Abstract
Purpose: We assessed the perceptions and practices of physical activity counselling and exercise prescription of physiotherapists in Nova Scotia. Method: A total of 146 physiotherapists in Nova Scotia completed an online self-reflection survey regarding their current practice of, confidence in, barriers to, and facilitators of providing physical activity and exercise (PAE) counselling to their patients. Results: Physiotherapists included physical activity counselling and exercise content in 85% of patient counselling appointments. They reported a high level of confidence (> 90%) in providing PAE information and answering patients’ PAE questions and moderate confidence in their patients’ abilities to maintain PAE over the long term (73%) and to follow through on their PAE recommendations (66%). Patients’ interest in PAE was the greatest barrier to providing PAE counselling. The physiotherapists reported being most comfortable when prescribing exercise for patients with musculoskeletal conditions and least comfortable with patients with cancer, insulin-dependent diabetes, and respiratory conditions. Most physiotherapists (71%) reported being interested in pursuing further education or training in PAE counselling and prescription. Conclusions: The physiotherapists frequently recommended PAE to their patients, had moderate confidence in their patients’ ability to follow through on their advice, and experienced patients’ disinterest in PAE as the greatest barrier to providing PAE counselling. The results of this study suggest a desire by physiotherapists for educational training opportunities, which we recommend be focused on providing behavioural strategies and further information to help overcome patient-focused barriers; this will help patients adopt and maintain physically active lifestyles.
Key Words: counselling, exercise therapy, prescriptions
Abstract
Objectif : évaluer les perceptions et les pratiques des physiothérapeutes de la Nouvelle-Écosse en matière de conseils sur l’activité physique et de prescription d’exercice. Méthodologie : au total, 146 physiothérapeutes de la Nouvelle-Écosse ont rempli un sondage d’autoréflexion en ligne sur les conseils qu’ils donnent à leurs patients en matière d’activité physique et d’exercice (APE) à leurs patients, leur confiance, les obstacles et les incitations à cet égard. Résultats : les physiothérapeutes incluaient des conseils en matière d’activité physique et un contenu d’exercice lors de 85 % des rendez-vous de conseils aux patients. Ils déclaraient un taux de confiance élevé (> 90 %) quant à l’information en matière d’APE et aux réponses aux questions des patients à ce sujet, et un taux de confiance modéré envers les capacités de leurs patients à maintenir leur APE à long terme (73 %) et à donner suite à leurs recommandations en matière d’APE (66 %). L’intérêt des patients envers l’APE était le principal obstacles aux conseils sur l’APE. Les physiothérapeutes ont déclaré être plus à l’aise de prescrire des exercices aux patients ayant des affections musculosquelettiques, mais moins à l’aise auprès des patients atteints de cancer, de diabète insulinodépendant et de troubles respiratoires. La plupart des physiothérapeutes (71 %) déclaraient souhaiter poursuivre leur formation sur les conseils et la prescription d’APE. Conclusions : les physiothérapeutes recommandaient fréquemment l’APE à leurs patients, avaient une confiance modérée dans les capacités de leurs patients à donner suite à leurs conseils et trouvaient que le désintérêt de leurs patients envers l’APE était le principal obstacle aux conseils en matière d’APE. Selon les résultats de cette étude, les physiothérapeutes souhaitent pouvoir suivre des formations. Les auteurs recommandent qu’elles portent sur des stratégies comportementales et sur l’information plus approfondie pour vaincre les obstacles liés aux patients, car ces stratégies aideront les patients à adopter et à maintenir un mode de vie actif.
Mots-clés : : conseils, prescription, thérapie par l’exercice
Despite the health benefits of leading a physically active lifestyle,1 only 15% of the Canadian population achieve the Canadian recommendation of 150 minutes of moderate- to vigorous-intensity physical activity every week.2 Compared with the rest of Canada, Nova Scotia has higher rates of obesity, cancer, diabetes, high blood pressure, and heart disease.3 Considering that the proportion of the population with chronic disease is increasing,3 promoting healthy lifestyle habits such as physical activity and exercise (PAE) are needed. Exercise is Medicine Canada is a multidisciplinary initiative aimed at providing national leadership in promoting physical activity as a chronic disease prevention and management strategy. Its objective is to have more health care providers across all professions assess, counsel, and prescribe PAE to their patients.4
To date, most of the literature has focused on physicians as promoters of PAE because of their frequent interactions with the public and the public’s perception that they provide credible health-related information.5–7 The role of physiotherapists as promoters of PAE is understudied, despite the fact that they are well informed about the benefits of a physically active lifestyle and that they incorporate PAE into their own daily practice.8,9 For example, 99% of physiotherapists from British Columbia reported personally meeting the PA guidelines; this is a much higher percentage than the Canadian adult population as a whole.10
The primary function of physiotherapists, as outlined by the Canadian Physiotherapy Association, is to
utilize diagnostic and assessment procedures and tools in order to develop and implement preventive and therapeutic courses of intervention. They apply a collaborative and reasoned approach to help clients achieve their health goals, in particular focusing on the musculoskeletal, neurological, cardiorespiratory, and multi-systems.11(p.2)
Physiotherapists are in an opportune position to promote PAE to a large proportion of the population because of their background education and public reach; their engagement in regular PAE promotion is particularly needed in Nova Scotia where rates of chronic disease are disproportionately high.
