Abstract
Background:
Because of the multiplying number of patients undergoing breast augmentation, nonprimary augmentation mastopexy will be increasingly requested in the future; this operation represents an even more significant challenge than primary augmentation mastopexy. The authors describe a standardized approach for subglandular-to-subpectoral implant pocket conversion in mastopexy that provides a tight neopocket with inferolateral muscular support, which minimizes implant displacement complications and allows operative strategies to reduce the risk of bacterial load on implants.
Methods:
The authors’ technique proposes the following: (1) modified subpectoral pocket, with muscular inferolateral support for the implant; (2) independent approaches to the submuscular pocket and subglandular (preexisting) pocket; and (3) preestablished four-step surgical sequence. The authors collected data from their private practices for 46 patients who underwent the technique from March of 2017 to April of 2020. Patient perception about aesthetic outcomes, photographs from multiple postoperative follow-ups, and surgical complications/reoperation rates were analyzed.
Results:
Overall results were positive; 89.1 percent of patients reported satisfaction with their aesthetic outcomes. No major complications occurred. The total revision rate was 15.2 percent, but only 2.1 percent in the last year, as the learning curve progressed.
Conclusions:
Secondary augmentation mastopexy is a complicated procedure. The four-step sequence approach is one reliable option for subglandular-to-subpectoral pocket conversion, once it produced high levels of patient satisfaction while producing low complication rates. Other surgeons’ experiences with the technique and further studies are necessary to validate these findings.
CLINICAL QUESTION/LEVEL OF EVIDENCE:
Therapeutic, IV.
Primary augmentation mastopexy is considered a great challenge for the plastic surgeon, presenting high complication and revision surgery rates.1–5 However, secondary augmentation mastopexy is an even greater problem, and because of the multiplying number of augmented patients, it is expected to be increasingly requested in the future.
We describe a standardized approach for subglandular-to-subpectoral pocket conversion combined with mastopexy, valid for patients without the need for total capsulectomy. This technique derives from that described in the article “Four-Step Augmentation Mastopexy: Lift and Augmentation at Single Time” for primary augmentation mastopexy,6 and the subpectoral pocket also features a lateral muscular sling. For those willing to try this pocket conversion technique, we strongly recommend reading the former article, for essential technical details and discussion elaborated there are not repeated in this present description to avoid redundancies.
The proposed approach organizes several concepts already described in the literature. The preestablished sequence made it easier for us to make intraoperative decisions and allowed reproducible and predictable results.
PATIENTS AND METHODS
We performed a retrospective chart review for all patients who underwent the technique. Patients with capsular contracture or previous submuscular implants were not chosen for the procedure. The study was performed in full conformity with ethical norms and standards in the Declaration of Helsinki. An informed consent statement was obtained from all 46 patients.
Surgical Technique
Step 1: Breast Implant Removal
The implant is removed through a periareolar or vertical incision to prevent communication and subsequent contamination of the new subpectoral pocket. The posterior capsule remains intact. Sutures seal the incision, isolating the preexisting pocket.
Step 2: Modified Subpectoral Pocket Creation
An incision is made through the inframammary fold, and dissection is carried out, undermining the deep surface of the posterior capsule until the fibers of the pectoralis major muscle are identified. We carefully preserve the posterior capsule integrity to avoid entering the subglandular pocket (Fig. 1).
