Abstract
Background
Inspired by nature, the biomimetic approach has been incorporated into drug nanocarriers for cancer targeted chemotherapy. The nanocarriers are cloaked in cell membranes, which enables them to incorporate the functions of natural cells.
Key scientific concepts of review
Nanocarriers surface engineered with cell membranes have emerged as a fascinating source of materials for cancer targeted chemotherapy. A distinctive characteristic of cell membrane-coated nanocarriers (CMCNs) is that they include carbohydrates, proteins, and lipids, in addition to being biocompatible. CMCNs are capable of interacting with the complicated biological milieu of the tumor because they contain the signaling networks and intrinsic functions of their parent cells. Numerous cell membranes have been investigated for the purpose of masking nanocarriers with membranes, and various tumor-targeting methods have been devised to improve cancer targeted chemotherapy. Moreover, the diverse structure of the membrane from different cell sources broadens the spectrum of CMCNs and offers an entirely new class of drug-delivery systems.
Aim of review
This review will describe the manufacturing processes for CMCNs and the therapeutic uses for different kinds of cell membrane-coated nanocarrier-based drug delivery systems, as well as addressing obstacles and future prospects.
Graphical Abstract
Keywords: Nanocarriers, Cell membrane, Cancer, Chemotherapy, Targeted drug delivery
Background
Cancer has been a worldwide concern for a long period of time and is the second largest cause of mortality [1]. Conventional chemotherapy, as one of the most frequently used methods for cancer treatment, remains unsatisfactory owing to the significant side effects and the poor targeting ability of anti-cancer drugs [2]. To overcome these issues, significant research and development has been conducted on targeted drug delivery systems (TDDS), particularly nanocarrier-based TDDS [3]. The benefits of nanocarriers, which include the ability to be modified, a large capacity for drug loading, and tunable physiochemical characteristics, make them ideal for encapsulating anti-cancer drugs and altering their stability, solubility, and in vivo behaviour [4]. Nevertheless, surface modification of nanocarriers may enhance their blood circulation and enable more precise targeting, thus increasing effectiveness while trying to minimize side effects [5]. However, there are also many disadvantages that make it difficult for nanocarriers to live up to clinical standards. The immune system recognizes and eliminates the majority of nanocarriers as foreign substances. Since the polyethylene glycol (PEG), a hydrophilic polymer, was initially incorporated into a protein medication [6], PEGylation has been the most frequently utilized modification technique in drug delivery applications [7]. Additionally, the targeted capacity of nanocarriers was highly reliant on the surface modification, which was challenging to manufacture and accomplish [8]. As a result, TDDS delivered through nanoparticles has not yet achieved its full therapeutic potential.
The drug-delivery system's (DDSs) technology continues to advance, making it possible to administer more potent drugs [9]. Drug research efforts are significantly aided by therapeutic compounds’ capacity to remain intact in a hostile extracellular milieu [10]. In this connection, efforts to reduce immunogenicity and improve biopharmaceutical stability through modification of biopharmaceuticals have increased [11]. Cells in the early 1980s were used as drug delivery vehicles, which substantially increased the drugs' retention and targeting capabilities [12]. Despite the increasing use of live cell-based carriers, several shortcomings persist. One major concern is passenger drug activity, as drugs may be digested by the cell carrier’s lysosomes [13]. Moreover, drug release is difficult to control due to exocytosis or leakage during transport [14]. Faced with these challenges, scientists recently discovered a natural way to design biomimetic cell membrane nanocarriers. At first, the biomimetic cell membrane nanocarriers were made from a poly (lactic-co-glycolic acid) (PLGA) core and a red blood cell (RBC) membrane shell, using a co-extrusion process [15]. Then, different cell membrane-coated nanocarriers (CMCNs) were explored with different nanocarrier cores and membrane materials. The incorporation of nanocarriers into the cell membrane merges the advantages of material science and biomimicry. It is important to note that CMCNs can be portrayed as autogenous cells to prolong blood circulation time and avoid immune system elimination, both of which are required for the enhanced permeability and retention (EPR) effect of cancer targeted chemotherapy [16] (Fig. 1).
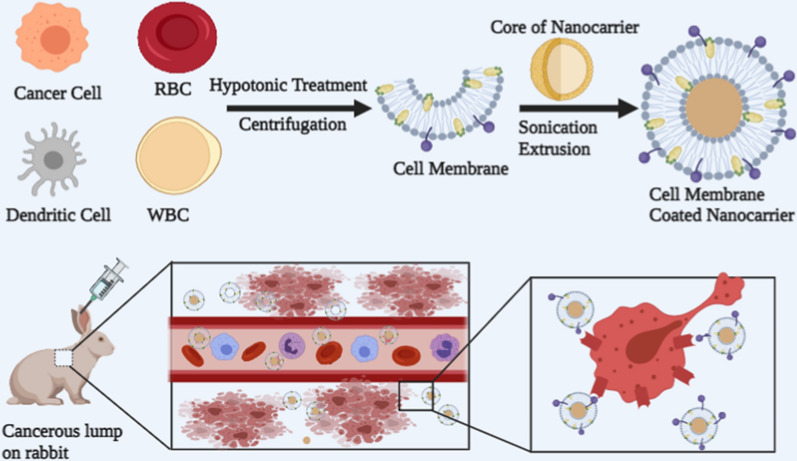
Fig. 1.
Nanocarriers with a cell membrane coating for cancer drug delivery. Different types of cell membranes are used to encapsulate various types of nanocarrier core for cancer treatment
Moreover, different cell membranes may confer different functions on CMCNs, resulting in varying in vivo behaviour. Biomimetic technology, a relatively new procedure, satisfies these requirements and is currently being used in designing drug nanocarriers [17, 18]. By drawing inspiration from nature that comprises biological elements and living matter, this technology aims to overcome the shortcomings of current drug delivery systems. An ideal biomimetic delivery system exploits pathogens’ immune evasion and intracellular uptake tactics. However, delivery systems derived from pathogens continue to raise safety concerns, including immunogenicity and virulence [19].
Advantages of CMCNs based drug delivery systems
CMCNs have notably contributed to suppressing drug resistance in the use of nanocarriers for cancer therapies. Biomimetic CMCNs possess special characteristics, such as prolonged drug delivery, immunological evasion, homotypic targeting, longer blood circulation, and specific ligand/receptor recognition. To get beyond the restrictions of cell toxicity, differentiation, and sensitivity in cell-based delivery systems, CMCNs utilize therapeutically relevant cell membrane proteins as an alternative to the whole cell. Because a longer circulation time benefits with the potential of sustained drug delivery and increases the probability of sustained distribution into the circulation [20]. The biomimetic CMCNs provide bio-modulation and more control in this regard. The CMCNs prepared by coating RBC membrane on PLGA nanocarriers improved the nanocarriers’ retention in the blood by 72 hours, compared to 15.8 hours for typical synthetic stealth nanocarriers [15]. Moreover, PLGA nanocarriers with a fluorocarbon core masked in an RBC membrane were used for delivering oxygen to solid tumours, demonstrating another application of CMCNs delivery to improve blood circulation time via the EPR approach [21].
The reduced immunogenic characteristics of cancer cell membranes and their homing abilities improve targeted drug delivery at the cancer site. In this respect, Cao et al. investigated the interaction between VCAM-1 of metastatic cancer cells with macrophage α4 proteins to transport cytotoxic anticancer drugs to the lungs [22]. Using the adhesion characteristics of galectin-3 and T antigen in cancer cell membranes, Fang et al. demonstrated homotypic tumour targeting [23]. Furthermore, when compared to other active targeting methods, incorporating iron oxide nanocarriers into fractured cancer cell membranes for tumor targeting demonstrated superior homing to homologous tumors in vivo [24]. Recently designed leuko-like vectors (LLV) targeting metastatic niches utilizing neutrophil membrane-coated nanocarriers have shown a two- to threefold increase in metastatic foci accumulation compared to PLGA-PEG nanocarriers and bare nanocarriers, respectively [25]. This affinity for metastatic niches is enhanced by the presence of N cadherin, Mac-1, and other sticky proteins produced on neutrophil membranes on CMCNs, as opposed to the usual PEG coating employed to prolong circulation half-life and prevent clearance [26]. Interestingly, PLGA nanocarriers coated with T lymphocyte membranes were also capable of retaining their lymphocyte coating and evading lysosome sequestration, while bare nanocarriers were caught in endolysosomal compartments prone to breakdown in in vivo [27]. Moreover, this study also discovered that T lymphocyte-coated nanocarriers had a twofold increase in particle density throughout tumours in mice when compared to naked nanocarriers. Numerous additional research groups are attempting to harness the cell membrane’s inherent properties to create biomimetic drug carriers for cancer treatments.
Considerations of CMCNs
Choice of cell membrane
A thorough understanding of the homeostasis, function, and structure of cells in their complex physiological context provides key hints for better biointerfacing of synthetic DDSs [28]. A delivery system with the ability to protect cargo and carry cell features like autonomous activity, compartmentalization, flexibility, and form can be more convenient and beneficial than other delivery systems. The cell membrane repeats the surface functionality of cells and extracellular vesicles as it is the fundamental structural component of them. It is primarily made up of carbohydrates, proteins, and lipids, and it interacts with the environment to survive and grow [29]. Carbohydrates play a part in cellular recognition, whereas proteins are responsible for adhesion and signaling, and lipid bilayer formation combines structural fluidity and stiffness [30–32]. Cell membranes can be differentiated based on the properties and composition of these three components in them. The potential to profit from native cell membrane functions has sparked tremendous scientific interest in coating nanocarriers. If done appropriately, the cell membrane retains its capability, and its coating enhances biointerfacing.
The selection of the appropriate cell type or cell membrane is crucial for ensuring site-specific distribution and targeting as well as for minimizing adverse interactions with complementing systems in vivo. Every cell type has unique biological features, making them suitable for certain therapeutic applications such as infectious diseases, inflammatory diseases, cancer, and personalized therapy [33]. For example, the membrane of RBCs is rich with glycophorins that play a key role in attracting pathogens to their surface and killing them via oxytosis [32]. The application of an RBC membrane to the nanocarriers thereby increases pathogen clearance, long-term circulation, and cell viability. Platelets interact with injured endothelial cells and engage with immune cells to mobilize them toward the inflamed site [34]. As a result, covering the nanocarriers with the platelet membranes allows for selective adherence to tumour tissues or wounded vessels, targeting circulatory tumour cells, pathogen eradication, and the capability to elude detection by macrophages. Similarly, macrophage membranes like other leukocytes carry adhesion molecules like VLA-4, LFA-1, PSGL-1, L-selectin, and P-selectin that help with cell adherence [35]. Thus, coating the nanocarrier with macrophage membrane has the ability to bind pathogens while avoiding macrophage recognition and offering active targeting at the cancer site. Moreover, tumor-specific adhesion molecules and antigens such as mucoprotein-1, epithelial-adhesion molecules, lymphocyte-homing receptors (like CD44), galectin-3, integrins, and cadherins are overexpressed on the surface of cancer cell membranes [36]. These antigens and adhesion molecules play a critical role in the contacts among cells and between cells and the surrounding tissue matrix. Generally, cancer cell membranes can cling to their homologous cells [37]. So, wrapping a nanocarrier with a cancer cell membrane prevents macrophage detection, allowing for homotypic tumour targeting, and contributes to the design of personalized cancer therapy.
Cell source
In order to use maximum cell membrane properties, it is essential to consider the state, form, and source of the cell. In this connection, Evangelopoulos et al. demonstrated that the cell source determines the immunogenicity of biomimetic nanocarriers [38]. They studied multilayer cell membrane generated vesicles from various sources for phagocytosis, opsonization, and targeting of inflamed regions. Literature showed that the use of a syngeneic cell membrane coating increased the avoidance of absorption by the liver and immunological repertoire cells [38]. To isolate the cell membrane for the coating of nanocarriers, it is preferred to choose homotypic cells in a healthy state and nourishing phase. The real therapeutic effectiveness of CMCNs requires homogeneity of the cell population. To fulfil this requirement, quantification or expression levels of specific surface markers (e.g., receptors or ligands) plays a dominant role. For this purpose, flow cytometry, Blot Western, and SDS-PAGE techniques can be used to evaluate the cellular state and homogeneity of cell membranes [39]. Identification of cell biomarkers and other ligands for signal transduction, targeting, or any other approach would enhance translational effects.
Membrane stability
CMCNs are preferred for use over targeting nanocarriers prepared via a bottom-up approach because they possess numerous characteristics, including signal transduction, immune evasion, targeting, and therapeutic advantages. To maximize the therapeutic potential of CMCNs, the structural and functional characteristics of the cell membrane should be preserved prior to coating drug carriers. The cell membrane’s stability is critical in determining the overall durability of CMCNs. The microenvironment of tissue and circulation naturally creates torque and shear forces on cells and nanocarriers. Cells survive with these forces and respond to them by actively modulating their cytoskeleton-membrane interactions, lipid profile, ligand density, and ligand concentration. For example, the interaction of intracellular proteins with the cell membrane strengthens the reliability of natural cells. During the isolation of the membrane, some key stability regulators of the cell membrane may be lost or changed. As a result, determining the overall membrane stability of CMCNs becomes critical before moving further with biomimetic-based treatment [40]. Numerous techniques for determining the stability of membrane structures are described in the literature. For visualizing the structural integrity and morphology of cell membranes, advanced fluorescence, lipophilic dye enhanced, Cryo-TEM, and spectrophotometric techniques, for example, are all extremely useful [41]. When it comes to the mechanical or elastic integrity of membranes, ektacytometry may be the best tool for determining membrane elongation in dynamic shear stress [42]. Additionally, the source of lipid composition in the cell also influences the overall stability of CMCNs. In one study comparing the lipidomic profiles of cells, a higher proportion of unsaturated phospholipids was observed in primary cell cultures than other cultured. X-ray scattering, FTIR, and colorimetric lipid assays are all useful tools for assessing the qualitative composition of phospholipids [43].
