Abstract
Background
Robotics represents the most technologically advanced approach in minimally invasive surgery (MIS). Its application in general surgery has increased progressively, with some early experience reported in emergency settings. The present position paper, supported by the World Society of Emergency Surgery (WSES), aims to provide a systematic review of the literature to develop consensus statements about the potential use of robotics in emergency general surgery.
Methods
This position paper was conducted according to the WSES methodology. A steering committee was constituted to draft the position paper according to the literature review. An international expert panel then critically revised the manuscript. Each statement was voted through a web survey to reach a consensus.
Results
Ten studies (3 case reports, 3 case series, and 4 retrospective comparative cohort studies) have been published regarding the applications of robotics for emergency general surgery procedures. Due to the paucity and overall low quality of evidence, 6 statements are proposed as expert opinions. In general, the experts claim for a strict patient selection while approaching emergent general surgery procedures with robotics, eventually considering it for hemodynamically stable patients only. An emergency setting should not be seen as an absolute contraindication for robotic surgery if an adequate training of the operating surgical team is available. In such conditions, robotic surgery can be considered safe, feasible, and associated with surgical outcomes related to an MIS approach. However, there are some concerns regarding the adoption of robotic surgery for emergency surgeries associated with the following: (i) the availability and accessibility of the robotic platform for emergency units and during night shifts, (ii) expected longer operative times, and (iii) increased costs. Further research is necessary to investigate the role of robotic surgery in emergency settings and to explore the possibility of performing telementoring and telesurgery, which are particularly valuable in emergency situations.
Conclusions
Many hospitals are currently equipped with a robotic surgical platform which needs to be implemented efficiently. The role of robotic surgery for emergency procedures remains under investigation. However, its use is expanding with a careful assessment of costs and timeliness of operations. The proposed statements should be seen as a preliminary guide for the surgical community stressing the need for reevaluation and update processes as evidence expands in the relevant literature.
Keywords: Emergency surgery, Robotic surgery, General surgery, Minimally invasive surgery
Background
Robotics represents the most technologically advanced approach in minimally invasive surgery (MIS). Its application has progressively gained acceptance in several surgical fields, being routinely used for elective urology, gynecology, digestive, and hepato-bilio-pancreatic surgery [1–8]. Conversely, robotic surgery in the emergency setting has not been explored, although some early experience has been reported in the literature [9–12]. Consequently, the issue regarding the role and potential applications of robotics for emergency procedures remains open. However, it deserves to be continuously monitored and updated in the future as evidence would emerge.
Project rationale and design
The present position paper is supported by the World Society of Emergency Surgery (WSES) and aims to provide a systematic review of the literature investigating the use of robotics in emergency general surgery to develop consensus statements based on the currently available evidence and practice. The present document should be seen as a preliminary guide for the surgical community stressing the need for reevaluation and update processes as evidence expands in the relevant literature.
For the purpose of this WSES position paper, the organizing committee (composed of Fausto Catena, Nicola de’Angelis, and Jim Khan) constituted a steering committee (made up of 16 experts), who had the task of drafting the present position paper, and an international expert panel composed of 21 experts who were asked to critically revise the manuscript and position statements. The position paper was conducted according to the WSES methodology [13]. We shall present the systematic review of the literature and provide the derived statements upon which a consensus was reached, specifying the quality of the supporting evidence and suggesting future research directions.
Systematic review
Methods
Review question, selection criteria, and search strategy
The systematic review of the literature was performed following the Cochrane Collaboration specific protocol [14] and was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [15].
The focus question was the following: what are the applications and outcomes of robotics for general surgery in emergency settings?
Studies reporting the use of a robotic surgical platform to manage general surgery emergencies and urgencies were searched in the following databases on June 30, 2021: MEDLINE (through PubMed), Embase, and the Cochrane Library. A specific research query was formulated for each database, using the following keywords and MeSH terms: emergency, emergency surgery, emergency setting, urgent, robotic surgery, robotic, robotics, robot-assisted, minimally invasive surgery, and minimally invasive surgery procedures.
According to the PICOS format, the following items were used as selection criteria for articles emerging from the literature search:
P, population: adult patients requiring surgery in emergent/urgent settings.
I, intervention: robotic or robot-assisted general surgery intervention.
C, comparisons: laparoscopy or open surgery or no comparison.
O, outcome(s): operative and postoperative surgical outcomes.
S, study design: due to the expected paucity of studies on the topic, all types of comparative study, but also case series and case reports were considered aiming to provide the most exhaustive picture of the current evidence and practice in robotic emergency general surgery.
The research was limited to studies published in English.
The literature search and selection were performed by two independent reviewers (GB and FM), who also screened the reference list of the selected articles to potentially include additional studies. First, all records from merged searches were reviewed for relevance concerning title and abstract. Records were removed when both reviewers excluded them. Otherwise, the disagreement was resolved via discussion or with the intervention of a tiebreaker (NdeA). Both reviewers then performed an independent full-text analysis, which allowed to finally include or exclude the preselected article.
Data extraction and synthesis
Data extraction was performed by filling in an electronic spreadsheet, which included the following items: first author’s name, year of publication, scientific journal, type of study, number of patients, pathological state requiring surgical intervention, type of surgical intervention, surgical approach, operative surgical outcomes, and postoperative surgical outcomes. The risk of bias in the selected studies was assessed by using validated systems according to the type of study design [16–18].
