Abstract
Background
The World Health Organization recommends mothers and infants be in direct skin-to-skin contact immediately after birth and initiate breastfeeding as soon as possible. Little is known in women with schizophrenia.
Methods
We conducted a population-based cohort study using administrative health data from Ontario, Canada (2012–2014), comparing women with (n = 471) and without schizophrenia (n = 218 435), and their infants, on the primary outcomes of any skin-to-skin contact and opportunity to initiate breastfeeding within the first 2 h after birth. For dyads with available data, secondary outcomes of intention to breastfeed, breastfeeding support, any breastmilk, and exclusive breastmilk at discharge were assessed. Modified Poisson regression was used to generate relative risks (aRR) and 95% confidence intervals (CI), adjusted for maternal age, parity, neighbourhood income, region of residence, smoking in pregnancy, and maternal medical and non-psychotic psychiatric comorbidity for all outcomes.
Results
Maternal schizophrenia was associated with lower likelihood of skin-to-skin contact (65.2% vs 78.1%; aRR 0.88, 95% CI: 0.82–0.94), and breastfeeding initiation post-delivery (38.9% vs 52.6% aRR 0.80, CI: 0.71–0.90) compared to dyads unexposed to maternal schizophrenia. Secondary outcomes followed a similar pattern. The magnitude of the effect was slightly less when restricting the cohort to full-term, vaginal deliveries, not admitted to NICU, and infant not discharged to social services.
Conclusions
Reduced maternal-infant skin-to-skin contact and breastfeeding initiation immediately after birth may significantly impact maternal–child bonding and the establishment breastfeeding in this population. Mothers with schizophrenia may require individualized support to promote these WHO recommended hospital practices in the early post-natal period.
Keywords: schizophrenia, skin-to-skin contact, initiation, breastfeeding
Introduction
The Baby Friendly Hospital Initiative (BFHI) has been developed by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) to promote positive hospital practices that support establishing exclusive breastfeeding in the immediate postpartum. As part of the 10 steps to successful breastfeeding, one of the recommendations is: “Facilitate immediate and uninterrupted skin-to-skin contact and support mothers to initiate breastfeeding as soon as possible after birth.” 1 Immediate skin-to-skin contact facilitates instinctive crawling and rooting reflexes in the infant, and prevents hypothermia.2,3 Early initiation of breastfeeding establishes the mother’s milk supply.1,4 Both are key to successful breastfeeding.1,5,6
Despite global initiatives to promote early skin-to-skin contact and breastfeeding initiation, a systematic review involving 35 studies from 28 countries found a wide range in prevalence of skin-to-skin contact after delivery of a full-term, healthy singleton infant (1–98%) with highly heterogeneous study designs and varying definitions of the construct.7 A systematic review of scientific studies and grey literature from a Lancet series on breastfeeding reported rates of initiation within 1 hour of birth in high-income countries with a range of 23–94%.8 There is variation in the rate and timing of skin-to-skin contact and the initiation of breastfeeding by sociodemographic and medical factors, with increased rates of both outcomes consistently observed among women with higher socioeconomic status, who are non-smoking and have given birth vaginally.9–11
Schizophrenia is a severe and typically persistent mental illness that affects almost 1 in 100 women, with onset during the reproductive years.12,13 Close to 50% of women with schizophrenia become mothers, but the extent of skin-to-skin contact and breastfeeding initiation in this population is largely unknown.14 Some women with schizophrenia may choose not to breastfeed their infants due to concerns around medication exposure through lactation, or as a means of protecting their own mental health stability.15,16 However, this population is also disproportionately affected by the risk factors for breastfeeding non-initiation detailed above. Due to the functional limitations associated with the disorder in terms of educational disruption and ability to work, women with schizophrenia have high rates of poverty.17 They are also at high risk for problems around the time of delivery that might delay or prevent skin-to-skin contact and breastfeeding initiation, including infant health complications, maternal medical and psychiatric complications, and early removal of the child from the mother’s custody.18–21
Knowledge about the extent to which breastfeeding initiation occurs in this population, and reasons for non-initiation are important for the design of supports and services that aim to ensure a healthy start in life for all children. Using data from a clinical maternity registry linked to health administrative data for the entire population of Ontario, Canada, this study provided the opportunity to measure rates of maternal-infant skin-to-skin contact and opportunity to initiate breastfeeding immediately after birth among maternal–infant dyads in this population, with comparison to unaffected women and children at the population level.
Methods
Study Design and Setting
This population-based study used provincial health databases housed securely at ICES in Ontario, Canada (www.ices.on.ca). These datasets were linked using unique encoded identifiers and analyzed at ICES. At ICES, a MOMBABY dataset, derived from administrative data captures all in-hospital deliveries in the Province (> 98% of all deliveries).22 Databases also comprise sociodemographic data via the Ontario Registered Persons Database (RPDB) (individual-level dates of birth, death, and postal codes of residence), hospitalization data via the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD, medical hospitalizations),23 and Ontario Mental Health Reporting System (OMHRS, inpatient psychiatric hospitalizations)24,25; outpatient billings and procedures via the Ontario Health Insurance Plan (OHIP).26
This study also leveraged linked data for fiscal years 2012–2014 from BORN, Ontario’s Better Outcomes Registry and Network (www.bornontario.ca), a clinical maternity registry covering Ontario, including detailed information such as maternal-infant skin-to-skin contact, and infant feeding during the birth hospitalization, with built-in checks (eg, automated algorithms, discrepancy reports) for verification at data entry. ICES and BORN have a Data Sharing Agreement permitting secure transfer of data linked at the individual maternal and infant levels (linkage success 93%). Clinical data are entered by hospital and midwifery staff during several health care encounters and are structured into infant-level and maternal-level datasets.