Important research that investigated the opinions and practices of physiotherapists in Australia demonstrated that they are well aware that they serve a role as PAE promoters: 95% of the respondents agreed that discussing the benefits of a physically active lifestyle with patients was part of a physiotherapist’s role, and 54% reported encouraging more than 10 patients per month to lead a physically active lifestyle.12 Lau and colleagues reported that 85% of physiotherapists discussed the health benefits of exercise with their stroke patients, although only 36% included community exercise education for more than 7 out of 10 patients with stroke.13 Other Australian research has shown that patients who received behavioural education on PAE from a physiotherapist were approximately three times more likely to increase their physical activity levels by at least 60 minutes per week compared with a control group.14
Despite physiotherapists’ skills and knowledge, barriers such as lack of time limit their ability to provide a PAE plan that falls within patients’ expectations, motivations, and goals while also managing the reason for the initial visit.15 A systematic review of the barriers to treatment adherence in physiotherapy outpatient clinics noted an absence of studies evaluating physiotherapists’ barriers.16 The current experience of Canadian physiotherapists in PAE counselling and prescription practices and the barriers they experience in providing such services are not fully described in the literature.
The purpose of this study was to assess the perceptions and practices of PAE counselling and prescription of physiotherapists across Nova Scotia.
Methods
Participants
Health care providers across Nova Scotia completed an online province-wide survey (FluidSurveys, Ottawa, ON), as part of an Exercise is Medicine Nova Scotia initiative led by the Nova Scotia Health Authority’s (NSHA’s) Office of Research and Innovation and Acadia University, with endorsement by many provincial organizations, including Doctors Nova Scotia and the Nova Scotia College of Physiotherapists. The survey was adapted from previous work in the area,17–19 edited, beta tested, and approved by the Exercise is Medicine Nova Scotia Steering Committee, which is composed of representatives from NSHA, provincial organizations, and research experts in the area. It was distributed to various groups of health care providers (e.g., physicians, nurses, physiotherapists) through NSHA and the respective provincial associations. The Nova Scotia College of Physiotherapists distributed links to the survey through their employee emails and online newsletters.
All procedures were approved by the Acadia University and NSHA research ethics boards, and all participants provided electronic consent for secondary use of anonymous group data analysis before completing the online survey.
Physiotherapists’ perception and practice questionnaire
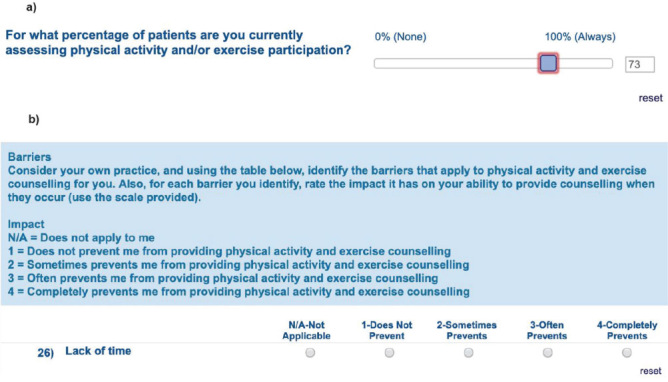
We developed the self-reflection questions in line with previous physical activity prescription questionnaires in health care.7,17–19 No personal information was required to complete the questionnaire. In brief, the questions addressed demographics, practice history, efficacy, barrier impact, and facilitator impact. Questions about demographic characteristics, current practice history, and barriers were based on previous research in diabetes education.20,21 Practice history and efficacy variables were collected using visual analogue scales ranging from 0% to 100%. Example survey questions are provided in the Appendix.
Multiple domains of self-efficacy (e.g., confidence in ability to provide information, prescribe exercise, make appropriate referrals) were quantified separately from other efficacy domains (such as participants’ confidence in their patients’ ability to follow through on their recommendations). Data on the impact of barriers and facilitators were collected using an ordinal scale ranging from 1 to 4; lower values indicated a barrier or a facilitator that had a weak impact on ability to provide PAE counselling (e.g., 1 = does not prevent me from counselling). A higher barrier or facilitator value indicated that a variable prevented providing PAE counselling (4 = completely prevents me from counselling). (See the Appendix.) Conversely, a higher facilitator value indicated that a variable made it very easy to complete a PAE practice.