Results
Literature search and selection
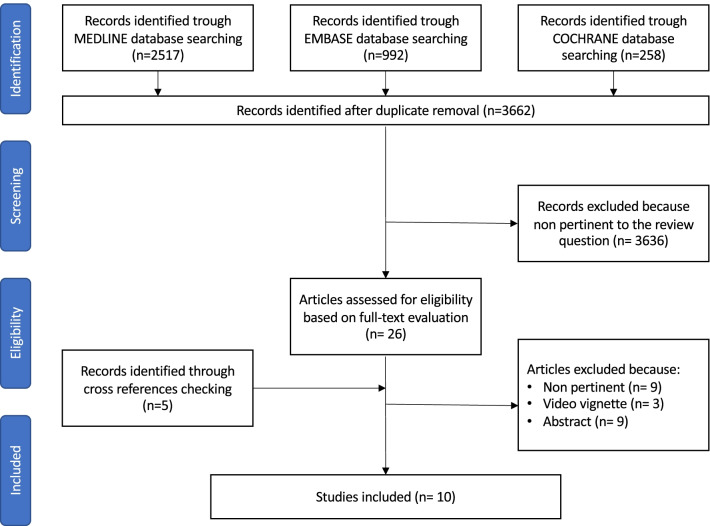
The initial search yielded 3767 results; after removing duplicates, 3662 articles were screened for eligibility based on title and abstract, and 31 articles were retrieved for a full-text evaluation. A total of 10 studies fulfilled the selection criteria and were finally included in the review (Fig. 1).
Fig. 1.
Flowchart of the literature search and selection
Study characteristics
The selected 10 studies were published between 2012 and 2021. They consisted of 5 cohort studies and 5 case reports conducted in Europe (n = 3) and North America (n = 7). The characteristics of the examined studies are summarized in Table 1. Overall, they considered 279 patients.
Table 1.
Studies reporting on urgent/emergent general surgery interventions performed with a robotic approach
| References | Study design | Nb. of patients | Time period | Pathology | Intervention | Robotic platform | Outcomes | Results |
|---|---|---|---|---|---|---|---|---|
| Comparative studies | ||||||||
| Hosein et al. [21] | Retrospective cohort study |
131 robotic cases 719 open cases 1517 laparoscopic cases |
January 2015–December 2017 | Hiatal hernia | Hiatal hernia repair | Unknown | Perioperative outcomes | Trend towards better outcomes in minimally invasive surgery (laparoscopic and robotic) as compared to open approach |
| Kubat et al. [22] | Retrospective cohort study |
76 robotic (elective) cases 74 robotic (urgent) cases |
May 2001–August 2013 | Acute cholecystitis, choledocholithiasis, severe chronic cholecystitis | Robotic single-site cholecystectomy | Intuitive Surgical da Vinci Si™ | Perioperative outcomes and learning curve | Robotic single-site cholecystectomy is safe and can be applied to urgent and elective settings with acceptable perioperative outcomes. Learning curve of 50 cases |
| Robinson et al. [12] | Retrospective cohort study |
4 robotic cases 0 laparoscopic cases |
2015–2019 | Perforated gastrojejunal ulcers following Roux-en-Y gastric bypass surgery | Repairs of perforated gastrojejunal ulcers | Intuitive Surgical da Vinci Si™/Xi™ | Perioperative outcomes | Outcomes are non-inferior to laparoscopy with the use of the robot. In-room-to-surgery time is reduced in the robotic group. Costs are greater in the robotic group |
| Anderson et al. [9] | Retrospective cohort study on a prospective database |
6 robotic cases 13 laparoscopic cases |
February 2015–February 2017 | Severe acute ulcerative colitis | Subtotal colectomy | Intuitive Surgical da Vinci Xi™ | Feasibility and perioperative outcomes | Robotic subtotal colectomy has similar perioperative outcomes of laparoscopic subtotal colectomy |
| Case series and case reports | ||||||||
| Kudsi et al. [25] | Case series | 34 robotic cases | February 2013–November 2019 | Ventral hernia | Robotic ventral hernia repair | Intuitive Surgical da Vinci™ | Perioperative outcomes and mid-term follow-up | Robotic ventral hernia repair is effective in the emergency setting |
| Ceccarelli et al. [21] | Case series | 3 robotic cases | December 2009–December 2019 | Giant hiatal hernia | Hernia repair ± fundoplication | Intuitive Surgical da Vinci Xi™ | Perioperative outcomes | Uneventful postoperative course in patients, one patient developed an antrum stenosis due to preoperative mucosal ischemia |
| Milone et al. [23] | Case series | 3 robotic cases | 2019 | Moderate acute calculous cholecystitis | Robotic cholecystectomy | Intuitive Surgical da Vinci Si™ | Perioperative outcomes | Uneventful postoperative course |
| Sudan et al. [24] | Case report | Robotic cases | 2001 | Complications of biliopancreatic diversion with duodenal switch |
Robotic strictureplasty Robotic suture of duodenal stump |
Intuitive Surgical da Vinci Si™ | Perioperative outcomes | Uneventful postoperative course |
| Felli et al. [10] | Case report | 1 robotic case | 2014 | Hemorrhagic right colon cancer | Robotic right colectomy with double-barreled ileocolostomy | Intuitive Surgical da Vinci Si™ | Perioperative outcomes | Uneventful postoperative course. At 5 months of follow-up, no recurrence was noted |
| Pedraza et al. [19] | Case report | 1 robotic case | 2001 | Iatrogenic colonoscopy perforation | Robotic colorrhaphy | Intuitive Surgical da Vinci Si™ | Perioperative outcomes | Uneventful postoperative course |
Three studies reported interventions of colorectal surgery [9, 10, 19], two studies reported on hiatal hernia surgery [20, 21], two studies reported on gallbladder surgery [22, 23], two studies reported on bariatric surgery [12, 24], and one study reported on abdominal wall surgery [25]. Only one case was a cancer-related emergency [10].
Qualitative synthesis of the literature
Robotics in emergency colorectal surgery
An early preliminary report of an emergent robotic repair of a colonic iatrogenic perforation was published by Pedraza et al. in 2012 [19]. The authors showed that such a procedure was feasible and successful. In 2014, Felli et al. [10] described the case of an 86-year old woman who underwent a robotic right colectomy for a bleeding ascending colon neoplasia. The surgery was uneventful and the reported postoperative outcomes were excellent. More recently, Anderson et al. [9] published a matched case–control study focusing on the use of robotics for urgent subtotal colectomies in patients presenting with ulcerative colitis. The results showed similar short-term outcomes for robotic and laparoscopic approaches.