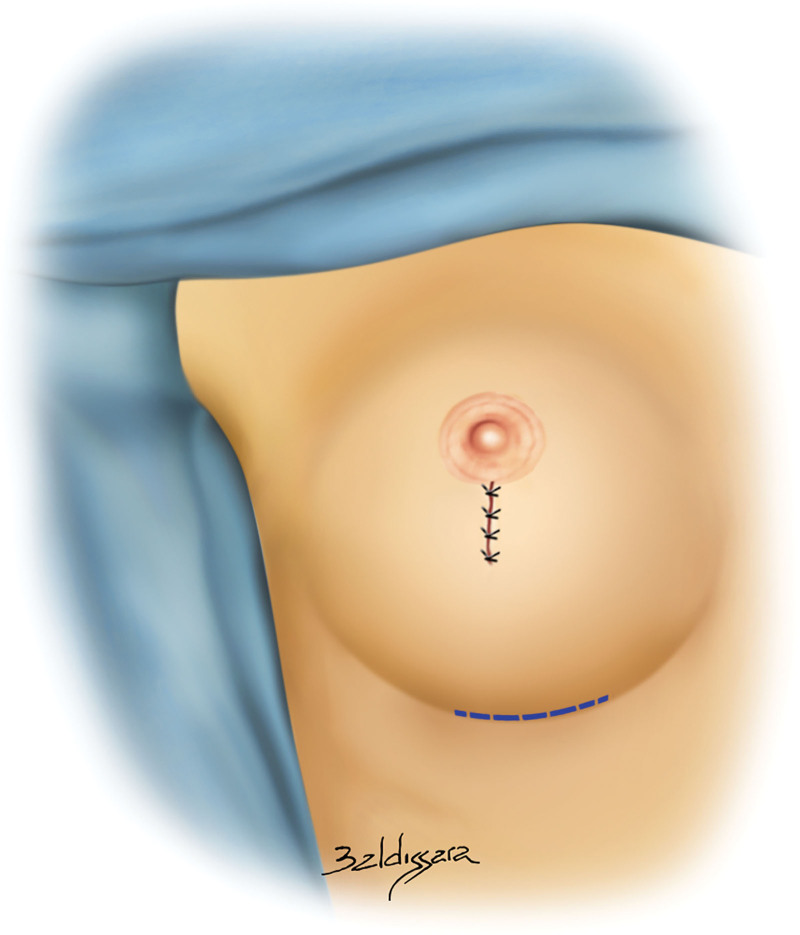
Fig. 1.
Blue trace shows inframammary approach markings for modified subpectoral pocket creation. Notice the previous subglandular pocket completely isolated (sutures).
As described previously,6 the inferomedial pectoralis costal origins are divided, except for a 1- to 2-cm-wide lateral border strip, which acts as a muscular sling. These fibers should be divided, preserving a 1-cm-high muscular cuff attached to the ribs. The sternal muscular origins are the maximum medial boundary for this division.
The upward muscular retraction results in an inferomedial area that lacks the pectoralis muscle layer. The subpectoral pocket should be tight enough to avoid