Participants were asked to identify (yes or no) whether they would be interested in receiving further PA education or training in counselling and exercise prescription. Knowledge was assessed using a five-point ordinal scale (not at all, slightly, moderately, very, extremely). Any difficulty they had encountered incorporating PA counselling into their patient sessions was also assessed using a five-point ordinal scale (not at all difficult, slightly difficult, somewhat difficult, difficult, very difficult). They were also given a list of common diseases or conditions and asked to select the ones for which they were least comfortable and most comfortable providing PAE advice to patients: cancer, cardiovascular disease, diabetes requiring insulin or secretagogue, diabetes not requiring insulin or secretagogue, hypertension, mental health, obesity, osteoarthritis, osteoporosis, other musculoskeletal conditions (e.g., low back pain), and respiratory disease. Participants were also given the option to add other conditions not on the list.
Data analysis and statistical analysis
The physiotherapists’ current practices and demographics were recorded as mean (SD) and range, where appropriate. Physiotherapists’ confidence in providing PAE information, assessing PAE readiness, answering patients’ questions about PAE, helping patients maintain PAE over the long term, assessing patients’ safety before starting PAE, providing advice about PAE to those with special considerations, and making appropriate referrals to PAE, as well as their confidence that their patients would follow through, are presented as mean (SD) with 95% CIs. The proportion of physiotherapists who identified each barrier and facilitator variable is presented as a percentage and the impact value as mean (SD). Physiotherapists’ knowledge of PAE counselling, knowledge of exercise prescription, difficulty providing PAE counselling in patient sessions, and interest in future PAE education or training are presented as proportional data (%). Each disease condition about which physiotherapists reported being most and least comfortable providing PAE advice is presented as proportional data (% of respondents).
Results
The survey was completed by 146 physiotherapists. According to the Nova Scotia College of Physiotherapists Annual Report for 2016, 612 physiotherapists were working in Nova Scotia that year;22 this indicates that our survey had an estimated response rate of 23.9%.
Demographic characteristics
The sample was predominantly Caucasian (94% of respondents) and female (81% of respondents). Participants were 44 (SD 11) years of age (range: 25–70) and had worked in their field for 19 (SD 12) years (range: 1–48). Many reported working in general practice (35%) or with people with musculoskeletal disorders (40%). Most respondents saw fewer than 15 patients per day (81%), and half spent more than 20 minutes per patient (50%).
Physical activity counselling and exercise prescription: practices
The participants reported incorporating PAE counselling and prescription into patient treatment sessions 89% (SD 17) of the time. They reported assessing PAE participation in 85% (SD 23) of their patients, assessing PAE readiness in 74% (SD 31), recommending PAE to 93% (SD 13), and providing written exercise prescriptions for 86% (SD 20). They indicated that they referred to other qualified exercise professionals or facilities for additional exercise assessment and counselling for 27% (SD 27) of their patients. Most (71%) identified an interest in obtaining further education or training in PAE counselling and prescription.
Physical activity counselling and exercise prescription: knowledge and confidence
Most participants rated their understanding of PAE counselling and prescription as very or extremely knowledgeable (counselling, 82%; prescription, 83%). Two-thirds (67%) reported experiencing no difficulty incorporating PAE counselling and prescription into their patient treatment sessions.
As shown in Table 1, physiotherapists reported a very high level of confidence (> 90%) in providing PAE information and answering patients’ questions about PAE (indicating self-efficacy). Overall, they reported high confidence in helping their patients maintain PAE and moderate confidence in their patients’ ability to follow through on their PAE recommendations (indicating other efficacy).
Table 1 .
Level of Confidence in Providing Components of Physical Activity Counselling and Exercise Prescription
| Component | Mean % (SD); 95% CI |
|---|---|
| Provide PAE information (n = 146) | 96.6 (8.4); 95, 98 |
| Assess PAE readiness (n = 142) | 83.2 (19.9); 80, 87 |
| Answer patients’ PAE questions (n = 146) | 93.3 (8.5); 92, 95 |
| Assess patients’ safety before providing PAE (n = 145) | 88.7 (14.0); 86, 91 |
| Provide PAE advice to patients with special considerations (CVD risk, T2DM; n = 145) | 80.9 (18.8); 78, 84 |
| Make appropriate PAE referrals to other qualified exercise professionals (n = 144) | 82.1 (21.9); 79, 86 |
| Help patients maintain PAE over the long term (n = 146) | 72.8 (25.0); 69, 77 |
| Patients will follow through on PAE recommendations (n = 141) | 66.3 (22.5); 63, 70 |
PAE = physical activity and exercise; CVD = cardiovascular disease; T2DM = Type 2 diabetes mellitus.