Participants
All live singleton deliveries occurring in-hospital in Ontario from April 1, 2012, to March 31, 2014, were considered. Dyads were excluded if data had invalid provincial identifiers, improbable dates of births, maternal age <15/≥50 years, unknown infant sex, and maternal or infant death prior to discharge from the delivery hospitalization. Deliveries that were linked to BORN, and for which data on the primary outcomes were entered were analyzed.
Maternal schizophrenia status was established using a validated algorithm comprising: (1) one or more hospitalizations or (2) 3 or more outpatient physician visits within 3 years, for schizophrenia or schizoaffective disorder (ICD-9 code: 295, or ICD-10 codes F20, F25) since database inception (1988 for hospitalization data, and 1992 for outpatient visits) and prior to the date of conception of the index pregnancy (sensitivity 90.1%, specificity 68.0%, positive predictive value 77.1%, and negative predictive value 88.7% for detecting a primary psychotic disorder in health administrative datasets compared with data abstracted from clinical charts).27 Those with psychotic diagnoses that did not reach the threshold for classification as schizophrenia as per the algorithm (eg, ICD-9 codes 297 or 298, ICD-10 codes F20.4, F22-F24, F28-F29, F53.1 or < 3 visits within 3 years) were not analyzed. All remaining mothers were classified as not having schizophrenia.
Outcomes
The Baby Friendly Hospital Initiative (BFHI), developed by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) was the framework for outcome selection.1 Step 4 of the revised BFHI recommends that all hospitals: “facilitate immediate and uninterrupted skin-to-skin contact and support mothers to initiate breastfeeding as soon as possible after birth.” The main outcomes for the current study were the two BORN variables that best approximated these recommendations: (1) any mother–infant skin-to-skin contact in the first 2 h after birth; (2) opportunity to initiate breastfeeding in first 2 h after delivery. Both outcomes were obtained from BORN infant level data. As secondary outcomes, additional variables were assessed from BORN maternal level datasets: (1) intention to breastfeed; (2) in-hospital assistance with breastfeeding within 6 h of delivery after initiation; (3) any breastmilk from birth to discharge from hospital, and (4) exclusive breastmilk from birth to discharge from hospital. For infants who received fluids other than breastmilk, reasons were recorded as: infant medical, maternal medical, or informed parent decision. The BORN data for “infant feeding at discharge” have been validated by re-abstraction from charts with 76.2% agreement and kappa scores of 0.67.28 Data have not been validated for skin-to-skin contact and breastfeeding initiation. Because data are entered separately into the different encounters of the BORN dataset, data were not available for all dyads on all secondary outcomes. For example, data on “infant feeding from birth to discharge” (ie, any breastmilk or exclusive breastmilk) was not recorded if an infant was born preterm, admitted to NICU or discharged elsewhere. If a mother and her infant were separated, for example ICU or NICU admission, data were not always entered on maternal level variables of breastfeeding support.
Covariates
Maternal socio-demographic characteristics were age, parity, neighborhood income quintile, and region of residence (rural regions < 10 000 individuals per square km) at the index birth (ICES datasets) and smoking in pregnancy (BORN).28 Medical morbidity in the 2 years pre-conception was measured in the ICES datasets using collapsed ambulatory diagnostic groups (CADGs) from the John Hopkins Adjusted Clinical Groups system (ACG®) (v10) to identify unstable chronic conditions.29 Non-schizophrenia maternal psychiatric comorbidity (mood/anxiety disorders, alcohol/substance use disorders, and “other”) in the 2 years prior to and during pregnancy was captured from inpatient and outpatient ICES datasets. Hospitalization records captured caesarean section and severe pregnancy complications, including pre-eclampsia, venous thromboembolism and other severe obstetric morbidities. Neonatal characteristics from the child’s birth record were child sex, preterm birth (<37 weeks), NICU admission, and child discharge to social services (ie, child custody loss) during at the birth hospitalization.
Analysis
Baseline characteristics of mother–infant dyads where the mother did and did not have a diagnosis of schizophrenia were described using proportions and where appropriate, means and standard deviations (SD). Modified Poisson regression estimated the relative risk (RR) and 95% confidence interval (CI) of each outcome in schizophrenia-exposed vs unexposed mother–infant dyads.30 Generalized estimating equations were used to account for clustering of multiple deliveries within women.31 RRs were adjusted for child sex (male/female), and potential confounders identified from the literature: maternal age at delivery, income quintile, rural/urban residence, smoking in pregnancy, maternal unstable chronic health conditions and psychiatric comorbidities documented in pregnancy or in the two years prior to conception.9–11,32
In an additional analyses of deliveries at low risk for maternal–infant separation at birth, the cohort was restricted to vaginal, full-term deliveries (> 37 weeks gestation), with infants neither admitted to NICU nor apprehended from the mother during the birth hospitalization.