-
2.
Robotics in emergency hiatal hernia surgery
Over the last years, two groups published their early experience with robotic surgery for emergency hiatal hernia repair. In a case series of 3 patients undergoing robotic surgery for complicated giant hiatal hernia, Ceccarelli et al. [21] showed that postoperative outcomes were good. The authors suggested that the potential advantages of robotics over a conventional laparoscopic approach were mainly related to the surgeon’s comfort and precision during the intervention. Hosein et al. [20] performed a cohort-based analysis using data from the 2015–2017 Vizient clinical database, which included inpatient data from over 300 hospitals in the USA. Trend analysis demonstrated that laparoscopy was the most common approach in emergency hiatal hernia repair, representing 64.09% of cases, followed by the open (30.38%) and the robotic approach (5.53%). Concerning operative and postoperative outcomes, a trend was also observed for better outcomes in case of MIS (laparoscopy or robotic) hiatal hernia repair as compared to open surgery.
-
3.
Robotics in emergency gallbladder surgery
In 2016, Kubat et al. [22] published a retrospective case series of 76 elective and 74 urgent robotic single-site cholecystectomies. The authors reported good perioperative outcomes, concluding that this approach was safe and efficient. In 2019, Milone et al. [23] described a case series of 3 patients who underwent robotic cholecystectomy for acute cholecystitis. The reported perioperative outcomes were excellent and the authors recommended the introduction of robotics in emergency settings in order to validate their preliminary results.
-
4.
Robotics in emergency bariatric surgery
The first report of robotic emergency surgery after complicated robotic biliopancreatic diversion with duodenal switch was published by Sudan et al. in 2012 [24]. The robotic approach was preferred over open surgery in the management of postoperative complications in order to preserve the benefits of the previous MIS approach. The authors highlighted how the adoption of the robotic platform was useful in a patient in order to identify the damage and to repair it. More recently, Robinson et al. [12] published a retrospective cohort study comparing emergent laparoscopic and robotic gastrojejunal ulcer repair. The authors showed that in-room-to-surgery-start time was significantly reduced in the robotic group. Additionally, perioperative outcomes were in favor of the robotic approach, although not significantly different. However, robotic surgery was significantly more expensive than laparoscopy.
-
5.
Robotics in emergency abdominal wall surgery
In 2020, Kudsi et al. [25] published an article on the perioperative and mid-term outcomes of 34 patients who underwent emergency robotic ventral hernia repair with different techniques between 2013 and 2019. With a 20.5% rate of minor postoperative complications (Clavien-Dindo grades I-II), a 11.7% rate of major postoperative complications (Clavien-Dindo grades III-IV), and only one (2.9%) patient experiencing hernia recurrence, the authors concluded that robotic ventral hernia repair was associated with promising results and overall feasibility in emergency settings, to be tested in further long-term follow-up studies.
Evaluation of the quality of evidence
Five out of 10 selected studies were retrospective cohort studies and were evaluated according to the NOS [18]. Two studies received a score of 8/9 [9, 12], one study was graded 7/9 [20], and two studies had a score of 6/9 [22, 25] (Table 2). The remaining studies were evaluated according to the tool described by Murad et al. [16]. All studies received a score of 6/8 [10, 19, 21, 23, 24] (Table 3).
Table 2.
Quality assessment for the selected retrospective cohort studies according to the Newcastle Ottawa Scale (NOS)
Table 3.
Quality assessment for the selected case series/case reports according to Murad et al. [16]
Position statements
Following a comprehensive literature review and the summary of current scientific evidence on the applications of robotics for emergency general surgery procedures, the following position statements (PS) were put forward. For each statement, the supporting literature, the level of evidence, and the strength of the consensus are indicated. The level of evidence is classified according to the GRADE system (https://training.cochrane.org/introduction-grade). For each statement, the consensus was assessed through a web survey (by means of a Google Form) open to all members of the steering committee and panel of experts and to the members of the Board of Governors of the WSES. If a statement reached < 70% of agreement, it was rediscussed via email or videoconference, modified, and resubmitted to the experts’ vote until a consensus was reached.
The experts involved were also asked to describe their current practice. The great majority (82.6%) worked in a hospital equipped with a robotic surgical platform. However, the access to the robotic surgical system for emergency procedures appeared to be limited, with difficult availability (39.1%) only during the day (13%), or not available at all (43.5%).
PS-1. Robotic surgery in emergency settings is highly dependent on the surgeon’s experience and should only be performed in an appropriately equipped operating room with trained nursing staff.
Supporting literature
Robotic surgery requires a high level of technical expertise when compared to open or even laparoscopic surgery. A complete specialized training is required to be proficient in performing standardized surgical interventions associated with acceptable operative and postoperative outcomes [26]. In a recent article, Thomas et al. [27] analyzed the robotic colorectal surgery activity of a tertiary colorectal unit and concluded that success relies on a structured training curriculum, a dedicated surgical team, the institution’s support, and many other variables in addition to the training at the robotic console itself. The adoption of the robot in the emergency setting does not change the rules of the game. Rather, it enhances the need for a safe and efficient strategy starting from the standardization of the robotic platform setting and docking, up to the execution of the surgical procedure. In order to successfully perform emergency cases with a robotic system, the on-call surgical team must be adequately trained with robotic technology. As reported by Robinson et al. [12] in a case series of 24 robotic emergency bariatric surgeries, which were compared to 20 laparoscopic procedures, the surgeon who adopted the robotic approach was the same in all cases. It is the proof that a specific attitude of the operator is fundamental. However, it also highlights the need for a “can do” attitude from the entire surgical team [28]. The importance of the shared viewpoint is reinforced by Sudan et al. [24] who described the adoption of the robotic platform during the night and during the weekend in order for the staff to be comfortable with this technology. In addition, proper team work and communication in such a challenging workspace are required [29] as much as the completion of the learning curve for the entire surgical team [30]. The ideal operating room team in an emergency setting should be made up of the first operating surgeon with an extensive expertise in robotic surgery, an assisting surgeon familiar with the robotic technology, and a scrub nurse dedicated to the robotic program. All team members should work in a simulation environment before starting a robotic emergency surgery program.