Physical activity counselling and exercise prescription: barriers and facilitators
As shown in Table 2, the barriers with the highest impact (impact rating out of 4) preventing PAE counselling and exercise prescription were the participants’ perception of their patients’ interest (2.4; SD 0.7) and their perception of their patients’ preference for medication management (2.1; SD 0.7). They rated the impact of other lifestyle changes being more important as 1.9 (SD 0.6). The impact of lack of time and lack of guidance or resources were 1.8 (SD 0.6) and 1.7 (SD 0.6), respectively. The facilitators with the highest impact (impact rating out of 4) assisting the participants in including PAE in their patient treatment sessions were their patients’ perceived readiness to do PAE (3.5; SD 0.7), their own personal comfort with including PAE (3.3; SD 0.7), and their patients’ perceived expectation or interest in PAE (3.3; SD 0.8). (See Table 3.)
Table 2 .
Perceived Impact of Barriers that Prevent Physical Activity Counselling and Exercise Prescription* (N = 146)
| Barrier | Identified, n (%) | Impact; mean (SD) |
|---|---|---|
| Patient not interested in exercise | 131 (90) | 2.36 (0.68) |
| Other lifestyle changes more important | 125 (86) | 1.87 (0.57) |
| Lack of time | 124 (85) | 1.79 (0.62) |
| Personal knowledge | 119 (82) | 1.39 (0.50) |
| Lack of guidance in exercise or resources for those with chronic disease | 117 (80) | 1.70 (0.62) |
| Lack of evidence for effectiveness of exercise | 113 (77) | 1.19 (0.40) |
| Patients prefer medication management | 112 (77) | 2.11 (0.66) |
| Lack of exercise education at professional school | 83 (57) | 1.29 (0.48) |
| Lack of appropriate billing structure | 61 (42) | 1.52 (0.72) |
Out of 4, where 4 = completely prevents physiotherapist from providing physical activity and exercise counselling.
Table 3 .
Perceived Impact of Facilitators that Promote Physical Activity Counselling and Exercise Prescription* (N = 146)
| Facilitator | Identified, n (%) of respondents | Impact; mean (SD) |
|---|---|---|
| Patient expectation or interest in physical activity | 129 (88) | 3.27 (0.75) |
| Patient having greater readiness to do physical activity and/or exercise | 127 (87) | 3.50 (0.67) |
| Having physical activity and exercise programmes in the community to refer to | 127 (87) | 3.11 (0.70) |
| Readily available resource supports and tools (pamphlets, Web sites) | 127 (87) | 2.90 (0.81) |
| Personal comfort and confidence in the subject area | 126 (86) | 3.33 (0.69) |
| Availability of continuing education opportunities | 126 (86) | 2.69 (0.73) |
| Having exercise facilities in the community | 125 (86) | 3.14 (0.65) |
| Flexibility in booking or scheduling patients | 111 (76) | 2.95 (0.75) |
| Other qualified exercise professionals available to refer to as needed | 108 (74) | 2.86 (0.91) |
| Support of practice group, management, manager or organization | 105 (72) | 2.95 (0.79) |
| Administrative assistance (EMR integration of PA or billing codes) | 55 (38) | 2.51 (1.00) |
Out of 4, where 4 = makes it very easy to provide physical activity and exercise counselling.
EMR = electronic medical record; PA = physical activity.
Comfort and discomfort with providing physical activity advice to special populations
On average, the respondents reported 6.1 (SD 3.0) conditions they were most comfortable providing PAE advice about and 2.2 (SD 1.8) conditions they were least comfortable providing PAE advice about (see Table 4). They were most comfortable providing PAE advice to patients with osteoarthritis (88% of respondents) and patients with other musculoskeletal disorders (86%). They were least comfortable providing PAE advice to patients with cancer (49%), followed by patients with insulin requiring diabetes (33%) and those with respiratory disease (32%).
Table 4 .