undesired implant lateral or cranial displacement (Fig. 2). The new implants are inserted into the subpectoral pocket (Fig. 3).
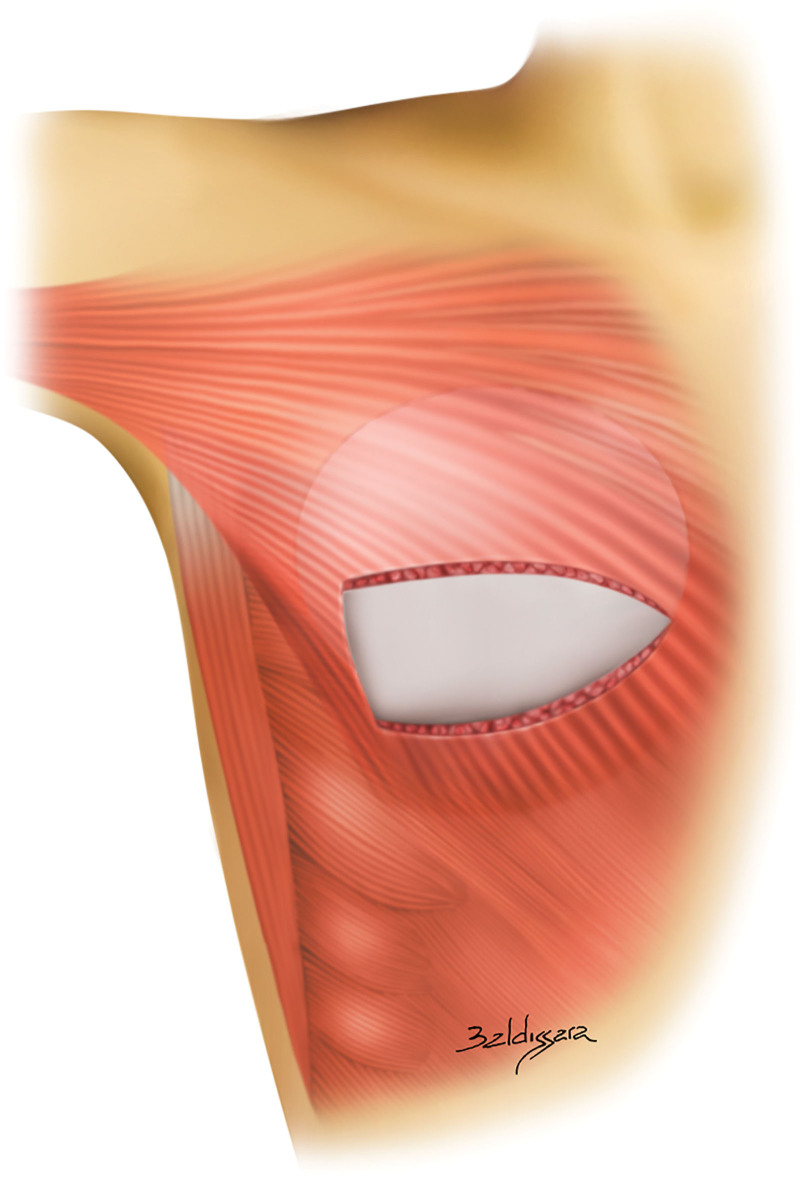
Fig. 2.
The modified subpectoral pocket. Inferomedial pectoralis origins are divided sparing a 1-cm-high muscular cuff. Inferolateral fibers are left intact (1 to 2 cm wide), creating a muscular sling.
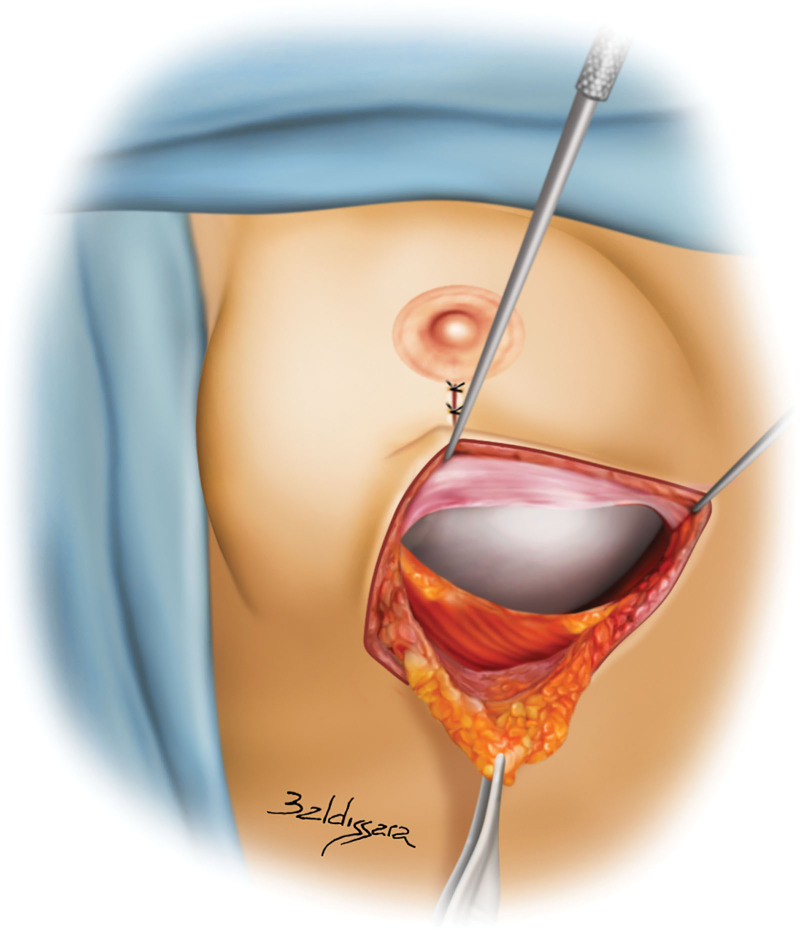
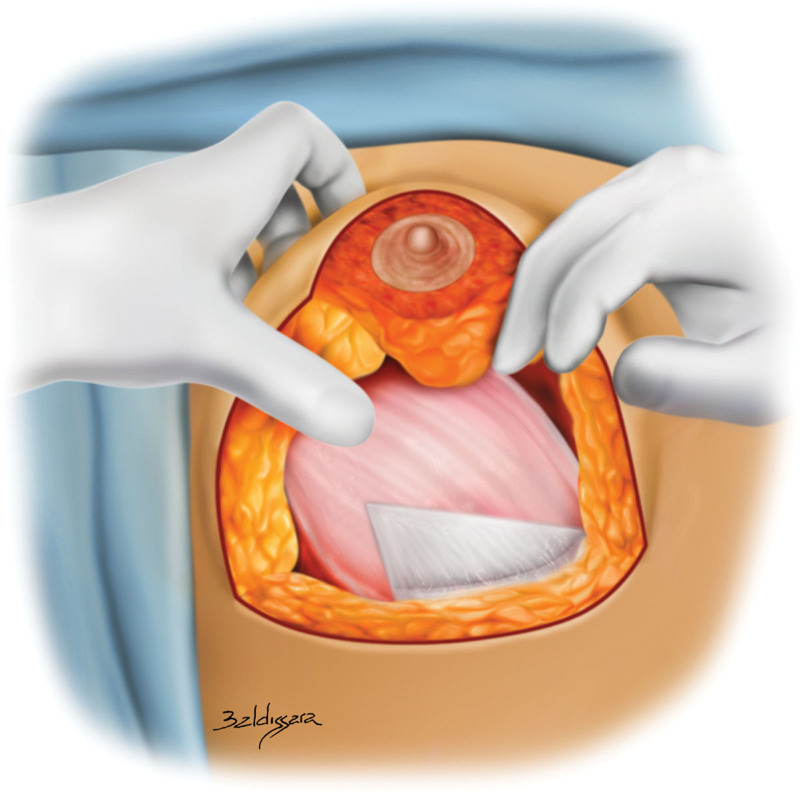
Fig. 3.
Implant inside pocket with inferolateral muscular sling support. The posterior surface of the preexisting posterior capsule is shown on the cranial border.
Step 3: Mastopexy Markings and Implant Pocket Sealing
