalene- 1,4-dione) Curr. Top. Med. Chem. 2020;20:121–131. doi: 10.2174/1568026619666191210160342. [DOI] [PubMed] [Google Scholar]
- 56.Sander T., Freyss J., Von Korff M., Reich J.R., Rufener C. OSIRIS, an Entirely in-House Developed Drug Discovery Informatics System. J. Chem. Inf. Model. 2009;49:232–246. doi: 10.1021/ci800305f. [DOI] [PubMed] [Google Scholar]
- 57.Daina A., Michielin O., Zoete V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017;7:42717. doi: 10.1038/srep42717. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are contained in the main text of the article.