Ethics Approval
Use of the data in this project is authorized under Section 45 of Ontario’s Personal Health Information Protection Act (PHIPA) and does not require review by a Research Ethics Board. This study was approved by the ICES privacy office (ICES logged study: 2020 0990 113 001). Data were analyzed at ICES using STATA MP 15.1. Due to privacy regulations, any cells with fewer than 6 participants were suppressed. As a prescribed entity under Ontario’s privacy legislation, ICES is authorized to collect and use health care data for the purposes of health system analysis, evaluation and decision support. Secure access to these data is governed by policies and procedures that are approved by the Information and Privacy Commissioner of Ontario.
Results
Characteristics
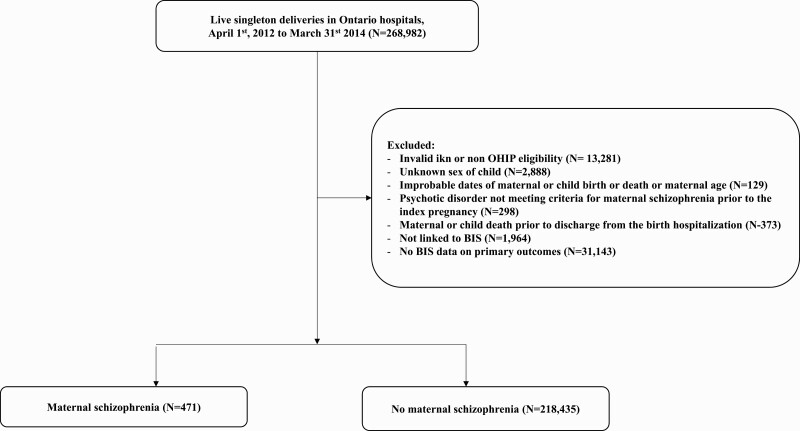
The final cohort comprised 218 906 mother–infant dyads, 471 (0.2%) with maternal schizophrenia and 218 435 (99.8%) without (figure 1). While there were no differences between the 2 groups in terms of maternal age and parity, mothers with schizophrenia were less likely to live in a rural area (8.3% vs 11.0%) and more likely to live in the lowest income quintile (38.0% vs 22.8%) (table 1). They were more likely to have medical morbidity (12.5% vs 8.2%) and non-schizophrenia psychiatric comorbidity (69.2% vs 14.4%), and to smoke in pregnancy (34.8% vs. 10.9%). Their infants were more likely to be born preterm (7.0% vs 5.8%), admitted to NICU (26.5% vs 12.4%) and apprehended during the birth hospitalization (7.0% vs 0.3%). Baseline characteristics were similar for those with (N = 31 143) and without (N = 218 906) missing data on the primary outcomes (table S1).
Fig. 1.
Cohort creation.
Table 1.
Characteristics of the Mothers and Their Children Included in the Study Cohort
| Maternal Schizophrenia (n = 471) | No Maternal Schizophrenia (n = 218 435) | |
|---|---|---|
| Sociodemographic characteristics | ||
| Mean (SD) maternal age at the index birth | 30.6 (±5.9) | 30.2 (±5.4) |
| Parity (primiparous) | 209 (44.4) | 95 313 (43.6) |
| Neighbourhood income quintile Q1 (lowest) | 179 (38.0) | 49 700 (22.8) |
| Rural residence at the index birth | 39 (8.3) | 23 945 (11.0) |
| Smoking during pregnancy | 164 (34.8) | 23 860 (10.9) |
| Infant sex (male) | 251 (53.3) | 112 049 (51.3) |
| Maternal psychiatric and medical history | ||
| Chronic unstable medical condition 2 years before pregnancy | 59 (12.5) | 17 971 (8.2) |
| Psychiatric diagnosis 2 years before or during pregnancy | ||
| Any (excluding psychotic disorder) | 326 (69.2) | 31 351 (14.4) |
| Mood disorder | 309 (65.6) | 29 694 (13.6) |
| Alcohol or substance use disorder | 37 (7.9) | 2251 (1.0) |
| Other (including personality disorders) | 59 (12.5) | 1162 (0.5) |
| Perinatal characteristics | ||
| Severe pregnancy complicationsa | 77 (16.4) | 27 770 (12.7) |
| Caesarean section | 147 (31.2) | 58 693 (26.9) |
| Preterm birth < 37 weeks’ gestation | 33 (7.0) | 12 690 (5.8) |
| Admitted to NICU in the index birth hospitalization | 125 (26.5) | 26 991 (12.4) |
| Child apprehension at birth | 33 (7.0) | 717 (0.3) |
All data are presented as a number (%) unless otherwise specified.
aComprises: pre-eclampsia, eclampsia, venous thromboembolism, severe obstetric morbidity (placental abruption, placental infarction, obstetric embolism, septic shock, uterine rupture) or systemic maternal complications in pregnancy or postpartum (cardiomyopathy, complications of anaesthesia, acute renal failure, MI/pulmonary enema, cerebrovascular disease, acute respiratory distress syndrome, DIC (disseminated intravascular coagulation), status epilepticus, hysterectomy.