Limitations linked to the adoption of robotic surgery in emergency settings are related to the time required for robotic setting and docking and the accessibility of the robotic platform for emergency surgical units. Concerning the time issue, Robinson et al. [12] reported that, when the entire team is appropriately trained and prepared, the in-room-to-surgery-start time is reduced and has no significant impact on the overall duration of the scheduled emergency procedure. However, in this study, the authors highlighted how the majority of the staff were familiar with the robotic technology, and there were no limitations to its accessibility. This may not be the case for all emergency care units, and trained nursing staff may not be always available during night shifts. A good coordination between the hospital administration, the surgeons, and the staff is the key point to have an efficient and extensive organization for the use of robotic technology, also in emergency surgery scenarios.
Level of evidence: case reports and case series → expert opinion
Strength of consensus (based on the survey evaluation): 100%
PS-2. Robotic surgery in emergency settings may be considered in highly selected clinically stable patients only.
Supporting literature
Due to the very limited evidence in the literature and the consensus that robotic surgery required a high level of expertise for the operating surgeon and the entire surgical team, particularly if performed in emergency settings, it should be considered for clinically stable patients only.
A recent review [31] on the anesthetic aspects of robotic surgery suggested that when the surgical team gains confidence, even more complex operations or patients with comorbidities can be considered candidates for the robotic approach. A precise preoperative assessment based on a case-by-case evaluation, and multidisciplinary decision-making are crucial to guarantee the choice of the most indicated surgical strategy. Even if a comprehensive preoperative assessment is not always possible in emergency situations, a careful patient selection is advised in order not to expose frail or unstable patients to longer emergency procedures or unnecessary complications related to the surgical technique.
Indeed, in unstable patients or patients with cardiopulmonary comorbidities, the adoption of MIS with the need for carbon dioxide insufflation may result in a higher intra-abdominal pressure and hypercarbia with metabolic and respiratory changes which may be deleterious [32]. Osagiede et al. [11] showed that the presence of a metastatic disease and the higher number of comorbidities negatively influenced the adoption of MIS in emergency colorectal cancer surgery. Likewise, Arnold et al. [33] demonstrated that the adoption of MIS is confined to physiologically clinically stable patients while those with abdominal gross contamination or severe infectious processes are more prone to undergo open surgery. Despite this selection bias, when the results are corrected for preoperative risk factors, the adoption of laparoscopy is associated with a reduced wound infection rate, risk of death, and length of hospital stay.
Recently, emergency laparoscopy was evaluated as a valid approach to the treatment of perforated diverticulitis with generalized peritonitis [34], iatrogenic colonoscopy perforations [35], and perforated peptic ulcers [36]. In addition, in simple cases of adhesive small bowel obstruction, a laparoscopic approach may be beneficial despite the considerable risk of conversion to open surgery and the higher probability of bowel injuries [37]. In all of the abovementioned pathological states, the prerequisite for a safe minimally invasive treatment is the selection of a stable patient.
In terms of anesthetic management in emergency settings, the robotic approach can be considered as an alternative to laparoscopy because it does not change the risk exposure but it may be associated with longer operative times if the surgical team is not properly trained. Additional costs must also be considered. Further studies are necessary in order to clarify the future role of a low pressure pneumoperitoneum in emergency robotic surgery [38].
Level of evidence: case reports and case series → expert opinion
Strength of consensus: 94.6%
PS-3. Robotic surgery may be considered in challenging situations, which are foreseen as a reason for conversion to open surgery if operating in laparoscopy.
Supporting literature
The available literature suggests that the main potential advantages of robotic surgery over laparoscopy are related to suturing and dissection. In case of emergency robotic surgery, the published studies described the following procedural steps: hiatoplasties [20, 21], ventral suturing or mesh fixations [25], colonic suturing [19], duodenal stump suturing [24], strictureplasty [24], and dissection of inflamed gallbladder [22, 23] or colon [9]. All of these tasks are particularly challenging in laparoscopic surgery and they often lead to conversion to open surgery, which can also be a source of postoperative complications [39, 40]. The technological advances of the robotic surgical platform, such as deep magnification, 3D stereoscopic vision, a stable field with elimination of physiological tremors, motion scaling, and improved ergonomics as compared to laparoscopy, may contribute to facilitate the performance of some difficult procedural steps and reduce the risk of conversion. However, this remains to be proven, especially for surgical interventions performed in emergency settings.
Level of evidence: case reports and case series → expert opinion.
Strength of consensus: 83.8% (based on the survey evaluation)
PS-4. In a near future, robotic surgery may offer the advantage of telementoring and telesurgery, which could be useful to promote a safe and standardized application of robotics, also in low-volume centers or specific environments.