Membrane-related proteins
The CMCNs interact with the local environment of tissues and cells through proteins present on the cell membranes. So, the appropriate membrane proteins must be kept up in the cell culture. Several transfection and chemical signaling methods may be used to regulate protein expression and cellular states in culture. In fact, long-term cell growth of some cell types may alter their desirable characteristics for CMCNs applications. For example, the culture condition affects the phenotypes of mesenchymal stem cells, which vary across individuals, cell groups, and even batches. The expansion of mesenchymal stem cells in in vitro not only alters mRNA expression patterns but also affects the surface proteins involved in migration and adhesion (e.g., C-met/HGF, CXCR7, CXCR4, etc.) [44]. In the case of nanocarriers coated with immune cell membrane, it is essential to consider the state and cellular source of immune cells, since they undergo different modifications throughout the pro- and post-inflammatory phases (e.g., pro- and post-inflammatory macrophages M1 and M2).
While obtaining the desired membranes is still an attractive approach, it is becoming increasingly favorable to modify the cell surface using proteins, peptides, or small molecules before harvesting the membranes [45]. In this scenario, cell membrane receptors are becoming less sensitive, and this is unknown at this time. In the case of highly biotinylated membranes of erythrocytes, they are more likely to be taken up by macrophages because of the presence of C3b proteins on them. It is suggested that biotinylation may also disable complement regulators or self-markers on the cell surface [46]. As CMCNs appear to have no significant effect on cellular behaviours, they do not entirely reflect what the cells naturally do. Stephan et al. performed a detailed investigation of nanocarriers-tethered T cells to monitor synapse formation, transmigration, antigen, and cell division. They found that the ability of the cell to perform physiological functions was not affected by the conjugation of nanocarriers to the cell membrane [40]. The degree of immune response variability is proportional to the variety of different sources employed in cell membrane engineering and to the technology used to design the membranes. To successfully apply biomimetic-based drug delivery applications to the clinic, it is essential to have extensive CMCNPs characterization and qualification.
Cell membrane extraction
In order to successfully isolate the cell membrane, cell membrane extraction protocols must ensure that there is minimal or no cytosol, mitochondrial, or nuclear contamination. Making use of a pure cell membrane improves surface coating efficiency and uniformity, allowing for maximum functional and structural replication on the nanocarrier surface. To preserve membrane proteins from degeneration, the extraction medium is supplemented with phosphatase/protease inhibitor cocktails that are stored at ice-cold temperatures. Prior to extraction, cells are thoroughly cleaned with saline buffer to remove any remaining remnants of the cell culture medium.
Some cells lack nuclei (e.g., RBCs and platelets), making membrane extraction easy. During membrane extraction, cells are separated first from their tissues using the most suitable techniques. For RBCs, a hypotonic treatment certainly disintegrates the cells and frees the cell membrane to collect through centrifugation in the form of a pink RBC pallet [47]. Again and again, centrifugation purifies the pallet from haemoglobin impurities. For platelets, it is recommended to do multiple freeze–thaw sequences to rapture their membrane by breaking ice crystals to release the cytosol [48]. The free cell membrane is then collected through centrifugation. Sometimes, the collected platelet membranes are treated with a discontinuous sucrose gradient to purify the platelet membrane from any high-density granules, proteins, and intact platelets.
Extraction of the membrane from nucleus-containing cells is slightly more difficult than from nucleus-free cells. Nucleus-containing cells include β-cells, fibroblasts, cancer stem cells, and immune cells (e.g., T cells, NK cells, neutrophils, monocytes/macrophages). These cells can be isolated from established cell lines like MCF-7, 4T1, J447, NK-92, etc., or from blood or tissues (stem cells, cancer cells, T cells, neutrophils, NK cells, etc.). By combining hypotonic treatment with physical disruption procedures, it produces an extract that contains high-density granules, intact cells, and free cell membranes. Finally, the cell membrane is isolated from the mixture through the use of discontinuous sucrose gradient ultrafiltration or differential centrifugation [49, 50].
Membrane functional components such as cholesterol (making structural components), carbohydrates (cellular recognition components), and transmembrane proteins (adhesion and signaling components) can be lost during membrane isolation. Cholesterol helps keep the cell membrane rigid. This loss may reduce the membrane’s mechanical stability. Moreover, proteins also act as membrane skeleton stabilizers by selectively attaching to the junction complex as well as other membrane proteins such as tropomyosin [51]. Therefore, hypotonic buffers containing divalent ions (such as MgCl2) or even adding cholesterol can be effective in reducing protein loss while maintaining membrane stability [52]. Moreover, the right pH, soft rapturing procedures, proper ice-cold conditions, and mild lysis buffer must be adopted for membrane extraction to avoid denaturation of transmembrane proteins/receptors. Once the cell membrane has been isolated, it is freeze dried and kept at − 80 °C to ensure that membrane proteins retain their long-term consistency and features.
Choice of template
A template is a structural component of the CMCNs which can be used for diagnosis and drug delivery due to its various desirable features. Templates can be classified as organic and inorganic, where liposomes, gelatin, and PLGA are organic templates, while inorganic templates include iron oxide (Fe3O4), gold, mesoporous silica, upconversion nanoparticles (UCNPs), PLNPs, and MOFs. Organic templates are simple to use and provide benefits, including biocompatibility, biodegradability, and nontoxicity [53]. Inorganic templates, on the other hand, have electrical, optical, and magnetic properties that influence their selection in a CMCN [54].
For clinical translation, template biodegradability and biocompatibility are critical which are influenced by the degradation and byproducts formation and their subsequent interactions with human body. 231,231 Renal clearance helps avoid the templates adverse effects [55]. FDA-approved templates are regarded the safest in terms of toxicities. Because most organic templates are safer than inorganic ones, they have been practiced in clinical trials [56]. In 2011, a PLGA nanoparticle was used as a template to build these imitating systems [15]. As a synthetic polymer, PLGA can be fabricated into nano and microparticles and have been commonly used for RBC, platelets, cancer cells, neutrophils, dendritic cells, macrophages, cardiac stem cells, and various other templates [47, 49, 57–60]. Gelatin, a natural polypeptide widely used in medicines, food, and cosmetics, has also been utilized for assembly of CMCNs. Patient-derived tumour cells, T-cell, stem cell, and RBC are employed to coat gelatin templates for CMCNs [61–64]. Liposomes have also been used as core for cancer cells, RBCs, and macrophages membranes [22, 65, 66]. Perfluorocarbons (PFCs) are also among the regulated templates where PFCs (Fuosol-DA) was approved in 1989 but was withdrawn from market shortly due to storage issues [67]. However, PFCs are biocompatible, biodegradable, and have high oxygen-carrying capacity with ~ 20 times greater than water thus can be used for oxygen delivery to smallest capillaries and hypoxic tumour locations [68].
The toxicity of inorganic templates depends on the type of utilized metal and its breakdown in vivo. Silica is the safest (FDA-approved) inorganic template and is biodegradable and biocompatible [69]. It has been a research focus for templates due to certain properties including high surface area, porosity, and drugs or photosensitizers loading capability [70]. CMCNs have been reported using spherical silica nanoparticles on RBC, cancer cells, and macrophage membranes [71, 72]. Mesoporous silica nanoparticles can be tuned and chemically modified into various shapes and sizes for desired applications, e.g., prolonged antibacterial property and regulating endogenous reactive oxygen species for oxidative treatment [73]. When combined with CMC mimics, these tunable features could offer therapeutic benefits. The surface charge of silica templates can be changed with 3- aminopropyl triethoxysilane for CTC detection [74, 75]. Iron ions are harmless biodegradation products of Fe3O4 nanoparticles. MSCs and HeLa cells were employed as membranes in several CMC mimics employing Fe3O4 templates [76–78]. MOFs are 3D structures generated by the complexation of organic ligands and metal ions [79]. Their toxicity is associated with the type of organic linkers and metals employed. For example, zinc-based MOFs [zeolitic imidazolate (ZIF-8)] degrade to release Zn2+ ions, an endogenous element with a less detrimental effect on the human body [80]. Post-degradation of TPP-based Gd/Zn MOFs releases gadolinium (Gd3+) and zinc (Zn2+) ions, where Gd3+ is harmful to the kidneys and can pass the blood–brain barrier to accumulate in the brain [81]. Due to their structural arrangement, MOFs have excellent porosity, surface area, and photosensitizer loading capability. Gold microparticles are another inorganic template, but they are not biodegradable and may be harmful thus, nano or ultra-small templates of gold for fast renal clearance is ideal [82]. Gold particles can be shaped into nanoparticles, nanoshells, nanorods, and nanocages, which are all used to fabricate CMCNs.
Procedures for engineering CMCNs
Preparation of CMCNs
The preparation of CMCNs can be processed through four major steps. The first step is to separate the membranes from the parent cells by using a hypotonic buffer to lysate them. Second, the purification of the mixture to separate cellular components and cell membranes by centrifugation [83]. The centrifugation process will be different depending on the cell type. For example, irregular sucrose gradient centrifugation is needed to prepare eukaryote cell membranes because this treatment separates the membrane from nuclei and other cell components. Whereas nuclei-free membranes like RBCs do not require this treatment. Third, preparation of the inner core. Liposomes, gelatin, PLGA, poly (-caprolactone), iron oxide nanoparticles, gold nanoparticles, mesoporous silica nano-capsules, silicon nanoparticles, and other synthetic materials make up the inner cores. The inner core selection for CMCNs is based on the types of cargo to be transported (Fig. 2).
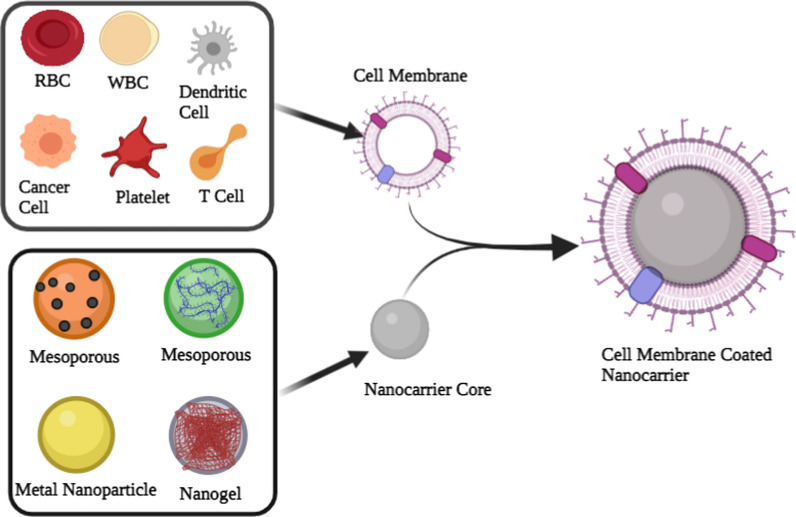
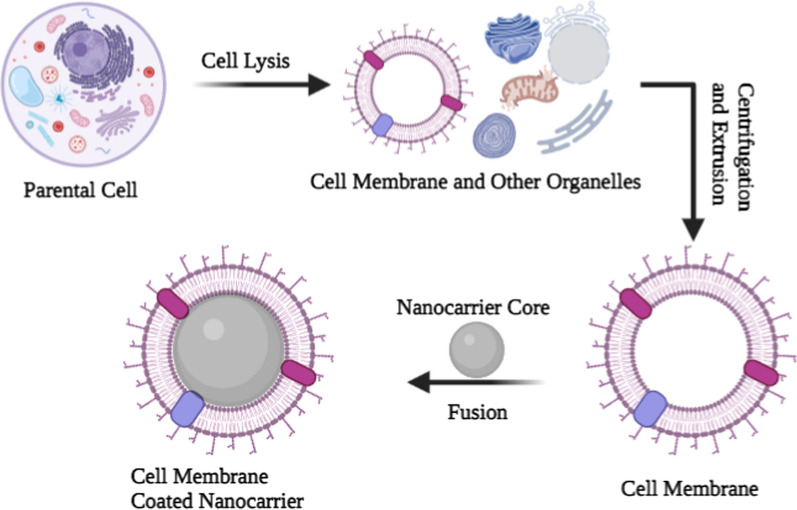
Fig. 2.
The preparation of cell membrane-coated nanocarriers is a multistep process. Cell membranes are typically synthesized in three steps: cell lysis, membrane separation, and extrusion to obtain homogenous cell membrane vesicles
To prepare CMCNs, the inner core nanoparticles and the cell membranes are fused together. The fusion process must be carried out in such a way that it should not result in protein denaturation or drug leakage. The two most frequently used procedures for the fusion of the inner core into cell membranes are ultrasonic treatment and membrane extrusion [84, 85]. Sonication has been employed to fuse the PLGA core into the platelet membrane, which exhibits various “self-recognized” proteins [86]. The duration, power, and frequency of the sonication should be adjusted to minimize drug leakage and protein denaturation and enhance fusion efficiency. In membrane extrusion, membranes are extruded using a technique known as sequential extrusion. In this technique, samples (a mixture of core nanoparticles and cell membrane) are extruded through different-sized pores. It is crucial to control the nanoparticle-to-cell membrane ratio in order to ensure complete surface coverage for both of these techniques [87]. A new microfluidic electroporation-based procedure has recently been developed to apply a full membrane coating on the inner core, which means that different factors, such as flow velocity, duration, and voltage, must be tailored to meet the desired results [88].
Modification of cell membrane
The structure, functions, and components of cell membranes have become more understandable as cell biology progresses [89]. The composition of the cell membrane is mainly composed of a lipid bilayer, while protein and carbohydrate molecules are lodged in the hydrophobic part of the lipid layer [90]. One of the major functions of the cell membrane is to protect the intracellular organelles, which transport nutrients, process waste, and regulate metabolism. Moreover, cell-to-cell contacting signaling is also regulated by the cell membrane. Therefore, the cell membrane can be modified for desirable functions. The modification of the cell membrane may be processed either before disrupting the parent cells (i.e., pre-modification) or additional components are subsequently introduced into membranes after isolation (i.e., post-modification).