Self-Reported Level of Comfort in Providing Physical Activity and Exercise (PAE) Advice to Patients with Disease (N = 146)
| Disease |
n (%) of respondents |
|
|---|---|---|
| Highest level of comfort | Lowest level of comfort | |
| Cancer | 39 (27) | 72 (49) |
| Cardiovascular disease | 85 (58) | 33 (23) |
| Diabetes (requiring insulin or secretagogue) | 58 (40) | 48 (33) |
| Diabetes (not requiring insulin or secretagogue) | 73 (50) | 24 (16) |
| Hypertension | 81 (55) | 21 (14) |
| Mental health | 50 (34) | 41 (28) |
| Obesity | 96 (66) | 9 (6) |
| Osteoarthritis | 129 (88) | 4 (3) |
| Osteoporosis | 96 (66) | 14 (10) |
| Other musculoskeletal (e.g. low back pain) | 125 (86) | 5 (3) |
| Respiratory | 57 (39) | 46 (32) |
Note: On average, physiotherapists reported 6.1 (SD 3.0) responses for conditions they were most comfortable providing PAE advice about and 2.2 (SD 1.8) responses for conditions they were least comfortable providing PAE advice about.
Discussion
The purpose of this study was to assess the perceptions and practices of PAE counselling and prescription of physiotherapists across Nova Scotia. Our results indicate that physiotherapists frequently discussed PAE and often provided their patients with written PAE prescriptions. They perceived themselves as both knowledgeable and confident in their ability to provide PAE counselling and prescribe exercise to the majority of their patients. They identified patient-focused barriers that might discourage them from engaging their clients in PAE counselling and prescription, but they also identified personal comfort with, and knowledge of, PAE counselling and prescription as facilitators of engaging clients in PAE counselling and prescription. The patients to whom they felt least comfortable giving advice were those with cancer, insulin requiring diabetes, and respiratory disease. Given that the majority of participants indicated being interested in receiving further PAE education or training, future research should explore the need for educational opportunities in this area. Education and training should focus on behaviour change strategies that would help physiotherapists encourage patients to engage in more PAE and follow through on their PAE recommendations.
Physiotherapists are in an optimal position to promote PAE because they have knowledge of exercise prescription and are on the front line of patient contact. Their rates of assessing and recommending PAE to patients were much higher than those reported by physicians across Canada.17 The physiotherapists in this study also revealed that they felt very comfortable providing PAE advice to patients with several disease conditions. A greater proportion of physiotherapists in our study described their knowledge of PAE counselling as very high (82%) compared with previously published samples of physicians (9%; n = 113) and non-physiotherapy allied health professionals (13%; n = 54), from across Canada.17
Interesting too is our finding that 71% of the physiotherapists surveyed were keen to pursue further education or training in PAE counselling and exercise prescription. The results of our study suggest that this interest may be related to the barriers identified by the respondents, an area explored by few studies in the literature.16 The barriers they identified as having the most impact were their patients’ perceived lack of interest in PAE and perceived preference for medication management. Lack of time had comparatively less impact, a finding that contrasts with some previous literature.12,15 A study evaluating the perception of the physiotherapists’ role in treating individuals in Canada noted that the most significant barriers preventing clients with obesity from following through with a PAE programme was their lack of motivation and lack of ability to self-identify obesity management as a goal.23
Patients’ disinterest in PAE has been cited as a primary barrier to promoting PAE by other Canadian health care providers.17–19 Certainly, health care providers’ perception of their patients’ interest in exercise influences their routine clinical care, yet this perception is modifiable. A previous study demonstrated that a training workshop on PAE prescription was effective at reducing the barrier of patient disinterest when physicians were followed up 3 months later.18 Previous research on diabetes educators showed that providing education and resources improved the providers’ confidence in their patients to be physically active and improved their patients’ perceived PA knowledge.21 Future research should evaluate the effects of education and training on the challenge that physiotherapists perceive they face and, in particular, their perception of their patients’ willingness to exercise.
Our study participants were confident (81%) in providing advice to individuals with special considerations (chronic health conditions). They identified that they were most comfortable providing PAE advice to patients with osteoarthritis and other musculoskeletal disorders and least comfortable providing PAE advice to those with cancer, insulin requiring diabetes, and respiratory disease. Other research has also reported that Canadian physiotherapists might have less confidence in providing key aspects of care to patients with diabetes.24 Considering that the rates of cancer, diabetes, and cardiovascular disease are higher in Nova Scotia compared with the rest of Canada3 and that physicians are less accessible in Nova Scotia compared with other provinces,25 physiotherapists may play an important role in promoting PAE to these special populations.
Our questionnaire did not ask about the participants’ level of comfort with these conditions; it questioned only which conditions they were least comfortable with. Altogether, our findings advocate for promoting physiotherapists’ role in providing PAE counselling and prescription to individuals with and without special conditions. Given that most physiotherapists in this survey were interested in more education, it would be useful for a future study to review to what extent these topics are addressed in Canadian entry-to-practice programmes and continuing education, as well as how effective they are; the resulting information could influence future educational initiatives. Most physiotherapists had already adopted PAE promotion strategies as part of their regular practice: they assessed the readiness of, and prescribed exercise to, a high proportion of their patients. Like the toolkit used by diabetes educators,21 a toolkit specific to physiotherapists, consisting of resources aimed at overcoming barriers and assisting them in providing advice and prescribing exercise to special populations might be useful.