Outcomes
Overall, immediately after birth, 78.1% (n = 170 905) of mother–infant dyads had skin-to-skin contact and 52.6% (n = 115 036) initiated breastfeeding. Compared to those with no schizophrenia, schizophrenia-exposed mother–infant dyads were less likely to have skin-to-skin contact (65.2% vs 78.1%, aRR 0.88, 95% CI 0.82–0.94) and to initiate breastfeeding (38.9% vs 52.6%, aRR 0.80, 95% CI 0.71–0.90) (table 2). Similarly for secondary outcomes, mothers who had schizophrenia were less likely to report the intent to breastfeed, to receive breastfeeding support, and there infants were less likely to have received either any breastmilk or exclusive breastmilk prior to discharge (table 2). Among infants who received breastmilk substitute in hospital, the most common reason reported was “informed parental decision to receive substitute,” endorsed for 90.3% (n = 149) and 92.6% (n = 61 550) of dyads where the mother did and did not have schizophrenia respectively, followed by “infant medical reasons” (9.1%, n = 15 vs 8.0%, n = 5309), and then “maternal medical reasons” (5.5%, n = 9 vs 1.5%, n = 976). In the additional analysis restricted to full-term infants delivered vaginally, not admitted to NICU, and not apprehended at birth, the direction of the effect was similar for all outcomes, although statistical significance was not always maintained (table 3).
Table 2.
Mother–Infant Skin-to-Skin Contact, Opportunity to Initiate Breastfeeding, and Secondary Breastfeeding Outcomes, Comparing Between Dyads Where the Mothers Had or Did Not Have Schizophrenia
| Variable | N (%) with Outcome | Relative Risk (95% CI) | Adjusted Relative Risk (95% CI) |
|---|---|---|---|
| Main outcomes | |||
| Skin-to-skin contact (first 2 h) | |||
| No maternal schizophrenia (n = 218 435) | 17 598 (78.1) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 471) | 307 (65.2) | 0.83 (0.78–0.90) | 0.88 (0.82–0.94) |
| Opportunity to initiate breastfeeding (first 2 h) | |||
| No maternal schizophrenia (n = 218 435) | 114 853 (52.6) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 471) | 183 (38.9) | 0.74 (0.66–0.83) | 0.80 (0.71–0.90) |
| Secondary outcomesa | |||
| Intention to breastfeed | |||
| No maternal schizophrenia (n = 20 314) | 191 882 (92.6) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 437) | 333 (76.2) | 0.83 (0.79–0.87) | 0.87 (0.82–0.91) |
| Breastfeeding support (first 6h) | |||
| No maternal schizophrenia (n = 190 442) | 111 495 (58.6) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 396) | 177 (44.7) | 0.76 (0.68–0.85) | 0.82 (0.73–0.91) |
| Any breastmilk prior to discharge | |||
| No maternal schizophrenia (n = 196 471) | 175 971 (89.6) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 351) | 261 (74.4) | 0.83 (0.78–0.89) | 0.87 (0.82–0.92) |
| Exclusive breastmilk at discharge | |||
| No maternal schizophrenia (n = 196 471) | 124 353 (63.3) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 351) | 171 (48.7) | 0.77 (0.69–0.86) | 0.85 (0.76–0.95) |
Adjusted for infant sex, maternal age at delivery, parity, income quintile, rurality, unstable chronic medical condition before pregnancy, co-morbid psychiatric diagnosis in the 2 years before or during pregnancy, smoking in pregnancy.
a Note: Data on all secondary outcomes were not available for all deliveries because data are entered separately into the different encounters of the BORN dataset and so not all dyads are eligible for all outcomes (eg, if an infant is transferred to NICU, data on infant feeding from birth to discharge from the hospital is not always entered).
Table 3.
Analysis Restricted to Full-Term Vaginal Deliveries, Where the Infant Was Not Admitted to NICU Nor Apprehended From the Mother During the Birth Hospitalization
| Variable | N (%) with Outcome | Relative Risk (95% CI) | Adjusted Relative Risk (95% CI) |
|---|---|---|---|
| Main outcomes | |||
| Skin-to-skin (first 2 h) | |||
| No maternal schizophrenia (n = 142 235) | 125 496 (88.2) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 247) | 205 (83.0) | 0.94 (0.89–0.99) | 0.95 (0.90–1.01) |
| Opportunity to initiate breastfeeding (first 2 h) | |||
| No maternal schizophrenia (n = 142 235) | 81 734 (57.5) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 247) | 122 (49.4) | 0.86 (0.76–0.98) | 0.90 (0.79–1.02) |
| Secondary outcomesa | |||
| Intention to breastfeed | |||
| No maternal schizophrenia (n = 135 385) | 126 101 (93.1) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 233) | 191 (82.0) | 0.90 (0.84–0.94) | 0.92 (0.87–0.97) |
| Breastfeeding support (first 6 h) | |||
| No maternal schizophrenia (n = 126 683) | 77 989 (61.6) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 218) | 113 (51.8) | 0.84 (0.74–0.96) | 0.88 (0.78–1.01) |
| Any breastmilk at discharge | |||
| No maternal schizophrenia (n = 136 994) | 123 810 (90.4) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 232) | 173 (74.6) | 0.83 (0.77–0.90) | 0.87 (0.80–0.93) |
| Exclusive breastmilk at discharge | |||
| No maternal schizophrenia (n = 136 994) | 94 795 (69.2) | 1.00 (referent) | 1.00 (referent) |
| Maternal schizophrenia (n = 232) | 120 (51.7) | 0.75 (0.67–0.86) | 0.82 (0.72–0.92) |
Adjusted for infant sex, maternal age at delivery, parity, income quintile, rurality, unstable chronic medical condition before pregnancy, co-morbid psychiatric diagnosis in the 2 years before or during pregnancy, smoking in pregnancy.