In pre-modification, the properties of the parent cell membrane are modified at metabolic or genetic levels. Parent cells are treated with certain chemical or physical stresses to induce the expression of specific lipid or protein components, or to modify the structure of membrane hydrocarbon chains [91]. Metabolic glycosylation is mainly used to control expression levels of native glycans, but it can also be used to introduce artificial monosaccharides into glycol-conjugates [92]. RBCs are one of the most frequently used sources for generating vesicles derived from cell membranes. However, it is impossible to modify mature RBCs genetically due to the absence of nuclei in mature RBCs. To overcome this problem, Lv et al. used the CRISPR gene-editing strategy to engineer an RBC membrane expressing the tripeptide Asn-Gly-Arg (NGR) [93]. Transgenic mice were generated in this study by inserting NRG peptide coding in the pre-embryo stage. A genetic analysis of newborn mice was used to validate the NGR expression. RBCs were isolated from these mice and used to generate RBC membrane vesicles for targeted delivery of an oncolytic virus to tumors. As exogenous physical or chemical coupling onto vesicles may alter protein function, so genetic engineering allows the biosynthesis of certain proteins using the parental protein machinery.
Pre-modification approach results in a more homogenous and secure source of membrane, but the types of ligand and component possibilities are inadequate as compared to the post-modification approach. Several post-modification methods have been developed due to the availability of divers and convenience modified materials. The materials used for modification range from natural lipids [94], nucleic acids [95], and proteins [96], to synthetic components [97]. Cholesterol is one lipid that is used to modify vesicles derived from cell membranes for CMCNs. It plays an important role in the formation of the cell membrane’s lipid bilayer structure. Changes in cholesterol ratios can affect the rigidity and fluidity of membranes [98]. The addition of cholesterol increases the stability of vesicles derived from cell membranes in terms of their resistance to environmental pH changes [94]. In the case of RBCs, adding cholesterol to RBCs and slightly heating them for 10 min increased the rigidity of their vesicles, significantly improving the efficacy of drug loading. Proteins can be conjugated to the cell membrane through insertion or conjugation. For instance, a bifunctional linker functionalized with N-hydroxysuccinimide at one end and maleimide at another terminal was used to conjugate hyaluronidase to the RBC membrane [96]. Another study used an amphiphilic lipid to anchor protein to the surface of a membrane vesicle [97]. In this approach, streptavidin was first attached to 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[maleimide (polyethylene glycol)-2000] and then the lipid tail was inserted into the cell membrane. Inserting a protein-conjugated lipid into the cell membrane enables protein affixing without disturbing membrane surface proteins, thereby increasing the likelihood of membrane proteins retaining their intact structure. However, chemical conjugation of lipid moieties with a protein may alter the configuration of associated proteins. Strategies for conjugating proteins with lipid moieties at specific sites must be carefully designed to minimize possible configurational changes. Another substance used to modify the vesicles derived from the cell membrane is nucleic acids. Aptamers are short single-strand oligonucleotides that may precisely attach to a target substrate. Peng et al. used the 26-mer G-quadruplex oligonucleotide AS1411, which binds to nucleolin, to modify the membrane of cancer cells [95]. The AS1411 aptamer enabled tumor-targeting of membrane vesicles because of the overexpression of nucleolin in tumor tissue (Fig. 3).
Fig. 3.
Post-modification of cell membrane. Cell membranes can be modified with different molecules or biomarkers to modulate their biological behaviors. An illustration of aptamers (A), protein (B), cholesterol (C), and synthetic polymer (D) conjugated cell membrane
It is well known that synthetic polymers, particularly PEG, have been used to modify cell membrane for the preparation of CMCNs [99, 100]. By protecting CMCNs from phagocytosis, PEG conjugation increases their colloidal stability and thus their circulation half-life in vivo. PEGylation can be accomplished merely through the incubating PEG lipid derivatives and cell membrane at 37 °C. PEG lipid tails easily insert into membrane layers in these conditions. One issue with current PEGylation methods for membrane vesicles is the lack of precise quantification. The outcome of PEGylation may be dependent on the compactness of PEG on the vesicles. As a next step, researchers should establish standard procedures for PEGylation of the cell membrane.
Cell membrane hybridization
It is possible to create a hybrid cell membrane by fusing two parent cell membranes. These cell membranes have both parental cell membrane properties. Hybrid cell membranes can synergistically carry out complex behaviors. Several studies have used hybrid cell membranes to coat synthetic nanocarriers [101, 102]. For example, RBC membrane-coated nanocarriers can avoid reticuloendothelial clearance because they express CD47 (immunoregulatory marker) [103]. Similarly, P-selectin is a ligand of the CD44 receptor found in platelet membranes, allowing it to be targeted at cancer cells [104]. These membranes can be used to coat nanocarriers to improve drug delivery efficiency. It was discovered that PLGA nanocarriers coated with RBC-platelet membrane have a longer blood circulation time and better binding to MDA-MB231 breast cancer cells than plain PLGA nanoparticles [103]. Another study used homotypic targeting by fusing cancer cell membranes with RBC membranes [105]. The hybridized MCF7-RBC membrane-coated nanocarriers were found to be highly effective in terms of photothermal effect and accumulation at tumor site in MCF7 tumor-bearing mice. This study established that the protein proportion of dual membranes was a significant predictor of homotypic impact and blood retention. To achieve the best performance, the ideal proportion of the two membranes must be found empirically. Not only may hybrid membranes be formed by fusing two cell membranes together, but they can also be formed by fusing a cell membrane and a liposome together. Pitchaimani et al. reported a nanocarrier coated with a hybridized membrane of the natural killer cell membranes and liposomes [106]. The hybridization of liposome membranes in this approach enables the incorporation of several lipid components of liposomes into the cell membrane.
Pure cell membrane used in nanocarrier coating
Red blood cells
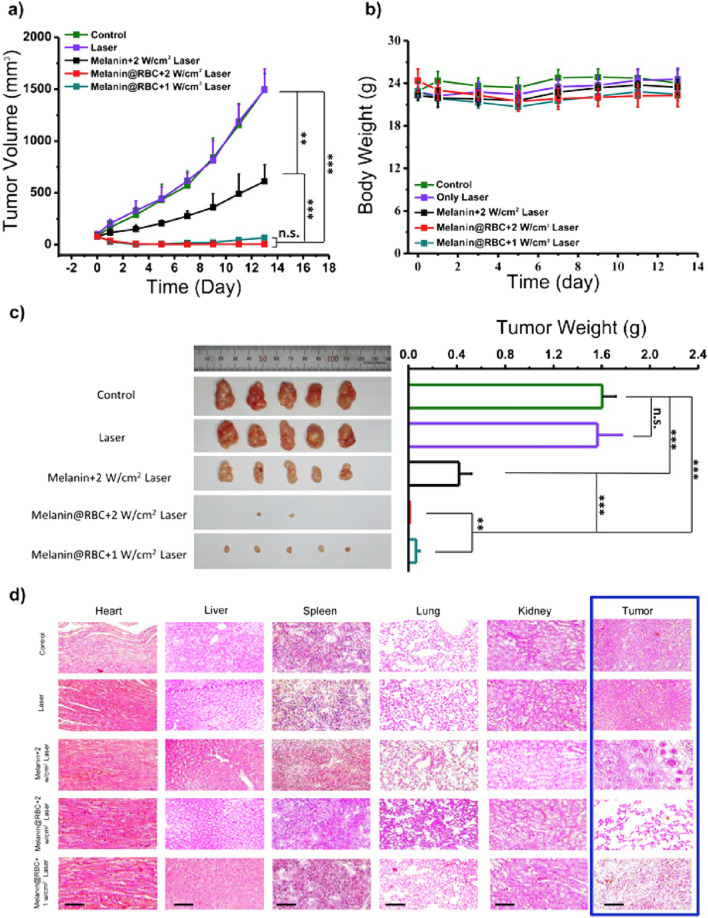
RBCs have attracted considerable interest as a biomaterial for nanocarriers coating [83]. In humans, RBCs have a short lifespan of up to 120 days. This short-lived property of RBCs makes them an excellent source of membrane for coating nanocarriers. RBCs have a significant role in the removal of pathogens from the body via oxycytosis during the transportation of oxygen [107]. RBCs also express the ‘don’t eat me’ marker CD47, which binds to the macrophage-expressed signal-regulatory protein α preventing it from being taken up [108]. Therefore, the use of an RBC membrane to coat the nanocarrier improves the detoxification process, the removal of pathogens, and long-term circulation. Because of these properties, the RBC membrane can be used for coating a variety of nanocarriers to deliver drugs targeting breast cancer and colon cancer [108–111]. However, RBC membrane can also be functionalized with iRGD peptide and folate receptor to target breast cancer [112, 113]. For targeting the brain, targeting ligands such as T7, cRGD peptide, DCDX peptide, and NGR peptide are incorporated into the RBC membrane [97, 114, 115]. Coating nanocarriers taking in anticancer drugs, photodynamic or photothermal agents with RBC membranes can be used to address the problem of short blood retention time. Recently, a study reported melanin nanocarriers coated with RBC membrane for effective photothermal cancer therapy [116]. They observed that melanin nanocarriers coated with RBC membrane had higher photo thermal efficacy in vivo than bare melanin nanocarriers due to improved blood retention and tumor site accumulation. RBC membranes have also been coated on iron oxide nanomaterials capable of photothermal conversion [111]. The iron oxide clusters coated with RBC membrane retain their photothermal properties while being less absorbed by macrophages. After intravenous injection, iron oxide clusters coated with RBC membrane showed less liver distribution and more tumor accumulation in mice. Mesoporous nanocarriers encapsulating doxorubicin have also been coated with RBC membranes for photochemotherapy of cancer [117]. Plain mesoporous nanocarriers have a short half-life and nonspecific macrophage uptake. To fight against cancer, the RBC membrane coating decreases non-specific uptake and increases blood circulation time while combining phototherapeutic and chemotherapeutic effects (Fig. 4).
Fig. 4.
a Curves of tumor volume in A549 tumor-bearing mice treated with various agents. b Curves of body weight of mice in each group. c Images of tumors dissected on the 13th day following photothermal treatment, as well as a comparison of each group’s tumor weight. d Hematoxylin and eosin staining images of major organs and tumor tissues dissected on the 13th day following photothermal treatment. Reproduced with permission from [116]
Modification of RBC membranes with specific ligands can improve delivery to target tissues. For example, when RGDyK peptide was inserted into the RBC membrane used for coating of drug nanocrystals, they had a better distribution to tumors and antitumor efficacy than nanocrystals coated with unmodified RBC membrane or plain nanocrystals [97]. The CDX peptide derived from the neurotoxin was also used for the modification of RBC membranes to target brain tissues [115]. The CDX peptide was anchored to RBC membranes by streptavidin–biotin. In a glioma mouse model, CDX peptide added to RBC membranes increased brain delivery. Zhou et al. chemically rooted hyaluronidase onto the surface of RBC membranes via bifunctional linker succinimidyl-[(N-maleimidopropionamido)-polyethyleneglycol] ester to improve tissue penetration [96]. The modification of RBC membranes did not affect their pharmacokinetics and hyaluronidase also showed its activity as usual.
White blood cells
White blood cells (WBCs) are colorless, nucleated spherical blood cells that influence disease progression. Nanocarriers surface engineered with a WBC membrane have been widely used as anticancer drug carriers in recent years due to their immune escape and active targeting abilities [118]. The most used WBCs for surface engineering of nanocarriers are neutrophils and macrophages. Neutrophils are the first immune cells to respond to tumours or infection and are closely linked to tumor progression, making them ideal carriers of antitumor drugs. They are activated by chemokines or cytokines like interferon-gamma, interleukin 8, granulocyte–macrophage colony-stimulating factor, and tumour necrosis factor α which direct them to the inflammation or infection site [119]. It has been shown that conformational variations in integrins such as L-selectin, P-selectin, macrophage-1 antigen, LFA-1, and VLA-4 also support neutrophil mobilization via extravasation from blood vessels [120]. Therefore, the neutrophil membrane can be used for surface engineering of nanocarriers to target breast cancer, circulating tumour cells, lung cancer, and premetastatic niches [25, 50, 121]. Zhao et al. reported a biomimetic nanocarrier (PTX-CL/NEs) prepared by coating PTX-loaded liposomes with neutrophil membranes [122]. PTX-CL/NEs successfully target tumor sites, release drugs, and inhibit tumor growth and recurrence. Cao et al. surface engineered Celastrol-loaded PEG-PLGA nanocarriers with neutrophil membranes [123]. Coating with neutrophil membranes allowed nanocarriers to pick up by chemokines, pass through the blood-pancreas barrier, and reach the tumor site. Although neutrophil membranes are rich in targeting content and fast to pick up by chemokines, they are preferred to use in acute treatment situations [124]. In the case of allogeneic blood as a source of WBC membranes, infectious disease screening and blood type compatibility are required because the WBCs are extremely diverse [125] (Fig. 5).