Supporting literature
One of the limitations of laparoscopic surgery is the absence of telementoring during a difficult procedure. Even if communicating systems dedicated to telementoring are available, no opportunity for the direct control of movements is present in laparoscopy. In robotic surgery, an in-person mentoring can be performed if a second robotic console is present in the hospital (such as telestration or tele-assisted surgery). In a near future, it can be expected to perform telementoring during elective and emergency robotic procedures. After the first transatlantic robot-assisted surgery performed by Jacques Marescaux in 2001 [41], the surgical community was waiting for a routine use of telesurgery which, however, was not feasible due to technical limitations. Today, thanks to the evolution of telecommunications, namely fifth generation (5G) networks, there is a growing opportunity for a surgeon with a proven expertise in the field to remotely operate on a distant patient [42, 43]. A digital connection with a reference center which can evaluate the case, suggest a solution, and eventually manage the surgical situation if need be, represents a powerful tool, especially in emergency settings. Indeed, in emergency surgery where a maximal experience improves outcomes, it would be beneficial to have a mentor observing and remotely participating in the intervention. Additionally, this technology could be applied to provide surgical care to rural areas, to establish surgical collaborations, and to eliminate the shortage of surgeons. This is also applicable for specific environments, such as in the space station, where an emergency medical condition has to be managed by a trained component of the crew, or close to a battlefield, where the surgeon may operate at a safe distance, or again at the bottom of the ocean [44]. Telesurgery could well be an option in such situations.
However, these applications conceal some limitations in terms of global network development, legal and ethical issues, costs, and cyber security. These issues are under examination. However, despite the current skepticism, it is unquestionable that robotic surgery can have a pivotal role in developing telemedicine and telesurgery [45, 46].
Level of evidence: case reports and case series → expert opinion
Strength of consensus: 89.2% (based on the survey evaluation)
PS-5. The use of robotic surgery for unscheduled and urgent operations needs to be implanted without creating scheduling conflicts in the occupation of the operating room. Moreover, the increased costs need to be justified in the context of an efficient implementation of robotic surgery. Currently, the availability and accessibility of the robotic platforms for emergency care surgical units are very limited.
Supporting literature
A consistently growing number of hospitals, mainly tertiary care and university-based hospitals, are acquiring a robotic surgical platform in order to satisfy daily requests and advertise the most advanced technology. The robotic platform is often shared between different specialties, subsequently limited in terms of availability for a single surgical field and not adaptable to changing schedules. In this perspective, several reports suggested that the use of the robotic surgical platform by experienced teams could be prolonged to night hours and even to the weekend. This approach was called “after hours” by Sudan et al. [24], whose report aimed to highlight the potential of a robotic system which is available 24 h/7 days per week. The availability of the platform during the night shift could potentially favor a more cost-effective use of the robotic system. However, this remains very limited and, as previously highlighted, a proper attitude and excellent training of the entire team are key to guarantee surgical proficiency and efficiently implement robotic surgery for emergency procedures.
Concerns for the adoption of robotics for emergency surgeries also persist in relation to the increased costs that a robotic surgical procedure implies also need to be justified in the context of an efficient implementation of robotic surgery.
Level of evidence: case reports and case series → expert opinion
Strength of consensus: 89.2% (based on the survey evaluation)
PS-6. The development of new modular robotic platforms may contribute to increase the applications of robotic surgery in emergency settings.
Supporting literature
The surgical marketplace was recently enhanced with several different robotic platforms either approved for human use, such as the CMR Versius (Cambridge Medical Robotics, Cambridge, UK) and the Distalmotion Dexter (Distalmotion, Epalinges, Switzerland) or under approval, such as the Medtronic Hugo (Medtronic Inc., Minneapolis, USA). Most of them share the opportunity of switching from a conventional laparoscopic setting to a robot-assisted one. This key point, which could be less relevant in elective surgery, should be carefully considered when approaching emergency surgery. In fact, when no specific port placement is required, the surgeon can simply use a different approach depending on the procedural step and on his/her own ability. In addition, these robotic platforms offer an improved vision with advanced near-infrared imaging, not routinely available in laparoscopic surgery. The objective evaluation of tissue anatomy or perfusion could limit the surgical bias in emergency settings by mitigating the personal opinion [47, 48].
In the future, advances in surgical technologies will offer multiple new opportunities, which are currently under development, like hyperspectral imaging [49] and robotic single-port surgery [50]. Their potential applications and outcomes in emergency surgery need to be evaluated and updated once evidence is available.
Level of evidence: case reports and case series → expert opinion
Strength of consensus: 94.6% (based on the survey evaluation)
Research agenda
The experts recognized that there is a substantial lack of evidence to support the use of robotic surgery for emerging general surgery procedures. For this reason, a research agenda has been proposed.
Observational (cohort study, case–control) and interventional studies are anticipated to investigate the applications and outcomes of robotic surgery in emergency settings and to compare them with those obtained with laparoscopy and open surgery.
Future studies should evaluate patient preferences considering patient-related outcome measures (PROMs), including pain evaluation and mid-/long-term quality of life.
Future studies should evaluate the cost-effectiveness of robotic surgery implementation in emergency settings at hospital level (e.g., scheduling conflict alleviation) and at the level of the healthcare system (e.g., length of hospital stay, productivity losses, reimbursement systems).
Future studies should evaluate the applicability of the robotic surgical platforms to perform telementoring and telesurgery, which are theoretically promising technologies to expand the applications of robotic surgery.
With the aim to enrich the available evidence and fill knowledge gaps, the WSES plans to launch an open registry on emergency robotic general surgery. The WSES calls for an international participation, which is essential to gather sufficient data and obtain generalizable results.
The establishment of a dedicated registry is also mandatory to perform a deep analysis on this technique, in order to define the following: characteristics of the patient candidate for emergency robotic procedures, operative and postoperative outcomes, PROMs, minimum requisites in terms of personnel and equipment, cost-effectiveness, and ethical issues.