One way to help physiotherapists and other health care providers provide ongoing exercise management to patients with chronic disease is increasing the availability of affordable exercise programmes, facilities, and professionals in the community to whom physiotherapists can refer their patients. Our participants identified a high level of confidence in referring their patients to other programmes and professionals (82%), but they referred less frequently (27% of patient appointments). There could be several reasons for this; for example, perhaps few other exercise professionals, community programmes, or facilities are accessible to most of the Nova Scotia population. Thus, physiotherapists may be interested in referring to other professionals and programmes more often but are either unaware of what options there are or know that there are no options. Similar challenges were identified by physiotherapists treating people with stroke in Ontario; the most frequently cited barriers to educating patients about exercise were a perceived lack of suitable programmes (53.2%) and a lack of awareness of local community-based exercise programmes (23.8%).13
Considering physiotherapists’ awareness of the challenges for patients to follow through and maintain PAE levels, cost-effective community programmes are needed that physiotherapists and other providers can refer their patients to. In addition, collaborating with other qualified exercise professionals may help with patient follow-up, ongoing exercise management, and patient adherence, especially for those with chronic disease and conditions of aging, which need more individual modification.
Qualified exercise professionals are those who have the education, scope of practice, and liability insurance to work with healthy individuals and those with chronic disease; examples are certified personal trainers (CPTs) and exercise physiologists (CEPs), both certified by the Canadian Society for Exercise Physiology (CSEP), and registered kinesiologists (RKin) in Ontario. CSEP CPTs have the training and scope to work with individuals with a stable medical condition who are able to exercise independently, such as those with obesity, diabetes, heart disease, hypertension, or osteoarthritis. CSEP CEPs and RKins have the training and scope to work with individuals with multiple comorbidities, the conditions just mentioned, and cancer, respiratory conditions, osteoporosis, and other musculoskeletal conditions. However, such professionals are only beginning to be included as part of family health teams in Ontario.26 These qualified exercise professionals may not be covered through provincially or privately funded insurance programmes in other provinces such as Nova Scotia, and this fee-for-service approach can be a deterrent to patient referrals and considered a barrier to access.
This study highlights the current practices of physiotherapists in Nova Scotia and the underlying confidence with and barriers to promoting PAE counselling and prescription as part of treating their patients. Integrating PAE into physiotherapy practice as a vital component of patient health care cannot be achieved solely through physician-delivered interventions; rather, a multidisciplinary approach needs to be developed that fosters collaboration among all health care providers. Physiotherapists who have expertise in exercise prescription, can join other allied health professionals in delivering a consistent message to help all patients achieve an active lifestyle. Although encouraging physical activity and general exercise may not be the primary focus of some physiotherapists’ daily treatment practices, they are in an ideal position to promote the importance of adopting a physically active lifestyle to ease the health care burden of excessively high rates of inactivity.
This study has several limitations. First, as with all survey studies, the respondents might have answered questions in a socially desirable way; reporting higher rates of, knowledge of, and confidence in providing PAE counselling and prescription. Second, although our respondents are representative of those physiotherapists practicing in Nova Scotia,22 our results may not be representative of all Canadian physiotherapists. However, this is the first Canadian study of its kind, and there are likely similarities in physical therapy education and practice among the provinces and territories. Third, the estimated response rate (24%) is somewhat low, but this is consistent with other e-mail-based survey studies.27
Moreover, there may be differences in physiotherapists’ knowledge, confidence and prescribing practices if they specialize in certain disease areas (e.g., neurology, respiratory) and differences between those working in a rural versus urban settings. These differences may warrant further investigation but were beyond the scope of this Nova Scotia survey. In addition, our physiotherapist participants primarily worked in a general practice setting or with people with musculoskeletal disorders (75%). Although most PTs (83%) across Nova Scotia report working in these two areas of practice,22 the challenges they identified (barriers and referral rates) may not be representative of all physiotherapists in all areas of practice. Finally, our survey did not define general practice, and it is possible that physiotherapists who identified working in a general practice setting see patients with various health conditions but mostly those with a musculoskeletal issue.