The patient is moved to the sitting position for precise evaluation of upper pole symmetry. The new nipple-areola complex position is defined. The markings for vertical and horizontal breast tissue resection are determined by conservatively pinching the skin.
In the supine position, the new subpectoral pocket is completely sealed. The caudal posterior capsule, which was initially dissected from the pectoralis anterior surface, is pulled down and sutured to the muscular strip laterally and to the muscular cuff medially, creating a composite muscle-capsule pocket (Fig. 4). At this point, the new implants are sealed and have no contact with the previous subglandular pocket or breast parenchyma.
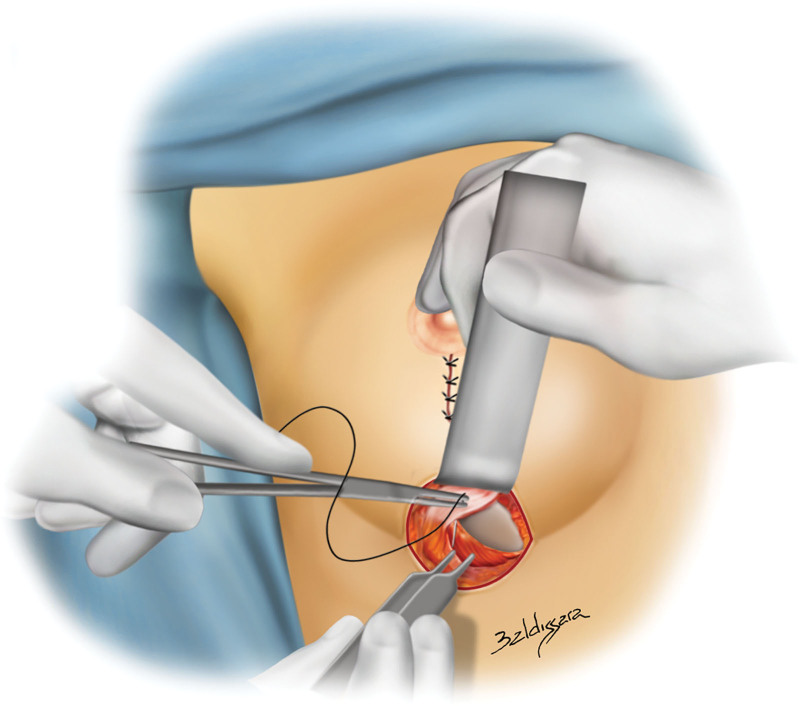
Fig. 4.