Discussion
Hospitals that are currently equipped with a robotic surgical platform need to implement it efficiently. The role of robotic surgery for emergency procedures remains under investigation. However, its use is expanding despite the lack of evidence-based guidelines. In this scenario, the WSES wished to provide this position paper to the surgical community. This position paper summarizes the current evidence and practice and proposes consensus statements to be reevaluated and updated as the evidence in the supporting literature emerges. For now, the experts recommend a strict patient selection while approaching emergent general surgery procedures with robotics. However, an emergency setting should not be seen as a contraindication for robotic surgery if adequate training of the operating surgical team is available. When such prerequisites are met, robotic surgery can be considered safe and feasible, and surgical outcomes related to an MIS approach are expected. Finally, the application of the robotic surgical platform may grow with improvements in telementoring and telesurgery, which are particularly valuable in emergency settings.
Acknowledgements
The authors are grateful to Guy Temporal and Christopher Burel, professionals in medical English proofreading, for their valuable help.
Abbreviations
- MIS
Minimally invasive surgery
- NOS
Newcastle–Ottawa Scale
- PROM
Patient-related outcome measures
- PS
Position statements
- WSES
World Society of Emergency Surgery
Authors' contributions
GB, FM, and NdeA conducted the systematic review of the literature and wrote the first draft of the manuscript. All authors were involved in the statement evaluation and consensus process. All authors critically reviewed the manuscript and approved the final version. All authors read and approved the final manuscript.
Funding
No funding or resources was received for the preparation of this article. The authors received a WSES institutional waiver for this publication.
Availability of data and materials
There are no data from individual authors that reach the criteria for availability.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
P Pessaux declared that he received consulting fees from 3M and Integra and has stock-options of Virtualisurg. E Kouwenhoven is proctor for Intuitive Surgical. M Sugrue received consulting fee with 3M, Smith and Nephew and Novus Scientific. G Spinoglio received honoraria as proctor for Intuitive Surgical. F. Ris reports research funding from Quantgene, personal fees from Arthrex, Stryker, Hollister, Fresenius Kabi and Distal Motion, outside the submitted work. E Espin Bsany received honoraria as proctor for Intuitive Surgical. JS Khan is a proctor for Intuitive Surgical. All other authors have no conflicts of interest to declare in relation to the matter of this publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nicola de’Angelis, Email: nic.deangelis@yahoo.it.
Jim Khan, Email: mkhan702@aol.com.
Francesco Marchegiani, Email: marchegiani.fra@gmail.com.
Giorgio Bianchi, Email: 87.giorgio.bianch@gmail.com.
Filippo Aisoni, Email: aisonifilippo@gmail.com.
Daniele Alberti, Email: daniele.alberti@asst-spedalicivili.it.
Luca Ansaloni, Email: aiace63@gmail.com.
Walter Biffl, Email: biffl.walter@scrippshealth.org.
Osvaldo Chiara, Email: ochiara@yahoo.com.
Graziano Ceccarelli, Email: g.cecca2003@libero.it.
Federico Coccolini, Email: federico.coccolini@gmail.com.
Enrico Cicuttin, Email: enrico.cqtn@gmail.com.
Mathieu D’Hondt, Email: mathieudhondt2000@yahoo.com.
Salomone Di Saverio, Email: salomone.disaverio@gmail.com.
Michele Diana, Email: michele.diana@ircad.fr.
Belinda De Simone, Email: desimone.belinda@gmail.com.
Eloy Espin-Basany, Email: eespin@me.com.
Stefan Fichtner-Feigl, Email: stefan.fichtner@uniklinik-freiburg.de.
Jeffry Kashuk, Email: jeffrykashuk@gmail.com.
Ewout Kouwenhoven, Email: e.kouwenhoven@zgt.nl.
Ari Leppaniemi, Email: ari.leppaniemi@hus.fi.
Nassiba Beghdadi, Email: nassiba.beghdadi@hotmail.fr.
Riccardo Memeo, Email: info@drmemeoriccardo.com.
Marco Milone, Email: milone.marco.md@gmail.com.
Ernest Moore, Email: ernest.moore@dhha.org.
Andrew Peitzmann, Email: peitzmanab@upmc.edu.
Patrick Pessaux, Email: patrick.pessaux@chru-strasbourg.gr.
Manos Pikoulis, Email: mpikoul@med.uoa.gr.
Michele Pisano, Email: mpisano@asst-pg23.it.
Frederic Ris, Email: frederic.ris@hcuge.ch.
Massimo Sartelli, Email: massimosartelli@gmail.com.
Giuseppe Spinoglio, Email: giuseppe.spinoglio90@gmail.com.
Michael Sugrue, Email: michaelesugrue@gmail.com.
Edward Tan, Email: edward.tan@radboudumc.nl.
Paschalis Gavriilidis, Email: pgavrielidis@yahoo.com.
Dieter Weber, Email: dietergweber@gmail.com.
Yoram Kluger, Email: y_kluger@rambam.health.gov.il.
Fausto Catena, Email: faustocatena@gmail.com.