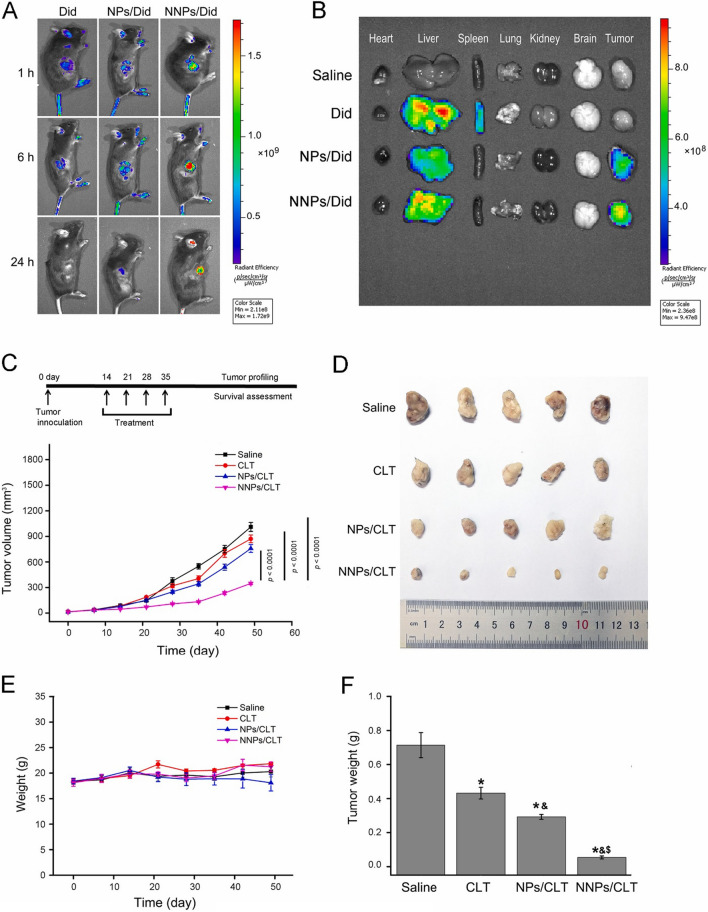
Fig. 5.
Antitumor efficacy of neutrophil membrane-coated nanocarriers in mice. A Images of mice after i.v. injections of Dil stain, Dil stain loaded PEG-PLGA nanocarriers, neutrophil membrane-coated Dil stain loaded PEG-PLGA nanocarriers. B Images of major organs and tumors after i.v. injections at 24 h, C average tumor volumes following various treatments over time, (D) morphology of tumors after 35 days, (E) variations in body weight, and (F) variations in tumor weight each treatment group over time [123]
Macrophages are classified as M1 or M2 depending on their activation state. M2 macrophages reduce inflammation, suppress the immune system, and promote tumour growth, whereas M1 macrophages cause inflammation, stimulate the immune system, and extinguish tumour tissue [126]. M1 macrophages’ antitumor effect is derived from surface markers like CD86, CD80, and MHC-II. Therefore, macrophage membrane-coated nanocarriers have been widely employed for developing antitumour nanocarriers targeting breast cancer and lung metastasis of breast cancer [22, 35, 127]. The microenvironment of cancer affects macrophages, so their antitumor effect is often enhanced by administrating macrophages with other therapies. Hu et al. synthesized biomimetic nanocarriers [(C/I)BP@B-A(D)&M1m] that were encapsulated in the M1 macrophage membrane [128]. Numerous molecules involved in over expression of major histocompatibility complex (MHC) and costimulatory signal transduction on the cell membrane enabled (C/I)BP@B-A(D)&M1m to target cancer tissues effectively. When combined with laser irradiation, (C/I)BP@B-A(D)&M1m efficiently released drugs at the site of application. Liu et al. synthesized a mixed micelle containing bilirubin (ROX-responsive) and chlorin e6 (photosensitizer), loaded with paclitaxel dimer, and wrapped into a macrophage membrane. By co-delivering paclitaxel dimer and Ce6, these nanocarriers effectively combine photodynamic and chemotherapy therapy. Macrophage membranes can shield drugs from being taken up by macrophages, which increases the likelihood of nanocarriers being absorbed and retained by tumor cells.
Platelet
Platelets are nucleate cells of blood produced by megakaryocyte fragmentation and are involved in tumor metastasis, thrombosis, and blood coagulation [129]. Platelet membranes have the ability to escape phagocytosis in systemic circulation. Like RBCs, the platelet membrane has CD47 receptors. CD47 receptors interact with regulatory proteins that inhibit macrophage receptors and can affect the pharmacokinetics of encapsulated drugs. Platelet glycoproteins may also interact with collagen-rich plaque [130], assisting in the targeting of atherosclerotic sites by platelet membrane-coated nanocarriers. So, platelet membrane coating enables nanocarriers to escape from macrophages and selectively bind injured vessels and tumour tissues. Because of these properties, platelet membrane coated nanocarriers can be used to target breast cancer lung metastasis and circulating tumour cells [57, 75]. When using nanocarriers coated with platelet membranes, it is suggested to focus on CD47 receptor integrity. A functional change in the CD47 receptor may affect biodistribution and pharmacokinetics of nanocarriers. Nanocarriers coated with platelet membranes should not be used in patients with autoimmune diseases. Platelet autoantibodies may form immune complexes with nanocarriers [131].
In recent years, the number of platelet membrane coated drug delivery systems has increased rapidly due to their easy extraction, purification, and accumulation at cancer sites [132]. Rong et al. reported a nanocarrier of platelet membrane coated black phosphorus quantum dots carrying hederagenin (PLT@BPQDsHED) [133]. PLT@BPQDs-HED had a stronger fluorescence signal at the cancer site and a higher retention rate than the control group after 48 h. A higher efficiency of drug delivery is achieved by PLT@BPQDs-HED because selectin on the platelet membrane specifically attaches to the CD44 receptor overexpressed in cancer tissue. Platelets are much more related to cancer cells, and the nanocarriers that are wrapped into platelet membranes avoid clearance by the immune system and specifically target cancer tissue via the proteins on the membrane surface. Platelet membrane-coated drug delivery systems have the potential to be used in combination with immunotherapy and phototherapy. Wu et al. wrapped nanocarriers comprising the anticancer drug and polypyrrole into platelet membranes [134]. Platelet membrane enables the drug delivery system to escape from immune systems and target the cancer tissue, laser irradiation triggers polypyrrole to cause hyperthermia and ablate the cancer cells, and anticancer drugs are also discharged from the nanocarriers to destroy the cancer tissue.
Cancer cell
Cancer is described as abnormal cell growth that could lead to metastasis. Cancerous cells’ membrane display a variety of tumour-specific adhesion and antigen moieties. There are a wide range of molecules involved in cell–cell and cell–matrix adhesion, such as mucoprotein-1, epithelial adhesion moieties, lymphocyte-homing receptors, galectin-3, integrins, and cadherins [36, 135, 136]. Cancer cells possess properties that collectively serve a self-protective function, such as homotypic cell adhesion and immune system evasion [137]. Since these cells have unique characteristics, their membranes have gained popularity as coating stuff for nanocarriers. The dispersed membrane of cancer cells on nanocarriers allows various characteristics of cancer cells to be introduced to the nanocarriers for targeting homotypic tumours and developing personalized cancer therapy [66, 138]. Metal oxide nanoparticles, gelatin particles, mesoporous silica, and PLGA nanocarriers have all been wrapped into cancer cell membranes and used to deliver anticancer drugs [24, 72, 139, 140].
Membranes of cancer cells have the feature of homologous targeting that can be used for targeting homologous toumors [24]. In this respect, iron oxide nanocarriers were coated with HeLa cell and UM-SCC-7 membranes. When these coated nanocarriers were allowed to incubate with HeLa, HepG2, UM-SCC-7, and COS7 cells. The coated nanocarriers showed a high affinity towards HeLa cells and UM-SCC-7 cells. They could also self-target a homologous tumor and effectively restrain tumor growth in vivo. Some studies also reported the blood–brain barrier crossing ability of cancer cell membranes [141, 142]. For example, nanoparticles of polycaprolactone/F68 were coated with secondary brain cancer cell membranes and then loaded with indocyanine green, a photothermal and imaging agent [141]. Intravenous injection of these nanocarriers into mice bearing U87MG-Luc glioma cells showed high distribution in the brain. Similarly, PEG-PLGA nanocarriers coated with MDA-MB-831 cancer cell membrane were investigated for use in treating brain cancer [142]. They found that the accumulation of coated nanocarriers in the brain was higher than uncoated nanocarriers.
T cells
T cells play an important role in adaptive immune responses [143]. T cells need antigen priming through a specific T-cell receptor (TCR) for activation. The dendritic cells (DCs) possess the MHC-antigen complex that engages with the TCR and activates T cells. Activated naive T cells become regulatory or effector T cells, depending on the DC-T cell immune synapse context. Effector T cells scavenge and kill cancerous or virus-infected cells in the bloodstream. Moreover, T cells can also mature into memory T cells, which offer long-lasting protection against foreign bodies that activated them. Therefore, T cell membranes coated nanocarriers can be used to target gastric cancer, liver cancer, and tumour tissues [85, 92, 144].
T cell membranes were used to wrap PLGA nanocarriers loaded with dacarbazine [145]. In this study, T cell membranes were extracted from the EL4 cell line and incubated with PLGA nanocarriers loaded with dacarbazine. T cell membrane-coated nanocarriers were able to bypass tumor immune suppression and neutralize TGF-b1 and PD-ligand 1 expression in the tumor environment. Furthermore, T cell membrane-coated nanocarriers improved dacarbazine delivery and enhanced apoptosis of tumor cells. Ma et al. reported the development of a nanocarrier composed of mesoporous silica holding IR780 nanoparticles wrapped into the membranes of chimeric antigen receptor T cells (CAR-T) to exclusively target hepatocellular carcinoma cells (HCCs) expressing GPC3 [85]. They engineered the CAR-T cell nanocarrier in such a way that it could detect GPC3-expressing HCCs. The results demonstrated that NP-coated CAR-T cell membranes were more effective at targeting HCC cells in vivo and in vitro than IR780-loaded mesoporous silica. CAR-T cell therapy is a newer blood cancer treatment. Ex vivo CAR-T cells are produced by genetically modifying TCR to recognize an antigen without antigen presentation. Ex vivo-amplifier CAR-T cells are then reinfused into hematological cancer patients. The FDA has approved CAR-T cell targeting of the CD19 antigen for the treatment of relapsed/refractory diffuse large B-cell lymphoma or acute lymphoblastic leukemia.
Dendritic cells
Dendritic cells (DCs) are immune cells that gather around cancer cells due to immune signals (such as pathogen-associated molecular patterns and proinflammatory cytokines). They transfer tumor-associated antigens to lymph nodes to establish communication with naive T cells for differentiation into attack cancer cells and mature T cells [146]. For this reason, designing tumor immunotherapy around DCs characteristics is a promising approach. However, issues like complex preparation methods, short efficacy periods, and high cost still need to be addressed [147]. DC membranes contain components like DC-originating molecules and can target and stimulate the immune systems of their source cells [148]. It has been shown that CD40/CD80/CD83/CD86 are upregulated on the DC membranes as co-stimulatory receptors [149]. The binding of these molecules to their respective receptors on T-cells activates DCs to produce cytokines such as IL-10, IL-12, and interleukin that distinguish T cells into their anti-inflammatory or pro-inflammatory subsets. Therefore, DC membranes coated nanocarriers can be used to target prostate cancer and ovarian cancer [150, 151]. Cheng et al. reported an IL-2-loaded PLGA nanocarrier warped in membranes derived from DCs [151]. The DCs derived membranes provide unique and potent stimulatory signals and sustain a strong T-cell response due to their intact surface proteins. The nano-dimensions of this carrier may be a significant contributor to the T cell response by eliminating spatial barriers throughout antigen presentation. Zhang et al. used a combination of a nanocarrier-based antigen delivery system and photochemical internalization to induce tumor-specific cytotoxic T cells in their study [152]. It was demonstrated that the combination of a hydrophobic photosensitizer (Pheophorbide A) and polyethyleneimine possessed the ability to evade endosomal degradation while also enabling near-infrared imaging. Moreover, by grafting the synthesized complex onto ovalbumin, a model antigen, light-sensitive nanocarriers were formed.
Hybrid membrane used in nanocarrier coating
Hybrid membranes can be used to combine the properties of a variety of cell membranes and optimize their function [101]. In general, hybrid membrane coated nanocarriers (HMCNs) more specifically interact with the cancer environment, resulting in improved specific targeting, minimizing non-specific interactions with abundant proteins and cellular components, and optimizing specific biological roles [153]. Moreover, a hybrid membrane incorporates at least two distinct biological activities. One is a competence for targeting, whereas the other refers to inherent properties conferred by the membranes of a source cell. The targeting potential is primarily comprised of homologous targeted delivery to tumor sites via DC membranes and cancer cell membranes, specific tumor targeting via PLT membranes, the capability of tumor targeting enhancement via membranes of stem cells, and circulating tumor cells targeting via WBC and PLT membranes [75, 154–156]. The latter biological function types mainly include prolongation of blood circulation via PLT and RBC membranes; specific adherence to injured vessels via PLT membranes; immune evasion via PLT and WBC membranes; toxin neutralization and absorption via RBC and macrophage membranes; and activation of the immune system via bacterial outer membranes, cancer cell membranes and immune cell membranes. Due to the membrane combination, HMCNs can achieve maximum functionality in diverse biomedical fields.
The leukocyte membrane is considered a naturally occurring coating material with the biomimetic potential, capable of evading immune system capture and inflammatory targeting via inducing inflammation via specialized ligand-receptor interaction [121]. Vectors that are similar to leukocytes could continue their capabilities, such as inhibiting particle phagocytosis and opsonization, facilitating the transportation over the endothelial layer while avoiding the lysosomal pathway and thereby delaying the clearance by the liver [27]. However, a drug delivery system based on a single leukocyte membrane is incapable of achieving adequate therapeutic efficiency because of its incapability towards tumor targeting. Thus, He et al. joined a leukocyte membrane with a cancer cell membrane to increase the targeting potential of HMCNs. The leutusome was produced by fusing together the membranes of leukocytes, tumor cells, and liposomal nanocarriers simultaneously [157]. Encapsulation of paclitaxel (PTX) with leutusomes significantly reduced tumor development without causing systemic damage (in vivo), suggesting that selective taken up of leutusomes by tumor cells. After 48 h, leutusomes labeled with DIR displayed substantial fluorescence in tumor sites that were 9.3-fold larger than those in the control. The liposomal NPs accumulation from leukocytes or cancer cells was 2.7-fold and 4.4-fold more in the tumor, respectively, than in the control. Additionally, the study indicated that coating outside of the cores or incorporation into liposomal nanocarriers had no effect on the unique features of different cell membranes. These composite biomimetic nanocarriers outperform solid tumour homing and have a longer circulation time due to surface markers expressed on both cell types.