a Note: Data on all secondary outcomes were not available for all deliveries because data are entered separately into the different encounters of the BORN dataset and so not all dyads are eligible for all outcomes (eg, if an infant is transferred to NICU, data on infant feeding from birth to discharge from the hospital is not always entered).
Discussion
This population-based study is the first to investigate measures of early mother–infant skin-to-skin contact and initiation of breastfeeding in women with schizophrenia. We found mothers with schizophrenia were less likely to achieve early skin-to-skin contact and to initiate breastfeeding compared to those who were not diagnosed with schizophrenia. They reported lower rates of intention to breastfeed and received less support to breastfeed in hospital. These effects were only slightly dampened when excluding dyads where infants were born preterm, by caesarean section, admitted to the NICU or apprehended during the birth hospitalization, suggesting that “mother–infant separations” are not the only factor at play in the lower rates. Given the potential benefits of skin-to-skin contact and the early initiation of breastfeeding, further investigation into the reasons for these differences is needed to ensure the equitable provision of postnatal care to all women independent of mental health history.
While there are no comparable data for skin-to-skin contact and breastfeeding initiation in the birth hospitalisation in women with schizophrenia, a recent study in women with severe mental illness including schizophrenia showed that overall, most women with severe mental illness had the intention to breastfeed and of those, 76.5% did so.15 A systematic review of 48 studies examining the effect of maternal mental illness on breastfeeding outcomes found no association between antenatal depression and breastfeeding initiation.33 However, previous research has demonstrated women with a pre-pregnancy mental health visit are less likely to initiate breastfeeding (OR 0.61, 95% CI: 0.56–0.67),34 and a longitudinal cohort study found maternal anxiety had a significant negative effect on exclusive breastfeeding at 3 to 4 days postpartum.35 The functional impact of schizophrenia is for the most part greater than that seen among women with mood and anxiety disorders, therefore the stronger association seen herein is not surprising.17
As was anticipated, maternal characteristics associated with lower rates of breastfeeding initiation were more common in the schizophrenia group (eg, lower income, smoking during pregnancy),10,32 as were complications that might increase early maternal–child separation (eg, caesarean section, NICU admission, infant apprehension).9,11,21,36 Yet, these factors did not account for all the effect observed. We did not measure the level of psychotic symptoms postpartum, which may have necessitated maternal–infant separation, even if the infant was not eventually discharged to children’s services. Research has shown that women with schizophrenia are at risk for severe relapses in the early postpartum.20,37,38 Postpartum psychoses are severe illnesses, and could potentially lead to serious harm to mother and infant, so protecting the mother’s mental health is of paramount importance.39–42 As such, the rates of intention to breastfeed and assistance with breastfeeding were much lower in this group, which may be appropriate due to concerns around sleep deprivation and the challenges of breastfeeding exacerbating symptoms,43 or concerns about adverse effects from medications used to manage schizophrenia and schizoaffective disorder such as antipsychotics and mood stabilizers, including side effects such as drowsiness in the mother and adverse effects in the infant. Due to the diagnosis of schizophrenia, even in the absence of psychotic symptoms however, staff may have been reluctant to leave mothers alone with their infants, potentially delaying breastfeeding initiation. However, even if women with schizophrenia choose not to breastfeed, these dyads may benefit from early mother–infant skin-to-skin contact. Skin-to-skin contact is an integral part of developing the early mother–infant bond, fostering later healthy mother–infant attachment relationships.44–46 Biological benefits of early mother–infant skin-to-skin contact for the infant may include sleep, heart rate, glycemic, and temperature regulation.44,47,48 Benefits to the mother, include vagal stimulation release of oxytocin and regulation of the autonomic nervous system.49–51 Studies have also shown a protective effect for postpartum depression, but this has not been explored in the context of relapse prevention among women with schizophrenia.52,53 Further, while antipsychotics and mood stabilizers do pass into breastmilk and data on both short- and long-term effects remain limited, many are compatible with breastfeeding.54–57 Recent qualitative research has highlighted contradicting and mixed advice from health professionals regarding medication as well as lack of support or prioritization of intentions to breastfeed in women with severe mental illness.15 It is important to ensure that counselling about, and assistance with, breastfeeding, is equitably provided to this group, so as to maximize skin-to-skin contact and breastfeeding initiation when appropriate, particularly as women with schizophrenia may lack family support, which is vital to support mother and infant post-delivery.32,58–60