Subpectoral pocket being sealed. Sutures bite the posterior capsule (cranial) and the muscular sling (caudal) in the lateral aspect, and the posterior capsule (cranial) and spared muscular cuff (caudal) in the medial aspect.
Step 4: Mastopexy and Anterior Capsule Resection
Skin and parenchyma resection is performed according to markings. It is important to stress that although the anterior capsule should be removed entirely, the posterior capsule will persist as a continuous viable flap.7 Besides providing a tight pocket, this flap ensures that the implant remains completely sealed and also prevents the window-shading effect. The implant inferolateral aspect will be covered by the muscular sling and the posterior capsule, whereas the inferomedial portion will be covered solely by the posterior capsule flap (Figs. 5 and 6).
Fig. 5.
Posterior capsule is kept as a continuous viable tissue layer covering the pectoralis muscle surface and the implant inferomedial portion.
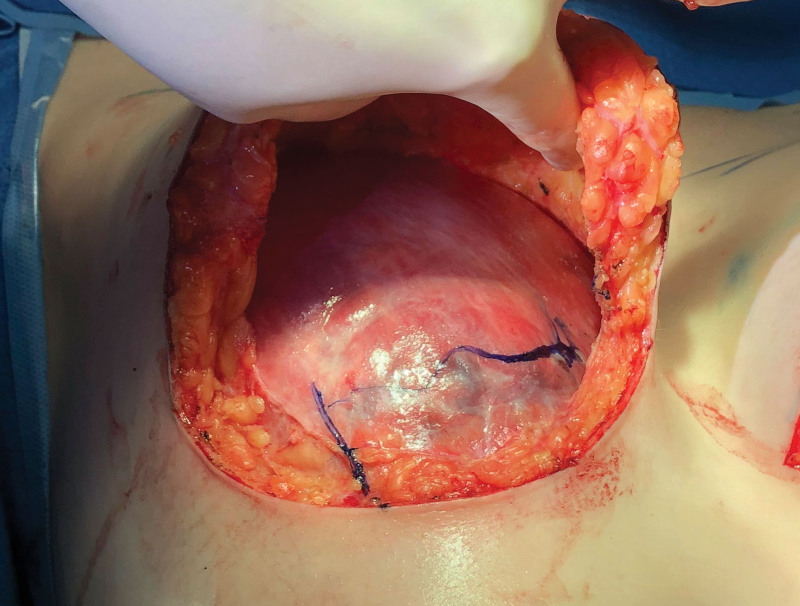
Fig. 6.
Intraoperative view of Figure 5. Subpectoral pocket and implant remain completely isolated from the mastopexy operative field. Blue marks outline the inferomedial aspect of the implant, which is covered by the posterior capsule layer only. After implant insertion but before mastopexy, the posterior capsule caudal border was sutured to the muscular sling laterally and to the muscular cuff medially.
If the remaining tissue on the retroareolar, lateral, or medial limbs is thicker than 2 cm, additional resection must be performed to prevent the snoopy nose deformity.6 Finally, the pillars are sutured medially, and the areolas are lifted, most commonly by rotation of superomedial pedicle areolar flaps. [See Video (online), which summarizes the key maneuvers of the four-step sequence for mastopexy with subglandular-to-subpectoral pocket conversion.]
Video. This video summarizes the key maneuvers of the four-step sequence for mastopexy with subglandular-to-subpectoral pocket conversion.