Sun et al. developed a cancer cell-RBC hybrid membrane coated gold nanocage loaded with doxorubicin to treat breast cancer via chemotherapy, photothermal therapy, and radiotherapy [158]. Homological targeting of the cancer cell membrane and reduced clearance by the RBC membrane made the HMCNs particularly effective in accumulating in tumor sites. Macrophages have been associated with the early dispersion of cancer and hence have a substantial effect on prolonging metastasis throughout the progression of cancer. Gong et al. developed a hybrid membrane composed of macrophages and cancer cells coated with doxorubicin-loaded PLGA nanocarriers for use in breast cancer treatment to specifically target lung metastases [159]. Since RAW264.7 membrane exhibits enhanced expression of high integrin α4β1, the resultant HMCNs demonstrate remarkable membrane-derived features, which include the capacity to target homologous cancer cells and improved particular metastatic targeting potential. The metastatic nodule numbers in the lung were reduced by about 88.9% after the therapy of lung metastases derived from breast cancer, which performed better than the pure CMCNs. This hybrid membrane derived platform demonstrates promise as a biomimetic nanoplatform for the metastasis treatment of breast cancer.
He and Su’s group previously described the use of HMCNs based on RBC and retinal endotheliocyte membranes for non-invasive therapy of choroidal neovascularization [160]. The RBC and retinal endotheliocyte membranes fusion provide protection to the nanocarrier against phagocytosis while also giving the potential to the HMCNs to bind with vascular endothelial growth factors, enhancing their potential to target choroidal neovascularization regions actively. particularly, the anti-VE-cadherin antibody suppressed the fluorescent signals in HMCNs-treated cells, demonstrating that the ability of self-targeting is dependent on surface binding molecules (N- and VE-cadherin) expression on the retinal endotheliocyte membrane [161]. The substantial fluorescence colocalization of angiogenic retinal endotheliocyte membranes and HMCNs in the tube formation experiment also indicated the nanocarriers’ targeting ability. Furthermore, using a quantitative examination of the mean fluorescence intensity, the group treated with HMCNs drastically decreased damage area and choroidal neovascularization leakage in contrast to the group treated with pure CMCNs in a choroidal neovascularization mouse model induced by laser. In conclusion, dual-fused membrane-based nanocarriers offer significant advantages over currently available invasive therapies.
Challenges and future directions
Numerous advantages have been reported for CMCNs, particularly in terms of biocompatibility and targeting. Synthetic DDSs currently available are basically foreign substances with the potential for immunogenicity and toxicity. Whereas cell membranes are endogenous, they are considered biocompatible and perform a variety of biological functions like the source cell. However, certain issues must be resolved before these carriers can continue to evolve and move from the laboratory to the clinic.
The first and most important question to be addressed is about the yield of cell membranes and extracellular vesicles. Not only do existing separation technologies produce a negligible amount of cell membranes and extracellular vesicles, but they are also prohibitively expensive for large-scale production. As a result, more sophisticated large-scale manufacturing methods are required to continue expanding the application of cell membrane. In recent years, to address the yield issue, extensive work has been carried out on techniques which are used for generating artificial vesicles when the membrane is ruptured via extrusion. For example, the same number of THP-1 cells yield more than twice as many simulated exosomes as natural exosomes, and the drug encapsulating and releasing rates of the simulated exosomes are also higher [162]. The extraction and purification procedures must also be revised and optimized, as many cells must still be cultured to obtain an adequate number of membranes, and the preparation procedure must still be simplified [118]. For RBCs membrane-coated nanocarriers that lack a targeting ability, the membranes must be modified to reach the target site for therapeutic cargo release, but this will likely change the membrane’s original structure and reduce its biocompatibility. Platelet membranes are highly sensitive, so finding an appropriate loading scheme to ensure adequate drug loading and reliable delivery to the target tissue is challenging. The toxicity and stability of modified membranes must also be studied, especially as nanocarriers for cancer therapy. To achieve the desired dose and release profile, the drug loading method should be chosen carefully [163].
Moreover, a complete understanding of the mechanism of transporting cell membranes extracted from different sources in vivo is unknown and requires further research. For example, therapeutic molecules delivered by white cell membrane carriers may activate immune system components and cause inflammation [164]. When cancer cell membrane is used, it may cause cancer in the body if the parent cancer cells’ genetic material is not completely removed. Procedures for purifying and characterizing cell membranes are not consistent and differ from laboratory to laboratory, causing confusion about the physicochemical features of the cell membrane. So, it is necessary to share the scientific data and develop a standardized procedure for cell membrane quality control that is highly repeatable. Nanocarriers wrapped into cell membranes and extracellular vesicles can target cancer tissues crossing biological barriers. Some cells can be used to both extract membranes and isolate extracellular vesicles to transport drugs. While it is relatively simple to extract and prepare the cell membrane, the targeting ability may be compromised due to protein loss during membrane extraction. However, extracellular vesicles are difficult to prepare, they generally retain all membrane components, giving them excellent targeting ability [165]. As a result, the appropriate carrier must be chosen according to the experiment’s objective in order to maximize the therapeutic effect.
Conclusions
The development of therapeutics derived from cell membrane material is a rapidly growing field of research that is particularly appealing because it involves an organic cellular networking system. Biomimetic technology has the advantage of taking advantage of the natural mechanisms of living matter, but it is also a double-edged sword. It is difficult to know which components, out of the multiple factors, confer membrane functionality, and so the ratio of each component needs to be modified as needed. To develop drug-containing membrane-coated carriers, a similarly and standardized manufacturing process will be required. Despite the difficulties associated with processing variables, manufacturing, and quality control, vesicles derived from natural cells have the advantage of being bioactive, reflecting the features of the parent cells. Although membrane-coated nanocarriers face numerous challenges, a powerful advantage of ‘mimicking nature’ overrides many disadvantages of traditional DDSs and offers a more efficient approach for cancer treatment. With the rapid advancement of nanotechnology, proteomics, bioinformatics, pharmacology, and material science, it is expected that the combination of DDSs and cells will overcome numerous obstacles, revolutionize current medical technology, and open up new avenues for targeted cancer therapy.
Acknowledgements
Authors are grateful to Hospital of Hangzhou Medical College for providing necessary facilities.
Authors’ contributions
WL, CY, YW, GR, XH, XT, and SW wrote different sections of the manuscript. WL, CY, and SW edited the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the Foundation of Science Technology Department of Zhejiang Province (No. LGF22H080012, LY19H160037, LGF18H160025) and the funds from Zhejiang Medical Technology Plan Project (No. 2020KY052).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have approved the final draft of this manuscript for submission and have given consent for the publication of identifiable details.
Competing interests
The authors have declared no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Wen Lei, Email: leiwen2017@zju.edu.cn.
Chen Yang, Email: yangchendldx@163.com.
Yi Wu, Email: wuyi10000@126.com.
Guoqing Ru, Email: ruqq111@163.com.
Xianglei He, Email: xianglh992004@163.com.
Xiangmin Tong, Email: tongxiangmin@163.com.
Shibing Wang, Email: wangshibing@hmc.edu.cn.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA: Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Chen W, Zheng R, Zeng H, Zhang S, He J. Annual report on status of cancer in China, 2011. Chin J Cancer Res. 2015;27:2. doi: 10.3978/j.issn.1000-9604.2015.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peer D, Karp JM, Hong S, Farokhzad OC, Margalit R, Langer R. Nanocarriers as an emerging platform for cancer therapy. Nat Nanotechnol. 2007;2:751–760. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- 4.Mitragotri S, Burke PA, Langer R. Overcoming the challenges in administering biopharmaceuticals: formulation and delivery strategies. Nat Rev Drug Discov. 2014;13:655–672. doi: 10.1038/nrd4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Danhier F, Feron O, Préat V. To exploit the tumor microenvironment: passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J Contr Rel. 2010;148:135–146. doi: 10.1016/j.jconrel.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 6.Ekladious I, Colson YL, Grinstaff MW. Polymer–drug conjugate therapeutics: advances, insights and prospects. Nat Rev Drug Discov. 2019;18:273–294. doi: 10.1038/s41573-018-0005-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou M, Huang H, Wang D, Lu H, Chen J, Chai Z, Yao SQ, Hu Y. Light-triggered PEGylation/dePEGylation of the nanocarriers for enhanced tumor penetration. Nano Lett. 2019;19:3671–3675. doi: 10.1021/acs.nanolett.9b00737. [DOI] [PubMed] [Google Scholar]
- 8.Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev. 2013;65:36–48. doi: 10.1016/j.addr.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 9.Moradi Kashkooli F, Soltani M, Souri M. Controlled anti-cancer drug release through advanced nano-drug delivery systems: static and dynamic targeting strategies. J Contr Rel. 2020;327:316–349. doi: 10.1016/j.jconrel.2020.08.012. [DOI] [PubMed] [Google Scholar]
- 10.Shreffler JW, Pullan JE, Dailey KM, Mallik S, Brooks AE. Overcoming hurdles in nanoparticle clinical translation: the influence of experimental design and surface modification. Int J Mol Sci. 2019;20:6056. doi: 10.3390/ijms20236056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walsh G. Biopharmaceutical benchmarks 2018. Nat Biotechnol. 2018;36:1136–1145. doi: 10.1038/nbt.4305. [DOI] [PubMed] [Google Scholar]
- 12.DeLoach J, Barton C, Culler K. Preparation of resealed carrier erythrocytes and in vivo survival in dogs. Am J Vet Res. 1981;42:667–669. [PubMed] [Google Scholar]
- 13.Pang L, Zhang C, Qin J, Han L, Li R, Hong C, He H, Wang J. A novel strategy to achieve effective drug delivery: exploit cells as carrier combined with nanoparticles. Drug Deliv. 2017;24:83–91. doi: 10.1080/10717544.2016.1230903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang X, Rocker C, Hafner M, Brandholt S, Dorlich RM, Nienhaus GU. Endo-and exocytosis of zwitterionic quantum dot nanoparticles by live HeLa cells. ACS Nano. 2010;4:6787–6797. doi: 10.1021/nn101277w. [DOI] [PubMed] [Google Scholar]
- 15.Hu C-MJ, Zhang L, Aryal S, Cheung C, Fang RH, Zhang L. Erythrocyte membrane-camouflaged polymeric nanoparticles as a biomimetic delivery platform. Proc Nat Acad Sci. 2011;108:10980–10985. doi: 10.1073/pnas.1106634108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maeda H. The enhanced permeability and retention (EPR) effect in tumor vasculature: the key role of tumor-selective macromolecular drug targeting. Adv Enzyme Regul. 2001;41:189–207. doi: 10.1016/s0065-2571(00)00013-3. [DOI] [PubMed] [Google Scholar]
- 17.Sabu C, Rejo C, Kotta S, Pramod K. Bioinspired and biomimetic systems for advanced drug and gene delivery. J Contr Rel. 2018;287:142–155. doi: 10.1016/j.jconrel.2018.08.033. [DOI] [PubMed] [Google Scholar]
- 18.Rasheed T, Nabeel F, Raza A, Bilal M, Iqbal H. Biomimetic nanostructures/cues as drug delivery systems: a review. Mater Today Chem. 2019;13:147–157. [Google Scholar]