Strengths of our study include a population-based cohort with detailed clinical maternity data covering the whole of Ontario, Canada. Population coverage means high external validity. Use of the BORN registry enabled investigation of measures not available in administrative data that were better proxies for the WHO recommendations than what has been reported in many prior studies.7,8,33 However, these data are not collected for research, data were missing on some outcome variables, and we were not able to ascertain the exact reasons for lack of skin-to-skin contact or non-initiation of breastfeeding in many cases. Further, covariates we could not measure, such as maternal education, ethnicity, gender, medication exposures, and hospital-level data such as cluster-level breastfeeding outcomes and specific policies aimed at BF support, might have helped better contextualize the study findings. There was no information on partner support, also an established predictor of breastfeeding outcomes.32
Maternal-infant skin-to-skin contact and feeding initiation may have implications for a child’s health and development. Due to the nature of their illness and its treatments, mothers with schizophrenia may require individualized counselling and support from care providers to optimize their rates of skin-to-skin contact and feeding initiation. Research on the BFHI has shown positive outcomes among other vulnerable groups, for example socio-economically disadvantaged mothers who may not be able to access to out-of-pocket lactation support services once they leave hospital.61,62 Recommendations for supporting these mother–infant dyads include encouraging obstetricians and mental health teams to provide prenatal education and encouragement to women. Providing additional education to obstetrical teams about the range of clinical presentations with which women with severe mental illness may present in the perinatal period may also help increase opportunities for skin-to-skin contact and initiation of breastfeeding when appropriate. Changes in hospital policy to lengthen post-delivery stays for mothers with schizophrenia to monitor their mental health and encourage early mother–infant bonding might also be important in this vulnerable group. Further research on the mechanisms underlying our study findings will help determine the extent and nature of future efforts to optimize skin-to-skin contact and breastfeeding rates in women with schizophrenia, and their children.
Supplementary Material
Acknowledgments
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). This study also received funding from the Canadian Institute of Health Research (CIHR PJT-156021). Parts of this material are based on data and/or information compiled and provided by the MOH and the Canadian Institute for Health Information (CIHI). The analyses, conclusions, opinions and statements expressed herein are those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. This Study is based in part on data provided by Better Outcomes Registry and Network (“BORN”), part of the Children’s Hospital of Eastern Ontario. The interpretation and conclusions contained herein do not necessarily represent those of BORN Ontario. CT, HB, NS, LB, SC, CLD, EC, JR have no conflict of interest. SV reports royalties from authorship of materials related to depression and pregnancy from UpToDate, Inc. Material preparation, data collection, and analysis were performed by Dr Clare Taylor and Simon Chen. The first draft of the manuscript was written by Dr Clare Taylor and Dr Simone Vigod and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by (1) funding from the Canadian Institute of Health Research (CIHR PJT-156021) and (2) Shirley A. Brown Memorial Chair for Women’s Mental Health Research.
References
- 1. World Health Organization. Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative. Geneva: World Health Organization, 2018. [Google Scholar]
- 2. Safari K, Saeed AA, Hasan SS, Moghaddam-Banaem L. The effect of mother and newborn early skin-to-skin contact on initiation of breastfeeding, newborn temperature and duration of third stage of labor. Int Breastfeed J. 2018;13:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Widström AM, Brimdyr K, Svensson K, Cadwell K, Nissen E. Skin-to-skin contact the first hour after birth, underlying implications and clinical practice. Acta Paediatr. 2019;108(7):1192–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bergman J, Bergman N. Whose choice? Advocating birthing practices according to baby’s biological needs. J Perinat Educ. 2013;22(1):8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews 2016;11:CD003519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bigelow AE, Power M, Gillis DE, Maclellan-Peters J, Alex M, McDonald C. Breastfeeding, skin-to-skin contact, and mother-infant interactions over infants’ first three months. Infant Ment Health J. 2014;35(1):51–62. [DOI] [PubMed] [Google Scholar]