RESULTS
This technique was performed in 46 patients from March of 2017 to April of 2020. All patients were women aged 19 to 56 years (average age, 38.3 years); all had subglandular implants from previous augmentation or augmentation mastopexy.
In all cases, round silicone implants, identical in both breasts, were used. The average implant volume was 340.1 cc (range, 255 to 450 cc). Texturized surface implants accounted for most cases [microtexture, n = 20 (43 percent); macrotexture, n = 13 (28.2 percent)], whereas nanotexture (Motiva SilkSurface; Establishment Labs, Alajuela, Costa Rica) implants were used in 13 patients (28.2 percent).
Postoperative follow-up ranged from 2 to 37 months. All cases were photographically documented at preoperative and several postoperative stages (Figs. 7 and 8). (See Figure, Supplemental Digital Content 1, which shows a 54-year-old patient with previous subglandular Mentor Round HP Siltex 250-cc implants. Mastopexy was performed with Polytech Meme THS MESMOSensitive 360-cc implants. The patient is shown preoperatively and at 5-month follow-up, http://links.lww.com/PRS/E834. See Figure, Supplemental Digital Content 2, which shows a 45-year-old patient with previous subglandular Eurosilicone Round High Profile Cristalline 260-cc implants. Mastopexy was performed with Polytech Meme THS MESMOSensitive 360-cc implants. The patient is shown preoperatively and at 29-month follow-up. Notice dog-ear late removal scars, http://links.lww.com/PRS/E835.)
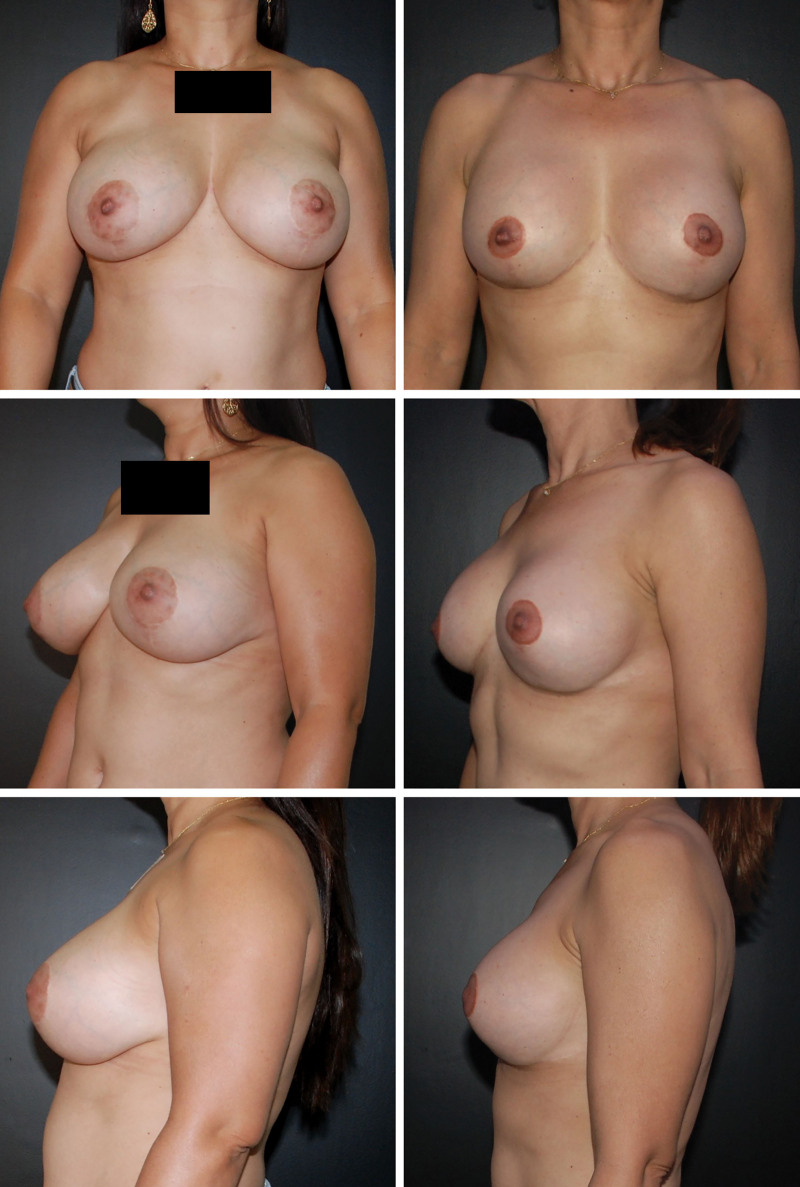
Fig. 7.