References
- 1.Yeo HL, Isaacs AJ, Abelson JS, Milsom JW, Sedrakyan A. Comparison of open, laparoscopic, and robotic colectomies using a large national database: outcomes and trends related to surgery center volume. Dis Colon Rectum. 2016;59:535–542. doi: 10.1097/dcr.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 2.Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, et al. The Miami International evidence-based guidelines on minimally invasive pancreas resection. Ann Surg. 2020;271:1–14. doi: 10.1097/sla.0000000000003590. [DOI] [PubMed] [Google Scholar]
- 3.Jung M, Morel P, Buehler L, Buchs NC, Hagen ME. Robotic general surgery: current practice, evidence, and perspective. Langenbecks Arch Surg. 2015;400:283–292. doi: 10.1007/s00423-015-1278-y. [DOI] [PubMed] [Google Scholar]
- 4.Hanly EJ, Talamini MA. Robotic abdominal surgery. Am J Surg. 2004;188:19s–26s. doi: 10.1016/j.amjsurg.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 5.Felder SI, Ramanathan R, Russo AE, Jimenez-Rodriguez RM, Hogg ME, Zureikat AH, et al. Robotic gastrointestinal surgery. Curr Probl Surg. 2018;55:198–246. doi: 10.1067/j.cpsurg.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu R, Wakabayashi G, Palanivelu C, Tsung A, Yang K, Goh BKP, et al. International consensus statement on robotic pancreatic surgery. Hepatobiliary Surg Nutr. 2019;8:345–360. doi: 10.21037/hbsn.2019.07.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.George EI, Brand TC, LaPorta A, Marescaux J, Satava RM. Origins of robotic surgery: from skepticism to standard of care. JSLS. 2018;22:e2018.00039. doi: 10.4293/jsls.2018.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de’Angelis N, Notarnicola M, Martínez-Pérez A, Memeo R, Charpy C, Urciuoli I, et al. Robotic versus laparoscopic partial mesorectal excision for cancer of the high rectum: a single-center study with propensity score matching analysis. World J Surg. 2020;44:3923–3935. doi: 10.1007/s00268-020-05666-0. [DOI] [PubMed] [Google Scholar]
- 9.Anderson M, Lynn P, Aydinli HH, Schwartzberg D, Bernstein M, Grucela A. Early experience with urgent robotic subtotal colectomy for severe acute ulcerative colitis has comparable perioperative outcomes to laparoscopic surgery. J Robot Surg. 2020;14:249–253. doi: 10.1007/s11701-019-00968-5. [DOI] [PubMed] [Google Scholar]
- 10.Felli E, Brunetti F, Disabato M, Salloum C, Azoulay D, de’Angelis N. Robotic right colectomy for hemorrhagic right colon cancer: a case report and review of the literature of minimally invasive urgent colectomy. World J Emerg Surg. 2014;9:32. doi: 10.1186/1749-7922-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Osagiede O, Spaulding AC, Cochuyt JJ, Naessens JM, Merchea A, Crandall M, et al. Factors associated with minimally invasive surgery for colorectal cancer in emergency settings. J Surg Res. 2019;243:75–82. doi: 10.1016/j.jss.2019.04.089. [DOI] [PubMed] [Google Scholar]
- 12.Robinson TD, Sheehan JC, Patel PB, Marthy AG, Zaman JA, Singh TP. Emergent robotic versus laparoscopic surgery for perforated gastrojejunal ulcers: a retrospective cohort study of 44 patients. Surg Endosc. 2021 doi: 10.1007/s00464-021-08447-5. [DOI] [PubMed] [Google Scholar]
- 13.Bala M, Kashuk J, Moore EE, Catena F, Leppaniemi A, Ansaloni L, et al. Establishing position papers by the WSES. World J Emerg Surg. 2018;13:1. doi: 10.1186/s13017-018-0163-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. In: Cochrane handbook for systematic reviews of interventions: Cochrane Book Series. 2008.
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60–63. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 18.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 19.Pedraza R, Ragupathi M, Martinez T, Haas EM. Robotic-assisted laparoscopic primary repair of acute iatrogenic colonic perforation: case report. Int J Med Robot. 2012;8:375–378. doi: 10.1002/rcs.1447. [DOI] [PubMed] [Google Scholar]
- 20.Hosein S, Carlson T, Flores L, Armijo PR, Oleynikov D. Minimally invasive approach to hiatal hernia repair is superior to open, even in the emergent setting: a large national database analysis. Surg Endosc. 2021;35:423–428. doi: 10.1007/s00464-020-07404-y. [DOI] [PubMed] [Google Scholar]
- 21.Ceccarelli G, Pasculli A, Bugiantella W, De Rosa M, Catena F, Rondelli F, et al. Minimally invasive laparoscopic and robot-assisted emergency treatment of strangulated giant hiatal hernias: report of five cases and literature review. World J Emerg Surg. 2020;15:37. doi: 10.1186/s13017-020-00316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kubat E, Hansen N, Nguyen HP, Wren SM, Eisenberg D. Urgent and elective robotic single-site cholecystectomy: analysis and learning curve of 150 consecutive cases. J Laparoendosc Adv Surg Tech A. 2016;26:185–191. doi: 10.1089/lap.2015.0528. [DOI] [PubMed] [Google Scholar]
- 23.Milone M, Vertaldi S, Bracale U, D’Ambra M, Cassese G, Manigrasso M, et al. Robotic cholecystectomy for acute cholecystitis: three case reports. Medicine (Baltimore) 2019;98:e16010. doi: 10.1097/MD.0000000000016010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sudan R, Desai SS. Emergency and weekend robotic surgery are feasible. J Robot Surg. 2012;6:263–266. doi: 10.1007/s11701-011-0289-0. [DOI] [PubMed] [Google Scholar]
- 25.Kudsi OY, Bou-Ayash N, Chang K, Gokcal F. Perioperative and midterm outcomes of emergent robotic repair of incarcerated ventral and incisional hernia. J Robot Surg. 2021;15:473–481. doi: 10.1007/s11701-020-01130-2. [DOI] [PubMed] [Google Scholar]