- 7. Abdulghani N, Edvardsson K, Amir LH. Worldwide prevalence of mother-infant skin-to-skin contact after vaginal birth: a systematic review. PLoS One. 2018;13(10):e0205696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Victora CG, Bahl R, Barros AJ, et al. ; Lancet Breastfeeding Series Group . Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490. [DOI] [PubMed] [Google Scholar]
- 9. Chalmers B, Kaczorowski J, Darling E, et al. ; Maternity Experiences Study Group of the Canadian Perinatal Surveillance System . Cesarean and vaginal birth in canadian women: a comparison of experiences. Birth. 2010;37(1):44–49. [DOI] [PubMed] [Google Scholar]
- 10. Cohen SS, Alexander DD, Krebs NF, et al. Factors associated with breastfeeding initiation and continuation: a meta-analysis. J Pediatr. 2018;203:190–196.e121. [DOI] [PubMed] [Google Scholar]
- 11. Redshaw M, Hennegan J, Kruske S. Holding the baby: early mother-infant contact after childbirth and outcomes. Midwifery. 2014;30(5):e177–e187. [DOI] [PubMed] [Google Scholar]
- 12. Goldner EM, Hsu L, Waraich P, Somers JM. Prevalence and incidence studies of schizophrenic disorders: a systematic review of the literature. Can J Psychiatry. 2002;47(9):833–843. [DOI] [PubMed] [Google Scholar]
- 13. Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1211–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vigod SN, Seeman MV, Ray JG, et al. Temporal trends in general and age-specific fertility rates among women with schizophrenia (1996–2009): a population-based study in Ontario, Canada. Schizophr Res. 2012;139(1–3):169–175. [DOI] [PubMed] [Google Scholar]
- 15. Baker N, Potts L, Jennings S, Trevillion K, Howard LM. Factors affecting infant feeding practices among women with severe mental illness. Front Glob Women’s Health. 2021;2:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Seeman MV. Clinical interventions for women with schizophrenia: pregnancy. Acta Psychiatr Scand. 2013;127(1):12–22. [DOI] [PubMed] [Google Scholar]
- 17. Häfner H, Maurer K, Trendler G, an der Heiden W, Schmidt M. The early course of schizophrenia and depression. Eur Arch Psychiatry Clin Neurosci. 2005;255(3):167–173. [DOI] [PubMed] [Google Scholar]
- 18. Park JM, Solomon P, Mandell DS. Involvement in the child welfare system among mothers with serious mental illness. Psychiatr Serv. 2006;57(4):493–497. [DOI] [PubMed] [Google Scholar]
- 19. Seeman MV. Intervention to prevent child custody loss in mothers with schizophrenia. Schizophr Res Treat. 2012; doi: 10.1155/2012/796763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Taylor CL, Stewart RJ, Howard LM. Relapse in the first three months postpartum in women with history of serious mental illness. Schizophr Res. 2019;204:46–54. [DOI] [PubMed] [Google Scholar]
- 21. Vigod SN, Kurdyak PA, Dennis CL, et al. Maternal and newborn outcomes among women with schizophrenia: a retrospective population-based cohort study. BJOG. 2014;121(5):566–574. [DOI] [PubMed] [Google Scholar]
- 22. Maaten S, Guttman A, Kopp A, Handa M, Jaakkimainen L. Care of women during pregnancy and childbirth. In: Jaakkimainen L, Upshur R, Klein-Geltink JE, et al. , eds. Primary Care in Ontario ICES Atlas Toronto: Institute for Clinical Evaluative Sciences. 2006:15–34. [Google Scholar]
- 23. Juurlink D, Preyra C, Croxford R, et al. Canadian institute for health information discharge abstract database: a validation study. In: ICES Investigative Report Institute for Clinical Evaluative Sciences, Toronto. 2006. [Google Scholar]
- 24. Hirdes JP, Marhaba M, Smith TF, et al. ; Resident Assessment Instrument-Mental Health Group . Development of the Resident Assessment Instrument–Mental Health (RAI-MH). Hosp Q. 2000;4(2):44–51. [DOI] [PubMed] [Google Scholar]
- 25. Hirdes JP, Smith TF, Rabinowitz T, et al. ; Resident Assessment Instrument-Mental Health Group . The Resident Assessment Instrument-Mental Health (RAI-MH): inter-rater reliability and convergent validity. J Behav Health Serv Res. 2002;29(4):419–432. [DOI] [PubMed] [Google Scholar]
- 26. Williams J, Young W. A summary of studies on the quality of health care administrative databases in Canada. In: Patterns of Health Care in Ontario: the ICES Practice Atlas. Vol 2. 2nd ed. Ottawa: Canadian Medical Association; 1996:45. [Google Scholar]
- 27. Kurdyak P, Lin E, Green D, Vigod S. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry. 2015;60(8):362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dunn S, Lanes A, Sprague AE, et al. Data accuracy in the Ontario birth registry: a chart re-abstraction study. BMC Health Serv Res. 2019;19(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johns Hopkins University. The Johns Hopkins ACG System: technical reference guide version 10.0, 2013. https://www.hopkinsacg.org/document/acg-system-version-10-0-technical-reference-guide/. Accessed January 16, 2021.