- 19.Shirley JL, de Jong YP, Terhorst C, Herzog RW. Immune responses to viral gene therapy vectors. Mol Ther. 2020;28:709–722. doi: 10.1016/j.ymthe.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Roemeling C, Jiang W, Chan CK, Weissman IL, Kim BY. Breaking down the barriers to precision cancer nanomedicine. Trends Biotechnol. 2017;35:159–171. doi: 10.1016/j.tibtech.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Gao M, Liang C, Song X, Chen Q, Jin Q, Wang C, Liu Z. Erythrocyte-membrane-enveloped perfluorocarbon as nanoscale artificial red blood cells to relieve tumor hypoxia and enhance cancer radiotherapy. Adv Mater. 2017;29:1701429. doi: 10.1002/adma.201701429. [DOI] [PubMed] [Google Scholar]
- 22.Cao H, Dan Z, He X, Zhang Z, Yu H, Yin Q, Li Y. Liposomes coated with isolated macrophage membrane can target lung metastasis of breast cancer. ACS Nano. 2016;10:7738–7748. doi: 10.1021/acsnano.6b03148. [DOI] [PubMed] [Google Scholar]
- 23.Orbach A, Zelig O, Yedgar S, Barshtein G. Biophysical and biochemical markers of red blood cell fragility. Transf Med Hemother. 2017;44:183–187. doi: 10.1159/000452106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu J-Y, Zheng D-W, Zhang M-K, Yu W-Y, Qiu W-X, Hu J-J, Feng J, Zhang X-Z. Preferential cancer cell self-recognition and tumor self-targeting by coating nanoparticles with homotypic cancer cell membranes. Nano Lett. 2016;16:5895–5901. doi: 10.1021/acs.nanolett.6b02786. [DOI] [PubMed] [Google Scholar]
- 25.Kang T, Zhu Q, Wei D, Feng J, Yao J, Jiang T, Song Q, Wei X, Chen H, Gao X. Nanoparticles coated with neutrophil membranes can effectively treat cancer metastasis. ACS Nano. 2017;11:1397–1411. doi: 10.1021/acsnano.6b06477. [DOI] [PubMed] [Google Scholar]
- 26.Spicer JD, McDonald B, Cools-Lartigue JJ, Chow SC, Giannias B, Kubes P, Ferri LE. Neutrophils promote liver metastasis via Mac-1-mediated interactions with circulating tumor cells. Can Res. 2012;72:3919–3927. doi: 10.1158/0008-5472.CAN-11-2393. [DOI] [PubMed] [Google Scholar]
- 27.Parodi A, Quattrocchi N, Van De Ven AL, Chiappini C, Evangelopoulos M, Martinez JO, Brown BS, Khaled SZ, Yazdi IK, Enzo MV. Synthetic nanoparticles functionalized with biomimetic leukocyte membranes possess cell-like functions. Nat Nanotechnol. 2013;8:61–68. doi: 10.1038/nnano.2012.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chugh V, Vijaya Krishna K, Pandit A. Cell membrane-coated mimics: a methodological approach for fabrication, characterization for therapeutic applications, and challenges for clinical translation. ACS Nano. 2021;15:17080–17123. doi: 10.1021/acsnano.1c03800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engelman DM. Membranes are more mosaic than fluid. Nature. 2005;438:578–580. doi: 10.1038/nature04394. [DOI] [PubMed] [Google Scholar]
- 30.Bucior I, Scheuring S, Engel A, Burger MM. Carbohydrate–carbohydrate interaction provides adhesion force and specificity for cellular recognition. J Cell Biol. 2004;165:529–537. doi: 10.1083/jcb.200309005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Simons K, Vaz WL. Model systems, lipid rafts, and cell membranes. Annu Rev Biophys Biomol Struct. 2004;33:269–295. doi: 10.1146/annurev.biophys.32.110601.141803. [DOI] [PubMed] [Google Scholar]
- 32.Casares D, Escribá PV, Rosselló CA. Membrane lipid composition: effect on membrane and organelle structure, function and compartmentalization and therapeutic avenues. Int J Mol Sci. 2019;20:2167. doi: 10.3390/ijms20092167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim J, Koo B-K, Knoblich JA. Human organoids: model systems for human biology and medicine. Nat Rev Mol Cell Biol. 2020;21:571–584. doi: 10.1038/s41580-020-0259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andrews RK, López J, Berndt MC. Molecular mechanisms of platelet adhesion and activation. Int J Biochem Cell Biol. 1997;29:91–105. doi: 10.1016/s1357-2725(96)00122-7. [DOI] [PubMed] [Google Scholar]
- 35.Si J, Shao S, Shen Y, Wang K. Macrophages as active nanocarriers for targeted early and adjuvant cancer chemotherapy. Small. 2016;12:5108–5119. doi: 10.1002/smll.201601282. [DOI] [PubMed] [Google Scholar]
- 36.Sökeland G, Schumacher U. The functional role of integrins during intra-and extravasation within the metastatic cascade. Mol Cancer. 2019;18:1–19. doi: 10.1186/s12943-018-0937-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bose RJ, Paulmurugan R, Moon J, Lee S-H, Park H. Cell membrane-coated nanocarriers: the emerging targeted delivery system for cancer theranostics. Drug Discov Today. 2018;23:891–899. doi: 10.1016/j.drudis.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 38.Evangelopoulos M, Parodi A, Martinez JO, Yazdi IK, Cevenini A, van de Ven AL, Quattrocchi N, Boada C, Taghipour N, Corbo C. Cell source determines the immunological impact of biomimetic nanoparticles. Biomaterials. 2016;82:168–177. doi: 10.1016/j.biomaterials.2015.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaneti L, Bronshtein T, Malkah Dayan N, Kovregina I, Letko Khait N, Lupu-Haber Y, Fliman M, Schoen BW, Kaneti G, Machluf M. Nanoghosts as a novel natural nonviral gene delivery platform safely targeting multiple cancers. Nano Lett. 2016;16:1574–1582. doi: 10.1021/acs.nanolett.5b04237. [DOI] [PubMed] [Google Scholar]
- 40.Stephan MT, Moon JJ, Um SH, Bershteyn A, Irvine DJ. Therapeutic cell engineering with surface-conjugated synthetic nanoparticles. Nat Med. 2010;16:1035–1041. doi: 10.1038/nm.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Deun J, Roux Q, Deville S, Van Acker T, Rappu P, Miinalainen I, Heino J, Vanhaecke F, De Geest BG, De Wever O. Feasibility of mechanical extrusion to coat nanoparticles with extracellular vesicle membranes. Cells. 2020;9:1797. doi: 10.3390/cells9081797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parrow NL, Violet P-C, Tu H, Nichols J, Pittman CA, Fitzhugh C, Fleming RE, Mohandas N, Tisdale JF, Levine M. Measuring deformability and red cell heterogeneity in blood by ektacytometry. J Vis Exp JoVE. 2018;2018:56910. doi: 10.3791/56910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuo Y-C, Wu H-C, Hoang D, Bentley WE, D’Souza WD, Raghavan SR. Colloidal properties of nanoerythrosomes derived from bovine red blood cells. Langmuir. 2016;32:171–179. doi: 10.1021/acs.langmuir.5b03014. [DOI] [PubMed] [Google Scholar]
- 44.Kim DS, Lee MW, Ko YJ, Jang IK, Jeon S, Na B, Chae JJ, Sung KW, Koo HH, Yoo KH. Effect of ex vivo culture density on CXCR7 expression in human mesenchymal stem cells. Int J Clin Exp Med. 2016;9:10802–10810. [Google Scholar]
- 45.Park JS, Suryaprakash S, Lao Y-H, Leong KW. Engineering mesenchymal stem cells for regenerative medicine and drug delivery. Methods. 2015;84:3–16. doi: 10.1016/j.ymeth.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muzykantov VR, Murciano JC, Taylor RP, Atochina EN, Herraez A. Regulation of the complement-mediated elimination of red blood cells modified with biotin and streptavidin. Anal Biochem. 1996;241:109–119. doi: 10.1006/abio.1996.0384. [DOI] [PubMed] [Google Scholar]
- 47.Wang Y, Zhang K, Qin X, Li T, Qiu J, Yin T, Huang J, McGinty S, Pontrelli G, Ren J. Biomimetic nanotherapies: red blood cell based core–shell structured nanocomplexes for atherosclerosis management. Adv Sci. 2019;6:1900172. doi: 10.1002/advs.201900172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hu C-MJ, Fang RH, Wang K-C, Luk BT, Thamphiwatana S, Dehaini D, Nguyen P, Angsantikul P, Wen CH, Kroll AV. Nanoparticle biointerfacing by platelet membrane cloaking. Nature. 2015;526:118–121. doi: 10.1038/nature15373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thamphiwatana S, Angsantikul P, Escajadillo T, Zhang Q, Olson J, Luk BT, Zhang S, Fang RH, Gao W, Nizet V. Macrophage-like nanoparticles concurrently absorbing endotoxins and proinflammatory cytokines for sepsis management. Proc Natl Acad Sci. 2017;114:11488–11493. doi: 10.1073/pnas.1714267114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deng G, Sun Z, Li S, Peng X, Li W, Zhou L, Ma Y, Gong P, Cai L. Cell-membrane immunotherapy based on natural killer cell membrane coated nanoparticles for the effective inhibition of primary and abscopal tumor growth. ACS Nano. 2018;12:12096–12108. doi: 10.1021/acsnano.8b05292. [DOI] [PubMed] [Google Scholar]
- 51.An X, Salomao M, Guo X, Gratzer W, Mohandas N. Tropomyosin modulates erythrocyte membrane stability. Blood. 2007;109:1284–1288. doi: 10.1182/blood-2006-07-036954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chakraborty S, Doktorova M, Molugu TR, Heberle FA, Scott HL, Dzikovski B, Nagao M, Stingaciu L-R, Standaert RF, Barrera FN. How cholesterol stiffens unsaturated lipid membranes. Proc Natl Acad Sci. 2020;117:21896–21905. doi: 10.1073/pnas.2004807117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Virlan MJR, Miricescu D, Radulescu R, Sabliov CM, Totan A, Calenic B, Greabu M. Organic nanomaterials and their applications in the treatment of oral diseases. Molecules. 2016;21:207. doi: 10.3390/molecules21020207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anselmo AC, Mitragotri S. A review of clinical translation of inorganic nanoparticles. AAPS J. 2015;17:1041–1054. doi: 10.1208/s12248-015-9780-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ehlerding EB, Chen F, Cai W. Biodegradable and renal clearable inorganic nanoparticles. Adv Sci. 2016;3:1500223. doi: 10.1002/advs.201500223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Su S, Kang PM. Systemic review of biodegradable nanomaterials in nanomedicine. Nanomaterials. 2020;10:656. doi: 10.3390/nano10040656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ye H, Wang K, Wang M, Liu R, Song H, Li N, Lu Q, Zhang W, Du Y, Yang W. Bioinspired nanoplatelets for chemo-photothermal therapy of breast cancer metastasis inhibition. Biomaterials. 2019;206:1–12. doi: 10.1016/j.biomaterials.2019.03.024. [DOI] [PubMed] [Google Scholar]
- 58.Xu C, Liu W, Hu Y, Li W, Di W. Bioinspired tumor-homing nanoplatform for co-delivery of paclitaxel and siRNA-E7 to HPV-related cervical malignancies for synergistic therapy. Theranostics. 2020;10:3325. doi: 10.7150/thno.41228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Q, Dehaini D, Zhang Y, Zhou J, Chen X, Zhang L, Fang RH, Gao W, Zhang L. Neutrophil membrane-coated nanoparticles inhibit synovial inflammation and alleviate joint damage in inflammatory arthritis. Nat Nanotechnol. 2018;13:1182–1190. doi: 10.1038/s41565-018-0254-4. [DOI] [PubMed] [Google Scholar]
- 60.Tang J, Shen D, Caranasos TG, Wang Z, Vandergriff AC, Allen TA, Hensley MT, Dinh P-U, Cores J, Li T-S. Therapeutic microparticles functionalized with biomimetic cardiac stem cell membranes and secretome. Nat Commun. 2017;8:1–9. doi: 10.1038/ncomms13724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li L-L, Xu J-H, Qi G-B, Zhao X, Yu F, Wang H. Core–shell supramolecular gelatin nanoparticles for adaptive and “on-demand” antibiotic delivery. ACS Nano. 2014;8:4975–4983. doi: 10.1021/nn501040h. [DOI] [PubMed] [Google Scholar]
- 62.Gao C, Lin Z, Jurado-Sánchez B, Lin X, Wu Z, He Q. Stem cell membrane-coated nanogels for highly efficient in vivo tumor targeted drug delivery. Small. 2016;12:4056–4062. doi: 10.1002/smll.201600624. [DOI] [PubMed] [Google Scholar]
- 63.Zhai Y, Ran W, Su J, Lang T, Meng J, Wang G, Zhang P, Li Y. Traceable bioinspired nanoparticle for the treatment of metastatic breast cancer via NIR-trigged intracellular delivery of methylene blue and cisplatin. Adv Mater. 2018;30:1802378. doi: 10.1002/adma.201802378. [DOI] [PubMed] [Google Scholar]
- 64.Rao L, Wang W, Meng Q-F, Tian M, Cai B, Wang Y, Li A, Zan M, Xiao F, Bu L-L. A biomimetic nanodecoy traps Zika virus to prevent viral infection and fetal microcephaly development. Nano Lett. 2018;19:2215–2222. doi: 10.1021/acs.nanolett.8b03913. [DOI] [PubMed] [Google Scholar]
- 65.Xie J, Shen Q, Huang K, Zheng T, Cheng L, Zhang Z, Yu Y, Liao G, Wang X, Li C. Oriented assembly of cell-mimicking nanoparticles via a molecular affinity strategy for targeted drug delivery. ACS Nano. 2019;13:5268–5277. doi: 10.1021/acsnano.8b09681. [DOI] [PubMed] [Google Scholar]
- 66.Nie D, Dai Z, Li J, Yang Y, Xi Z, Wang J, Zhang W, Qian K, Guo S, Zhu C. Cancer-cell-membrane-coated nanoparticles with a yolk–shell structure augment cancer chemotherapy. Nano Lett. 2019;20:936–946. doi: 10.1021/acs.nanolett.9b03817. [DOI] [PubMed] [Google Scholar]
- 67.Castro CI, Briceno JC. Perfluorocarbon-based oxygen carriers: review of products and trials. Artif Organs. 2010;34:622–634. doi: 10.1111/j.1525-1594.2009.00944.x. [DOI] [PubMed] [Google Scholar]