A 43-year-old patient with previous subglandular Perthese High Profile Micro-Texture 325-cc implants. Mastopexy was performed with Allergan CUI Round Full Height 300-cc implants. The patient is shown preoperatively and at 25-month follow-up.
Fig. 8.
A 46-year-old patient with previous subglandular Eurosilicone Round Ultra-High Profile Cristalline 300-cc implants. Mastopexy was performed with Mentor Round HP Siltex 300-cc implants. The patient is shown preoperatively and at 30-month follow-up. Despite significant weight loss, breast shape and position are stable.
In this series of 46 cases, no significant adverse health events or infections occurred. There were no cases of hematoma or nipple-areola complex ischemia. Seven patients required revision surgery (overall revision rate, 15.2 percent). The most common reoperation cause was dog-ear resection [n = 3 (6.5 percent)], followed by implant malposition [n = 2 (4.3 percent)], and one case of bottoming-out (2.17 percent) and one case of breast asymmetry (2.17 percent).
DISCUSSION
As the number of patients seeking breast surgery with silicone implants grows, secondary mastopexy is expected to be increasingly requested in the future. This approach uses previously described features such as a four-step rigid sequence, separated augmentation/mastopexy stages, minimal skin tension on sutures, implant inferior and lateral muscular support, tight implant pocket, and reduced implant exposure time. It also allows the surgeon to follow the 14-point plan8 for the new implant because the previous subglandular and the new subpectoral pockets do not communicate. The standardized sequence allows the average plastic surgeon to achieve predictable results with decreased risk of complications successfully.
The preserved posterior capsule directly covers the implant from the divided pectoralis caudal edge to the chest wall, which keeps the subglandular and the subpectoral pockets separated from each other, avoids the muscle window-shading effect, and prevents the implant from migrating to the subglandular space. The composite muscular/capsule flap supports the implant and offloads weight on the skin. Because the breast skin blood supply is somewhat impaired because of previous surgery, minimal skin tension on sutures adds safety to skin healing and contributes to more inconspicuous scars. Even if skin/parenchyma dehiscence occurs, a second independent viable tissue barrier protects the implant. The anterior capsule complete removal obviates the need for remnant subglandular pocket obliteration6–9 once it creates a raw surface for proper scarring.
The muscular sling stabilizes the implant, which helps maintain long-term upper pole fullness and decrease implant postoperative descent. Because the breast mound long-term position will not differ much from the postoperative one, the new nipple-areola complex position’s decision may be more reliable. The composite pocket is tight and has inferolateral support, which prevents implant dislocation and bottoming-out, and thus is useful for smooth/nanotexture surface implants.10
This approach requires the capsule not to be suspicious of any pathologic condition. The indication for total capsulectomy overrides the potential benefits of the muscular/capsule composite coverage. The composite pocket has a limited volume capacity. It is more difficult to keep adequate pocket stability when using larger than 400-cc implants.
In patients with too cranial pectoralis costal origins (fifth rib), it may not be possible to preserve the muscular sling because implants might stand too cranial on the thorax; however, the same standardized sequence may be applied.6 Because the new implant pocket is created through the inframammary fold, T-shaped scars will occur in all cases.
If the remaining parenchyma overlying the implants is too thick, there is a significant risk of undesired snoopy nose/waterfall effect. Adequate final parenchymal thickness is of utmost importance for good results; therefore, patients who are young/nulliparous or present with dense/bulky breasts are not ideal candidates.6 In contrast, patients who have previously undergone subglandular augmentation frequently already present with some degree of parenchymal atrophy, so aggressive parenchymal resection is a less common issue in nonprimary surgery.