Conclusion
The physiotherapists in Nova Scotia who responded to our questionnaire, frequently included PAE counselling and prescription and were confident performing many aspects of PAE promotion as part of their clinical practice. Consistent with other Canadian health care providers, they experienced patient-focused barriers that might discourage PAE counselling, prescription, and referral, such as perceiving that their patients lacked interest in PAE. The availability of community-based exercise programmes and qualified exercise professionals may help to support patient engagement with ongoing exercise, as well as PAE education for physiotherapists in training and practice. This education should include behavioural approaches to help patients overcome barriers, and it should target the disease conditions about which physiotherapists report being the least comfortable providing advice (cancer, diabetes, and respiratory diseases). Future research can determine the effectiveness of such educational interventions on physiotherapy clinical practice.
Key Messages
What is already known on this topic
There are undisputed health benefits to leading a physically active lifestyle, but most Canadians do not meet the current physical activity guidelines. Physicians and nurses have low confidence in, knowledge of, and experience in providing physical activity and exercise (PAE) counselling. Physiotherapists are educated in, and aware of, the benefits of PAE, and often recommend PAE to their patients, but their specific perceptions of and practices in providing PAE counselling and prescription as part of their regular patient treatment is largely understudied in Canada.
What this study adds
Physiotherapists working in Nova Scotia identify challenges in helping patients maintain PAE; like other providers, they also perceive patients’ disinterest in PAE as the greatest barrier to PA promotion, but they rate the impact of barriers lower than other physician-focused studies. Most physiotherapists are interested in further PAE education or training and identify that such training should include behavioural strategies to help patients overcome barriers to being active and include the disease states about which they feel least comfortable providing advice on (e.g., cancer, diabetes, respiratory conditions).
Appendix: Screenshot of Example Questions
References
- 1. McKinney J, Lithwick DJ, Morrison BN, et al. The health benefits of physical activity and cardiorespiratory fitness. BC Med J. 2016;58(3):131–7. [Google Scholar]
- 2. Colley RC, Garriguet D, Janssen I, et al. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011;22(1):7–14. Medline:21510585. [PubMed] [Google Scholar]
- 3. Nova Scotia health profile 2015 [Internet]. Halifax: Department of Public Health; 2015. [cited 2018. June 1]. Available from: https://novascotia.ca/dhw/publichealth/documents/Population-Health-Profile-Nova-Scotia.pdf. [Google Scholar]
- 4. Exercise is Medicine Canada [Internet]. Indianapolis (IN): American College of Sports Medicine; 2019. [cited 2018. June 1]. Available from: http://www.exerciseismedicine.org/canada. [Google Scholar]
- 5. Marcus BH, Goldstein MG, Jette A, et al. Training physicians to conduct physical activity counseling. Prev Med. 1997;26(3):382–8. 10.1006/pmed.1997.0158. Medline:9144763 [DOI] [PubMed] [Google Scholar]
- 6. Tulloch H, Fortier M, Hogg W. Physical activity counseling in primary care: who has and who should be counseling? Patient Educ Couns. 2006;64(1–3):6–20. 10.1016/j.pec.2005.10.010. Medline:16472959 [DOI] [PubMed] [Google Scholar]
- 7. Petrella RJ, Lattanzio CN, Overend TJ. Physical activity counseling and prescription among Canadian primary care physicians. Arch Intern Med. 2007;167(16):1774–81. 10.1001/archinte.167.16.1774. Medline:17846397 [DOI] [PubMed] [Google Scholar]
- 8. Rea BL, Hopp Marshak H, Neish C, et al. The role of health promotion in physical therapy in California, New York, and Tennessee. Phys Ther. 2004;84(6):510–23. 10.1093/ptj/84.6.510. Medline:15161417 [DOI] [PubMed] [Google Scholar]
- 9. Black B, Marcoux BC, Stiller C, et al. Personal health behaviors and role-modeling attitudes of physical therapists and physical therapist students: a cross-sectional study. Phys Ther. 2012;92(11):1419–36. 10.2522/ptj.20110037. Medline:22822236 [DOI] [PubMed] [Google Scholar]
- 10. Neil-Sztramko SE, Ghayyur A, Edwards J, et al. Physical activity levels of physiotherapists across practice settings: a cross-sectional comparison using self-report questionnaire and accelerometer measures. Physiother Can. 2017;69(2):152–60. 10.3138/ptc.2015-64. Medline:28539695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Canadian Physiotherapy Association. Description of physiotherapy in Canada 2012 [Internet]. Ottawa: The Association; 2012. [cited 2018. June 1]. Available from: https://physiotherapy.ca/sites/default/files/site_documents/dopen-en.pdf. [Google Scholar]