- 68.Zou MZ, Liu WL, Gao F, Bai XF, Chen HS, Zeng X, Zhang XZ. Artificial natural killer cells for specific tumor inhibition and renegade macrophage re-education. Adv Mater. 2019;31:1904495. doi: 10.1002/adma.201904495. [DOI] [PubMed] [Google Scholar]
- 69.Watermann A, Brieger J. Mesoporous silica nanoparticles as drug delivery vehicles in cancer. Nanomaterials. 2017;7:189. doi: 10.3390/nano7070189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jafari S, Derakhshankhah H, Alaei L, Fattahi A, Varnamkhasti BS, Saboury AA. Mesoporous silica nanoparticles for therapeutic/diagnostic applications. Biomed Pharmacother. 2019;109:1100–1111. doi: 10.1016/j.biopha.2018.10.167. [DOI] [PubMed] [Google Scholar]
- 71.Xuan M, Shao J, Zhao J, Li Q, Dai L, Li J. Cover picture: magnetic mesoporous silica nanoparticles cloaked by red blood cell membranes: applications in cancer therapy. Angew Chem Int Ed. 2018;57:5955–5955. doi: 10.1002/anie.201712996. [DOI] [PubMed] [Google Scholar]
- 72.Cai D, Liu L, Han C, Ma X, Qian J, Zhou J, Zhu W. Cancer cell membrane-coated mesoporous silica loaded with superparamagnetic ferroferric oxide and Paclitaxel for the combination of Chemo/Magnetocaloric therapy on MDA-MB-231 cells. Sci Rep. 2019;9:1–10. doi: 10.1038/s41598-019-51029-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hao N, Yang H, Li L, Li L, Tang F. The shape effect of mesoporous silica nanoparticles on intracellular reactive oxygen species in A375 cells. New J Chem. 2014;38:4258–4266. [Google Scholar]
- 74.Hu C-MJ, Fang RH, Copp J, Luk BT, Zhang L. A biomimetic nanosponge that absorbs pore-forming toxins. Nat Nanotechnol. 2013;8:336–340. doi: 10.1038/nnano.2013.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li J, Ai Y, Wang L, Bu P, Sharkey CC, Wu Q, Wun B, Roy S, Shen X, King MR. Targeted drug delivery to circulating tumor cells via platelet membrane-functionalized particles. Biomaterials. 2016;76:52–65. doi: 10.1016/j.biomaterials.2015.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Meng Q-F, Rao L, Zan M, Chen M, Yu G-T, Wei X, Wu Z, Sun Y, Guo S-S, Zhao X-Z. Macrophage membrane-coated iron oxide nanoparticles for enhanced photothermal tumor therapy. Nanotechnology. 2018;29:134004. doi: 10.1088/1361-6528/aaa7c7. [DOI] [PubMed] [Google Scholar]
- 77.Lai P-Y, Huang R-Y, Lin S-Y, Lin Y-H, Chang C-W. Biomimetic stem cell membrane-camouflaged iron oxide nanoparticles for theranostic applications. RSC Adv. 2015;5:98222–98230. [Google Scholar]
- 78.Zhu J, Zhang M, Zheng D, Hong S, Feng J, Zhang X-Z. A universal approach to render nanomedicine with biological identity derived from cell membranes. Biomacromol. 2018;19:2043–2052. doi: 10.1021/acs.biomac.8b00242. [DOI] [PubMed] [Google Scholar]
- 79.Cook TR, Zheng Y-R, Stang PJ. Metal–organic frameworks and self-assembled supramolecular coordination complexes: comparing and contrasting the design, synthesis, and functionality of metal–organic materials. Chem Rev. 2013;113:734–777. doi: 10.1021/cr3002824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hoop M, Walde CF, Riccò R, Mushtaq F, Terzopoulou A, Chen X-Z, deMello AJ, Doonan CJ, Falcaro P, Nelson BJ. Biocompatibility characteristics of the metal organic framework ZIF-8 for therapeutical applications. Appl Mater Today. 2018;11:13–21. [Google Scholar]
- 81.Huang J, Shen H, Wu J, Hu X, Zhu Z, Lv X, Liu Y, Wang Y. Spine Explorer: a deep learning based fully automated program for efficient and reliable quantifications of the vertebrae and discs on sagittal lumbar spine MR images. Spine J. 2020;20:590–599. doi: 10.1016/j.spinee.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 82.Carnovale C, Bryant G, Shukla R, Bansal V. Identifying trends in gold nanoparticle toxicity and uptake: size, shape, capping ligand, and biological corona. ACS Omega. 2019;4:242–256. [Google Scholar]
- 83.Fang RH, Kroll AV, Gao W, Zhang L. Cell membrane coating nanotechnology. Adv Mater. 2018;30:1706759. doi: 10.1002/adma.201706759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang X, He S, Ding B, Qu C, Zhang Q, Chen H, Sun Y, Fang H, Long Y, Zhang R. Cancer cell membrane-coated rare earth doped nanoparticles for tumor surgery navigation in NIR-II imaging window. Chem Eng J. 2020;385:123959. [Google Scholar]
- 85.Ma W, Zhu D, Li J, Chen X, Xie W, Jiang X, Wu L, Wang G, Xiao Y, Liu Z. Coating biomimetic nanoparticles with chimeric antigen receptor T cell-membrane provides high specificity for hepatocellular carcinoma photothermal therapy treatment. Theranostics. 2020;10:1281. doi: 10.7150/thno.40291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mishra P, Jain N. Folate conjugated doxorubicin-loaded membrane vesicles for improved cancer therapy. Drug Deliv. 2003;10:277–282. doi: 10.1080/drd_10_4_277. [DOI] [PubMed] [Google Scholar]
- 87.Xuan M, Shao J, Dai L, Li J, He Q. Macrophage cell membrane camouflaged Au nanoshells for in vivo prolonged circulation life and enhanced cancer photothermal therapy. ACS Appl Mater Interfaces. 2016;8:9610–9618. doi: 10.1021/acsami.6b00853. [DOI] [PubMed] [Google Scholar]
- 88.Michael M, Vermeren S. A neutrophil-centric view of chemotaxis. Essays Biochem. 2019;63:607–618. doi: 10.1042/EBC20190011. [DOI] [PubMed] [Google Scholar]
- 89.Sekeres J, Zarsky V. Concepts in cell biology-history and evolution. Berlin: Springer; 2018. 180 years of the cell: from Matthias Jakob Schleiden to the cell biology of the twenty-first century; pp. 7–37. [Google Scholar]
- 90.Goñi FM. The basic structure and dynamics of cell membranes: An update of the Singer-Nicolson model. Biochim Biophys Acta (BBA) Biomembr. 2014;1838:1467–1476. doi: 10.1016/j.bbamem.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 91.Shi Y, Xie F, Rao P, Qian H, Chen R, Chen H, Li D, Mu D, Zhang L, Lv P. TRAIL-expressing cell membrane nanovesicles as an anti-inflammatory platform for rheumatoid arthritis therapy. J Contr Rel. 2020;320:304–313. doi: 10.1016/j.jconrel.2020.01.054. [DOI] [PubMed] [Google Scholar]
- 92.Han Y, Pan H, Li W, Chen Z, Ma A, Yin T, Liang R, Chen F, Ma Y, Jin Y. T cell membrane mimicking nanoparticles with bioorthogonal targeting and immune recognition for enhanced photothermal therapy. Adv Sci. 2019;6:1900251. doi: 10.1002/advs.201900251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lv P, Liu X, Chen X, Liu C, Zhang Y, Chu C, Wang J, Wang X, Chen X, Liu G. Genetically engineered cell membrane nanovesicles for oncolytic adenovirus delivery: a versatile platform for cancer virotherapy. Nano Lett. 2019;19:2993–3001. doi: 10.1021/acs.nanolett.9b00145. [DOI] [PubMed] [Google Scholar]
- 94.Zhang X, Angsantikul P, Ying M, Zhuang J, Zhang Q, Wei X, Jiang Y, Zhang Y, Dehaini D, Chen M. Remote loading of small-molecule therapeutics into cholesterol-enriched cell-membrane-derived vesicles. Angew Chem Int Ed. 2017;56:14075–14079. doi: 10.1002/anie.201707598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Peng L-H, Zhang Y-H, Han L-J, Zhang C-Z, Wu J-H, Wang X-R, Gao J-Q, Mao Z-W. Cell membrane capsules for encapsulation of chemotherapeutic and cancer cell targeting in vivo. ACS Appl Mater Interfaces. 2015;7:18628–18637. doi: 10.1021/acsami.5b05065. [DOI] [PubMed] [Google Scholar]
- 96.Zhou H, Fan Z, Lemons PK, Cheng H. A facile approach to functionalize cell membrane-coated nanoparticles. Theranostics. 2016;6:1012. doi: 10.7150/thno.15095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chai Z, Ran D, Lu L, Zhan C, Ruan H, Hu X, Xie C, Jiang K, Li J, Zhou J. Ligand-modified cell membrane enables the targeted delivery of drug nanocrystals to glioma. ACS Nano. 2019;13:5591–5601. doi: 10.1021/acsnano.9b00661. [DOI] [PubMed] [Google Scholar]
- 98.Kaddah S, Khreich N, Kaddah F, Charcosset C, Greige-Gerges H. Cholesterol modulates the liposome membrane fluidity and permeability for a hydrophilic molecule. Food Chem Toxicol. 2018;113:40–48. doi: 10.1016/j.fct.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 99.Chen Z, Zhao P, Luo Z, Zheng M, Tian H, Gong P, Gao G, Pan H, Liu L, Ma A. Cancer cell membrane–biomimetic nanoparticles for homologous-targeting dual-modal imaging and photothermal therapy. ACS Nano. 2016;10:10049–10057. doi: 10.1021/acsnano.6b04695. [DOI] [PubMed] [Google Scholar]
- 100.Song Y, Huang Z, Liu X, Pang Z, Chen J, Yang H, Zhang N, Cao Z, Liu M, Cao J. Platelet membrane-coated nanoparticle-mediated targeting delivery of Rapamycin blocks atherosclerotic plaque development and stabilizes plaque in apolipoprotein E-deficient (ApoE−/−) mice. Nanomed Nanotechnol Biol Med. 2019;15:13–24. doi: 10.1016/j.nano.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 101.Chen H-Y, Deng J, Wang Y, Wu C-Q, Li X, Dai H-W. Hybrid cell membrane-coated nanoparticles: a multifunctional biomimetic platform for cancer diagnosis and therapy. Acta Biomater. 2020;112:1–13. doi: 10.1016/j.actbio.2020.05.028. [DOI] [PubMed] [Google Scholar]
- 102.Liang X, Ye X, Wang C, Xing C, Miao Q, Xie Z, Chen X, Zhang X, Zhang H, Mei L. Photothermal cancer immunotherapy by erythrocyte membrane-coated black phosphorus formulation. J Contr Rel. 2019;296:150–161. doi: 10.1016/j.jconrel.2019.01.027. [DOI] [PubMed] [Google Scholar]
- 103.Dehaini D, Wei X, Fang RH, Masson S, Angsantikul P, Luk BT, Zhang Y, Ying M, Jiang Y, Kroll AV. Erythrocyte–platelet hybrid membrane coating for enhanced nanoparticle functionalization. Adv Mater. 2017;29:1606209. doi: 10.1002/adma.201606209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.St John AE, Newton JC, Martin EJ, Mohammed BM, Contaifer D, Jr, Saunders JL, Brophy GM, Spiess BD, Ward KR, Brophy DF. Platelets retain inducible alpha granule secretion by P-selectin expression but exhibit mechanical dysfunction during trauma-induced coagulopathy. J Thromb Haemost. 2019;17:771–781. doi: 10.1111/jth.14414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sun D, Chen J, Wang Y, Ji H, Peng R, Jin L, Wu W. Advances in refunctionalization of erythrocyte-based nanomedicine for enhancing cancer-targeted drug delivery. Theranostics. 2019;9:6885. doi: 10.7150/thno.36510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pitchaimani A, Nguyen TDT, Aryal S. Natural killer cell membrane infused biomimetic liposomes for targeted tumor therapy. Biomaterials. 2018;160:124–137. doi: 10.1016/j.biomaterials.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 107.Minasyan H. Phagocytosis and oxycytosis: two arms of human innate immunity. Immunol Res. 2018;66:271–280. doi: 10.1007/s12026-018-8988-5. [DOI] [PubMed] [Google Scholar]
- 108.Wang H, Sun Y, Zhou X, Chen C, Jiao L, Li W, Gou S, Li Y, Du J, Chen G, et al. CD47/SIRPα blocking peptide identification and synergistic effect with irradiation for cancer immunotherapy. J Immunother Cancer. 2020;8:e000905. doi: 10.1136/jitc-2020-000905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cao Z, Cheng S, Wang X, Pang Y, Liu J. Camouflaging bacteria by wrapping with cell membranes. Nat Commun. 2019;10:1–10. doi: 10.1038/s41467-019-11390-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liu J-M, Zhang D-D, Fang G-Z, Wang S. Erythrocyte membrane bioinspired near-infrared persistent luminescence nanocarriers for in vivo long-circulating bioimaging and drug delivery. Biomaterials. 2018;165:39–47. doi: 10.1016/j.biomaterials.2018.02.042. [DOI] [PubMed] [Google Scholar]
- 111.Ren X, Zheng R, Fang X, Wang X, Zhang X, Yang W, Sha X. Red blood cell membrane camouflaged magnetic nanoclusters for imaging-guided photothermal therapy. Biomaterials. 2016;92:13–24. doi: 10.1016/j.biomaterials.2016.03.026. [DOI] [PubMed] [Google Scholar]
- 112.Rao L, Meng Q-F, Bu L-L, Cai B, Huang Q, Sun Z-J, Zhang W-F, Li A, Guo S-S, Liu W. Erythrocyte membrane-coated upconversion nanoparticles with minimal protein adsorption for enhanced tumor imaging. ACS Appl Mater Interfaces. 2017;9:2159–2168. doi: 10.1021/acsami.6b14450. [DOI] [PubMed] [Google Scholar]
- 113.Su J, Sun H, Meng Q, Yin Q, Tang S, Zhang P, Chen Y, Zhang Z, Yu H, Li Y. Long circulation red-blood-cell-mimetic nanoparticles with peptide-enhanced tumor penetration for simultaneously inhibiting growth and lung metastasis of breast cancer. Adv Func Mater. 2016;26:1243–1252. [Google Scholar]
- 114.Fu S, Liang M, Wang Y, Cui L, Gao C, Chu X, Liu Q, Feng Y, Gong W, Yang M. Dual-modified novel biomimetic nanocarriers improve targeting and therapeutic efficacy in glioma. ACS Appl Mater Interfaces. 2018;11:1841–1854. doi: 10.1021/acsami.8b18664. [DOI] [PubMed] [Google Scholar]