The long-term subglandular implant pressure over the pectoralis surface may result in severe atrophy, sometimes to the point that the muscle might tear with stretching. Therefore, occasionally, the safer approach is a two-stage procedure—explant and mastopexy only, postponing implantation until the healing process is complete and muscular recovery has occurred. Patients should be previously warned about that possibility.
Despite a 15.2 percent overall reoperation rate, almost all of them (six of seven) occurred during the first 2 years performing the technique and were mainly related to refining expertise on managing the muscular sling technique (dog-ears and implant positioning). The reduction in revision rates resulted mainly from learning that the implant position will remain practically still, therefore: (1) no skin redundancy on the medial and lateral aspects will be forgiven (perform longer than usual transverse scars); and (2) the nipple-areola complex should be positioned higher than usual (do not count on the round-out effect of the lower pole). Also, the correct selection of suitable cases for the technique played a crucial role in lowering the revision rates (patients with dense/bulky breasts are poor candidates).
CONCLUSIONS
The standardized surgical sequence allows the average surgeon to fully concentrate on performing each staged, simpler task, not on the complex whole challenging procedure. As an increasing number of patients will seek secondary breast surgery, the importance of developing multiple surgical solutions is obvious. The technique presents some shortcomings (e.g., limited implant volume capacity) and requires specific conditions (e.g., the absence of capsular abnormality and the need for healthy pectoralis muscle). When the plan is to change the subglandular to a subpectoral implant pocket, and once the conditions allow, this approach is one valuable option to be considered, because it results in reliably good outcomes and produces low complication rates. Although we did not apply quantitative questionnaires to measure, the patient’s overall feedback is very positive. As with any other technique, other surgeons should perform it before it is possible to measure its reproducibility and effectiveness.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related digital media are available in the full-text version of the article on www.PRSJournal.com.
REFERENCES
- 1.Calobrace MB, Herdt DR, Cothron KJ. Simultaneous augmentation/mastopexy: A retrospective 5-year review of 332 consecutive cases. Plast Reconstr Surg. 2013;131:145–156. [DOI] [PubMed] [Google Scholar]
- 2.Beale EW, Ramanadham S, Harrison B, Rasko Y, Armijo B, Rohrich RJ. Achieving predictability in augmentation mastopexy. Plast Reconstr Surg. 2014;133:284e–292e. [DOI] [PubMed] [Google Scholar]
- 3.Spear SL, Boehmler JH, Clemens MW. Augmentation/mastopexy: A 3-year review of a single surgeon’s practice. Plast Reconstr Surg. 2006;118(Suppl):136S–147S; discussion 148S–149S, 150S–151S. [DOI] [PubMed] [Google Scholar]
- 4.Spear SL. Augmentation/mastopexy: “Surgeon, beware.” Plast Reconstr Surg. 2006;118(Suppl):133S–134S. [DOI] [PubMed] [Google Scholar]
- 5.Sarosiek K, Maxwell GP, Unger JG. Getting the most out of augmentation-mastopexy. Plast Reconstr Surg. 2018;142:742e–759e. [DOI] [PubMed] [Google Scholar]
- 6.Ono MT, Karner BM. Four-step augmentation mastopexy: Lift and augmentation at single time (LAST). Plast Reconstr Surg Glob Open. 2019;7:e2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown MH, Somogyi RB, Aggarwal S. Secondary breast augmentation. Plast Reconstr Surg. 2016;138:119e–135e. [DOI] [PubMed] [Google Scholar]
- 8.Deva AK, Adams WP, Jr, Vickery K. The role of bacterial biofilms in device-associated infection. Plast Reconstr Surg. 2013;132:1319–1328. [DOI] [PubMed] [Google Scholar]
- 9.Spear SL, Carter ME, Ganz JC. The correction of capsular contracture by conversion to “dual-plane” positioning: Technique and outcomes. Plast Reconstr Surg. 2006;118(Suppl):103S–113S; discussion 114S. [PubMed] [Google Scholar]
- 10.Atlan M, Nuti G, Wang H, Decker S, Perry T. Breast implant surface texture impacts host tissue response. J Mech Behav Biomed Mater. 2018;88:377–385. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.