- 12. Shirley D, van der Ploeg HP, Bauman AE. Physical activity promotion in the physical therapy setting: perspectives from practitioners and students. Phys Ther. 2010;90(9):1311–22. 10.2522/ptj.20090383. Medline:20651009 [DOI] [PubMed] [Google Scholar]
- 13. Lau C, Chitussi D, Elliot S, et al. Facilitating community-based exercise for people with stroke: cross-sectional e-survey of physical therapist practice and perceived needs. Phys Ther. 2016;96(4):469–78. 10.2522/ptj.20150117. Medline:26294684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sheedy J, Smith B, Bauman A, et al. A controlled trial of behavioural education to promote exercise among physiotherapy outpatients. Aust J Physiother. 2000;46(4):281–9. 10.1016/s0004-9514(14)60289-0. Medline:11676813 [DOI] [PubMed] [Google Scholar]
- 15. Verhagen E, Engbers L. The physical therapist’s role in physical activity promotion. Br J Sports Med. 2009;43(2):99–101. 10.1136/bjsm.2008.053801. Medline:18838405 [DOI] [PubMed] [Google Scholar]
- 16. Jack K, McLean SM, Moffett JK, et al. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther. 2010;15(3):220–8. 10.1016/j.math.2009.12.004. Medline:20163979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O’Brien MW, Shields CA, Oh P, et al. Health care provider confidence and exercise prescription practices of Exercise is Medicine Canada workshop attendees. Appl Physiol Nutr Metab 2017;42(4);384–90. 10.1139/apnm-2016-0413. Medline:28177736 [DOI] [PubMed] [Google Scholar]
- 18. Fowles JR, O’Brien MW, Solmundson, et al. Exercise is Medicine Canada physical activity counselling and exercise prescription training improves counselling, prescription, and referral practices among physicians across Canada. Appl Physiol Nutr Metab. 2018;43(5):535–9. 10.1139/apnm-2017-0763. Medline:29316409 [DOI] [PubMed] [Google Scholar]
- 19. O’Brien M, Shields C, Crowell S, et al. The effects of previous educational training on physical activity counselling and exercise prescription practices among physicians across Nova Scotia: a cross-sectional study. Can Med Educ J. 2018;9(4):e35–345. Medline:30498542. [PMC free article] [PubMed] [Google Scholar]
- 20. Dillman CJ, Shields CA, Fowles JR, et al. Including physical activity exercise in diabetes management: diabetes educators’ perceptions of their own abilities the abilities of their patients. Can J Diab. 2010;34(3):218–26. 10.1016/s1499-2671(10)43010-5. [DOI] [Google Scholar]
- 21. Shields CA, Fowles JR, Dunbar P, et al. Increasing diabetes educators’ confidence in physical activity and exercise counselling: the effectiveness of the “Physical Activity and Exercise Toolkit” training intervention. Can J Diab. 2013;37(6):381–87. 10.1016/j.jcjd.2013.08.265. Medline:24321718 [DOI] [PubMed] [Google Scholar]
- 22. Nova Scotia College of Physiotherapists. Annual report for 2016 [Internet]. Smiths Cove (NS): The College; 2017. [cited 2018. Jun 1]. Available from: https://nsphysio.com/images/Annual_Reports/2016_Annual_Report.pdf. [Google Scholar]
- 23. You L, Sadler G, Majumdar S, et al. Physiotherapists’ perceptions of their role in the rehabilitation management of individuals with obesity. Physiother Can. 2012;64(2):168–75. 10.3138/ptc.2011-01. Medline:23450159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Doehring K, Durno S, Pakenham C, et al. Knowledge, attitudes, and current practices of Canadian physiotherapists in preventing and managing diabetes. Physiother Can. 2016;68(3):298–306.. 10.3138/ptc.2015-63. Medline:27909380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Doctors Nova Scotia. Road map to a stable physician workforce: recommendations to stabilize the physician workforce in Nova Scotia [Internet]. Dartmouth (NS): Doctors Nova Scotia; 2018. [cited 2019. Aug 11[. Available from: https://doctorsns.com/sites/default/files/2018-09/next-steps/Road-Map-to-a-Stable-Physician-Workforce_0.pdf. [Google Scholar]
- 26. Moore C, Lee J, Milligan J, et al. Physical activity as medicine among family health teams: an environmental scan of physical activity services in an interdisciplinary primary care setting. Appl Physiol Nutr Metab. 2015;40(3):302–5. 10.1139/apnm-2014-0387. Medline:25641026 [DOI] [PubMed] [Google Scholar]
- 27. Yun GW, Trumbo CW. Comparative response to a survey executed by post, e-mail, & web form. J Comput Mediat Commun. 2006;6(1):JCMC613. 10.1111/j.1083-6101.2000.tb00112.x. [DOI] [Google Scholar]