- 26.Panteleimonitis S, Popeskou S, Aradaib M, Harper M, Ahmed J, Ahmad M, et al. Implementation of robotic rectal surgery training programme: importance of standardisation and structured training. Langenbecks Arch Surg. 2018;403:749–760. doi: 10.1007/s00423-018-1690-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomas A, Altaf K, Sochorova D, Gur U, Parvaiz A, Ahmed S. Effective implementation and adaptation of structured robotic colorectal programme in a busy tertiary unit. J Robot Surg. 2020 doi: 10.1007/s11701-020-01169-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schuessler Z, Scott Stiles A, Mancuso P. Perceptions and experiences of perioperative nurses and nurse anaesthetists in robotic-assisted surgery. J Clin Nurs. 2020;29:60–74. doi: 10.1111/jocn.15053. [DOI] [PubMed] [Google Scholar]
- 29.Kanji F, Catchpole K, Choi E, Alfred M, Cohen K, Shouhed D, et al. Work-system interventions in robotic-assisted surgery: a systematic review exploring the gap between challenges and solutions. Surg Endosc. 2021;35:1976–1989. doi: 10.1007/s00464-020-08231-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith AL, Scott EM, Krivak TC, Olawaiye AB, Chu T, Richard SD. Dual-console robotic surgery: a new teaching paradigm. J Robot Surg. 2012;7:113–118. doi: 10.1007/s11701-012-0348-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ashrafian H, Clancy O, Grover V, Darzi A. The evolution of robotic surgery: surgical and anaesthetic aspects. Br J Anaesth. 2017;119:i72–i84. doi: 10.1093/bja/aex383. [DOI] [PubMed] [Google Scholar]
- 32.Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110:810–815. doi: 10.1378/chest.110.3.810. [DOI] [PubMed] [Google Scholar]
- 33.Arnold M, Elhage S, Schiffern L, Lauren Paton B, Ross SW, Matthews BD, et al. Use of minimally invasive surgery in emergency general surgery procedures. Surg Endosc. 2020;34:2258–2265. doi: 10.1007/s00464-019-07016-1. [DOI] [PubMed] [Google Scholar]
- 34.Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32. doi: 10.1186/s13017-020-00313-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de’Angelis N, Di Saverio S, Chiara O, Sartelli M, Martínez-Pérez A, Patrizi F, et al. 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation. World J Emerg Surg. 2018;24:5. doi: 10.1186/s13017-018-0162-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tarasconi A, Coccolini F, Biffl WL, Tomasoni M, Ansaloni L, Picetti E, et al. Perforated and bleeding peptic ulcer: WSES guidelines. World J Emerg Surg. 2020 doi: 10.1186/s13017-019-0283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.ten Broek RPG, Krielen P, Di Saverio S, Coccolini F, Biffl WL, Ansaloni L, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2017;2018:13. doi: 10.1186/s13017-018-0185-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Celarier S, Monziols S, Célérier B, Assenat V, Carles P, Napolitano G, et al. Low-pressure versus standard pressure laparoscopic colorectal surgery (PAROS trial): a phase III randomized controlled trial. Br J Surg. 2021 doi: 10.1093/bjs/znab069. [DOI] [PubMed] [Google Scholar]
- 39.Granero L, Cienfuegos JA, Baixauli J, Pastor C, Sánchez Justicia C, Valentí V, et al. Predictive risk factors for postoperative complications and its impact on survival in laparoscopic resection for colon cancer. Surg Laparosc Endosc Percutan Tech. 2021 doi: 10.1097/SLE.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 40.Payá-Llorente C, Domingo-del Pozo C, Gonzálvez-Guardiola P, Santarrufina-Martínez S, Pareja-Ibars E, Martínez-Pérez A. Conversion to open surgery during laparoscopic common bile duct exploration: predictive factors and impact on the perioperative outcomes. HPB (Oxford) 2021 doi: 10.1016/j.hpb.2021.05.009. [DOI] [PubMed] [Google Scholar]
- 41.Marescaux J, Leroy J, Gagner M, Rubino F, Mutter D, Vix M, et al. Transatlantic robot-assisted telesurgery. Nature. 2001;413:379–380. doi: 10.1038/35096636. [DOI] [PubMed] [Google Scholar]
- 42.Tian W, Fan M, Zeng C, Liu Y, He D, Zhang Q. Telerobotic spinal surgery based on 5G network: the first 12 cases. Neurospine. 2020;17:114–120. doi: 10.14245/ns.1938454.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zheng J, Wang Y, Zhang J, Guo W, Yang X, Luo L, et al. 5G ultra-remote robot-assisted laparoscopic surgery in China. Surg Endosc. 2020;34:5172–5180. doi: 10.1007/s00464-020-07823-x. [DOI] [PubMed] [Google Scholar]
- 44.Reichenbach M, Frederick T, Cubrich L, Bircher W, Bills N, Morien M, et al. Telesurgery with miniature robots to leverage surgical expertise in distributed expeditionary environments. Mil Med. 2017;182:316–321. doi: 10.7205/milmed-d-16-00176. [DOI] [PubMed] [Google Scholar]
- 45.Mohan A, Wara UU, Arshad Shaikh MT, Rahman RM, Zaidi ZA. Telesurgery and robotics: an improved and efficient era. Cureus. 2021;13:e14124. doi: 10.7759/cureus.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anvari M, Manoharan B, Barlow K. From telementorship to automation. J Surg Oncol. 2021;124:246–249. doi: 10.1002/jso.26562. [DOI] [PubMed] [Google Scholar]
- 47.Bronikowski D, Lombardo D, DeLa’O C, Szoka N. Robotic subtotal cholecystectomy in a geriatric acute care surgery patient with super obesity. Case Rep Surg. 2021;2021:9992622. doi: 10.1155/2021/9992622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liot E, Assalino M, Buchs NC, Schiltz B, Douissard J, Morel P, et al. Does near-infrared (NIR) fluorescence angiography modify operative strategy during emergency procedures? Surg Endosc. 2018;32:4351–4356. doi: 10.1007/s00464-018-6226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barberio M, Felli E, Seyller E, Longo F, Chand M, Gockel I, et al. Quantitative fluorescence angiography versus hyperspectral imaging to assess bowel ischemia: a comparative study in enhanced reality. Surgery. 2020;168:178–184. doi: 10.1016/j.surg.2020.02.008. [DOI] [PubMed] [Google Scholar]
- 50.Klazura G, Sims T, Rojnica M, Koo N, Lobe T. Single port robotic splenectomy for pyruvate kinase deficiency in a five-year-old patient, a case report of a surgical first. Int J Surg Case Rep. 2021;84:106122. doi: 10.1016/j.ijscr.2021.106122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
There are no data from individual authors that reach the criteria for availability.