- 115.Chai Z, Hu X, Wei X, Zhan C, Lu L, Jiang K, Su B, Ruan H, Ran D, Fang RH. A facile approach to functionalizing cell membrane-coated nanoparticles with neurotoxin-derived peptide for brain-targeted drug delivery. J Contr Rel. 2017;264:102–111. doi: 10.1016/j.jconrel.2017.08.027. [DOI] [PubMed] [Google Scholar]
- 116.Jiang Q, Luo Z, Men Y, Yang P, Peng H, Guo R, Tian Y, Pang Z, Yang W. Red blood cell membrane-camouflaged melanin nanoparticles for enhanced photothermal therapy. Biomaterials. 2017;143:29–45. doi: 10.1016/j.biomaterials.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 117.Chen W, Zeng K, Liu H, Ouyang J, Wang L, Liu Y, Wang H, Deng L, Liu YN. Cell membrane camouflaged hollow prussian blue nanoparticles for synergistic photothermal-/chemotherapy of cancer. Adv Func Mater. 2017;27:1605795. [Google Scholar]
- 118.Li B, Wang F, Gui L, He Q, Yao Y, Chen H. The potential of biomimetic nanoparticles for tumor-targeted drug delivery. Nanomedicine. 2018;13:2099–2118. doi: 10.2217/nnm-2018-0017. [DOI] [PubMed] [Google Scholar]
- 119.Rosales C. Neutrophil: a cell with many roles in inflammation or several cell types? Front Physiol. 2018;9:113. doi: 10.3389/fphys.2018.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Morikis VA, Simon SI. Neutrophil mechanosignaling promotes integrin engagement with endothelial cells and motility within inflamed vessels. Front Immunol. 2018;9:2774. doi: 10.3389/fimmu.2018.02774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.He Z, Zhang Y, Feng N. Cell membrane-coated nanosized active targeted drug delivery systems homing to tumor cells: a review. Mater Sci Eng C. 2020;106:110298. doi: 10.1016/j.msec.2019.110298. [DOI] [PubMed] [Google Scholar]
- 122.Xue J, Zhao Z, Zhang L, Xue L, Shen S, Wen Y, Wei Z, Wang L, Kong L, Sun H. Neutrophil-mediated anticancer drug delivery for suppression of postoperative malignant glioma recurrence. Nat Nanotechnol. 2017;12:692–700. doi: 10.1038/nnano.2017.54. [DOI] [PubMed] [Google Scholar]
- 123.Cao X, Hu Y, Luo S, Wang Y, Gong T, Sun X, Fu Y, Zhang Z. Neutrophil-mimicking therapeutic nanoparticles for targeted chemotherapy of pancreatic carcinoma. Acta Pharmaceut Sin B. 2019;9:575–589. doi: 10.1016/j.apsb.2018.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Combes F, Meyer E, Sanders NN. Immune cells as tumor drug delivery vehicles. J Control Rel. 2020;327:70–87. doi: 10.1016/j.jconrel.2020.07.043. [DOI] [PubMed] [Google Scholar]
- 125.Wu M, Le W, Mei T, Wang Y, Chen B, Liu Z, Xue C. Cell membrane camouflaged nanoparticles: a new biomimetic platform for cancer photothermal therapy. Int J Nanomed. 2019;14:4431. doi: 10.2147/IJN.S200284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233:6425–6440. doi: 10.1002/jcp.26429. [DOI] [PubMed] [Google Scholar]
- 127.Najafi M, Hashemi Goradel N, Farhood B, Salehi E, Nashtaei MS, Khanlarkhani N, Khezri Z, Majidpoor J, Abouzaripour M, Habibi M. Macrophage polarity in cancer: a review. J Cell Biochem. 2019;120:2756–2765. doi: 10.1002/jcb.27646. [DOI] [PubMed] [Google Scholar]
- 128.Hu C, Lei T, Wang Y, Cao J, Yang X, Qin L, Liu R, Zhou Y, Tong F, Umeshappa CS. Phagocyte-membrane-coated and laser-responsive nanoparticles control primary and metastatic cancer by inducing anti-tumor immunity. Biomaterials. 2020;255:120159. doi: 10.1016/j.biomaterials.2020.120159. [DOI] [PubMed] [Google Scholar]
- 129.Gay LJ, Felding-Habermann B. Contribution of platelets to tumour metastasis. Nat Rev Cancer. 2011;11:123–134. doi: 10.1038/nrc3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.De Witt SM, Swieringa F, Cavill R, Lamers MM, Van Kruchten R, Mastenbroek T, Baaten C, Coort S, Pugh N, Schulz A. Identification of platelet function defects by multi-parameter assessment of thrombus formation. Nat Commun. 2014;5:1–13. doi: 10.1038/ncomms5257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nelson VS, Jolink A-TC, Amini SN, Zwaginga JJ, Netelenbos T, Semple JW, Porcelijn L, de Haas M, Schipperus MR, Kapur R. Platelets in ITP: victims in charge of their own fate? Cells. 2021;10:3235. doi: 10.3390/cells10113235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chen S, Lv M, Fang S, Ye W, Gao Y, Xu Y. Poly (I: C) enhanced anti-cervical cancer immunities induced by dendritic cells-derived exosomes. Int J Biol Macromol. 2018;113:1182–1187. doi: 10.1016/j.ijbiomac.2018.02.034. [DOI] [PubMed] [Google Scholar]
- 133.Shang Y, Wang Q, Wu B, Zhao Q, Li J, Huang X, Chen W, Gui R. Platelet-membrane-camouflaged black phosphorus quantum dots enhance anticancer effect mediated by apoptosis and autophagy. ACS Appl Mater Interfaces. 2019;11:28254–28266. doi: 10.1021/acsami.9b04735. [DOI] [PubMed] [Google Scholar]
- 134.Wu H, Mu X, Liu L, Wu H, Hu X, Chen L, Liu J, Mu Y, Yuan F, Liu W. Bone marrow mesenchymal stem cells-derived exosomal microRNA-193a reduces cisplatin resistance of non-small cell lung cancer cells via targeting LRRC1. Cell Death Dis. 2020;11:1–14. doi: 10.1038/s41419-020-02962-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nath S, Mukherjee P. MUC1: a multifaceted oncoprotein with a key role in cancer progression. Trends Mol Med. 2014;20:332–342. doi: 10.1016/j.molmed.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gordon-Alonso M, Hirsch T, Wildmann C, van der Bruggen P. Galectin-3 captures interferon-gamma in the tumor matrix reducing chemokine gradient production and T-cell tumor infiltration. Nat Commun. 2017;8:1–15. doi: 10.1038/s41467-017-00925-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 138.Zhang J, Miao Y, Ni W, Xiao H, Zhang J. Cancer cell membrane coated silica nanoparticles loaded with ICG for tumour specific photothermal therapy of osteosarcoma. Artif Cells Nanomed Biotechnol. 2019;47:2298–2305. doi: 10.1080/21691401.2019.1622554. [DOI] [PubMed] [Google Scholar]
- 139.Rao L, Yu GT, Meng QF, Bu LL, Tian R, Lin LS, Deng H, Yang W, Zan M, Ding J. Cancer cell membrane-coated nanoparticles for personalized therapy in patient-derived xenograft models. Adv Func Mater. 2019;29:1905671. [Google Scholar]
- 140.Jin J, Krishnamachary B, Barnett JD, Chatterjee S, Chang D, Mironchik Y, Wildes F, Jaffee EM, Nimmagadda S, Bhujwalla ZM. Human cancer cell membrane-coated biomimetic nanoparticles reduce fibroblast-mediated invasion and metastasis and induce T-cells. ACS Appl Mater Interfaces. 2019;11:7850–7861. doi: 10.1021/acsami.8b22309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wang C, Wu B, Wu Y, Song X, Zhang S, Liu Z. Camouflaging nanoparticles with brain metastatic tumor cell membranes: a new strategy to traverse blood–brain barrier for imaging and therapy of brain tumors. Adv Func Mater. 2020;30:1909369. [Google Scholar]
- 142.Kumar P, Van Treuren T, Ranjan AP, Chaudhary P, Vishwanatha JK. In vivo imaging and biodistribution of near infrared dye loaded brain-metastatic-breast-cancer-cell-membrane coated polymeric nanoparticles. Nanotechnology. 2019;30:265101. doi: 10.1088/1361-6528/ab0f46. [DOI] [PubMed] [Google Scholar]
- 143.Ribas A. Adaptive immune resistance: how cancer protects from immune attack. Cancer Discov. 2015;5:915–919. doi: 10.1158/2159-8290.CD-15-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zhang L, Li R, Chen H, Wei J, Qian H, Su S, Shao J, Wang L, Qian X, Liu B. Human cytotoxic T-lymphocyte membrane-camouflaged nanoparticles combined with low-dose irradiation: a new approach to enhance drug targeting in gastric cancer. Int J Nanomed. 2017;12:2129. doi: 10.2147/IJN.S126016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Um W, Ko H, You DG, Lim S, Kwak G, Shim MK, Yang S, Lee J, Song Y, Kim K, Park JH. Necroptosis-inducible polymeric nanobubbles for enhanced cancer sonoimmunotherapy. Adv Mater. 2020;32:1907953. doi: 10.1002/adma.201907953. [DOI] [PubMed] [Google Scholar]
- 146.Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39:1–10. doi: 10.1016/j.immuni.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 147.Palmer DH, Midgley RS, Mirza N, Torr EE, Ahmed F, Steele JC, Steven NM, Kerr DJ, Young LS, Adams DH. A phase II study of adoptive immunotherapy using dendritic cells pulsed with tumor lysate in patients with hepatocellular carcinoma. Hepatology. 2009;49:124–132. doi: 10.1002/hep.22626. [DOI] [PubMed] [Google Scholar]
- 148.Zhang B, Yin Y, Lai RC, Lim SK. Immunotherapeutic potential of extracellular vesicles. Front Immunol. 2014;5:518. doi: 10.3389/fimmu.2014.00518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Mbongue JC, Nieves HA, Torrez TW, Langridge WH. The role of dendritic cell maturation in the induction of insulin-dependent diabetes mellitus. Front Immunol. 2017;8:327. doi: 10.3389/fimmu.2017.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Gardner A, Ruffell B. Dendritic cells and cancer immunity. Trends Immunol. 2016;37:855–865. doi: 10.1016/j.it.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cheng S, Xu C, Jin Y, Li Y, Zhong C, Ma J, Yang J, Zhang N, Li Y, Wang C. Artificial mini dendritic cells boost T cell-based immunotherapy for ovarian cancer. Adv Sci. 2020;7:1903301. doi: 10.1002/advs.201903301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhang C, Zhang J, Shi G, Song H, Shi S, Zhang X, Huang P, Wang Z, Wang W, Wang C. A light responsive nanoparticle-based delivery system using pheophorbide a graft polyethylenimine for dendritic cell-based cancer immunotherapy. Mol Pharm. 2017;14:1760–1770. doi: 10.1021/acs.molpharmaceut.7b00015. [DOI] [PubMed] [Google Scholar]
- 153.Fang RH, Jiang Y, Fang JC, Zhang L. Cell membrane-derived nanomaterials for biomedical applications. Biomaterials. 2017;128:69–83. doi: 10.1016/j.biomaterials.2017.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sun Q, Wu J, Jin L, Hong L, Wang F, Mao Z, Wu M. Cancer cell membrane-coated gold nanorods for photothermal therapy and radiotherapy on oral squamous cancer. J Mater Chem B. 2020;8:7253–7263. doi: 10.1039/d0tb01063d. [DOI] [PubMed] [Google Scholar]
- 155.Rao L, Bu LL, Meng QF, Cai B, Deng WW, Li A, Li K, Guo SS, Zhang WF, Liu W. Antitumor platelet-mimicking magnetic nanoparticles. Adv Func Mater. 2017;27:1604774. [Google Scholar]
- 156.Wu H-H, Zhou Y, Tabata Y, Gao J-Q. Mesenchymal stem cell-based drug delivery strategy: from cells to biomimetic. J Contr Rel. 2019;294:102–113. doi: 10.1016/j.jconrel.2018.12.019. [DOI] [PubMed] [Google Scholar]
- 157.He H, Guo C, Wang J, Korzun WJ, Wang X-Y, Ghosh S, Yang H. Leutusome: a biomimetic nanoplatform integrating plasma membrane components of leukocytes and tumor cells for remarkably enhanced solid tumor homing. Nano Lett. 2018;18:6164–6174. doi: 10.1021/acs.nanolett.8b01892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Sun M, Duan Y, Ma Y, Zhang Q. Cancer cell-erythrocyte hybrid membrane coated gold nanocages for near infrared light-activated photothermal/radio/chemotherapy of breast cancer. Int J Nanomed. 2020;15:6749. doi: 10.2147/IJN.S266405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gong C, Yu X, You B, Wu Y, Wang R, Han L, Wang Y, Gao S, Yuan Y. Macrophage-cancer hybrid membrane-coated nanoparticles for targeting lung metastasis in breast cancer therapy. J Nanobiotechnol. 2020;18:1–17. doi: 10.1186/s12951-020-00649-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Li M, Xu Z, Zhang L, Cui M, Zhu M, Guo Y, Sun R, Han J, Song E, He Y, Su Y. Targeted noninvasive treatment of choroidal neovascularization by hybrid cell-membrane-cloaked biomimetic nanoparticles. ACS Nano. 2021;15:9808–9819. doi: 10.1021/acsnano.1c00680. [DOI] [PubMed] [Google Scholar]
- 161.Giampietro C, Taddei A, Corada M, Sarra-Ferraris GM, Alcalay M, Cavallaro U, Orsenigo F, Lampugnani MG, Dejana E. Overlapping and divergent signaling pathways of N-cadherin and VE-cadherin in endothelial cells. Blood J Am Soc Hematol. 2012;119:2159–2170. doi: 10.1182/blood-2011-09-381012. [DOI] [PubMed] [Google Scholar]
- 162.Pisano S, Pierini I, Gu J, Gazze A, Francis LW, Gonzalez D, Conlan RS, Corradetti B. Immune (Cell) derived exosome mimetics (IDEM) as a treatment for ovarian cancer. Front Cell Dev Biol. 2020;8:553576. doi: 10.3389/fcell.2020.553576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Susa F, Limongi T, Dumontel B, Vighetto V, Cauda V. Engineered extracellular vesicles as a reliable tool in cancer nanomedicine. Cancers. 1979;2019:11. doi: 10.3390/cancers11121979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Jin K, Luo Z, Zhang B, Pang Z. Biomimetic nanoparticles for inflammation targeting. Acta Pharmaceut Sin B. 2018;8:23–33. doi: 10.1016/j.apsb.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Xia Y, Rao L, Yao H, Wang Z, Ning P, Chen X. Engineering macrophages for cancer immunotherapy and drug delivery. Adv Mater. 2020;32:2002054. doi: 10.1002/adma.202002054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.