- 30. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 31. Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22(6):661–670. [DOI] [PubMed] [Google Scholar]
- 32. Dennis CL. Breastfeeding initiation and duration: A 1990-2000 literature review. J Obstet Gynecol Neonatal Nurs. 2002;31(1):12–32. [DOI] [PubMed] [Google Scholar]
- 33. Dias CC, Figueiredo B. Breastfeeding and depression: a systematic review of the literature. J Affect Disord. 2015;171:142–154. [DOI] [PubMed] [Google Scholar]
- 34. Wouk K, Stuebe AM, Meltzer-Brody S. Postpartum mental health and breastfeeding practices: an analysis using the 2010–2011 Pregnancy Risk Assessment Monitoring System. Matern Child Health J. 2017;21(3):636–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wallwiener S, Müller M, Doster A, et al. Predictors of impaired breastfeeding initiation and maintenance in a diverse sample: what is important? Arch Gynecol Obstet. 2016;294(3):455–466. [DOI] [PubMed] [Google Scholar]
- 36. Haiek LN. Measuring compliance with the baby-friendly hospital initiative. Public Health Nutr. 2012;15(5):894–905. [DOI] [PubMed] [Google Scholar]
- 37. Munk-Olsen T, Laursen TM, Mendelson T, Pedersen CB, Mors O, Mortensen PB. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66(2):189–195. [DOI] [PubMed] [Google Scholar]
- 38. Rochon-Terry G, Gruneir A, Seeman MV, et al. Hospitalizations and emergency department visits for psychiatric illness during and after pregnancy among women with schizophrenia. J Clin Psychiatry. 2016;77(4):541–547. [DOI] [PubMed] [Google Scholar]
- 39. Austin MP, Kildea S, Sullivan E. Maternal mortality and psychiatric morbidity in the perinatal period: challenges and opportunities for prevention in the Australian setting. Med J Aust. 2007;186(7):364–367. [DOI] [PubMed] [Google Scholar]
- 40. Cantwell R, Clutton-Brock T, Cooper G, et al. Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer: 2006–2008. The Eighth Report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG. 2011;118:1–205. [DOI] [PubMed] [Google Scholar]
- 41. Jones I, Chandra PS, Dazzan P, Howard LM. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014;384(9956):1789–1799. [DOI] [PubMed] [Google Scholar]
- 42. Spinelli MG. Maternal infanticide associated with mental illness: prevention and the promise of saved lives. Am J Psychiatry. 2004;161(9):1548–1557. [DOI] [PubMed] [Google Scholar]
- 43. Da Silva Tanganhito D, Bick D, Chang YS. Breastfeeding experiences and perspectives among women with postnatal depression: a qualitative evidence synthesis. Women Birth. 2020;33(3):231–239. [DOI] [PubMed] [Google Scholar]
- 44. Norholt H. Revisiting the roots of attachment: a review of the biological and psychological effects of maternal skin-to-skin contact and carrying of full-term infants. Infant Behav Dev. 2020;60:101441. [DOI] [PubMed] [Google Scholar]
- 45. Gibbs BG, Forste R, Lybbert E. Breastfeeding, parenting, and infant attachment behaviors. Matern Child Health J. 2018;22(4):579–588. [DOI] [PubMed] [Google Scholar]
- 46. Peñacoba C, Catala P. Associations between breastfeeding and mother–infant relationships: a systematic review. Breastfeed Med. 2019;14(9):616–629. [DOI] [PubMed] [Google Scholar]
- 47. Rollins NC, Bhandari N, Hajeebhoy N, et al. ; Lancet Breastfeeding Series Group . Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387(10017):491–504. [DOI] [PubMed] [Google Scholar]
- 48. Chiruvolu A, Miklis KK, Stanzo KC, et al. Effects of skin-to-skin care on late preterm and term infants at-risk for neonatal hypoglycemia. Pediatr Qual Saf. 2017;2(4):e030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Uvänas-Moberg K, Arn I, Magnusson D. The psychobiology of emotion: the role of the oxytocinergic system. Int J Behav Med. 2005;12(2):59–65. [DOI] [PubMed] [Google Scholar]
- 50. Uvnäs-Moberg K. Oxytocin may mediate the benefits of positive social interaction and emotions. Psychoneuroendocrinology. 1998;23(8):819–835. [DOI] [PubMed] [Google Scholar]
- 51. Winberg J. Mother and newborn baby: mutual regulation of physiology and behavior–a selective review. Dev Psychobiol. 2005;47(3):217–229. [DOI] [PubMed] [Google Scholar]
- 52. Badr HA, Zauszniewski JA. Kangaroo care and postpartum depression: the role of oxytocin. Int J Nurs Sci. 2017;4(2):179–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Scime NV, Gavarkovs AG, Chaput KH. The effect of skin-to-skin care on postpartum depression among mothers of preterm or low birthweight infants: a systematic review and meta-analysis. J Affect Disord. 2019;253:376–384. [DOI] [PubMed] [Google Scholar]
- 54. Betcher HK, Montiel C, Clark CT. Use of antipsychotic drugs during pregnancy. Curr Treat Options Psychiatry. 2019;6(1):17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gentile S. Neurodevelopmental effects of prenatal exposure to psychotropic medications. Depress Anxiety. 2010;27(7):675–686. [DOI] [PubMed] [Google Scholar]
- 56. Uguz F. Second-generation antipsychotics during the lactation period: a comparative systematic review on infant safety. J Clin Psychopharmacol. 2016;36(3):244–252. [DOI] [PubMed] [Google Scholar]
- 57. Uguz F, Sharma V. Mood stabilizers during breastfeeding: a systematic review of the recent literature. Bipolar Disord. 2016;18(4):325–333. [DOI] [PubMed] [Google Scholar]
- 58. Amiel Castro RT, Glover V, Ehlert U, O’Connor TG. Antenatal psychological and socioeconomic predictors of breastfeeding in a large community sample. Early Hum Dev. 2017;110:50–56. [DOI] [PubMed] [Google Scholar]
- 59. Taylor CL, Stewart R, Ogden J, Broadbent M, Pasupathy D, Howard LM. The characteristics and health needs of pregnant women with schizophrenia compared with bipolar disorder and affective psychoses. BMC Psychiatry. 2015;15:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Jeong Y-J, Nho J-H, Kim HY, Kim JY. Factors influencing quality of life in early postpartum women. Int J Environ Res Public Health 2021;18(6):2988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Balogun OO, O’Sullivan EJ, McFadden A, et al. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev. 2016;11:CD001688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Munn AC, Newman SD, Mueller M, Phillips SM, Taylor SN. The impact in the United States of the baby-friendly hospital initiative on early infant health and breastfeeding outcomes. Breastfeed Med. 2016;11:222–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.